
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 13 July 2023
Sec. Occupational Health and Safety
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1218191
This article is part of the Research Topic Environmental and occupational exposure and chronic diseases View all 25 articles
 Xiaodan Xu1,2†
Xiaodan Xu1,2† Liangliang Zhao1,2†
Liangliang Zhao1,2† Yong Zhu3
Yong Zhu3 Bing Du4
Bing Du4 Baoli Zhu1,2
Baoli Zhu1,2 Hengdong Zhang1,2
Hengdong Zhang1,2 Lei Han1,2
Lei Han1,2 Xin Liu1,2*
Xin Liu1,2*Introduction: Respirators chosen based on their assigned protection factor (APF) enable wearers to effectively reduce particulate matter concentrations to safe levels when used correctly. As a crucial factor in achieving the intended APF, the fit test has become a necessary procedure in respiratory disease protection.
Methods: This study involved 225 participants who underwent a fit test using two reusable types of half masks and two types of full masks. Condensation nuclei counting (CNC) and controlled negative pressure (CNP) were performed.
Results: The results revealed that the passing rate of full masks was higher compared to half masks. Specifically, the passing rate for the half masks and the full masks were 84.7 and 91.6%, respectively. Gender exerted a statistically significant effect on the passing rate. Nevertheless, age, educational background, and training exhibited relatively negligible effects. Certain movements, such as facing forward, were identified as key actions with strong correlation. Additionally, talking was considered a key action with a high failure rate due to instantaneous leakages. Most participants failed at the initial step of CNP, but nearly all of them passed the fit test using CNC.
Discussion: Therefore, putting on full masks, especially for women, provides optimal protection during work. Furthermore, attention should be given to the displacement and deformation of the respirator during the key actions. When it comes to fit test methods, CNC was found to be more practical and comprehensive compared to CNP. Moreover, additional physiological characteristics, such as double chins, could be explored as potential influential factors.
When considering various occupational hazards, inhalation poses a significant risk, with substances such as particulate matter, toxic gases, and vapors being major causes of human injury. These hazards can lead to conditions such as pneumoconiosis, occupational poisoning, and other occupational diseases (1–4). For instance, the COVID-19 outbreak was primarily caused by the virus being carried on particulate matter and transmitted to people through contact (5–9). As of the end of 2021, occupational pneumoconiosis cases continued to rank first among occupational diseases (10). Despite the presence of engineering protection facilities, the concentration of particulate matter in many workplaces cannot be reduced to safe levels on certain occasions. Hence, respirators are indispensable in preventing harm to workers by respirable gases or particulate matter. A respirator worn correctly can trap most particles, thus delivering purified air to the wearer (11–14).
There are various types of respiratory protective equipment (RPE). The assigned protection factor (APF) serves as the basis for determining the level of protection provided by masks, as stipulated in the recommended China national standard GB/T 18664-2002, “Selection, Use, and Maintenance of Respiratory Protective Equipment” (15). The APF refers to “a respiratory protective device or class of respirators that, when used correctly, is expected to reduce the concentration of air pollutants to an acceptable level” (16–18). The Occupational Safety and Health Administration of the United States (OSHA) standards explicitly state that “APFs are effective only if the employer implements an ongoing respiratory protection program that includes training, fit test, maintenance, and usage requirements” (19). Therefore, the respirator fit test and proper wearing of RPE are prerequisites for achieving the intended APF value.
The fit test for respirators can be performed using various qualitative and quantitative methods (20). Quantitative testing methods are often applied to various devices. The respirator fit test performed by PortaCount of TSI and MT of SIBATA yielded similar results by quantitative methods (21). The relative impact of fit test exercises and mask donning on respirator fit was measured using controlled negative pressure and an ambient aerosol fit test system. Donning was found to have a greater effect on respirator fit compared to fit test exercises (22). Recent studies have focused on respirator fit tests to evaluate the effects of wearing a breathing apparatus, indicating a new trend (23–25). Further research is needed on the fit test procedures and application details of various respirators. Thus, this article aimed to intensively study the influencing factors of the respirator effectiveness and key actions in the fit test through the test data of two technological paths.
A total of 225 chemical plant operators and maintenance and laboratory personnel were selected as subjects. Each subject could perform multiple tests. The gender, age, educational background, and training of the subjects were collected. Persons being fit tested were to be medically cleared to wear the respirator prior to fit testing, while subjects with respiratory diseases were to be excluded. Persons to be fit tested were to understand the test procedure and could complete the test process independently.
The fit test operators were to be familiar with respirator fit testing, inspection, cleaning, maintenance, and storage in the respiratory protection program.
In this study, four types of RPE currently produced by MSA Safety Incorporated were selected: two half masks (a 410 air-purifying respirator and 420 air-purifying respirator) and two full masks [a 3S air-purifying respirator and Ultra Elite self-contained breathing apparatus (SCBA)]. The 3S air-purifying respirator includes the 3S (black rubber frame) and 3S economy (white frame) types. An air-purifying respirator is designed with a filter, cartridge, or canister, which efficiently eliminates specific air contaminants by filtering air through a purification element. A self-contained breathing apparatus is an atmosphere-supplying respirator for which the breathing air source is designed to be carried by the user.
The QuantiFit tester by OHD (Hoover, Alabama, United States) and PortaCount Pro8038 fitting tester by TSI (Shoreview, Minnesota, United States) were used to perform the test. The testers had undergone annual factory calibration authorized service facility.
The QuantiFit functions by creating and maintaining a negative pressure in the respirator. Once the adapter valve is closed, sealing the respirator, the QuantiFit removes air from the respirator until the challenge pressure is reached. During the fit test, the QuantiFit measures exactly how much air the instrument removed from the respirator after reaching the challenge pressure. Air inhalation or exhalation, even slightly, creates dramatic changes within the respirator. Actions such as swallowing or opening the mouth can adversely affect the pressure sensor and cause tests to fail. Daily verification is required for each day of testing. This verification measures the leak rate of the leak orifice on the tube assembly at various pressure levels and confirms that the diaphragm pump and other processes are working correctly. The QuantiFit with respirators is displayed in Figure 1.
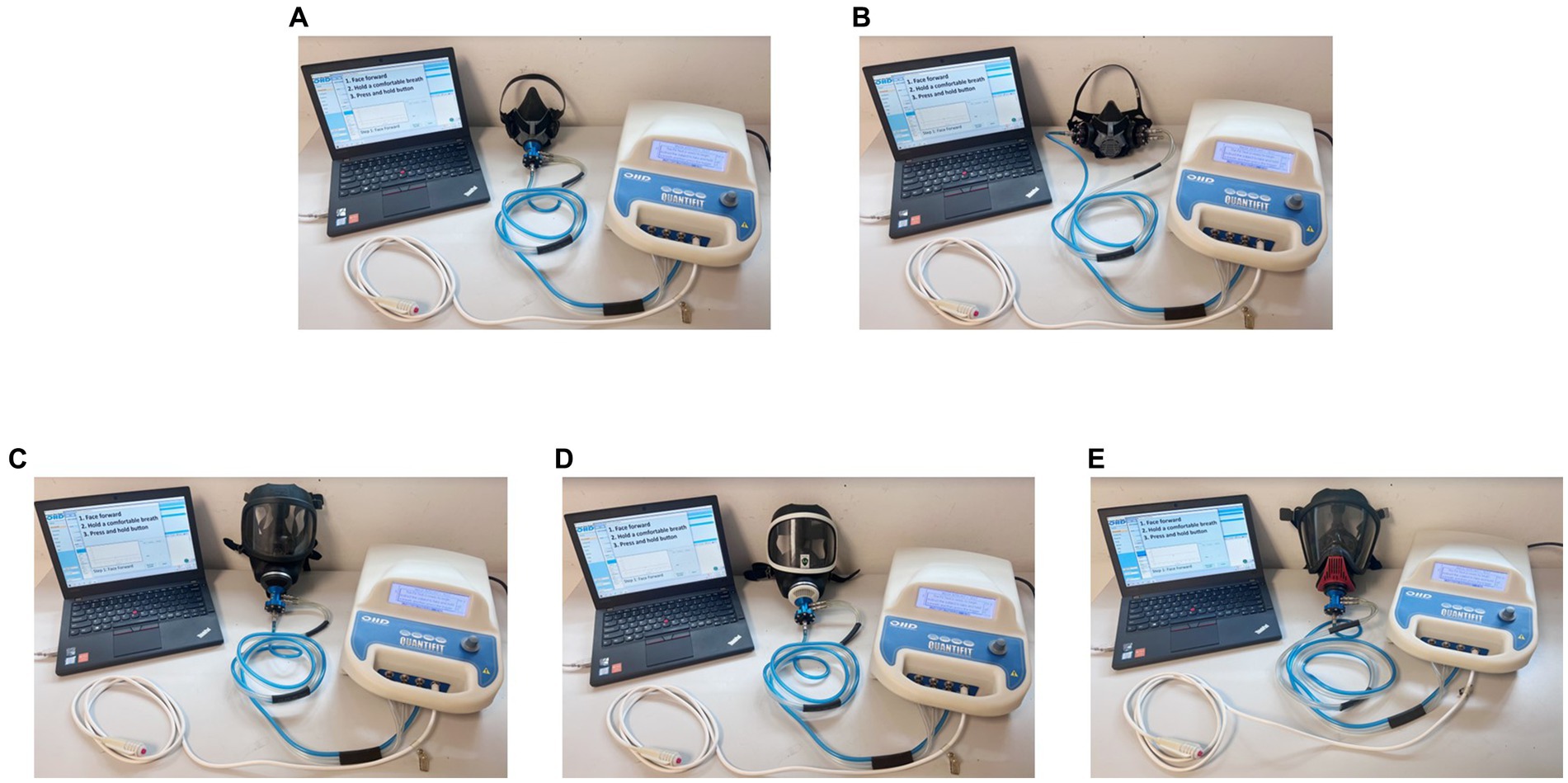
Figure 1. Respirators connected with the QuantiFit. (A) 410 air-purifying respirator; (B) 420 air-purifying respirator; (C) 3S air-purifying respirator—black rubber frame; (D) 3S air-purifying respirator—white frame; (E) Ultra Elite self-contained breathing apparatus.
The PortaCount Pro8038 fitting tester is designed to operate using the microscopic particles in the ambient air. It can measure particle concentrations and fit factors when generated aerosols (such as corn oil, salt, or ambient air) are used; however, these aerosols may cause the PortaCount Pro8038 to need more frequent cleaning and calibration checks. Instruments with adapters can perform daily verification, which determines if the tester is working correctly and if the concentration of particles in the ambient air is sufficient to conduct fit testing. The effective operation of the instrument is limited by aerosol concentrations. Completed daily checks provide confidence that the test results are reliable. Moreover, it is very important to instruct individuals not to smoke for at least 30 min prior to fit testing. The PortaCount Pro8038 with respirators is displayed in Figure 2.
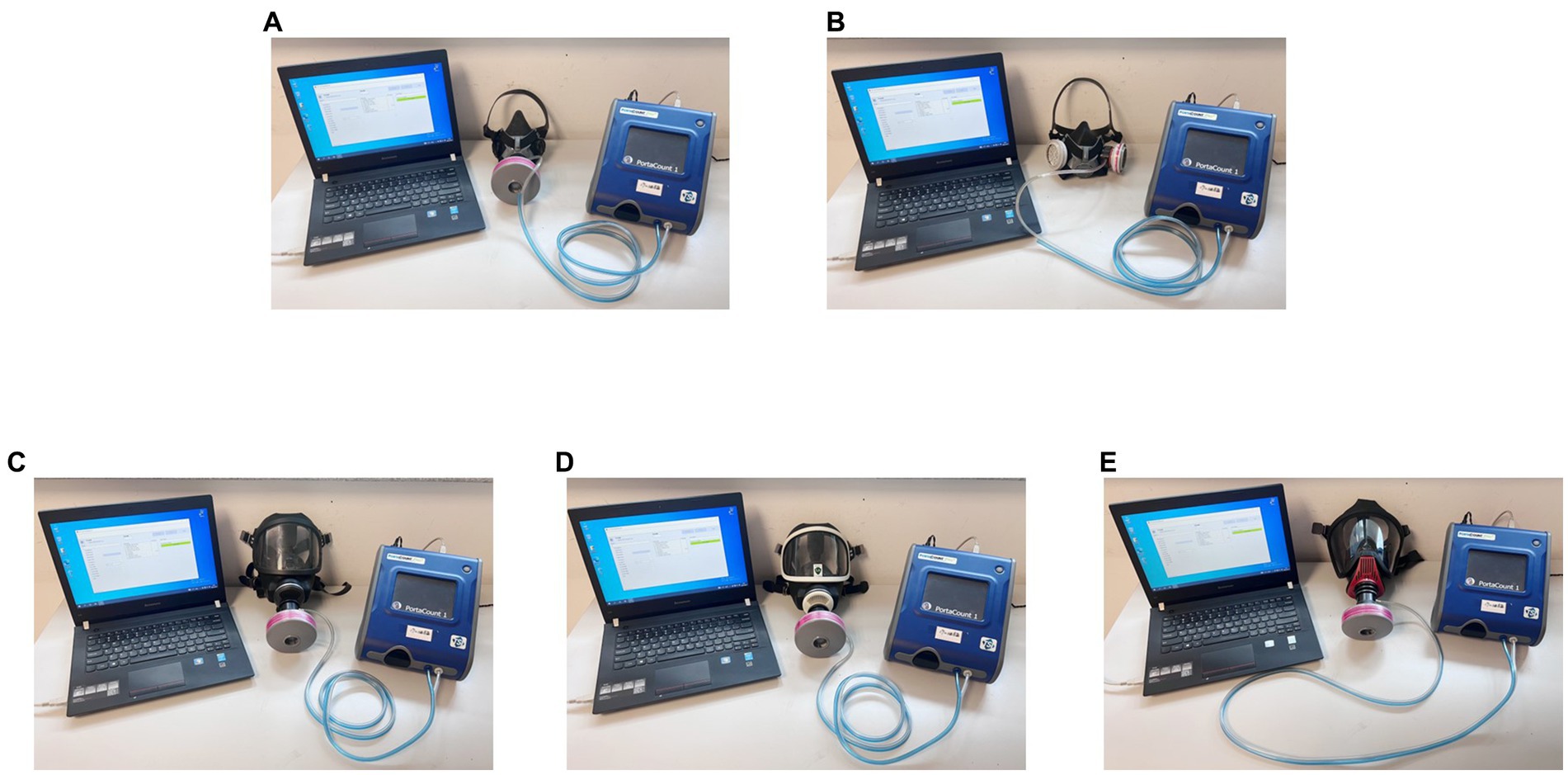
Figure 2. Respirators connected with the PortaCount Pro8038. (A) 410 air-purifying respirator; (B) 420 air-purifying respirator; (C) 3S air-purifying respirator—black rubber frame; (D) 3S air-purifying respirator—white frame; (E) Ultra Elite self-contained breathing apparatus.
OSHA-accepted quantitative fit tests were used in this study: controlled negative pressure (CNP) and condensation nuclei counting (CNC).
CNP enables the direct measurement of air flow into the mask under negative pressure conditions (20), which is applicable only to re-usable respirators, such as the four types of masks used in this study. The fit test procedure took about 2–3 min and consisted of several parts. First, the mask was connected to the QuantiFit tester and was put on correctly. Second, the test subjects performed a specific movement and then held their breath for 10 s. The fit factor (FF) was given by the tester after breath holding (Equation 1). Third, five movements were prescribed: facing forward, bending over (stayed), shaking the head, wearing of the mask again, and wearing of the mask again. Fourth, the fit test was ended, and the mask was taken off. The instrument finally presented the overall FF (Equation 2).
CNC measures the aerosol concentration inside and outside the breathing zone of the respirator using a probe (21, 24, 26, 27). The aerosols measured inside the respirator are assumed to be the result of face seal leakage. Ambient air aerosol was used in this study. The CNC test period is longer than that of CNP by about 8–9 min. First, the mask was connected to the PortaCount Pro8038 fitting tester and put on correctly. Second, the test subjects performed a specified movement repeatedly for 60 s. The instrument displayed the FF at the end of 60 s (Equation 3). Third, eight movements were prescribed: normal breathing, deep breathing, moving the head side to side, moving the head up and down, talking, grimacing, bending over (repetitive), and normal breathing. In particular, the grimace lasted for 15 s with no FF. Fourth, the fit test was ended, and the mask was taken off. Here, to assess whether the mask would re-close to the face after leakage, we deliberately carried out grimacing to create leaks. However, this action would not be considered in the calculation of the overall FF. After the remaining seven actions had been completed, the instrument showed the overall FF (Equation 2).
where N is the number of movements and FFn is the fit factor for the nth movement.
OSHA requires a fit factor of at least 100 for half masks and 500 for full masks when using an OSHA-accepted quantitative fit test method. If the overall FF of a half mask is ≥100 (required FF, RFF) and the overall FF of a full mask is ≥500 (RFF), the respirator fit test is considered successful. Consequently, the mask is deemed suitable for the wearer; otherwise, it is deemed unsuitable.
The original data from the test software were exported and organized using Excel. Statistical analysis was performed using SPSS 27.0.1. Chi-square test was used to analyze the influencing factors of the fit test, while multiple linear regression was employed to analyze the FFs.
The test categories are displayed in Table 1. The CNP and CNC test results for the different respirators were analyzed. The passing rates for the half masks and full masks were 84.7 and 91.6%, respectively. The overall passing rate followed the order: half masks < full masks. The difference was statistically significant (p < 0.05).
Full masks provide better coverage by eliminating exposed areas such as the cheekbones and bridge of the nose. Therefore, full masks can meet the fitting requirements and achieve the desired APF more easily. A worker wearing a half mask will be extremely vulnerable to exposure to toxic environments when the mask is put on without a fit test.
Those who failed in the first test were asked to participate in the second test after receiving intervention. The main interventions included re-explaining the test method, a mask-putting-on demonstration, and changing the mask size if necessary. In the secondary test, eight subjects passed after the intervention. Among them, three passed the 420 air-purifying respirator test, two passed the 3S air-purifying respirator test, and three passed the Ultra Elite SCBA test. They increased the passing rate for the half masks and the full masks to 86.0 and 93.0%, respectively. The overall passing rate slightly increased after the intervention.
In this article, the factors of gender (man and woman), age (≤45 and >45 years old), education background (below high school; high school or above), and training (yes or no) were investigated for their potential impact on the respirator fit test (Table 2). We only considered the assigned gender at birth in this part. A preliminary chi-square test was conducted to determine whether it had an effect on the test results (Table 3) (28). A chi-square test showed that gender had a p value < 0.05.
The results revealed a significant influence of gender on the passing rate of the respirator fit test. In this study, we found that the passing rate of the men participants was 88.1%, while the passing rate of the women was 75.6%. As presented in Table 4, women generally exhibited a lower passing rate in the respirator fit test compared to men. Some participants tested different types of masks, so the total number of tests recorded exceeded the total number of participants. Moreover, women tended to choose smaller respirators in the testing process. After trying out different sizes of masks, a majority of women preferred the S-size. In terms of the low passing rate for women, a plausible reason may be the combined effect of having a thin face and sharp chin, which finally led to face seal leakage in the respirator fit test. Furthermore, in the CNP test, the subjects must hold their breath to maintain the mask’s negative pressure. The women tended to hold their breath for a shorter period of time, which was also a reason for the low passing rate.
Meanwhile, age, education background, and training demonstrated negligible influence on the passing rate. Consequently, efforts to improve the protective effectiveness of respirators should primarily focus on physiological characteristics, such as gender, facial characteristics, and so on.
From the introduction of the test methods, it is evident that the method consists of several test actions. Each test action is a step in the fit test, and it can be considered that a CNP test contains 5 steps, while a CNC test contains 8 steps.
There are two kinds of key actions. One key action is strongly correlated with the final test result, and it can be found by the correlation between the steps’ FFs and overall FF. In this article, we define it as “key actions with strong correlation.” An effective and accepted statistical method for analyzing correlations is multiple linear regression (29). In consequence, multiple linear regressions for the CNP and CNC tests were presented to explore the key actions with strong correlation. We treated the steps’ FFs as the independent variables and the overall FF as the dependent variables in multiple linear regression, with consideration of the 3S air-purifying respirator as an example. In multiple linear regression, the smaller the p value, the stronger the correlation between the variables. In this article, a p value < 0.001 was considered as the criterion for determining the key actions.
Prior to the analysis, necessary regression checks were performed on the CNP data. The rules were as follows: Step 1: facing forward; Step 2: bending over (stayed); Step 3: shaking the head; Step 4: wearing of the mask again; and Step 5: wearing of the mask again.
The collinearity diagnostic criteria show that the greater the tolerance of the independent variables, the weaker the multicollinearity between the variables. A tolerance greater than 0.1 is acceptable, indicating that there is no multicollinearity problem between the independent variables (30, 31). As shown in Table 5, the FF tolerance values in collinearity statistics were all greater than 0.1, indicating no significant multicollinearity issues with FFs. The Durbin–Watson test yielded a value of 1.888, indicating that the data residuals can be considered independent.
The overall FF increased and decreased according to the steps’ FFs in Figure 3, suggesting a simple linear relationship between the steps’ FFs and overall FF. The histogram of residuals, as shown in Figure 4, demonstrated a normal distribution with an average value of 0 and a standard deviation of 1, indicating a good fit to the normal distribution. As shown in Figure 5, the regression-standardized residuals were distributed around 0, with symmetrical data points above and below. Consequently, the data residuals met the assumptions of the homogeneity of variance. Based on the above checks, the steps’ FFs and overall FF can be analyzed via multiple linear regression.
Similar checks confirmed that CNC also satisfied the conditions for multiple linear regression, enabling the identification of key actions in CNC. The following rules were applied: Step 1: normal breathing; Step 2: deep breathing; Step 3: moving the head side to side; Step 4: moving the head up and down; Step 5: talking; Step 6: bending over (repetitive); and Step 7: normal breathing. Since the grimace step does not have an F value, this step was not included in multiple linear regression, and seven steps were listed in the CNC test.
Multiple linear regression analyses were carried out for the CNP and CNC data. The results of the multiple linear regression for CNP revealed a significant regression equation, with an F value of 123.349 and p < 0.05. The steps’ FFs can account for 80.7% of the variation in the overall FF (Table 6). The p values of the steps indicated that all of them had a positive and strong effect on the overall FF. Thus, facing forward, bending over (stayed), shaking the head, and wearing of the mask again were all key actions with strong correlation.
The results of the multiple linear regression for CNC indicated a significant regression equation, with an F value of 9.724 and p < 0.05. The steps’ FFs can explain 61.6% of the variation in the overall FF (Table 7). Step 4 FF (p < 0.001) had a positive and strong impact on the overall FF. During the 60 s up-and-down head movement, the neck surface experienced frequent squeezing and stretching, increasing the likelihood of gas leakage at the lower end of the mask. Based on this finding, only moving the head up and down was considered a key action with strong correlation in CNC.
Through the multiple linear regression analysis of the CNP and CNC test data, we can conclude that the key actions with strong correlation are facing forward, bending over (stayed), shaking the head, wearing of the mask again, and moving the head up and down. When applying a respirator, these key actions need to be given high attention to ensure that the wearer’s breathing environment is sustainable and safe.
Another key action has a high failure rate, and we define it as “key actions with high failure rate” in this article. There will be several instantaneous leakages during key action with a high failure rate, which is usually the main reason for the high failure rate of the step. Instantaneous leakage refers to temporary air leakage that occurs despite resealing, leading to a poor sealing situation. In cases where a fit test ultimately passed despite failing one or two steps, key actions with high failure rate were observed. As shown in Table 8, about one-third of the failure steps can be attributed to “Talking.” Talking produces multiple instantaneous leakages, which can result in step failure, and is not conducive to the effect of respiratory protection. This finding aligns with the conclusion drawn by Sietsema M et al., who reported that talking can disrupt the fit of a respirator due to facial movements that may dislodge the facepiece (26). The high step failure rate attributed to instantaneous leakage highlights the significance of considering talking as a key action in the fit test.
Among the participants who failed the test in CNP, more than half of them discontinued the test at the first step, indicating their unsuitability for this particular method (Table 9). This outcome highlights the limitations of the CNP test despite its speed and accuracy. The test requirements, such as breath holding, pose challenges that some individuals are unable to meet. Interestingly, in the experiments conducted, the participants who dropped out of the CNP test were often able to pass the CNC test easily. However, those who failed the CNC test often failed the CNP test as well. In addition, the CNC test includes any tight-fitting respirator and a wide variety of actions, which is more realistic. This suggests that people generally exhibit higher adaptability to the CNC method in actual situations.
This study focused on the respirator fit test with four kinds of masks using QuantiFit and PortaCount Pro8038. The experiments involved 225 participants and presented the CNP and CNC test systems. The results indicated that putting on full masks had a higher passing rate compared to half masks. The passing rates for the 410 air-purifying respirator, 420 air-purifying respirator, 3S air-purifying respirator, and Ultra Elite SCBA were found to be 81.6, 86.5, 90.0, and 95.2%, respectively. Specifically, the passing rates for the half masks and the full masks were 84.7 and 91.6%, respectively. Interventions were shown to slightly improve the passing rate. Through chi-square tests, it was determined that gender significantly influenced the passing rate. The low passing rate among women was attributed to their facial features and shorter breath-holding time. Key actions were identified using correlation and step failure rate analysis. Based on the correlation of the steps’ FFs and overall FF, the key actions with strong correlation were identified as facing forward, bending over (stayed), shaking the head, wearing the mask again, and moving the head up and down. Additionally, talking was considered a key action with a high failure rate due to the occurrence of several instantaneous leakages. In terms of fit test methods, CNC was found to be more practical and comprehensive compared to CNP and should be the first choice for occupational safety and health practitioners.
Moreover, the presence of facial hair, such as beards and certain hairstyles, can affect the effectiveness of face masks (32, 33). Any external objects between the face and the respirator will interfere with the tightness, and it is recommended to remove foreign objects and keep the face clean and smooth before putting on a mask or performing a fit test. When exploring meaningful influencing factors, it is important to consider facial features such as the double chin. Furthermore, attention should be given to the displacement and deformation of the respirator during the key actions. Improper mask wearing can result in wearers being exposed to excessive or toxic particulate matter. Therefore, regular fit tests and the use of various masks, especially smaller sizes for women, are recommended to ensure optimal protection.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethical Committee of Jiangsu Provincial Center for Disease Control and Prevention (JSJK2022-B002-01). The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This work was funded by the Jiangsu Provincial Social Development Program of Key R&D Project (BE2022803) and Jiangsu Provincial Key Medical Discipline (ZDXK202249).
The authors would like to acknowledge the contributions of BASF-YPC Company Limited for their contributions to this research.
BD was employed by BASF-YPC Company Limited.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Singh, D, Marrocco, A, Wohlleben, W, Park, H-R, Diwadkar, AR, Himes, BE, et al. Release of particulate matter from nano-enabled building materials (NEBMs) across their lifecycle: potential occupational health and safety implications. J Hazard Mater. (2022) 422:126771. doi: 10.1016/j.jhazmat.2021.126771
2. Peng, S, Xiaoyue, X, Shuhua, X, Hongmei, J, Jiamei, Y, Zhushan, F, et al. Trends in global, regional and national incidence of pneumoconiosis caused by different aetiologies: an analysis from the global burden of disease study 2017. Occup Environ Med. (2020) 77:407–14. doi: 10.1136/oemed-2019-106321
3. Li, J, Yin, P, Wang, H, Wang, L, You, J, Liu, J, et al. The burden of pneumoconiosis in China: an analysis from the global burden of disease study 2019. BMC Public Health. (2022) 22:1114. doi: 10.1186/s12889-022-13541-x
4. Barnes, H, and Glaspole, I. Occupational interstitial lung diseases. Immunol Allergy Clin N Am. (2023) 43:323–39. doi: 10.1016/j.iac.2023.01.006
5. Suman, R, Javaid, M, Choudhary, SK, Haleem, A, Singh, RP, Nandan, D, et al. Impact of COVID-19 pandemic on particulate matter (PM) concentration and harmful gaseous components on Indian metros. Sustain Oper Comput. (2021) 2:1–11. doi: 10.1016/j.susoc.2021.02.001
6. Santurtún, A, Colom, ML, Fdez-Arroyabe, P, Real, Á, Fernández-Olmo, I, and Zarrabeitia, MT. Exposure to particulate matter: direct and indirect role in the COVID-19 pandemic. Environ Res. (2022) 206:112261. doi: 10.1016/j.envres.2021.112261
7. Prinz, AL, and Richter, DJ. Long-term exposure to fine particulate matter air pollution: an ecological study of its effect on COVID-19 cases and fatality in Germany. Environ Res. (2022) 204:111948. doi: 10.1016/j.envres.2021.111948
8. Becchetti, L, Beccari, G, Conzo, G, Conzo, P, De Santis, D, and Salustri, F. Particulate matter and COVID-19 excess deaths: decomposing long-term exposure and short-term effects. Ecol Econ. (2022) 194:107340. doi: 10.1016/j.ecolecon.2022.107340
9. Baron, YM. Could changes in the airborne pollutant particulate matter acting as a viral vector have exerted selective pressure to cause COVID-19 evolution? Med Hypotheses. (2021) 146:110401. doi: 10.1016/j.mehy.2020.110401
10. China DoPDaITNHCotPsRo. 2021 Statistical Communique on the Development of China’s Health Services. Chin. J. Viral Dis. (2022) 12:10.
11. Wang, L, Bian, Y, Lim, CK, Niu, Z, Lee, PKH, Chen, C, et al. Tribo-charge enhanced hybrid air filter masks for efficient particulate matter capture with greatly extended service life. Nano Energy. (2021) 85:106015. doi: 10.1016/j.nanoen.2021.106015
12. Liu, H, Cao, C, Huang, J, Chen, Z, Chen, G, and Lai, Y. Progress on particulate matter filtration technology: basic concepts, advanced materials, and performances. Nanoscale. (2020) 12:437–53. doi: 10.1039/C9NR08851B
13. Leung, N, Chu, D, Shiu, E, Chan, KH, Mcdevitt, JJ, Hau, B, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. (2020) 26:676–80. doi: 10.1038/s41591-020-0843-2
14. Feng, S, Shen, C, Xia, N, Song, W, Fan, M, and Cowling, BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. (2020) 8:434–6. doi: 10.1016/S2213-2600(20)30134-X
15. Park, SH, Hwang, SY, Lee, G, Park, JE, Kim, T, Shin, TG, et al. Are loose-fitting powered air-purifying respirators safe during chest compression? A simulation study. Am J Emerg Med. (2021) 44:235–40. doi: 10.1016/j.ajem.2020.03.054
16. Zhuang, E, Chen, HH, Kolesnik, O, and Hines, SE. Tolerability, user acceptance and preference for a novel reusable respirator among health care workers. Am J Infect Control. (2022) 51:821–6. doi: 10.1016/j.ajic.2022.09.006
17. Howard, RA, Lathrop, GW, and Powell, N. Sterile field contamination from powered air-purifying respirators (PAPRs) versus contamination from surgical masks. Am J Infect Control. (2020) 48:153–6. doi: 10.1016/j.ajic.2019.08.009
18. Cass, HG, Hanlon, GC, McKenzie, DP, Harley, NS, Kelly, DN, and Barrett, JA. The adequacy of user seal checking for N95 respirators compared to formal fit testing: a multicentred observational study. Aust Crit Care. (2022). doi: 10.1016/j.aucc.2022.08.012
19. OSHA. OSHA revised respiratory protection standards. Washington DC, United States: Department of Health (2003).
21. Han, D-H, Seo, H, Kang, B-k, Jang, H, Kim, H, and Shim, S. Comparisons of fit factors between two quantitative fit testers (PortaCount vs. MT). Safety and health at. Work. (2022) 13:500–6. doi: 10.1016/j.shaw.2022.10.001
22. Crutchfield, CD, Fairbank, EO, and Greenstein, SL. Effect of test exercises and mask donning on measured respirator fit. Appl Occup Environ Hyg. (1999) 14:827–37. doi: 10.1080/104732299302062
23. MacIntyre, CR, Wang, Q, Cauchemez, S, Seale, H, Dwyer, DE, Yang, P, et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers [article]. Influenza Other Respir Viruses. (2011) 5:170–9. doi: 10.1111/j.1750-2659.2011.00198.x
24. Knobloch, JK, Franke, G, Knobloch, MJ, Knobling, B, and Kampf, G. Overview of tight fit and infection prevention benefits of respirators (filtering face pieces). J Hosp Infect. (2023) 134:89–96. doi: 10.1016/j.jhin.2023.01.009
25. He, W, Yue, Y, Guo, Y, Zhao, Y-B, Liu, J, and Wang, J. A comparison study of the filtration behavior of air filtering materials of masks against inert and biological particles. Sep Purif Technol. (2023) 313:123472. doi: 10.1016/j.seppur.2023.123472
26. Sietsema, M, and Brosseau, LM. Comparison of two quantitative fit-test methods using N95 filtering facepiece respirators. J Occup Env Hyg. (2016) 13:621–7. doi: 10.1080/15459624.2016.1159690
27. Ahmed, A, Zhong, Z, Suprono, M, Savignano, R, Riter, H, Oyoyo, U, et al. Enhancement of peripheral seal of medical face masks using a 3-dimensional–printed custom frame. J Am Dent Assoc. (2021) 152:542–50. doi: 10.1016/j.adaj.2021.03.011
28. Williams, LL, and Quave, K. Chapter 10 - tests of proportions: Chi-Square, likelihood ratio, Fisher's exact test In: Quantitative anthropology : Pennsylvania, United States: Academic Press (2019). 123–41.
29. Cabral, DF, Bigliassi, M, Cattaneo, G, Rundek, T, Pascual-Leone, A, Cahalin, LP, et al. Exploring the interplay between mechanisms of neuroplasticity and cardiovascular health in aging adults: a multiple linear regression analysis study. Auton Neurosci. (2022) 242:103023. doi: 10.1016/j.autneu.2022.103023
30. Park, J. Tolerance intervals from ridge regression in the presence of multicollinearity and high dimension. Stat Prob Lett. (2017) 121:128–35. doi: 10.1016/j.spl.2016.10.016
32. Prince, SE, Chen, H, Tong, H, Berntsen, J, Masood, S, Zeman, KL, et al. Assessing the effect of beard hair lengths on face masks used as personal protective equipment during the COVID-19 pandemic [article]. J Expo Sci Environ Epidemiol. (2021) 31:953–60. doi: 10.1038/s41370-021-00337-1
Keywords: respiratory protective device, mask, quantitative fit test, fit factor, controlled negative pressure, condensation nuclei counting
Citation: Xu X, Zhao L, Zhu Y, Du B, Zhu B, Zhang H, Han L and Liu X (2023) Conducting quantitative mask fit tests: application details and affecting factors. Front. Public Health. 11:1218191. doi: 10.3389/fpubh.2023.1218191
Received: 06 May 2023; Accepted: 29 June 2023;
Published: 13 July 2023.
Edited by:
Sara Rojas, University of Granada, SpainReviewed by:
Victor C. W. Hoe, University of Malaya, MalaysiaCopyright © 2023 Xu, Zhao, Zhu, Du, Zhu, Zhang, Han and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Liu, bGl1eEBqc2NkYy5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.