- 1Department of Preventive Medicine, School of Health, Quanzhou Medical College, Quanzhou, China
- 2Department of Nursing, Quanzhou First Hospital, Quanzhou, China
Aim: The objective of this study is to investigate the mental health status of nurses during the outbreak of novel coronavirus pneumonia. Additionally, we aim to analyze the relationship between anxiety, depression, and burnout among nurses. The findings will provide a scientific basis for promoting the psychological health of nurses.
Methods: Using a cross-sectional study, nurses in Quanzhou in May 2020 completed a general information questionnaire, the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and the Maslach Burnout Inventory (MBI). Data analysis was conducted using structural equation model.
Results: 372 questionnaires were returned, with a response rate of 92.5%. The prevalence of anxiety and depression among the participants were 45.2 and 41.4%, respectively. The prevalence of severe burnout among nurses was found to be 7.3%. There was a correlation between nurses’ anxiety, depression, and job burnout. The correlation coefficients between anxiety and job burnout, depression and job burnout, and anxiety and depression were found to be statistically significant (p < 0.001). Depression plays a mediating role between anxiety and jod burnout (0.584/1.413, 41.3%).
Conclusion: The COVID-19 epidemic has resulted in moderate to high levels of job burnout among nurses. In this context, depression has been found to play a mediating role in the relationship between anxiety and job burnout. It is imperative for hospital administrators to prioritize the mental health of nurses and the provide necessary support to ensure their well-being.
1. Introduction
Nurses are increasingly being acknowledged for their significant contributions in the areas of primary care, public health emergencies, chronic disease management, surveillance, and the identification of new and emerging infectious diseases (1, 2). Four distinct roles for nurses in primary care and public health collaboration have been identified: relationship builder, outreach professional, program facilitator, and care coordinator (3). The prolonged engagement in these medical tasks will have an impact on the physical and mental health of nurses.
Nurses are a significant group within the medical field, comprising the largest proportion of personnel in various medical institutions at all levels. Research conducted in the past has demonstrated a correlation between nurse burnout and negative mental health outcomes, specifically depression and anxiety (4, 5). Numerous studies have demonstrated that public health emergencies, including infectious disease outbreaks and natural disasters, can significantly impact the physical and mental well-being of nurses, leading to job burnout (6, 7). In addition to their daily workload, nurses are also at the forefront of preventing and controlling the spread of the new coronavirus in a unique work environment. As a result, their workload has significantly increased. The scale and duration of the COVID-19 pandemic is larger and longer compared to previous infectious disease epidemics. As a result, the impact on the mental health of nurses has been more significant and widespread (8, 9). Prolonged exposure to high levels of stress can cause nurses to experience emotional, attitudinal, and behavioral exhaustion, ultimately resulting in job burnout.
The concept of burnout was first introduced by Freudenberger in 1974 (10), who believed that long-term exposure to interpersonal stressors at work caused a state of physical and mental exhaustion related to nursing activities. Later, Maslach identified the psychological syndrome caused by long-term emotional and interpersonal stressors at work as job burnout, which is characterized by emotional exhaustion, depersonalization, and decreased personal accomplishment (11). This study employed the aforementioned concept to establish a comprehensive definition of burnout within the nursing profession.
This study aims to investigate the current state of job burnout among nurses in Quanzhou City during the COVID-19 epidemic, as well as the factors that contribute to it. The study hypothesizes that there is a close relationship between anxiety, depression and job burnout, and utilizes a structural equation model to explore the relationship between the three variables. The findings of this study will provide valuable data to help alleviate nurses’ job burnout, maintain their mental health, and increase their motivation to work.
2. Theoretical background
There is a body of research that has focused extensively on COVID-19 pandemic affected the mental health of nurses. Mental problems related to the health emergency, such as stress, anxiety, depression, traumatic distress response, post-traumatic stress disorder (PTSD), and sleep disorders are more likely to affect medical and nursing staff (12–15). The first paper carried on the mental health of 994 healthcare workers in Wuhan, and the results indicated that 36.9% had subthreshold mental health disturbances, 34.4% had mild disturbances, 22.4% had moderate disturbances and 6.2% had severe disturbance (16). A systematic review and meta-analysis, which included in the analysis with a combined total of 33,062 participants from thirteen studies, showed that anxiety with a pooled prevalence of 23.2%, depression with a prevalence rate of 22.8% and insomnia with a prevalence rate of 38.9% (17). Another literature was reviewed for mental health problems of healthcare workers during the COVID-19 pandemic. The findings reported that pooled prevalence of mental health problems for post-traumatic stress disorder, anxiety, depression, and distress was 49, 40, 37, and 37%, respectively (18).
Amidst the COVID-19 pandemic, nurses find themselves susceptible to experiencing anxiety and depression due to the numerous psychological stressors they encounter. Consequently, managing and coping with these mental health challenges has become a prevalent issue worldwide (19). The current literature on COVID-19 supports the idea that the increased workload during a pandemic can lead to higher levels of anxiety and depression among individuals, which in turn poses a significant threat to the overall well-being of nurses (20, 21). Anxiety and depression often occur together (22, 23), although the exact relationship between these two conditions is still uncertain (24). The temporal relationship between anxiety and depression is a topic that has been widely discussed and debated among researchers. Some researchers posit that anxiety serves as a precursor to depression, implying a unidirectional association (25, 26). On the contrary, there are proponents who suggest a bidirectional association between the two aforementioned conditions (27, 28). Nevertheless, it has been observed that symptoms of anxiety have a stronger predictive value for later depressive symptoms compared to the reverse relationship.
Burnout is often occurred in the nurse, which has negatively impacted the quality of care, patient safety, and the functioning of staff workers in the health care industry (29). Substantial systematic reviews and meta-analyses have already shown that the prevalence of burnout is different between regions and times (30, 31). Mental health is one of primary health outcomes of burnout, and it refers to the nurse’s mental health as an individual, the high rates of trauma, depression, stress, and anxiety seen in many nurses, and how poor mental health often leads to burnout and vice-versa (32). Due to, the pandemic of COVID-19 exacerbating the complexity of the work environment, the problem of burnout among nurses has become more pronounced. Anxiety and depression are the most common psychological problems that can easily lead to job burnout, as evidenced by many literatures (5, 33, 34). In addition, burnout is affected by many other factors such as psychological resilience (35, 36), fear (37, 38), and psychological inflexibility (39).
Burnout, depression, and anxiety are postulated to exhibit interrelationships. We aimed to test the mediating role of depression in the relationship between anxiety and burnout. Based on the above literature review, we propose the following model. From this model, we propose three main hypotheses: (see Figure 1)
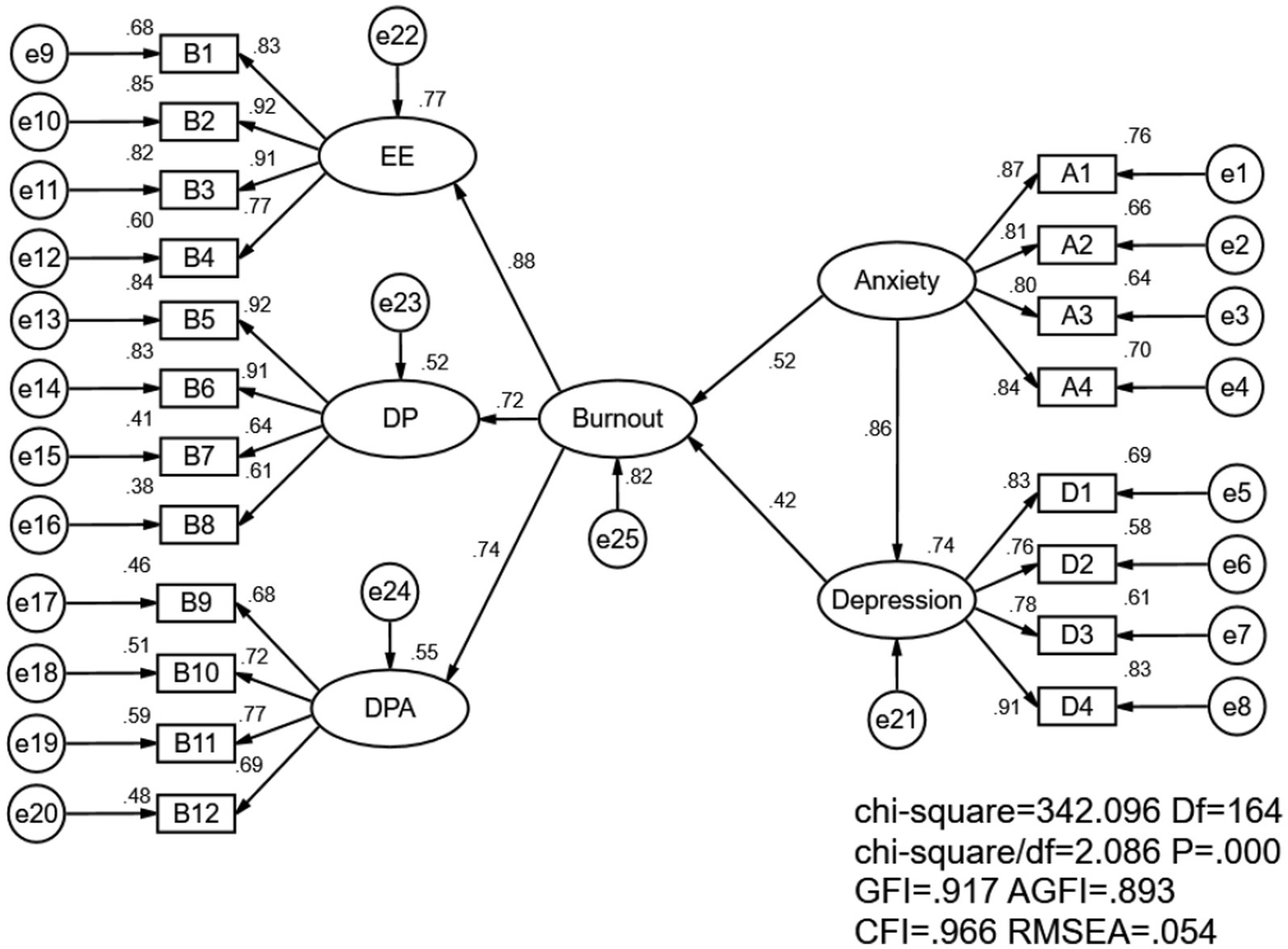
Figure 1. Structural equation model for nurse burnout, anxiety, and depression. EE indicate emotional exhaustion; DP indicate depersonalization and DPA indicate decreased personal accomplishment.
H1: Anxiety has a positive and significant impact on job burnout.
H2: Depression has a positive and significant impact on job burnout.
H3: Depression mediate the relationship between anxiety and job burnout.
3. Materials and methods
3.1. Participants
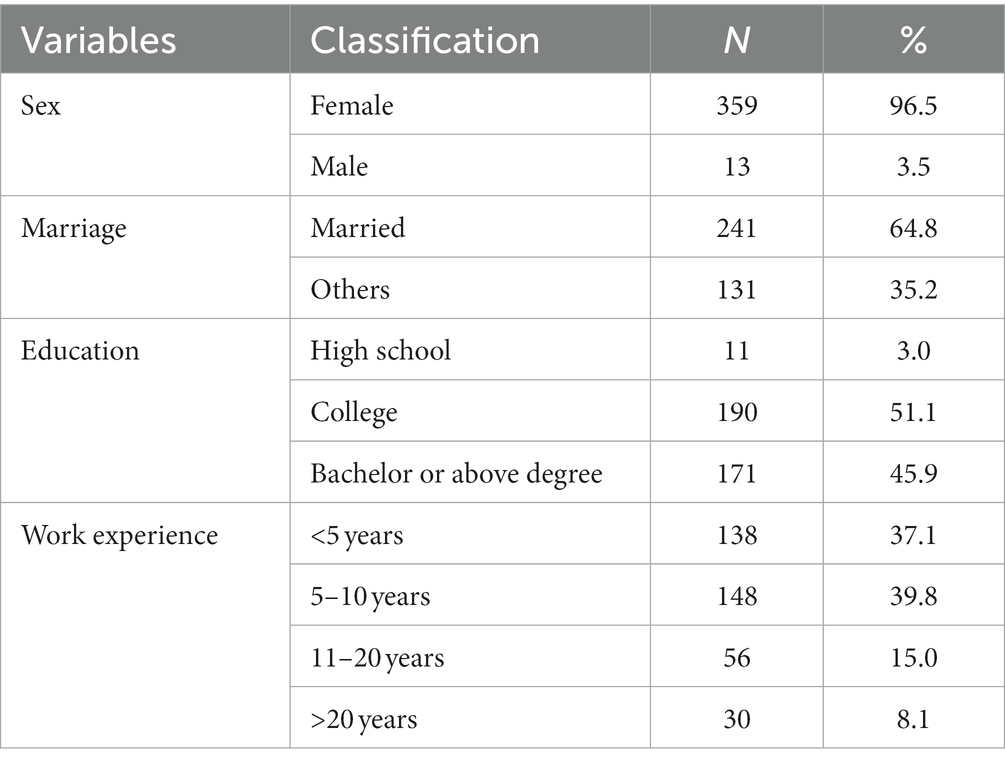
The sample for this study included 372 nurses (96.5% females) whose ages ranged between 20 and 59 years, with a mean age of 30.8 ± 6.3 years. 64.8% of participants were married and 190 (51.1%) have a junior college degree. The majority of nurses (76.9%) have less than 10 years of work experience (Table 1).
3.2. Measures
3.2.1. General information questionnaire
A self-designed general situation questionnaire has been created based on literature research and expert opinions The questionnaire includes basic demographic information such as age, gender, and marital status.
3.2.2. The 7-item generalized anxiety disorder questionnaire (GAD-7)
There are 9 items in the scale, and 4 grades are used for scoring (40). The scoring rules are as follows: 0–4 is normal, 5–9 is mild anxiety, 10–14 is moderate anxiety, and 15–21 is severe anxiety (41). In this study, Cronbach’s α coefficient = 0.943; KMO = 0.926, Bartlett sphericity test p < 0.01.
3.2.3. Patient health questionnaire-9 (PHQ-9)
There are 9 items in the scale, and 4 grades are used for scoring (42). The scoring rules are as follows: 0–4 means no depression, 5–9 means mild depression, 10–14 means moderate depression, and 15–19 means moderate depression. Major depressive disorder, 20–27 may have major depressive disorder (43). In this study, Cronbach’s α coefficient = 0.922; KMO = 0.902, Bartlett sphericity test p < 0.01.
3.2.4. Maslach burnout inventory (MBI)
This test includes three aspects of job burnout: the scale contains 3 dimensions, 22 items, and uses Likert 7-level scoring, scoring rules: 9 items of emotional exhaustion (EE), indicating the emotional response caused by work pressure, with a total score of 0–54. Scores ≤19, 20–25 and ≥ 26 represent low, medium and high level of EE respectively; 5 items of depersonalization (DP) indicate the attitudes and feelings of clients caused by work pressure, with a total score of 0–30 and scores ≤6, 7 ~ 8 and ≥ 9 represent low, medium, and high level of DP respectively; 8 items with decreased personal accomplishment (DPA) indicate negative self-evaluation, accompanied by a decline in work ability experience and achievement experience (11). The total score is 0 ~ 48 points, and the score is ≤34, 35 ~ 38, and ≥ 39 represent high, medium, and low level of DPA, respectively, and the scores are reversed. We operationalized high-level burnout as the presence of elevated levels in all three dimensions. Medium-level burnout was defined as elevated levels in two dimensions, while low-level burnout was characterized by elevated levels in only one dimension. The absence of burnout was indicated when all levels were low (44–46). In this study, Cronbach’s α coefficient = 0.906, KMO = 0.926, Bartlett sphericity test p < 0.01.
3.3. Procedures
A quantitative research design using a self-reported questionnaire was used to collect data from a tertiary designated hospital in Quanzhou, Fujian Province who were treating patients with new coronary pneumonia. The hospital has a total of 1,621 nurses, who are assigned to various wards, with a distribution of 67 wards. To gather data from nurses, the quota sampling method was employed, wherein 6 participants were randomly selected from each ward, resulting in a total sample size of 402.
The inclusion criteria were: (1) working for at least one year, (2) providing informed consent to participate in the study, and (3) working during the COVID-19 epidemic. The exclusion criteria were: (1) receiving psychological counseling or treatment in the past year, and (2) having a prior history of mental illness.
We designed the online questionnaire using the Wenjuanxing platform and sent the survey link to nurses via WeChat, QQ or email. We completed data collection from May 1st to 30th, 2020. The entire questionnaire took at least 5 min to complete, and samples with response times below this standard were removed. At the beginning of the questionnaire, there is an informed consent form, participants need to read this section and click on consent. We are also making a statement that the data from this survey will only be used for scientific research and will not disclose the personal information of the participants. This study was approved by the ethical committee of Quanzhou First Hospital (NO.Quan Yi lun 2,020,181).
3.4. Data analysis
Data cleaning, normality test and correlation analysis were performed using SPSS Version 26.0. A structural equation model was established using AMOS24.0 software to fit the relationship model between nurses’ anxiety, depression and job burnout. Following the suggestion of Gerbing and Anderson (47), we estimate the measurement model separately for each construct before constructing the model. In this study, the model was estimated by the maximum likelihood estimation, and the model was corrected with square multiple correlation (SMC) (48) and the modification index (MI). Since all aspects are reflective indicators, if the requirements of SMC and MI are not met during model modification, we will delete the question (49, 50). We has performed the Sobel test (51) and bootstrap method (52) for assessing the mediating effects. Five indices were employed to evaluate the adequacy of fit for both the measurement and structural models: Normed Chi-square (χ2/df < 3) (53, 54), Goodness of Fit Index (GFI > 0.90), Adjusted-Goodness of Fit Index (AGFI>0.90), Comparative Fit Index (CFI > 0.90) (55), Root Mean Square Error of Approximation (RMSEA<0.08) (56).
4. Results
4.1. Anxiety, depression and burnout among nurses based on demographic information
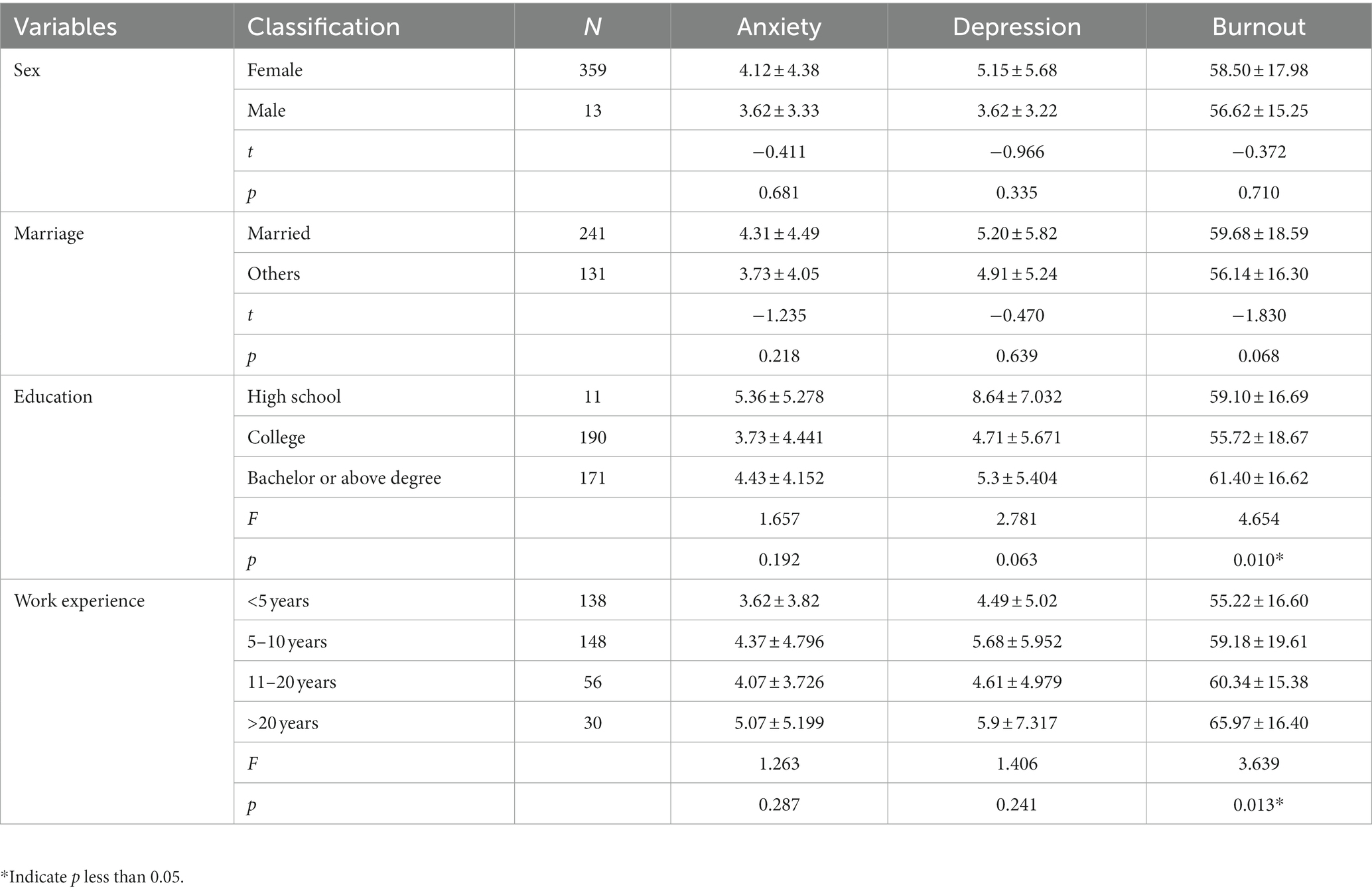
Burnout was statistically different in education and work experience, but the rest were not different (Table 2).
4.2. Anxiety, depression and burnout among nurses
The anxiety score was (4.10 ± 4.34), and the depression score was (5.09 ± 5.62). The prevalence of anxiety and depression among the participants were 45.2 and 41.4%, respectively.
The research conducted on the phenomenon of job burnout among nurses yielded noteworthy findings. Specifically, the average score for emotional exhaustion was determined to be 22.12, with a significant proportion of participants (59.4%) displaying medium to high levels of this particular dimension. Similarly, the average score for depersonalization was found to be 9.62, and a substantial majority of nurses (70.4%) exhibited moderate to high levels of this aspect. Additionally, the average score for decreased personal accomplishment was calculated to be 26.70, with 64.0% of participants falling within the medium to high range for this dimension. The prevalence of severe burnout among nurses was found to be 7.3% (Table 3).
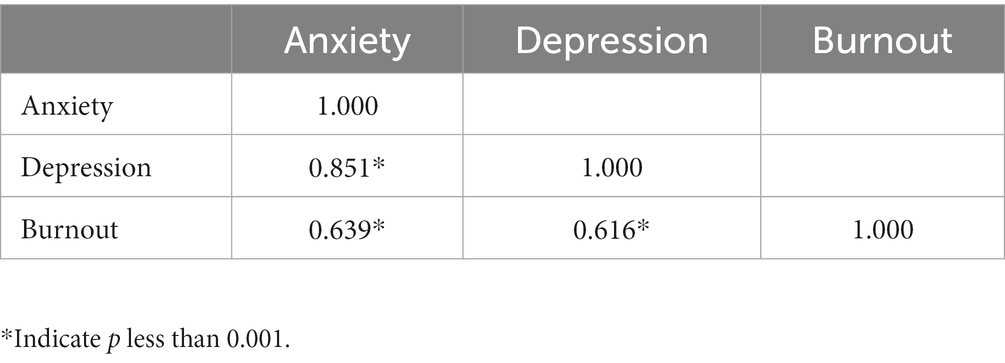
4.3. Analysis of anxiety, depression and burnout among nurses
The pearson correlation was used to analyze the relationship between anxiety, depression and burnout among nurses, which showed a positive correlation between anxiety and depression on burnout (Table 4).
4.4. Structural equation model of burnout, anxiety, and depression among nurses
4.4.1. Selection of the model metrics
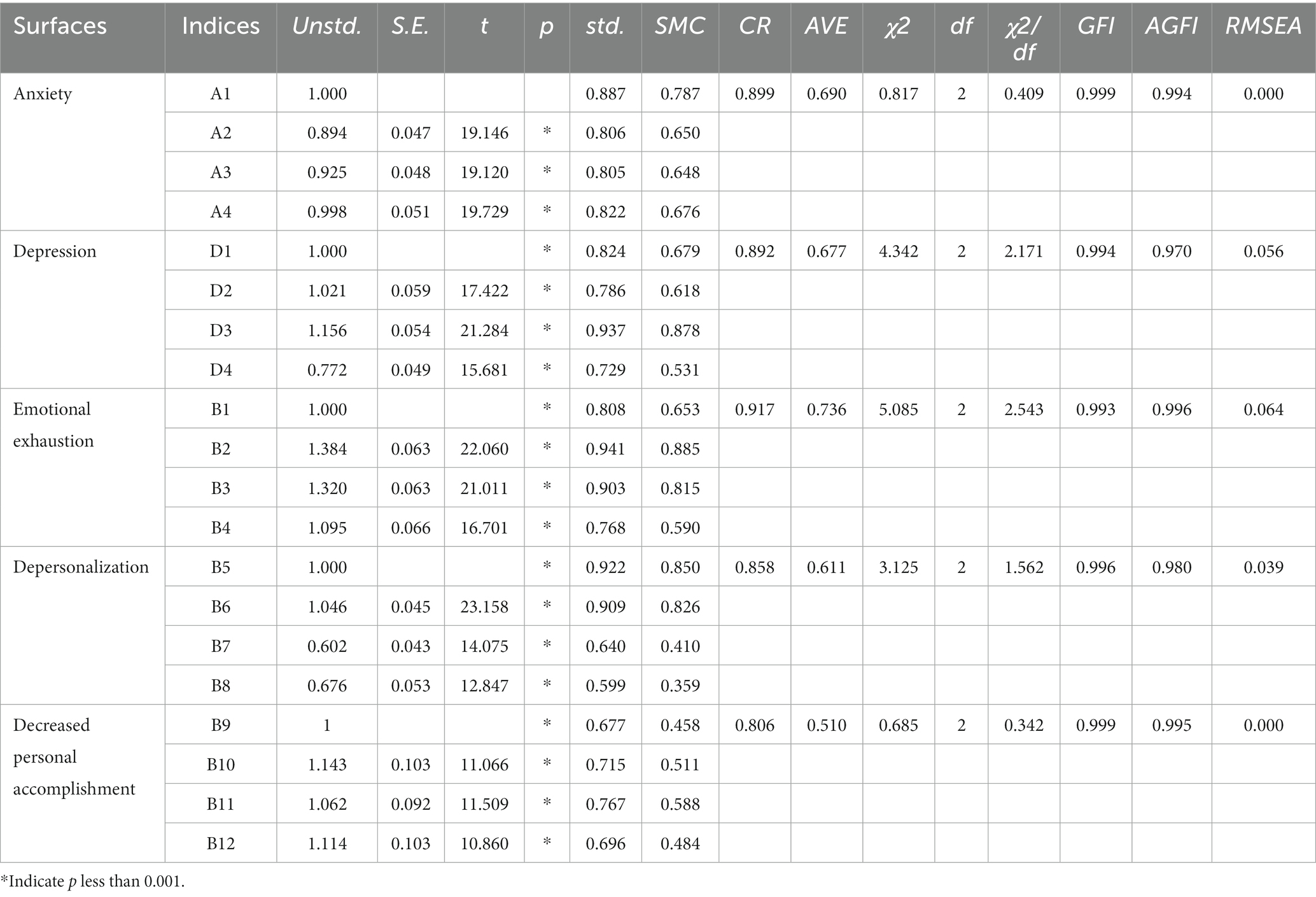
To assess whether the measurement indicators accurately reflected the latent variables, a Confirmatory Factor Analysis (CFA) was conducted on all constructs.
Out of the original 7 items in the anxiety questionnaire, only 4 items had standardized factor loadings above 0.7 (but not exceeding 0.95) and significant positive residuals after CFA. These 4 questions were deemed reliable with a Composite Reliability (CR) of 0.899 (exceeding the standard of 0.7) (57) and an Average Variance Extracted (AVE) of 0.690 (exceeding the standard of 0.5) (58). Additionally, the fitting index fell within the acceptable range, thus confirming the retention of these 4 questions.
Out of the 9 items in the depression questionnaire, only 4 had standardized factor loadings exceeding 0.7 but not exceeding 0.95, and all residuals were positive and significant after CFA. The CR was 0.892, surpassing the standard of 0.7, and the AVE was 0.677, surpassing the standard of 0.5. The fitting index was within the acceptable range, therefore, these 4 questions were retained.
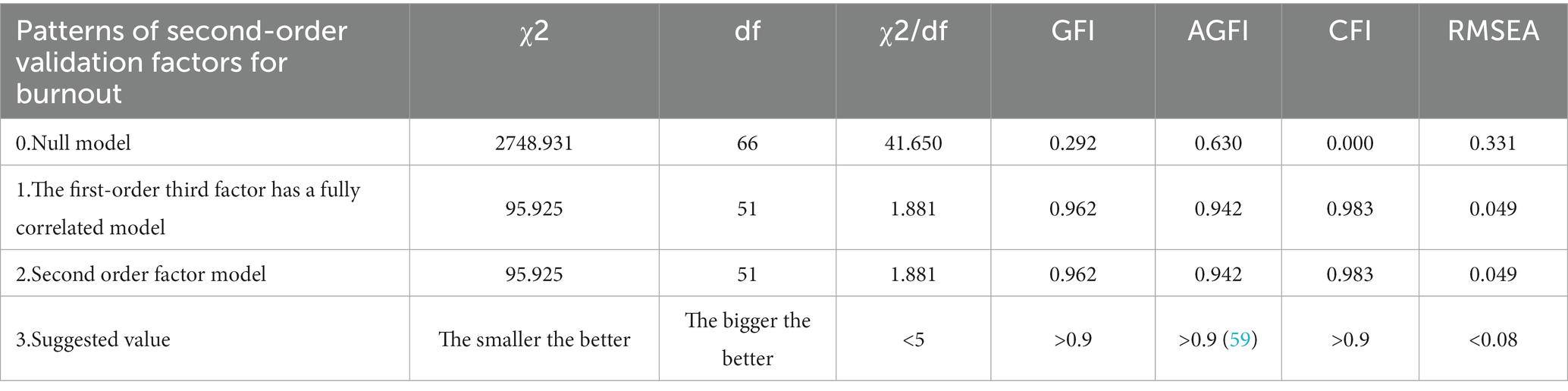
In this study, job burnout was analyzed as a second-order aspect and deconstructed into three dimensions: emotional exhaustion, depersonalization, and decreased personal accomplishment. To ensure the validity of these dimensions, a first-order three-factor complete correlation model and a second-order factor model were analyzed. This study utilized the first-order three-factor complete correlation model to analyze the data. The results showed that the first-order factors had moderate to high correlations. Specifically, emotional exhaustion and job apathy had a correlation coefficient of 0.66, depersonalization and decreased personal accomplishment had a correlation coefficient of 0.52, and emotional exhaustion and decreased personal accomplishment had a correlation coefficient of 0.63. Additionally, the target coefficient was 100%, indicating that the second-order job burnout in this study met the requirements of the theoretical model. The residuals of the standardized factor loadings for the three deconstructed constructs were all found to be positive and significant after the second-order CFA. Additionally, the CR exceeded the standard of 0.7, the AVE exceeded the standard of 0.5, and the fitting index fell within the acceptable range. As a result, the second-order three-facet model was retained for further analysis (Tables 5, 6).
4.4.2. Construction of the model
This study explores the relationship between job burnout, anxiety, and depression based on a theoretical model. The model suggests that anxiety and depression can impact job burnout, and a hypothetical model was created using nurses’ anxiety as an independent variable and depression as an intermediary variable. The model fit indices, with χ2 = 342.096, df = 164, χ2/df = 2.086, GFI = 0.917, AGFI = 0.893、CFI = 0.966, RMSEA = 0.054, falls within an acceptable range, indicating a good model fitting effect (Figure 1).
4.4.3. Analysis of the total, direct, and indirect effects of the model
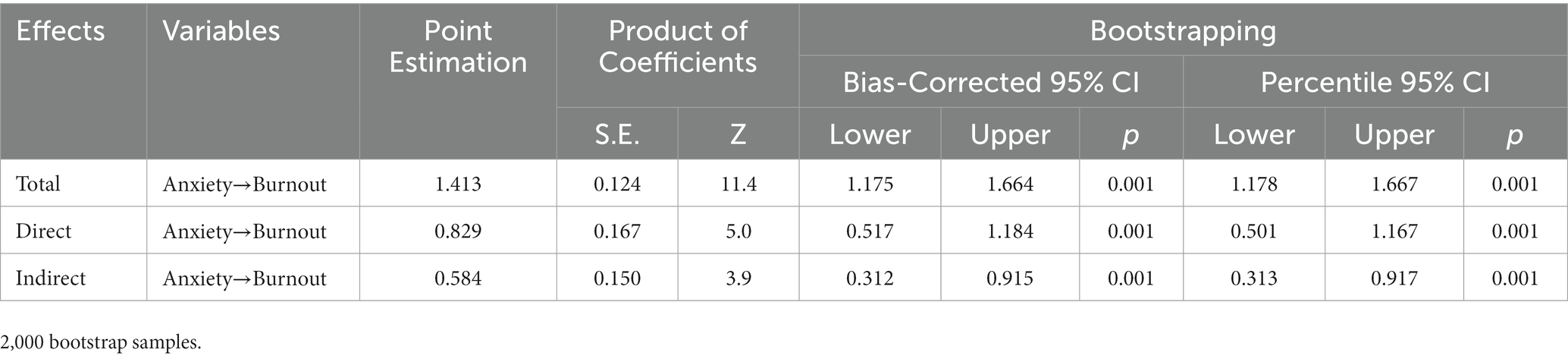
To determine if the model had a mediation effect, both Sobel and Bootstrap methods were used. The Sobel mediation effect was verified with a Z value of 4.55, which exceeded the standard of 2, indicating a mediation effect. The Bootstrap method also confirmed a partial mediation effect. The results indicate that anxiety has a total effect of 1.413 on job burnout, with a direct effect of 0.829 and an indirect effect of 0.584 (Table 7).
5. Discussion
The findings of the study indicate that the mean score for emotional exhaustion among participants is 22.12, indicating moderate levels of this phenomenon. Similarly, the average score for depersonalization is 9.62, suggesting high levels of this condition. Additionally, the mean score for decreased personal accomplishment is 26.70, indicating high levels of this aspect. Furthermore, the study reveals that the prevalence of severe burnout among nurses is 7.3%. The scores obtained in this study were found to be higher than the previous record of burnout among 1,621 nurses in Rizhao City before the epidemic. Specifically, the average score for emotional exhaustion was 18.14, depersonalization was 4.64, and decreased personal accomplishment was 34.59 (60). The study found that the average subdimension score of emotional exhaustion was 18.9, the average score of depersonalization subdimension was 7.3, and the average score of decreased personal accomplishment subdimension was 11.4, which was higher than another study (61). In comparison, the average subdimension score of emotional exhaustion was 26.6, the average score of depersonalization subdimension was 10.2, and the average score of decreased personal accomplishment subdimension was 27.3 in the other study (62). These results suggest that burnout scores differ across time, regions, and groups. Overall, nurses experienced higher burnout scores during the epidemic than before. This is likely due to the added pressure of the uncertain hospital environment of the new crown epidemic, as well as additional tasks such as nursing, sample collection, and out-of-home support. These factors increase the work pressure of nurses and promote the emergence of job burnout. However, a systematic review found that nurses’ burnout scores did not differ significantly before and during the pandemic (63). Consequently, both in emergencies and in normal daily routines, healthcare institutions should develop tailored occupational health programs and improve working conditions (64).
The incidence of job burnout is known to increase in poor psychological conditions. Various studies conducted both domestically and internationally have found a positive correlation between anxiety, depression, and job burnout. A cross-sectional survey of 3,527 samples found anxiety (OR = 4.87) and depression (OR = 4.06) to be risk factors for job burnout (65). One study in China have also found anxiety to be positively correlated with emotional exhaustion (r = 0.637), depersonalization (r = 0.417), and decreased personal accomplishment (r = −0.242), while depression is positively correlated with job burnout (34). This study also found a positive correlation between anxiety, depression, and job burnout (emotional exhaustion: r = 0.569, depersonalization: r = 0.406, decreased personal accomplishment: r = −0.378), but the causal relationship between the three is still unclear. To further explore the relationship between anxiety, depression, and job burnout, a structural equation model was constructed.
Previous studies have shown that anxiety and depression can both impact job burnout through other mediating variables (66, 67). Additionally, other investigations have revealed that burnout can serve as a mediating factor in the regulation of anxiety and depression (68–70). In the current research, we have developed a hypothesis positing that anxiety could potentially exert an indirect influence on burnout through the mediating factor of depression. This particular aspect of our study sets it apart from previous inquiries in the field. The findings of our study further corroborate this hypothesis. The results indicate that anxiety has a partial mediating effect on job burnout, with both direct (0.829) and indirect (0.584) effects observed. The direct effect accounts for 58.7% of the total effect, while the indirect effect accounts for 41.3%. These findings suggest that nurses who experience higher levels of anxiety are more likely to experience burnout, and that depression can exacerbate this relationship. Overall, these results highlight the importance of addressing both anxiety and depression in the prevention and management of job burnout among nurses. The comprehensive findings of the study offer substantial evidence in favor of accepting all the proposed hypotheses and their underlying assumptions.
Some questions in the scale were deleted in this study based on the modification index and square multiple correlation. The model fit could be improved based on the modification index. However, it is important to note that this correction is data-driven and may introduce coincidental errors in probability, limiting its generalizability to other samples (71). If the square multiple correlation falls below 0.6, it suggests that the corresponding topic should be removed from the analysis as it fails to adequately represent the construct characteristics (47, 48). Furthermore, it is recommended that a construct should ideally consist of 4 to 6 measurement variables (72), and all constructs in this study met this criterion by including 4 variables. Since the process of model generation is implicated in data-driven issues and there is no guarantee that the results of the model correction will be consistent with the overall results, the current study requires a new set of samples to perform the test of cross validity to assess the stability of the model (73, 74).
There are many scales used to measure different symptoms of anxiety and depression, this study used GAD-7 and PHQ-9 to measure anxiety and depression, respectively, (75). Although these two scales are classic psychological scales with high reliability and validity, the process of using the scales is only to add up the scores of the respondents to get a total score, and then determine whether there are symptoms of anxiety and depression according to the criteria. Anxiety and depression, as a complex mental illness, have many different symptoms, and the practice of grouping different symptoms into a total score cannot truly reflect the behavior and symptoms of an individual (40, 76). In addition, the current study deleted some questions in the scale to obtain a better model during model modification, a practice that improves the fit of the model but loses important information to a certain extent. Therefore, the scale can only be used as an auxiliary tool in clinical applications, and the most crucial thing is to rely on the questioning technique.
6. Limitations
Several limitations of the study should be settled. First, an self-assessment online questionnaire was implemented in this study, the participants will fill in the answer at random affected by response and social desirability bias. Second, we only surveyed health workers in Quanzhou, the calculated sample size could not be fully achieved, and the applicability to other regions requires further research. At last, SEM was often used to quantitatively verify relationships between variables, limiting conclusions about causality because of the cross-sectional data.
7. Contributions and conclusions
Our findings showed that a positive correlation between anxiety and depression on burnout, which was conform to our hypothesis. This finding contributes to understanding the relationship between burnout and mental health as well as providing additional data support for existing models. In addition, this result may also explain that during times of emergency, such as a pandemic with COVID-19 or public health emergencies, caregivers may be under more stress leading to burnout.
Nurses exhibit a greater prevalence of anxiety, depression, and burnout. Anxiety not only directly impacts burnout, but also indirectly influences burnout through its association with depression. Depression was identified as a mediating factor in the connection between anxiety and burnout. It is imperative for hospital administrators to prioritize the mental health of nurses and support them to strengthen psychological testing and counselling.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the ethical committee of Quanzhou First Hospital (NO.Quan Yi lun 2020181). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FL conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft. YZ authored or reviewed drafts of the article, and approved the final draft. YC prepared figures and/or tables and authored or reviewed drafts of the article. ZT conceived and designed the experiments, authored or reviewed drafts of the article, and approved the final draft. All authors contributed to the article and approved the submitted version.
Funding
This study was granted by the Natural Science Foundation of Quanzhou (Grant No.2021N124S PI: Fuzhi Liu) and the University-level Scientific Research Fund of Quanzhou Medical College (GrantNo. XJK2009B; PI: FL). The funders had no role in study design, data collection andanalysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We thank the participated nurses in the study. We also acknowledge the reviewers and editors for viewing our work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1221501/full#supplementary-material
References
1. Beggs-Yeager, C, Sharts-Hopko, N, and McDermott-Levy, R. The role of nurses in surveillance to enhance global health security: a delphi study. Nurs Outlook. (2021) 69:1021–9. doi: 10.1016/j.outlook.2021.05.011
2. Guilamo-Ramos, V, Thimm-Kaiser, M, Benzekri, A, Hidalgo, A, Lanier, Y, Tlou, S, et al. Nurses at the frontline of public health emergency preparedness and response: lessons learned from the HIV/AIDS pandemic and emerging infectious disease outbreaks. Lancet Infect Dis. (2021) 21:e326–33. doi: 10.1016/S1473-3099(20)30983-X
3. Swanson, M, Wong, ST, Martin-Misener, R, and Browne, AJ. The role of registered nurses in primary care and public health collaboration: a scoping review. Nurs Open. (2020) 7:1197–207. doi: 10.1002/nop2.496
4. Danet, AD. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med Clin (Barc). (2021) 156:449–58. doi: 10.1016/j.medcle.2020.11.003
5. Cañadas-de la Fuente, GA, Albendín-García, L, Ortega-Campos, E, and de la Fuente-Solana, EI. Nurse burnout in critical care units and emergency departments: intensity and associated factors. Emergencias. (2018) 30:328–31.
6. Chemali, Z, Ezzeddine, FL, Gelaye, B, Dossett, ML, Salameh, J, Bizri, M, et al. Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Public Health. (2019) 19:1337. doi: 10.1186/s12889-019-7713-1
7. Maunder, R, Lancee, W, Balderson, K, Bennett, J, Borgundvaag, B, Evans, S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. (2006) 12:1924–32. doi: 10.3201/eid1212.060584
8. Habas, K, Nganwuchu, C, Shahzad, F, Gopalan, R, Haque, M, Rahman, S, et al. Resolution of coronavirus disease 2019 (COVID-19). Expert Rev Anti-Infect Ther. (2020) 18:1201–11. doi: 10.1080/14787210.2020.1797487
9. Stelnicki, AM, Carleton, RN, and Reichert, C. Nurses' mental health and well-being: COVID-19 impacts. Can J Nurs Res. (2020) 52:237–9. doi: 10.1177/0844562120931623
10. Tricas Moreno, JM, Salavera Bordas, C, Lucha Lopez, MO, Vidal Peracho, C, Lucha Lopez, AC, Estebanez de Miguel, E, et al. Descriptive study of stress and satisfaction at work in the Saragossa university services and administration staff. Int J Ment Health Syst. (2010) 4:7. doi: 10.1186/1752-4458-4-7
11. Maslach, C, and Jackson, SE. The measurement of experienced burnout. J Occup Behav. (1981) 2:99–113. doi: 10.1002/job.4030020205
12. Tamrakar, P, Pant, SB, and Acharya, SP. Anxiety and depression among nurses in COVID and non-COVID intensive care units. Nurs Crit Care. (2023) 28:272–80. doi: 10.1111/nicc.12685
13. Giorgi, G, Lecca, LI, Alessio, F, Finstad, GL, Bondanini, G, Lulli, LG, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. (2020) 17:7857. doi: 10.3390/ijerph17217857
14. Cortés-Álvarez, NY, and Vuelvas-Olmos, CR. COVID 19: psychological effects and associated factors in Mexican nurses. Disaster Med Public Health Prep. (2022) 16:1377–83. doi: 10.1017/dmp.2020.495
15. Greenberg, N, Weston, D, Hall, C, Caulfield, T, Williamson, V, and Fong, K. Mental health of staff working in intensive care during Covid-19. Occup Med (Lond). (2021) 71:62–7. doi: 10.1093/occmed/kqaa220
16. Kang, L, Ma, S, Chen, M, Yang, J, Wang, Y, Li, R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
17. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
18. Saragih, ID, Tonapa, SI, Saragih, IS, Advani, S, Batubara, SO, Suarilah, I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
19. Xiang, YT, Yang, Y, Li, W, Zhang, L, Zhang, Q, Cheung, T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228. doi: 10.1016/S2215-0366(20)30046-8
20. Salari, N, Khazaie, H, Hosseinian-Far, A, Khaledi-Paveh, B, Kazeminia, M, Mohammadi, M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. doi: 10.1186/s12960-020-00544-1
21. Marvaldi, M, Mallet, J, Dubertret, C, Moro, MR, and Guessoum, SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
22. Liu, L, Liu, C, Wang, Y, Wang, P, Li, Y, and Li, B. Herbal medicine for anxiety, depression and insomnia. Curr Neuropharmacol. (2015) 13:481–93. doi: 10.2174/1570159X1304150831122734
23. Choi, KW, Kim, YK, and Jeon, HJ. Comorbid anxiety and depression: clinical and conceptual consideration and Transdiagnostic treatment. Adv Exp Med Biol. (2020) 1191:219–35. doi: 10.1007/978-981-32-9705-0_14
24. Wen, FH, Chou, WC, Huang, CC, Hu, TH, Chiang, MC, Chuang, LP, et al. ICU bereaved surrogates' comorbid psychological-distress states and their associations with prolonged grief disorder. Crit Care. (2022) 26:102. doi: 10.1186/s13054-022-03981-7
25. Wilkinson, PO, Croudace, TJ, and Goodyer, IM. Rumination, anxiety, depressive symptoms and subsequent depression in adolescents at risk for psychopathology: a longitudinal cohort study. BMC Psychiatry. (2013) 13:250. doi: 10.1186/1471-244X-13-250
26. Horn, PJ, and Wuyek, LA. Anxiety disorders as a risk factor for subsequent depression. Int J Psychiatry Clin Pract. (2010) 14:244–7. doi: 10.3109/13651501.2010.487979
27. Barber, KE, Zainal, NH, and Newman, MG. Positive relations mediate the bidirectional connections between depression and anxiety symptoms. J Affect Disord. (2023) 324:387–94. doi: 10.1016/j.jad.2022.12.082
28. Jacobson, NC, and Newman, MG. Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychol Bull. (2017) 143:1155–200. doi: 10.1037/bul0000111
29. Bakhamis, L, Paul, DP 3rd, Smith, H, and Coustasse, A. Still an epidemic: the burnout syndrome in hospital registered nurses. Health Care Manag (Frederick). (2019) 38:3–10. doi: 10.1097/HCM.0000000000000243
30. Sullivan, D, Sullivan, V, Weatherspoon, D, and Frazer, C. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. (2022) 57:79–99. doi: 10.1016/j.cnur.2021.11.006
31. Galanis, P, Vraka, I, Fragkou, D, Bilali, A, and Kaitelidou, D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. (2021) 77:3286–302. doi: 10.1111/jan.14839
32. Maslach, C. What have we learned about burnout and health? Psychol Health. (2001) 16:607–11. doi: 10.1080/08870440108405530
33. Golonka, K, Mojsa-Kaja, J, Blukacz, M, Gawłowska, M, and Marek, T. Occupational burnout and its overlapping effect with depression and anxiety. Int J Occup Med Environ Health. (2019) 32:229–44. doi: 10.13075/ijomeh.1896.01323
34. Hu, D, Kong, Y, Li, W, Han, Q, Zhang, X, Zhu, LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. (2020) 24:100424. doi: 10.1016/j.eclinm.2020.100424
35. Yıldırım, M, Kaynar, Ö, Chirico, F, and Magnavita, N. Resilience and extrinsic motivation as mediators in the relationship between fear of failure and burnout. Int J Environ Res Public Health. (2023) 20:5895. doi: 10.3390/ijerph20105895
36. Yıldırım, M, and Solmaz, F. COVID-19 burnout, COVID-19 stress and resilience: initial psychometric properties of COVID-19 burnout scale. Death Stud. (2022) 46:524–32. doi: 10.1080/07481187.2020.1818885
37. Yıldırım, M, and Ashraf, F. Fear of COVID-19, coronavirus anxiety, COVID-19 burnout, and resilience: examining psychometric properties of COVID-19 burnout scale in Urdu. J Asian Afr Stud. (2023) 002190962311531. doi: 10.1177/00219096231153161
38. Çağış, ZG, and Yıldırım, M. Understanding the effect of fear of COVID-19 on COVID-19 burnout and job satisfaction: a mediation model of psychological capital. Psychol Health Med. (2023) 28:279–89. doi: 10.1080/13548506.2022.2077970
39. Chen, X, Yang, Q, Yıldırım, M, Ye, B, and Wang, R. How COVID-19 prevention burnout impacts emotional symptoms among Chinese college students: a moderated mediation model. J Health Psychol. (2023) 13591053231189419. doi: 10.1177/13591053231189419
40. Spitzer, RL, Kroenke, K, Williams, J, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
41. Aljaberi, MA, Alareqe, NA, Alsalahi, A, Qasem, MA, Noman, S, Uzir, MUH, et al. A cross-sectional study on the impact of the COVID-19 pandemic on psychological outcomes: multiple indicators and multiple causes modeling. PLoS One. (2022) 17:e0277368. doi: 10.1371/journal.pone.0277368
42. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
43. Hu, Y, Chen, Y, Zheng, Y, You, C, Tan, J, Hu, L, et al. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav Immun. (2020) 89:587–93. doi: 10.1016/j.bbi.2020.07.016
44. Zhang, H, Xiao, Y, Dai, T, Li, Q, Huang, L, Huang, X, et al. A cross-sectional study on burnout and its individual and environmental correlates among hepatological surgery nurses in Hunan Province, China. PLoS One. (2023) 18:e0283373. doi: 10.1371/journal.pone.0283373
45. Yue, Z, Qin, Y, Li, Y, Wang, J, Nicholas, S, Maitland, E, et al. Empathy and burnout in medical staff: mediating role of job satisfaction and job commitment. BMC Public Health. (2022) 22:1033. doi: 10.1186/s12889-022-13405-4
46. Bordoagni, G, Fino, E, and Agostini, A. Burnout, attachment and Mentalization in nursing students and nurse professionals. Healthcare (Basel). (2021) 9:1576. doi: 10.3390/healthcare9111576
47. Gerbing, DW, and Anderson, JC. An updated paradigm for scale development incorporating unidimensionality and its assessment. J Mark Res. (1988) 25:186–92. doi: 10.1177/002224378802500207
48. Hooper, D, Mullen, J, and Hooper, D. Structural equation modeling: guidelines for determining model fit. Electron J Bus Res Methods. (2008) 6:53–60. doi: 10.3109/03005364000000039
49. Jarvis, CB, MacKenzie, SB, and Podsakoff, PM. A critical review of construct indicators and measurement model misspecification in marketing and consumer research. J Consum Res. (2003) 30:199–218. doi: 10.1086/376806
50. Mac Kenzie, SB, Podsakoff, PM, and Jarvis, CB. The problem of measurement model misspecification in behavioral and organizational research and some recommended solutions. J Appl Psychol. (2005) 90:710–30. doi: 10.1037/0021-9010.90.4.710
51. Sobel, ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. (1982) 13:290–312. doi: 10.2307/270723
53. Kline, RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press (2005).
54. Carmines, E, and Mciver, J. Analyzing models with unobserved variables: analysis of covariance structures. Soc Meas Current Issues. (1981) 10:65–115. doi: 10.117/0049124183011003003
55. Bentler, PM. Comfirmatory factor analysis via noniterative estimation: a fast, inexpensive method. J Mark Res. (1983) 19:417–24. doi: 10.1177/002224378201900403
56. Browne, MW, and Cudeck, R. Alternative ways of assessing model fit. Sociol Methods Res. (1993) 154:132–62. doi: 10.1177/004912419021002005
58. Fornell, C, and Lacker, D. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. (1981) 18:39–50. doi: 10.1177/002224378101800104
59. Mac Callum, RC, and Hong, S. Power analysis in covariance structure modeling using GFI and AGFI. Multivar Behav Res. (1997) 32:193–210. doi: 10.1207/s15327906mbr3202_5
60. Na, C, Xin-sheng, W, Xiang-hua, C, Liqi, T, Jiangfeng, L, Li, Y, et al. Study on the influencing factors of nurses’ job burnout in Rizhao City under COVID- 19 epidemic: based on the analysis of structural equation model. Chin Hosp Manag. (2021) 41:84–7.
61. Murat, M, Köse, S, and Savaşer, S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30:533–43. doi: 10.1111/inm.12818
62. Jalili, M, Niroomand, M, Hadavand, F, Zeinali, K, and Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Arbeitsmed. (2021) 94:1345–52. doi: 10.1007/s00420-021-01695-x
63. Rizzo, A, Yıldırım, M, Öztekin, GG, Carlo, AD, Nucera, G, Szarpak, Ł, et al. Nurse burnout before and during the COVID-19 pandemic: a systematic comparative review. Front Public Health. (2023) 11:1225431. doi: 10.3389/fpubh.2023.1225431
64. Nucera, G, Chirico, F, Yildirim, M, Szarpak, L, and Magnavita, N. Addressing burnout and PTSD among paramedics and emergency staff after the COVID-19 pandemic: the role of occupational health services and workplace health promotion programs. Disaster Emerg Med J. (2023) 8:131–33. doi: 10.5603/DEMJ.a2023.0031
65. Denning, M, Goh, ET, Tan, B, Kanneganti, A, Almonte, M, Scott, A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS One. (2021) 16:e0238666. doi: 10.1371/journal.pone.0238666
66. Martins, V, Serrão, C, Teixeira, A, Castro, L, and Duarte, I. The mediating role of life satisfaction in the relationship between depression, anxiety, stress and burnout among Portuguese nurses during COVID-19 pandemic. BMC Nurs. (2022) 21:188. doi: 10.1186/s12912-022-00958-3
67. Serrão, C, Duarte, I, Castro, L, and Teixeira, A. Burnout and depression in Portuguese healthcare workers during the COVID-19 pandemic-the mediating role of psychological resilience. Int J Environ Res Public Health. (2021) 18:636. doi: 10.3390/ijerph18020636
68. Sun, Y, Liu, F, Wang, Y, Zhou, M, Yang, B, and Cao, F. Mindfulness improves health worker's occupational burnout: the moderating effects of anxiety and depression. Int Arch Arbeitsmed. (2021) 94:1297–305. doi: 10.1007/s00420-021-01685-z
69. Chen, J, Li, J, Cao, B, Wang, F, Luo, L, and Xu, J. Mediating effects of self-efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. J Adv Nurs. (2020) 76:163–73. doi: 10.1111/jan.14208
70. Tucker, S, Melnyk, B, Corona, L, Corona, C, and Roberts, H. A model of depression in university faculty, staff, and health care workers using an automated mental health screening tool. J Occup Environ Med. (2022) 64:607–13. doi: 10.1097/JOM.0000000000002538
71. Diamantopoulos, A, and Siguaw, JA. Introducing LISREL: a guide for the uninitiated. London: SAGE (2000).
72. Noar, SM. The role of structural equation modeling in scale development. Struct Equ Model Multidiscip J. (2003) 10:622–47. doi: 10.1207/S15328007SEM1004_8
73. Browne, MW, and Cudeck, R. Single sample cross-validation indices for covariance structures. Multivar Behav Res. (1989) 24:445–55. doi: 10.1207/s15327906mbr2404_4
74. Diamantopoulos, A. Modelling with LISREL: a guide for the uninitiated. J Mark Manag. (1994) 10:105–36. doi: 10.1080/0267257X.1994.9964263
75. Kroenke, K, Spitzer, RL, Williams, JB, and Löwe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
76. Fried, EI. Moving forward: how depression heterogeneity hinders progress in treatment and research. Expert Rev Neurother. (2017) 17:423–5. doi: 10.1080/14737175.2017.1307737
Glossary
Keywords: nurse, anxiety, depression, burnout, occupational health, structural equation model
Citation: Liu F, Zhao Y, Chen Y and Tu Z (2023) The mediation effect analysis of nurse’s mental health status and burnout under COVID-19 epidemic. Front. Public Health. 11:1221501. doi: 10.3389/fpubh.2023.1221501
Edited by:
Murat Yildirim, Ağrı İbrahim Çeçen University, TürkiyeReviewed by:
Daniel Joseph Berdida, University of Santo Tomas, PhilippinesMarcin Moroń, University of Silesia in Katowice, Poland
Copyright © 2023 Liu, Zhao, Chen and Tu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhuote Tu, MjAwNTAxNkBxem1jLmVkdS5jbg==
 Fuzhi Liu
Fuzhi Liu Yanyan Zhao2
Yanyan Zhao2