- 1Department of Health Policy and Management, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 2Department of Natural Science, Duke Kunshan University, Kunshan, China
- 3Institute for Disaster Management and Reconstruction (IDMR), Sichuan University, Chengdu, China
- 4Institute for Hospital Management, West China Hospital, Sichuan University, Chengdu, China
Background: The COVID-19 pandemic has exacerbated the trends of childhood overweight, obesity, and malnutrition, as well as increased psychological stress and family conflicts among family members. It is important to explore the relationship between changes in the family environment during the COVID-19 on child nutrition.
Objective: This study aims to analyze the nutritional status of Chinese children during the COVID-19 pandemic and its relationship with family diet, family environment, and parental anxiety, in order to provide evidence for further interventions in children’s nutritional status.
Method: This study included 7,645 primary and secondary school students and their parents from five schools in Chengdu, China. Chi-square tests were used to analyze the categorical variables of children’s malnutrition, overweight, obesity, and parental anxiety. T-tests were used to assess changes in the continuous variable of family environment between two rounds of follow-up surveys. Multiple logistic regression analysis was employed to examine the impact of changes in family diet during the COVID-19 pandemic on children’s nutritional status. Generalized estimating equations were used to analyze the effects of family environment and parental anxiety on childhood obesity.
Result: The prevalence of malnutrition and obesity decreased from 11.64% and 11.60% in wave 1 to 4.96% and 10.50% in wave 2, and the rate of overweight increased from 13.11% in wave 1 to 13.73% in wave 2. Children whose families reduced consumption of staple foods during the COVID-19 were more likely to be frail, and families increased consumption of sugary drinks, take-out or meal delivery services, living in towns, family environmental barriers, and parental anxiety were risk factors for overweight obesity. Mother’s education level in middle and high school and low age were protective factors for overweight obesity.
Conclusion: The physical environment of the family, the emotions of family members, and children’s perceptions of the family’s soft environment can influence children’s eating behaviors, children’s nutritional intake, and malnutrition and obesity in children under public health emergencies, and family-based dietary interventions may be effective. Parents can increase consumption of healthy foods and improve the family environment, which improve their growth.
1. Introduction
During the COVID-19 pandemic, there has been a simultaneous presence of childhood overweight and obesity as well as malnutrition, with the pandemic response measures exacerbating this challenge (1, 2). According to the World Health Organization, nearly 39 million children were overweight in 2020, and there were almost 340 million overweight or obese children aged 5 to 18 years (3). Additionally, over 149 million children under the age of five experienced stunted growth, and in 2021, the global population affected by hunger reached 828 million (4). The school-age period is a nutritionally sensitive period for growth, and inadequate or excessive nutrient intake can impact children’s cognitive and physical development, as well as their long-term health in adulthood (5, 6). Good nutrition is beneficial for well-being throughout the entire lifespan (1, 7, 8).
The outbreak of the COVID-19 pandemic has brought challenges to the stability of the family environment and the emotions of family members. According to reports, during the outbreak in China, about 25 million rural migrant workers were unemployed or waiting to return to work, and nearly one-fourth of the urban employed population was economically affected (9, 10). Financial difficulties caused by the pandemic have forced many families to make cheaper and unhealthy food choices when purchasing food. Poverty and low-income families may not be able to access sufficient nutrition and food (11, 12). The “lockdown” or “semi-lockdown” situation has caused instability in the family environment, increased parental stress, increased family conflicts, and impaired family functioning, severely affecting the children’s food environment and promoting the selection and purchase of unhealthy foods (13, 14).
The daily calorie intake of children at home accounts for about 65%–72% of their total intake, making the family food environment crucial for their dietary intake and nutritional development (15, 16). In Chinese society, there is a strong culture of parental authority, with parents having high control over their children’s diet and limited autonomy for the children (17). Throughout childhood, parents make choices about purchasing and providing food, establish rules regarding meal times, meal frequency, and structure (18, 19). The family’s food consumption determines the types and frequency of food children are exposed to, and the availability and accessibility of healthy food can promote children’s intake of nutritious food (12). If the family provides a variety of fruits, vegetables, and healthy proteins, children have more opportunities to consume a range of nutrients (20, 21).
The nutrition of children is not only related to the family’s dietary consumption, but also to the family’s environmental atmosphere. In Chinese family culture, great importance is placed on family meals, where family members come together to share food, engage in emotional communication, and pass on healthy knowledge to children. This determines that the family environment in Chinese families plays an important role in children’s diet (22–24). A positive dining atmosphere can stimulate children’s appetite, reduce anxiety or resistance towards food, encourage children to taste a variety of foods, balance their nutritional intake, and promote their healthy growth (25, 26).
The theory of the family’s healthy ecosystem suggests that the family is a complex system composed of multiple interactive relationships and roles, with parents being considered as core members who guide and educate children (24, 27–29). Negative emotions of parents can affect children’s nutritional status. If parents display anxious and worried emotions, children will perceive these emotions and experience unease and stress, leading to a decrease in appetite or aversion to food, or using overeating as a way to cope with stress or anxiety (26, 30, 31).
The family is considered the most fundamental and important unit. The COVID-19 pandemic has had a wide-ranging impact on family members’ eating behaviors, childhood overweight and obesity, and intra-family relationships. These aspects have become hot topics in research, but there are still many unknown areas that require further investigation regarding changes in household food consumption as a unit, changes in the Chinese family environment, and the impact of these changes on children’s nutritional status. This study investigated the nutritional status of children after 6 and 18 months of continuous COVID-19 pandemic through a longitudinal study, enriching the understanding of the epidemiological trends of childhood overweight/obesity and malnutrition during the pandemic. Previous research has primarily focused on household dietary consumption during routine periods, but this study examined families as units to complement the understanding of changes in household dietary consumption during the COVID-19 pandemic. In China, family culture emphasizes family cohesion and close relationships, thus this study utilized the Chinese Family Assessment Instrument to assess family atmosphere and explore the relationship between family environment and child nutrition. By analyzing the association between household dietary consumption, family environment, parental anxiety, and child nutrition during the COVID-19 pandemic, this study filled gaps in relevant knowledge and can contribute to the development of effective, family-based interventions during significant public health events.
2. Materials and methods
2.1. Study design
Chengdu Positive Child Development (CPCD) (32) is a longitudinal cohort study designed to understand the status of children’s positive development as well as psychological, social, and behavioral problems. It also assesses the impact of positive child development programs on promoting the positive development of children. The study employed a multi-stage random cluster sampling method. After stratifying based on geographical and economic conditions, a total of 5 primary and secondary schools in downtown Chengdu, suburban counties, and townships were selected. Students with cognitive disabilities or those unable to independently complete the questionnaire were excluded, and all remaining students were included in the study. With two trained research assistants present in each classroom, data collection was conducted through on-site face-to-face questionnaire interviews in the classroom environment of the selected schools.
This program began with a baseline survey in December 2019. The wave 1 data (W1) was collected in June 2020 and the wave 2 data (W2) was collected in June 2021, with each wave lasting 1 month. This study used data from the first and second rounds, with a sample of 7- to 15-year-old primary and secondary school students and their parents. A total of 7,877 individuals participated in the study. Due to missing matching information between parents and students’ questionnaires, as well as a significant amount of missing data (≥20%) for some questionnaire items, the final sample consisted of 7,645 children aged 7–15.
The study was conducted in accordance with the Helsinki Declaration, and all parents and children participating in the study provided informed consent prior to inclusion. Children also obtained parental informed consent before being included in the study. The research protocol was approved by the Medical.
2.2. Measures
A basic information questionnaire was used to collect demographics about the subjects and their parents, including the gender, grade, and age of the elementary school students, and education level, age, and current place of residence.
The nutritional status of children is measured by BMI with reference to the Chinese children’s standard. Due to the restrictions on the aggregation of people during the pandemic, the basic information of students’ height and weight was reported by their parents in both waves of the survey. Overweight, obesity, and malnutrition was defined according to BMI, which was calculated by dividing weight (kg) by the square of height (m) (33, 34). According to the Chinese National Health Commission’s standards, which are based on nationwide surveys of student physical health, this study assessed the nutritional status of Chinese students. These standards take into account the genetic characteristics and environmental influences, such as socioeconomic differences, of the Chinese population. They provide percentile thresholds based on age and gender for screening the nutritional status of school-age children (6–18 years old) in China, including various ethnic groups (35, 36). “Malnutrition” refers to acute malnutrition caused by an immediate deficiency in dietary protein and energy intake, resulting in a body mass index (BMI) below the age-specific BMI threshold range for screening (37, 38). In this study, “moderate to severe malnutrition” and “mild malnutrition” were collectively categorized as “malnutrition.”
Regarding family diet consumption, Parents were asked since June 2020 (the wave 1 survey) about the changes in meal patterns and consumption of major foods during the pandemic, including” going outside to buy groceries,” “using take-out or meal delivery services,” “dine out in the restaurants,” “cooking at home”etc., and check the corresponding box, Including: “decreased,” “decreased a little,” “no change,” “increased a little,” and “increased.” Parents were also asked whether their household consumption of “staple food,” “vegetables,” “fruits,” and “sugary drinks and desserts,” “increased,” “remained the same,” or “decreased” during the COVID-19 pandemic.
Family environment variables were measured using the Chinese Family Assessment Instrument (C-FAI) scale developed by Shek and Ma (39). There were 33 items, and for each item, participants were asked to answer the question, “How similar is this to your family environment?.” Similarity to each statement was scored on a scale of 1–5 out of 165, with higher scores indicating less similarity to the statement. The Cronbach’s ɑ reliability of the scale in this study was tested to be 0.88.
Parental anxiety variables were measured using the Anxiety Self-Assessment Scale (SAS) scale developed by Zung (40), the SAS is an internationally influential anxiety self-assessment tool. It was introduced to China in 1986, but the five items in the scale were difficult for the general public to understand, which affected the accuracy of the scale. Chinese scholars have revised and tested the scale, and achieved a reliability Cronbach’s ɑ of 0.93. The Chinese revised version of the Self-Rating Anxiety Scale has been validated (41, 42). The SAS has 20 items and parents are asked to answer the question “How similar is this to your situation,” each entry is rated on a scale of 1–4 out of 80, the higher the score, the more severe the anxiety, and those with scores of 50 and above are judged to have anxiety. The Cronbach’s ɑ reliability of the scale in this study was tested to be 0.80.
2.3. Data analysis
The data was input using EpiData 3.2 and statistical analysis was performed using SPSS 26.0 to calculate the rates among the variables. Chi-square test or T test was used to compare whether the changes among the variables in the two waves of the survey were statistically significant. Multiple logistic regression was used to analyze the effect of changes in family diet consumption on the nutrition status of children and adolescents. A generalized estimation model was used to analyze the effects of family environment and parental anxiety on childhood overweight and obesity. A two-sided test with a test level of 0.05 was used.
3. Results
3.1. Demographic characteristics
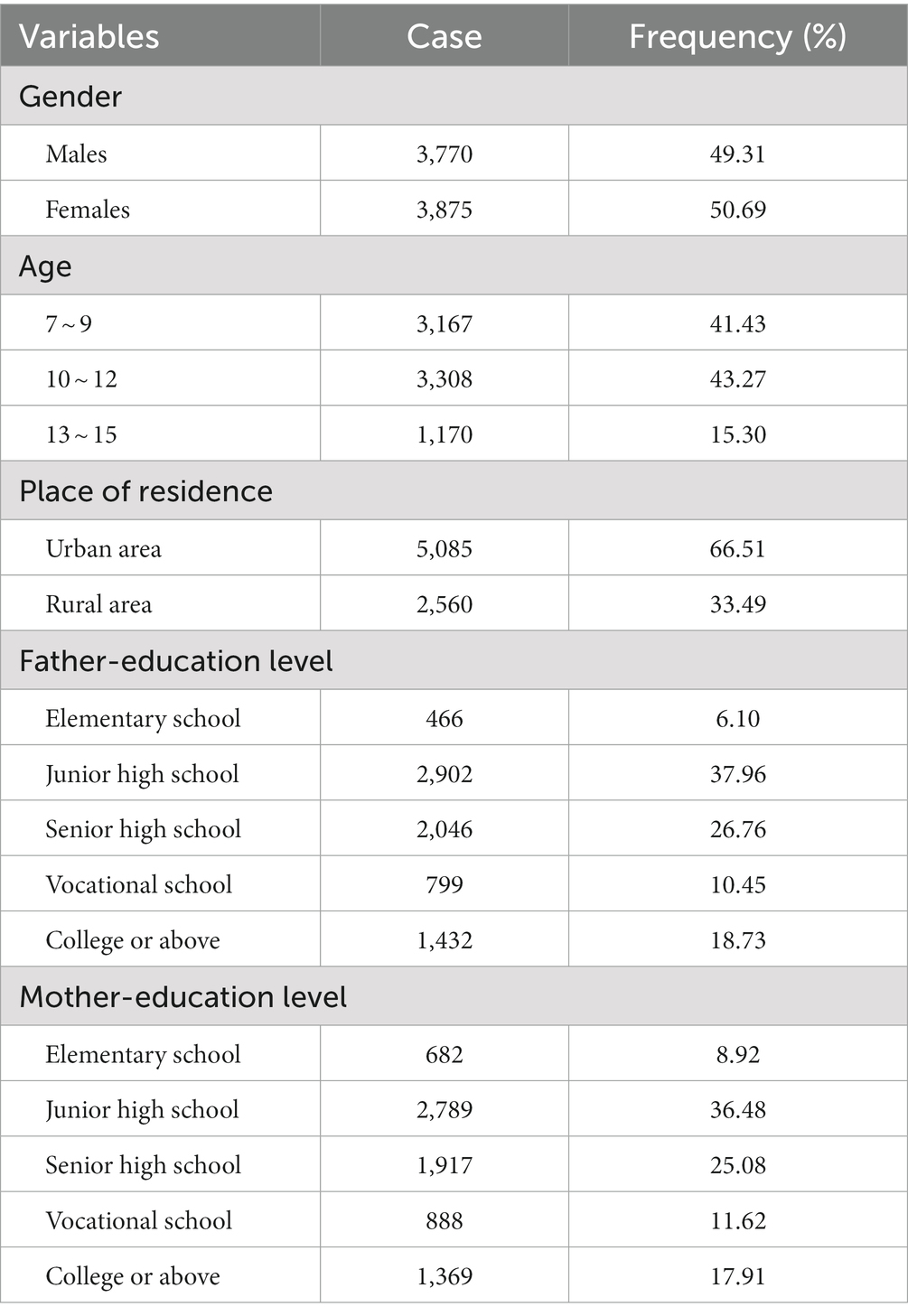
A total of 7,645 students were included in the study, of whom 3,770 (49.31%)were boys and 3,875 (50.69%)were girls; 3,167 (43.43%)were students aged 7–9 years, 3,308 (43.27%)were students aged 10–12 year, and 1,170 (15.30%)were students aged 13–15 years. 5,085 (66.51%)students were living in urban areas and 2,560 (33.49%) students were living in rural areas. 3,368 (44.05%) father’s education level was at junior high school or below, 4,277 (55.95%) at high school and above. 3,471 (45.40%) mother’s education level was at junior high school or below, and 4,714 (54.60%)at high school or above (see Table 1).
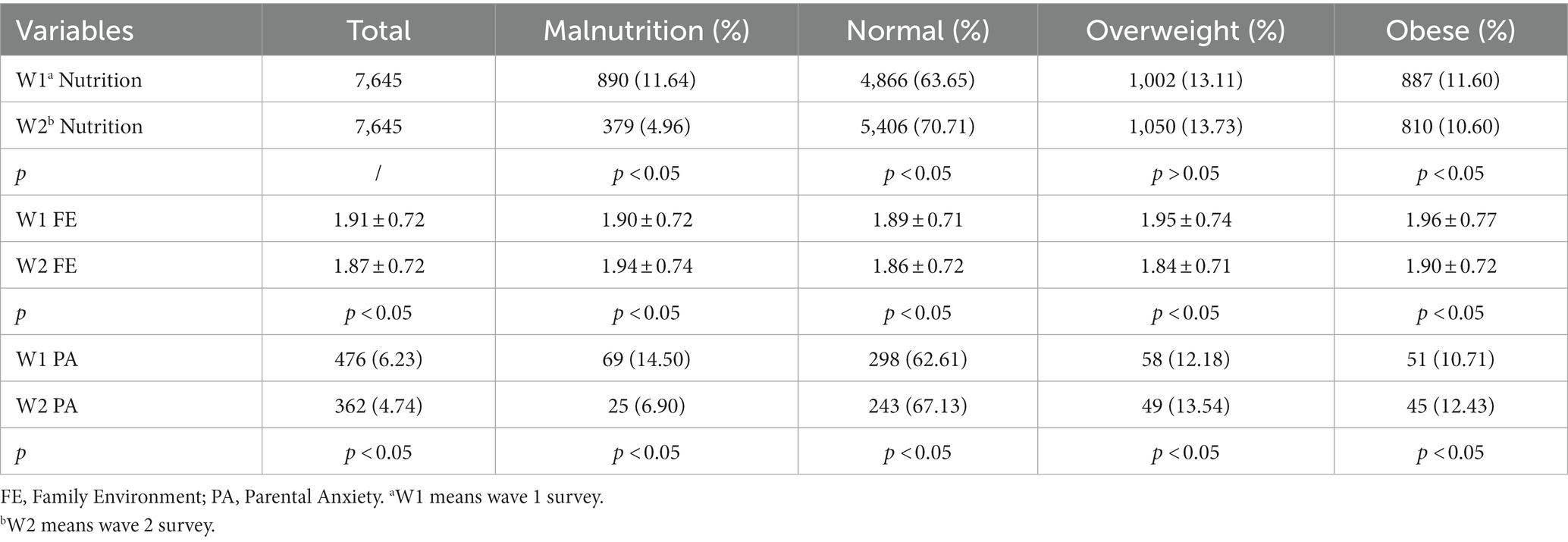
3.2. Nutrition status of children
According to the results, the prevalence rate of malnutrition in wave 1 was 11.64%, the prevalence rate of overweight was 13.11%, and the prevalence rate of obesity was 11.60%. In wave 2, the prevalence rate of malnutrition was 4.96%, the prevalence rate of overweight was 13.73%, and the prevalence rate of obesity was 10.60%. The prevalence rates of malnutrition and obesity in wave1 were higher than those in wave 2, and the differences were statistically significant (p < 0.05). As the duration of the COVID-19 pandemic increases, the prevalence of malnutrition and obesity among children has decreased (see Table 2).
Overall, the degree of family environmental barriers and the prevalence of parental anxiety were higher in wave 1 than wave 2. The degree of family environmental barriers in malnutrition children and the prevalence rate of parental anxiety in obese children were higher in wave1 than wave 2, and the differences were statistically significant. With the increasing duration of the COVID-19 pandemic, the degree of family environmental barriers increased in malnutrition children, and the level of parental anxiety increased in obese children. The family environment of obese children and the prevalence of parental anxiety in malnutrition children were higher in wave 1 than wave 2, and the differences were statistically significant (p < 0.05). With the increasing duration of the COVID-19 pandemic, the degree of family environmental barriers decreased in obese children, and the level of parental anxiety decreased in malnutrition children (see Table 2).
3.3. Family diet consumption
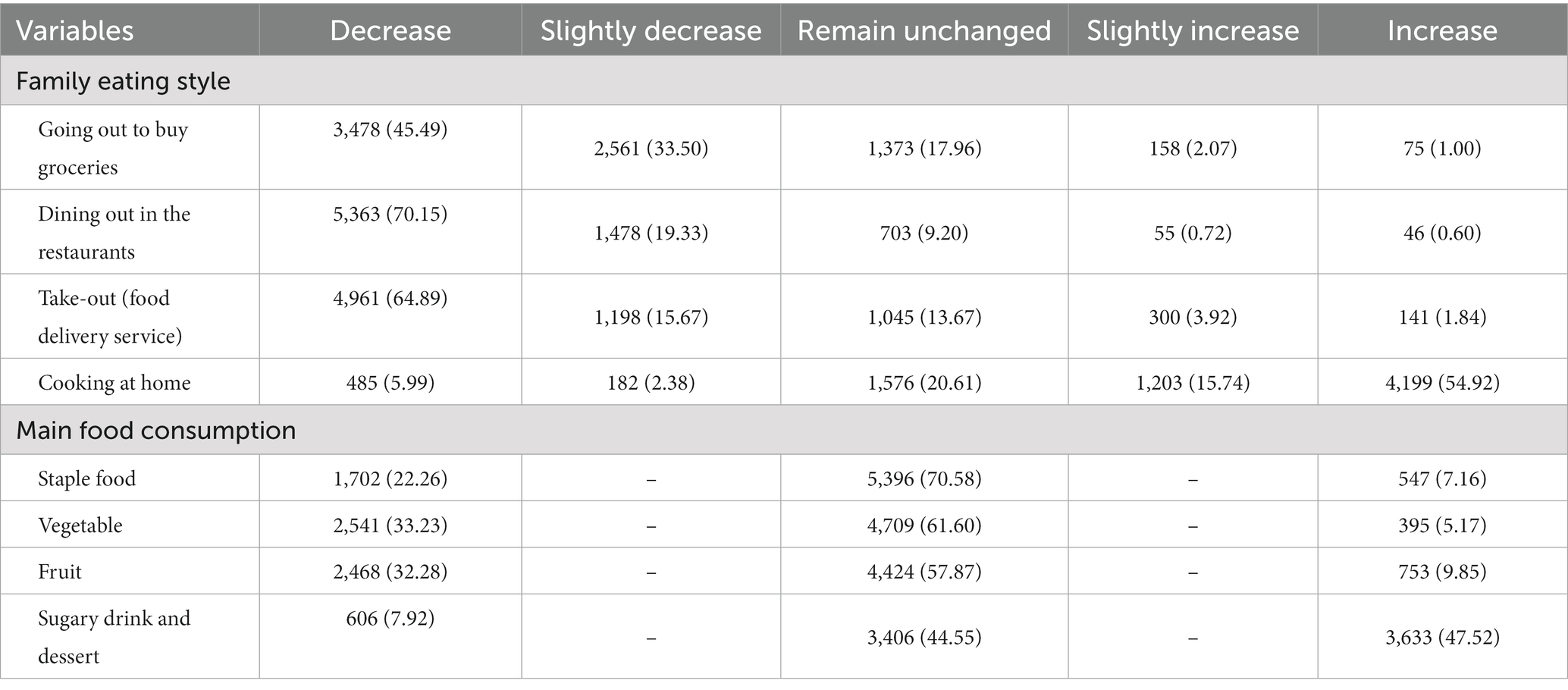
Compared to the wave 1 of surveys the wave 2 of surveys 45.49% of households decreased going to the street to buy groceries, 70.15% of households decreased eating behavior at restaurants, 64.89% of households decreased behavior through take-out or meal delivery services, 54.92% of households increased cooking behavior at home. In the second survey, 22.26% of households reduced their consumption of staple foods, 33.23% reduced their consumption of vegetables, 32.28% reduced their consumption of fruits, and 50.70% increase their consumption of sugary beverages and desserts (see Table 3).
3.4. Impact of dietary changes on the nutrition status of children
A multifactorial logistic analysis of the wave 2 of the survey showed that the prevalence rate of child malnutrition was higher in households with reduced staple food consumption compared to households with constant staple food consumption (OR = 1.88, 95%CI: 1.05–3.37), higher rates of overweight prevalence among children in families with increased take-out and meal delivery behavior (OR = 1.33, 95%CI: 1.02–1.75) compared to families with constant consumption of take-out and meal delivery services. Families with increased consumption of sugary drinks had higher prevalence rates of childhood obesity compared to families with unchanged sugary drink consumption (OR = 1.22, 95%CI: 1.01–1.48) (see Table 4).
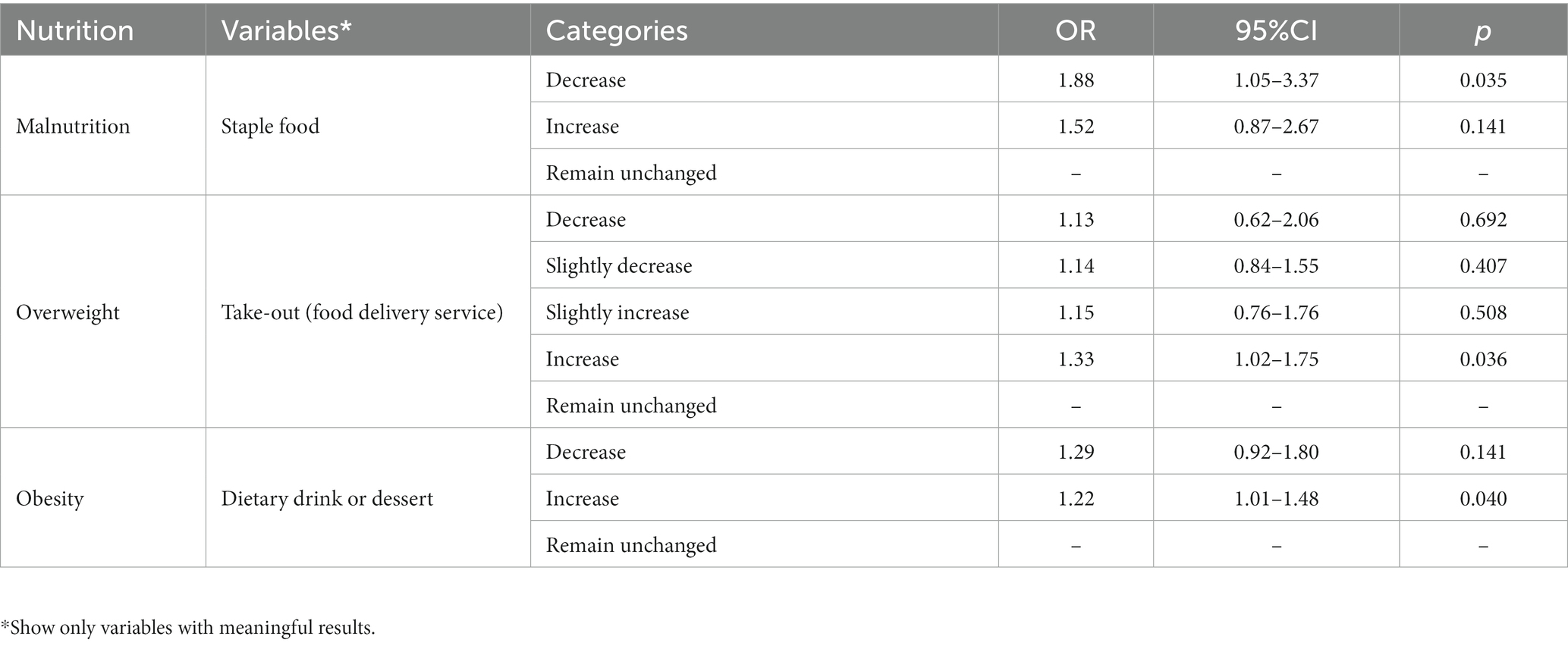
Table 4. Multifactorial unordered multi-categorial logistic regression analysis of factors influencing children’s nutrition status.
3.5. Impact of family environment and parental anxiety on the nutrition status of children
We used GEE models, exchangeable work-related matrices, ordered logistic regression, and main effects models to explore the factors influencing childhood obesity. Participants’ demographic data, family environment, and parental anxiety were entered as factors in the GEE model, and the results of the generalized estimating equations are shown in the table. Low maternal education, low age, living in town, high family dysfunction, and parental anxiety were risk factors for obesity (p < 0.05) (see Table 5).
4. Discussion
The aim of this study was to investigate the nutritional status of children in China during the COVID-19 pandemic and its association with family dietary consumption, family environment, and parental anxiety. The findings revealed that increased consumption of unhealthy food by families, chaotic or dysfunctional family environments, and heightened parental psychological stress were risk factors for childhood overweight and obesity. Furthermore, reduced consumption of staple foods by families was identified as a risk factor for childhood malnutrition.
Research has found that during the initial outbreak of the COVID-19 pandemic, the rates of childhood overweight, malnutrition, parental anxiety, and levels of family environmental disruption were higher compared to the period when the pandemic was prevalent. The drastic changes in the environment during the early stages of the COVID-19 outbreak disrupted many systems that children and parents rely on for health, livelihood, education, diet, and exercise (43, 44). The pandemic had an extremely disruptive effect on the family environment, known as the “hammer effect” (45). As the pandemic continued, on one hand, people gradually restored their daily routines, reducing the impact on children’s diet and exercise. On the other hand, families exhibited a certain level of resilience in the face of traumatic stress, which alleviated the psychological distress experienced by family members (46–48). Both family functioning and parental anxiety levels showed signs of recovery.
During the COVID-19 pandemic, reducing staple food consumption in households is a risk factor for child undernutrition. Staple foods are the main source of energy intake. A cohort study has shown that government lockdown measures significantly altered food intake (49). In 2020, the global prevalence of food insufficiency was 8.4%, with 418 million people in Asia unable to access adequate food (4, 50). Due to the severe economic recession caused by the pandemic, food access is jeopardized, and there is a positive correlation between food shortages and malnutrition (51).
Increasing consumption of take-out meals, sugary beverages, and desserts in households is a risk factor for child overweight and obesity. Take-out meals tend to be more energy-dense and have poorer nutrition, often containing high amounts of unhealthy ingredients such as fat, salt, and sugar, which are associated with weight gain and various negative health outcomes (52, 53). Compared to solid foods, sugary beverages provide less satiety and are easier to consume in excess, leading to energy accumulation. On the other hand, sugary beverages have a pleasant taste that can stimulate children’s appetite, leading to increased energy intake (10, 54, 55).
Our research found that family dysfunction and parental anxiety are risk factors for childhood obesity. Epidemiological studies have shown that family functioning plays a significant role in children’s diet and weight status (25). A chaotic family environment exacerbates negative parenting behaviors, leading to children’s preference for high-sugar, high-fat foods (14, 56). Anxious parents may use controlling or restrictive feeding practices, resulting in disrupted eating patterns and emotional eating in children, or they may be more inclined to use food as a means to soothe their children, thereby providing them with more convenient and unhealthy food options (57–59). Previous studies have indicated that there is a bidirectional relationship between family functioning and parental anxiety (60–62). Although this research provides evidence for the relationship between family functioning and nutrition, and parental anxiety and nutrition, the complex mechanisms underlying the interactions between parental anxiety, family functioning, and child nutrition have not been fully elucidated. The extent to which parental anxiety and family functioning jointly contribute to these effects, as well as whether there are mediating or moderating factors between them, requires further research.
5. Theoretical implications
Firstly, gaining a better understanding of the nutritional status of children during the ongoing COVID-19 pandemic has highlighted the changes in childhood obesity and malnutrition. This prompts us to not only focus on the issue of childhood obesity during major public health events but also pay attention to the problem of childhood malnutrition. This is important for informing the development of public health policies, which may involve food safety regulations, dietary education, social support systems, and other aspects, in order to protect the nutritional health of children.
This study provides limited evidence on the relationship between changes in household dietary consumption, family environment, parental anxiety, and child nutrition. The study suggests that dietary rules and food accessibility within the family, as well as parental emotions and parenting behaviors, can influence children’s dietary choices and quality. By further applying the theory of the family health ecosystem to research on family nutrition, the study enriches the theoretical understanding in this field. Additionally, it provides a theoretical basis for further analyzing and addressing child nutrition issues. However, it is important to note that the evidence is still limited, and further research is needed to validate and gain a deeper understanding of these relationships. Lastly, exploring the importance of the social environment in child nutrition has significant implications for policymakers and the design of intervention measures.
6. Practice implications
Research promotes the development of intervention measures, and family diet can influence children’s eating habits and intake. Family-based dietary interventions may be effective, as families can increase the consumption of healthy foods and reduce the consumption of obesity-promoting foods such as sugary beverages. At the same time, parents can improve their children’s nutritional status by establishing a supportive family environment, improving their own mental well-being, and maintaining family stability. These factors are crucial for promoting healthy eating and overall growth in children.
Research promotes family nutrition education, and the influence of family factors on child nutrition is undoubtedly important. The family is a microcosm of society, and China has its unique cultural background. For example, parents express love through food, and grandparents tend to overfeed children. When intervening in child nutrition, cultural differences should be taken into account (63). Chinese culture emphasizes parental authority and focuses on collectivism (64). In the context of Chinese social culture, it may be very effective to establish children’s healthy behaviors through role modeling and providing healthy diets. In Chinese families, the choice of what to eat is rarely an individual decision. It reminds promoters of healthy eating that nutrition education may be more effective if designed for the entire family rather than just individuals.
The research findings can provide recommendations for governments and relevant organizations to take measures to mitigate the negative impact of the COVID-19 pandemic on children’s nutrition status. This may include providing economic assistance, improving the food supply chain, promoting healthy eating campaigns, and implementing other measures to ensure children have access to adequate nutrition during the pandemic.
7. Strength, limitations, and future studies
In this study, a large sample of children and adolescents was used, focusing not only on overweight and obesity, but also on malnutrition. The study focused on the impact of “family-based” eating behaviors on children and adolescents, which was conducted 2 years into the COVID-19 pandemic, helping to complement the impact of families on the nutritional status of children and adolescents in the ongoing pandemic.
However, there are some limitations to the research. Firstly, the study sample was limited to the Sichuan province, which may reduce the generalizability of the findings. Future research could consider recruiting participants from other regions in China to have a more comprehensive understanding of the nutritional status and weight-related behaviors of Chinese children. Secondly, due to the restrictions of the COVID-19 pandemic, the height and weight of children were reported by parents rather than measured by professionals, which may affect the accuracy of the measurements. Future research could consider using professional measurements of height and weight to improve the accuracy of the data. Thirdly, the survey on household food consumption was relatively simple and may not cover the comprehensive aspects of dietary consumption. Future research could design more detailed and scientific questionnaires to have a more comprehensive understanding of household dietary consumption patterns and changes in the consumption of food types. Lastly, there may be other confounding factors that could influence the associations found in the study. Future research could consider other confounding factors such as genetics, seasonality, weather, physical conditions, and lifestyle factors to enhance the reliability of the research findings.
8. Conclusion
In summary, the material environment of the family, the emotions of family members, and children’s perceptions of the family environment can all influence children’s eating behaviors and nutritional intake. Research findings indicate that the prevalence of malnutrition and obesity among children may be more severe during the COVID-19 pandemic. As the duration of the pandemic progresses, the rate of malnutrition in children decreases significantly, while the rate of obesity slightly decreases and the rate of overweight slightly increases. Therefore, the issue of childhood overweight and obesity should not be overlooked. The COVID-19 pandemic has also led to changes in family food consumption, family functioning, and parental emotions. Reduced consumption of staple foods by families is a risk factor for child under-nutrition, while increased consumption of take-out food and sugary beverages is a risk factor for child overweight and obesity. Family dysfunction and parental anxiety are also risk factors for childhood obesity. Family food consumption, family environment, and parental emotions are all factors that influence children’s nutrition. This study provides additional insights into the changing trends of childhood overweight, malnutrition, and other related issues during the ongoing COVID-19 pandemic. It also provides a theoretical basis for family-based intervention measures.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Sichuan University ethics number: K2020025. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
LZ: funding acquisition. LP and RH: methodology. LZ and LJ: project administration and resources. LP: software and writing—original draft. RH, YF, WS, LZ, and LJ: supervision. LP, RH, YF, and WS: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National Natural Science Foundation of China, Approval No.: 82273748.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1228626/full#supplementary-material
References
1. Norris, SA, Frongillo, EA, Black, MM, Dong, Y, Fall, C, Lampl, M, et al. Nutrition in adolescent growth and development. Lancet. (2022) 399:172–84. doi: 10.1016/S0140-6736(21)01590-7
2. The Lancet Public Health. Childhood obesity beyond COVID-19. Lancet Public Health. (2021) 6:e534. doi: 10.1016/S2468-2667(21)00168-7
3. D'Auria, E, Calcaterra, V, Verduci, E, Ghezzi, M, Lamberti, R, Vizzuso, S, et al. Immunonutrition and SARS-CoV-2 infection in children with obesity. Nutrients. (2022) 14:1701. doi: 10.3390/nu14091701
4. World Health Organization. UN Report: global hunger numbers rose to as many as 828 million in 2021. Geneva: World Health Organization (2022).
5. Llewellyn, A, Simmonds, M, Owen, CG, and Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. (2016) 17:56–67. doi: 10.1111/obr.12316
6. Black, MM. Impact of nutrition on growth, brain, and cognition. Nestle Nutr Inst Workshop Ser. (2018) 89:185–95. doi: 10.1159/000486502
7. Rundle, AG, Park, Y, Herbstman, JB, Kinsey, EW, and Wang, YC. COVID-19-related school closings and risk of weight gain among children. Obesity. (2020) 28:1008–9. doi: 10.1002/oby.22813
8. The Lancet Child Adolescent Health. The hidden crisis of adolescent nutrition. Lancet Child Adolesc Health. (2022) 6:1. doi: 10.1016/S2352-4642(21)00381-3
11. Curatola, A, Ferretti, S, Gatto, A, Valentini, P, Giugno, G, Della Marca, G, et al. The effects of COVID-19 pandemic on Italian school-aged children: sleep-related difficulties and trauma reactions. J Child Neurol. (2022) 37:568–74. doi: 10.1177/08830738221096194
12. Miller, P, Moore, RH, and Kral, TV. Children's daily fruit and vegetable intake: associations with maternal intake and child weight status. J Nutr Educ Behav. (2011) 43:396–400. doi: 10.1016/j.jneb.2010.10.003
13. Fosco, GM, Sloan, CJ, Fang, S, and Feinberg, ME. Family vulnerability and disruption during the COVID-19 pandemic: prospective pathways to child maladjustment. J Child Psychol Psychiatry. (2022) 63:47–57. doi: 10.1111/jcpp.13458
14. Martin-Biggers, J, Quick, V, Zhang, M, Jin, YH, and Byrd-Bredbenner, C. Relationships of family conflict, cohesion, and chaos in the home environment on maternal and child food-related behaviours. Matern Child Nutr. (2018) 14:14. doi: 10.1111/mcn.12540
15. Rosenkranz, RR, and Dzewaltowski, DA. Model of the home food environment pertaining to childhood obesity. Nutr Rev. (2008) 66:123–40. doi: 10.1111/j.1753-4887.2008.00017.x
16. Campbell, KJ, Crawford, DA, Salmon, J, Carver, A, Garnett, SP, and Baur, LA. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity. (2007) 15:719–30. doi: 10.1038/oby.2007.553
17. Zhang, W, Wei, X, Ji, L, Chen, L, and Deater-Deckard, K. Reconsidering parenting in Chinese culture: subtypes, stability, and change of maternal parenting style during early adolescence. J Youth Adolesc. (2017) 46:1117–36. doi: 10.1007/s10964-017-0664-x
18. Scaglioni, S, De Cosmi, V, Ciappolino, V, Parazzini, F, Brambilla, P, and Agostoni, C. Factors influencing children's eating behaviours. Nutrients. (2018) 10:10. doi: 10.3390/nu10060706
19. Costa, A, and Oliveira, A. Parental feeding practices and children's eating behaviours: an overview of their complex relationship. Healthcare. (2023) 11:11. doi: 10.3390/healthcare11030400
20. Egli, V, Hunter, L, Roy, R, Te, ML, De Backer, C, Teunissen, L, et al. Household mealtimes during the 2020 COVID-19 lockdown in Aotearoa New Zealand: the influence of household type and psychological distress. Front Nutr. (2022) 9:855866. doi: 10.3389/fnut.2022.855866
21. Neufeld, LM, Andrade, EB, Ballonoff, SA, Barker, M, Beal, T, Blum, LS, et al. Food choice in transition: adolescent autonomy, agency, and the food environment. Lancet. (2022) 399:185–97. doi: 10.1016/S0140-6736(21)01687-1
22. Ma, G. Food, eating behavior, and culture in Chinese society. J Ethn Foods. (2015) 2:195–9. doi: 10.1016/j.jef.2015.11.004
23. Utter, J, Larson, N, Berge, JM, Eisenberg, ME, Fulkerson, JA, and Neumark-Sztainer, D. Family meals among parents: associations with nutritional, social and emotional wellbeing. Prev Med. (2018) 113:7–12. doi: 10.1016/j.ypmed.2018.05.006
24. Novilla, M, Barnes, MD, De La Cruz, NG, Williams, PN, and Rogers, M. Public health perspectives on the family – an ecological approach to promoting health in the family and community. Fam Community Health. (2006) 29:28–42. doi: 10.1097/00003727-200601000-00005
25. Anderson, SE, and Keim, SA. Parent-child interaction, self-regulation, and obesity prevention in early childhood. Curr Obes Rep. (2016) 5:192–200. doi: 10.1007/s13679-016-0208-9
26. Harbec, MJ, and Pagani, LS. Associations between early family meal environment quality and later well-being in school-age children. J Dev Behav Pediatr. (2018) 39:136–43. doi: 10.1097/DBP.0000000000000520
27. Grzywacz, JG, and Fuqua, J. The social ecology of health: leverage points and linkages. Behav Med. (2000) 26:101–15. doi: 10.1080/08964280009595758
28. Holland, J.M.M.S. Family matters: communicating health messages in the family. Health Education Authority Family Health Research Reports (1996).
29. Vandeweghe, L, Moens, E, Braet, C, Van Lippevelde, W, Vervoort, L, and Verbeken, S. Perceived effective and feasible strategies to promote healthy eating in young children: focus groups with parents, family child care providers and daycare assistants. BMC Public Health. (2016) 16:1045. doi: 10.1186/s12889-016-3710-9
30. Baskind, MJ, Taveras, EM, Gerber, MW, Fiechtner, L, Horan, C, and Sharifi, M. Parent-perceived stress and its association with children's weight and obesity-related behaviors. Prev Chronic Dis. (2019) 16:E39. doi: 10.5888/pcd16.180368
31. Oliver, G, Wardle, J, and Gibson, EL. Stress and food choice: a laboratory study. Psychosom Med. (2000) 62:853–65. doi: 10.1097/00006842-200011000-00016
32. Zhao, L, Shek, D, Zou, K, Lei, Y, and Jia, P. Cohort profile: Chengdu Positive Child Development (CPCD) Survey. Int J Epidemiol. (2022) 51:e95–e107. doi: 10.1093/ije/dyab237
33. Flint, SW. Error in NHS England's BMI calculator and daily calorie recommendations. Lancet. (2023) 401:913–4. doi: 10.1016/S0140-6736(23)00347-1
35. National Health and Wellness Commission of the People's Republic of China. Screening for overweight and obesity in school-age children and adolescents (2022).
36. Li, H, Zong, XN, Ji, CY, and Mi, J. Body mass index cut-offs for overweight and obesity in Chinese children and adolescents aged 2–18 years. Zhonghua Liu Xing Bing Xue Za Zhi. (2010) 31:616–20.
37. Wang, X, Hojer, B, Guo, S, Luo, S, Zhou, W, and Wang, Y. Stunting and 'overweight' in the WHO child growth standards – malnutrition among children in a poor area of China. Public Health Nutr. (2009) 12:1991–8. doi: 10.1017/S1368980009990796
38. National Health and Wellness Commission of the People's Republic of China. Screening for malnutrition in school-age children and adolescents (2022).
39. Shek, DTL, and Ma, CM. The Chinese Family Assessment INSTRUMENT (C-FAI): hierarchical confirmatory factor analyses and factorial invariance. Res Soc Work Pract. (2010) 1:112–23. doi: 10.1177/1049731509355145
40. Zung, W. Rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
41. Tao, M, and Gao, J. The validity and reliability of SAS-CR (SAS-Chinese revised). Chin J Nerv Ment Dis. (1994) 20:301–3.
42. Qian, W. Evaluation on college students’ anxiety and social media usage during Shanghai closure. Sci Insights Educ Front. (2023) 15:2227–45. doi: 10.15354/sief.23.or123
43. Kramer, A, and Kramer, KZ. The potential impact of the Covid-19 pandemic on occupational status, work from home, and occupational mobility. J Vocat Behav. (2020) 119:103442. doi: 10.1016/j.jvb.2020.103442
44. Penninx, B, Benros, ME, Klein, RS, and Vinkers, CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. (2022) 28:2027–37. doi: 10.1038/s41591-022-02028-2
45. Prime, H, Wade, M, and Browne, DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. (2020) 75:631–43. doi: 10.1037/amp0000660
46. Walsh, F. The concept of family resilience: crisis and challenge. Fam Process. (1996) 35:261–81. doi: 10.1111/j.1545-5300.1996.00261.x
47. Suzuki, K, Hiratani, M, Mizukoshi, N, Hayashi, T, and Inagaki, M. Family resilience elements alleviate the relationship between maternal psychological distress and the severity of children's developmental disorders. Res Dev Disabil. (2018) 83:91–8. doi: 10.1016/j.ridd.2018.08.006
48. Jones, LB, Kiel, EJ, Luebbe, AM, and Hay, MC. Resilience in mothers during the COVID-19 pandemic. J Fam Psychol. (2022) 36:815–26. doi: 10.1037/fam0000985
49. Huber, BC, Steffen, J, Schlichtiger, J, and Brunner, S. Altered nutrition behavior during COVID-19 pandemic lockdown in young adults. Eur J Nutr. (2021) 60:2593–602. doi: 10.1007/s00394-020-02435-6
50. World Health Organization. UN Report: pandemic year marked by spike in world hunger. Geneva: World Health Organization (2022).
51. Mumena, WA, Francis-Granderson, I, Phillip, LE, Johnson-Down, L, and Gray-Donald, K. Food insecurity is linked to dietary intake but not growth of children in the Caribbean. West Ind Med J. (2021) 69:421–6. doi: 10.7727/wimj.2016.586
52. Janssen, HG, Davies, IG, Richardson, LD, and Stevenson, L. Determinants of takeaway and fast food consumption: a narrative review. Nutr Res Rev. (2018) 31:16–34. doi: 10.1017/S0954422417000178
53. Lachat, C, Nago, E, Verstraeten, R, Roberfroid, D, Van Camp, J, and Kolsteren, P. Eating out of home and its association with dietary intake: a systematic review of the evidence. Obes Rev. (2012) 13:329–46. doi: 10.1111/j.1467-789X.2011.00953.x
54. Klevay, LM. Letter by Klevay regarding article, "long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US adults". Circulation. (2019) 140:E651. doi: 10.1161/CIRCULATIONAHA.119.041133
55. Ma, JT, McKeown, NM, Hwang, SJ, Hoffmann, U, Jacques, PF, and Fox, CS. Sugar-sweetened beverage consumption is associated with change of visceral adipose tissue over 6 years of follow-up. Circulation. (2016) 133:370–7. doi: 10.1161/CIRCULATIONAHA.115.018704
56. Romeo, RD. The teenage brain: the stress response and the adolescent brain. Curr Dir Psychol. (2013) 22:140–5. doi: 10.1177/0963721413475445
57. Dimitratos, SM, Swartz, JR, and Laugero, KD. Pathways of parental influence on adolescent diet and obesity: a psychological stress-focused perspective. Nutr Rev. (2022) 80:1800–10. doi: 10.1093/nutrit/nuac004
59. Bould, H, Koupil, I, Dalman, C, DeStavola, B, Lewis, G, and Magnusson, C. Parental mental illness and eating disorders in offspring. Int J Eat Disord. (2015) 48:383–91. doi: 10.1002/eat.22325
60. Bogels, SM, and Brechman-Toussaint, ML. Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev. (2006) 26:834–56. doi: 10.1016/j.cpr.2005.08.001
61. Westrupp, EM, Bennett, C, Berkowitz, T, Youssef, GJ, Toumbourou, JW, Tucker, R, et al. Child, parent, and family mental health and functioning in Australia during COVID-19: comparison to pre-pandemic data. Eur Child Adolesc Psych. (2023) 32:317–30. doi: 10.1007/s00787-021-01861-z
62. Feinberg, ME, A, MJ, Lee, JK, Tornello, SL, Hostetler, ML, Cifelli, JA, et al. Impact of the COVID-19 pandemic on parent, child, and family functioning. Fam Process. (2022) 61:361–74. doi: 10.1111/famp.12649
63. Wong, OL. Meaning of food in childhood obesity: an exploratory study in a Chinese family context. Soc Work Health Care. (2010) 49:362–77. doi: 10.1080/00981380903212149
Keywords: children’s nutrition status, family diet consumption, family environment, parent anxiety, COVID-19
Citation: Peng L, Hu R, Feng Y, Shi W, Zhao L and Jiang L (2023) The relationship between family diet consumption, family environment, parent anxiety and nutrition status children during the COVID-19 pandemic: a longitudinal study. Front. Public Health. 11:1228626. doi: 10.3389/fpubh.2023.1228626
Edited by:
Songlin He, Chongqing Medical University, ChinaReviewed by:
Majed Jebril, Xian Jiaotong University, ChinaJosué Edison Turpo-Chaparro, Peruvian Union University, Peru
Copyright © 2023 Peng, Hu, Feng, Shi, Zhao and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lihua Jiang, bGhqaWFuZ0BzY3UuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Lili Peng1†
Lili Peng1† Rui Hu
Rui Hu Yiwei Feng
Yiwei Feng Wei Shi
Wei Shi Li Zhao
Li Zhao Lihua Jiang
Lihua Jiang