- 1School of Nursing, Chengdu Medical College, Chengdu, China
- 2The Clinical Hospital of Chengdu Brain Science Institute, MOE Key Laboratory for Neuroinformation, University of Electronic Science and Technology of China, Chengdu, China
Introduction: With the progressive aging of the population, frailty is now a significant challenge in geriatrics research. A growing amount of evidence suggests that sleep disturbance and depression have independent effects on frailty, although the underlying mechanisms are not yet clear. This study aimed to investigate the mediating role of depression in the relationship between sleep disturbance and frailty in older adult patients with type 2 diabetes (T2DM) in the community.
Method: Purposive sampling was used to collect face-to-face data from 342 community-dwelling T2DM patients in Chengdu, Sichuan Province, China, between February and May 2023. The Pittsburgh Sleep Quality Index (PSQI) scale was used to evaluate sleep quality, the Simple Geriatric Depression Scale (GDS-15) was used to evaluate depressive symptoms, and the FRAIL Scale (FRAIL) was used to evaluate frailty. Linear regression equation and bootstrap self-sampling were used to verify the mediating role of depressive symptoms in sleep disturbance and frailty.
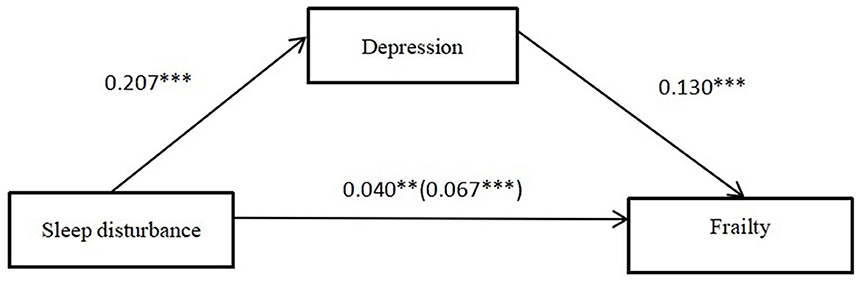
Result: The study found that sleep disturbance had a direct positive effect with frailty [β = 0.040, 95% CI: (0.013, 0.069)]. Additionally, depression had a direct positive effect on frailty [β = 0.130, 95% CI: (0.087, 0.173)], and depression was found to partially mediate the relationship between sleep disturbance and frailty.
Conclusion: Poor sleep quality and frailty are common in patients with T2DM. To reduce the frailty of older adult T2DM patients, all levels of society (government, medical institutions, and communities) must pay more attention to mental health. A variety of interventions should be considered to improve sleep quality and depression, which in turn may prevent or control frailty.
Introduction
The aging population presents a significant challenge for contemporary societies and has garnered greater global attention. It is projected that by 2050, a fifth of the population will be over the age of 65 (26.1%) (1, 2). China has the largest population of older adult citizens and is now one of the fastest aging nations globally (3). The rise in the aging population has coincided with the growing prevalence of several chronic ailments, especially diabetes (4). With the findings of the survey conducted by the International Diabetes Federation (IDF) (5), the current global population of adults with diabetes is ~537 million. China has been identified as the country with the largest number, with over 110 million diabetic patients (6). Type 2 diabetes mellitus (T2DM) accounts for more than 90% (7). The prevalence of T2DM is 23.9% in people aged 60–69 and 27.3% in those aged 70 and over (8). It can be seen that the situation regarding the prevalence of diabetes in the country has become even more critical.
Frailty poses a significant challenge to older adults as they age (9). Frailty is a complex concept that must account for the intricate interplay of various factors often manifesting in three dimensions: physical, psychological, and social frailty (10). In China, the older adult patient population with T2DM had 22.7% higher frailty detection rates than patients without T2DM (11, 12). Moreover, frailty may heighten the risk of falls, disability, and mortality in older adult patients with T2DM, jeopardizing the physical and mental health of older adults and causing a significant economic strain on families, society, and healthcare (13). These findings highlight the significance of prioritizing frailty management in older adult T2DM patients amidst a rapidly aging population.
Previous studies showed that sleep disturbance may associated with frailty (14), But the underlying mechanism has not yet been revealed. Sleep disturbance impacts many older people with T2DM (15). Older adult people with T2DM have a higher incidence of sleep disturbance due to obstructive sleep apnoea or nocturnal symptoms such as hypoglycemia, nocturia, or neuralgia (16, 17). Poor sleep quality can lead to impaired protein synthesis and muscle loss, and these changes are a significant cause of frailty in older people (18, 19). A previous prospective cohort study found a high risk of frailty in older adults with sleep problems (20). Older adults with sleep problems were 49.95 times more likely to be frail than those without sleep problems (21). Several studies have shown a positive association between sleep problems and frailty (21, 22). Therefore, sleep disturbance may be one of the factors affecting frailty among T2DM patients. In this study, we focused on sleep disturbance in T2DM patients and hypothesized that their sleep disturbance would be positively correlated with their frailty. In addition, sleep disturbances may associated with depression and can lead to low mood (23).
Depression is a common and complex mental illness. Globally, depression is one of the most common mental illnesses in people 65 years and older, affecting one in seven older adults (24). Studies have shown that sleep disturbance is a risk factor for depression in older patients with T2DM (25). Previous study of older adult people with T2DM, sleep disturbance was positively associated with depression. There is also evidence that sleep disturbance is strongly associated with depression, with an increasing prevalence of sleep disturbance and higher detection rates of depression in older adults (26). Additionally, Almeida et al. demonstrated that depression may be associated with frailty among older adult T2DM patients (27).
People with depression are more likely to be frailty (28, 29). A previous study found that older adult, depression people with T2DM are at high risk of frailty (30). Depression increases the risk of adverse outcomes with older adult T2DM patients in frailty. Compared with non-depressed people with diabetes, people with depression have a significantly lower quality of life in physical and mental functioning, which can lead to disability and death (31). As a result, we further predicted depression as a mediator in the relationship between sleep disturbance and frailty among community-dwelling older adult T2DM patients.
A review of previous studies found that most previous studies in this area have examined the relationship between sleep disturbance, depression, and frailty. However, the combined effects of these factors on frailty and the underlying mechanisms of these relationships were unclear. In addition, few studies have examined frailty in a specific group—older adult T2DM patients. Therefore, this study investigated the association between sleep disturbance, depression, and frailty in community older adult T2DM patients in Chengdu and the possible underlying mechanisms.
Based on previous studies, we propose 4 hypotheses: (1) Sleep disturbance has a direct positive effect on frailty; (2) Sleep disturbance has a direct positive effect on depression; (3) Depression has a direct positive effect on frailty; (4) The relationship between sleep disturbance and frailty is mediated by depression. Our findings identified the critical factors for preventing and controlling frailty in older adult T2DM patients in the community, which is essential for reducing frailty and improving the health of T2DM patients.
Materials and methods
Participants
This was a cross-sectional study conducted between February 2023 and May 2023. Approval was obtained from the Ethics Committee of Chengdu Fourth Hospital was obtained prior to this study. Our study used purposive sampling method to select two community health centers in Chengdu city, and purposive sampling was applied in the community to select respondents who met the study criteria. Respondents were asked to meet the following inclusion criteria: (1) Diagnosed by the attending physician meeting the diagnostic criteria for T2DM by the World Health Organization (WHO) in 1999 (32); (2) age ≥60 years; (3) diagnosis ≥3 months; (4) no significant (or corrected) impairment of vision, hearing or communication; and (5) voluntary participation and signing an informed consent form. Exclusion criteria were as follows: (1) diagnosed psychiatric disease; (2) presence of severe organic disease intolerant of the survey; (3) patients with severe acute complications of diabetes mellitus in combination were excluded. In the end, a total of 342 questionnaires were distributed and, after excluding invalid questionnaires, 319 valid questionnaires were finally obtained and 93% (319/342) valid responses were obtained and analyzed. In addition, we refer to the sample size estimation formula for cross-sectional studies (33): . Where n is the sample size, Z is the statistic corresponding to the confidence level, P is the expected prevalence, and d is the precision. We assumed a confidence level of 95.0%, an expected prevalence of frailty of 19.2% based on the prevalence of frailty of T2DM in the community of Xianning City, Hubei Province, China, as reported by Linglin Kong et al. and a precision of 5.0%. Therefore, taking into account the formula, we obtained n ≈ 239. Taking into account a questionnaire loss rate of 20%, the sample size was calculated to be at least 287 cases.
Measures
All measures in this study would be conducted in Chinese.
Basic sociodemographic data
A self-designed questionnaire was adopted, including gender, age, ebody fat index (BMI), education, marital status, residential status, monthly income., physical activity, disease duration, and complications. BMI is calculated by dividing weight (kg) by the square of height (m), with a value of 18.5–23.9 as normal and a value of < 18.5 or >23.9 as abnormal BMI (34). Marital status is classified as married and single. Being single includes being unmarried, widowed, and divorced.
Physical Activity is exercising more than 3 times or 300 min a week (35). Types of exercise include: walking, jogging/cycling, Tai chi, swimming, apparatus sports, dance exercises (square dancing, aerobics, yoga), and ball games (36). Complications include peripheral neuropathy, retinopathy, diabetic nephropathy, diabetic foot, cerebrovascular, and cardiovascular disease (37).
Frailty
Frailty was assessed using the frailty scale (38). The scale consists of 5 questions: (1) Fatigue: Have you felt tired frequently in the past 4 weeks? (2) Low resistance: Is it difficult to climb stairs without AIDS and help from others? (3) Low walking amount: Is it difficult to walk a block of about 500 m without AIDS and help from others? (4) Weight loss: Have you lost at least 5% of your body weight in the past year? (5) Diseases: Have you had five or more diseases? The scale is scored on a scale of 0–5. If the old person answered “yes”, they got a “1” and if they answered “no”, they got a “0”. Scores of 0, 1–2, and 3–5 represent robust, prefrail, and frail, respectively. Dong et al. (39) applied its translation to the older adult in Chinese communities and found that the frailty scale had good validity and reliability (40). It showed good validity and test–retest reliability in Chinese patients with type 2 diabetes (41).
Sleep disturbance
Sleep quality in patients with T2DM was assessed using the Pittsburgh Sleep Quality Index (PSQI) (42). The scale was compiled by Dr. Buysse in 1989. The PSQI scale included sleep quality, sleep time, sleep duration, sleep efficiency, sleep disorders, hypnotic drugs, and daytime dysfunction. Nineteen self-rated items were scored and composed of 7 components. Each component was scored on a scale of 0 3. The cumulative score of each component was the total PSQI score, with the total score ranging from 0 to 21, and PSQI score > 7 was considered as sleep disorder. Cronbach's α coefficient in this study was 0.79. The Chinese version of PSQI has been proven to be reliable and valid in the community-dwelling older population (43).
Depression
The Geriatric Depression Scale-15 (GDS-15) was developed from the Geriatric Depression Scale developed by Reisberg et al. in 1982 (44). GDS-15 consists of 15 items, each with “yes” and “no” options. The total score is 0–15 points, among which items 1, 5, 7, and 11 are scored in reverse. A score of 0–4 indicates no symptoms of depression, and a score of ≥5 indicates symptoms of depression. The Chinese version of GDS-15 is a reliable and valid screening tool for assessing geriatric depressive symptoms in the Chinese population (45). The Cronbach α coefficient of this scale in this study was 0.77.
Procedure
To ensure consistency in survey methodology, all information was collected in face-to-face interviews by uniformly trained investigators with a medical background. All items were explained in an unbiased manner by the investigator and, after written informed consent was obtained, all participants were assured that their responses would be anonymous and confidential. The questionnaire also explained the purpose of the survey, how to complete it, and the promise of confidentiality. Finally, face-to-face data collection took place and questionnaires were returned on the spot.
Statistical analysis
The data was entered using Epidata software. Data quality was ensured by consistent coding of the questionnaires, and separate entry by two individuals. All analyses were conducted using IBM SPSS Statistics version 25.0 (Armonk, NY, United States). The significance level for the two-tailed test to α = 0.05. We expressed continuous data as mean ± standard deviation and categorical data as (n) and percentage (%). We tested the correlation between variables using Pearson correlation analysis. In a similar way, McKinnon's four-step approach (46) was used in our study to analyze the mediating role with four specific criteria that had to be met: (1) There was a significant association between the independent variable (sleep disturbance) and the dependent variable (frailty); (2) There was also a significant association between the independent variable (sleep disturbance) and the mediator variable (depression); (3) There was a significant correlation between the mediator variable (depression) and the dependent variable (frailty) after adjusting for the control of the independent variable (sleep disturbance); (4) The coefficient of indirect correlation between the independent variable (sleep disturbance) and the dependent variable (frailty) through the mediator variable (depression) is significant. The first three steps were individually tested by means of a linear regression equation with αin = 0.05 and αout = 0.01. Finally, the mediation effect was analyzed using the PROCESS version 3.0 macro for SPSS (model 4), with bootstrap 5,000 self-sampling to verify the final condition. Statistical significance is indicated when 0 is excluded from the 95% confidence interval.
Results
Common method biases test
We used Harman's Single Factor Test to examine the common method bias in the study. The analysis showed that the first common factor analyzed explained only 24.45% (< 40%) of the variance. This suggests that there was no significant common method bias in the study, even though we used the questionnaire.
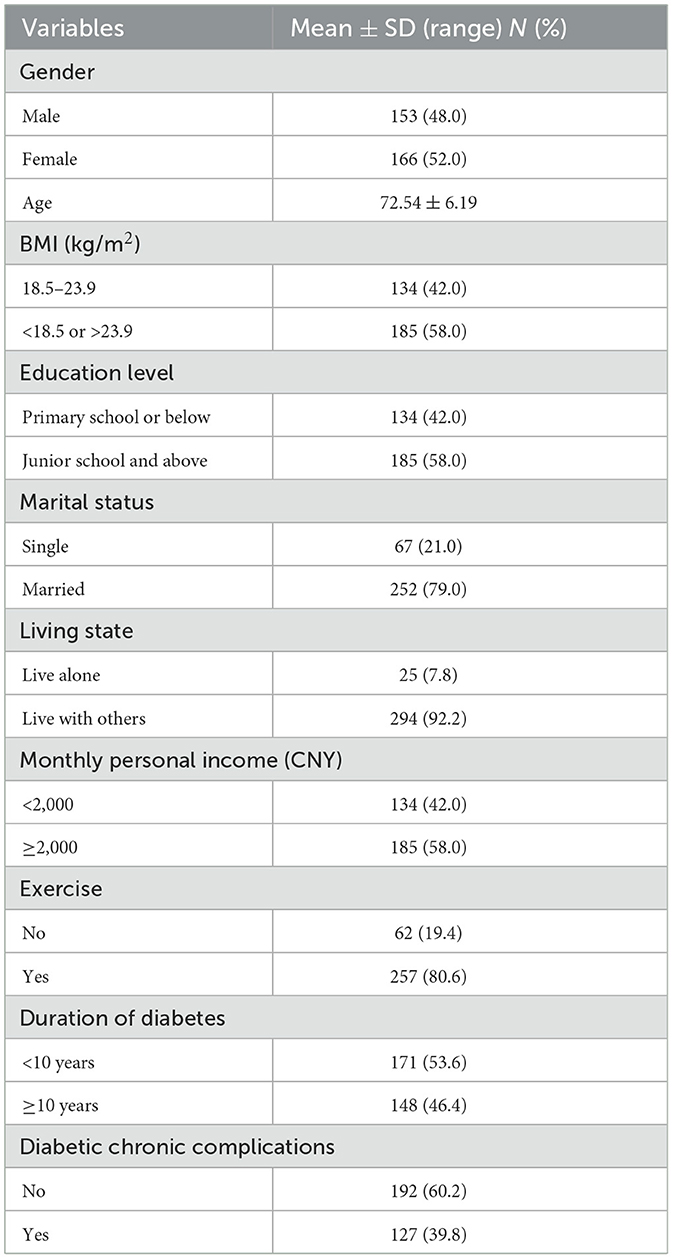
Table 1 shows the sociodemographic characteristics of the older adult T2DM patients. Of the 319 eligible patients, 166 (52.0%) were female and 153 (48.0%) were male. The mean age of the participants was (72.54 ± 6.19) years. One hundred and thirty-four (42.0%) of the participants had a normal BMI and 185 (58.0%) had a high or low BMI. The educational background of the participants was as follows: 134 (42.0%) had a junior high school education or less, and 185 (58.0%) had a high school education or more. The participants' marital status was as follows: 67 (21.0%) were single and 252 (79.0%) were married. Of the total number of patients surveyed, 25 (7.8%) were living alone and the remaining 194 (30.7%) were not living alone. There were 134 patients (42.0%) with a monthly personal income of < $2,000 and 185 patients (58.0%) with a monthly personal income of more than $2,000. There were 257 (80.6%) participants who exercised regularly, while 62 (19.4%) exercised less. There were 171 (53.6%) patients with a disease duration of < 10 years and 148 (46.4%) participants with a disease duration of >10 years. Finally, 127 (39.8%) patients had chronic complications of diabetes and the remaining 192 (60.2%) did not.
Correlations of the study variable
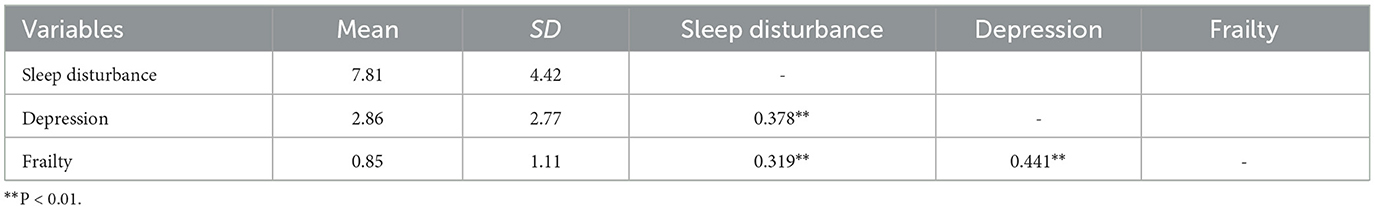
Table 2 shows Spearman's correlations for the study variables. Sleep disturbance (r = 0.319, p < 0.01) and depression (r = 0.441, p < 0.01) were significantly positively correlated with frailty. In addition, sleep disturbance was significantly positively correlated with depression (r = 0.378, p < 0.01).
The mediation effect analysis
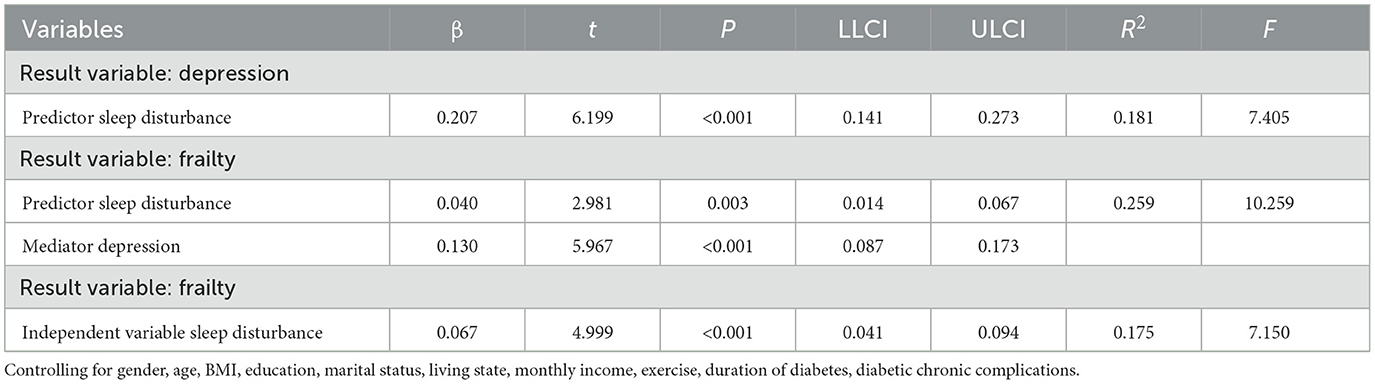
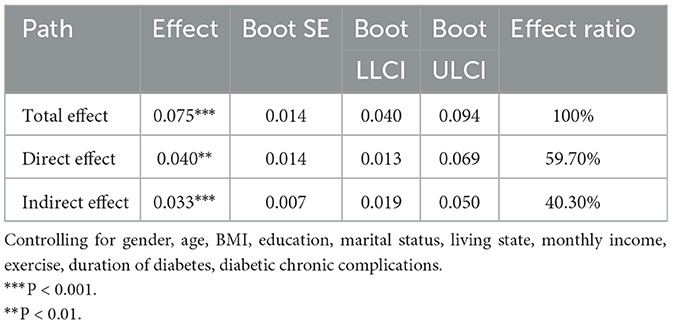
Table 3 reports the analysis of mediating effects among the variables. After controlling for variables, there was a significant direct effect of sleep disturbances on frailty [β = 0.067, CI (0.041, 0.094)]. In addition, sleep disturbance had a significant positive effect on depression [β = 0.207, CI (0.141, 0.273)]. Depression were significantly effected frailty [β = 0.130, CI (0.087, 0.173)]. Furthermore, the effect of sleep disturbance on frailty was statistically significant even when the mediating variable was included (see Table 4; β = 0.040, CI (0.014, 0.067)]. Based on the bootstrap 95% CI (see Table 4; depression = 0.033, 95% CI = 0.019 ~ 0.050) not containing 0, it can be concluded that depression partially mediates the relationship between sleep disturbance and frailty. Thus, hypothesis was confirmed. Note that the final mediation model is shown in Figure 1.
Discussion
This study aimed to examine the relationship between sleep disturbance, depression, and frailty in older adult T2DM patients among the community in Chengdu, China. To the best of our knowledge, this is the first study to report the mediating role of depression between sleep disturbance and frailty in older adult T2DM patients in the community. The results of this study may provide possible informations and directions for the formulation and implementation of intervention strategies and measures to improve frailty in older adult T2DM patients.
As speculated, our results suggest that sleep disturbance positively effects the frailty of older adult T2DM patients. This is consistent with existing studies (47). One possible explanation is that chronic sleep disturbance in older adult T2DM patients may lead to multisystem disease and dysfunction. Sleep disturbance often lead to daytime sleepiness and increased fatigue in older patients (14). It may also reduce social interaction or lead to a lack of social interaction in older adult T2DM patients. Over time, older adult T2DM patients may experience a significant decline in muscle strength and fitness and a lack of sensory stimulation, eventually leading to frailty (48). Therefore, providing adequate sleep security is an effective strategy to reduce frailty in older adult T2DM patients. Furthermore, lifestyle modifications, appropriate diabetes management, and increased social interaction may help to reduce frailty among older adult T2DM patients with poor sleep quality (49, 50).
After controlling for variables, depression plays a mediating role between sleep disturbance and frailty, as supported by a previous study (51). Depression is a crucial mechanism by which sleep disturbances effect frailty in T2DM, and sleep disturbances may further lead to frailty by depression in T2DM patients. Hypothesis 4 is supported. Numerous studies have demonstrated a complex biological connection between the duration of sleep and the symptoms of depression (52, 53). Sleep disturbance can cause significant variations in blood glucose levels, leading to challenges in its management (54). It also reduces insulin sensitivity, exacerbating the condition. Moreover, patients often face difficulty managing their diet in the presence of frequent fluctuations in blood glucose levels, leading to helplessness, reduced confidence in the battle against the illness, and depression (55). Older adult T2DM patients with depression have significantly elevated levels of C-reactive protein, interleukin-6 and tumor cytokines, which also contribute to frailty (56, 57). Meanwhile, older adult T2DM patients with depression are significantly less sociable and active and are more likely to have a sedentary lifestyle (58), which further contributes to muscle wasting. And muscle wasting and reduced muscle strength are important markers of frailty (59). In addition, co-morbidities with other chronic conditions can further exacerbate frailty (60). As a result, it is important to address the sleep problems of patients with type 2 diabetes mellitus to prevent the harmful impact of prolonged lack of sleep on their mental health and frailty.
Conclusion
The study suggests a significant and positive association between sleep disturbance and frailty in older adult T2DM patients living in the Chengdu community, with depression as a mediator. Thus, this study may help to elucidate the pathogenesis of frailty. A high-quality sleep may decrease the risk of depression and, consequently, frailty. Therefore, we suggest the following recommendations. To reduce frailty in T2DM patients, firstly, Government and community should provide more social opportunities for patients and actively encourage their participation in activities. Secondly, nursing managers should provide emotional regulation and management training to older adult T2DM patients in the community, which will improve their ability to cope with depression and increase their resilience. Also, patients with T2DM who need more social support from their families to improve the quality of sleep.
Limitations
This study has the following limitations: First, the sample size of this study was small. Secondly, the variables of “sleep disturbance,” “depression,” and “frailty” in this study were all subjectively reported by the subjects themselves, which may have information bias. Third, we tested only one mediating variable. Future studies need to further explore the influence of other potential variables, such as social support and self-efficacy, that are associated with frailty. Finally, the sample of this study comes from only two communities in Chengdu. Due to the differences in social culture, economy, and lifestyle, attention should be paid to the universality of the findings.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XC and XP was involved in all aspects of the study and preparation of the manuscript. CH, QM, ML, and XL was involved with the design of the study and preparation of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Chengdu Science and Technology Bureau Science and Technology Training Project (2022JDKP0022).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fang EF, Xie C, Schenkel JA, Wu C, Long Q, Cui H, et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. (2020) 64:101174. doi: 10.1016/j.arr.2020.101174
2. Chhetri JK, Chan P, Ma L, Peng D, Rodríguez-Mañas L, Cesari M, et al. Prevention of disability in the frail Chinese older population. J Frality Aging. (2019) 8:2–6. doi: 10.14283/jfa.2018.27
3. Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol A Biol. (2017) 73:102–8. doi: 10.1093/gerona/glx098
4. Farooque R, Herekar F, Iftikhar S, Patel MJ. The frequency of poor sleep quality in patients with diabetes mellitus and its association with glycemic control. Cureus J Med Sci. (2020) 12:e11608. doi: 10.7759/cureus.11608
5. Tönnies T, Rathmann W, Hoyer A, Brinks R, Kuss O. Quantifying the underestimation of projected global diabetes prevalence by the International Diabetes Federation (IDF) Diabetes Atlas. BMJ Open Diab Res CA. (2021) 9:2122. doi: 10.1136/bmjdrc-2021-002122
6. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pr. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
7. Alam U, Asghar O, Azmi S, Malik RA. General aspects of diabetes mellitus. Handb Clin Neurol. (2014) 126:211–22. doi: 10.1016/B978-0-444-53480-4.00015-1
8. Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. (2021) 326:2498–506. doi: 10.1001/jama.2021.22208
9. Weiss CO. Frailty and chronic diseases in older adults. Clin Geriatr Med. (2011) 27:39–52. doi: 10.1016/j.cger.2010.08.003
10. Dong L, Liu N, Tian X, Qiao X, Gobbens R, Kane RL, et al. Reliability and validity of the Tilburg Frailty Indicator (TFI) among Chinese community-dwelling older people. Arch Gerontol Geriat. (2017) 73:21–8. doi: 10.1016/j.archger.2017.07.001
11. Zeng X, Jia N, Meng L, Shi J, Li Y, Hu X, et al. A study on the prevalence and related factors of frailty and pre-frailty in the older population with diabetes in China: a national cross-sectional study. Front Public Health. (2022) 10:996190. doi: 10.3389/fpubh.2022.996190
12. Lee D, Kim M, Won CW. Common and different characteristics among combinations of physical frailty and sarcopenia in community-dwelling older adults: the Korean Frailty and Aging Cohort Study. Geriatr Gerontol Int. (2022) 22:42–9. doi: 10.1111/ggi.14314
13. Sands JD. The relationship of stressful life events to intellectual functioning in women over 65. Int J Aging Hum Dev. (1981) 14:11–22. doi: 10.2190/7RDC-2RUK-0GLR-J2KB
14. Liu X, Wang C, Qiao X, Si H, Jin Y. Sleep quality, depression and frailty among Chinese community-dwelling older adults. Geriatr Nurs. (2021) 42:714–20. doi: 10.1016/j.gerinurse.2021.02.020
15. Antza C, Kostopoulos G, Mostafa S, Nirantharakumar K, Tahrani A. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. (2021) 252:125–41. doi: 10.1530/JOE-21-0155
16. Wang W, Meng H, Liu Y, Yin W, Li Z, Wan M, et al. Effects of sleep duration and sleep quality in early pregnancy and their interaction on gestational diabetes mellitus. Sleep Breath. (2022) 26:489–96. doi: 10.1007/s11325-021-02391-3
17. Lavrentaki A, Ali A, Cooper BG, Tahrani AA, Mechanisms Mechanisms of Endocrinology. Mechanisms of disease: the endocrinology of obstructive sleep apnoea. Eur J Endocrinol. (2019) 180:R91–125. doi: 10.1530/EJE-18-0411
18. Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Env Res Pub He. (2021) 18:1082. doi: 10.3390/ijerph18031082
19. Wen Q, Yan X, Ren Z, Wang B, Liu Y, Jin X. Association between insomnia and frailty in older population: a meta-analytic evaluation of the observational studies. Brain Behav. (2023) 13:e2793. doi: 10.1002/brb3.2793
20. Ensrud KE, Blackwell TL, Redline S, Ancoli-Israel S, Paudel ML, Cawthon PM, et al. Sleep disturbances and frailty status in older community-dwelling men. J Am Geriatr Soc. (2009) 57:2085–93. doi: 10.1111/j.1532-5415.2009.02490.x
21. Sun R, Xie Y, Jiang W, Wang E, Li X. Effects of different sleep disorders on frailty in the elderly: a systematic review and meta-analysis of observational studies. Sleep Breath. (2023) 27:91–101. doi: 10.1007/s11325-022-02610-5
22. Nemoto Y, Sato S, Kitabatake Y, Nakamura M, Takeda N, Maruo K, et al. Bidirectional relationship between insomnia and frailty in older adults: a 2-year longitudinal study. Arch Gerontol Geriat. (2021) 97:104519. doi: 10.1016/j.archger.2021.104519
23. Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, et al. Clarifying the role of sleep in depression: a narrative review. Psychiat Res. (2020) 291:113239. doi: 10.1016/j.psychres.2020.113239
24. Patra P, Alikari V, Fradelos EC, Sachlas A, Kourakos M, Rojas GA, et al. Assessment of depression in elderly. Is perceived social support related? A nursing home study: depression and social support in elderly. Adv Exp Med Biol. (2017) 987:139–50. doi: 10.1007/978-3-319-57379-3_13
25. Sinclair AJ, Abdelhafiz AH. Multimorbidity, frailty and diabetes in older people-identifying interrelationships and outcomes. J Pers Med. (2022) 12:1911. doi: 10.3390/jpm12111911
26. Wium-Andersen IK, Jørgensen T, Jørgensen MB, Osler M, Wium-Andersen MK. Diabetes, sleep disorders and risk of depression - A Danish register-based cohort study. J Diabetes Complicat. (2022) 36:108266. doi: 10.1016/j.jdiacomp.2022.108266
27. Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Norman PE, et al. Duration of diabetes and its association with depression in later life: the health in men study (HIMS). Maturitas. (2016) 86:3–9. doi: 10.1016/j.maturitas.2016.01.003
28. Ma L, Zhang L, Sun F, Li Y, Tang Z. Frailty in Chinese older adults with hypertension: prevalence, associated factors, and prediction for long-term mortality. J Clin Hypertens. (2018) 20:1595–602. doi: 10.1111/jch.13405
29. Lohman M, Dumenci L, Mezuk B. Depression and frailty in late life: evidence for a common vulnerability. J Gerontol B-Psychol. (2016) 71:630–40. doi: 10.1093/geronb/gbu180
30. Adame PS, Senior PA, Field CJ, Jindal K, Mager DR. Frailty, health-related quality of life, cognition, depression, vitamin D and health-care utilization in an ambulatory adult population with type 1 or type 2 diabetes mellitus and chronic kidney disease: a cross-sectional analysis. Can J Diabetes. (2019) 43:90–7. doi: 10.1016/j.jcjd.2018.06.001
31. Donald M, Dower J, Ware R, Mukandi B, Parekh S, Bain C. Living with diabetes: rationale, study design and baseline characteristics for an Australian prospective cohort study. BMC Public Health. (2012) 12:8. doi: 10.1186/1471-2458-12-8
32. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med. (1998) 15:539–53.
33. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. (2013) 6:14–7.
34. Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. Treasure Island, FL: Stat Pearls Publishing (2023).
35. Okely AD, Kontsevaya A, Ng J, Abdeta C. 2020 WHO guidelines on physical activity and sedentary behavior. Sports Med Health Sci. (2021) 3:115–8. doi: 10.1016/j.smhs.2021.05.001
36. Wenhua Z, Keji L. Composing and editorial board of physical activity guidelines for chinese. Zhonghua Liu Xing Bing Xue Za Zhi. (2022) 43:5–6. doi: 10.3760/cma.j.cn112338-20211119-00903
37. Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. (2020) 18:110–6. doi: 10.2174/1570161117666190405165151
38. Abellan VKG, Rolland YM, Morley JE, Vellas B. Frailty: toward a clinical definition. J Am Med Dir Assoc. (2008) 9:71–2. doi: 10.1016/j.jamda.2007.11.005
39. Dong L, Qiao X, Tian X, Liu N, Jin Y, Si H, et al. Cross-cultural adaptation and validation of the FRAIL scale in Chinese community-dwelling older adults. J Am Med Dir Assoc. (2018) 19:12–7. doi: 10.1016/j.jamda.2017.06.011
40. Woo J, Leung J, Morley JE. Comparison of frailty indicators based on clinical phenotype and the multiple deficit approach in predicting mortality and physical limitation. J Am Geriatr Soc. (2012) 60:1478–86. doi: 10.1111/j.1532-5415.2012.04074.x
41. Tang Z, Shen C, Tong W, Xiang X, Feng Z, Han B. Frailty in community-dwelling adults aged 40 years and over with type 2 diabetes: association with self-management behaviors. Int J Env Res Pub He. (2022) 19:9092. doi: 10.3390/ijerph19159092
42. Buysse DJ, Reynolds CR, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiat Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
43. Zhu B, Xie M, Park CG, Kapella MC. Adaptation of the Pittsburgh sleep quality index in Chinese adults with type 2 diabetes. J Chin Med Assoc. (2018) 81:242–7. doi: 10.1016/j.jcma.2017.06.021
44. Reisberg B, Ferris SH. Diagnosis and assessment of the older patient. Hosp Community Psychiatry. (1982) 33:104–10. doi: 10.1176/ps.33.2.104
45. Mohebbi M, Nguyen V, McNeil JJ, Woods RL, Nelson MR, Shah RC, et al. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. Gen Hosp Psychiat. (2018) 51:118–25. doi: 10.1016/j.genhosppsych.2017.08.002
46. VanderWeele TJ. Introduction to statistical mediation analysis by Mackinnon, D. P Biometrics. (2009) 65:998–1000. doi: 10.1111/j.1541-0420.2009.01315_12.x
47. Liu JY. The severity and associated factors of participation restriction among community-dwelling frail older people: an application of the International Classification of Functioning, Disability and Health (WHO-ICF). BMC Geriatr. (2017) 17:43. doi: 10.1186/s12877-017-0422-7
48. Soysal P, Veronese N, Thompson T, Kahl KG, Fernandes BS, Prina AM, et al. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res Rev. (2017) 36:78–87. doi: 10.1016/j.arr.2017.03.005
49. Huang TY, Chou MY, Liang CK, Lin YT, Chen RY, Wu PF. Physical activity plays a crucial role in multidomain intervention for frailty prevention. Aging Clin Exp Res. (2023) 35:1283–92. doi: 10.1007/s40520-023-02412-z
50. Schmidt SK, Hemmestad L, MacDonald CS, Langberg H, Valentiner LS. Motivation and barriers to maintaining lifestyle changes in patients with type 2 diabetes after an intensive lifestyle intervention (The U-TURN Trial): a longitudinal qualitative study. Int J Env Res Pub He. (2020) 17:454. doi: 10.3390/ijerph17207454
51. Chu W, Chang SF, Ho HY, Lin HC. The relationship between depression and frailty in community-dwelling older people: a systematic review and meta-analysis of 84,351 older adults. J Nurs Scholarship. (2019) 51:547–59. doi: 10.1111/jnu.12501
52. Yuan C, Zhang Y. Modifiable risk factors of cognitive frailty in community-dwelling older adults: a systematic review and meta-analysis. Int J Nurs Knowl. (2023). doi: 10.1111/2047-3095.12437. [Epub ahead of print].
53. Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacol. (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
54. Mostafa SA, Mena SC, Antza C, Balanos G, Nirantharakumar K, Tahrani AA. Sleep behaviours and associated habits and the progression of pre-diabetes to type 2 diabetes mellitus in adults: a systematic review and meta-analysis. Diabetes Vasc Dis Re. (2022) 19:1486931512. doi: 10.1177/14791641221088824
55. King LK, Waugh E, MacKay C, Stanaitis I, Stretton J, Weisman A, et al. ‘It's a Dance Between Managing Both': a qualitative study exploring perspectives of persons with knee osteoarthritis and type 2 diabetes mellitus on the impact of osteoarthritis on diabetes management and daily life. BMJ Open. (2022) 12:e61472. doi: 10.1136/bmjopen-2022-061472
56. Coen PM, Jubrias SA, Distefano G, Amati F, Mackey DC, Glynn NW, et al. Skeletal muscle mitochondrial energetics are associated with maximal aerobic capacity and walking speed in older adults. J Gerontol A Biol. (2013) 68:447–55. doi: 10.1093/gerona/gls196
57. Santanasto AJ, Glynn NW, Jubrias SA, Conley KE, Boudreau RM, Amati F, et al. Skeletal muscle mitochondrial function and fatigability in older adults. J Gerontol A Biol. (2015) 70:1379–85. doi: 10.1093/gerona/glu134
58. Cao X, Li X, Zhang J, Sun X, Yang G, Zhao Y, et al. Associations between frailty and the increased risk of adverse outcomes among 38,950 UK biobank participants with prediabetes: prospective cohort study. Jmir Public Hlth Sur. (2023) 9:e45502. doi: 10.2196/45502
59. Richardson CA, Glynn NW, Ferrucci LG, Mackey DC. Walking energetics, fatigability, and fatigue in older adults: the study of energy and aging pilot. J Gerontol A Biol. (2015) 70:487–94. doi: 10.1093/gerona/glu146
Keywords: frailty, sleep disturbance, depression, type 2 diabetes, older adult
Citation: Chen X, Liu M, Ma Q, Liu X, Peng X and He C (2023) Mediating effects of depression on sleep disturbance and frailty in older adult type 2 diabetes patients in the community. Front. Public Health 11:1237470. doi: 10.3389/fpubh.2023.1237470
Received: 12 June 2023; Accepted: 07 November 2023;
Published: 28 November 2023.
Edited by:
Silvia Giovannini, Catholic University of the Sacred Heart, ItalyCopyright © 2023 Chen, Liu, Ma, Liu, Peng and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changjiu He, NTE5MDI5NDNAcXEuY29t
†These authors have contributed equally to this work and share first authorship
 Xushu Chen
Xushu Chen Mengdan Liu1†
Mengdan Liu1† Xueping Peng
Xueping Peng