- 1Mental Health Center, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Neurobiology, Affiliated Mental Health Center and Hangzhou Seventh People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 3NHC and CAMS Key Laboratory of Medical Neurobiology, MOE Frontier Science Center for Brain Science and Brain-machine Integration, School of Brain Science and Brain Medicine, Zhejiang University, Hangzhou, China
With the aging of the population, the prevalence of osteoporosis and multimorbidity is increasing. Patients with osteoporosis often experience varying levels of emotional distress, including anxiety and depression. However, few studies have explored the patterns of multiple conditions and their impact on patients’ emotional distress. Here, we conducted a network analysis to explore the patterns of multimorbidities and their impact on emotional distress in 13,359 Chinese Han patients with osteoporosis. The results showed that multimorbidity was prevalent in Chinese patients with osteoporosis and increased with age, and was more frequent in males than in females, with the most common pattern of multimorbidity being osteoporosis and essential (primary) hypertension. Finally, we found that patients’ emotional distress increased with the number of multimorbidities, especially in female patients, and identified eight multimorbidities with high correlation to patients’ emotional distress.
Introduction
The prevalence of osteoporosis is increasing as the population of China ages. Osteoporosis is a systemic skeletal disease that is age-related and characterized by progressive loss of bone mass. It leads to a serious impairment in health-related quality of life and causes a high economic burden, especially in the older people, making it a major public health concern (1–3). Globally, the prevalence of osteoporosis is 23.1% in women and 11.7% in men among those aged 15–105 years (4). In China, the prevalence in osteoporosis is 20.6% in women and 5.0% in men among those over 40 years of age (5).
Patients with osteoporosis often experience varying levels of emotional distress, including anxiety and depression (6, 7). Studies have found that high levels of anxiety or depression may be associated with lower bone mineral density (6, 8, 9). This association may be due to excessive inflammatory responses that disrupt the normal metabolism of bone (10). Additionally, alterations in emotion-related hormone levels, such as cortisol, 25-hydroxyvitamin D and parathyroid hormone, may also contribute to bone loss and the development of osteoporosis (11, 12).
Moreover, the risk of multiple conditions, including hypertension, diabetes, coronary heart disease, and other chronic or acute diseases, also increases with age (13, 14), and multiple conditions may increase the risk of anxiety and depression (15–17). This makes the clinical treatment and management of osteoporosis more complex. A study in the United States found that women with osteoporosis have more comorbidities and depression than those without osteoporosis (18). However, among the world’s largest ethnic group, the Chinese Han, few studies have explored the patterns of multiple conditions and their impact on emotional well-being of patients with osteoporosis.
In this study, we utilized diagnostic and psychometric data obtained from a large general tertiary hospital in Southwest China to explore the patterns of multiple conditions and their impact on the emotional distress of Chinese Han patients with osteoporosis using network analysis. Our aim is to improve the understanding and management of osteoporosis in clinical settings.
Methods
Data source
For this study, we collected clinical data from the electronic medical records (EMR) of Chinese Han patients with osteoporosis aged 50 or older who were hospitalized in nonpsychiatric departments between January 1, 2015 and December 31, 2020. The dataset contained 25,999 records, of which 70.8% (18,417) were unique patients, and included patient demographics such as age, sex and marital status, and diagnostic information classified according to the 10th revision of the International Statistical Classification of Diseases (ICD-10). In this study, we extracted the first three characteristics of the ICD codes from EMR to classify the multiple conditions classification of osteoporosis. Ultimately, 669 disease codes were extracted, including a variety of codes for both chronic and acute diseases. According to VDA Harrison et al. (19), this concurrence of multiple chronic or acute conditions in a patient is defined as multimorbidity. Based on this definition, we named any disease other than osteoporosis as multimorbidity and counted the number of multimorbidities, with no multimorbidity counted as 0. Among these recodes, 13,359 (51.4%) patients underwent psychological evaluation using the Huaxi Emotional-distress Index (HEI) on a voluntary basis on admission for all non-psychiatric patients and were included in this analysis. The HEI is a self-reported nine-item scale widely used to screen emotional distress (anxiety and/or depression) in non-psychiatric clinical settings in China. It has demonstrated good reliability and validity and has been applied in online and offline survey and intervention studies (20–23). We defined a total score ≥ 11 as clinically significant anxiety and/or depression (CSAD) based on the optimal cutoff score for the HEI (20).
Statistical analysis
Differences among groups were compared using t-test or χ2 test for quantitative or categorical variables, respectively. We evaluated risk factors for emotional distress in patients with osteoporosis, including sex, age, marital status, and number of multimorbidities from the EMR, by multivariable logistic regression analysis. We assessed statistical significance using a two-tailed alpha level of 0.05 with Stata v15.0 statistical software. To visualize variation, we created figures using EXCEL (Microsoft).
Network analysis
In this study, we used a network analysis method to explore the multimorbidity patterns in patients with osteoporosis. This method is effective in analyzing and visualizing complex networks of diseases by identifying highly connected individual nodes and specific communities of nodes (13, 20, 23). Each node in the network represents a disease. Larger node diameters indicate higher prevalence, while the darker colors indicate more relationships with other diseases. The lines between nodes represent significant associations between diseases, while thicker lines indicating stronger associations. We used a relative risk to measure the correlations between disease pairs, calculated as the observed prevalence (O) divided by the expected prevalence (E) of the disease pair (24–26). For one disease pair composed of A and B, we computed the expected prevalence (E) as the prevalence of disease A multiplied by the prevalence of disease B, i.e., expected prevalence (E) = prevalence of disease A × prevalence of disease B. We considered a correlation significant if relative risk (O/E) was greater than 1.0. Using disease pairs with significant correlations, we constructed a network of multimorbidities and explore and visualize the network maps using Gephi 0.10, an open source software.
Results
Demographic and clinical characteristics in patients with osteoporosis
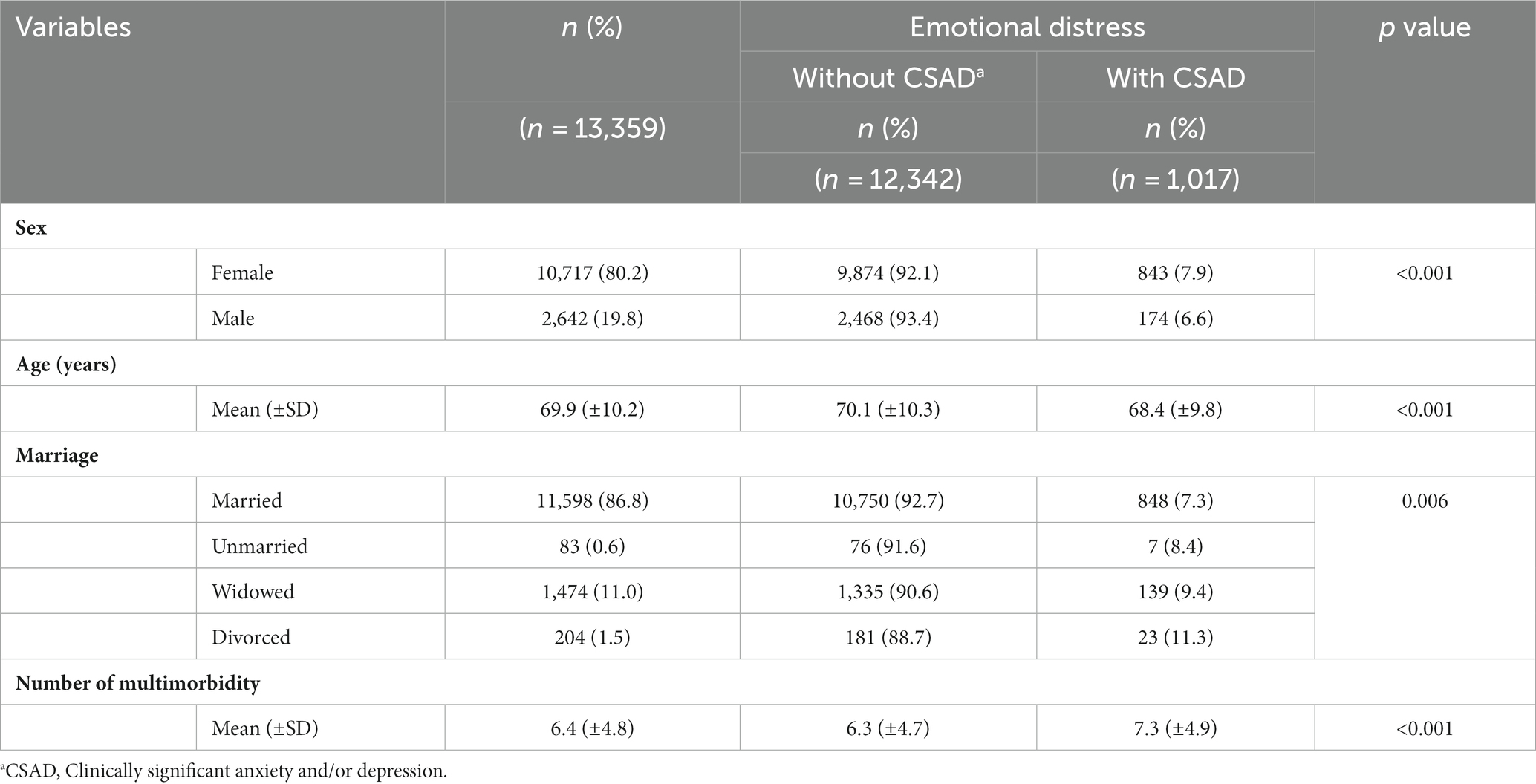
In this study, we included patients aged 50–101 years with an average age of 69.9 (SD = 10.2) years. Table 1 presents the demographic characteristics and emotional distress of the patients with osteoporosis. There were more female patients (10,717/13,359, 80.2%) than male patients (2,642/13,359, 19.8%). The prevalence of clinically significant anxiety and depression (CSAD) was higher among female patients, and married patients has the lowest CSAD rate. The prevalence of CSAD decreased with age but increased with the number of multimorbidities. All differences between groups were statistically significant (p < 0.05).
Distribution of multimorbidities
As shown in Table 1 and Figure 1A, nearly all patients (97.2%) had at least one multimorbidity, with an average number of 6.4 (SD = 4.8) multimorbidities ranging from 0 to 28. The most common pattern was having three multimorbidities. The average number of multimorbidities was approximately 1.4 times higher in male patients (8.3 ± 5.3) than in female patients (5.9 ± 4.5), and the number of multimorbidities increased with age (Figure 1B). Among male patients, the highest number of multimorbidities was five at 50–59 years, four at 60–69 years, six at 70–79 years, and seven at ≥80 years (Figure 1C). In female patients, the highest number of multimorbidities was three in all age groups, except for those aged ≥80 years, who had four (Figure 1D). Overall, the number of multimorbidities in male patients declined slowly compared to that in female patients, suggesting that the pattern of multimorbidities in male patients with osteoporosis was more complex than that in female patients.
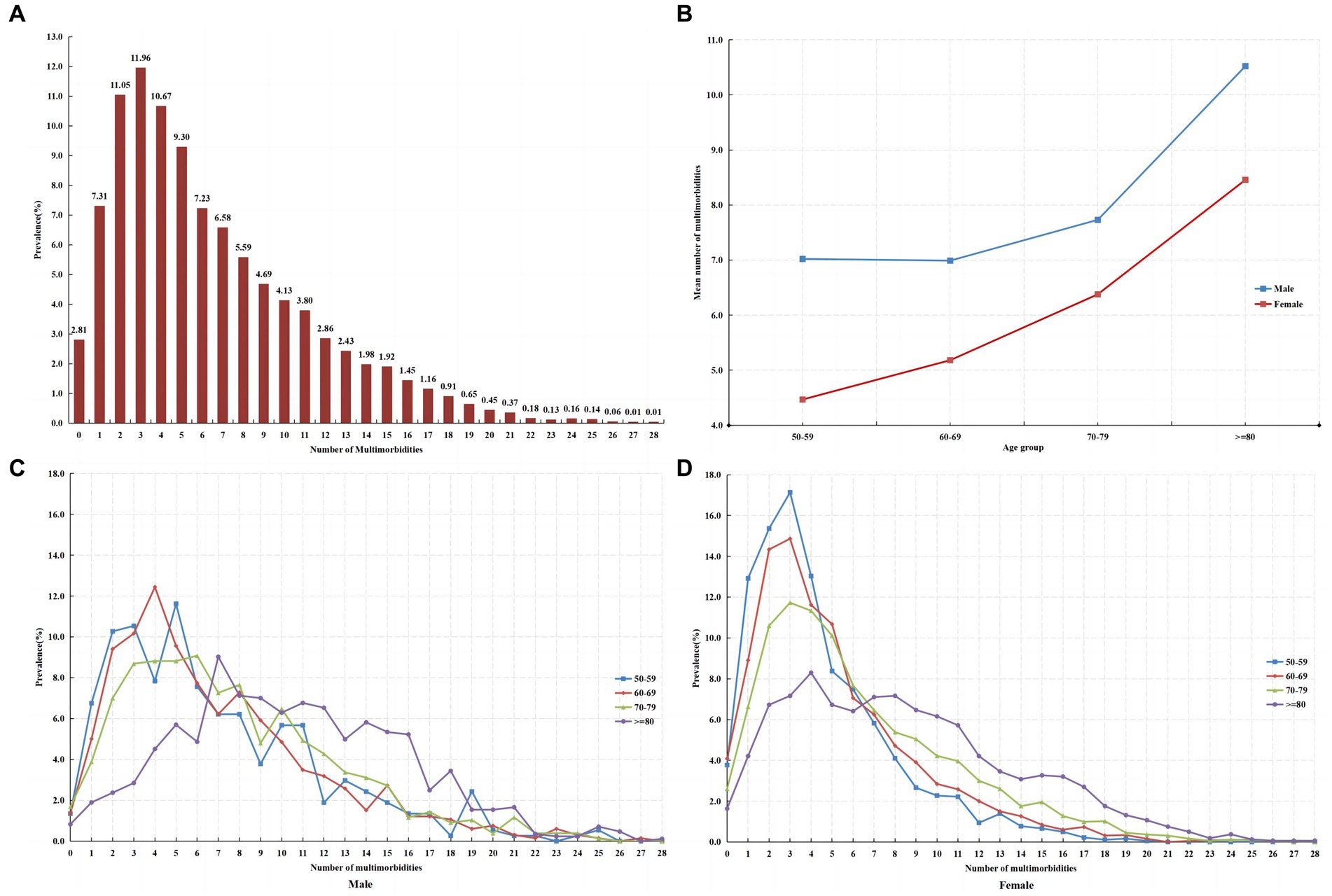
Figure 1. (A) The number of multimorbidities in patients with osteoporosis. (B) The average number of multimorbidities in patients with osteoporosis by age and sex. (C) The number of multimorbidities in male patients with osteoporosis by age group. (D) The number of multimorbidities in female patients with osteoporosis by age group.
Table 2 summarizes the 16 separate multimorbidities with a prevalence over 10.0% in patients with osteoporosis, and two or more separate multimorbidities co-occurrence with each other are shown by network analysis. The most common separate multimorbidity was essential (primary) hypertension with code I10 (5,869, 43.9%) across all sex and age groups. Among osteoporosis, 14 separate multimorbidities showed a significantly different prevalence between female and male patients. In female patients, the second and third most common separate multimorbidities were other intervertebral disk disorders (M51) and gonarthrosis [arthrosis of knee] (M17), while non-insulin-dependent diabetes mellitus (E11) and other chronic obstructive pulmonary disease (J44) were the second and third most common separate multimorbidities in male patients. Furthermore, it is evident that for most multimorbidities, prevalence increases with age. In addition to essential (primary) hypertension (I10), in patients aged 50–69 years, diseases of liver (K76), other intervertebral disk disorders (M51), and gonarthrosis [arthrosis of knee] (M17) were the major multimorbidities. For those aged 70–79 years, non-insulin-dependent diabetes mellitus (E11), other intervertebral disk disorders (M51), and gonarthrosis [arthrosis of knee] (M17) were the predominant multimorbidities. Lastly, in patients aged 80 years and older, other chronic obstructive pulmonary disease (J44), atherosclerosis (I70), and heart failure (I50) emerged as the major multimorbidities.
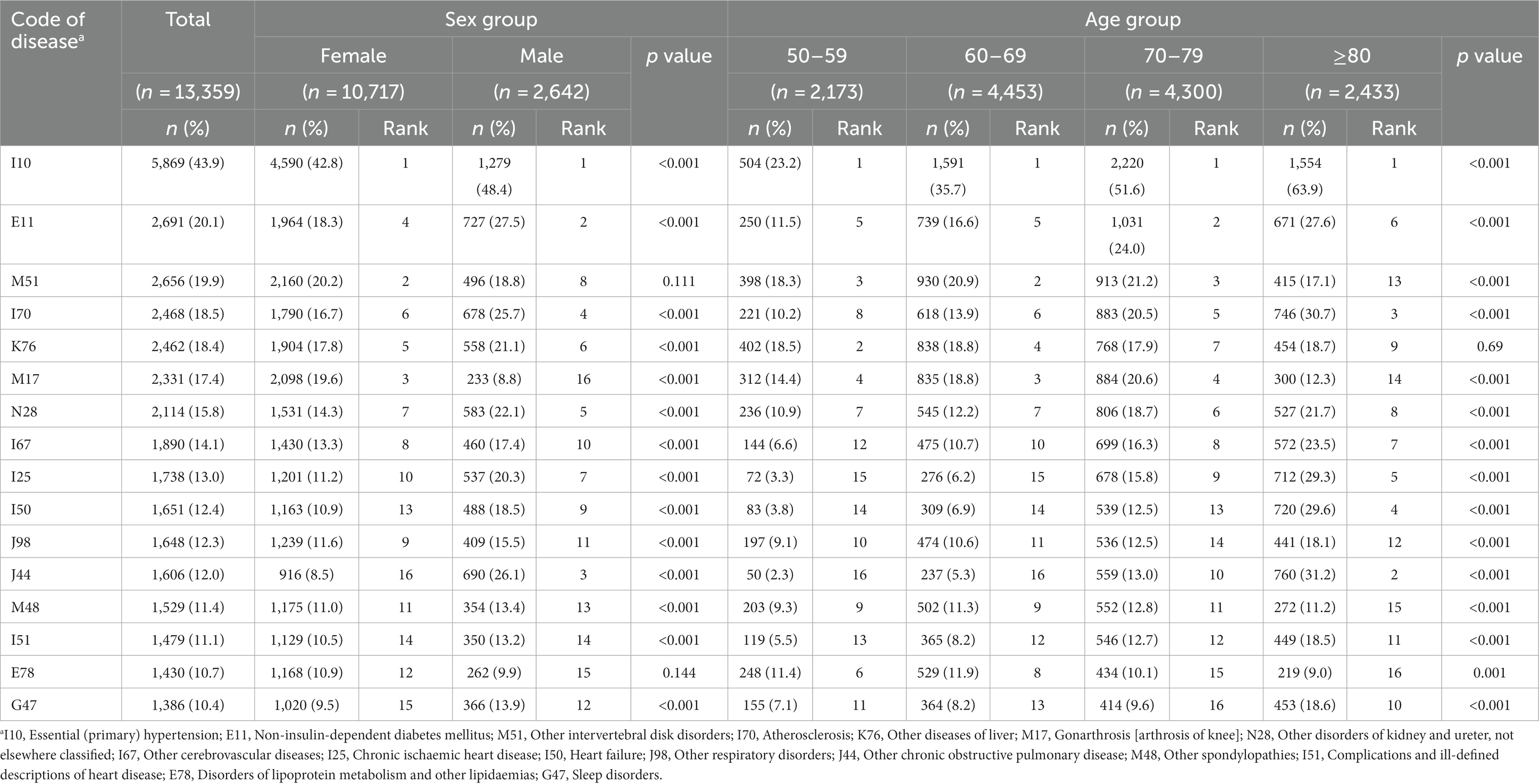
Table 2. Comparison of separate multimorbidities with a prevalence over 10% in patients with osteoporosis by sex and age groups.
Risk factors for emotional distress in patients with osteoporosis
According to Table 1, there were differences in both demographic information (including sex, age, and marital status) and the number of multimorbidities for emotional distress, so the multivariable logistic regression analysis included all of these variables in the model for analysis. And, given that females and males would typically have different multimorbidity patterns, we conducted further analyses for the female and male groups separately. Table 3 presents the odds ratios of selected risk factors associated with emotional distress (CSAD) in patients with osteoporosis. The findings indicate that the female patients have a 1.23 times higher risk of experiencing CSAD compared to male patients. In female patients, widowhood has been identified as a significant risk factor for CSAD, and the risk of CSAD increases in correlation with the number of multimorbidities. These risk factors have not been identified in male patients. In addition, for both female and male patients, the risk of CSAD decreases with age.
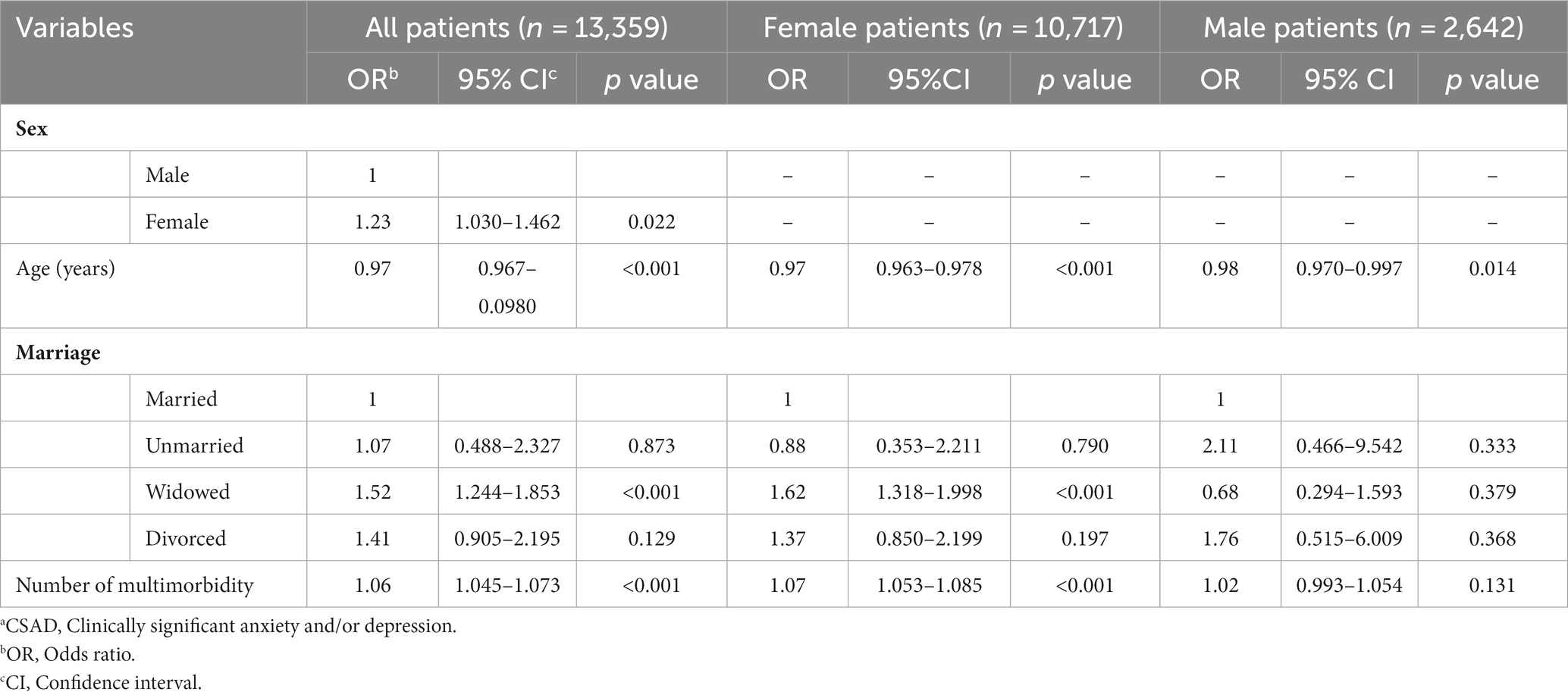
Table 3. Risk factors for emotional distress (CSADa) in patients with osteoporosis.
Multimorbidity network of osteoporosis
In this study, a total of 669 diseases were diagnosed alongside osteoporosis. Of these, diseases with a prevalence of multimorbidity greater than 1.0% and a relative risk (O/E) greater than 1.0 were incorporated into Gephi to create the osteoporosis multimorbidity map. This map consisted of 67 nodes, each representing a multimorbidity, and 407 links depicting the correlations between them, ultimately forming the osteoporosis multimorbidity network (Figure 2A).
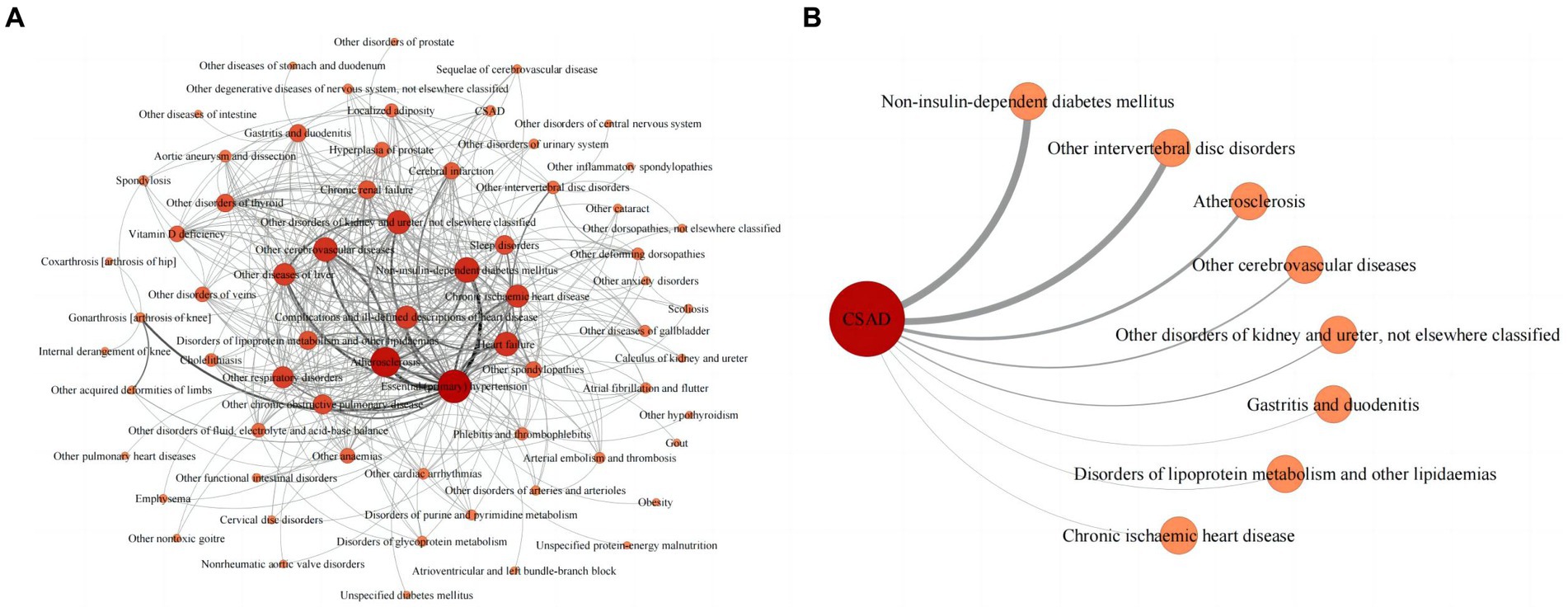
Figure 2. (A) Multimorbidity network in patients with osteoporosis. (B) CSAD* multimorbidity network in patients with osteoporosis. *CSAD, clinically significant anxiety and/or depression.
The strongest link within this network connected essential (primary) hypertension (I10) and non-insulin-dependent diabetes mellitus (E11), with 1,835 co-occurrences. The next strongest link joined essential (primary) hypertension (I10) and atherosclerosis (I70), with 1,483 co-occurrences. The network’s three most prevalence categories were diseases of the circulatory system (e.g., essential (primary) hypertension, atherosclerosis, heart failure, other cerebrovascular diseases, and chronic ischemic heart disease), diseases of the musculoskeletal system and connective tissue (e.g., other spondylopathies, other intervertebral disk disorders, other deforming dorsopathies, gonarthrosis [arthrosis of knee], and other acquired deformities of limbs), and endocrine, nutritional and metabolic diseases (e.g., non-insulin-dependent diabetes mellitus, disorders of lipoprotein metabolism and other lipidemias, other disorders of thyroid, vitamin D deficiency, and localized adiposity). Essential (primary) hypertension (I10) and atherosclerosis (I70) served as the central hubs of the multimorbidity network. Additionally, the study identified eight multimorbidities that demonstrated a strong correlation with patients’ emotional distress. The most strongly correlated multimorbidity was non-insulin-dependent diabetes mellitus (E11), with 247 co-occurrences (Figure 2B).
Discussion
In this study, we uncovered a high incidence of multimorbidities among patients with osteoporosis and identified a strong link between these multimorbidities and patients’ emotional distress. Utilizing network analysis, we determined common multimorbidities in osteoporosis and examined the interconnected relationships between them. Targeting these associated multimorbidities for specialized clinical interventions or clinical screening could benefit patients with osteoporosis.
The current study discovered that osteoporosis was more prevalent among female inpatients compared to male inpatients with osteoporosis. This sex disparity might be related to the higher occurrence of osteoporosis in females than in males. Previous studies, including those conducted in China, have also observed a higher prevalence of osteoporosis in females compared to males, which supports this observation (4, 5, 27).
In the evaluation of patients’ emotional distress, the prevalence of CSAD was found to be higher in female patients compared to male patients. Additionally, divorced, widowed, and unmarried patients exhibited a higher prevalence of CSAD than married patients. Regression analysis results indicated that female and widowhood were risk factors for CSAD, which aligns with previous findings that identified female, experiencing loss events, and poor social support as risk factors for anxiety or depression (28, 29).
Interesting, this study revealed that the prevalence of CSAD decreased with increasing age, and regression analysis identified advanced age as a protective factor for CSAD. Prior research on older adults suggests that this phenomenon may be due to improved emotional regulation and experience with age, as well as reduced stress reactivity to younger individuals, resulting in a smaller increase in negative emotions when faced with stressful events (30, 31). Similar phenomena have also been found in some disease-specific studies. For example, the study of irritable bowel syndrome (IBS) patients found that younger people had higher levels of anxiety and depression than older people (32), and the study of systemic lupus erythematosus (SLE) patients found that those who had the disease at a younger age had a higher risk of future depression (33). On the other hand, there were also some studies found that the risk of people suffering from anxiety or depression increases with age, as they experience more somatic illnesses and have less social support from important family members and friends (34–36). To our knowledge, few studies have examined this age-related difference in negative emotions among patients with osteoporosis. Furthermore, this study found that the patients with CSAD had a shorter average age and a higher average number of multimorbidities compared to patients without CSAD. These findings contribute additional evidence to the understanding of how emotional distress negatively impacts life expectancy and health status, highlighting the importance of addressing these issues during clinical treatment (37–40).
In analyzing multimorbidity among patients, this study observed that the number of multimorbidities increased with age, aligning with previous studies (41, 42). We also discovered that 97.2% of patients with osteoporosis had at least one multimorbidity, slightly higher than the results from a survey of osteoporosis patients in Germany, where over 95% of adults with osteoporosis had at least one comorbidity (1). This highlights high prevalence of multimorbidity among patients with osteoporosis, which requires attention. Moreover, we found that although the prevalence of osteoporosis was higher in female patients, male patients had more multimorbidities than that in female patients. This is consistent with the finding reported by Wang et al. (43), which reported a higher average number of multimorbidities in male inpatients in Chengdu, China. However, some studies have reported the opposite (41), suggesting that the inconsistency may be due to variations in observed diseases and the sample age ranges, which warrant further investigation.
In addition, this study found that female osteoporosis patients had a higher prevalence of CSAD and a lower number of multimorbidities compared to male osteoporosis patients. This is consistent with previous studies, which have found that females are more likely to suffer from anxiety or depression than males (44–46). Moreover, the results of the regression analysis showed that the number of multimorbidities significantly increased the risk of CSAD in female osteoporosis patients but not in male osteoporosis patients. This suggests that better management of multimorbidities in female patients would likely benefit female patients more.
Network analysis results demonstrated connections between osteoporosis and hypertension, diabetes, atherosclerosis, and other diseases across several systems, consistent with previous multimorbidity studies on osteoporosis (1, 41, 47). This supports the notion that osteoporosis is a systematic disease that often coexists with various common disorders in older individuals. Notably, this study was the first to identify eight somatic diseases strongly associated with emotional distress in patients with osteoporosis (Figure 2B). In clinical practice, focusing on the screening and management of these multimorbidities and implementing comprehensive intervention strategies can promote disease recovery and reduce emotional distress in patients with osteoporosis.
Limitations
This study had several limitations. Firstly, as a single-center study, it relied on data from a large general tertiary hospital, with patients primarily from Southwest China, making the results regional-specific. Secondly, all data of the study were obtained from the EMR, which covers a wide range of disease types. Therefore, we assessed patients’ multimorbidity status using only disease counts, rather than using tools that include a limited number of disease categories that do not cover the types of diseases involved in this study, such as the Charlson Comorbidity Index, which includes 19 conditions and is widely used to measure patients’ comorbidity/multimorbidity status (48). Thirdly, due to the retrospective cross-sectional nature of the study based on patients’ hospitalization data, the sequence and risk factors for the occurrence of individual diseases were not investigated, and there was a deficiency of information on patients’ quality of life and disease prognosis, which made it unachievable to infer the causal relationship between individual diseases and different clusters of multimorbidity and to assess the specific impact of multimorbidity on patients. In light of these limitations, future research should investigate the quality of life and disease prognosis in patients with osteoporosis to better understand the impact of multimorbidity. Additionally, efforts should be made to analyze the differences in multimorbidities and to incorporate multimorbidity data to predict prognostic outcomes.
Conclusion
This study examined emotional distress and investigated multimorbidities patterns using network analysis in patients with osteoporosis. The findings revealed that multimorbidities were prevalent among patients and increased with age. Significant differences in emotional distress and the majority of the multimorbidities were observed across sex and age groups. Emotional distress in patients decreased with age and increased with the number of multimorbidities, especially in female patients. The most common patterns of multimorbidity among patients with osteoporosis was osteoporosis and essential (primary) hypertension, while non-insulin-dependent diabetes, other intervertebral disk diseases and atherosclerosis were also major multimorbidities and strongly correlated with patients’ emotional distress. These results offer valuable insight for enhancing the prevention and management of multimorbidities and emotional distress in osteoporosis patients, ultimately contributing to an improved quality of life for those affected.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of West China Hospital, Sichuan University, Chengdu, Sichuan, China. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because The Ethics Committee waived the requirement for consent because the study is a retrospective analysis of routinely collected administrative data.
Author contributions
HW, QX, and TL: conceptualization, methodology, validation, and writing—original draft. ZD, WG, WD, LZ, and WK: conceptualization, methodology, and writing—review. All authors contributed to the article and approved the submitted version.
Acknowledgments
We extend our gratitude to all colleagues who contributed to this study and to the members of the Collaborative Group of Sunshine Hospital Project in West China Hospital for their invaluable support and collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Puth, MT, Klaschik, M, Schmid, M, Weckbecker, K, and Munster, E. Prevalence and comorbidity of osteoporosis- a cross-sectional analysis on 10,660 adults aged 50 years and older in Germany. BMC Musculoskelet Disord. (2018) 19:144. doi: 10.1186/s12891-018-2060-4
2. Weng, SF, Hsu, HR, Weng, YL, Tien, KJ, and Kao, HY. Health-related quality of life and medical resource use in patients with osteoporosis and depression: a cross-sectional analysis from the National Health and nutrition examination survey. Int J Environ Res Public Health. (2020) 17:1124. doi: 10.3390/ijerph17031124
3. Bahouq, H, and Soulaymani, A. Depression, quality of life, and self-esteem of Moroccan postmenopausal women with osteoporosis before the occurrence of fractures. J Menopausal Med. (2020) 26:121–9. doi: 10.6118/jmm.19008
4. Salari, N, Ghasemi, H, Mohammadi, L, Behzadi, MH, Rabieenia, E, Shohaimi, S, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. (2021) 16:609. doi: 10.1186/s13018-021-02772-0
5. Wang, L, Yu, W, Yin, X, Cui, L, Tang, S, Jiang, N, et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open. (2021) 4:e2121106. doi: 10.1001/jamanetworkopen.2021.21106
6. Catalano, A, Martino, G, Bellone, F, Gaudio, A, Lasco, C, Langher, V, et al. Anxiety levels predict fracture risk in postmenopausal women assessed for osteoporosis. Menopause. (2018) 25:1110–5. doi: 10.1097/GME.0000000000001123
7. Keshishi, D, Makunts, T, and Abagyan, R. Common osteoporosis drug associated with increased rates of depression and anxiety. Sci Rep. (2021) 11:23956. doi: 10.1038/s41598-021-03214-x
8. Jacka, FN, Pasco, JA, Henry, MJ, Kotowicz, MA, Dodd, S, Nicholson, GC, et al. Depression and bone mineral density in a community sample of perimenopausal women: Geelong osteoporosis study. Menopause. (2005) 12:88–91. doi: 10.1097/00042192-200512010-00015
9. Drosselmeyer, J, Rapp, MA, Hadji, P, and Kostev, K. Depression risk in female patients with osteoporosis in primary care practices in Germany. Osteoporos Int. (2016) 27:2739–44. doi: 10.1007/s00198-016-3584-9
10. Pitsavos, C, Panagiotakos, DB, Papageorgiou, C, Tsetsekou, E, Soldatos, C, and Stefanadis, C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study. Atherosclerosis. (2006) 185:320–6. doi: 10.1016/j.atherosclerosis.2005.06.001
11. Kashfi, SS, Abdollahi, G, Hassanzadeh, J, Mokarami, H, and Khani, JA. The relationship between osteoporosis and depression. Sci Rep. (2022) 12:11177. doi: 10.1038/s41598-022-15248-w
12. Hong-Jhe, C, Chin-Yuan, K, Ming-Shium, T, Fu-Wei, W, Ru-Yih, C, Kuang-Chieh, H, et al. The incidence and risk of osteoporosis in patients with anxiety disorder: a population-based retrospective cohort study. Medicine (Baltimore). (2016) 95:e4912. doi: 10.1097/MD.0000000000004912
13. Gu, J, Chao, J, Chen, W, Xu, H, Wu, Z, Chen, H, et al. Multimorbidity in the community-dwelling elderly in urban China. Arch Gerontol Geriatr. (2017) 68:62–7. doi: 10.1016/j.archger.2016.09.001
14. Almagro, P, Ponce, A, Komal, S, de la Asuncion, VM, Castrillo, C, Grau, G, et al. Multimorbidity gender patterns in hospitalized elderly patients. PLoS One. (2020) 15:e0227252. doi: 10.1371/journal.pone.0227252
15. Farooq, S, Khan, T, Zaheer, S, and Shafique, K. Prevalence of anxiety and depressive symptoms and their association with multimorbidity and demographic factors: a community-based, cross-sectional survey in Karachi, Pakistan. BMJ Open. (2019) 9:e029315. doi: 10.1136/bmjopen-2019-029315
16. Tong, L, Pu, L, Guo, X, Sun, M, Guo, F, Zhao, S, et al. Multimorbidity study with different levels of depression status. J Affect Disord. (2021) 292:30–5. doi: 10.1016/j.jad.2021.05.039
17. Gould, CE, O’Hara, R, Goldstein, MK, and Beaudreau, SA. Multimorbidity is associated with anxiety in older adults in the health and retirement study. Int J Geriatr Psychiatry. (2016) 31:1105–15. doi: 10.1002/gps.4532
18. O’Malley, CD, Tran, N, Zapalowski, C, Daizadeh, N, Olenginski, TP, and Cauley, JA. Multimorbidity in women with and without osteoporosis: results from a large US retrospective cohort study 2004-2009. Osteoporos Int. (2014) 25:2117–30. doi: 10.1007/s00198-014-2740-3
19. Harrison, C, Fortin, M, van den Akker, M, Mair, F, Calderon-Larranaga, A, Boland, F, et al. Comorbidity versus multimorbidity: why it matters. J Multimorb Comorb. (2021) 11:2633556521993993. doi: 10.1177/2633556521993993
20. Wang, J, Guo, WJ, Zhang, L, Deng, W, Wang, HY, Yu, JY, et al. The development and validation of Huaxi emotional-distress index (HEI): a Chinese questionnaire for screening depression and anxiety in non-psychiatric clinical settings. Compr Psychiatry. (2017) 76:87–97. doi: 10.1016/j.comppsych.2017.04.001
21. Dong, ZQ, Ma, J, Hao, YN, Shen, XL, Liu, F, Gao, Y, et al. The social psychological impact of the COVID-19 pandemic on medical staff in China: a cross-sectional study. Eur Psychiatry. (2020) 63:e65. doi: 10.1192/j.eurpsy.2020.59
22. Kang, Y, Wang, H, Li, X, Tao, Y, Yang, X, Deng, W, et al. A brief web-based screening plus emotional-disorder health education was associated with improvement of mental health awareness and service-seeking attitudes among patients seeking nonpsychiatric clinical services in China. Depress Anxiety. (2021) 38:571–87. doi: 10.1002/da.23118
23. Chen, JL, Luo, R, and Liu, M. Prevalence of depression and anxiety and associated factors among geriatric orthopedic trauma inpatients: a cross-sectional study. World J Clin Cases. (2022) 10:919–28. doi: 10.12998/wjcc.v10.i3.919
24. Marengoni, A, Rizzuto, D, Wang, HX, Winblad, B, and Fratiglioni, L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. (2009) 57:225–30. doi: 10.1111/j.1532-5415.2008.02109.x
25. Mu, XM, Wang, W, Jiang, YY, and Feng, J. Patterns of comorbidity in hepatocellular carcinoma: a network perspective. Int J Environ Res Public Health. (2020) 17:3108. doi: 10.3390/ijerph17093108
26. Zhang, R, Lu, Y, Shi, L, Zhang, S, and Chang, F. Prevalence and patterns of multimorbidity among the elderly in China: a cross-sectional study using national survey data. BMJ Open. (2019) 9:e024268. doi: 10.1136/bmjopen-2018-024268
27. Kanis, JA, Norton, N, Harvey, NC, Jacobson, T, Johansson, H, Lorentzon, M, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. (2021) 16:82. doi: 10.1007/s11657-020-00871-9
28. Hubbard, G, den Daas, C, Johnston, M, and Dixon, D. Sociodemographic and psychological risk factors for anxiety and depression: findings from the Covid-19 health and adherence research in Scotland on mental health (CHARIS-MH) cross-sectional survey. Int J Behav Med. (2021) 28:788–800. doi: 10.1007/s12529-021-09967-z
29. Cho, SM, Saw, YM, Saw, TN, Than, TM, Khaing, M, Khine, AT, et al. Prevalence and risk factors of anxiety and depression among the community-dwelling elderly in Nay Pyi Taw union territory, Myanmar. Sci Rep. (2021) 11:9763. doi: 10.1038/s41598-021-88621-w
30. Sliwinski, MJ, Almeida, DM, Smyth, J, and Stawski, RS. Intraindividual change and variability in daily stress processes: findings from two measurement-burst diary studies. Psychol Aging. (2009) 24:828–40. doi: 10.1037/a0017925
31. Scott, SB, Ram, N, Smyth, JM, Almeida, DM, and Sliwinski, MJ. Age differences in negative emotional responses to daily stressors depend on time since event. Dev Psychol. (2017) 53:177–90. doi: 10.1037/dev0000257
32. Thakur, ER, Quigley, BM, El-Serag, HB, Gudleski, GD, and Lackner, JM. Medical comorbidity and distress in patients with irritable bowel syndrome: the moderating role of age. J Psychosom Res. (2016) 88:48–53. doi: 10.1016/j.jpsychores.2016.07.006
33. Maneeton, B, Maneeton, N, and Louthrenoo, W. Prevalence and predictors of depression in patients with systemic lupus erythematosus: a cross-sectional study. Neuropsychiatr Dis Treat. (2013) 9:799–804. doi: 10.2147/NDT.S44248
34. Belov, OO, and Pshuk, NG. Age and gender features of depressive and anxiety symptomatics of depressive disorders. Wiad Lek. (2020) 73:1476–9. doi: 10.36740/WLek202007130
35. Erdogan Yuce, G, Doner, A, and Muz, G. Psychological distress and its association with unmet needs and symptom burden in outpatient Cancer patients: a cross-sectional study. Semin Oncol Nurs. (2021) 37:151214. doi: 10.1016/j.soncn.2021.151214
36. Polikandrioti, M, Vasilopoulos, G, Koutelekos, I, Panoutsopoulos, G, Gerogianni, G, Alikari, V, et al. Depression in diabetic foot ulcer: associated factors and the impact of perceived social support and anxiety on depression. Int Wound J. (2020) 17:900–9. doi: 10.1111/iwj.13348
37. Lee, H, and Singh, GK. Psychological distress, life expectancy, and all-cause mortality in the United States: results from the 1997-2014 NHIS-NDI record linkage study. Ann Epidemiol. (2021) 56:9–17. doi: 10.1016/j.annepidem.2021.01.002
38. Rashedi, V, Ebrahimi, B, Sharif Mohseni, M, and Hosseini, M. Death anxiety and life expectancy among older adults in Iran. J Caring Sci. (2020) 9:168–72. doi: 10.34172/jcs.2020.025
39. Belialov, FI. Depression, anxiety, stress, and mortality. Ter Arkh. (2016) 88:116–9. Depressiia, trevoga, stress i smertnost’. doi: 10.17116/terarkh20168812116-119
40. Walker, RJ, Garacci, E, Campbell, JA, and Egede, LE. The influence of daily stress on glycemic control and mortality in adults with diabetes. J Behav Med. (2020) 43:723–31. doi: 10.1007/s10865-019-00109-1
41. Yao, SS, Cao, GY, Han, L, Chen, ZS, Huang, ZT, Gong, P, et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: results from the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. (2020) 75:1974–80. doi: 10.1093/gerona/glz185
42. Abad-Diez, JM, Calderon-Larranaga, A, Poncel-Falco, A, Poblador-Plou, B, Calderon-Meza, JM, Sicras-Mainar, A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. (2014) 14:75. doi: 10.1186/1471-2318-14-75
43. Wang, L, Qiu, H, Luo, L, and Zhou, L. Age- and sex-specific differences in multimorbidity patterns and temporal trends on assessing hospital discharge Records in Southwest China: network-based study. J Med Internet Res. (2022) 24:e27146. doi: 10.2196/27146
44. Melin, EO, Wanby, P, Neumark, T, Holmberg, S, Neumark, AN, Johansson, K, et al. Depression was associated with younger age, female sex, obesity, smoking, and physical inactivity, in 1027 patients with newly diagnosed type 2 diabetes: a Swedish multicentre cross-sectional study. BMC Endocr Disord. (2022) 22:273. doi: 10.1186/s12902-022-01184-3
45. Turen, S, and Turen, S. Gender differences in early complications after STEMI and their associations with anxiety and depression. Eur Rev Med Pharmacol Sci. (2023) 27:2936–45. doi: 10.26355/eurrev_202304_31925
46. Al-Owesie, RM, Moussa, NM, and Robert, AA. Anxiety and depression among traumatic spinal cord injured patients. Neurosciences (Riyadh). (2012) 17:145–50.
47. Nuno-Solinis, R, Rodriguez-Pereira, C, Alonso-Moran, E, and Orueta, JF. Comorbidity and healthcare expenditure in women with osteoporosis living in the Basque Country (Spain). J Osteoporos. (2014) 2014:205954. doi: 10.1155/2014/205954
Keywords: osteoporosis, multimorbidity, emotional distress, anxiety, depression
Citation: Wang H, Xia Q, Dong Z, Guo W, Deng W, Zhang L, Kuang W and Li T (2024) Emotional distress and multimorbidity patterns in Chinese Han patients with osteoporosis: a network analysis. Front. Public Health. 11:1242091. doi: 10.3389/fpubh.2023.1242091
Edited by:
Ozgur Karcioglu, Taksim Training and Research Hospital, TürkiyeReviewed by:
Tingyan Wang, University of Oxford, United KingdomLaura Downey, University of New South Wales, Australia
Copyright © 2024 Wang, Xia, Dong, Guo, Deng, Zhang, Kuang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weihong Kuang, a3doaGxqQDE2My5jb20=; Tao Li, bGl0YW96anVzY0B6anUuZWR1LmNu
 Huiyao Wang1
Huiyao Wang1 Wanjun Guo
Wanjun Guo Wei Deng
Wei Deng Weihong Kuang
Weihong Kuang Tao Li
Tao Li