- 1Department of Public Health, Debre Berhan University, Debre Berhan, Ethiopia
- 2Department of Nursing, Mizan Tepi University, Mizan Teferi, Ethiopia
- 3School of Nursing and Midwifery, Debre Berhan University, Debre Berhan, Ethiopia
- 4Department of Midwifery, Mizan Tepi University, Mizan Teferi, Ethiopia
- 5School of Medicine, Debre Berhan University, Debre Berhan, Ethiopia
- 6School of Public Health, The University of Queensland, Herston, QLD, Australia
Background: Although the impact of illness perception on medication adherence is well-established, its specific influence on medication adherence in Ethiopia remains unclear. Consequently, the objective of this study was to examine the association between illness perception and medication adherence among patients with diabetes mellitus in the North Shoa Zone.
Methods: An institution-based cross-sectional study was conducted from 24 May to 25 June 2022 in the North Shoa zone. The study included a random sample of 552 individuals with diabetes from four public hospitals. Data was collected and entered into Epi Data V.3.1, and analysis was performed using SPSS version 22. Descriptive statistics were used to summarize continuous variables as means with standard deviations, while categorical variables were presented as percentages. The study variables were analyzed using binary logistic regression models to assess the associations between illness perception and medication adherence. In the bivariable analysis, variables with p-values less than 0.20 were entered into a multivariable logistic regression model. Associations with a p-value ≤0.05 and an odds ratio with a 95% confidence interval were considered statistically significant.
Results: The study results revealed that medication adherence was 64.4% (95% CI: 60.1, 67.9), while illness perception was 54.7% (95% CI, 41.2, 49.4). There was a significant and strong association between illness perception and medication adherence (p < 0.0001). In the adjusted model, the illness perception components of consequence showed a significant association with medication adherence (AOR = 3.10, 95% CI: 2.11, 4.55). Similarly, personal control (AOR = 1.77, 95% CI: 1.20, 2.61) and emotional representation of diabetes (AOR = 2.26, 95% CI: 1.54, 3.32) were also significantly associated with medication adherence in patients with diabetes.
Conclusion: The findings of this study indicate a positive association between higher illness perception and increased medication adherence and practice. Therefore, when engaging in discussions about diabetic self-management, diabetes educators should employ psychoeducational approaches that take into account the illness perceptions of patients.
Background
Diabetes is a significant global health issue, with a considerable impact on the adult population. In 2021, it was estimated that approximately 537 million adults worldwide were affected by diabetes. Projections indicate a steady rise, with an expected increase to 643 million by 2030 and 783 million by 2045. The prevalence of diabetes in Africa is also a concern, with an estimated 24 million adults affected in 2021. Alarmingly, this number is projected to rise to 55 million by 2045, highlighting the urgent need for effective prevention and management strategies in the region (1). Diabetes is increasingly becoming a significant public health challenge in Ethiopia, with a national prevalence rate of 2.8% in 2022 (2) and gradually increasing from 1% in 2000 (3) to 3.3% in 2020, according to the Report of the International Diabetes Federation (1).
The long-term social, health, and economic impacts of diabetes on individuals and countries are substantial. Consequently, treatment adherence serves as a crucial indicator of healthcare quality in the effective management of diabetes (4). Adherence to treatment refers to the voluntary cooperation of patients in following the prescribed dosage, timing, and frequency of medication as directed by healthcare professionals (5, 6).
Medication adherence plays an important role in glycemic control and prevention of complications (7) and the effectiveness of treatment also depends on adherence to recommended medication (8). Low adherence to medications in people with diabetes is significantly associated with poor glycemic control (9). Although a wide range of antidiabetic drugs is available, many patients with diabetes still fail to control blood glucose levels associated with diabetes (10). Patients’ adherence to prescribed medications is influenced by personal beliefs about chronic diseases (11). Adherence to antidiabetic medications improves with better illness perception (12). Illness perception (IP) is characterized as the patient’s implicit and common sense beliefs regarding their illness (10).
Illness perception plays a key role in the study of patients’ perceptions of their illness and significantly impacts medication adherence (13). Individuals with diabetes are more motivated to adhere to their treatment regimen when they hold the belief that their medications are effective and that their disease is well-managed (14, 15). IP plays an important role in managing adherence and is related to adherence in diabetes (16). Research findings indicate that having knowledge about one’s illness positively influences self-care behaviors, which in turn help individuals with diabetes to mitigate the consequences of the disease (14).
Hence, it is crucial to manage illness perception among individuals with diabetes as it has the potential to enhance treatment adherence. Research evidence strongly indicates a significant relationship between illness perception and treatment adherence in diabetes, resulting in improved management and control of the disease (13, 17). Patient perception is a psychological factor in diabetes that directly or indirectly influences treatment adherence, emphasizing the need for additional research to investigate the role of psychological factors in diabetes management (18). Patient perception, as a psychological aspect, should be integrated into diabetes care and effectively communicated across all levels of the healthcare system.
To the best of our knowledge, there are no studies that have investigated the relationship between illness perception and treatment adherence in Ethiopia. The hypothesis put forth is that a positive recognition of diabetes as an illness may have a favorable influence on medication adherence. Therefore, the objective of this study was to examine the association between disease perception and treatment adherence in the Northern Shoa.
Methods
Study design and setting
The facility-based cross-sectional study design was performed at public hospitals in the North Shoa Zone from 24 May to 25 June 2022. North Shoa is one of the thirteenth zones of the Amhara region located in northern Ethiopia. There are 24 districts, 3 municipalities, and 13 hospitals. All public hospitals have diabetes care and follow-up services.
Subjects and sample selection
The sample size was determined using the formula for the proportion of the single population considering the proportion of medication adherence of 68% in Ethiopia (19) with a precision level of 5 and 15% for non-response and a design effect of 1.5, resulting in 552 subjects. Diabetic subjects aged ≥18 years who had been followed for more than three months were included in the study. The mean of Fasting Blood Sugar (FBS) measurements in three consecutive months was used for FBS analysis. Patients who were medically judged unable to participate in the study (e.g., acute illness, mental illness, and dementia) and patients with severe visual impairment were excluded from the study. Study participants were recruited from four hospitals, selected according to a proportional allocation among hospitals. Study participants were selected using a systematic randomization procedure. Because each patient had at least one appointment within one month, we waited up to one month for a selected study participant.
Data measurement and tool
Medication adherence was evaluated through a set of four questions, including: Have you ever forgotten to take a prescribed medication? Do you sometimes discontinue taking your medication? Are there instances when you are not diligent about taking your medicine? And if you experience worsening symptoms after taking your medication, do you cease taking it?
The scoring method for this questionnaire focuses solely on item four. A response of “Yes” is assigned a score of 1, while a response of “No” is given a score of 0. The total score is obtained by summing the scores of all items in the questionnaire. The total score ranges from zero to four, where a score above 1 suggests low compliance, while a score of 0 indicates high compliance. The questionnaire underwent face and content validity assessment by experts, and its reliability was measured using the Cronbach’s alpha method, resulting in values ranging from 0.75 to 0.81.
The evaluation of individuals’ perception of their illness utilized the modified Illness Perception Questionnaire (IPQ-R). This questionnaire consists of seven subscales and a 38-item version (20). The instrument employed in this study consists of 38 items that assess seven domains of illness perception (20, 21). Each domain of illness perception was treated as an independent variable and examined to assess its influence on medication adherence. Participants providing their perception of illness using a 5-point Likert scale for each question within each domain. The responses were summed to calculate an average score for each domain. Furthermore, individual scores were computed for each component, and an overall score was computed to the overall level of illness perception. A higher score indicates stronger feelings associated with each aspect of illness perception (20, 22). The Cronbach’s alpha coefficients for the subscales ranged from 0.70 to 0.89.
The data collection process was carried out by four trained data collectors, all of whom held bachelor’s degrees. These collectors conducted interviews to gather the required data. Prior to data collection, both the data collectors and their supervisors underwent comprehensive training on the research objectives, questionnaire content, and the importance of maintaining confidentiality and privacy throughout the data collection process. To ensure data quality, all authors and supervisors performed daily checks to verify completeness, accuracy, and consistency of the collected data. The principal investigator closely monitored the data collection activities on a daily basis, ensuring questionnaire completeness and providing further clarification when needed. Detailed review of patients’ medical records was conducted, capturing essential information such as fasting blood sugar (FBS) levels, diabetic complications, comorbidities, and the medications being taken.
Data management and analysis
The collected data was entered into Epi Data version 4.6 and then exported to SPSS version 25 for analysis. Descriptive analysis was utilized to present the frequency distribution of each variable in the study. Continuous variables were reported as mean ± standard deviation, while categorical variables were presented as percentages.
To examine the relationship between illness perception and medication adherence, binary logistic regression analysis was conducted. Multicollinearity was assessed using the variance inflation factor, with a threshold value of less than 10 considered acceptable. The goodness of fit of the model was evaluated using the Homer-Lemeshow test.
Variables that demonstrated a p-value of less than 0.20 in the bivariate analysis were included in the subsequent model analysis. The significance of the associations was determined using the p-value and 95% confidence interval (CI) for the odds ratios (OR).
Results
Socio-demographic and clinical characteristics of respondents
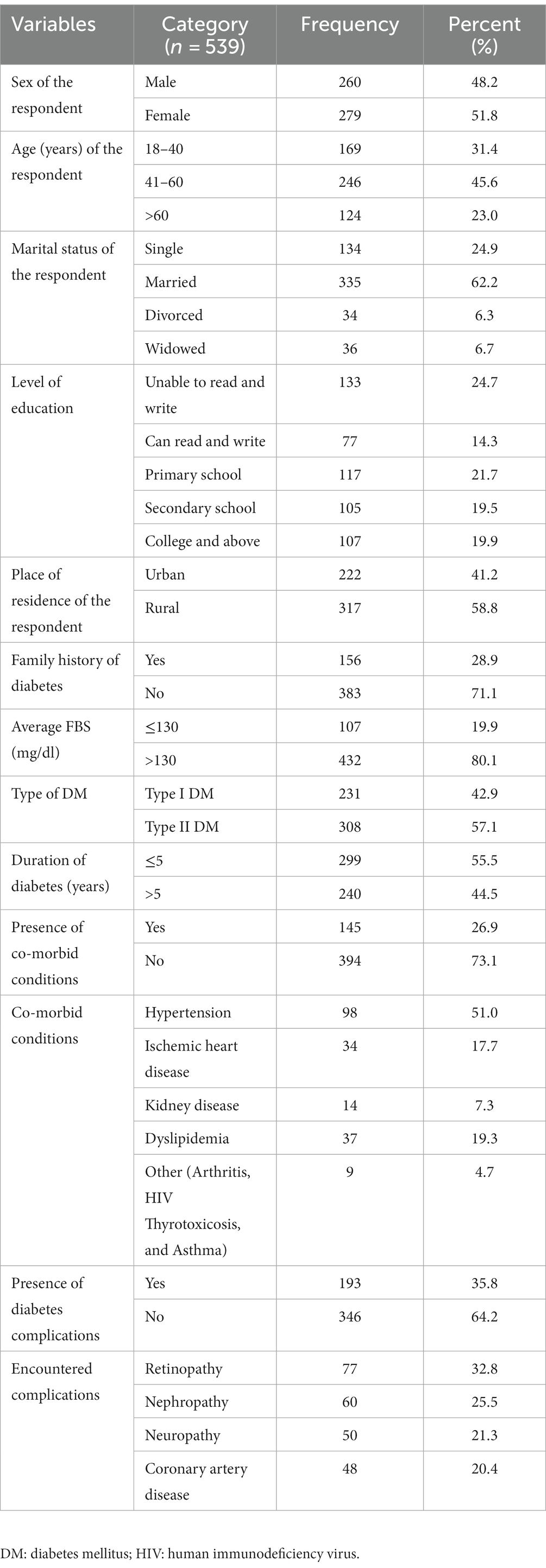
The study included 539 individuals diagnosed with diabetes, resulting in a high response rate of 98%. The gender distribution was nearly equal among the participants. A majority of respondents (52.1%) fell within the age range of 41 to 60 years, and a significant proportion (45.6%) were married. Moreover, a majority of the participants had received formal education.
Among all the study participants, a substantial percentage (80.1%) had fasting blood sugar (FBS) levels that were uncontrolled, surpassing 130 mg/dL. Regarding diabetic complications, 35.8% of the participants had developed chronic complications, with retinopathy (32.8%) being the most prevalent. Additionally, 145 individuals (26.9%) had comorbidities, with hypertension (51.0%) being the most frequently reported comorbidity (Table 1).
Participant’s perception of their diabetes illness
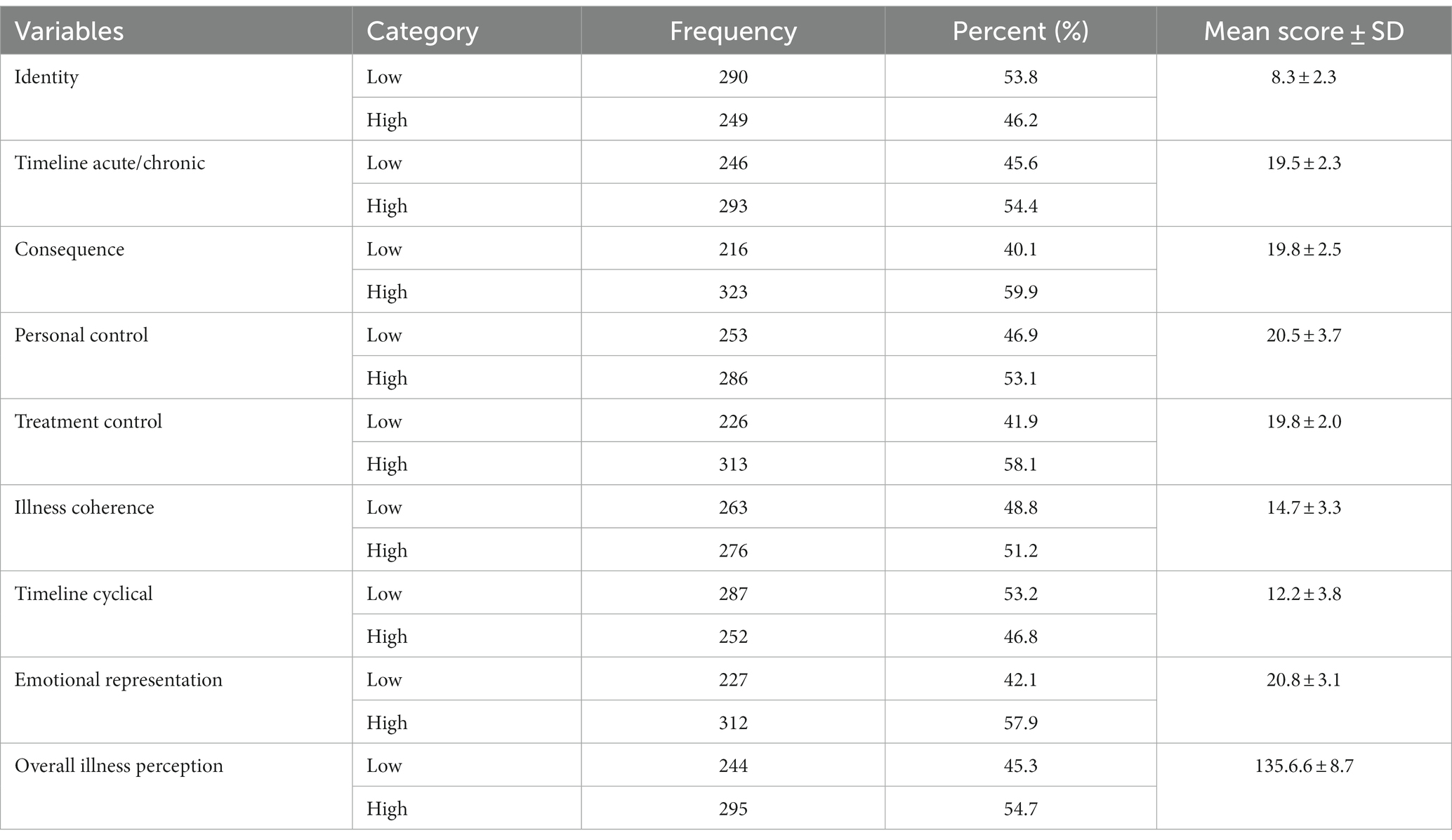
In the study, the overall illness perception was found to be 54.7% (95%CI: 41.2–49.4%). The mean score for illness perception was 135.6 ± 8.7 SD. Among the various dimensions of illness perception, illness perception/personal control ability had the highest mean score of 20.5 ± 3.7 SD, followed by emotional illness response with a mean score of 20.8 ± 3.1 SD. On the other hand, illness identity had the lowest mean score of 8.3 ± 2.3 SD.
Table 2 presents the frequency distribution of the reported illness perceptions. The most commonly reported illness perceptions were perception of consequences (59.9%), treatment control (58.1%), and emotional expression (57.9%) (Table 2).
Relationship between illness perception and medication adherence
In the study, the overall adherence to antidiabetic medication was determined to be 64.4%, with a mean of 0.67 ± 1.02 SD. Chi-square test analysis revealed a significant association between illness perception and adherence to antidiabetic medication (χ2 = 4.01; p < 0.05). Several domains of illness perception were found to be significantly associated with medication adherence. These domains included perception of acute/chronic timeline (p = 0.025), perception of diabetic consequences (p < 0.0001), perception of personal control (p = 0.001), and perception of emotional representation (p < 0.0001) (Table 3).
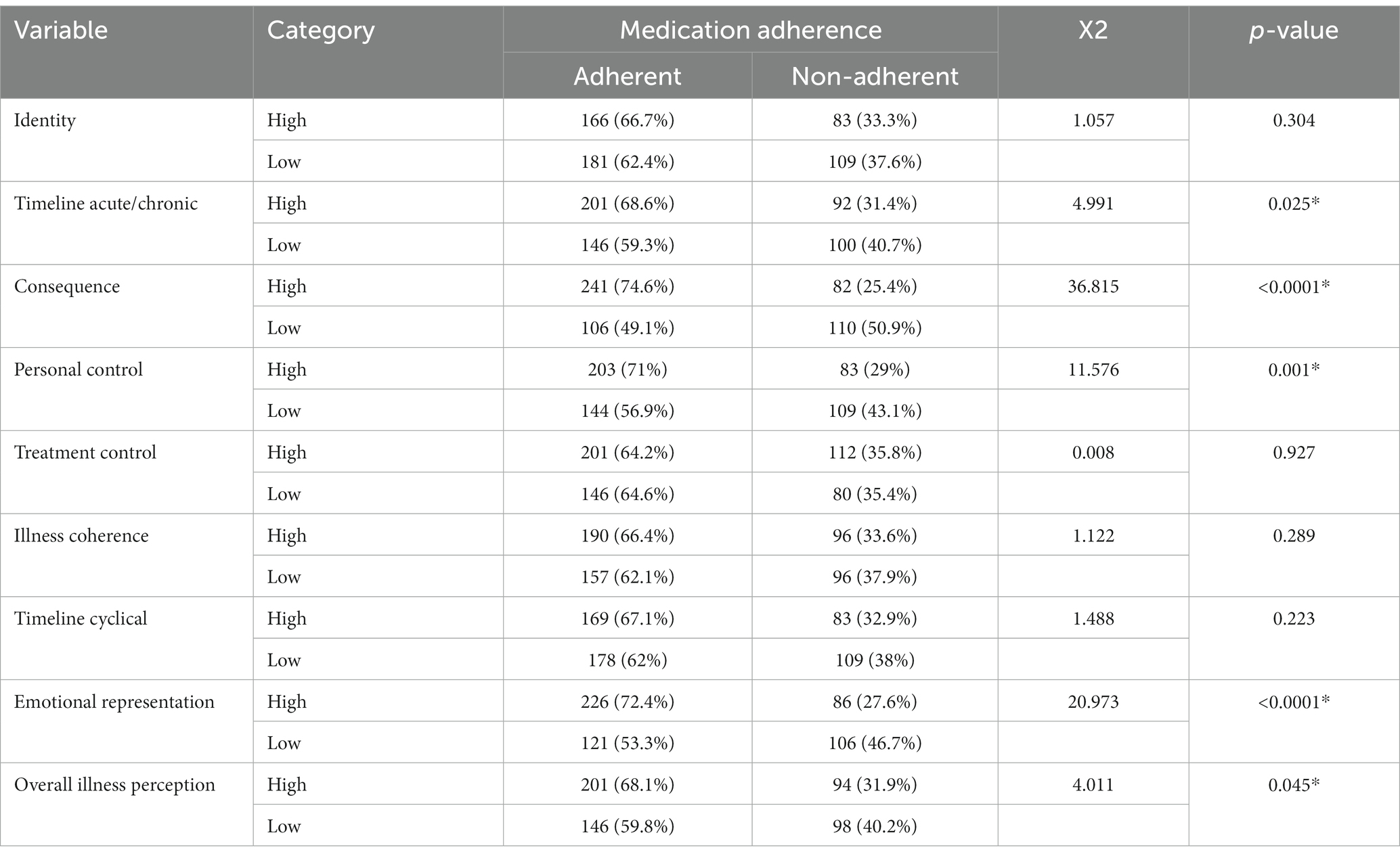
Table 3. Relationship of illness perception and medication adherence of diabetic patients in North Shoa 2022 (n = 539).
Association between only illness perception domain and medication adherence
In the adjusted model, patients who had higher perceptions of diabetic consequences were found to be three times more likely to adhere to treatment compared to other patients (adjusted odds ratio [AOR] = 3.10, 95% CI: 2.11, 4.55). Similarly, individuals with a sense of personal control over their diabetes (AOR = 1.77, 95% CI: 1.20, 2.61) and those with an emotional perception (AOR = 2.26, 95% CI: 1.54, 3.32) were more inclined to adhere to treatment (Table 4).
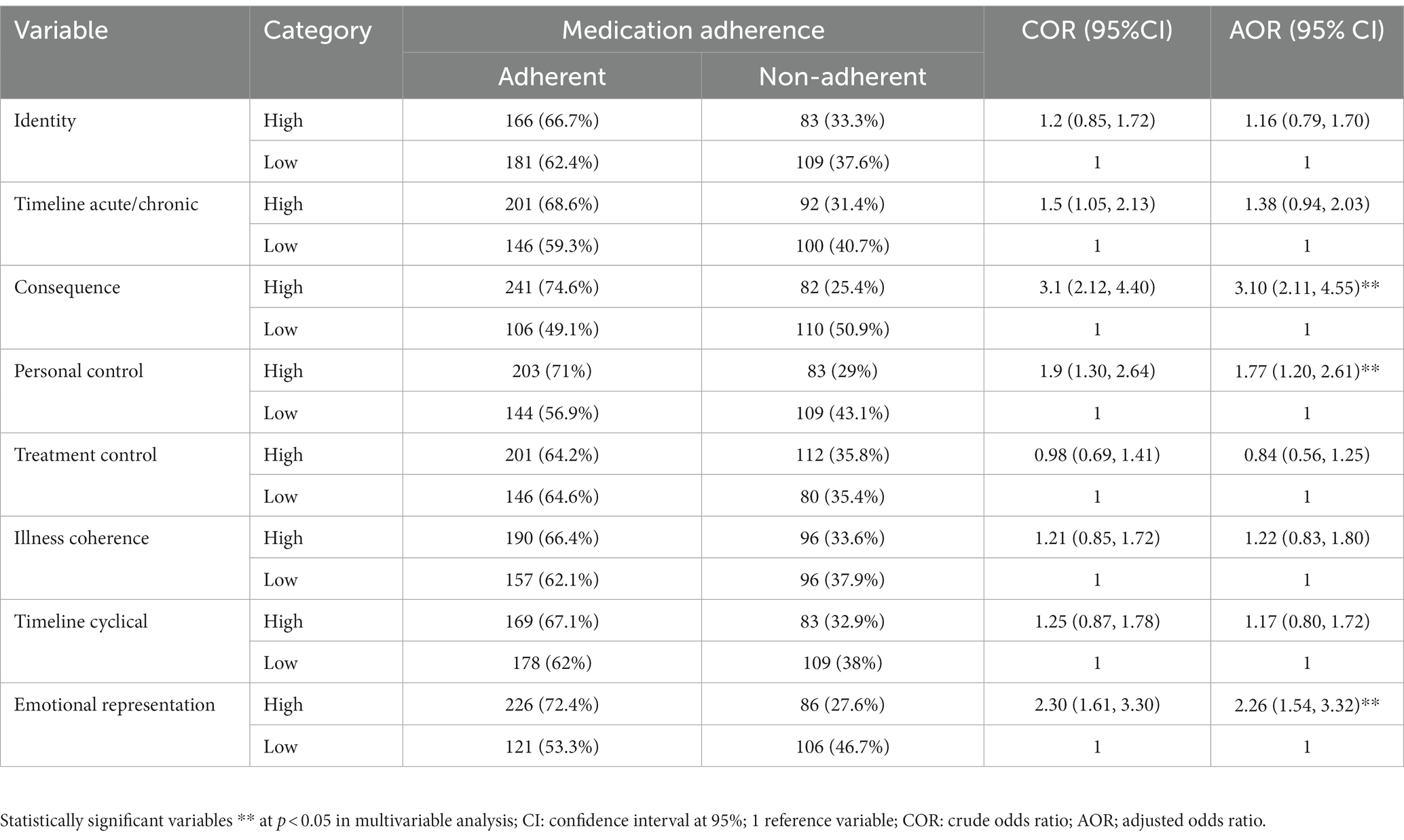
Table 4. Binary logistic regression analysis of the relationship of illness perception and medication adherence in North Shoa, 2022 (n = 539).
Association of medication adherence with illness perception and background information
The final model included sociodemographic, patient-related, care-related, clinical, and medication-related variables. Variables that demonstrated a p-value of less than 0.20 in the bivariate analysis were considered for inclusion. After adjusting for potential confounding factors, it was observed that patients with a higher perception of diabetic consequences (AOR = 2.5, 95% CI: 1.64, 3.72), patients with good personal control over their diabetes (AOR = 1.78, 95% CI: 1.19, 2.68), and those with an emotional perception (AOR = 2.39, 95% CI: 1.59, 3.58) were more likely to adhere to their treatment (Table 5).
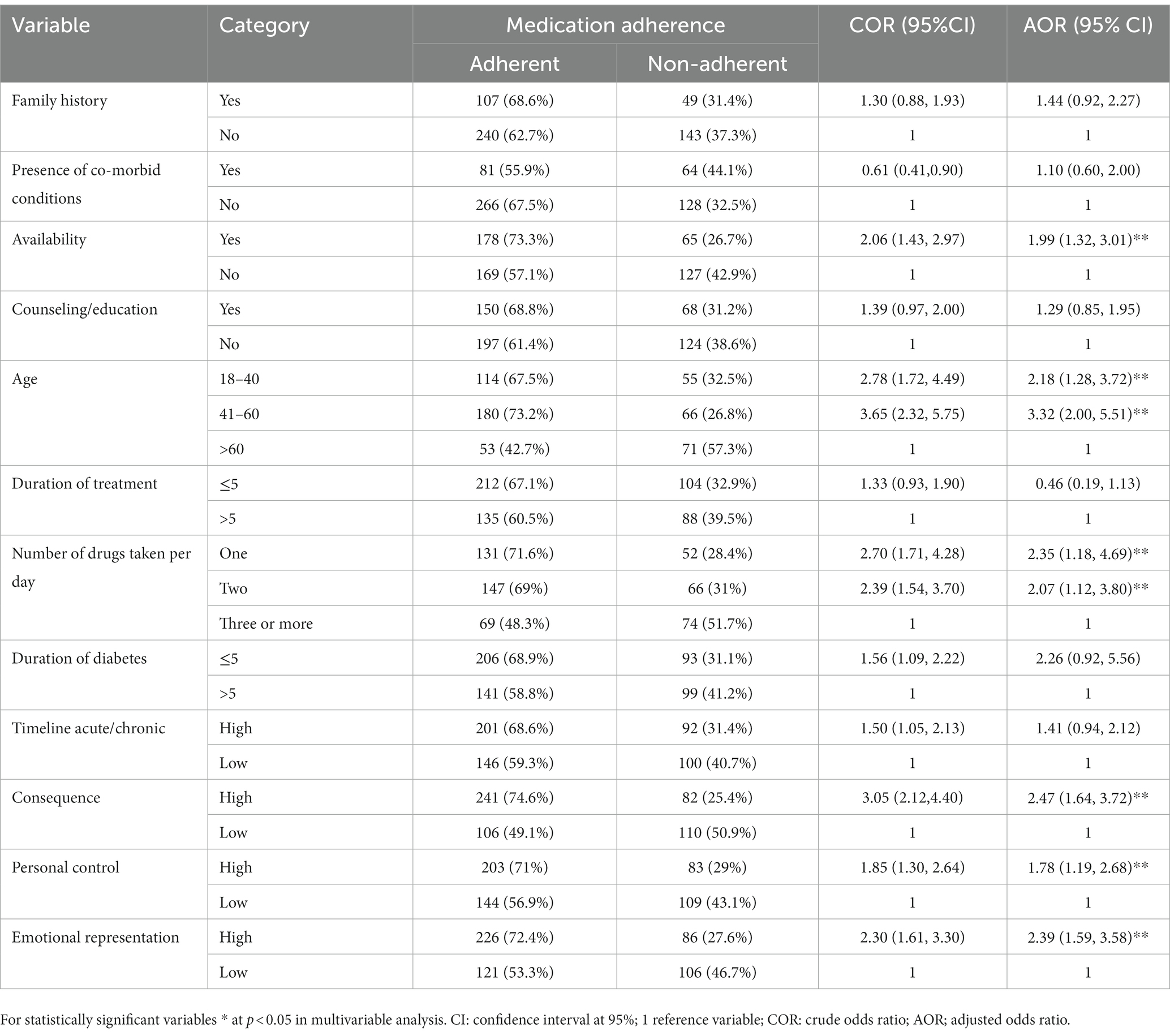
Table 5. Logistic regression analysis of medication adherence with illness perception and background information among the participants in North Shoa Zone, 2022.
Discussion
The current study aimed to examine the relationship between illness perception and medication adherence in the North Shao Zone. The findings revealed a significant association between illness perception and adherence to antidiabetic medication (X2 = 4.01; p < 0.05). These results align with previous research indicating a positive relationship between illness perception and treatment adherence (13, 16, 23–26). Illness perception influences treatment adherence by affecting patients’ behavior and actions (14, 27, 28). Interpersonal problems and illness perceptions significantly influence the emotional adjustment of individuals with diabetes (29).
Although illness perception has been found to have a positive impact on treatment adherence and diabetes management, a considerable number of patients in this study (54.7%) reported suboptimal illness perception. Given the significance of illness perception, it is crucial to prioritize this aspect in educational interventions aimed at improving adherence. It is essential to integrate patient illness perception into diabetes care at all healthcare levels. Furthermore, patients with negative perceptions of their disease can benefit from practical interventions, such as psychoeducational and cognitive-behavioral approaches. By addressing illness perception comprehensively, healthcare providers can contribute to better patient outcomes in diabetes care (11).
This study aimed to examine the influence of illness perception domains on medication adherence. The results demonstrated significant associations between medication adherence and three domains of illness perception: acute/chronic timelines (p = 0.025), consequences (p < 0.0001), and emotional representation (p < 0.0001). The findings of this study are consistent with previous research (23, 24), reinforcing the importance of understanding illness perception in order to enhance medication adherence. The results of the study highlight the significance of gaining insights into individuals’ perceptions of their illness, as it can guide the development of strategies to improve medication adherence.
Based on the final model, medication adherence showed a positive association with illness consequences, personal control, and perception of emotional representation. Individuals with diabetes who have a comprehensive understanding of their condition are more likely to adhere to their prescribed medication. Particularly, patient-perceived illness consequences emerged as a significant factor influencing diabetes medication adherence, which is in line with previous research findings (16, 30). The influence of patient-perceived illness consequences on diabetes medication adherence can be attributed to various factors, including motivation, personal relevance, and sense of control, emotional responses, and patient-provider collaboration. Recognizing these factors can assist healthcare providers in customizing interventions and support strategies to improve medication adherence among patients with diabetes.
In this current study, patients who had a positive perception of personal diabetes control were more likely to take diabetes medication. This result is consistent with studies conducted in Saudi Arabia (16), Tripoli (24), and Iran (13). These results suggest that positive perceptions of diabetes control can promote better health outcomes. Perceived personal control is closely related to a patient’s commitment and confidence in their capacity to manage their disease and take their medications as prescribed. People are becoming more aware of their condition and health, and they feel more accountable to adhere to treatment regimens more closely. As a result, patients are confident in their ability to control their illness, which influences adherence to medications.
According to this study, a stronger perception of emotional representation was linked to a higher probability of taking diabetic medicine as prescribed. Similar results were obtained in Ghana (30), however different results were obtained in Malaysia (17). This suggests that interventions to improve emotional representation could help improve treatment adherence. Interventions could include better communication between health care providers and patients, improved patient education, and better recognition of emotional needs. In addition, we need to understand how patients perceive diabetes, because without emotional representation, treatment may not be appropriately tailored to the patient’s needs.
One of the strengths of this study is its examination of the relationship between various dimensions of illness perception and medication adherence. This highlights the need for healthcare professionals to target specific aspects of illness perception when addressing medication adherence. However, it is important to acknowledge the limitations of this study. Firstly, self-reported measures are susceptible to response bias, which may lead to an overestimation of behavioral performance. Additionally, participant recall bias regarding antidiabetic medication adherence could influence the study’s results. Moreover, the instrument used in the study should be further refined to ensure accurate and reliable data, taking into account the local context.
The implication of the study
Research examining the association between illness perception and medication adherence in patients with Diabetes mellitus has made significant contributions to the field. By understanding how individuals perceive their illness and how it impacts their adherence to medication regimens, valuable insights have been gained for healthcare professionals, leading to the development of effective interventions. Illness perception refers to an individual’s cognitive and emotional understanding of their illness, including their beliefs, expectations, and perceived consequences. Studies have shown that patients with positive illness perceptions are more likely to adhere to their medication regimens. This includes patients who have a better understanding of the chronic nature of diabetes, believe in the effectiveness of their treatment, and feel empowered to manage their condition.
The comprehensive understanding of illness perception and its impact on patient behavior has paved the way for the development of personalized interventions that address the unique needs of each patient, ultimately improving long-term treatment outcomes. It emphasizes the importance of incorporating illness perception as a key focus in educational interventions aimed at enhancing adherence. These research findings have significant implications for clinical practice. Healthcare professionals can utilize this knowledge to tailor interventions and enhance medication adherence in patients with Diabetes mellitus. By addressing patients’ illness perceptions, correcting misconceptions through education, and fostering a sense of control and self-efficacy, healthcare providers can make strides in improving medication adherence and, subsequently, patient outcomes. Gaining insight into the influence of illness perception on patient adherence and developing appropriate strategies should be a priority for healthcare professionals.
In summary, research on the association between illness perception and medication adherence in patients with Diabetes mellitus has shed light on the psychological factors that influence adherence behaviors. This valuable knowledge has the potential to inform interventions, support patient-centered care, and ultimately enhance the management of diabetes.
Conclusion
The current study demonstrates a positive association between higher illness perception and increased medication adherence and practice. Specifically, personal control, illness consequences, and emotional representation were identified as significant aspects of illness perception strongly linked to enhanced medication adherence.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The studies involving humans were approved by Asrat Woldeyes Health Science Campus, Debre Berhan University, and Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BG and AE: conceptualization, formal analysis, project administration, and writing – original draft. AE, BG, GA, BaT, EM, BeT, DZ, TD, TK, and YA: investigation, methodology, and writing – review & editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
We extend our heartfelt appreciation to the dedicated members of the research team who played a vital role in the successful completion of this study. Furthermore, we would like to express our thoughtful gratitude to all the participants, diligent data collectors, and supervisors for their valuable time and unwavering commitment to this research endeavor.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CI, confidence interval; DM, diabetes mellitus; IP, Illness perception; IPQ-R, modified illness perception questionnaire; SD, standard divisions
References
1. IDF, IDF Diabetes Atlas 10th Edition, Brussels, Belgium: International Diabetes Federation, 2021 Reports; Available at: www.diabetesatlas.org. (2021).
2. Koye, DN, Melaku, YA, Gelaw, YA, Zeleke, BM, Adane, AA, Tegegn, HG, et al. Mapping national, regional and local prevalence of hypertension and diabetes in Ethiopia using geospatial analysis. BMJ Open. (2022) 12:e065318. doi: 10.1136/bmjopen-2022-065318
3. IDF., Diabetes Atlas (2000), Brussels, Belgium: International Diabetes Federation; Available at: www.diabetesatlas.org.
4. Kerru, N, Singh-Pillay, A, Awolade, P, and Singh, P. Current anti-diabetic agents and their molecular targets: a review. Eur J Med Chem. (2018) 152:436–88. doi: 10.1016/j.ejmech.2018.04.061
5. Morrison, A, Stauffer, ME, and Kaufman, AS. Defining medication adherence in individual patients. Patient Prefer Adherence. (2015) 9:893–7. doi: 10.2147/PPA.S86249
6. Gast, A, and Mathes, T. Medication adherence influencing factors—an (updated) overview of systematic reviews. Syst Rev. (2019) 8:112. doi: 10.1186/s13643-019-1014-8
7. Yazew, KG, Walle, TA, and Azagew, AW. Prevalence of anti-diabetic medication adherence and determinant factors in Ethiopia: a systemic review and meta-analysis, 2019. Int J Africa Nurs Sci. (2019) 11:100167. doi: 10.1016/j.ijans.2019.100167
8. World Health Organization. Adherence to long-term therapies: Evidence for action. World Health Organization, (2003). Available at: https://apps.who.int/iris/handle/10665/42682.
9. Sendekie, AK, Netere, AK, Kasahun, AE, and Belachew, EA. Medication adherence and its impact on glycemic control in type 2 diabetes mellitus patients with comorbidity: a multicenter cross-sectional study in Northwest Ethiopia. PLoS One. (2022) 17:e0274971. doi: 10.1371/journal.pone.0274971
10. Broadbent, E, Petrie, KJ, Main, J, and Weinman, J. The brief illness perception questionnaire. J Psychosom Res. (2006) 60:631–7. doi: 10.1016/j.jpsychores.2005.10.020
11. Shahin, W, Kennedy, GA, and Stupans, I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Prefer Adherence. (2019) 13:1019–35. doi: 10.2147/PPA.S212046
12. Tang, J, and Gao, L. Illness perceptions among patients with type 2 diabetes mellitus: a cross-sectional study. Int J Nurs Pract. (2020) 26:e12801. doi: 10.1111/ijn.12801
13. Bilondi, SS, Noghabi, AD, and Aalami, H. The relationship between illness perception and medication adherence in patients with diabetes mellitus type II: illness perception and medication adherence. J Prev Med Hyg. (2021) 62:E966–e971. doi: 10.15167/2421-4248/jpmh2021.62.4.2277
14. Kugbey, N, Oppong, AK, and Adulai, K. Illness perception, diabetes knowledge and self-care practices among type-2 diabetes patients: a cross-sectional study. BMC Res Notes. (2017) 10:381. doi: 10.1186/s13104-017-2707-5
15. Milicevic, R, Jaksic, N, Aukst-Margetic, B, and Jakovljevic, M. Personality traits and treatment compliance in patients with type 2 diabetes mellitus. Psychiatr Danub. (2015) 2:586–9.
16. Alyami, M, Serlachius, A, Mokhtar, I, and Broadbent, E. Illness perceptions, HbA1c, and adherence in type 2 diabetes in Saudi Arabia. Patient Prefer Adherence. (2019) 13:1839–50. doi: 10.2147/PPA.S228670
17. Balasubramaniam, S, Lim, SL, Goh, LH, Subramaniam, S, and Tangiisuran, B. Evaluation of illness perceptions and their associations with glycaemic control, medication adherence and chronic kidney disease in type 2 diabetes mellitus patients in Malaysia. Diabetes Metab Syndr. (2019) 13:2585–91. doi: 10.1016/j.dsx.2019.07.011
18. Wolde, HF, Derso, T, Biks, GA, Yitayal, M, Ayele, TA, Gelaye, KA, et al. High hidden burden of diabetes mellitus among adults aged 18 years and above in urban Northwest Ethiopia. J Diabetes Res. (2020) 2020:1–9. doi: 10.1155/2020/9240398
19. Siraj, J, Abateka, T, and Kebede, O. Patients' adherence to anti-diabetic medications and associated factors in Mizan-Tepi university teaching hospital: a cross-sectional study. Inquiry. (2021) 58:004695802110674. doi: 10.1177/00469580211067477
20. Moss-Morris, R, Weinman, J, Petrie, K, Horne, R, Cameron, L, and Buick, D. The revised illness perception questionnaire (IPQ-R). Psychol Health. (2002) 17:1–16. doi: 10.1080/08870440290001494
21. Skinner, TC, Carey, ME, Cradock, S, Dallosso, HM, Daly, H, Davies, MJ, et al. Comparison of illness representations dimensions and illness representation clusters in predicting outcomes in the first year following diagnosis of type 2 diabetes: results from the DESMOND trial. Psychol Health. (2011) 26:321–35. doi: 10.1080/08870440903411039
22. Susan, H. The illness perceptions questionnaire-revised (IPQ-R). J Physiother. (2010) 56:280. doi: 10.1016/S1836-9553(10)70062-X
23. Saudi, RA, Abbas, RA, Nour-Eldein, H, and Sayed Ahmed, HA. Illness perception, medication adherence and glycemic control among primary health-care patients with type 2 diabetes mellitus at Port Said City. Egypt Diabetol Int. (2022) 13:522–30. doi: 10.1007/s13340-021-00567-6
24. Ashur, ST, Shah, SA, Bosseri, S, Morisky, DE, and Shamsuddin, K. Illness perceptions of Libyans with T2DM and their influence on medication adherence: a study in a diabetes center in Tripoli. Libyan J Med. (2015) 10:29797. doi: 10.3402/ljm.v10.29797
25. Kim, H, Sereika, SM, Lingler, JH, Albert, SM, and Bender, CM. Illness perceptions, self-efficacy, and self-reported medication adherence in persons aged 50 and older with type 2 diabetes. J Cardiovasc Nurs. (2021) 36:312–28. doi: 10.1097/JCN.0000000000000675
26. Ngetich, E, Pateekhum, C, Hashmi, A, Nadal, IP, Pinyopornpanish, K, English, M, et al. Illness perceptions, self-care practices, and glycemic control among type 2 diabetes patients in Chiang Mai, Thailand. Arch Public Health. (2022) 80:134. doi: 10.1186/s13690-022-00888-1
27. Alharbi, S, and Alhofaian, A. And a. MM., illness perception and medication adherence among adult patients with type 2 diabetes mellitus: a scoping review. Clin Pract. (2023) 13:71–83. doi: 10.3390/clinpract13010007. p. 71-83
28. Abdollahi, F, Bikdeli, H, Zeabadi, SM, Sepasi, RR, Kalhor, R, and Motalebi, SA. Predicting role of illness perception in treatment self-regulation among patients with type 2 diabetes. J Prev Med Hyg. (2022) 63:E604–e610. doi: 10.15167/2421-4248/jpmh2022.63.4.2727
29. Berry, E, Davies, M, and Dempster, M. Illness perception clusters and relationship quality are associated with diabetes distress in adults with type 2 diabetes. Psychol Health Med. (2017) 22:1118–26. doi: 10.1080/13548506.2017.1281976
Keywords: medication adherence, illness perception, patient with diabetes, perception towards medication, North Shoa Zone
Citation: Eshete A, Getye B, Aynaddis G, Tilaye B, Mekonnen E, Taye B, Zeleke D, Deresse T, Kifleyohans T and Assefa Y (2023) Association between illness perception and medication adherence in patients with diabetes mellitus in North Shoa, Zone: cross-sectional study. Front. Public Health. 11:1214725. doi: 10.3389/fpubh.2023.1214725
Edited by:
Ping Wang, Michigan State University, United StatesReviewed by:
Edward Zimbudzi, Monash University, AustraliaJoseph O. Fadare, Ekiti State University, Nigeria
Copyright © 2023 Eshete, Getye, Aynaddis, Tilaye, Mekonnen, Taye, Zeleke, Deresse, Kifleyohans and Assefa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akine Eshete, YWtpbmUuZXNoZXRlQHlhaG9vLmNvbQ==
 Akine Eshete
Akine Eshete Birhan Getye
Birhan Getye Getachew Aynaddis
Getachew Aynaddis Bantalem Tilaye
Bantalem Tilaye Elda Mekonnen3
Elda Mekonnen3 Dereje Zeleke
Dereje Zeleke Tilahun Deresse
Tilahun Deresse