
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 28 July 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1233975
This article is part of the Research TopicElucidating the Determinants Between the Environment and Individuals’ Behaviors Amidst the COVID-19 Pandemic and the Post-COVID EraView all 25 articles
 Junzhe Cheng1,2†
Junzhe Cheng1,2† Mei Liao1,3†
Mei Liao1,3† Ziping He2
Ziping He2 Rui Xiong4
Rui Xiong4 Yumeng Ju1,3
Yumeng Ju1,3 Jin Liu1,3
Jin Liu1,3 Bangshan Liu1,3
Bangshan Liu1,3 Bei Wu5*
Bei Wu5* Yan Zhang1,3
Yan Zhang1,3Background: Chinese people experienced a nationwide coronavirus disease 2019 (COVID-19) pandemic after the adjustment of epidemic response policies from December 2022 to January 2023. This study aims to explore the prevalence of mental and cognitive symptoms and their associated factors among medical students after the COVID-19 pandemic.
Methods: A cross-sectional study was conducted between February 27th and March 8th, 2023. The symptoms of anxiety, depression, insomnia, post-traumatic stress disorder (PTSD), and cognitive function among medical students were examined using the Generalized Anxiety Disorder-7 (GAD-7), the Patient Health Questionnaire-9 (PHQ-9), the Athens Insomnia Scale (AIS), the Impact of Event Scale-6 (IES-6), and the Perceived Deficits Questionnaire-Depression-5 (PDQ-D-5). Data on demographic information was also collected. Statistical analyses were conducted to describe the prevalence and explore the associated factors of mental and cognitive symptoms.
Results: Among 947 participants, the proportion of students experiencing anxiety, depression, insomnia, and PTSD symptoms was 37.8, 39.3, 28.3, and 29.5%, respectively. The self-reported COVID-19 infection rate was 72.2%. Higher grades, childhood, and current rural residence were identified as potential risk factors for mental and cognitive symptoms. Gender, age, average monthly household income, and COVID-19 diagnosis were not associated with mental and cognitive symptoms among medical students.
Conclusion: Our findings revealed a high prevalence of mental and cognitive symptoms among Chinese medical students after the COVID-19 pandemic. Special attention should be paid to the mental health of higher-grade students and those residing in rural areas.
With the alterations of the Chinese epidemic prevention policy, China experienced a nationwide wave of the coronavirus disease 2019 (COVID-19) pandemic from December 2022 to January 2023. The Chinese Center for Disease Control and Prevention (CDC) reported a 6.94 million peak in the number of infected people (1). According to reports, the general public’s physical and mental health has been adversely affected by the COVID-19 epidemic (2, 3). To embark on targeted therapies after the COVID-19 pandemic, it is imperative to emphasize people’s mental health and identify the susceptible population. Compared to other social populations, college students exhibited a higher vulnerability to the COVID-19 outbreak, encountering uncertainty and unexpected disruptions to their academic semesters (4). The COVID-19 pandemic and subsequent quarantine measures gave rise to various outcomes for college students (5). They found it challenging academically to transition from traditional face-to-face learning to online learning (6, 7). Long-term isolation at home and minimal social interaction may contribute to mental disorders, including depression and anxiety (8).
Medical students were considered a high-risk group for suffering from mental disorders (9). The mental health of medical students had already started to deteriorate prior to the COVID-19 pandemic (10–12). Some of them even actively participated in efforts to provide COVID-19 aid during the pandemic (11, 13). Additionally, lockdown measures including digital learning, home quarantine, and social distancing were unprecedented experiences for them. A cross-sectional survey conducted on medical students in China showed that the outbreak of COVID-19 aggravated medical students’ negative emotional outcomes (14). During the long-term pandemic, medical students tended to suffer from several cognitive symptoms and mental disorders, such as anxiety, depression, insomnia, post-traumatic stress disorder (PTSD), and cognitive dysfunction (15–17). The impaired mental health and cognitive function may negatively impact the future professional identity and capacity to care for patients. Examining the extent of physical and psychological well-being in the post-epidemic era is crucial for ensuring the future quality of healthcare services (18).
Medical students were considered as a high-risk group for mental disorders (9). The mental health of medical students had already started to deteriorate prior to the COVID-19 pandemic (10–12). Some medical students even actively participated in efforts to provide COVID-19 aid during the pandemic (11, 13). Additionally, lockdown-associated changes including digital learning, home quarantine, and social distancing were unprecedented experiences for them. A cross-sectional survey conducted on medical students in China showed that the outbreak of COVID-19 aggravated medical students’ negative emotional outcomes (14). During the long-term pandemic, medical students tended to suffer from several cognitive symptoms and mental disorders, such as anxiety, depression, insomnia, post-traumatic stress disorder (PTSD), and cognitive dysfunction (15–17). The impaired mental health and cognitive function may negatively impact their enthusiasm and capacity to care for patients. Examining the level of physical and psychological well-being of medical students in the post-epidemic era is crucial for ensuring the quality of healthcare services in the future (18).
Previous studies primarily investigated the physical and mental well-being of college students during the early stage of the pandemic from 2020 to 2022 (19, 20). Although extensive research has been conducted on the initial phases of the epidemic, inadequate effort has been emphasized for medical students in the post-COVID-19 period. However, most of the students who were infected during the first wave of the COVID-19 pandemic in China were psychologically prepared for the subsequent infection, given their prior experience. As a result, they may perceive themselves well-informed about the pandemic during this period, which might reduce their anxiety and fear (21, 22). Moreover, residence (urban or rural) and family income stability are also associated with psychological well-being (23). In response, we conducted a survey on Chinese medical students to investigate the prevalence and severity of mental and cognitive symptoms and their associated factors, and to provide validated empirical data on mental health and cognitive function after the COVID-19 pandemic. Our study was expected to enrich the evidence of mental health and cognitive function among medical students in the post-COVID-19 period and provide clues for identifying a targeted population for psychological intervention.
A cross-sectional survey was conducted offline using nonprobability sampling among medical students. It started on February 27th, 2023, and ended on March 8th, 2023, after China experienced the first round of the COVID-19 pandemic nationwide. The survey was administered offline using paper questionnaires at Central South University, Changsha, Hunan, China. A total of 1,049 medical students participated in the survey. Every student who followed the survey gave informed consent about the research protocol. Participants who met the following criteria were included: (1) medical students, (2) students studying at Central South University, and (3) volunteered for the survey. The exclusion criteria included missing or inadequate information and/or any major physical or mental illness. Ultimately, 947 medical students were included in the study.
This study had been approved by the Ethics Committee of the Second Xiangya Hospital of Central South University (approval number: 047).
Participants provided demographic information on their age, gender, grade, average monthly household income, childhood residence, current residence, history of physical illness, psychiatric history, and whether they had been diagnosed with COVID-19 infection.
The seven-item General Anxiety Disorder-7 (GAD-7) was used to record anxiety symptoms (24). Participants rated the frequency of experiencing seven symptoms during the previous 2 weeks as: (0) not at all, (1) on several days, (2) on more than half of the days, and (3) nearly every day. Scores range from 0 to 21, with higher scores indicating more anxiety symptoms. The total score S of GAD-7 is categorized as follows: S ≤ 4 = minimal symptoms; 5 ≤ S ≤ 9 = mild symptoms; 10 ≤ S ≤ 13 = moderate symptoms; 14 ≤ S ≤ 18 = moderately severe symptoms; S ≥ 19 = severe symptoms. With a Cronbach’s alpha of 0.879, the GAD-7 in the current sample shows a strong level of internal consistency.
Depressive symptoms were assessed using the nine-item Patient Health Questionnaire (PHQ-9) (25, 26). A Likert scale (0 = “Not at all” to 3 = “Nearly every day”) was used to assess the frequency of experiencing nine symptoms during the previous 2 weeks. Scores range from 0 to 27, with higher scores indicating more depressive symptoms. The total score S of PHQ-9 is categorized as follows: S ≤ 4 = minimal symptoms; 5 ≤ S ≤ 9 = mild symptoms; 10 ≤ S ≤ 14 = moderate symptoms; 15 ≤ S ≤ 19 = moderately severe symptoms; S ≥ 20 = severe symptoms. The PHQ-9 in the current sample has shown an internal consistency of 0.908 (Cronbach’s alpha).
The eight-item Athens Insomnia Scale (AIS) was used to record the severity of insomnia for all subjects (27). A Likert scale including five items related to sleep difficulties and three related to daytime functional impairment (0 = “Not at all” to 3 = “Extremely”) was used to assess the severity during the past month. The total score ranges from 0 to 24 points. Previous studies have confirmed that a score of 6 is a reasonable cutoff for insomnia (28). On this basis, an AIS score < 4 was defined as normal, a 4 ≤ score < 6 was defined as suspected insomnia, and a score ≥ 6 was defined as insomnia. The AIS in the current sample has internal consistency (Cronbach’s alpha, 0.805).
The level of PTSD is usually measured by the Impact of Event Scale-6 (IES-6) for research in epidemiological studies or clinical practice. IES-6 is validated and shortened based on the Impact of Events Scale-Revised (IES-R) (29). Participants were asked to report their PTSD symptoms in the past 7 days on six items from 0 (not at all) to 4 (extremely). Scores range from 0 to 24, with higher scores indicating more PTSD symptoms. It can associate the COVID-19 pandemic with PTSD symptoms through its three subscales (intrusion, avoidance, and hyperarousal). We used the mean score S of IES-6 to measure the level of PTSD: S < 1.09 = normal; 1.09 ≤ S < 1.5 = showing PTSD symptoms; S ≥ 1.5 = may be diagnosed with probable PTSD (30). The IES-6 in our study sample showed an internal consistency of 0.862 (Cronbach’s alpha).
The five-item Perceived Deficits Questionnaire-Depression (PDQ-D-5) was used to record the severity of self-reported cognitive symptoms over the previous 7 days (31). The frequency of experiencing these symptoms is rated using a scale ranging from 0 to 4 (0 = “not at all” to 3 = “nearly every day”). The total score ranges from 0 to 20, with higher scores indicative of more severe cognitive symptoms. With a Cronbach’s alpha of 0.852, the PDQ-D-5 in the current sample exhibits a favorable score for internal consistency.
Data were analyzed using SPSS Version 25.0 (IBM SPSS, Armonk NY, USA). Descriptive statistical analyses were conduct to exhibit the sample’s demographic profile and level of mental health and cognitive function. Reliability tests were used to check the internal consistency of IES-6, GAD-7, PHQ-9, AIS, and PDQ-D-5 in the current sample. Based on the data type and data distribution, independent t-tests, person correlation analysis and spearman correlation analysis were respectively adopted to examine the relationships between participants’ demographics and mental health, sleep quality, and cognitive function. A two-tailed p<0.05 was considered statistically significant.
The general demographic characteristics of these 947 medical students are shown in Table 1. The final sample of participants for the present study consisted of 947 medical students, with a median age of 18.88 (SD: 0.23) years and the majority of participants between the ages of 15 and 24. Four hundred and fifty-nine (48.5%) male and five hundred and twelve (51.5%) female participants responded to the survey. The sample of medical students consists of 521 freshmen (55.0%) and 426 sophomores (45.0%). Most participants had an average monthly household income of <10,000 yuan (81.1%). Most participants had the urban census register in childhood (65.2%), and the ratio has increased to 82.2% at present. Most participants reported a history of a positive diagnosis of COVID-19 (72.2%).
Overall, the proportion of participants reporting mild, moderate, moderately severe, and severe anxiety symptoms was 28.0, 6.1, 2.7, and 1.0%, respectively. The proportion of participants reporting mild, moderate, moderately severe, and severe depressive symptoms was 30.2, 6.3, 1.9, and 0.8%, respectively. The proportions of participants reporting suspected insomnia and insomnia were 31.2 and 28.3%, respectively. Whereas, the proportions of participants reporting PTSD symptoms and probable PTSD were 13.2 and 16.3%, respectively (Figure 1).
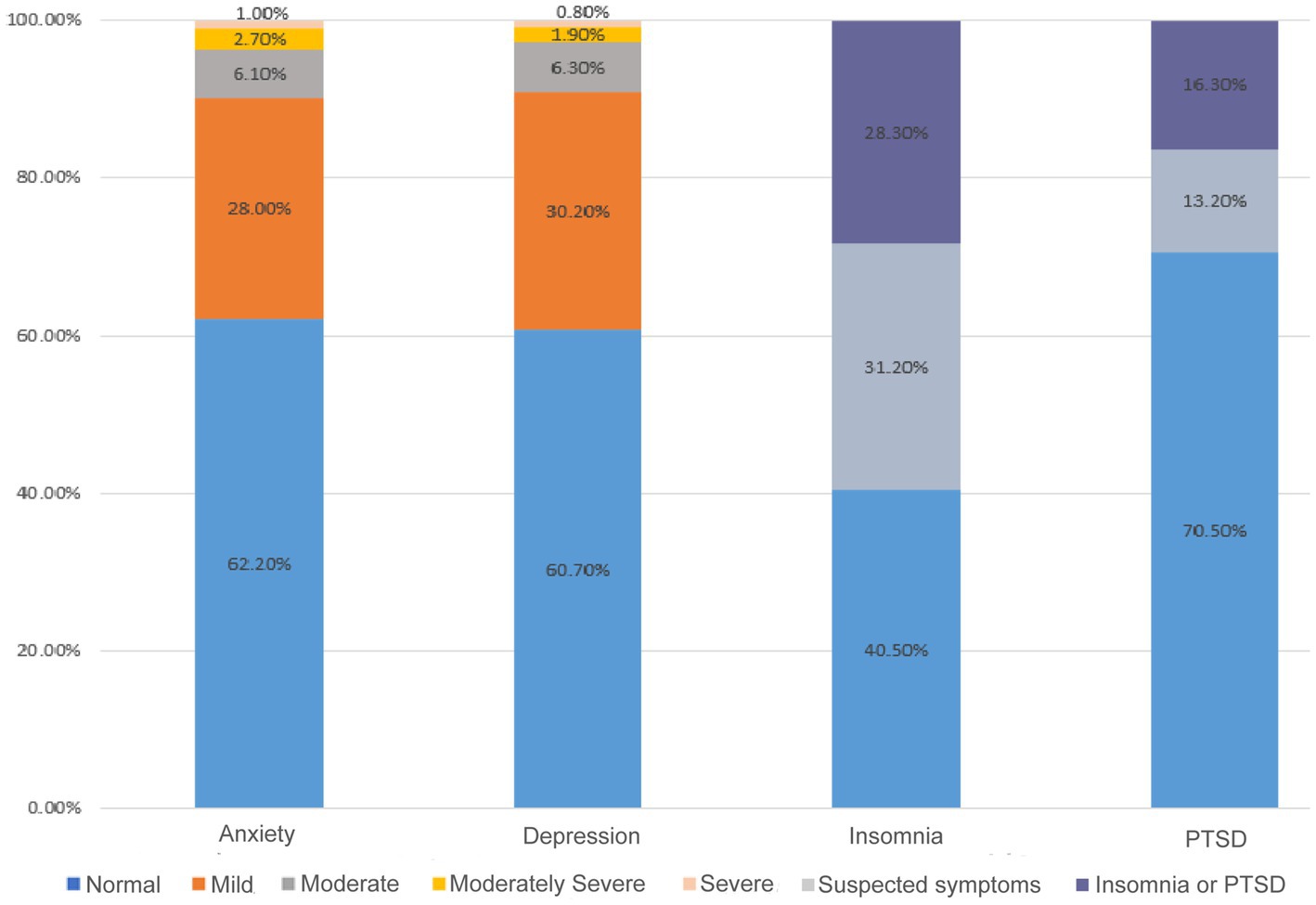
Figure 1. The prevalence of anxiety, depression, insomnia, and PTSD symptoms among medical students. PTSD: post-traumatic stress disorder.
Table 2 displays the factors that may be associated with mental and cognitive symptoms. There were no significant gender differences in either mental health or cognitive function. It was found that compared to freshmen, sophomores had higher levels of anxiety symptoms (p = 0.03), depressive symptoms (p < 0.01), insomnia (p < 0.01), and PTSD symptoms (p < 0.01). Moreover, there was no significant difference in cognitive symptoms between different grades. The rural students showed significantly higher cognitive symptoms both in their childhood residence (p < 0.01) and current residence (p = 0.03) than the urban students. However, there was no significant difference in mental health and cognitive function whether the participant was diagnosed with COVID-19 or not.
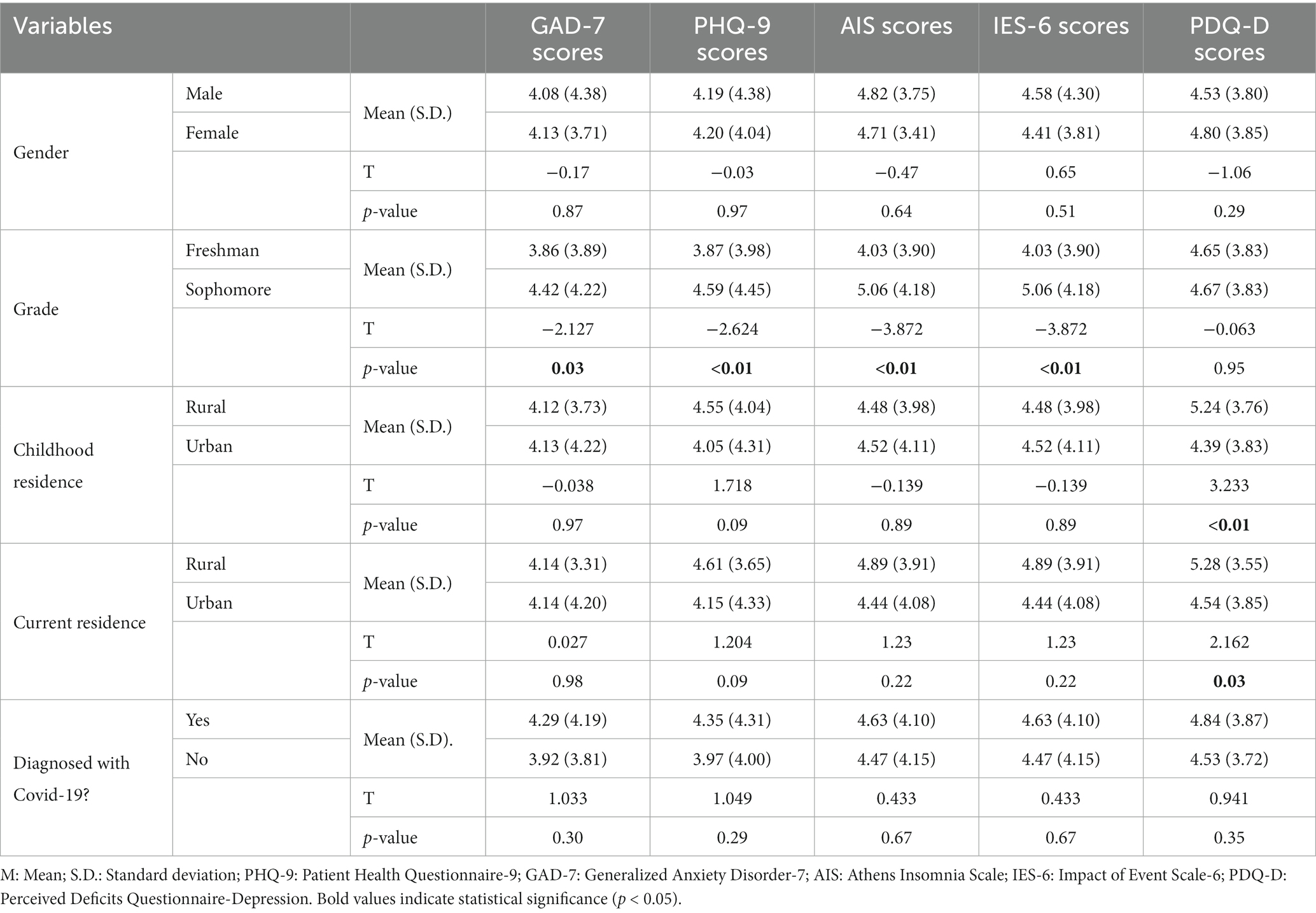
Table 2. Independent t-tests of sociodemographic characteristics and mental health of medical students.
In the correlation analysis of age with mental problems and cognitive symptoms, the grade was considered as a covariate. Childhood and current residence were taken as covariates in the correlation analysis of average monthly household income with mental problems and cognitive symptoms. Table 3 displays the results of the bivariate partial correlation analysis of age, average monthly household income, anxiety, depression, insomnia, PTSD, and cognitive symptoms. There were statistically significant positive correlations between anxiety, depression, insomnia, PTSD, and cognitive symptoms. None of the mental or cognitive symptoms were significantly correlated with age or the average monthly household income.
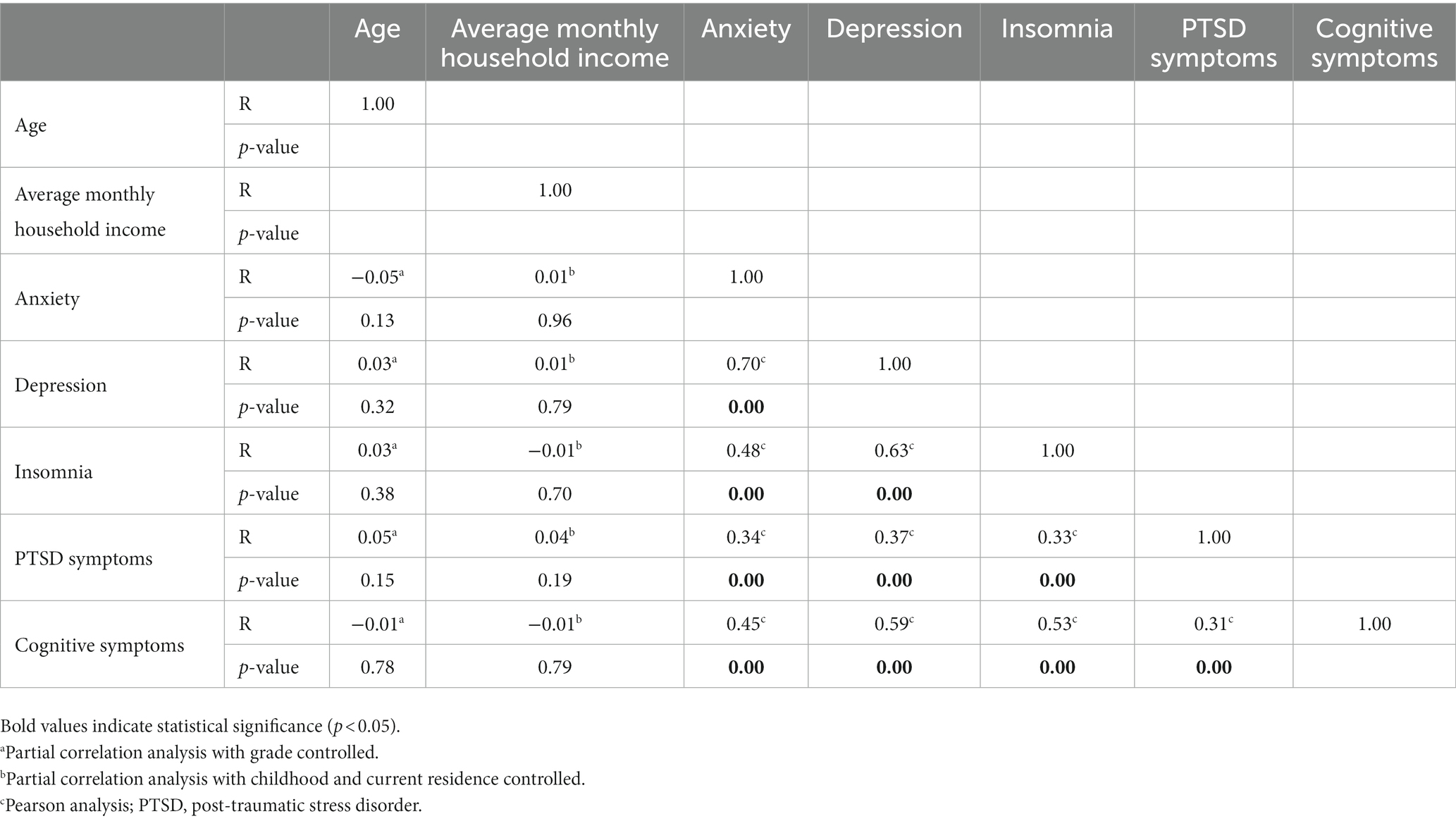
Table 3. Correlation analysis of age, average monthly household income, mental health, and cognitive function of medical students.
To the best of our knowledge, this is the first study that has examined the mental health and cognitive function of medical students after the first nationwide COVID-19 pandemic in China. Particularly, few studies investigated the cognitive function of medical students during or after the COVID-19 pandemic. The proportions of medical students who experienced symptoms of anxiety, depression, insomnia, or PTSD were 37.8, 39.3, 28.3, and 29.5%, respectively, which were significantly higher than general college students post COVID-19 pandemic (32–34). A cross-sectional study of medical students in Greece during the COVID-19 pandemic reported a higher prevalence of anxiety (67.6%), depression (43.7%), and insomnia (65.9%) than our study (35). It is possible that in our study, with sufficient knowledge about the coronavirus infection and long-term adaptation to the pandemic and quarantine policies, the prevalence of mental and symptoms in medical students faded away to a lower level. Our study showed no significant differences in mental health and cognitive function between male and female students. It might be owing to the similar stresses and negative emotions among male and female medical students as a result of the environment of medical education (23). In addition, sophomores were statistically more likely to experience anxiety, depression, insomnia, and PTSD symptoms than freshmen. It is possible due to increasing pressure from learning, exams, and career choices in higher-grade students.
It is interesting to note that despite receiving a COVID-19 diagnosis, the mental health and cognitive function of the medical students have not changed significantly. Prior investigations have demonstrated that the COVID-19 pandemic’s detrimental repercussions dramatically elevated levels of anxiety and depression (36–38). However, after the long-standing COVID-19 pandemic, the negative impacts, including stigma and fear of COVID-19, progressively subsided in China. Moreover, we speculated that a series of COVID-19-related factors jointly impair the mental health of medical students during the COVID-19 pandemic, including the lockdown measurement, the disruption of clinical training or plans, the excessive learning stress, long screen time due to online learning, less social contact, less exercise, exposure to high-risk environments, and a lack of capacity to handle the unpredictable incident effectively (39–42). The COVID-19 infection is merely one of the factors impairing mental health. Since the COVID-19 pandemic has ended and epidemic policy has been altered, some of the social influences previously mentioned did not pose a threat to medical students anymore.
Medical students with childhood or current rural census registers had significantly higher PDQ-D-5 scores, indicating worse cognitive function compared with urban medical students. Due to the financial, cultural, and educational differences between rural and urban environments, rural medical students may experience an inadaptation to a new life when coming to a university in an urban area (43). The inadaptation may induce concentration and memory decreases, which cause significant differences in PDQ-D-5 scores between rural and urban students. These results indicated the importance of considering the adaptation of rural medical students to the college environment. There was no significant difference between rural and urban students concerning anxiety, depression, insomnia, or PTSD symptoms. The finding of undifferentiated mental health among medical students from rural and urban regions does not corroborate the findings of other rural–urban disparities surveys in China, which generally show that rural college students tend to have worse mental health (depression and anxiety) than urban students (44). However, a prior survey also showed that there was no significant difference in the prevalence of some mental disorders (anxiety, insomnia) between rural and urban students (45). It does not imply that the data collected from regular college students or medical students was “incorrect” or “not replicated.” Rather, these inconsistent findings reveal the importance of considering the differences between medical and nonmedical college students in terms of their respective learning environments, educational cultures, and social expectations.
Some limitations are important to consider in light of the current investigation. The survey was conducted in the first and second months after the COVID-19 epidemic instead of during the pandemic. Hence, the variations in prevalence at other time points could not be detected. Moreover, several associated factors, such as the major of medical students, the impact of COVID-19 on students’ family, quarantine experience, and history of mental illness, have not been explored in this study. It may interfere with the accuracy of the rates of mental health problems among participants. Also, the participants were recruited from low-grade medical students at Central South University. It is incapable to represent the medical students across the whole country. Therefore, future investigations should recruit medical students from different schools and different regions across the country to constitute a more representative sample.
Overall, the study investigated the current status of mental health and cognitive function in medical students. We analyzed the correlation between sociodemographic characteristics and mental health and cognitive function in medical students and speculated on the potential factors that may induce the significant difference in each group. These findings will contribute to confirming the high-risk populations and providing target interventions to support medical students who suffered various mental and cognitive dysfunctions post-COVID-19 pandemic.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Xiangya Hospital of Central South University (approval number: 047). The patients/participants provided their written informed consent to participate in this study.
JC, ML, ZH, BW, YZ, and BL designed the study and wrote the protocols. JC, ML, JL, YJ, RX, BL, and BW participated in the data collection and organization. JC and ZH undertook the statistical analysis and wrote the manuscript, and then all authors participated in the revision. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chinese Center for Disease Control and Prevention (2023). Epidemic situation of COVID-19 infection in China. Available at: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_13141/202304/t20230429_265709.html [Accessed April 29, 2023]
2. Crook, H, Raza, S, Nowell, J, Young, M, and Edison, P. Long covid-mechanisms, risk factors, and management. BMJ. (2021) 374:n1648. doi: 10.1136/bmj.n1648
3. Ceban, F, Ling, S, Lui, LMW, Lee, Y, Gill, H, Teopiz, KM, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. (2022) 101:93–135. doi: 10.1016/j.bbi.2021.12.020
4. Wang, X, Zhang, N, Pu, C, Li, Y, Chen, H, and Li, M. Anxiety, depression, and PTSD among college students in the post-COVID-19 era: a cross-sectional study. Brain Sci. (2022) 12:1553. doi: 10.3390/brainsci12111553
5. Zhang, D, Qin, L, Huang, A, Wang, C, Yuan, T, Li, X, et al. Mediating effect of resilience and fear of COVID-19 on the relationship between social support and post-traumatic stress disorder among campus-quarantined nursing students: a cross-sectional study. BMC Nurs. (2023) 22:164. doi: 10.1186/s12912-023-01319-4
6. Zhang, Y, Wang, D, Zhao, J, CHEN, XY, Chen, H, Ma, Z, et al. Insomnia and other sleep-related problems during the remission period of the COVID-19 pandemic: a large-scale survey among college students in China. Psychiatry Res. (2021) 304:114153. doi: 10.1016/j.psychres.2021.114153
7. Wang, F, Zhang, L, Ding, L, Wang, L, and Deng, Y. Fear of COVID-19 among college students: a systematic review and Meta-analysis. Front Public Health. (2022) 10:846894. doi: 10.3389/fpubh.2022.846894
8. Ke, T, Li, W, Sanci, L, Reavley, N, Williams, I, and Russell, MA. The mental health of international university students from China during the COVID-19 pandemic and the protective effect of social support: a longitudinal study. J Affect Disord. (2023) 328:13–21. doi: 10.1016/j.jad.2023.02.014
9. Quek, TT, Tam, WW, Tran, BX, Zhang, M, Zhang, Z, Ho, CS, et al. The global prevalence of anxiety among medical students: a Meta-analysis. Int J Environ Res Public Health. (2019) 16:2735. doi: 10.3390/ijerph16152735
10. Rotenstein, LS, Ramos, MA, Torre, M, Segal, JB, Peluso, MJ, Guille, C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and Meta-analysis. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
11. Stanislawski, ER, Saali, A, Magill, EB, Deshpande, R, Kumar, V, Chan, C, et al. Longitudinal mental health outcomes of third-year medical students rotating through the wards during COVID-19. Psychiatry Res. (2023) 320:115030. doi: 10.1016/j.psychres.2022.115030
12. Frajerman, A, Morvan, Y, Krebs, MO, Gorwood, P, and Chaumette, B. Burnout in medical students before residency: a systematic review and meta-analysis. Eur Psychiatry. (2019) 55:36–42. doi: 10.1016/j.eurpsy.2018.08.006
13. Luo, C, Santos-Malave, G, Taku, K, Katz, C, and Yanagisawa, R. Post-traumatic growth and resilience among American medical students during the COVID-19 pandemic. Psychiatry Q. (2022) 93:599–612. doi: 10.1007/s11126-022-09981-8
14. Liu, Z, Liu, R, Zhang, Y, Zhang, R, Liang, L, Wang, Y, et al. Association between perceived stress and depression among medical students during the outbreak of COVID-19: the mediating role of insomnia. J Affect Disord. (2021) 292:89–94. doi: 10.1016/j.jad.2021.05.028
15. Çimen, İ, Alvur, TM, Coşkun, B, and Şükür, NEÖ. Mental health of Turkish medical students during the COVID-19 pandemic. Int J Soc Psychiatry. (2022) 68:1253–62. doi: 10.1177/00207640211066734
16. Yuan, K, Zheng, YB, Wang, YJ, Sun, YK, Gong, YM, Huang, YT, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. (2022) 27:3214–22. doi: 10.1038/s41380-022-01638-z
17. Gunnarsson, DV, Miskowiak, KW, Pedersen, JK, Hansen, H, Podlekareva, D, Johnsen, S, et al. Physical function and association with cognitive function in patients in a post-COVID-19 clinic-a cross-sectional study. Int J Environ Res Public Health. (2023) 20:5866. doi: 10.3390/ijerph20105866
18. Bashir, MBA, Mohamed, SOA, Nkfusai, CN, Bede, F, Oladimeji, O, Tsoka-Gwegweni, JM, et al. Assessment of minor psychiatric morbidity, stressors, and barriers of seeking help among medical students at the University of Khartoum, Khartoum, Sudan. Pan Afr Med J. (2020) 35:87. doi: 10.11604/pamj.2020.35.87.17512
19. Copeland, WE, McGinnis, E, Bai, Y, Adams, Z, Nardone, H, Devadanam, V, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. (2021) 60:134–141.e2. doi: 10.1016/j.jaac.2020.08.466
20. Ma, Z, Zhao, J, Li, Y, Chen, D, Wang, T, Zhang, Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. doi: 10.1017/S2045796020000931
21. Simegn, W, Dagnew, B, Yeshaw, Y, Yitayih, S, Woldegerima, B, and Dagne, H. Depression, anxiety, stress and their associated factors among Ethiopian university students during an early stage of COVID-19 pandemic: an online-based cross-sectional survey. PLoS One. (2021) 16:e0251670. doi: 10.1371/journal.pone.0251670
22. Lasheras, I, Gracia-García, P, Lipnicki, D, Bueno-Notivol, J, López-Antón, R, de la Cámara, C, et al. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with Meta-analysis. Int J Environ Res Public Health. (2020) 17:6603. doi: 10.3390/ijerph17186603
23. Cao, W, Fang, Z, Hou, G, Han, M, Xu, X, Dong, J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
24. Spitzer, RL, Kroenke, K, Williams, JBW, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
25. Zhang, YL, Liang, W, Chen, ZM, Zhang, HM, Zhang, JH, Weng, XQ, et al. Validity and reliability of patient health Questionnaire-9 and patient health Questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. (2013) 5:268–75. doi: 10.1111/appy.12103
26. Smarr, KL, and Keefer, AL. Measures of depression and depressive symptoms: Beck depression inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health Questionnaire-9 (PHQ-9). Arthritis Care Res. (2011) 63:S454–66. doi: 10.1002/acr.20556
27. Soldatos, CR, Dikeos, DG, and Paparrigopoulos, TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. doi: 10.1016/S0022-3999(00)00095-7
28. Mao, X, Zhang, F, Wei, C, Li, Z, Huang, C, Sun, Z, et al. The impact of insomnia on anxiety and depression: a longitudinal study of non-clinical young Chinese adult males. BMC Psychiatry. (2023) 23:360. doi: 10.1186/s12888-023-04873-y
29. Motlagh, H. Impact of event scale-revised. J Physiother. (2010) 56:203. doi: 10.1016/S1836-9553(10)70029-1
30. Jalloh, MF, Li, W, Bunnell, RE, Ethier, KA, O’Leary, A, Hageman, KM, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. (2018) 3:e000471. doi: 10.1136/bmjgh-2017-000471
31. Mattingly, GW, Ren, H, Christensen, MC, Katzman, MA, Polosan, M, Simonsen, K, et al. Effectiveness of Vortioxetine in patients with major depressive disorder in real-world clinical practice: results of the RELIEVE study. Front Psychol. (2022) 13:824831. doi: 10.3389/fpsyt.2022.824831
32. Basheti, IA, Assaraira, TY, Obeidat, NM, al-Abed al-haq, F, and Refai, M. Assessing anxiety and depression among students post-COVID-19: exploring associating factors. Psychol Res Behav Manag. (2023) Volume 16:1797–810. doi: 10.2147/PRBM.S409632
33. Chen, H, Feng, H, Liu, Y, Wu, S, Li, H, Zhang, G, et al. Anxiety, depression, insomnia, and PTSD among college students after optimizing the COVID-19 response in China. J Affect Disord. (2023) 337:50–6. doi: 10.1016/j.jad.2023.05.076
34. Wang, JY, Li, Q, Liu, W, Yang, Y, Wang, XG, Liu, CY, et al. Posttraumatic stress disorder symptoms among Chinese college students following the COVID-19 outbreak. Front Neurosci. (2023) 17:1075272. doi: 10.3389/fnins.2023.1075272
35. Eleftheriou, A, Rokou, A, Arvaniti, A, Nena, E, and Steiropoulos, P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. (2021) 9:775374. doi: 10.3389/fpubh.2021.775374
36. Paz, DC, Bains, MS, Zueger, ML, Bandi, VR, Kuo, VY, Cook, K, et al. COVID-19 and mental health: a systematic review of international medical student surveys. Front Psychol. (2022) 13:1028559. doi: 10.3389/fpsyg.2022.1028559
37. Saddik, B, Hussein, A, Sharif-Askari, FS, Kheder, W, Temsah, MH, Koutaich, RA, et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. Risk Manag Healthc Policy. (2020) Volume 13:2395–406. doi: 10.2147/RMHP.S273333
38. Ito, Y, Kako, J, Kajiwara, K, Kimura, Y, Kakeda, T, Hamanishi, S, et al. Impact of the COVID-19 pandemic on the mental health of nursing students in Japan: a cross-sectional study. Environ Health Prev Med. (2022) 27:40. doi: 10.1265/ehpm.22-00128
39. Simone, M, Geiser, C, and Lockhart, G. The importance of face-to-face contact and reciprocal relationships and their associations with depressive symptoms and life satisfaction. Qual Life Res. (2019) 28:2909–17. doi: 10.1007/s11136-019-02232-7
40. Feng, Q, Zhang, QL, du, Y, Ye, YL, and He, QQ. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. (2014) 9:e100914. doi: 10.1371/journal.pone.0100914
41. Liu, M, Zhang, J, Hu, E, Yang, H, Cheng, C, and Yao, S. Combined patterns of physical activity and screen-related sedentary behavior among Chinese adolescents and their correlations with depression, anxiety and self-injurious behaviors. Psychol Res Behav Manag. (2019) Volume 12:1041–50. doi: 10.2147/PRBM.S220075
42. Guessoum, SB, Lachal, J, Radjack, R, Carretier, E, Minassian, S, Benoit, L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
43. Saenz, JL, Downer, B, Garcia, MA, and Wong, R. Rural/urban dwelling across the life-course and late-life cognitive ability in Mexico. SSM Popul Health. (2022) 17:101031. doi: 10.1016/j.ssmph.2022.101031
44. Sun, X, Wang, ZJ, Li, YY, Chan, KQ, Miao, XY, Zhao, S, et al. Trends of college students' mental health from 2005 to 2019 and its rural-urban disparities in China. J Affect Disord. (2022) 302:160–9. doi: 10.1016/j.jad.2022.01.042
Keywords: medical students, post-COVID-19 period, mental health, cognitive function, risk factors
Citation: Cheng J, Liao M, He Z, Xiong R, Ju Y, Liu J, Liu B, Wu B and Zhang Y (2023) Mental health and cognitive function among medical students after the COVID-19 pandemic in China. Front. Public Health. 11:1233975. doi: 10.3389/fpubh.2023.1233975
Received: 07 June 2023; Accepted: 14 July 2023;
Published: 28 July 2023.
Edited by:
Ayesha Mumtaz, Hangzhou Normal University, ChinaReviewed by:
Shaohua Hu, Zhejiang University, ChinaCopyright © 2023 Cheng, Liao, He, Xiong, Ju, Liu, Liu, Wu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bei Wu, d3ViZWl0cmVlQGhvdG1haWwuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.