- 1Biostatistics, Epidemiology and Scientific Computing Department, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
- 2Research Department, King Salman Center for Disability Research, Riyadh, Saudi Arabia
- 3SABIC Psychological Health Research & Applications Chair (SPHRAC), College of Medicine, King Saud University, Riyadh, Saudi Arabia
- 4National Center for Mental Health Promotion, Ministry of Health, Riyadh, Saudi Arabia
- 5Department of Psychiatry, Edrak Medical Center, Riyadh, Saudi Arabia
- 6Universitair Psychiatrisch Centrum - Katholieke Universiteit Leuven (UPC-KUL), Campus Gasthuisberg, Leuven, Belgium
- 7Psychiatry Department, King Fahd University Hospital, Khobar, Saudi Arabia
Introduction: Comorbidities of mental disorders and chronic physical conditions are a common medical burden reported among Western countries. National estimates of such comorbidities among the general population of Arab countries like Saudi Arabia are unknown. This study examined the prevalence of lifetime chronic physical conditions among the Saudi general population with DSM-IV 12-month mental disorders, and the associations with disability in the Kingdom of Saudi Arabia (KSA).
Methods: The Saudi National Mental Health Survey, a cross-sectional household study – part of the World Mental Health (WMH) Survey Consortium – was conducted between 2013–2016 in the KSA, with 4,001 Saudi citizens aged 15–65 (response rate 61%). The World Health Organization Composite International Diagnostic Interview 3.0 was used to assess prevalence of lifetime chronic physical conditions and 12-month mental disorders; disability was measured in terms of days out of role.
Results: The prevalence of any comorbid 12-month mental disorder among those with chronic physical conditions was 24%. Major depressive disorder, social phobia, and adult separation anxiety disorder were the most common comorbid mental disorders across all chronic physical conditions. Gender, education, income, urbanicity, region, and employment were associated with the presence of any chronic physical condition. Respondents with mental / physical comorbidities had 2.97 days out of role (on average) in the last 30 days.
Conclusion: Comorbidities of mental disorders and chronic physical conditions are common among Saudis. National efforts are needed to increase awareness of such comorbidities among the general population, and develop prevention and treatment services tailored to the needs of individuals at-risk for comorbidities.
1 Introduction
Medical comorbidity is a substantial and common societal burden, posing important challenges in terms of proper identification, prevention, and management strategies on the personal, clinical, and societal level. Comorbidity is usually defined as the presence of one or more additional diseases in a person diagnosed with an index-disease, i.e., a physical or mental condition (1, 2). However, such a co-presence does not imply that one disease is more central or severe than the other (3). Comorbidities between mental and physical disorders are commonly prevalent among general populations globally, regardless of the chronological order of onset, or the causal pathway linking the conditions (2, 4). For instance, individuals with chronic physical conditions are reported to have a higher prevalence of mental disorders than those without chronic physical conditions (2); the physical conditions were also more chronic when a mental disorder was present (5). The New Zealand Mental Health Survey found mental disorders among nearly 68% of individuals with medical conditions, particularly comorbidities related to high rates of depression and anxiety (6). The National Comorbidity Survey Replication in the United States found physical disorders among more than 68% of adults with a mental disorder and mental disorders among 29% of adults with a physical disorder (7). A meta-analysis reported that mental/physical comorbidities ranged from 19.0 to 68.1% in developing countries (8). Other global studies suggest an association between chronic pain conditions and mental disorders, including mood, anxiety, somatoform, substance use, and personality disorders (9–15). Such comorbidities have been largely linked to functional disability and significant loss of quality of life (10, 13).
The Arab world reports similar findings on mental/physical comorbidities (16). According to a study conducted in Aleppo, Syria, depression was higher in people with stroke and heart disease (17). In the context of the Kingdom of Saudi Arabia (KSA), up to 30% of patients with colorectal cancer meet criteria for major depressive disorder (18). Other Saudi studies suggest a strong association between depression and cardiovascular disease (19), high rates of anxiety and depression among children and adolescents with chronic pain conditions (20), with 71% of those with a pain condition related to a disease — such as cancer and osteoarthritis — meeting criteria of depression (21).
Specific sociodemographic risk factors for mental/physical comorbidity include: higher age, female gender, and lower education (22). Those with pain conditions in the KSA, who are financially discontent, are three times more likely to have depression compared to those who are financially content (21). Compared to other age groups, Saudis aged 40–59 with chronic pain have an increased risk of depression (21). Mental disorders and chronic physical conditions are associated with higher levels of disability and role impairment among Saudis (23, 24): yet only a small percentage receive or seek treatment (25). The effects of comorbid mental disorders are reported to lead to higher treatment costs, functional impairment, and prolonged duration of treatment (23, 26). It is important to note that there are several possible reasons for such comorbidities to exist: (1) the mental disorder causes the chronic physical condition (or vice versa), (2) the conditions influence and mutually maintain each other in some way, (3) a third factor (e.g., a sociodemographic characteristic) increases the risk of developing both mental disorders and chronic physical conditions, or (4) the conditions occur independently, by a mechanism that is unrelated to the other (27). These outlined findings emphasize the critical need for evidence based-studies aimed at understanding the burden of comorbidities, in order to develop policy frameworks for interventions to prevent further comorbidity development.
Although informative, basic epidemiological findings on mental/physical comorbidity in the KSA general population are lacking. Overall, previous Saudi studies have focused on such comorbidity patterns between selected chronic physical conditions and mental disorders (22, 28–30), and this among specific populations (31). To the best of our knowledge, there are no published studies that have used rigorous field methods to examine comorbidities of broad chronic physical conditions and mental disorders, and the correlates of such comorbidities among the general population in the KSA.
This study uses data collected by the Saudi National Mental Health Survey (SNMHS), a national epidemiological survey conducted in the KSA, as part of the World Mental Health (WMH) Survey Initiative (32). Under the WMH Consortium (33), all participating countries conduct general population surveys using the World Health Organization (WHO) WMH Composite International Diagnostic Interview 3.0 (CIDI) to retrospectively assess mental disorders, based on the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV). The present study is one of the first Arab studies under the WMH Consortium to investigate the relationship between mental disorders and chronic conditions. The aims of the study are to examine (i) the prevalence of DSM-IV 12-month mental disorders among Saudis with lifetime chronic physical conditions, (ii) the sociodemographic correlates of chronic physical conditions, (iii) the interaction of 12-month mental disorders with sociodemographic correlates of chronic physical conditions, and (iv) the associations between such comorbidities and disability among Saudis in the KSA. National estimates on such comorbidities are needed to inform mental health stakeholders, and policymakers involved in improving the quality of life of the affected individuals.
2 Materials and methods
2.1 Sample
The sample was obtained from the SNMHS. As described previously, (34, 35) the SNMHS was based on a multi-stage clustered probability sample of Arabic-speaking household citizens aged between 15 and 65 years old, living in urban and rural areas of the KSA. Over 28 months between 2014 and 2016, trained lay interviewers conducted face-to-face interviews, as per the general methods of the WMH survey initiative. The response rate for a total sample of 4,004 participants was 61%. The interviews were conducted in two parts in an effort to reduce respondent burden and control study costs, thereby enhancing the data collection process and enabling a comprehensive assessment of research objectives. Part I included a core diagnostic assessment that was given to all respondents. Part II included questions about risk factors, consequences, other correlates, and assessments of additional disorders. Part II was given to all Part I respondents who had any core disorder, as well as a 25% probability sub-sample of other Part I respondents (n = 1981). Prior to the interview, the interviewers obtained written informed consent. This study was performed in line with the principles of the Declaration of Helsinki. Field procedures and consent were approved by the Institutional Review Board committee at the King Faisal Specialist Hospital & Research Centre, Riyadh, Saudi Arabia. The characteristics of the sub-sample with chronic physical conditions are presented in Table 1.
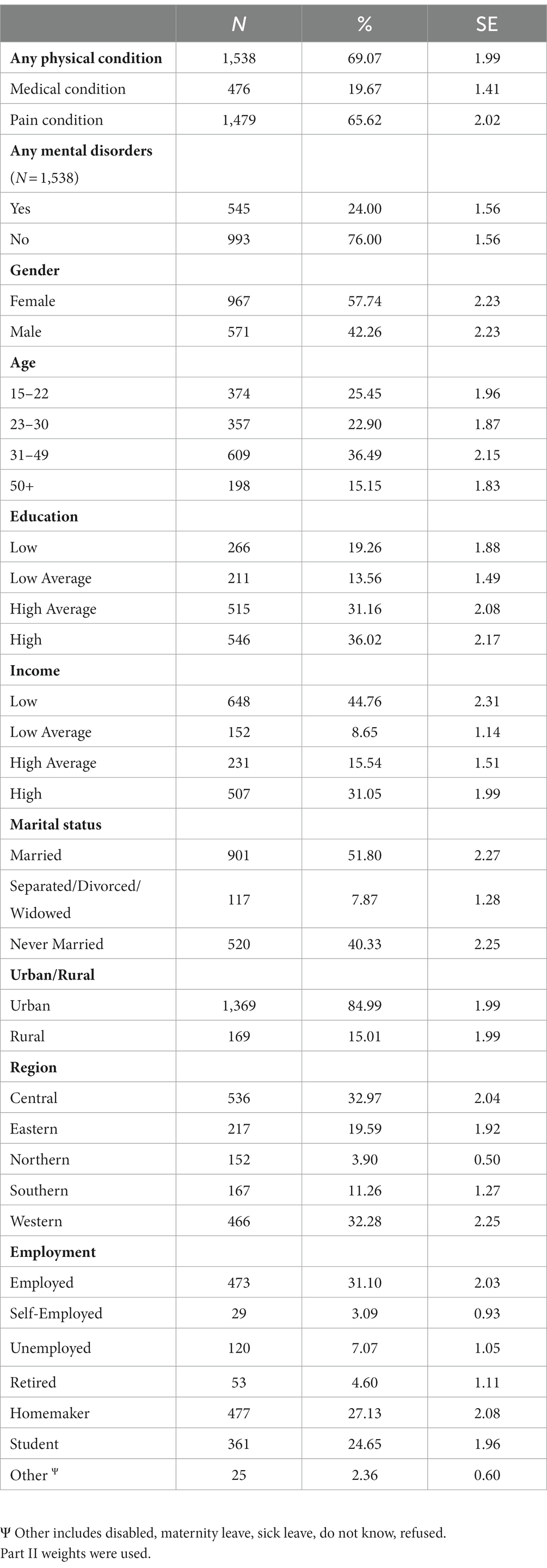
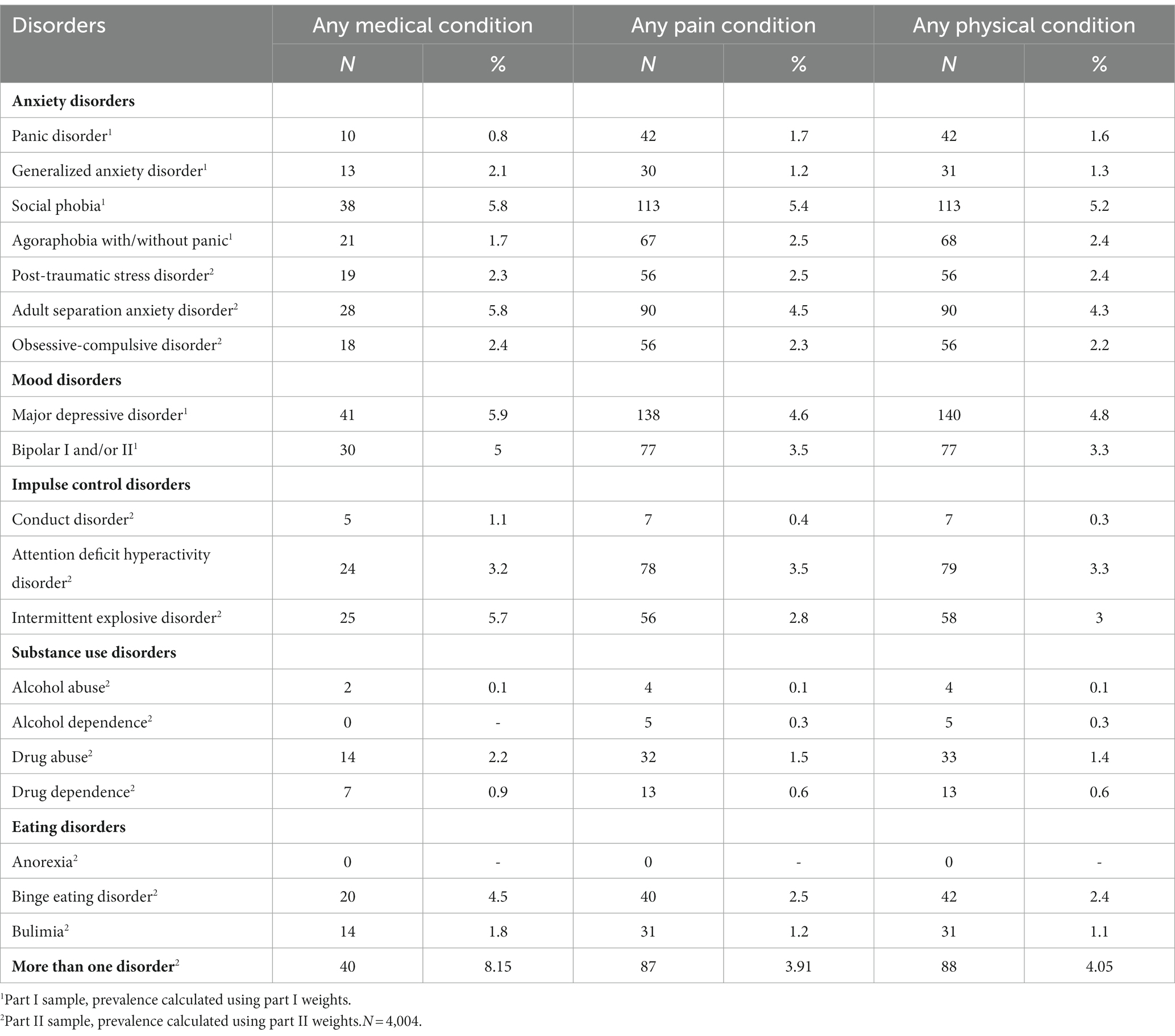
Table 1. Prevalence of chronic physical conditions in the total sample, and the characteristics of the sub-sample.
2.2 Measures
2.2.1 Mental disorders
The mental disorder diagnoses were based on the WHO-WMH CIDI 3.0 – a fully structured lay administered interview that generates diagnoses according to the criteria of DSM-IV (36). The computerized version of CIDI 3.0 was translated into Arabic and adapted to suit the local culture, then validated in the Arabic-speaking local population (34, 37, 38). The clinical reappraisal study of the Saudi CIDI showed valid and conservative diagnoses of common mental disorders in the Saudi population (39).
Twelve-month disorders assessed by the instrument criteria were used, and classified as follows: anxiety disorders (panic disorder, generalized anxiety disorder, agoraphobia without panic disorder, social phobia, posttraumatic stress disorder, obsessive-compulsive disorder, separation anxiety disorder), mood disorders (major depressive disorder, bipolar disorder I or II), impulse control disorders (conduct disorder, attention-deficit/hyperactivity disorder, intermittent explosive disorder), substance use disorders (alcohol and drug abuse and dependence) and eating disorders (anorexia, binge eating disorder, bulimia). The DSM-IV organic exclusion rules and diagnostic hierarchy rules were applied to the diagnoses as described elsewhere (24).
2.2.2 Chronic physical conditions
Lifetime chronic conditions were assessed as part of the adapted CIDI 3.0, and were grouped into the following categories in this study: any medical condition (heart disease, high blood pressure, asthma, other chronic lung diseases [like chronic obstructive pulmonary disease, tuberculosis or emphysema], cancer; any pain condition (arthritis, chronic back or neck pain, frequent or severe headaches, other chronic pain); and any physical condition (any condition reported in either the medical or pain category).
2.2.3 Sociodemographic correlates
Sociodemographic correlates included age (15–24 years, 25–34 years, 35–49 years, and 50 and above years), gender, completed years of education (0–6 years, i.e., low; 7–9 years, i.e., low-average; 10–15 years, i.e., high-average; and 16 years or more, i.e., high), and marital status (married, separated or widowed or divorced, and never married). Family income was defined as the household income divided by the number of people in the household. A case was assigned a category on a scale based on the per capita income of the respondent’s household divided by the median income for the country, where it was categorized as low if it was less than half the median, low-average if half the whole median, high-average if up to twice the median, and high if greater than twice the median. Employment included those who are employed, self-employed, unemployed, retired, a homemaker, a student, and others (such as disabled, maternity leave, sick leave, refused to answer, do not know). Urbanicity (rural, and urban) and region (Central [Riyadh, Al Qaseem, Hail], Eastern [Eastern Province], Northern [Northern Frontier, Al-Jouf, Tabouk], Southern [Aseer, Al-Baha], and Western [Makkah, Al-Madinah]) (35) were extracted from the sample frame (2010 Census) that was provided by the General Authority for Statistics in Saudi Arabia.
2.2.4 Disability
Assessment of disability was similar to previous WMH studies (23, 40). Disability was measured in terms of ‘days out of role’ in the last 30 days, using the Work Loss Days (WLD) index of the World Health Organization Disability Assessment Schedule (WHODAS-II) (41). The WLD index assesses both days with full disability (i.e., in which the respondent is totally unable to perform daily tasks as usual (42), and days with partial disability (43). Full disability was estimated by asking respondents the number of days in the 30 days before interview (that is, beginning yesterday and going back 30 days) they were totally unable to work or carry out your normal activities because of problems with either their physical health, mental health, or use of alcohol or drugs. Partial disability was defined as the number of days in which respondents (a) had to cut down on what they did, assessed by the following item ‘How many days out of the past 30 were you able to work and carry out your normal activities, but had to cut down on what you did or not get as much done as usual because of problems with either your physical health, your mental health, or your use of alcohol or drugs?’; (b) had to cut back on the quality of what they did, assessed by the following item: ‘How many days out of the past 30 did you cut back on the quality of your work or how carefully you worked because of problems with either your physical health, your mental health, or your use of alcohol or drugs?’; and (c) experienced extreme effort to perform as usual, assessed by the following item: ‘How many days out of the past 30 did it take an extreme effort to perform up to your usual level at work or at your other normal daily activities because of problems with either your physical health, your mental health, or your use of alcohol or drugs?’. Using these four questions, a weighted sum of activity limitation days in the prior month was estimated. The following terms were added together: (1) The number of days totally unable to carry out normal activities in the prior month; (2) One-half the number of days of reduced activities; (3) One-half the number of days of reduced quality or care in work activities; and (4) One-quarter the number of days requiring extreme effort to perform at one’s usual level. If this sum exceeded 30, it was recoded to equal 30 so that the sum had a range from 0 to 30. The sum was then divided by 30 and multiplied by 100 so that the resulting WLD index score also ranged from 0 to 100.
2.3 Analysis
Sample weights were used to adjust for differential probabilities of selection in between-household and within-household as well as sample and population distrubutions. In brief, Part I weights were used for core-section disorders, while Part II weights were used for noncore-section disorders. Further detail on weighting procedures can be found elsewhere (35). For chronic physical conditions, respondents who reported any medical condition, and any pain condition were counted once each to calculate the total frequencies for both categories; and counted only once for the total frequency of the third category, i.e., any physical condition. Similarly, for all classes of mental disorders (e.g., any anxiety disorders), respondents who reported comorbid mental disorders from other classes of mental disorders (e.g., any mood disorders) were counted once each to calculate total frequencies. Prevalence of mental disorders with each comorbid chronic condition were obtained using crosstabulations with appropriate weights (35) for each disorder. Differences across chronic physical conditions and mental disorders classes were considered at p-value threshold of <0.05, using cross tabulations with the Wald chi-square test. The cross tabulations were done using the PROC SURVEYFREQ procedure in SAS 9.2 (SAS Institute Inc., Cary, NC, USA). Multiple logistic regression models were created to investigate associations between the chronic physical conditions, mental disorders, and sociodemographic correlates, as well as for the interaction between comorbidities and sociodemographic correlates. All logistic regression models were created using the PROC LOGISTIC procedure, and reported using odds ratios with 95% confidence intervals, with Wald chi-square tests with p-value threshold of <0.05. The WLD means were also calculated with 95% confidence intervals using the PROC MEANS procedure.
3 Results
The prevalence of any lifetime chronic physical condition among Saudis was 69.1%; and the prevalence of any 12-month comorbid mental disorder among those with chronic physical conditions was 24% (Table 1). The majority among those who reported chronic physical conditions were female, aged 31–49, with high education and low income, married, living in an urban area, in the Central or Western region, or employed.
3.1 Mental disorders among respondents with physical conditions
Major depressive disorder (5.9%), social phobia (5.8%), and adult separation anxiety disorder (5.8%) were the most common comorbid mental disorders among Saudis with any medical condition (Table 2). By comparison, social phobia (5.4%) and major depressive disorder (4.6%) were the most prevalent comorbid mental disorders among respondents with any pain condition. These disorders were also the most common comorbid mental disorders among Saudis with any physical condition (with prevalence estimates of 5.2 and 4.8%, respectively).
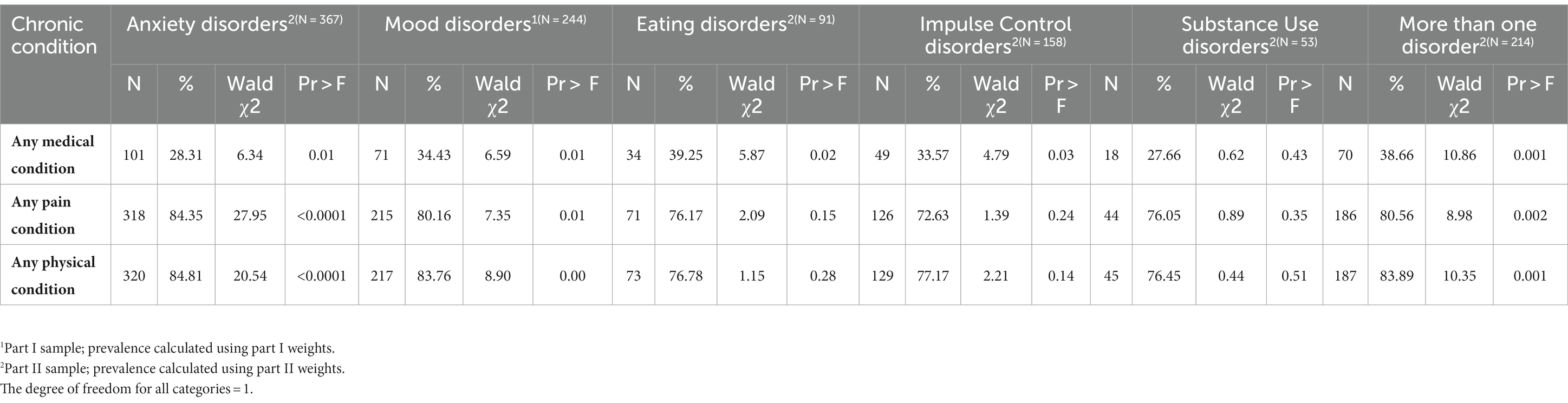
With regard to impulse control disorders, high rates of attention deficit disorder and intermittent explosive disorder were found among Saudis belonging to all three categories of chronic physical conditions. Binge eating disorder was particularly high (4.5%) among Saudis with any medical condition. Relative to other disorders, substance use disorders such as alcohol abuse (0.1%) were not as prevalent as anxiety disorders and mood disorders among Saudis with chronic physical conditions. Anxiety disorders and mood disorders were the most common comorbid mental disorders across all categories of chronic physical conditions (Table 3). Eating disorders (39.25%) and impulse control disorders (33.57%) were only prevalent and comorbid among Saudis with any medical condition.
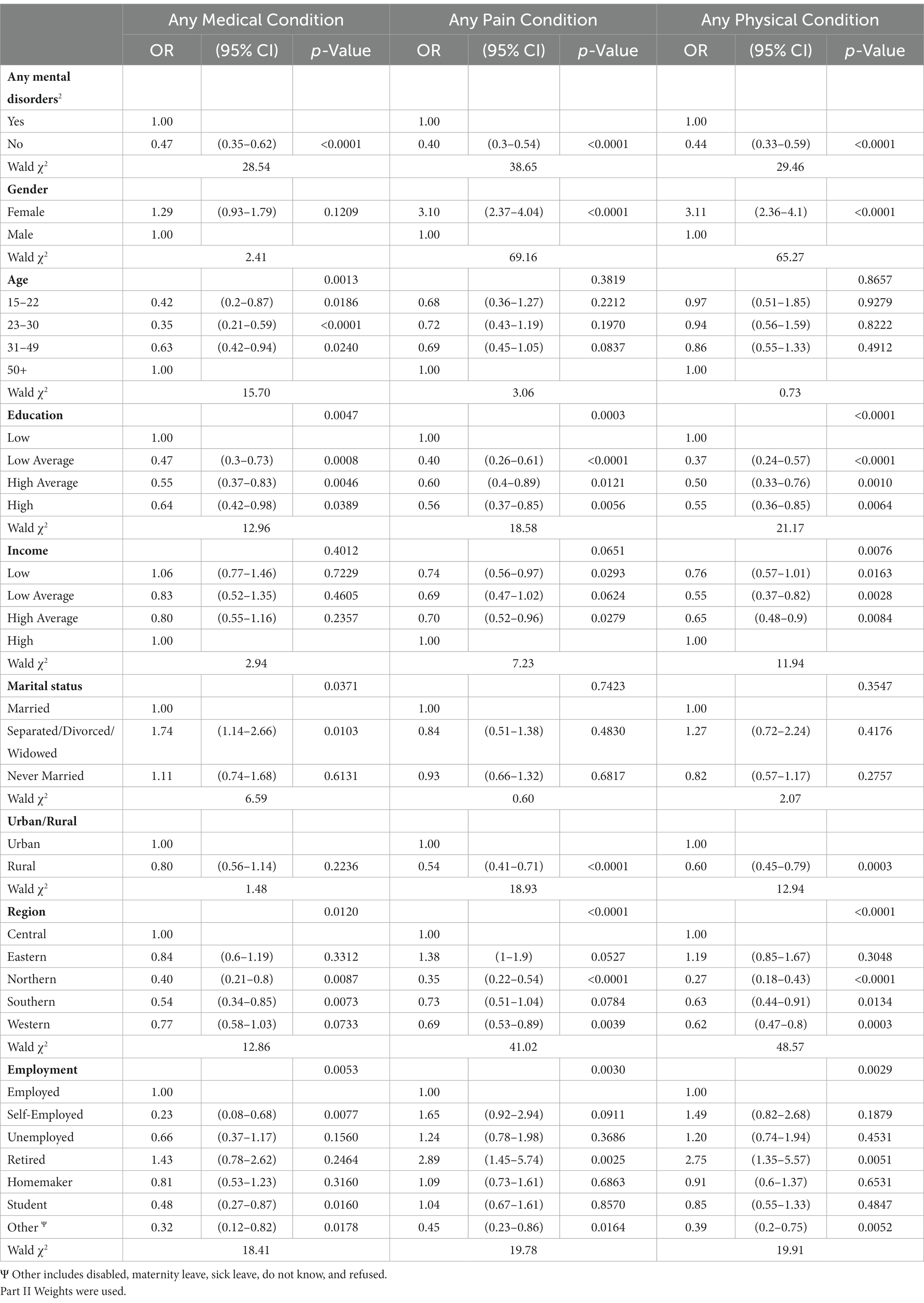
3.2 Correlates of physical conditions
Females were three times more likely than males to report any pain condition, or any physical condition. Compared to older Saudis (50+), those in other age groups had lower risk of any medical condition. Those who had low-average, high average and high levels of education were less likely to report any medical condition (OR = 0.47, p = 0.0008; OR = 0.55, p = 0.0046; OR = 0.64, p = 0.0389), any pain condition (OR = 0.40, p < 0.0001; OR = 0.60, p = 0.0121; OR = 0.56, p = 0.0056), and any physical condition (OR = 0.37, p < 0.0001; OR = 0.50, p = 0.0010; OR = 0.55, p = 0.0064) compared to those who had low levels of education.
Saudis with low average and high average income had lower risk of any pain condition (OR = 0.69, p = 0.0624; OR = 0.70, p = 0.0279) and any physical condition (OR = 0.55, p = 0.0028; OR = 0.65, p = 0.0084) compared to those with high income. Being separated/divorced/widowed vs. married was associated with increased risk of any medical condition (OR = 1.74, p = 0.0103). Those living in rural areas compared to urban areas were less likely to report any pain condition (OR = 0.54, p < 0.0001), and any physical condition (OR = 0.60, p = 0.0003). Northern and Southern region vs. Central region of the KSA were associated with lower rates of any medical condition (OR = 0.40, p = 0.0087; OR = 0.54, p = 0.0073); Northern and Western region vs. Central region were associated with lower rates of any pain condition (OR = 0.35, p < 0.0001; OR = 0.69, p = 0.0039); and Northern, Southern and Western region vs. Central region were associated with lower rates of any physical condition (OR = 0.27, p < 0.0001; OR = 0.63, p = 0.0134; OR = 0.62, p = 0.0003).
Saudis, who were self-employed and students vs. employed had lower risk of any medical condition (OR = 0.23, p = 0.0077; OR = 0.48, p = 0.0160). Those who were retired were almost three times more likely than those who were employed to report any pain condition and any physical condition (OR = 2.89, p = 0.0025). Employment reports of other types (disabled, maternity leave, sick leave, do not know, refused, etc.) were associated with lower rates of any medical condition (OR = 0.32, p = 0.0178), any pain condition (OR = 0.45, p = 0.0164), and any physical condition (OR = 0.39, p = 0.0052).
Saudis without mental disorders had systematically lower risk of any medical condition (OR = 0.47, p < 0.0001), any pain condition (OR = 0.40, p < 0.0001), and any physical condition (OR = 0.44, p < 0.0001) compared to those who had a comorbid 12-month mental disorder (Table 4).
Mental disorders were found to interact with gender, age, income, and employment to exert an effect on the risk of any medical condition (Table 5). There were mental disorders interactions with all sociodemographic characteristics except for marital status for the category of any pain condition. Gender, education, income, urbanicity, region, and employment interacted with mental disorders to predict the risk of any physical condition. For instance, females with mental disorders were found to be at a considerably higher risk of developing physical conditions than males (p < 0.0001). Additionally, individuals with mental disorders who had high (p = 0.0009) and high-average (p = 0.0001) education levels had reduced risks of experiencing physical conditions. Individuals in rural areas were also at a notably lower risk of physical conditions (p < 0.0001). Furthermore, relative to those living in the Western region, individuals with mental disorders residing in the Central and Eastern regions (p = 0.0003 & 0.0003) were at a significantly higher risk for physical conditions, while those in the Northern region were at a lower risk (p = 0.0001) (Supplementary Table S1).
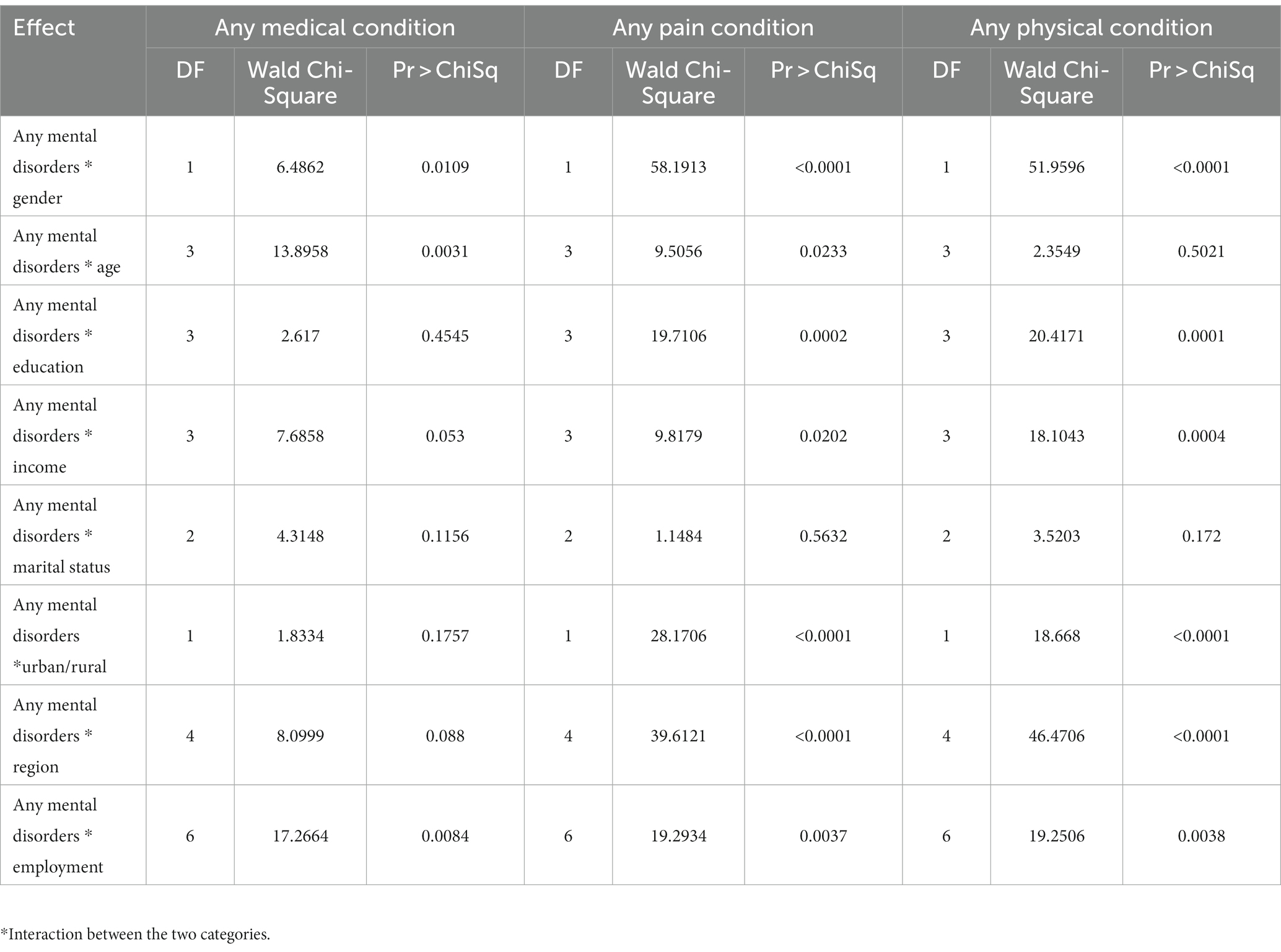
Table 5. Mental disorders interactions of sociodemographic correlates and chronic physical conditions.
3.3 Mental/physical comorbidity and work loss days indices
We found meaningful associations between comorbidities and days out of role in the last 30 days (Table 6): respondents without mental disorders or chronic physical conditions had 0.27 days out of role (CI: 0.12–0.43, SE: 0.11) — on average — in the last 30 days. Those with 12-month mental disorders but without any physical conditions had 4.44 (CI: 2.73–6.15, SE: 0.86) days out of role. Saudis with chronic physical conditions but without any mental disorder had 1.18 (CI: 0.90–1.47, SE: 0.14) days out of role, and those with comorbidities of mental disorder and chronic physical condition had an average of 2.97 (CI: 2.45–3.49, SE: 0.26) days out of role in the last 30 days.
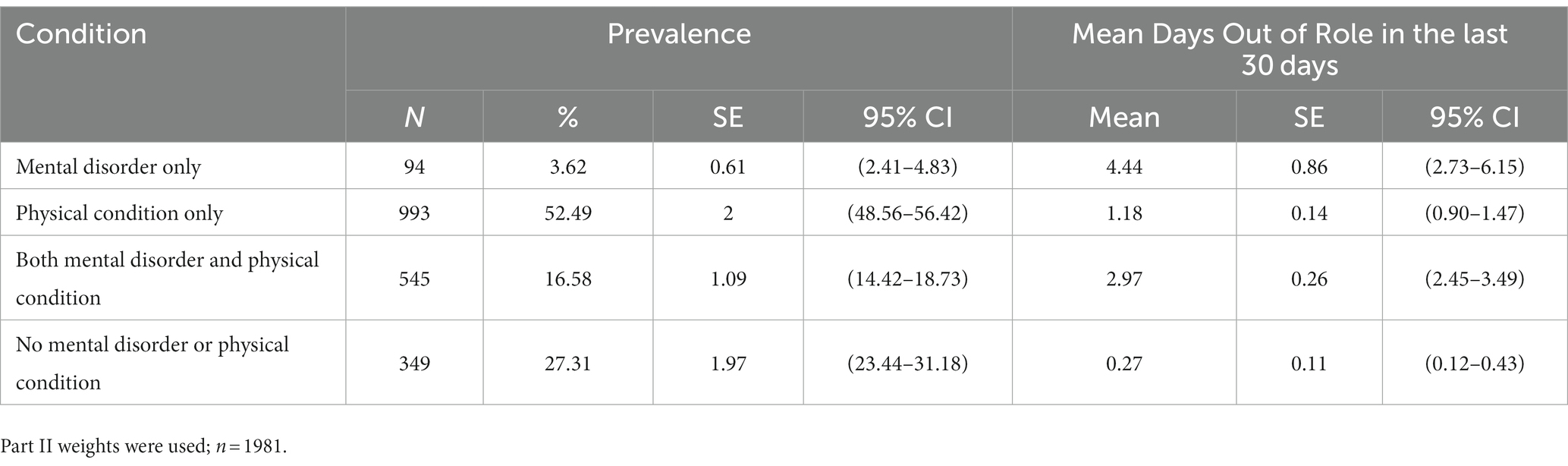
Table 6. Days out of role in the last 30 days for Saudis with 12-month mental disorders and lifetime chronic physical conditions.
4 Discussion
This is one of the first Arab studies under the WMH Consortium to examine comorbidities of chronic physical conditions and mental disorders in the general population of a country from the Gulf Cooperation Council (GCC). We found that chronic physical conditions among Saudis were common. In addition, about one in four Saudis with chronic physical conditions reported comorbid mental disorders. Specifically social phobia, adult separation anxiety disorder, and major depressive disorder were common mental disorders across all chronic physical condition categories. Overall, anxiety disorders were commonly comorbid across all chronic physical conditions; a large proportion (84.34%) of Saudis with any pain condition had comorbid anxiety disorders, as well as any physical condition comorbid with anxiety disorders (84.81%). These results were similar to other WMH studies (4, 9, 11, 40, 44), as well as with Arab (16) and Saudi studies with chronic physical condition clinical patients (18, 21).
Also in line with global (4, 11, 13, 45, 46), Arab (16), and Saudi studies (21, 29, 47), Saudis without comorbid 12-month mental disorders had lower rates of chronic physical conditions. Also, our findings related to the burden of comorbidities, and disability in terms of days out of role were supported by the Global Burden of Disease Study in the KSA (48). These results highlight the role of such burdens on impairment and loss of productivity, thereby pointing to the importance of addressing the large impact of mental/physical comorbidities on quality of life in local healthcare reforms (23). Additionally, that substance use disorders were generally less associated with chronic physical conditions than has been previously reported (15) can be largely attributed to the ban on alcohol and drug consumption and the limited availability of substances in the country (49).
Older age, low education, being separated/divorced/widowed, living in the Central region of the KSA, and being employed were associated with increased risk of any medical condition. Mental disorders interacted with the sociodemographic correlates (excluding marital status) to predict the risk of chronic physical conditions categories among Saudis. Future research is warranted, given that this study did not examine the temporal relationships between the conditions, and causal mechanisms of such comorbidities. However, as previously mentioned, a number of relationship scenarios are possible between the conditions. It is possible that the mental disorder or chronic physical condition cause or influence one another in certain ways, or that certain sociodemographic factors increase vulnerability to either condition, or even that the conditions do not influence each other, but simply coincide (27).
Within the context of the KSA, the New Models of Care – outlined by the Ministry of Health for the Vision 2030, Health Sector Transformation Strategy (50) – specify chronic conditions as a prioritized system of care, and recognize that the mental health services in the country are underdeveloped, and need to be taken into account as the healthcare development progresses. Currently, the Saudi government ensures that ‘Comprehensive Health Guidance Initiative’ under the primary mental health program of the Ministry of Health, provides integrated mental health treatment – to some extent – in physical health treatment. The aims of this program include early detection of depression and anxiety among primary health centres’ outpatients, and provision of primary mental health services for prevention of chronic diseases (51). Previous Saudi reports also indicate that pharmacotherapy – specifically polypharmacy, i.e., use of multiple medication – is common among outpatients with medical conditions (52) and mental disorders (53). However it is unclear how effectively and explicitly comorbidities are targeted, or addressed in the healthcare sector, or across other sectors in the KSA generally. Saudi studies in the past has advocated for multidisciplinary approaches such as the biopsychosocial model to be considered by healthcare professionals, to address mental disorders among individuals with chronic physical conditions, especially in hospitals (21, 47). Furthermore, although the National Center for Mental Health Promotion provides accessible psychological education services to the public (54), tailored healthcare efforts, support services, and awareness campaigns explicitly addressing comorbidities of mental disorders and chronic physical conditions among the general population are needed.
The findings of this study must be interpreted in light of the following limitations. First, the assessment of comorbidities in this study may be different from that of a clinical population survey. Symptoms of mental disorders such as fatigue in depressive disorders may also be common for chronic illnesses; comorbidities in this study were assessed without applying any exclusionary criteria for entangled symptoms of physical and mental disorders (40). Also, psychotic disorders, such as schizophrenia, that did not fall within the scope of the SNMHS may also be commonly linked with medical comorbidities (55). Second, due to the stigma surrounding mental disorders and self-reporting of symptoms and chronic conditions, the prevalence of comorbidities in this study may be an underestimation. However, there is evidence to support that self-reports generally show good concordance with medical reports for chronic diseases (46, 56). Third, given the cross-sectional nature of this study, any indicated associations between comorbidities and correlates do not imply causation. Prospective research studies could investigate ages of onset of mental disorders and chronic physical conditions to understand the relationship between these disorders as well as determine the course of comorbid chronic conditions (9).
5 Conclusion
Using nationally representative data from the SNMHS, this study investigated the dual burden of mental disorders and chronic physical conditions and their association with sociodemographic correlates and disability. Our findings demonstrate that such comorbidities were common among the Saudi population, particularly mood and anxiety disorders. Mental/physical disorders were linked to a number of sociodemographic correlates as well as significant disability. Overall, the findings of this study provide a valuable point of comparison alongside other surveys from high-income countries under the WMH Consortium — the vast majority of which were conducted among Western populations. Our study also contributes to a growing body of Saudi literature, and provides national estimates related to comorbidities that were unavailable before. These estimates will inform social, mental and health policies across the country and the GCC, in terms of identifying vulnerable groups at risk for comorbidities, and developing prevention and treatment services tailored to their specific health needs.
Data availability statement
The datasets presented in this article are not readily available because of restrictions in the informed consent language used to recruit respondents and WMH consortium agreements. Requests to access the datasets should be directed to the corresponding author at eWFzbWludEBrZnNocmMuZWR1LnNh.
Ethics statement
The studies involving humans were approved by Institutional Review Board committee at the King Faisal Specialist Hospital & Research Centre, Riyadh, Saudi Arabia. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
YA and LB: conceptualization and supervision. YA, LB, AA-S, and AA-H: project administration, investigation, funding acquisition, and resources. YA, LB, MN: methodology. MN: Formal analysis. LB, SH, and AA: writing - original draft preparation. YA, RB, LB, SH, and AA: writing - review and editing. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the King Salman Center for Disability Research; Saudi Basic Industries Corporation; King Abdulaziz City for Science and Technology; Ministry of Health (Saudi Arabia); and King Saud University. Funding in-kind was provided by King Faisal Specialist Hospital & Research Center, and Ministry of Economy & Planning, General Authority for Statistics, Riyadh.
Acknowledgments
We would like to thank the National Center for Mental Health Promotion for their support in developing this paper. The Saudi National Mental Health Survey (SNMHS) is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative, which is supported by the National Institute of Mental Health, the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, GlaxoSmithKline, and Bristol-Myers Squibb. We also thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis. None of the funders had any role in the design, analysis, interpretation of results, or preparation of this paper. A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh. We thank Beth-Ellen Pennell, Yu-chieh Lin and other staff at the Survey Research Center, University of Michigan, Ann Arbor for supporting the SNMHS with its design and implementation. We also thank the SNMHS team, including those that worked with us in the past, for their contributions to the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1238326/full#supplementary-material
References
1. Gijsen, R, Hoeymans, N, Schellevis, FG, Ruwaard, D, Satariano, WA, and van den Bos, GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. (2001) 54:661–74. doi: 10.1016/s0895-4356(00)00363-2
2. Teesson, M, Slade, T, and Mills, K. Comorbidity in Australia: findings of the 2007 National Survey of mental health and wellbeing. Aust N Z J Psychiatry. (2009) 43:606–14. doi: 10.1080/00048670902970908
3. Boyd, CM, and Fortin, M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Rev. (2010) 32:451–74. doi: 10.1007/BF03391611
4. Scott, KM, Bruffaerts, R, Tsang, A, Ormel, J, Alonso, J, Angermeyer, MC, et al. Depression-anxiety relationships with chronic physical conditions: results from the world mental health surveys. J Affect Disord. (2007) 103:113–20. doi: 10.1016/j.jad.2007.01.015
5. Bertrem, C, Bruffaerts, R, Bonnewyn, A, Oyen, HV, Demarest, S, and Demyttenaere, K. Mental and pain comorbidity of chronic somatic disorders in the general population in Belgium. Arch public health. (2006) 64:199–214.
6. Scott, KM, Oakley Browne, MA, McGee, MA, and Wells, JE. Mental-physical comorbidity in Te Rau Hinengaro: the New Zealand mental health survey. Aust N Z J Psychiatry. (2006) 40:882–8. doi: 10.1080/j.1440-1614.2006.01907.x
7. Gadermann, AM, Alonso, J, Vilagut, G, Zaslavsky, AM, and Kessler, RC. Comorbidity and disease burden in the National Comorbidity Survey Replication (Ncs-R). Depress Anxiety. (2012) 29:797–806. doi: 10.1002/da.21924
8. Daré, LO, Bruand, PE, Gérard, D, Marin, B, Lameyre, V, Boumédiène, F, et al. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. (2019) 19:304. doi: 10.1186/s12889-019-6623-6
9. Demyttenaere, K, Bruffaerts, R, Lee, S, Posada-Villa, J, Kovess, V, Angermeyer, MC, et al. Mental disorders among persons with chronic Back or neck pain: results from the world mental health surveys. Pain. (2007) 129:332–42. doi: 10.1016/j.pain.2007.01.022
10. Abdin, E, Chong, SA, Vaingankar, JA, Shafie, S, Seah, D, Chan, CT, et al. Changes in the prevalence of comorbidity of mental and physical disorders in Singapore between 2010 and 2016. Singap Med J. (2022) 63:196–202. doi: 10.11622/smedj.2020124
11. Askari, MS, Andrade, LH, Filho, AC, Silveira, CM, Siu, E, Wang, YP, et al. Dual burden of chronic physical diseases and anxiety/mood disorders among São Paulo megacity mental health survey sample. Brazil J Affect Disord. (2017) 220:1–7. doi: 10.1016/j.jad.2017.05.027
12. Correll, CU, Solmi, M, Veronese, N, Bortolato, B, Rosson, S, Santonastaso, P, et al. Prevalence, Incidence and Mortality from Cardiovascular Disease in Patients with Pooled and Specific Severe Mental Illness: A Large-Scale Meta-Analysis of 3,211,768 Patients and 113,383,368 Controls. World Psychiatry. (2017) 16:163–80. doi: 10.1002/wps.20420
13. Dai, H, Mei, Z, An, A, and Wu, J. Epidemiology of physical and mental comorbidity in Canada and implications for health-related quality of life, suicidal ideation, and healthcare utilization: a Nationwide cross-sectional study. J Affect Disord. (2020) 263:209–15. doi: 10.1016/j.jad.2019.11.146
14. Jürisson, M, Pisarev, H, Uusküla, A, Lang, K, Oona, M, Elm, L, et al. Physical-mental health comorbidity: a population-based cross-sectional study. PLoS One. (2021) 16:e0260464. doi: 10.1371/journal.pone.0260464
15. Scott, KM, Lim, C, Al-Hamzawi, A, Alonso, J, Bruffaerts, R, Caldas-de-Almeida, JM, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry. (2016) 73:150–8. doi: 10.1001/jamapsychiatry.2015.2688
16. Alkhadhari, S, Alsabrrie, AO, Ohaeri, JU, Varghese, R, Zahid, MA, and Mulsant, BH. Mental and physical comorbidity in an Arab primary health care setting. BMC Psychiatry. (2018) 18:313. doi: 10.1186/s12888-018-1903-8
17. Kilzieh, N, Rastam, S, Maziak, W, and Ward, KD. Comorbidity of depression with chronic diseases: a population-based study in Aleppo. Syria Int J Psychiatry Med. (2008) 38:169–84. doi: 10.2190/PM.38.2.d
18. Shaheen Al Ahwal, M, Al Zaben, F, Khalifa, DA, Sehlo, MG, Ahmad, RG, and Koenig, HG. Depression in patients with colorectal cancer in Saudi Arabia. Psychooncology. (2015) 24:1043–50. doi: 10.1002/pon.3706
19. Abdul-Mohsen, MF. Frequency of depression among patients with acute coronary syndrome, eastern region. Saudi Arabia J Family Community Med. (2004) 11:23–9.
20. Al-Khotani, A, Naimi-Akbar, A, Gjelset, M, Albadawi, E, Bello, L, Hedenberg-Magnusson, B, et al. The associations between psychosocial aspects and Tmd-pain related aspects in children and adolescents. J Headache Pain. (2016) 17:30. doi: 10.1186/s10194-016-0622-0
21. Al-Maharbi, S, Abolkhair, A, Al Ghamdi, H, Haddara, M, Tolba, Y, El Kabbani, A, et al. Prevalence of depression and its association with sociodemographic factors in patients with chronic pain: a cross-sectional study in a tertiary Care Hospital in Saudi Arabia. Saudi J Anaesth. (2018) 12:419–25. doi: 10.4103/sja.SJA_771_17
22. Marengoni, A, Winblad, B, Karp, A, and Fratiglioni, L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. (2008) 98:1198–200. doi: 10.2105/ajph.2007.121137
23. Altwaijri, YA, Puac-Polanco, V, Al-Subaie, AS, Ad-Dab'bagh, Y, Al-Habeeb, AH, Bilal, L, et al. The comparative importance of mental and physical disorders for health-related days out of role in the general population of Saudi Arabia. BMC Public Health. (2022) 22. doi: 10.1186/s12889-022-12721-z
24. Altwaijri, YA, Al-Habeeb, A, Al-Subaie, AS, Bilal, L, Al-Desouki, M, Shahab, MK, et al. Twelve-month prevalence and severity of mental disorders in the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1831. doi: 10.1002/mpr.1831
25. Al-Habeeb, A, Altwaijri, YA, Al-Subaie, AS, Bilal, L, Almeharish, A, Sampson, NA, et al. Twelve-month treatment of mental disorders in the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1832. doi: 10.1002/mpr.1832
26. Ciechanowski, PS, Katon, WJ, and Russo, JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. (2000) 160:3278–85. doi: 10.1001/archinte.160.21.3278
27. Asmundson, GJ, and Katz, J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. (2009) 26:888–901. doi: 10.1002/da.20600
28. Almuneef, M, Hollinshead, D, Saleheen, H, AlMadani, S, Derkash, B, AlBuhairan, F, et al. Adverse childhood experiences and association with health, mental health, and risky behavior in the Kingdom of Saudi Arabia. Child Abuse Negl. (2016) 60:10–7. doi: 10.1016/j.chiabu.2016.09.003
29. Al-Rahimi, JS, Nass, NM, Hassoubah, SA, Wazqar, DY, and Alamoudi, SA. Levels and predictors of fear and health anxiety during the current outbreak of Covid-19 in immunocompromised and chronic disease patients in Saudi Arabia: a cross-sectional correlational study. PLoS One. (2021) 16:e0250554. doi: 10.1371/journal.pone.0250554
30. Alhabib, KF, Batais, MA, Almigbal, TH, Alshamiri, MQ, Altaradi, H, Rangarajan, S, et al. Demographic, Behavioral, and cardiovascular disease risk factors in the Saudi population: results from the prospective urban rural epidemiology study (pure-Saudi). BMC Public Health. (2020) 20:1213. doi: 10.1186/s12889-020-09298-w
31. Alkhormi, AH, Mahfouz, MS, Alshahrani, NZ, Hummadi, A, Hakami, WA, Alattas, DH, et al. Psychological health and diabetes self-management among patients with type 2 diabetes during Covid-19 in the southwest of Saudi Arabia. Ed. A. A. Rizvi. Medicina (Kaunas). (2022) 58. doi: 10.3390/medicina58050675
32. Al-Subaie, AS, Al-Habeeb, A, and Altwaijri, YA. Overview of the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1835. doi: 10.1002/mpr.1835
33. Kessler, RC, and Üstün, TB. The who world mental health surveys: Global perspectives on the epidemiology of mental disorders. Eds. RC Kessler and TB Ustun. Cambridge: Cambridge University Press (2008).
34. Altwaijri, YA, Al-Habeeb, A, Bilal, L, Shahab, MK, Pennell, BE, Mneimneh, Z, et al. The Saudi National Mental Health Survey: survey instrument and field procedures. Int J Methods Psychiatr Res. (2020) 29:e1830. doi: 10.1002/mpr.1830
35. Mneimneh, ZN, Heeringa, SG, Lin, Y-C, Altwaijri, YA, and Nishimura, R. The Saudi National Mental Health Survey: sample design and weight development. Int J Methods Psychiatr Res. (2020) 29:e1829. doi: 10.1002/mpr.1829
36. Kessler, RC, and Ustün, TB. The world mental health (Wmh) survey initiative version of the World Health Organization (who) composite international diagnostic interview (Cidi). Int J Methods Psychiatr Res. (2004) 13:93–121. doi: 10.1002/mpr.168
37. Mneimneh, Z, Hibben, KC, Bilal, L, Hyder, S, Shahab, M, Binmuammar, A, et al. Probing for sensitivity in translated survey questions: differences in respondent feedback across cognitive probe types. Translation & Interpreting-the International Journal of Translation and Interpreting. (2018) 10:73–88. doi: 10.12807/ti.110202.2018.a06
38. Shahab, M, Al-Tuwaijri, F, Kattan, N, Bilal, L, Hyder, S, Mneimneh, Z, et al. Implementing the Trapd model for the Saudi adaptation of the world mental health composite international diagnostic interview 3.0. Int J Ment Heal Syst. (2019) 13:12. doi: 10.1186/s13033-019-0267-x
39. Kessler, RC, Al-Desouki, M, King, AJ, Sampson, NA, Al-Subaie, AS, Al-Habeeb, A, et al. Clinical reappraisal of the composite international diagnostic interview version 3.0 in the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1828. doi: 10.1002/mpr.1828
40. Teesson, M, Mitchell, PB, Deady, M, Memedovic, S, Slade, T, and Baillie, A. Affective and anxiety disorders and their relationship with chronic physical conditions in Australia: findings of the 2007 National Survey of mental health and wellbeing. Aust N Z J Psychiatry. (2011) 45:939–46. doi: 10.3109/00048674.2011.614590
41. Von Korff, M, Crane, PK, Alonso, J, Vilagut, G, Angermeyer, MC, Bruffaerts, R, et al. Modified Whodas-ii provides valid measure of global disability but filter items increased skewness. J Clin Epidemiol. (2008) 61:1132–43. doi: 10.1016/j.jclinepi.2007.12.009
42. Alonso, J, Petukhova, M, Vilagut, G, Chatterji, S, Heeringa, S, Üstün, TB, et al. Days out of role due to common physical and mental conditions: results from the who world mental health surveys. Mol Psychiatry. (2011) 16:1234–46. doi: 10.1038/mp.2010.101
43. Bruffaerts, R, Vilagut, G, Demyttenaere, K, Alonso, J, Alhamzawi, A, Andrade, LH, et al. Role of common mental and physical disorders in partial disability around the world. Br J Psychiatry. (2012) 200:454–61. doi: 10.1192/bjp.bp.111.097519
44. Nakash, O, Levav, I, Aguilar-Gaxiola, S, Alonso, J, Andrade, LH, Angermeyer, MC, et al. Comorbidity of common mental disorders with cancer and their treatment gap: findings from the world mental health surveys. Psycho-Oncology. (2014) 23:40–51. doi: 10.1002/pon.3372
45. Bonnewyn, A, Katona, C, Bruffaerts, R, Haro, JM, de Graaf, R, Alonso, J, et al. Pain and depression in older people: comorbidity and patterns of help seeking. J Affect Disord. (2009) 117:193–6. doi: 10.1016/j.jad.2009.01.012
46. Scott, K, McGee, MA, Schaaf, D, and Baxter, J. Mental-physical comorbidity in an ethnically diverse population. Soc Sci Med. (2008) 66:1165–73. doi: 10.1016/j.socscimed.2007.11.022
47. Al-Zahrani, J, Shubair, MM, Al-Ghamdi, S, Aldossari, KK, Alsalamah, M, Al-Khateeb, BF, et al. Psychological predictors of chronic pain in Al Kharj region, Saudi Arabia. Ann General Psychiatry. (2021) 20:23. doi: 10.1186/s12991-021-00345-3
48. Tyrovolas, S, El Bcheraoui, C, Alghnam, SA, Alhabib, KF, Almadi, MAH, Al-Raddadi, RM, et al. The burden of disease in Saudi Arabia 1990-2017: results from the global burden of disease study 2017. The Lancet Planetary Health. (2020) 4:e195–208. doi: 10.1016/S2542-5196(20)30075-9
49. Saquib, N, Rajab, AM, Saquib, J, and AlMazrou, A. Substance use disorders in Saudi Arabia: a scoping review. Subst Abuse Treat Prev Policy. (2020) 15:1–12.
50. Ministry of Health SA. Health sector transformation strategy. Vision Realization Office: Ministry of Health (2019).
51. Comprehensive health guidance initiative—primary mental care program [internet]. Ministry of Health, Saudi Arabia (2021). Available at: https://www.moh.gov.sa/en/Pages/Default.aspx.
52. Salih, SB, Yousuf, M, Durihim, H, Almodaimegh, H, and Tamim, H. Prevalence and associated factors of polypharmacy among adult Saudi medical outpatients at a tertiary care Center. J Family Community Med. (2013) 20:162–7. doi: 10.4103/2230-8229.121987
53. Alharbi, FF, Alharbi, SF, Salih, SB, and Al-Surimi, K. Correlates of psychotropic polypharmacy in outpatient psychiatric clinics of two military tertiary hospitals in Saudi Arabia. J Family Community Med. (2019) 26:213–20. doi: 10.4103/jfcm.JFCM_31_19
54. National Center for Mental Health Promotion SA. National Centre for Mental Health Promotion (2022). Available at: https://ncmh.org.sa/.
55. Rodrigues, M, Wiener, JC, Stranges, S, Ryan, BL, and Anderson, KK. The risk of physical multimorbidity in people with psychotic disorders: a systematic review and meta-analysis. J Psychosom Res. (2021) 140:110315. doi: 10.1016/j.jpsychores.2020.110315
56. Kriegsman, DM, Penninx, BW, van Eijk, JT, Boeke, AJ, and Deeg, DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of Patients' self-reports and on determinants of inaccuracy. J Clin Epidemiol. (1996) 49:1407–17. doi: 10.1016/s0895-4356(96)00274-0
Keywords: comorbidity, chronic physical conditions, mental disorders, Saudi Arabia, disability
Citation: Altwaijri Y, Al-Habeeb A, Al-Subaie A, Bruffaerts R, Bilal L, Hyder S, Naseem MT and Alghanim AJ (2023) Dual burden of chronic physical conditions and mental disorders: Findings from the Saudi National Mental Health Survey. Front. Public Health. 11:1238326. doi: 10.3389/fpubh.2023.1238326
Edited by:
Brandon Gaudiano, Brown University, United StatesReviewed by:
Dushad Ram, Shaqra University, Saudi ArabiaAdegboyega Ogunwale, Neuropsychiatric Hospital, Aro, Nigeria
Copyright © 2023 Altwaijri, Al-Habeeb, Al-Subaie, Bruffaerts, Bilal, Hyder, Naseem and Alghanim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yasmin Altwaijri, WWFzbWluVEBrZnNocmMuZWR1LnNh
†Present Address: Sanaa Hyder, Health and Meaningful Dialogue (HAMD) Centre, Manchester, United Kingdom
 Yasmin Altwaijri
Yasmin Altwaijri Abdulhameed Al-Habeeb4
Abdulhameed Al-Habeeb4 Lisa Bilal
Lisa Bilal Sanaa Hyder
Sanaa Hyder Mohammad Talal Naseem
Mohammad Talal Naseem Abdullah J. Alghanim
Abdullah J. Alghanim