
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 19 September 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1236099
 Jinsoo Min1
Jinsoo Min1 Ju Sang Kim2
Ju Sang Kim2 Hyung Woo Kim2
Hyung Woo Kim2 Yousang Ko3
Yousang Ko3 Jee Youn Oh4
Jee Youn Oh4 Yun-Jeong Jeong5
Yun-Jeong Jeong5 Eun Hye Lee6
Eun Hye Lee6 Bumhee Yang7
Bumhee Yang7 Ki Man Lee7
Ki Man Lee7 Joong Hyun Ahn2
Joong Hyun Ahn2 Jin Woo Kim8
Jin Woo Kim8 Yong Il Hwang9
Yong Il Hwang9 Sung Soon Lee10
Sung Soon Lee10 Jae Seuk Park11
Jae Seuk Park11 Hyeon-Kyoung Koo10*
Hyeon-Kyoung Koo10*Background: Poor nutrition increases disease severity and mortality in patients with tuberculosis (TB). There are gaps in our understanding of the effects of being underweight or overweight on TB in relation to sex.
Methods: We generated a nationwide TB registry database and assessed the effects of body mass index (BMI) on mortality in patients with pulmonary TB. The cause of death was further classified as TB-related or non-TB-related deaths. First, logistic regression analysis was performed to assess the association between BMI (a continuous variable) and mortality, and subgroup analyses of the multivariable logistic regression model were performed separately in male and female patients. Second, we categorized BMI into three groups: underweight, normal weight, and overweight, and assessed the impact of being underweight or overweight on mortality with reference to normal weight.
Results: Among 9,721 patients with pulmonary TB, the mean BMI was 21.3 ± 3.4; 1,927 (19.8%) were underweight, and 2,829 (29.1%) were overweight. In multivariable logistic regression analysis, mortality was significantly increased with the decrement of BMI (adjusted odds ratio [aOR] = 0.893, 95% confidence interval [CI] = 0.875–0.911). In subgroup analyses, underweight patients had significantly higher odds of mortality, especially TB-related deaths (aOR = 2.057, 95% CI = 1.546–2.735). The association with mortality and male patients was higher (aOR = 2.078, 95% CI = 1.717–2.514), compared with female patients (aOR = 1.724, 95% CI = 1.332–2.231). Being overweight had a significant protective effect against TB-related death only in females (aOR = 0.500, 95% CI = 0.268–0.934), whereas its effect on non-TB-related death was observed only in males (aOR = 0.739, 95% CI = 0.587–0.930).
Conclusion: Being underweight was linked to high mortality, whereas being overweight had beneficial effects in patients with pulmonary TB.
Tuberculosis (TB) is a public health problem affecting millions of people worldwide (1). Among several modifiable factors associated with TB, undernutrition is a leading risk factor worldwide (2, 3). Nutritional status, such as body mass index (BMI), is one of the key factors that categorizes the phenotypes in patients with TB (4). Prevalence of being underweight was approximately 3-fold higher in patients with TB (5). Poor nutritional status is associated with increased severity and mortality of TB disease (6, 7). According to a large study conducted in India, each unit increase in BMI at baseline is associated with a 22% reduction in mortality (8).
Despite the economic growth over the last century, the world still faces a heavy burden of malnutrition that crosses geographical and generational boundaries. The United Nations estimated that 118 million more people experienced hunger in 2020 than in 2019 (9). Undernutrition, which is a key social determinant of health, requires urgent attention (10). Climate change threatens food production and distribution systems in regions with high TB burden. Undernutrition and food security issues are likely to become more prevalent owing to the COVID-19 pandemic and ongoing conflicts with increased forced migration (11).
Despite the increasing number of studies on the impact of nutrition on TB, several gaps remain to be addressed (2, 12). First, BMI has been extensively used to assess the nutritional status in clinical practice because of its easy accessibility. However, many prior studies have used either BMI as a continuous variable or dichotomized nutritional status based on a single BMI cut-off (typically 18.5 kg/m2) (13). Using BMI as a continuous variable implies its linear relationship with the outcome of interest. A binary BMI variable cannot differentiate among different degrees of nutritional status, which may have various impacts on health outcomes (14). In addition, association between being overweight and treatment outcome has not been extensively studied (7, 15). Therefore, we aimed to evaluate the impact of being underweight and overweight on anti-TB treatment outcome. Furthermore, men and women with TB have different clinical presentation and treatment outcomes. Indeed, significant differences were found regarding location of TB in the body and disease severity between sexes, especially during women's reproductive age (16). In addition, sex differences in anti-TB treatment outcomes were observed (17). Women are particularly vulnerable to nutritional deficiencies because of the cyclical iron loss and childbearing. It is known that poor nutrition in early life reduces females' learning potential, worsens reproductive and maternal health risks, and decreases productivity. However, how the effects of nutritional deficit on TB differ according to sex has not yet been thoroughly investigated. We hypothesized that impact of nutritional status at the baseline on anti-TB treatment outcomes would be different between men and women with TB.
To address these research gaps, we assessed data from the validated nationwide TB cohort registry in Korea and evaluated whether the effects of being underweight or overweight on all-cause mortality vary by sex among patients with pulmonary TB.
In the Republic of Korea, a country with an intermediate TB burden (18), physicians are required to report the diagnosis and treatment of TB when it is first diagnosed or suspected. Under the public–private mix (PPM) TB control project (19), all patients are monitored and reported until treatment completion by TB nurse specialists at PPM-participating hospitals. Approximately 77.4% of newly registered TB patients in Korea were treated at PPM hospitals in 2020. Within this project, we constructed the Korean TB Cohort Database, a prospective observational registry database, which comprised TB patients notified at PPM-participating hospitals, regardless of age and sex. In this database, every TB patient notified from the 1st to the 10th day of each month was consecutively enrolled across the country. For this study, the only exclusion criterion was extra-pulmonary TB. Finally, the data of patients with pulmonary TB who were notified from January 2019 to December 2020 were retrieved from the national registry database (Figure 1).
Our study was designed as a prospective cohort study, which aimed to assess association between nutritional status and mortality. All the notified TB patients were followed up until the end of anti-TB treatment to confirm their treatment outcomes. The anti-TB treatment outcomes were defined according to the Korean TB guidelines adopted from the World Health Organization. During this period, data of participants were collected by TB specialist nurses using the case report form.
Baseline characteristics such as age, sex, BMI, smoking and alcohol history, prior anti-TB treatment history, and coexisting comorbidities were collected as independent variables. We used standard BMI categories for the Asian population: underweight (<18.5 kg/m2), normal weight (18.5–22.9 kg/m2), and overweight (≥23.0 kg/m2). The results of radiographic and microbiological tests, such as sputum acid-fast bacilli (AFB) smear and culture tests, nucleic acid amplification test (NAAT), and drug susceptibility test, were also collected. We collected data on TB-related symptoms using a predefined checklist that included cough, sputum production, dyspnea, chest pain, hemoptysis, fever, general weakness, and body weight loss. If patients denied all the listed symptoms, they were regarded as asymptomatic. The primary outcome of interest was all-cause mortality during anti-TB treatment. The cause of death was further classified as TB-related or non-TB-related based on the medical death certificate.
The baseline characteristics of all enrolled patients are presented as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables. Continuous variables were compared using the t-test, and categorical variables were compared using the chi-square test or Fisher's exact test. To explore the associations between initial clinical presentation (TB-related symptoms, positive results of smear, culture, NAAT, and chest radiographic findings of cavitary and bilateral diseases) and BMI among patients with pulmonary TB, their proportions were plotted against BMI (a continuous variable). The adjusted odds ratios (aORs) for four baseline severity indices (symptom presence, AFB smear positivity, and cavitary and bilateral disease) were calculated using multivariable logistic regression, which was adjusted for age, sex, current smoking status, heavy alcohol intake, and presence of comorbidities.
To explore the impact of BMI on the mortality (all-cause mortality, TB-related death, and non-TB-related death) among patients with pulmonary TB, their proportions were plotted against the BMI (as a continuous variable) and additionally stratified by sex. The aORs for mortality were calculated using logistic regression. For multivariable analysis, age, sex, current smoking status, heavy alcohol intake, and presence of comorbidities were adjusted. For the interaction analysis between BMI and sex, interaction terms with sex and BMI were further added to the previous model, and subgroup analyses of the multivariable logistic regression model were performed separately in male and female patients. For a sensitivity analysis, we excluded patients with resistance to isoniazid or rifampicin and followed the same analytical process to explore the effect of BMI on mortality in patients with isoniazid- and rifampicin-susceptible pulmonary TB.
We conducted extended analyses to assess the impact of BMI categories on mortality among patients with pulmonary TB. First, we categorized patients according to BMI into three groups–underweight, normal weight, and overweight–and set the normal weight group as a reference for logistic regression analysis. Second, we calculated the ORs for the mortality in the underweight group with respect to the normal weight reference group. Univariable and multivariable logistic regression analyses were performed. Interaction and subgroup analyses of the multivariable analyses stratified by sex were then conducted. Third, the ORs for mortality in the overweight group were calculated using the same analytical process. All statistical analyses were performed using R software (version 4.2.1). A p < 0.05 was considered statistically significant.
This study was conducted in accordance with the principles of the Declaration of Helsinki. The Institutional Review Board of Ilsan Paik Hospital, Inje University approved the study protocol (ISPAIK 2021-08-012). The Korea Disease Control and Prevention Agency (KDCA) has the authority to hold and analyze surveillance data for public health and research purposes. The KDCA approved the data use and provided the data without personal identification information.
A total of 9, 721 patients with pulmonary TB, with the mean age of 61.8 years, and 3, 544 (36.5%) female patients were included (Table 1). The mean value of BMI was 21.3 ± 3.4; 1, 927 (19.8%) were underweight, and 2, 829 (29.1%) overweight. Among the enrolled patients, 22.1% were current smokers, 8.2% were heavy drinkers, and 61.1% had underlying comorbidities. The proportions of current smokers and heavy drinkers in the underweight group were 23.2 and 10.8%, respectively, which were significantly higher than those in the other groups. The proportions of resistance to isoniazid and rifampicin were 5.4% (522) and 1.5% (151), respectively.
At least one TB-related symptom was observed in 64.6% of the patients. The most common symptom was cough with or without sputum (41.3%), followed by dyspnea (16.0%) (Supplementary Table S1). Cough, with or without sputum, had a negative linear association with BMI (Supplementary Figure S1). The positivity rates for the AFB smear, NAAT, and AFB culture were 26.2, 41.0, and 53.2%, respectively. Cavitary and bilateral lesions on chest radiography were observed in 15.7 and 30.9% of patients, respectively. The proportion of positive microbiological test results was negatively correlated with BMI (Supplementary Figure S2). Similar trends were observed for cavitary and bilateral diseases on chest radiographs. In the multivariable logistic regression analysis, we observed a consistent inverse relationship between BMI and all baseline severity indices: symptom presence (aOR = 0.942, 95% confidence interval [CI] = 0.930–0.954), positive AFB smear test results (aOR = 0.918, 95% CI = 0.905–0.931), cavitary disease (aOR = 0.926, 95% CI = 0.910–0.942), and bilateral disease (aOR = 0.919, 95% CI = 0.907–0.932) (Table 2).
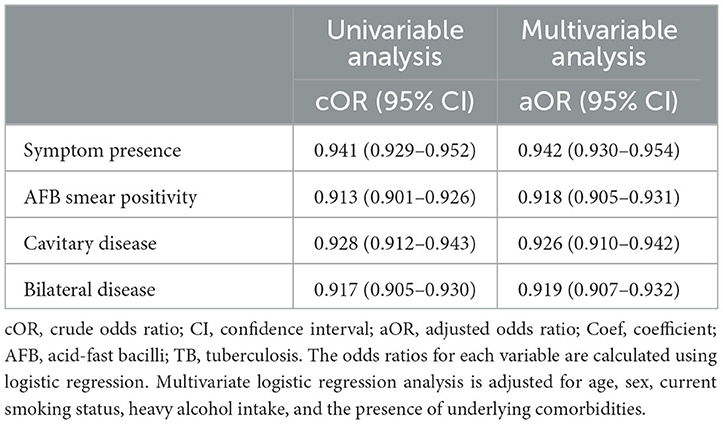
Table 2. Effect of body mass index on initial clinical presentation among patients with pulmonary tuberculosis.
During the course of anti-TB treatment, 1, 101 (11.3%) deaths occurred, including 244 (2.5%) TB-related and 837 (8.6%) non-TB-related deaths. The proportion of all-cause mortality was decreased as BMI increased; however, the slopes became less steep after a BMI of 22 kg/m2 (Figure 2A), especially among female patients (Figure 2B). Both TB-related and non-TB-related deaths showed similar decreasing trends. At all BMI intervals, female patients had higher rates of TB-related death than male patients did (Figure 2C). In contrast, the non-TB-related death rate was higher in male patients than in female patients (Figure 2D). All-cause mortality was increased with the decrement of BMI (aOR = 0.893, 95% CI = 0.875–0.911) (Table 3). Both TB-related (aOR = 0.878, 95% CI = 0.844–0.914) and non-TB-related (aOR = 0.909, 95% CI = 0.889–0.929) deaths were also increased with the decrement of BMI. We did not identify any interaction between BMI and sex with respect to the mortality rate. After excluding 559 patients with isoniazid- or rifampicin-resistant pulmonary TB, we further conducted a sensitivity analysis to assess association between BMI and mortality among 9, 162 patients with isoniazid- and rifampicin-susceptible pulmonary TB, which revealed the similar findings to those in the original analysis (Table 4).

Figure 2. Presence of subtypes of mortality according to body mass index in pulmonary tuberculosis patients. (A) All-cause mortality and TB-related and non-TB-related deaths. (B) All-cause mortality stratified by sex. (C) TB-related death stratified by sex. (D) Non-TB-related death stratified by sex. TB, tuberculosis.
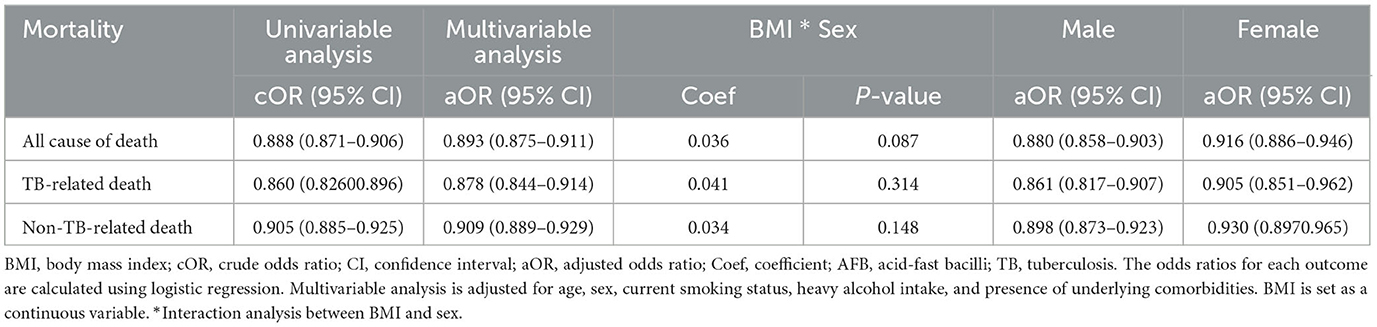
Table 3. Effect of body mass index on mortality among all the enrolled patients with pulmonary tuberculosis.
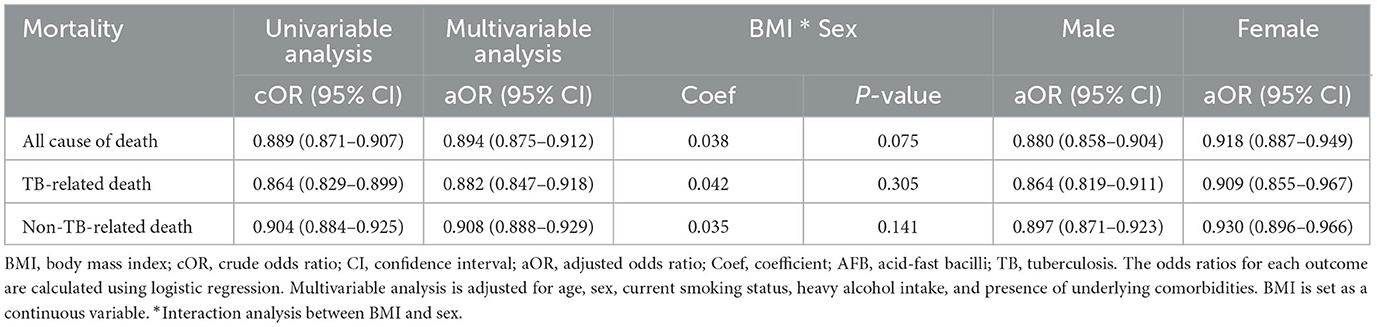
Table 4. Sensitivity analysis of the effect of body mass index on mortality among 9,162 patients with isoniazid- and rifampicin-susceptible pulmonary tuberculosis.
We categorized BMI into three groups and conducted a subgroup analysis to assess the impact of underweight and overweight status on mortality (Table 5). Underweight individuals had significantly higher odds of death, especially TB-related deaths (aOR = 2.057, 95% CI = 1.546–2.735). Its association with male patients was higher (aOR = 2.078, 95% CI = 1.717–2.514), compared with female patients (aOR = 1.724, 95% CI = 1.332–2.231). Being overweight had a negative correlation with both TB-related (aOR = 0.692, 95% CI = 0.452–0.995) and non-TB-related death (aOR = 0.793, 95% CI = 0.659–0.955). However, the negative association between being overweight and TB-related death was statistically significant solely in female patients (aOR = 0.500, 95% CI = 0.268–0.934). In contrast, the protective effects of being overweight on non-TB-related deaths were significant only in male patients (aOR = 0.739, 95% CI = 0.587–0.930).
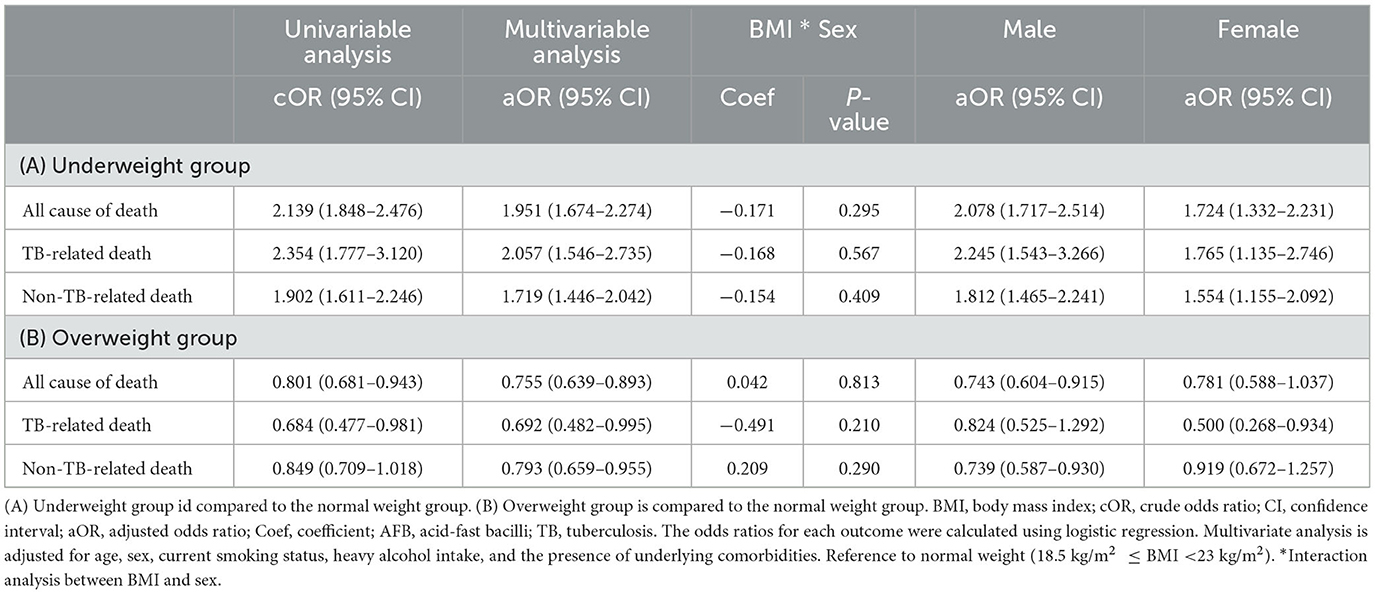
Table 5. Subgroup analysis of the effect of body mass index on mortality among all the enrolled patients with pulmonary tuberculosis.
To our knowledge, this is the largest observational study using a prospectively collected nationwide database to evaluate the impact of underweight and overweight status on the initial disease severity and mortality of pulmonary TB. Using nationwide surveillance data from Korea, we identified the impact of baseline nutrition on the clinical presentation and prognosis in patients with pulmonary TB. A higher BMI was associated with a severe initial clinical presentation and worse prognosis. Compared to patients with a normal weight, those who were underweight had severe baseline disease and higher mortality, and those who were overweight had mild baseline disease and lower mortality. The protective effects of being overweight on TB-related and non-TB-related deaths differed between male and female patients.
We found that not only in low- and middle-income countries but also in high-income countries, such as Korea, undernutrition still existed in the twenty first century, and this deleteriously affected the outcomes of anti-TB treatment. Based on our findings, clinicians should actively assess the nutritional status of patients with pulmonary TB at treatment initiation to determine the risk of unfavorable outcomes, recognize the possible causes of undernutrition, and assist in restoring their underlying nutrition. According to a retrospective observational study in Korea (20), which investigated longitudinal changes in BMI from diagnosis to a 2-year follow-up, the majority of patients were able to recover their body weight during the early phase of anti-TB treatment; however, their BMI at the end of the 2-year follow-up period was still lower than that of the general population. A recent large prospective cohort study in India (13) found that severe undernutrition at treatment initiation and lack of BMI increase during treatment were associated with 4- and 5-fold higher mortality rates, respectively. It is necessary to systematically screen nutritional status at treatment initiation, identify and monitor those with undernutrition, and provide nutritional support to ensure that patients can gain weight.
The detrimental impact of undernutrition on mortality rate was higher in male patients than in female patients in our study. Men are more susceptible to contracting TB and have a more severe clinical presentation and poorer outcomes than women. This sex disparity may be due to a combination of biological, epidemiological, and sociocultural factors. For example, men are more likely to be addicted to tobacco and alcohol, both of which are risk factors for TB development. Because men and women with the same BMI status have different body compositions, men with lower fat mass and less energy reserves at the time of TB diagnosis might be at a greater risk of death than women (21). However, few research studies evaluated sex differences in the context of association between BMI and mortality during TB treatment, which requires further attention.
Obesity, which is frequently accompanied by metabolic syndrome, is typically associated with a higher prevalence of cardiovascular disorders, cancer, and diabetes as well as a shortened life expectancy. In contrast, recent studies (22–24) showed a clear inverse relationship between BMI and TB incidence, which suggests an obesity paradox. According to the recent population-based longitudinal study, higher BMI also reduced long-term mortality among TB survivors (25). However, effect of being overweight on mortality during anti-TB treatment was controversial (7, 15). One of our key findings was the protective impact of being overweight on the clinical presentation and mortality in patients with pulmonary TB, based on the results of our multivariable logistic regression analysis. This phenomenon of better clinical outcomes among obese patients has been frequently observed in many diseases, such as cardiovascular disease (26). Higher daily protein and energy intakes among obese patients, which could improve immune function, could benefit TB outcomes.
It is noteworthy that the protective effects of being overweight on TB-related- and non-TB-related deaths differed between female and male patients. The protective effect of being overweight on TB-related death, which is frequently observed during the early phase of anti-TB treatment, was apparent in female patients. This aligns well with the finding of milder forms of initial clinical presentation in female patients, which could be associated with a lower likelihood of early TB-related death. In male patients, being overweight was associated with a lower rate of non-TB-related death, which occurred during the late phase of anti-TB treatment. There are several common modes of death among patients with non-TB-related conditions, such as acute respiratory failure, cancer, septic shock, and cardiovascular disease, including sudden cardiac death (27). Male patients may benefit more from being overweight in avoiding these complications, which could be ascribed to the obesity paradox (28). Because we used BMI to define overweight status and did not collect other data, we could not identify the mechanisms that could explain our results. Knowledge of other aspects of being overweight and obesity, such as body composition, visceral adiposity, sarcopenic obesity, and cardiac fitness, will help to better explain the relationship between being overweight and TB outcomes.
The key strength of our study is the analysis of a large number of notified TB cases collected systematically across the country, representing the actual TB burden in Korea. Thus, policymakers can use it to prioritize curative and preventive action plans. However, this study has several limitations that should be acknowledged. We could not collect additional laboratory findings, such as blood cell counts and C-reactive protein, albumin, and interferon-gamma levels, owing to the lack of relevant inflammatory biomarkers in the prospective design of a nationwide cohort database. This study was performed in a high-income country with an intermediate TB burden and a low prevalence of human immunodeficiency virus infection, which may limit the generalizability of our findings.
In conclusion, being underweight at treatment initiation was associated with severe clinical presentation and a higher mortality rate among patients with pulmonary TB. In contrast, being overweight was associated with better outcomes, depending on patient sex. Although a large amount of literature supports the importance of controlling undernutrition among patients with TB, it has not been emphasized in the TB world in terms of both research and clinical aspects. Nutritional assessment at the time of TB diagnosis should be incorporated into standard TB care. Furthermore, it is necessary to design and implement appropriate nutritional support programs to improve the treatment outcomes in malnourished patients with TB.
The data analyzed in this study is subject to the following licenses/restrictions: The Korea Disease Control and Prevention Agency (KDCA) has the authority to hold and analyze surveillance data for public health and research purposes. The KDCA approved the data use and provided the data without personal identification information. Requests to access these datasets should be directed to H-KK, gusrud9@yahoo.co.kr.
The studies involving humans were approved by Institutional Review Board of Ilsan Paik Hospital, Inje University. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the study analyzed surveillance data for public health and research purposes.
JM and H-KK conceived the study, performed all analyses, and drafted the manuscript. JSK, SL, and JP supervised the research project. JM, JSK, HK, YK, JO, Y-JJ, EL, BY, KL, JA, JWK, YH, SL, JP, and H-KK collected data. All authors have read and approved the final manuscript.
The Public-Private Mix Tuberculosis Control Project was supported by the National Health Promotion Fund, funded by the Korea Disease Control and Prevention Agency, Republic of Korea.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1236099/full#supplementary-material
1. Stephenson J. WHO report: years of progress in global tuberculosis upset by COVID-19 pandemic. JAMA Health Forum. (2022) 3:e224994. doi: 10.1001/jamahealthforum.2022.4994
2. Sinha P, Bhargava A, Carwile M, Cintron C, Cegielski JP, Lönnroth K, et al. Undernutrition can no longer be an afterthought for global efforts to eliminate TB. Int J Tuberc Lung Dis. (2022) 26:477–80. doi: 10.5588/ijtld.22.0197
3. Cho SH, Lee H, Kwon H, Shin DW, Joh H-K, Han K, et al. Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study. Sci Rep. (2022) 12:16207. doi: 10.1038/s41598-022-20550-8
4. Koo H-K, Min J, Kim HW, Ko Y, Oh JY, Jeong Y-J, et al. Cluster analysis categorizes five phenotypes of pulmonary tuberculosis. Sci Rep. (2022) 12:10084. doi: 10.1038/s41598-022-13526-1
5. Badawi A, Gregg B, Vasileva D. Systematic analysis for the relationship between obesity and tuberculosis. Public Health. (2020) 186:246–56. doi: 10.1016/j.puhe.2020.06.054
6. Hoyt KJ, Sarkar S, White L, Joseph NM, Salgame P, Lakshminarayanan S, et al. Effect of malnutrition on radiographic findings and mycobacterial burden in pulmonary tuberculosis. PLoS ONE. (2019) 14:e0214011. doi: 10.1371/journal.pone.0214011
7. Yen YF, Tung FI, Ho BL, Lai YJ. Underweight increases the risk of early death in tuberculosis patients. Br J Nutr. (2017) 118:1052–60. doi: 10.1017/S0007114517003166
8. Bhargava A, Chatterjee M, Jain Y, Chatterjee B, Kataria A, Bhargava M, et al. Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality. PLoS ONE. (2013) 8:e77979. doi: 10.1371/journal.pone.0077979
9. FAO UNICEF. WFP WHO in Brief to the State of Food Security and Nutrition in the World 2021. Transforming Food Systems for Affordable Healthy Diets. Rome: FAO (2020).
11. Hendriks SL, Montgomery H, Benton T, Badiane O, Mata GCd, Fanzo J, et al. Global environmental climate change, covid-19, and conflict threaten food security and nutrition. BMJ. (2022) 378:e071534. doi: 10.1136/bmj-2022-071534
12. Sinha P, Lönnroth K, Bhargava A, Heysell SK, Sarkar S, Salgame P, et al. Food for thought: addressing undernutrition to end tuberculosis. Lancet Infect Dis. (2021) 21:e318–e25. doi: 10.1016/S1473-3099(20)30792-1
13. Sinha P, Ponnuraja C, Gupte N, Babu SP, Cox SR, Sarkar S, et al. Impact of undernutrition on tuberculosis treatment outcomes in india: a multicenter prospective cohort analysis. Clin Infect Dis. (2022) 8:1483–91. doi: 10.2139/ssrn.4077891
14. Sinha P, White LF, Hochberg NS, Cegielski JP. Avoiding pitfalls in calculating the population attributable fraction of undernutrition for TB. Int J Tuberc Lung Dis. (2022) 26:80. doi: 10.5588/ijtld.21.0634
15. Yen Y-F, Chuang P-H, Yen M-Y, Lin S-Y, Chuang P, Yuan M-J, et al. Association of body mass index with tuberculosis mortality: a population-based follow-up study. Medicine. (2016) 95:e2300. doi: 10.1097/MD.0000000000002300
16. Min J, Park JS, Kim HW, Ko Y, Oh JY, Jeong Y-J, et al. Differential effects of sex on tuberculosis location and severity across the lifespan. Sci Rep. (2023) 13:6023. doi: 10.1038/s41598-023-33245-5
17. Feng J-Y, Huang S-F, Ting W-Y, Chen Y-C, Lin Y-Y, Huang R-M, et al. Gender differences in treatment outcomes of tuberculosis patients in Taiwan: a prospective observational study. Clin Microbiol Inf. (2012) 18:E331–E7. doi: 10.1111/j.1469-0691.2012.03931.x
18. Min J, Kim HW, Kim JS. Tuberculosis: Republic of Korea, 2021. Tuberc Respir Dis. (2023) 86:67–9. doi: 10.4046/trd.2022.0111
19. Min J, Kim HW, Ko Y, Oh JY, Kang JY, Lee J, et al. Tuberculosis surveillance and monitoring under the national public-private mix tuberculosis control project in South Korea 2016-2017. Tuberc Respir Dis. (2020) 83:218–27. doi: 10.4046/trd.2020.0016
20. Ko Y, Kim C, Park YB, Mo EK, Moon JW. Changes in nutritional status in pulmonary tuberculosis: longitudinal changes in bmi according to acid-fast bacilli smear positivity. J Clin Med. (2020) 9:12. doi: 10.3390/jcm9124082
21. Mupere E, Zalwango S, Chiunda A, Okwera A, Mugerwa R, Whalen C. Body composition among HIV-seropositive and HIV-seronegative adult patients with pulmonary tuberculosis in Uganda. Ann Epidemiol. (2010) 20:210–6. doi: 10.1016/j.annepidem.2009.11.001
22. Kim SJ, Ye S, Ha E, Chun EM. Association of body mass index with incident tuberculosis in Korea. PLoS ONE. (2018) 13:e0195104. doi: 10.1371/journal.pone.0195104
23. Cegielski JP, Arab L, Cornoni-Huntley J. Nutritional risk factors for tuberculosis among adults in the United States, 1971-1992. Am J Epidemiol. (2012) 176:409–22. doi: 10.1093/aje/kws007
24. Choi H, Yoo JE, Han K, Choi W, Rhee SY, Lee H, et al. Body mass index, diabetes, and risk of tuberculosis: a retrospective cohort study. Front Nutr. (2021) 8:739766. doi: 10.3389/fnut.2021.739766
25. Choi H, Han K, Jung JH, Park SH, Kim SH. Long-term mortality of tuberculosis survivors in korea: a population-based longitudinal study. Clin Infect Dis. (2023) 76:e973–e81. doi: 10.1093/cid/ciac411
26. Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. (2021) 26:27–35. doi: 10.1007/s40519-019-00815-4
27. Min J, Kim JS, Kim HW, Shin AY, Koo H-K, Lee S-S, et al. Clinical profiles of early and tuberculosis-related mortality in South Korea between 2015 and 2017: a cross-sectional study. BMC Infect Dis. (2019) 19:735. doi: 10.1186/s12879-019-4365-9
Keywords: tuberculosis, undernutrition, nutrition, death, mortality, body mass index
Citation: Min J, Kim JS, Kim HW, Ko Y, Oh JY, Jeong Y-J, Lee EH, Yang B, Lee KM, Ahn JH, Kim JW, Hwang YI, Lee SS, Park JS and Koo H-K (2023) Effects of underweight and overweight on mortality in patients with pulmonary tuberculosis. Front. Public Health 11:1236099. doi: 10.3389/fpubh.2023.1236099
Received: 07 June 2023; Accepted: 31 August 2023;
Published: 19 September 2023.
Edited by:
Adwoa Asante-Poku, University of Ghana, GhanaReviewed by:
Yih-Yuan Chen, National Chiayi University, TaiwanCopyright © 2023 Min, Kim, Kim, Ko, Oh, Jeong, Lee, Yang, Lee, Ahn, Kim, Hwang, Lee, Park and Koo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyeon-Kyoung Koo, gusrud9@yahoo.co.kr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.