
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 01 August 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1219573
This article is part of the Research Topic Active and Healthy Aging and Quality of Life: Interventions and Outlook for the Future, volume II View all 25 articles
Background: Active aging has been listed as an important indicator to measure the quality of life of the older adults and the construction of the senior care system. There is an imbalance between the supply and demand of senior care services for the disabled older adults in rural areas, and the quality of life needs to be improved.
Objectives: We aimed to analyze the current situation of active aging and the influencing factors of the rural disabled older adults, in order to provide a reference basis for improving the quality of life of the rural disabled older adults.
Methods: We conducted a multicenter and cross-sectional study, using the Barthel Index Scale and Chinese version of the Active Aging Scale, to facilitate the selection of 304 rural older adults with disability in 26 villages under Henan Province for a questionnaire survey.
Results: The mean score for the level of active aging of rural older adults with disability was 1.87 (SD 0.36), with the highest score for the dimension of being self-reliant (Mean2.29, SD 0.61) and lower scores for the dimension of active contribution to society (Mean 1.37, SD 0.55) and building up financial security (Mean 1.37, SD 0.57). The results of the multiple regression analysis showed higher levels of active aging among the disabled older adults with retirement pay, mild disability, and longer time per activity/rehabilitation exercise (p < 0.05).
Conclusion: Active aging of the rural disabled older adults is at a low level, with insufficient economic security and social participation. The national government should help improve the quality of primary health care in rural areas, build a friendly environment for senior communities, and improve policies to protect the welfare of the older adults, so as to collaboratively empower the disabled older adults in rural areas at three levels: health, participation, and protection.
The number and proportion of older people in countries around the world is on the rise, with the number of people over 60 increasing from 1 billion to 1.4 billion between 2020 and 2030, and the number of people over 60 expected to increase to 2.1 billion in 2050, and the number of people over 80 tripling to 426 million, with the greatest trend of change in low-and middle-income countries (1). China’s seventh census data show that by 2020 China’s older adults aged 60 and above has reached 264 million (2), the scale of disabled older adults has reached 6.18 million, the proportion of disabled older adults in rural areas reached 50.16%, the disablement rate of rural older adults reached 2.86%, which is 0.58% higher than that in urban areas (3), the phenomenon of aging and disablement in rural areas is serious and has gradually become the strategic focus of the country to actively deal with the problem of aging population.
In 2002, the World Health Organization officially introduced the concept of active aging and defined active aging in its Global Report on Aging and Health as “the process of optimizing the health, social participation and security opportunities of older adults in order to improve their quality of life (4). Active aging has been recognized by the international community as a fundamental initiative to address population aging (5). The European Union, as the regional international organization that has used and studied the concept of active aging the most and the earliest, has further validated the feasibility and socio-economic benefits of active aging strategies by transforming policy advocacy into concrete policy actions based on coordination among member states (6). In addition, establishing the perception of active aging has been proven to improve physical function, cognitive function, mental health, social health and sleep status of older adults (7).
In 2017, China issued the “13th Five-Year Plan for the Development of the National Aging Career and the Construction of the Pension System,” which listed active aging as an important indicator for measuring the quality of life of the older adults and the construction of the pension system (8). In 2021, the “Outline of the 14th Five-Year Plan for National Economic and Social Development and Vision 2035” established the national strategic position of actively coping with population aging (9). In order to implement this national strategy, the “Opinions on Strengthening the Work on Aging in the New Era” issued by the Central Committee of the Communist Party of China and the State Council put forward a number of macroscopic guidelines on the senior care service system, health support system, social participation of the older adults and silver hair economy, and emphasized the need to integrate the concept of active aging and healthy aging into the whole process of economic and social development, advocate the implementation of mutual aid and medical and nursing care models, and strengthen long-term care services and protection for the disabled older adults (10). However, there are still many dilemmas in the actual operation of the combined medical and nursing care and mutual care models in rural China, such as incomplete integration of resources, lack of nursing professionals, and difficulties in building organizational support (11, 12). Additionally, multiple factors such as lack of medical care, financial difficulties, age discrimination and social exclusion also seriously hinder the development of active aging in rural areas (13).
Health, participation, and security are the three pillars of active aging. Rural older adults with disability have declining physical functions, lack of health knowledge, cognitive bias, weak awareness, limited social and productive participation (14), lack of adequate protection of their rights and interests in material economy, medical assistance, spiritual and cultural life (15), and low level of well-being and self-assessed health (16). However, the rural older adults with disability have strong needs in terms of health knowledge, social participation, and social security, and a comprehensive assessment is urgently needed to improve their active aging (17). Currently, there is an increasing number of studies on active aging, which mainly focus on policy exploration, pathways and multidimensional factor analysis at the theoretical level (18, 19), and related intervention studies are mostly focused on older adults in urban communities, but less benefit older adults in rural and remote areas, and only the research team has conducted a qualitative study focusing on the level of active aging of older adults with disability in rural areas (17). Therefore, this study combines the qualitative research results of the previous research group and adopts quantitative thinking to investigate the current status of active aging of rural disabled older adults on a large scale, in order to provide a reference basis for improving the rural senior care service system.
This study used a multicenter and cross-sectional survey research design. From July to December 2022, a random number table method was used to select three prefectures from 17 prefectures in Henan Province, China, as the study site, and subsequently to facilitate the selection of questionnaires from 26 administrative villages under them for the older adults with disability. Inclusion criteria: ① ≧60 years old; ② Have rural household registration in China and have lived in the local area for at least 1 year; ③ Barthel index (BI) assessment <100 points, those with partial or total loss of self-care ability; ④ No serious visual–auditory or communication dysfunction; ⑤ Informed consent and voluntary participation in this study. Disabled rural older adults with severe mental illness or cognitive dysfunction who were unable to cooperate with the survey were excluded. We used the empirical method to calculate the sample size, which involved a total of 19 demographics variables and 7 active aging variables in this study, taking 5–10 times the number of variables, and then considering a 10–20% missed visit rate, the calculated sample size range was 144–325.
Participants reported their gender, age, ethnicity, religion, education level, marital status, number of children, residence status, economic source, monthly income (RMB), medical expenses/month, form of medical insurance, level of disability, length of disability (years), and reason for disability. The researchers also collected the status of rural health activity facilities, the number and length of activity/rehabilitation exercises for the disabled older adults, and the degree of family support for the disabled older adults to participate in social activities.
The Barthel index (BI) scale consists of 10 items: eating, bathing, grooming, dressing, bowel control, urinary control, toileting, bed and wheelchair transfer, level walking, and stair climbing, and is scored out of 100 according to the degree of assistance the patient needs to complete each item (independent, partially assisted, extremely assisted, and totally dependent). Rural older adults with disability are classified into three levels based on BI scores: 61–99 mild disability, 41–60 moderate disability, and 0–40 severe disability. The BI scale is simple to use and has high sensitivity and reliability, with a retest reliability of 0.89 and inter-rater reliability greater than 0.95, and has been widely used to assess patients’ ability to perform activities of daily living (20).
The Active Aging Scale (AAS) was developed by Thai scholar Thanakwang et al. (21) based on the theory of active aging, and research team member Jiange et al. (22) used the Brislin translation model (23) to translate, back-translate, and culturally adapt the scale based on the authorization of the original authors, and revised the item presentation by combining the results of cognitive interviews with rural older adults to form the Chinese version of the Active Aging Scale, which is used to measure the level of active aging of rural older adults with disability. AAS contains 7 dimensions: being self-reliant (7 items), active learning and social integration (8 items), growing spiritual wisdom (5 items), building up financial security (4 items), maintaining healthy lifestyle (5 items), active contribution to society (4 items), and passing on filial piety by example (3 items). 36 items were evaluated on a 4-point Likert scale with a total score range of 36–144, with higher scores indicating higher levels of active aging. The Chinese version of the AAS has good reliability and validity, the scale content validity index (S-CVI/Ave) is 0.981, the content validity index of each item (I-CVI) is 0.83 ~ 1.00, the Cronbach’s alpha coefficient is 0.932, the Cronbach’s alpha coefficient of each dimension is in the range of 0.777–0.913, and the retest reliability is 0.725.
Data collection was conducted by three graduate students (YTT, YWY, HZZ) trained in uniform questionnaire distribution, using on-site distribution of paper versions of the questionnaires. First, the research team mentor (YZ) contacted the township health centers under the three local municipalities to obtain support and informed consent, and then entered each rural area under the leadership of a member of the township health center, accompanied by a village doctor to conduct a questionnaire survey in the households. Then we introduced the purpose and method of the study to the rural older adults with disability and distributed the questionnaires on site. The graduate students uniformly read the questionnaire entries to the older adults with disabilities in a neutral manner and assisted them in checking the boxes, which were collected immediately after completion, and all questionnaires were surveyed anonymously. After 5 months of survey, a total of 308 questionnaires were returned, of which 304 were valid, with a valid questionnaire return rate of 98.7%.
We conducted all data entry and statistical analysis using SPSS 25.0 (SPSS Inc., Chicago, IL, USA), with categorical data described by frequency and percentage and continuous data described by mean and standard deviation (SD). We also reported the minimum, maximum, and 95% confidence intervals for the mean of each dimension score. Additionally, we applied Q-Q plots to test for normality and the results showed that the outcome variable data points were normally distributed around the diagonal. Two independent samples t-test was used to compare the means of two groups, and one-way ANOVA was used to compare the means of three or more independent samples, and Bonferroni method was chosen for chi-square and Tamheni method and reference Welch test correction results were chosen for chi-square. Furthermore, we used multiple linear regression for impact factor analysis with a significance level of 0.05.
The 304 rural older adults with disabilities ranged in age from 60 to 92 (Mean 71.84, SD 8.23) years, BI score from 10 to 95 (Mean 69.72, SD 19.02) and length of disability from 1 to 40 (Mean 6.17, SD 5.40) years, and all of the disabled older adults suffered from different conditions of chronic diseases, in order of prevalence: hypertension (203/66.8%), neurological diseases (181/59.5%), joint pain (125/41.1%), diabetes mellitus (57/18.8%), coronary heart disease (41/13.5%), cataract (23/7.6%), gastritis (20/6.6%), respiratory diseases (12/3.9%), hyperlipidemia (9/3.0%), etc., with specific demographic information shown in Table 1.
The mean score of the active aging level of the rural disabled older adults was 67.38 (SD 13.11) and the mean score of the items was 1.87 (SD 0.36), which was at a low level, and the specific scores of each dimension are shown in Table 2.
There was a statistical difference in the scores of active aging level of rural older adults with disabilities by “education level, residence status, economic source, monthly income (RMB), medical expenses/month, medical insurance form, disability level, length of disability (years), number of activities/rehabilitation exercises, length of activities/rehabilitation exercises/time, and degree of family support for the disabled older adults to participate in social activities”(p < 0.05), as shown in Table 1. The results of the two-by-two comparison between groups showed that the active aging level of the disabled older adults in primary school and below was lower than that of those in junior high school, those living with children were lower than those living with children and spouses and those living alone, those living with spouses were lower than those living alone, and those on government assistance were lower than those on other (working, farming, etc.) economic incomes (p < 0.05). The higher the monthly income and the lower the degree of disability, the better the active aging level of the older adults, those with retired salary were higher than those with other economic sources, those with monthly medical expenses of 100 or more were significantly higher than those with 500 or more, those with length of disability of 1 year or more were significantly higher than those with 5 and 10 years or more, and those with 15 years or more were significantly higher than those with 10 years or more (p < 0.05). The level of active aging was significantly higher for the disabled older adults with activity/rehabilitation exercise 2–3 times per week than for those who never, 1 time per month, and 2–4 times per month, and for those with activity/rehabilitation exercise 1 h or more than for those who never, less than 30 min, and 30 min or more (p < 0.05).
Taking the score of active aging level of rural disabled older adults as the dependent variable, and taking the statistically significant variables in the comparison between groups as the independent variables, multiple linear regression analysis was performed after assigning values to the independent variables, as shown in Table 3. The results showed that the four independent variables “economic source, disability level, activity/rehabilitation exercise hours/time” entered the regression equation (F = 23.596, R = 0.773, R2 = 0.597, DW = 1.815, VIF < 10), see Table 4 for details.
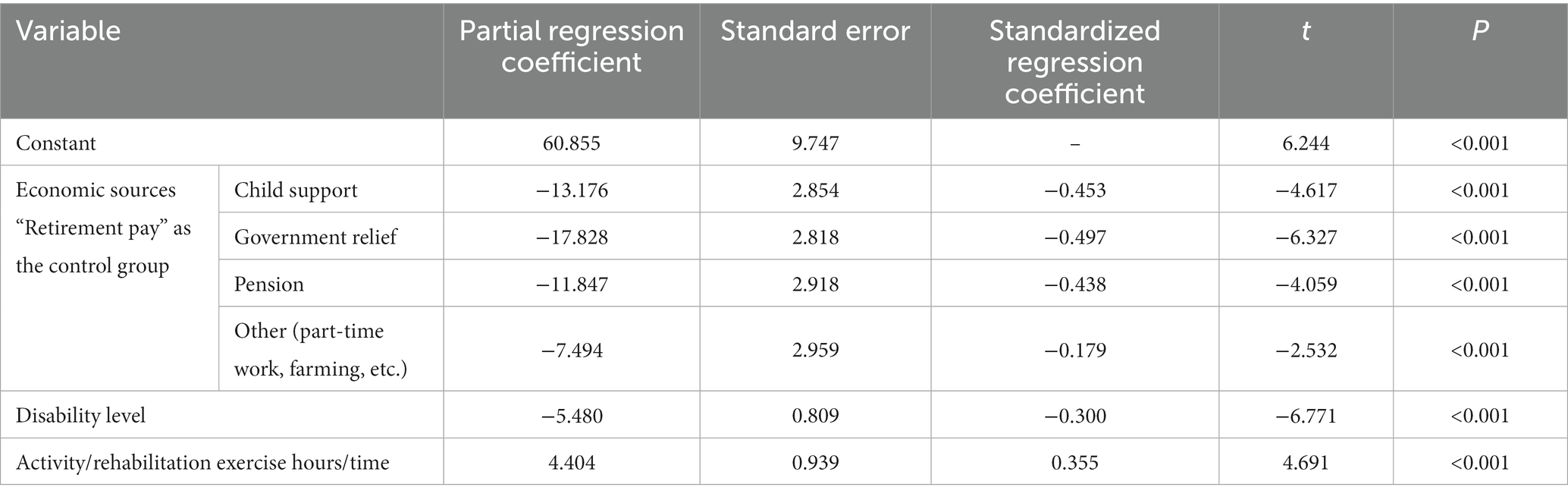
Table 4. Multiple regression analysis results on the level of active aging of rural disabled older adults.
The active aging of rural older adults with disability is at a low level, and the level of economic security and social participation need to be improved. Economic source, disability level, and activity/rehabilitation exercise hours/time are the influencing factors of the level of active aging of rural older adults with disability (p < 0.05).
The total score of 67.38 (SD 13.11) for active aging among rural older adults with disability is lower than the findings of Huiying et al. (24) for rural older adults, which may be related to the fact that the rural older adults with disability surveyed have reduced activities of daily living (ADLs) and all suffer from different conditions and numbers of chronic diseases, mostly hypertension, neurological diseases and joint pain, which to a certain extent reduce the level of active aging among the older adults with disability. The health and community mobility of older adults is somewhat reduced, limiting the level of active aging (25). Xuelian et al. (26) demonstrated that declining ADL reduces active aging in older adults, that depression is a mediating influence, and that comorbid depression and declining ADL have a cumulative effect on active aging. Siltanen et al. (27) found lower levels of active aging in older adults with mobility impairments and that psychological flexibility could mitigate the negative effects of early walking difficulties on active aging. Furthermore, health literacy can help older adults with disability cope with illness and functional limitations and maintain a high level of active aging (28). Diverse applications of information and communication technology (ICT) can reduce isolation and enhance social participation of the older adults with disability. However, in the process of urbanization, the investment and resource distribution of senior care in rural areas are lower than those in cities, and the traditional perception of senior care makes the lack of organizational atmosphere for social participation of older adults in rural areas (29), the lack of active health behavior of disabled older adults and the prominent phenomenon of digital divide (30), which seriously restrict the process of active aging in rural areas. This suggests that we should build a rural and aging-appropriate information technology platform according to the current situation of electronic health literacy of the disabled older adults in rural areas, and integrate virtual reality and augmented reality technologies to conduct health lectures, train memory or perform rehabilitation exercises to increase the health knowledge reserve of the disabled older adults and enhance their dynamic interaction with the surrounding environment (31).
The highest score of 2.29 (SD 0.61) for the being self-reliant dimension of rural older adults with disability is consistent with the findings of Celmira et al. (32) and Hongjie et al. (33) for rural older adults, which may be related to the fact that 72.0% of the surveyed older adults are in a mild state of disability, and the lack of adequate human resources for the disabled due to the shortage of family caregivers in rural areas, coupled with the fact that the disabled older adults do not want to bring financial and caregiving burdens to their families, they still actively try to cope with daily activities independently and insist on doing the work they can. The lowest score of the active contribution to society (Mean 1.37, SD 0.55) dimension indicates that the social participation of the older adults with disability in rural areas is poor. The reason for this may be that the physical functional impairment of the older adults with disability is very likely to make them have low self-esteem and even close themselves off, avoiding or refusing social interactions, decreasing the mobility of their living space, and feeling that they have no experience and skills to pass on to others (34). Sariyamon et al. (35) found that the level of community friendly environment and healthy lifestyles were contributing factors to active aging among older adults. Two community empowerment factors, leisure and welfare facilities for older adults and cooperative alliances, were significantly associated with active aging (36). This suggests that village councils should actively create a caring community environment for the older adults, such as age-friendly renovation of neighborhoods, improving the hygiene of outdoor spaces (37), integrating multiple resources to provide regular home visits, or creating virtual health and age-friendly environments based on ICT to reduce social isolation and promote social participation (38).
The economic source was an influential factor in the level of active aging of rural disabled older adults, consistent with the findings of Huiying et al. (24). The highest level of active aging (p < 0.05) was found among the disabled older adults with retirement pay, who were mostly village workers returning to their hometowns, with higher education and monthly income overall, better health literacy and active health behaviors, and with sufficient financial security to reduce the psychological stress and financial burden of the disabled older adults, supporting their access to better material and health services and promoting a positive mindset toward social participation (39, 40). But only 7.6% of the rural disabled older adults had a retirement salary, and their main sources of financial support were still pension (37.2%), child support (28.9%) and government relief (15.8%), which indicates that the national pension welfare policy has gradually become the main financial security for the rural disabled older adults. Rural older adults with disability who relied on part-time work and farming to generate income accounted for 10.5% of the total, and their active aging scores were higher than those on government relief (p < 0.05). This may be related to the better overall physical and psychological health of the disabled older adults who engage in productive participation (41). However, the average score of building up financial security dimension for rural older adults with disability was only 1.37 (SD 0.57), with 63.5% of the older adults with disability had a monthly income of less than 500 (RMB), but 24.7% of the older adults with disability had monthly medical expenses of more than 500 (RMB), and their financial income microblogging and inability to make ends meet were obvious, and their overall financial security was not sufficient. This can be attributed to the weakened self-working capacity of the disabled older adults, reduced productive participation and economic income generation (14), weakened economic contribution to the family, and increased levels of depressive symptoms, which can easily lead to negative changes in aging attitudes (42). The national government should accelerate the implementation of long-term care insurance and medical assistance insurance for major diseases in rural areas, provide re-employment opportunities for the older adults with the ability to participate in production from the perspective of poverty alleviation, organize rural third-age universities to teach health knowledge (43), and gradually improve and implement the national welfare policy for the older adults.
The degree of disability was a negative predictor of the level of active aging among rural disabled older adults (p < 0.05), consistent with the results of the analysis by Hairu et al. (44). Decreased self-care can be a barrier to daily living and socialization, causing a passive reduction in the level of social participation and even negative emotions in older adults (45). A study by Sini et al. (46) confirmed that decreasing social distance reduces the chances of older adults to lead an active life. In this study, 69.4% of the older adults had been disabled for less than 5 years, 49.3% had become disabled within the last year, and 81.3% were disabled due to illness. The physical status of the older adults with short-term disability is still in the recovery stage, their physiological, role and self-concept adaptation levels are low, their overall health status is poor, and their healthcare needs are diverse (47). However, rural primary health care resources are limited, and home-bound disabled older adults only enjoy basic public health services and lack professional guidance and treatment at the health level, which to a certain extent affects their level of active aging (48). This indicates that the level of comprehensive primary health care in rural areas needs to be improved. Consider using the “Internet+” channel to help push active aging, promote the sinking of quality medical resources through medical associations/medical communities, and integrate multiple resources to provide personalized consultation and health promotion services (49). Reyhane et al. (50) provided a six-week health education component (once a week) on nutrition, physical activity, responsibility, stress management, communication and spirituality to older adults, demonstrating that training based on a health-enhancing approach can be effective in promoting active aging in older adults.
The longer the duration of each activity/rehabilitation exercise, the higher the level of active aging in rural older adults with disability, and 2–3 exercises per week for 1 h and more was a better activity/rehabilitation dose (p < 0.05). Sport/rehabilitation exercise is a health-level social participation that increases contact and communication with the outside world, and prolonged, regular exercise can help older adults with disability to improve their physical fitness, prevent or mitigate the negative effects of disease, and improve cognitive function (51, 52). Moreover, older adults with disability who actively participate in village activities or rehabilitation exercises tend to have better health awareness and active social participation, and higher levels of subjective well-being (53). However, there are still 37.2% of the disabled older adults never participate in activities and rehabilitation exercises, which may be related to the older adults’ fear of falling, and 47.7% of the surveyed disabled older adults’ family members do not support their participation in social activities, coupled with the low level of professional treatment in rural areas and the lack of rehabilitation specialists in rural health centers, resulting in the inability of the disabled older adults to obtain professional rehabilitation guidance and medical assistance. The negative impact on the participation of the older adults in activities (54). It suggests that grassroots governments should strengthen the construction of village activity facilities, actively mobilize the participation of multiple subjects such as village committees, kindergartens and volunteer associations, and organize multimodal social activities through channels such as jitterbug, radio and village stages (55). Silvia et al. (56) used new technology to create “scavenger hunts” to promote physical activity, where participants use a receiver GPS to hide or find real or virtual objects, adding gamification to self-tracking to promote participation and active aging in older adults. Furthermore, the role of “health mentors” can be established in villages to enhance the active aging of rural older adults with disability through the establishment of senior learning communities and intergenerational-based learning.
Rural older adults with disability have a low level of active aging and insufficient financial security and social participation. Rural older adults with moderate to severe disability are a key concern for the government in actively addressing population aging. The national government should actively improve older adult welfare policies to enhance economic security, promote the construction of medical associations/medical communities to improve the quality of rural primary health care, create a virtual senior community-friendly environment based on ICT, and innovate multi-modal physical exercise activities to promote social participation of the disabled older adults. However, this study only selected disabled older adults from rural in Henan Province, and the sample size was limited and not representative of the overall level of the disabled older adults in rural areas. Additionally, the questionnaire was completed with the help of the researcher to understand the subjective perceptions of the respondents, and some items such as “chronic diseases suffered” may be biased due to the respondents’ lack of knowledge about the diseases.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The study was approved by the Life Science Ethics Review Committee of Zhengzhou University (ZZUIRB2021–155) and conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). This survey was voluntary, anonymous and completely confidential. The older adults were informed that submitting the completed questionnaire was considered implied consent.
YTT: investigation, data curation, formal analysis, writing - original draft, and writing – review and editing. YZ: conceptualization, resources, methodology, Writing – review and editing, and funding acquisition. YWY: investigation, formal analysis, visualization. HZZ: investigation and data curation. XZL: data curation and formal analysis. All authors contributed to the article and approved the submitted version.
Funding support was provided by the National Natural Science Foundation of China (71874162).
We thank all participants of the fund application.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1219573/full#supplementary-material
1. World Health Organization . Ageing and health 2022 Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
2. Statistics NBo . The seventh national population census (2021) Available at: http://www.stats.gov.cn/sj/pcsj/rkpc/7rp/indexch.htm
3. Rui, T . Analysis of disability status and change of elderly population in China——based on the data of the sixth and seventh national population census. Health Econom Res. (2023) 40:6–11. doi: 10.14055/j.cnki.33-1056/f.2023.03.005
4. Eum, MJ , and Kim, HS . Relationship between active aging and quality of life in middle-aged and older Koreans: analysis of the 2013–2018 KNHANES. Healthcare. (2021) 9:240. doi: 10.3390/healthcare9020240
5. Sanxiu, W . A preliminary study on the concept of positive aging in China's education and elderly care service model. J ZheJiang Party Sch CPC. (2017) 33:73–80. doi: 10.15944/j.cnki.33-1010/d.2017.01.009
6. López-López, R , and Sánchez, M . The institutional active aging paradigm in Europe (2002–2015). The Gerontologist. (2020) 60:406–15. doi: 10.1093/geront/gnz094
7. Dogra, S , Dunstan, DW , Sugiyama, T , Stathi, A , Gardiner, PA , and Owen, N . Active aging and public health: evidence, implications, and opportunities. Annu Rev Public Health. (2022) 43:439–59. doi: 10.1146/annurev-publhealth-052620-091107
8. China SCo . Notice of the state council on printing and distributing the 13th five-year plan for the development of the national aging career and the construction of the pension system (2017) Available at: http://www.gov.cn/zhengce/content/2017-03/06/content_5173930.htm
9. China CPsGotPsRo . The 14th five-year pan for people's Republic of China's national economic and social development and the outline of the long-term goals in 2035. (2021) Available at: http://www.gov.cn/xinwen/2021-03/13/content_5592681.htm
10. China SCo . Opinions of the CPC central committee and the state council on strengthening the work on aging in the new era (2021) Available at: http://www.gov.cn/zhengce/2021-11/24/content_5653181.htm
11. Ling, L , and Jiahui, L . Exploration of integrating pension service with medical service in China. J China Agric Univ. (2021) 38:91–102. doi: 10.13240/j.cnki.caujsse.2021.04.007
12. Peng, Q . On dilemma and transformation of rural happiness house. J Nanjing Agric Univ. (2022) 22:105–16. doi: 10.19714/j.cnki.1671-7465.2022.0044
13. Teshome, ZA , E AM, Messay, GK . Barriers to active aging in rural Ethiopia: a call for a paradigm shift to a rights-based approach. J Aging Soc Policy (2022) 35:1–23. doi: 10.1080/08959420.2022.2139988
14. Sia, BK , Tey, NP , Goh, KL , and Ng, S-T . Productive engagement of older adults in China: a multilevel analysis. Geriatr Gerontol Int. (2021) 21:1138–46. doi: 10.1111/ggi.14299
15. Derhun, FM , GAS, S , Castro, VC , Llobet, MP , Salci, MA , and Carreira, L . A possibility for active aging: university activities for the elders. Rev Gaucha Enferm. (2022) 43:e20200493. doi: 10.1590/1983-1447.2022.20200493.en
16. Stessa, CT , Xiaoqin, J , Yi, S , and Jheng, ZY . A space-time analysis of rural older People's outdoor mobility and its impact on self-rated health: evidence from a Taiwanese rural village. Int J Environ Res Public Health. (2021) 18:5902. doi: 10.3390/ijerph18115902
17. Hongjie, L , Yan, Z , Ronghua, W , Zijuan, Y , Cancan, D , and Jing, Z . Study on the status quo of active aging in rural disabled elders in Zhengzhou. Med Soc. (2019) 32:56–8. doi: 10.13723/j.yxysh.2019.10.014
18. Costa, A , Henriques, J , Alarcao, V , Henriques, A , Madeira, T , Virgolino, A, et al. Active aging awareness and well-being among older adults in Portugal. Front Public Health. (2023) 11:1149731. doi: 10.3389/fpubh.2023.1149731.
19. Tamayo Giraldo, FJ , Baracaldo Pinzón, LI , Valencia Almonacid, SL , Ortega Lenis, D , and Giraldo Cárdenas, MM . Active aging index in Colombia: analysis based on the national survey of health, well-being, and aging (SABE Colombia 2015) Índice de envelhecimento ativo na Colômbia: uma análise a partir da Pesquisa Nacional de Saúde, Bem-estar e Envelhecimento (SABE da Colômbia 2015). Rev Panam Salud Publica. (2021) 45:e69. doi: 10.26633/RPSP.2021.69
20. Mahoney, FI . Barthel DW Functional evaluation: the barthel index. Md State Med J. (1965) 14:61–2
21. Thanakwang, K , Isaramalai, SA , and Hatthakit, U . Development and psychometric testing of the active aging scale for Thai adults. Clin Interv Aging. (2014) 9:1211–21. doi: 10.2147/CIA.S66069
22. Jiange, Z , Yan, Z , Yan, S , and Erhuan, H . Reliability and validity of the Chinese version of the positive aging scale. Chin J Gerontol. (2017) 37:5424–6. doi: 10.3969/j.issn.1005-9202.2017.21.092
23. Brislin, RW . Back-translation for cross-cultural research. J Cross Cult Psychol. (1970) 1:185–216. doi: 10.1177/135910457000100301
24. Huiying, Z , Yan, Z , Sijin, G , Bebe, Z , Jiange, Z , Zijuan, Y, et al. The level of active aging of the elderly in rural areas of Henan Province and its influencing factors. Chin J Gerontol. (2019) 39:962–5. doi: 10.3969/j.issn.1005-9202.2019.04.065
25. Erja, P , Milla, S , Heidi, L , Kaisa, K , Johanna, E , and Taina, R . Impact of mobility restrictions on active aging; cross-sectional associations and longitudinal changes parallel to COVID-19 restrictions. Arch Gerontol Geriatr. (2022) 98:104522. doi: 10.1016/j.archger.2021.104522
26. Xuelian, F , Yinli, S , Chunyan, Z , Liqiong, L , Yang, G , and Yuanyuan, W . The mediation and interaction of depressive symptoms in activities of daily living and active aging in rural elderly: a cross-sectional survey. Front Public Health. (2022) 10:942311. doi: 10.3389/fpubh.2022.942311
27. Siltanen, S , Tourunen, A , Saajanaho, M , Palmberg, L , Portegijs, E , and Rantanen, T . Psychological resilience and active aging among older people with mobility limitations. Eur J Aging. (2020) 18:65–74. doi: 10.1007/s10433-020-00569-4
28. Eronen, J , Paakkari, L , Portegijs, E , Saajanaho, M , and Rantanen, T . Health literacy supports active aging. Prev Med. (2020) 143:106330. doi: 10.1016/j.ypmed.2020.106330
29. Yue, L , and Jiehua, L . Social participation of the elderly in China: connotation, status quo and challenges. Populat Fam Plann. (2018) 11:14–7.
30. Lingchen, L , Fan, W , Huiying, T , Cuihong, H , and Tingting, X . The digital divide and active aging in China. Int J Environ Res Public Health. (2021) 18:12675. doi: 10.3390/ijerph182312675
31. Álvaro, A , Paula, C , Beatriz, G , Lorena, V , and Carmen, ZM . Efficacy of interventions based on the use of information and communication Technologies for the Promotion of active aging. Int J Environ Res Public Health. (2022) 19:1534. doi: 10.3390/ijerph19031534
32. Lange, C , Heidemann, ITSB , Castro, DSP , Pinto, AH , Peters, CW , and Durand, MK . Promoting the autonomy of rural older adults in active aging. Rev Bras Enferm. (2018) 71:2411–7. doi: 10.1590/0034-7167-2017-0570
33. Hongjie, L , Yan, Z , Zijuan, Y , Ronghua, W , Jing, Z , Cancan, D, et al. Status quo of active aging among rural elderly and its influencing factors. Chin Gen Pract. (2020) 23:1989–95. doi: 10.12114/j.issn.1007-9572.2020.00.120
34. Rantanen, T , Eronen, J , Kauppinen, M , Kokko, K , Sanaslahti, S , Kajan, N, et al. Life-space mobility and active aging as factors underlying quality of life among older people before and during COVID-19 lock-down in Finland – a longitudinal study. J Gerontol A Biol Sci Med Sci. (2021) 76:e60–7. doi: 10.1093/gerona/glaa274
35. Sariyamon, T , Vijj, K , Doungjai, B , Murallitharan, M , Huu, NT , and Aung, HM . Active aging in ASEAN countries: influences from age-friendly environments, lifestyles, and socio-demographic factors. Int J Environ Res Public Health. (2021) 18:8290. doi: 10.3390/ijerph18168290
36. Kim, J , Lee, H , Cho, E , Lee, KH , Park, CG , and Cho, B-H . Multilevel effects of community capacity on active aging in community-dwelling older adults in South Korea. Asian Nurs Res. (2020) 14:36–43. doi: 10.1016/j.anr.2020.01.001
37. Yu, J , Ma, G , and Wang, S . Do age-friendly rural communities affect quality of life? A comparison of perceptions from middle-aged and older adults in China. Int J Environ Res Public Health. (2021) 18:7283. doi: 10.3390/ijerph18147283
38. Bernardo, J , Apóstolo, J , Loureiro, R , Santana, E , Yaylagul, NK , Dantas, C, et al. eHealth platforms to promote autonomous life and active aging: a scoping review. Int J Environ Res Public Health. (2022) 19:15940. doi: 10.3390/ijerph192315940
39. Silva, SNFD , Guimarães, LM , and Azevedo, BMB . Social inequalities in indicators of active aging: a population-based study. Ciencia Saude Coletiva. (2021) 26:5069–80. doi: 10.1590/1413-812320212611.3.24432019
40. Sousa, NFDS , and Barros, MBDA . Level of active aging: influence of environmental, social and health-related factors. Arch Gerontol Geriatr. (2020) 90 (prepublish:104094. doi: 10.1016/j.archger.2020.104094
41. Yanrong, C , Jian, L , and Qinying, C . Employment and mental health of the Chinese elderly: evidence from CHARLS 2018. Int J Environ Res Public Health. (2023) 20:2791. doi: 10.3390/ijerph20042791
42. Zhang, Y , and Xigang, Q . The trajectory of rural elders’ attitudes toward aging: an empirical study based on the framework of active aging. South China Populat. (2020) 35:68–80. doi: 10.3969/j.issn.1004-1613.2020.04.006
43. Maria, DF , SGAd, S , Karina, RL , Aparecida, SM , Puig, LM , and Lígia, C . Contributions of university activities to active aging: grounded theory. Rev Esc Enferm USP. (2022) 56:e20210237. doi: 10.1590/1980-220X-REEUSP-2021-0237
44. Hairu, Z , Qian, L , Zihan, Y , and Mei, J . Positive aging level and influencing factors of elderly in the community. Chin J Gerontol. (2021) 41:5397–401. doi: 10.3969/j.issn.1005-9202.2021.23.056
45. Lan, M , Lifang, G , Yue, L , Yingfei, L , Le, L , and Qingfeng, T . Intermediary role of social participation on relationship between daily life ability and mental health status in elderly people. Chin J Public Health. (2021) 37:358–60. doi: 10.11847/zgggws1126239
46. Sini, S , Erja, P , Milla, S , Katja, P , Katja, K , and Taina, R . Self-rated resilience and mobility limitations as predictors of change in active aging during COVID-19 restrictions in Finland: a longitudinal study. Eur J Ageing. (2021) 19:475–84. doi: 10.1007/s10433-021-00634-6
47. Mengke, G , Yan, Z , Yutong, T , Yue, G , Xiaohua, L , and Yixin, L . A qualitative exploration of Chinese rural older adults' adaption experience to disability in Henan Province. BMC Public Health. (2023) 23:512. doi: 10.1186/s12889-023-15425-0
48. Yu, J , Huang, W , and Kahana, E . Investigating factors of active aging among Chinese older adults: a machine learning approach. Gerontologist. (2022) 62:332–41. doi: 10.1093/geront/gnab058
49. Taina, R , Mary, H , Katja, P , Sini, S , Katja, K , Laura, K, et al. The effect of individualized, theory-based counselling intervention on active aging and quality of life among older people (the AGNES intervention study). Aging Clin Exp Res. (2020) 32:2081–90. doi: 10.1007/s40520-020-01535-x
50. Reyhane, DS , Hamidreza, Z , Masoud, Z , and Hamidreza, BV . Effect of health promotion interventions in active aging in the elderly: a randomized controlled trial. Int J Comm Based Nurs Midwifery. (2023) 11:34–43. doi: 10.30476/IJCBNM.2022.96246.2117
51. Qianqian, C , and Yong, H . A study on the effect of community old-age service on the mental health improvement of the elderly. Northwest Population Journal. (2020) 41:79–91. doi: 10.15884/j.cnki.issn.1007-0672.2020.03.008
52. Finlay, J , Esposito, M , Li, M , Colabianchi, N , Zhou, H , Judd, S, et al. Neighborhood active aging infrastructure and cognitive function: a mixed-methods study of older Americans. Prev Med. (2021) 150:106669. doi: 10.1016/j.ypmed.2021.106669
53. Yamashita, T , Bardo, AR , and Liu, D . Experienced subjective well-being during physically active and passive leisure time activities among adults aged 65 years and older. Gerontologist. (2019) 59:718–26. doi: 10.1093/geront/gny106
54. Mengyi, W , Huamin, P , and Huijie, Z . A study on the relationship between dual welfare access and social participation of older people – an empirical analysis based on China's moderately inclusive social welfare database. J Soc Sci. (2018) 9:101–9. doi: 10.13644/j.cnki.cn31-1112.2018.09.011
55. Paulo, C , José, M , Ana, C , Luís, L , Catarina, P , and Jorge, B . Creative dance associated with traditional Portuguese singing as a strategy for active aging: a comparative cross-sectional study. BMC Public Health. (2022) 21:2334. doi: 10.1186/s12889-022-12978-4
Keywords: aging, older adults, disability, active aging, health aging, quality of life
Citation: Tian Y, Zhang Y, Yan Y, Zhang H and Li X (2023) The active aging level of the rural older adults with disability in China: a cross-sectional study. Front. Public Health. 11:1219573. doi: 10.3389/fpubh.2023.1219573
Received: 09 May 2023; Accepted: 07 July 2023;
Published: 01 August 2023.
Edited by:
Petra Heidler, IMC University of Applied Sciences Krems, AustriaReviewed by:
Adriano Pasqualotti, The University of Passo Fundo, BrazilCopyright © 2023 Tian, Zhang, Yan, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Zhang, emhhbmd5YW4yMDEwQHp6dS5lZHUuY24=
†ORCID: Yutong Tian https://orcid.org/0000-0001-6301-5048
Yan Zhang https://orcid.org/0000-0001-7941-9952
Yuwen Yan https://orcid.org/0009-0004-1659-0372
Huizhong Zhang https://orcid.org/0009-0000-2893-898X
Xizheng Li https://orcid.org/0009-0002-2844-3789
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.