- 1Laboratory of Sport and Exercise Psychology, Department of Physical Education, Santa Catarina State University, Florianópolis, Brazil
- 2Department of Human Sciences, Society and Health, University of Cassino and Lazio, Cassino, Italy
Background: The COVID-19 pandemic has changed our habits and lifestyle due to social isolation and mobility restrictions. This new scenario, together with the fear of contracting the coronavirus, influenced mental health, especially among older adults, who presented reductions in social contact and physical activity (PA). Thus, the objective of the study was to analyze the impact caused by social isolation during the COVID-19 pandemic on the mood states of active and sedentary older adults.
Methods: This is an observational study conducted during the COVID-19 pandemic. Older adults aged over 60 years, who were registered in the database of the Secretariat for the Promotion of Citizenship from a city in southern Brazil, participated in the research. An online questionnaire was applied with questions about sociodemographic characteristics, level of PA, confinement, and mood states in two periods: May 2020 and June 2021. The Mann–Whitney U test was used to compare the mood states of active and inactive individuals during the pandemic.
Results: One hundred and fifty participants answered the questionnaire, of which 80 (53.3%) reported practicing PA. More active older adults suffered fewer changes in mood when compared to inactive older adults, with lower levels of confusion (p = 0.035), depression (p = 0.002), and fatigue (p = 0.000). Older adults confined for more than 50 days were more likely to develop depression. In addition, the mood state correlated with the variable fear of contracting the coronavirus; the greater the fear, the greater the mental confusion, depression, fatigue, and tension, and the lower the vigor in the older adults. The practice of PA is also correlated with the mood state; the greater the number of hours dedicated to PA, the lower the confusion, depression, fatigue, and tension of the older adults.
Conclusion: The practice of PA positively influenced the mental health of older adults during periods of isolation and social restrictions. PA has a protective factor for the development of mental health problems and improves mood states, with greater time performing PA leading to more benefits.
Introduction
In March 2020, the World Health Organization (WHO) declared the COVID-19 pandemic a public health concern (1). Due to the high transmission rate of the disease, social isolation measures were used worldwide to reduce transmission of the virus and prevent associated diseases and deaths (2, 3).
The pandemic has presented new challenges for society. It has been shown that the COVID-19 pandemic is associated with higher levels of worry, fatigue, loneliness, avoidance, and covid-anxiety syndrome across different countries (4, 5). In Brazil, the first case of COVID-19 was in February 2020, but soon the cases began to grow, with Brazil being the second country with the most deaths from COVID-19 in the world (6). In this context, the older adult population was characterized as a risk group, with greater chances of developing more severe forms of the disease, requiring intensive care, due to a higher rate of hospitalizations and a higher incidence of deaths (7, 8). Thus, these factors directly implied the severity of the degree of isolation of this population (9), which negatively affected mental health and well-being (10), due to emotional stress factors, such as activity restrictions, mourning for family and friends, and conflicting information from social media (11).
As a result of these factors, significant increases in anxiety and depression rates were observed during this period (12). Deleterious effects were also observed in mood states, which are frequently temporary and can vary in intensity and duration (13). The ideal mood profile is known as the iceberg profile, characterized by a high level of vigor and low levels of tension, fatigue, anger, depression, and confusion (14, 15). Although researchers have reported that with advancing age, the mood profile tends to approach the iceberg profile, in the midst of confinement, negative changes were observed, which demonstrated that most mood variables suffered oscillations mediated by the restrictive measures of each moment (16).
The COVID-19 pandemic presented several challenges for the population due to lifestyle changes related to social isolation (17). Older adults, characterized as a risk group, presented significantly reduced practice of physical activity (PA) and social contact and were exposed to several psychological stress factors that negatively affected mental health (18, 19). Studies have revealed disturbances in the mood profile of the population, reporting increased levels of tension, depression, fatigue, anger, and confusion, as well as a reduction in vigor, compared to previously observed patterns (20).
In the context prior to the pandemic, physical inactivity was already considered a global health problem, being considered the fourth largest risk factor for mortality in the world and an economic burden for society (21, 22). In addition, the isolation related to COVID-19 negatively influenced health-related behaviors because, during this period, older adults presented a reduction in the quality of nutritional standards, increased alcohol consumption, and more expressively, significantly reduced practice of physical activity (11). This reduction was associated with an increase in sitting time, and reductions in the value of metabolic equivalents of task (METs), and the number of daily steps (23). While the practice of PA during the pandemic was associated with improved well-being, quality of life, and mood in general (24, 25), deprivation or reduced practice was associated with several negative effects on the physical and mental health of older adults, reinforcing the relevance of maintaining the practice of PA within the possibilities of low exposure to the virus in this context (26).
In this way, social isolation negatively influences mood states and the level of PA (27, 28), and lower levels of PA directly impact mood states (29), thus a vicious cycle is formed. However, the use of PA to interrupt this cycle has been shown to be efficient. In younger people (19–59 years), moderate PA during the isolation period improved mental health (30), being a strategy used in different populations even before periods of restriction. Considering the relevance of the topic and the lack of studies that relate mood in older adults and the practice of PA during social isolation due to the COVID-19 pandemic, the aim of the current study was to analyze the impact caused by social isolation during the COVID-19 pandemic on the mood states of active and sedentary older adults.
Methods
Study design and participants
This observational study was conducted using self-administered online questionnaires during two moments of the pandemic: May 2020 and June 2021, periods characterized by a higher and lower level of social isolation according to the restrictive measures of the Brazilian health authorities, respectively. The older adults were recruited from the databases of the Secretariat for the Promotion of Citizenship from a city in southern Brazil. A telephone contact was made to verify the interest in participating in the study. For those interested, a link was sent to access the questionnaire through Google Forms. People aged 60 or over of both sexes, residents of their own homes or family members, were included in the sample.
The study was approved by the Ethics Committee for Research Involving Human Beings of the State University of Santa Catarina, under number 40392220.2.0000.0118. The questionnaire was evaluated anonymously. The patients/participants provided their written informed consent to participate in this study. Sociodemographic data related to social isolation/confinement, level of PA, and mood states were collected.
Sociodemographic and clinical aspects
Self-administered questionnaires were used to collect data on sociodemographic and clinical characteristics, including sex, age, marital status, and occupation, as well as PA, level of apprehension/fear about contracting COVID-19, and period of social isolation. The levels of PA were collected from the participants according to the question: How many hours a week do you dedicate to physical exercises and sports during the quarantine period? Participants were classified as inactive (no exercise) or active (performed physical exercise for at least 30 min a week). Confinement levels were collected with the following question: Approximately how many days have you been confined for? For the classification of confinement levels, the criterion based on the analysis of the likelihood test was used, thus the best classification used was up to 50 days confined and more than 50 days confined.
Mood states
The Profile of Mood States (POMS) is one of the most used tools for assessing moods across various populations (31, 32). The Brunel Mood Scale (BRUMS), derived from the POMS, was used to assess mood states (tension, depressed mood, anger, vigor, fatigue, and confusion) (33). The BRUMS consists of 24 questions, with response options for each one ranging from 0 (none) to 4 (extremely), depending on the mood state at the time of assessment. The total score for each mood ranges from 0 to 16. The BRUMS has proven to be a valid and reliable tool to assess the mood state of Brazilian and the older adult population (33, 34).
Statistical analysis
Data analysis was performed using the software Statistical Package for the social sciences (version 20.0), with descriptive statistics (mean, standard deviation, frequency, and percentage) and inferential statistics. The distribution of data normality was determined by the Kolmogorov–Smirnov test. The Mann–Whitney U test was used to compare the mood states of active and inactive individuals during the pandemic, in addition to comparing the mood of older adults at the beginning and end of social isolation. Spearman’s correlation test was used to verify the correlation between mood and the degree of social isolation. Data were stratified by age (over 70 years old or under 70 years old). The Mann–Whitney U test was used to compare age ratings. Factors associated with depression in older adults during the pandemic were analyzed using logistic regression. Thus, it was possible to estimate the crude and adjusted odds ratios (OR), as well as their respective 95% confidence intervals (95% CI). The independent variables were inserted according to the following hierarchical model: sex, marital status, and educational level in the first level, days of confinement and fear of contracting coronavirus in the second level, and physical activity in the third level. The hierarchical model is used when the choice of factors to be included in the model is based on a conceptual structure, which describes the hierarchical relationships between risk factors. This model is used to study the determinants of childhood infectious diseases, illnesses, malnutrition, low birth weight, infant mortality, hypertension and obesity (35). While the following examples are derived from the field of child health, the general principles apply to many other health issues as well. The hierarchical model was applied in this article with the objective of estimating the factors associated with the presence of mood state depression in the older adult during the pandemic. Socioeconomic factors are the distal determinants (gender, marital status, and education) and can affect, directly or indirectly, all other groups of risk factors. Second-level variables include, in turn, days of confinement and fear of contracting the coronavirus and can affect third-level variables, in this case physical activity (36).
For the categorization of variables, a likelihood test was used, as proposed by Bu et al. (37), using a proportion of 0.5. Variables were included in the adjusted model regardless of the p-value of the crude analysis. The significance level used in this study was p < 0.05.
Results
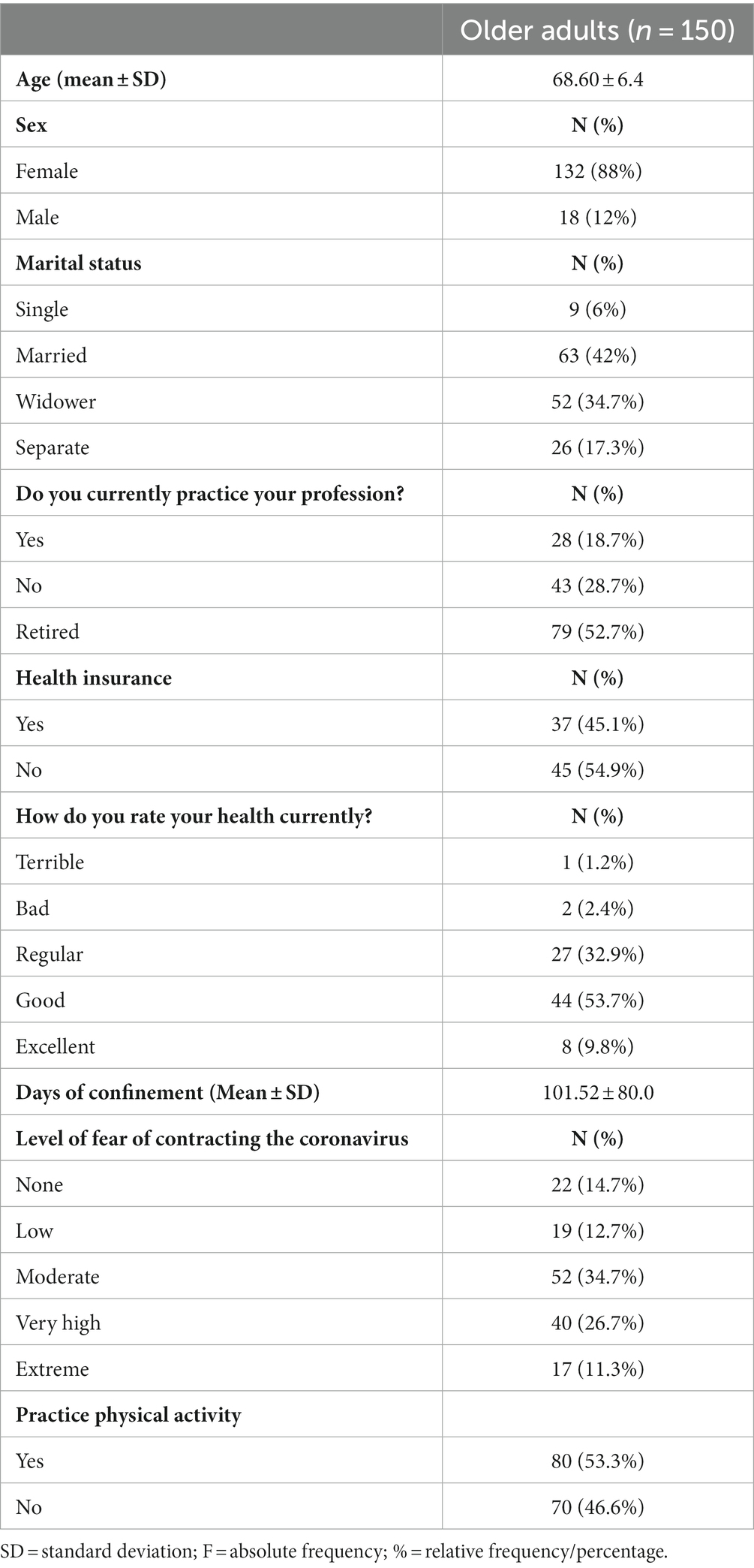
A total of 255 older adults were invited to participate in the study, of which 150 answered the questionnaires, 83 in the first data collection and 67 in the second. Most of the older adults were women (88%) and were between 60 and 87 years old. Table 1 presents the sociodemographic characteristics of these individuals.
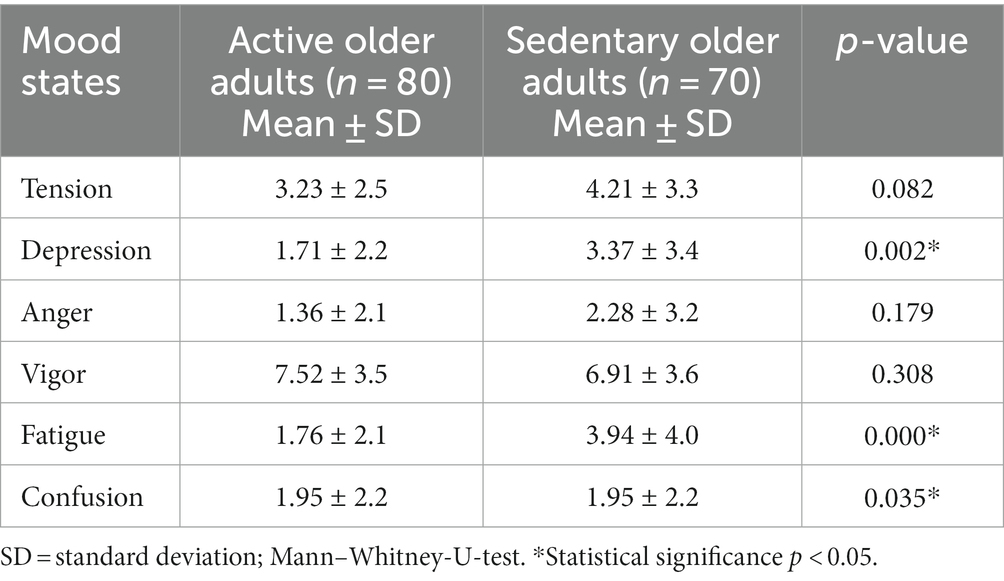
Older adults who remained active during the pandemic showed a more positive mood for mental health and had lower levels of confusion (p = 0.035), depression (p = 0.002), and fatigue (p = 0.000) compared to sedentary older adults (Table 2). When stratifying by age, there was a difference in depression (p = 0.034) and fatigue (p = 0.030) between active and sedentary older adults aged less than 70 years, in addition to a difference in depression between active and sedentary older adults aged over 70 years (p = 0.038).
In addition, older adults who remained confined for more than 50 days were more likely (23 times) to develop mood depression (OR 0.23; CI 1.10–0.61) (Table 3).
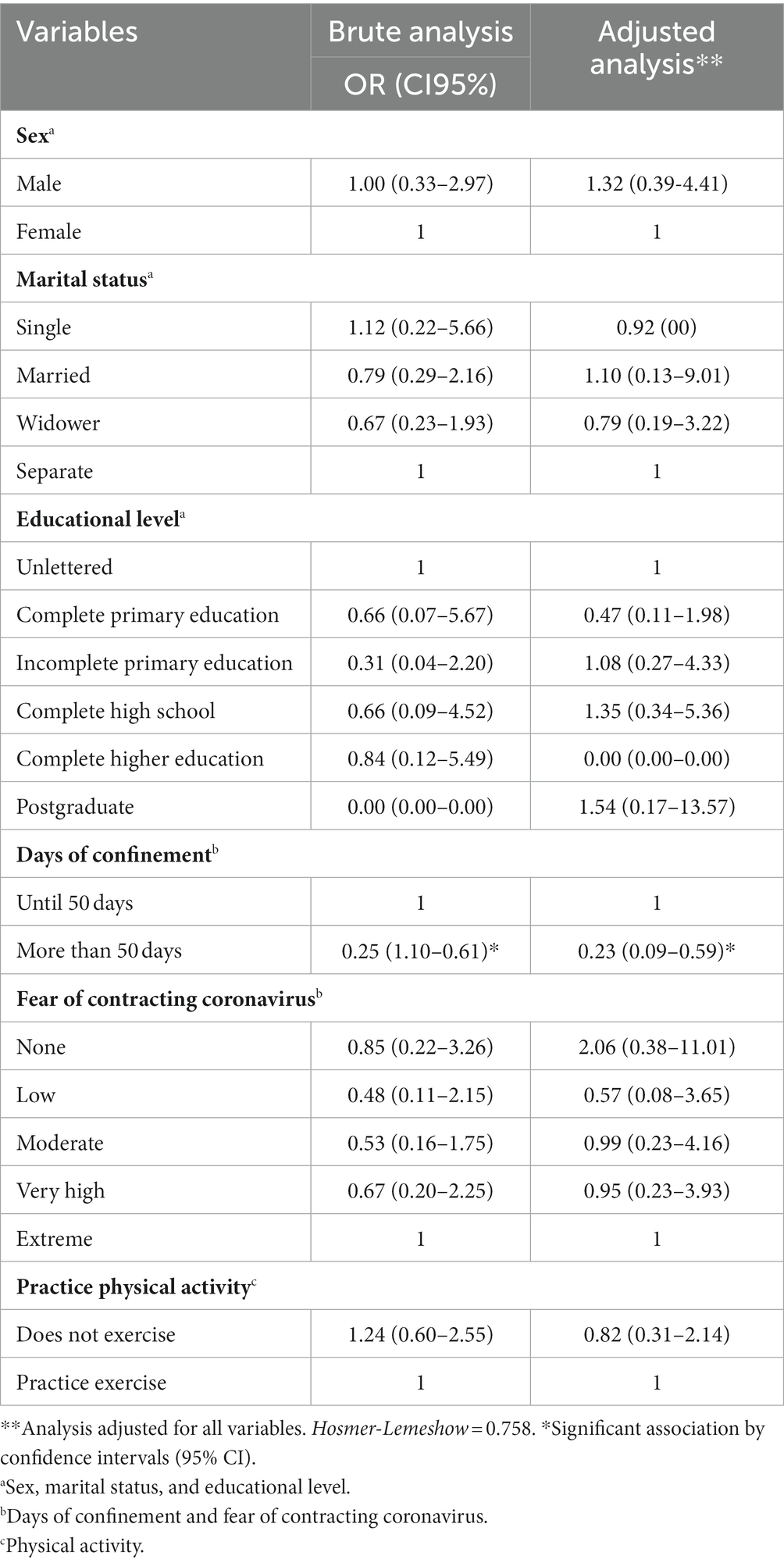
Table 3. Factors associated with the presence of mood state depression in the older adults during the pandemic.
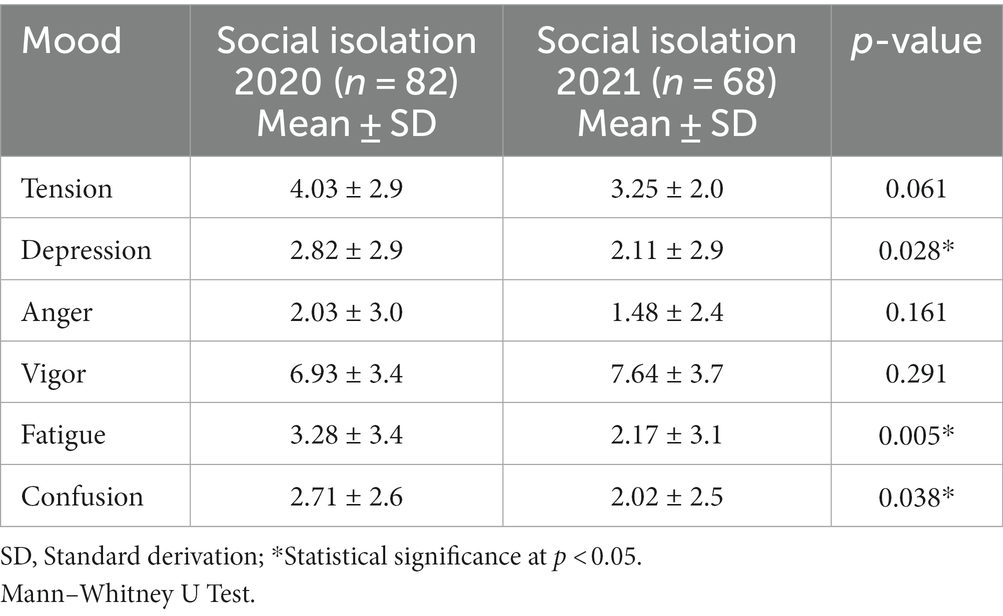
Older adults at the end of social isolation showed a reduction in confusion, depression, and fatigue when compared to the beginning of isolation (2020) (Table 4). In the stratification by age, there was a difference in fatigue (p = 0.022) in older adults under 70 years old, whereas in older adults over 70 years old, the differences were in the variables depression (p = 0.005) and fatigue (p = 0.048) between days of social isolation.
Figure 1 represents the iceberg profile identified in the older adults according to the practice of physical activity, the pandemic period, and age.
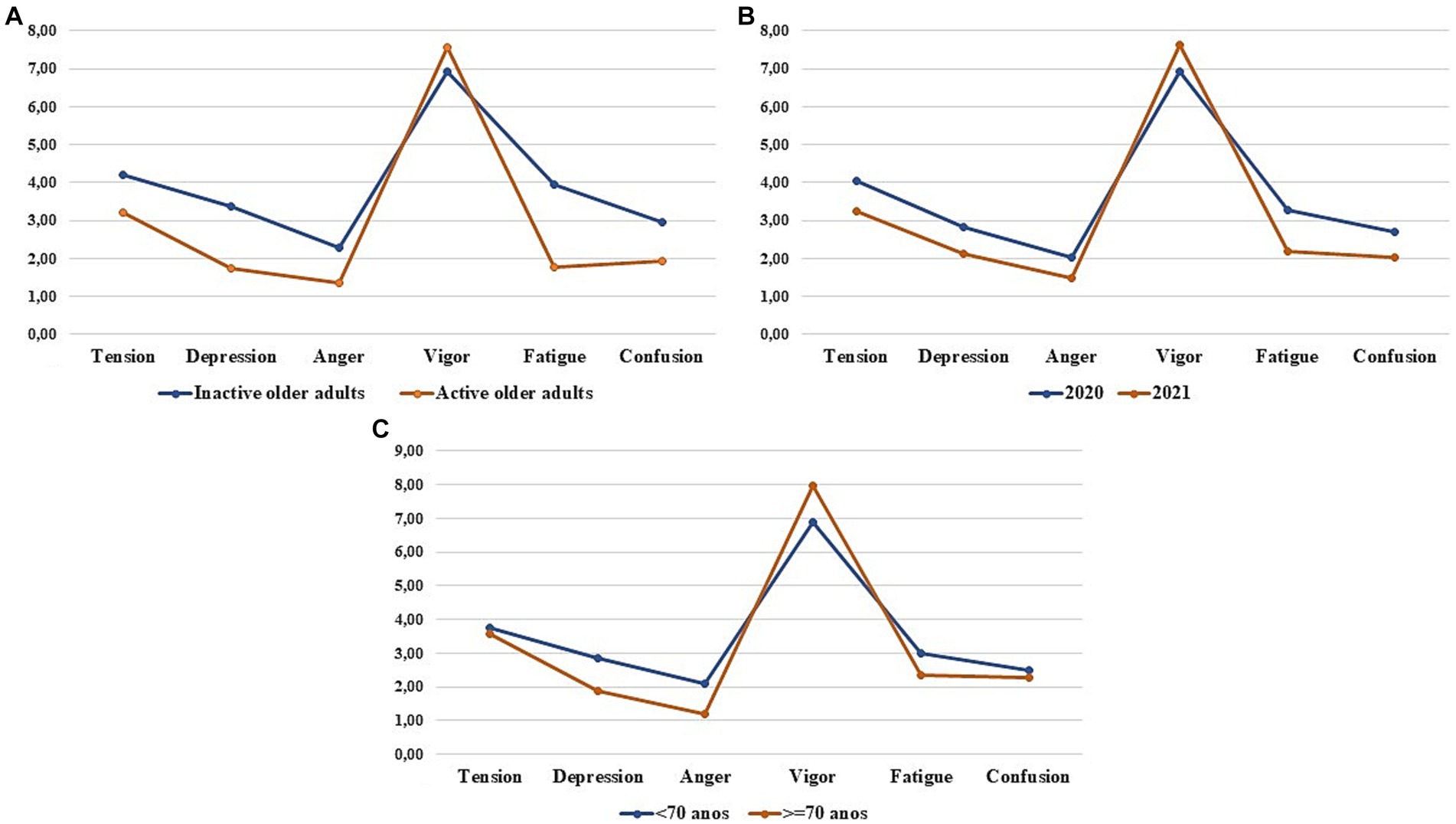
Figure 1. Mood profile of older adults according to physical activity (A), pandemic period (B) and age (C).
Correlations were observed between the degree of social isolation and mood in the older adults during the COVID-19 pandemic. The older adults who left home more frequently during the pandemic performed more hours of physical activity (p = 0.000; r = 0.487), and presented the following characteristics in terms of mood: less confusion (p = 0.022; r = −0.250), depression (p = 0.001; r = −0.358), fatigue (p = 0.019; r = −0.256), and tension (p = 0.014; r = −0.268) when compared to older adults with more days of social isolation.
Similar results were observed when stratifying by age. In older adults under 70 years of age, the variable number of times a week they left home correlated with depression (p = 0.031; r = −0.305) and vigor (p = 0.046; r = 0.283). In the older adults over 70 years of age, it was found that the greater the number of days they left home, the less the confusion (p = 0.003; r = −0.509), depression (p = 0.016; r = −0.421), and tension (p = 0.009; r = −0.457), suggesting that a greater the number of days in social isolation is associated with worsening mental health of the older adults.
The mood state also correlated with the variable fear that the older adults have of contracting the coronavirus; the greater the fear of contracting the coronavirus, the greater the confusion (p = 0.020; r = 0.189), depression (p = 0.026; r = 0.181), fatigue (p = 0.022; r = 0.186), and tension (p = 0.002; r = 0.251), and the lower the vigor (p = 0.033; r = −0.173) in older adults.
The practice of physical activity also correlated with mood states; the greater the number of hours dedicated to physical activity, the lower the mental confusion (p = 0.022; r = −0.244), depression (p = 0.000; r = −0.308), fatigue (p = 0.000; r = −0.372), and tension (p = 0.015; r = −0.197) of older adults (Table 5).
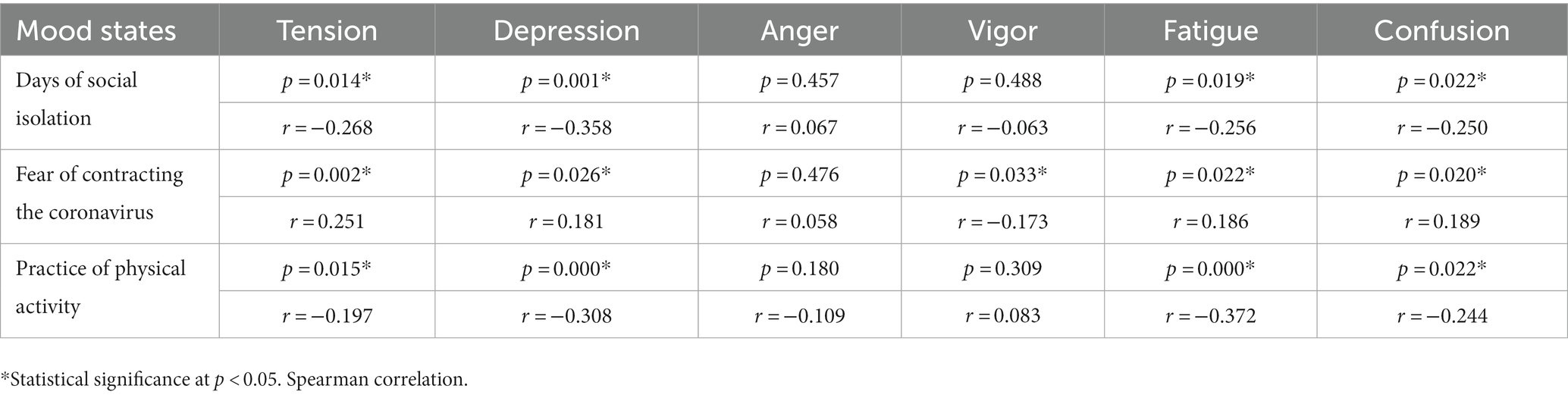
Table 5. Mood state correlations with days of social isolation, fear of contracting the coronavirus and practice of physical activity.
Discussion
During the COVID-19 pandemic, an increase in the prevalence of mood disorders was observed due to social isolation and fear of contracting the disease (10, 20, 38), allied with a reduction in the level of PA (26). However, the practice of PA has been shown to mitigate the deleterious effects of confinement on mental health (25).
In the present study, less confined older adults who left the house on more days performed more PA and presented a better mood profile, with lower levels of mental confusion, depression, fatigue, and tension, when compared to the more confined older adults, reinforcing the associations between confinement, PA, and mental health, already evidenced in other studies (39, 40).
Relationship between confinement and mental health
According to Santomauro et al. (41) the reduction in human mobility was considered one of the biggest factors associated with the emergence of mood disorders during the pandemic. In the study conducted by Richardson et al. (16) with older adults in the United Kingdom, depressive mood increased until the beginning of the easing of restrictive measures, reinforcing the possible relationship between isolation and mental health. In our study, older adults who were confined for more than 50 days were 23 times more likely to develop a depressed mood. When analyzing the mood profile during different periods of the pandemic, it was observed that at the end of 2021, the older adults presented a better mood profile (less confusion, depression, and fatigue) than in 2020.
Factors such as fear, uncertainty, economic hardship, and changes in daily habits showed a negative correlation with the general population’s mental health (42). Fear of COVID-19 has been shown to be significantly associated with worsening mental health status, negatively influencing factors such as anxiety, stress, depression, and sleep quality (43). In our study, the variable fear of contracting the coronavirus was positively correlated with confusion, depression, fatigue, and tension, and negatively correlated with vigor in the older adults, thus demonstrating that individual concern related to COVID-19 potentiated the deleterious effects of confinement in older adults. This result may be associated with the fact that due to the fear of contracting COVID-19, many older adults were isolated, which reduced the level of PA.
Mood profile and levels of physical activity
The practice of PA during the pandemic seems to be a factor that promotes mental health and protects against depression, fatigue, and confusion in mood in older adults.
PA was already recommended for the older adult population before the outbreak of COVID-19, as it helps to maintain physical and mental health, in addition to being considered a form of treatment for various diseases and health problems (44–49). Furthermore, PA can help improve the quality of life (50, 51) and psychological well-being associated with positive mood indices (52, 53). Therefore, during the pandemic, maintaining PA levels was essential to reduce the damage caused by isolation. However, a reduction in PA was observed in the general population, including among older adults (26).
PA proved to be fundamental during the pandemic, as active older adults had lower levels of confusion, depression, and fatigue. Analyzing other factors, the practice of PA continued to show positive results. When comparing older adults over and under 70 years of age, we found that the younger group presented more benefits with the practice of PA, since among those over 70 years old there were significant improvements only in depression. With increasing age, it is expected that older adults will have more difficulties in moving and performing exercises, which may explain the differences between the groups since the PA practice was not controlled. In the study carried out by Sojli et al. (54), emotional stress related to COVID-19 was similar in individuals aged 65–75 years or older and relatively low when compared to other age groups, however, the practice of PA was not analyzed.
Corroborating the findings related to the protective effect of PA on the mental health of older adults, other studies observed a relationship between PA and depressive symptoms (55, 56). In addition, a review showed that higher levels of PA in volume, frequency, and regularity are associated with lower levels of symptoms of depression and anxiety in the general population (57). Important dose-response relationships that enhance the protective effect were also observed through the negative correlation between the number of hours dedicated to PA and the mood profile observed in the older adults in the variables confusion, depression, fatigue, and tension.
The WHO recommends the practice of at least 150 min of PA per week and reinforces that any level of PA greater than none can be beneficial to health when compared to physical inactivity (58). In the current study, it was observed that 30 min of PA or more were enough to improve the mental health of the older adults during the pandemic, reinforcing the relevance of protection and promotion that increased levels of PA provided. These results are in line with scientific evidence, since PA presents, through various functions such as psychological, physiological and immunological, a vital component for the health of different populations, one of them investigated in the present study as the older adults (59, 60). In this regard, home-based physical exercise programs for older adults seem to offer a safe, easily accessible, and low-cost PA alternative for this population (61).
Limitations and future studies
Despite the important results verified, this study has some limitations, such as the small sample size, the sample being from a single municipality, and the majority of participants being female. In addition, it was not verified whether the participants had mental health problems before the pandemic and the intensity of the practice of PA was not evaluated.
Future studies should be developed, including monitoring variables regarding the type of physical exercises, volume, intensity, duration, and weekly sessions, among others, in addition to expanding mental health variables during the post-pandemic process of COVID-19.
Future studies should try to measure the level of daily activity of the participants, considering that activities of daily living (for example, gardening, sweeping the house, among others), can also be considered physical activities, depending on the amount performed weekly, and may also impact the physical and mental health of participants.
Another point to be considered as a limitation is the level of distraction that the participants had, when they did not remain in isolation, since in our findings, the older adults who left home more presented a better mood profile, compared to the group with more days in social isolation. In new studies, it would be interesting to identify the level of distraction or interaction when the older adults do not remain in social isolation (outside their homes), in order to identify if there are any additional relationships, considering the greater chance of social contact and even levels of daily activities, affecting physical activity. In addition, future studies should consider the role of possible pharmacological or psychological treatments.
Studies with proposals and applications of different physical exercise protocols for older adults are recommended, both at the individual level and for future public policies.
Strengths, innovations, and applications of the study
Our study is one of the rare empirical investigations on this subject, being innovative as it presents a comprehensive view of changes in the mood of older adults during the pandemic associated with the practice of PA. One of the strengths of the study is the analysis of the time of social confinement to which many older adults were subjected during the pandemic, its effects on mood and mental health, and the role of PA in this context. Relevant aspects of the effects of social confinement and the possible protective effect of PA on the mental health of older adults in a pandemic context were demonstrated.
As applications of the findings, we can highlight the need for attention to the time of social isolation that older adults are subjected to, during pandemics or even in social isolation contexts, to reduce these periods as much as possible and provide options for PA remotely, face-to-face, or with the use of technologies, seeking to motivate and promote PA for older adults, knowing the benefits to physical and mental health. These findings can be used as a source of inspiration to guide public policies.
Conclusion
The practice of PA positively influences the mental health of older adults during periods of isolation and social restrictions. PA, for older adults in social isolation, seems to be a protective factor against the development of mental health problems, and may improve mood states, especially depression, fatigue, and confusion. Exposure to long periods of social confinement is a high-risk factor for mood and mental health problems, especially when associated with a sedentary lifestyle.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee for Research Involving Human Beings of the State University of Santa Catarina. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AA contributed to the design and coordination in the production of the study. AA, AD’O, and GV contributed to data acquisition, data analysis and interpretation. AA, AD’O, GV, SC, and PD critically reviewed the article for intellectual content. KS contributed to data analysis and interpretation. AB, AD’O, and GV drafted the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Research and Innovation Support Foundation of the State of Santa Catarina (FAPESC), Grant Ref: 2019031000035, and call number no. 027/2020. This funding refers to FAPESC public call no. 27/2020: Infrastructure support for UDESC research groups. This study was a subproject of an umbrella project of the Laboratory of Sports and Exercise Psychology (LAPE) and for that reason did not receive individual funding.
Acknowledgments
We are grateful to CAPES (Coordination for the Improvement of Higher Education Personnel—Brazil), and to the Secretariat for the Promotion of Citizenship, and the City Hall of Itajaí—Santa Catarina, Brazil, for providing the list of assisted older adults, necessary to the present research, as well as for having given all the necessary support throughout the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19): Interim guidance, 19 march 2020 World Health Organization (2020). 4 p. Available at: https://apps.who.int/iris/handle/10665/331497
2. Qian, M, and Jiang, J. COVID-19 and social distancing. J Public Health (Germany). (2022) 30:259–61. doi: 10.1007/s10389-020-01321-z
3. Diotaiuti, P, Valente, G, Mancone, S, Falese, L, Bellizzi, F, Anastasi, D, et al. Perception of risk, self-efficacy and social trust during the diffusion of Covid-19 in Italy. Int J Environ Res Public Health. (2021) 18:3427. doi: 10.3390/IJERPH18073427
4. Brailovskaia, J, Cosci, F, Mansueto, G, Miragall, M, Herrero, R, Baños, RM, et al. The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: an investigation in Germany, Italy, Russia, and Spain. Psychiatry Res. (2021) 295:113596. doi: 10.1016/j.psychres.2020.113596
5. Mansueto, G, Palmieri, S, Marino, C, Caselli, G, Sassaroli, S, Ruggiero, GM, et al. The Italian COVID-19 anxiety syndrome scale: investigation of the COVID-19 anxiety syndrome and its association with psychological symptoms in an Italian population. Clin Psychol Psychother. (2022) 29:1972–90. doi: 10.1002/cpp.2767
6. WHO. WHO coronavirus (COVID-19) dashboard. (2023). Available at: https://covid19.who.int/ (Accessed October 11, 2021).
7. Bonanad, C, García-Blas, S, Tarazona-Santabalbina, F, Sanchis, J, Bertomeu-González, V, Fácila, L, et al. The effect of age on mortality in patients with COVID-19: a Meta-analysis with 611, 583 subjects. J Am Med Dir Assoc. (2020) 21:915–8. doi: 10.1016/j.jamda.2020.05.045
8. Centers for Disease Control And Prevention. Older Adults Risks and Vaccine Information | cdc. (2021). Available at: https://www.cdc.gov/aging/covid19/covid19-older-adults.html (Accessed December 6, 2022).
9. MacLeod, S, Tkatch, R, Kraemer, S, Fellows, A, McGinn, M, Schaeffer, J, et al. COVID-19 era social isolation among older adults. Geriatrics. (2021) 6:52. doi: 10.3390/geriatrics6020052
10. Diotaiuti, P, Valente, G, Mancone, S, Corrado, S, Bellizzi, F, Falese, L, et al. Effects of cognitive appraisals on perceived self-efficacy and distress during the COVID-19 lockdown: an empirical analysis based on structural equation modeling. Int J Environ Res Public Health. (2023) 20:5294. doi: 10.3390/IJERPH20075294
11. Visser, M, Schaap, L, and Wijnhoven, H. Self-reported impact of the COVID-19 pandemic on nutrition and physical activity behaviour in Dutch older adults living independently. Nutrients. (2020) 12:1–11. doi: 10.3390/nu12123708
12. Webb, LM, and Chen, CY. The COVID-19 pandemic’s impact on older adults’ mental health: contributing factors, coping strategies, and opportunities for improvement. Int J Geriatr Psychiatry. (2022) 37:10.1002/gps.5647. doi: 10.1002/gps.5647
13. Lane, AM, and Terry, PC. The nature of mood: development of a conceptual model with a focus on depression. J Appl Sport Psychol. (2000) 12:16–33. doi: 10.1080/10413200008404211
14. Parsons-Smith, RL, Terry, PC, and Machin, MA. Identification and description of novel mood profile clusters. Front Psychol. (2017) 8:1958. doi: 10.3389/FPSYG.2017.01958/FULL
15. Terry, PC, Parsons-Smith, RL, King, R, and Terry, VR. Influence of sex, age, and education on mood profile clusters. PLoS One. (2021) 16:e0245341. doi: 10.1371/JOURNAL.PONE.0245341
16. Richardson, DL, Tallis, J, Duncan, MJ, Clarke, ND, and Myers, TD. The ongoing effects of the COVID-19 pandemic on perceived physical activity, physical function and mood of older adults in the U.K: a follow-up study (march 2020–June 2021). Exp Gerontol. (2022) 165:111838. doi: 10.1016/J.EXGER.2022.111838
17. Tosato, M, Ciciarello, F, Zazzara, MB, Janiri, D, Pais, C, Cacciatore, S, et al. Lifestyle changes and psychological well-being in older adults during COVID-19 pandemic. Clin Geriatr Med. (2022) 38:449–59. doi: 10.1016/J.CGER.2022.05.002
18. Botero, JP, Farah, BQ, de Correia, MA, Lofrano-Prado, MC, Cucato, GG, Shumate, G, et al. Impact of the COVID-19 pandemic stay at home order and social isolation on physical activity levels and sedentary behavior in Brazilian adults. Einstein (São Paulo). (2021) 19:eAE6156. doi: 10.31744/einstein_journal/2021AE6156
19. Klaiber, P, Wen, JH, Delongis, A, and Sin, NL. The ups and downs of daily life during COVID-19: age differences in affect, stress, and positive events. J Gerontol Ser B Psychol Sci Soc Sci. (2021) 76:E30–7. doi: 10.1093/geronb/gbaa096
20. Terry, PC, Parsons-Smith, RL, and Terry, VR. Mood responses associated with COVID-19 restrictions. Front Psychol. (2020) 11:589598. doi: 10.3389/FPSYG.2020.589598/FULL
21. Ding, D, Lawson, KD, Kolbe-Alexander, TL, Finkelstein, EA, Katzmarzyk, PT, van Mechelen, W, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet. (2016) 388:1311–24. doi: 10.1016/S0140-6736(16)30383-X
22. World Health Organization. The global health observatory-physical inactivity. (2012). Available at: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3416 (Accessed January 11, 2022).
23. Silva, LRB, Seguro, CS, de Oliveira, CGA, Santos, POS, de Oliveira, JCM, de Souza Filho, LFM, et al. Physical inactivity is associated with increased levels of anxiety, depression, and stress in Brazilians during the COVID-19 pandemic: a cross-sectional study. Front Psych. (2020) 11:1257. doi: 10.3389/FPSYT.2020.565291/BIBTEX
24. Fennell, C, Eremus, T, Puyana, MG, and Sañudo, B. The importance of physical activity to augment mood during COVID-19 lockdown. Int J Environ Res Public Health. (2022) 19:1270. doi: 10.3390/IJERPH19031270
25. Marconcin, P, Werneck, AO, Peralta, M, Ihle, A, Gouveia, ÉR, Ferrari, G, et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. (2022) 22:1–14. doi: 10.1186/S12889-022-12590-6/TABLES/2
26. Oliveira, M, Sudati, I, Konzen, V, Campos, A, Wibelinger, L, Correa, C, et al. Covid-19 and the impact on the physical activity level of elderly people: a systematic review. Exp Gerontol. (2022) 159:111675. doi: 10.1016/j.exger.2021.111675
27. Mon-López, D, García-Aliaga, A, Ginés Bartolomé, A, and Muriarte, SD. How has COVID-19 modified training and mood in professional and non-professional football players? Physiol Behav. (2020) 227:113148. doi: 10.1016/j.physbeh.2020.113148
28. Batalla-Gavalda, A, Cecilia-Gallego, P, Revillas-Ortega, F, and Beltran-Garrido, JV. Variations in the mood states during the different phases of COVID-19’s lockdown in young athletes. Int J Environ Res Public Health. (2021) 18:9326. doi: 10.3390/ijerph18179326
29. Hansen, CJ, Stevens, LC, and Coast, JR. Exercise duration and mood state: how much is enough to feel better? Health Psychol. (2001) 20:267–75. doi: 10.1037/0278-6133.20.4.267
30. Reigal, RE, Páez-Maldonado, JA, Pastrana-Brincones, JL, Morillo-Baro, JP, Hernández-Mendo, A, Morales-Sánchez, V, et al. Physical activity is related to mood states, anxiety state and self-rated health in COVID-19 lockdown. Sustainability. (2021) 13:5444. doi: 10.3390/su13105444
31. Terry, PC, Lane, AM, and Fogarty, GJ. Construct validity of the profile of mood states — adolescents for use with adults. Psychol Sport Exerc. (2003) 4:125–39. doi: 10.1016/S1469-0292(01)00035-8
32. Sakano, K, Ryo, K, Tamaki, Y, Nakayama, R, Hasaka, A, Takahashi, A, et al. Possible benefits of singing to the mental and physical condition of the elderly. Biopsychosoc Med. (2014) 8:11. doi: 10.1186/1751-0759-8-11
33. Rohlfs, ICPDM, Rotta, TM, Luft, CDB, Andrade, A, Krebs, RJ, and De Carvalho, T. Brunel mood scale (BRUMS): an instrument for early detection of overtraining syndrome. Rev Bras Med Esporte. (2008) 14:176–81. doi: 10.1590/S1517-86922008000300003
34. Sroykham, W, and Wongsawat, Y. Effects of brain activity, morning salivary cortisol, and emotion regulation on cognitive impairment in elderly people. Medicine. (2019) 98:e16114. doi: 10.1097/MD.0000000000016114
35. Victora, CG, Huttly, SR, Fuchs, SC, and Olinto, MTA. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. (1997) 26:224–7. doi: 10.1093/IJE/26.1.224
36. Wright, LJ, Williams, SE, and Veldhuijzen van Zanten, JJCS. Physical activity protects against the negative impact of coronavirus fear on adolescent mental health and well-being during the COVID-19 pandemic. Front Psychol. (2021) 12:580511. doi: 10.3389/FPSYG.2021.580511
37. Bu, F, Steptoe, A, and Fancourt, D. Depressive and anxiety symptoms during the COVID-19 pandemic: a two-year follow-up. med Rxiv 2022.05.24.22275529. (2022). doi: 10.1101/2022.05.24.22275529
38. Pietrabissa, G, and Simpson, SG. Psychological consequences of social isolation during COVID-19 outbreak. Front Psychol. (2020) 11:2201. doi: 10.3389/FPSYG.2020.02201/BIBTEX
39. Amo, C, Almansour, N, and Harvey, IS. Physical activity and mental health declined during the time of the COVID-19 pandemic: a narrative literature review. Int J Environ Res Public Health. (2022) 19:11230. doi: 10.3390/ijerph191811230
40. da Cruz, WM, D’Oliveira, A, Dominski, FH, Diotaiuti, P, and Andrade, A. Mental health of older people in social isolation: the role of physical activity at home during the COVID-19 pandemic. Sport Sci Health. (2022) 18:597–602. doi: 10.1007/S11332-021-00825-9
41. Santomauro, DF, Mantilla Herrera, AM, Shadid, J, Zheng, P, Ashbaugh, C, Pigott, DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
42. Pedrosa, AL, Bitencourt, L, Fróes, ACF, Cazumbá, MLB, Campos, RGB, de Brito, SBCS, et al. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front Psychol. (2020) 11:1–18. doi: 10.3389/fpsyg.2020.566212
43. Şimşir, Z, Koç, H, Seki, T, and Griffiths, MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. (2022) 46:515–23. doi: 10.1080/07481187.2021.1889097
44. Kujala, UM. Evidence on the effects of exercise therapy in the treatment of chronic disease. Br J Sports Med. (2009) 43:550–5. doi: 10.1136/bjsm.2009.059808
45. Pedersen, BK, and Saltin, B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. (2015) 25:1–72. doi: 10.1111/SMS.12581
46. Anderson, E, and Durstine, JL. Physical activity, exercise, and chronic diseases: a brief review. Sports Med Health Sci. (2019) 1:3–10. doi: 10.1016/J.SMHS.2019.08.006
47. Sieczkowska, SM, de Orleans Casagrande, P, Coimbra, DR, Vilarino, GT, Andreato, LV, and Andrade, A. Effect of yoga on the quality of life of patients with rheumatic diseases: systematic review with meta-analysis. Complement Ther Med. (2019) 46:9–18. doi: 10.1016/j.ctim.2019.07.006
48. Sties, SW, Andreato, LV, de Carvalho, T, Gonzáles, AI, Angarten, VG, Ulbrich, AZ, et al. Influence of exercise on oxidative stress in patients with heart failure. Heart Fail Rev. (2018) 23:225–35. doi: 10.1007/S10741-018-9686-Z
49. Haraldstad, K, Rohde, G, Stea, TH, Lohne-Seiler, H, Hetlelid, K, Paulsen, G, et al. Changes in health-related quality of life in elderly men after 12 weeks of strength training. Eur Rev Aging Phys Act. (2017) 14:8–6. doi: 10.1186/s11556-017-0177-3
50. Andrade, A, Sieczkowska, SM, and Vilarino, GT. Resistance training improves quality of life and associated factors in patients with fibromyalgia syndrome. PM and R. (2019) 11:703–9. doi: 10.1016/j.pmrj.2018.09.032
51. Sieczkowska, SM, Vilarino, GT, de Souza, LC, and Andrade, A. Does physical exercise improve quality of life in patients with fibromyalgia? Ir J Med Sci. (2019) 189:341–7. doi: 10.1007/s11845-019-02038-z
52. Andrade, A, de Azevedo Klumb Steffens, R, Sieczkowska, SM, Peyré Tartaruga, LA, and Torres Vilarino, G. A systematic review of the effects of strength training in patients with fibromyalgia: clinical outcomes and design considerations. Adv Rheumatol. (2018) 58:36. doi: 10.1186/s42358-018-0033-9
53. Vilarino, GT, Andreato, LV, de Souza, LC, Branco, JHL, and Andrade, A. Effects of resistance training on the mental health of patients with fibromyalgia: a systematic review. Clin Rheumatol. (2021) 40:4417–25. doi: 10.1007/S10067-021-05738-Z
54. Sojli, E, Tham, WW, Bryant, R, and McAleer, M. COVID-19 restrictions and age-specific mental health—U.S. probability-based panel evidence. Transl Psychiatry. (2021) 11:1–7. doi: 10.1038/s41398-021-01537-x
55. Callow, DD, Arnold-Nedimala, NA, Jordan, LS, Pena, GS, Won, J, Woodard, JL, et al. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am J Geriatr Psychiatr. (2020) 28:1046–57. doi: 10.1016/j.jagp.2020.06.024
56. Lage, A, Carrapatoso, S, de Queiroz, S, Neto, E, Gomes, S, Soares-Miranda, L, et al. Associations between depressive symptoms and physical activity intensity in an older adult population during COVID-19 lockdown. Front Psychol. (2021) 12:644106. doi: 10.3389/FPSYG.2021.644106/FULL
57. Wolf, S, Seiffer, B, Zeibig, JM, Welkerling, J, Brokmeier, L, Atrott, B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. (2021) 51:1771–83. doi: 10.1007/S40279-021-01468-Z
58. Bull, FC, Al-Ansari, SS, Biddle, S, Borodulin, K, Buman, MP, Cardon, G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
59. Koziel Ly, NK, Mohamud, L, Villeneuve, PJ, Matheson, K, Anisman, H, and Chee, MJ. Protective effects of physical activity on mental health outcomes during the COVID-19 pandemic. PLoS One. (2022) 17:e0279468. doi: 10.1371/journal.pone.0279468
60. Mikkelsen, K, Stojanovska, L, Polenakovic, M, Bosevski, M, and Apostolopoulos, V. Exercise and mental health. Maturitas. (2017) 106:48–56. doi: 10.1016/J.MATURITAS.2017.09.003
Keywords: physical exercise, mood states, mental health, public health, aged, SARS-CoV-2
Citation: Andrade A, D’Oliveira A, dos Santos KM, Bastos ACRdF, Corrado S, Vilarino GT and Diotaiuti P (2023) Impact of social isolation caused by the COVID-19 pandemic on the mood profile of active and sedentary older adults: physical activity as a protective factor. Front. Public Health. 11:1221142. doi: 10.3389/fpubh.2023.1221142
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Laisa Liane Paineiras-Domingos, Federal University of Bahia (UFBA), BrazilQi Wang, The University of Hong Kong, Hong Kong SAR, China
Giovanni Mansueto, University of Florence, Italy
Copyright © 2023 Andrade, D’Oliveira, dos Santos, Bastos, Corrado, Vilarino and Diotaiuti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandro Andrade, YWxleGFuZHJvLmFuZHJhZGUucGhkQGdtYWlsLmNvbQ==
 Alexandro Andrade
Alexandro Andrade Anderson D’Oliveira
Anderson D’Oliveira Keyla Mara dos Santos
Keyla Mara dos Santos Ana Cecilia Rosatelli de Freitas Bastos
Ana Cecilia Rosatelli de Freitas Bastos Stefano Corrado
Stefano Corrado Guilherme Torres Vilarino
Guilherme Torres Vilarino Pierluigi Diotaiuti
Pierluigi Diotaiuti