
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 03 August 2023
Sec. Environmental Health and Exposome
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1210102
 Surekha Kishore1
Surekha Kishore1 Vandana Shah2
Vandana Shah2 Om Prakash Bera3
Om Prakash Bera3 U. Venkatesh4*
U. Venkatesh4* Rakesh Kakkar5
Rakesh Kakkar5 Pradeep Aggarwal6
Pradeep Aggarwal6 Pankaj Bhardwaj7
Pankaj Bhardwaj7 C. M. Singh8
C. M. Singh8 Chetna Maliye9
Chetna Maliye9 Suneela Garg10
Suneela Garg10 Geetha R. Menon11
Geetha R. Menon11 Puneet Misra12
Puneet Misra12 Shival Kishore Verma13 and the COVID SHS Study Group
Shival Kishore Verma13 and the COVID SHS Study GroupIntroduction: Exposure to secondhand smoke (SHS) is an established causal risk factor for cardiovascular disease (CVD) and chronic lung disease. Numerous studies have evaluated the role of tobacco in COVID-19 infection, severity, and mortality but missed the opportunity to assess the role of SHS. Therefore, this study was conducted to determine whether SHS is an independent risk factor for COVID-19 infection, severity, mortality, and other co-morbidities.
Methodology: Multicentric case–control study was conducted across six states in India. Severe COVID-19 patients were chosen as our study cases, and mild and moderate COVID-19 as control were evaluated for exposure to SHS. The sample size was calculated using Epi-info version 7. A neighborhood-matching technique was utilized to address ecological variability and enhance comparability between cases and controls, considering age and sex as additional matching criteria. The binary logistic regression model was used to measure the association, and the results were presented using an adjusted odds ratio. The data were analyzed using SPSS version 24 (SPSS Inc., Chicago, IL, USA).
Results: A total of 672 cases of severe COVID-19 and 681 controls of mild and moderate COVID-19 were recruited in this study. The adjusted odds ratio (AOR) for SHS exposure at home was 3.03 (CI 95%: 2.29–4.02) compared to mild/moderate COVID-19, while SHS exposure at the workplace had odds of 2.19 (CI 95%: 1.43–3.35). Other factors significantly related to the severity of COVID-19 were a history of COVID-19 vaccination before illness, body mass index (BMI), and attached kitchen at home.
Discussion: The results of this study suggest that cumulative exposure to secondhand cigarette smoke is an independent risk factor for severe COVID-19 illness. More studies with the use of biomarkers and quantification of SHS exposure in the future are needed.
Globally, more than 460 million SARS-CoV-2 infection (COVID-19) cases, with 6 million deaths, have been reported in people of all age groups (1). COVID-19 has been known to cause severe respiratory illness and multi-organ inflammatory disease (2). Smoking, cardiovascular disease (CVD), hypertension, and chronic lung diseases are risk factors for COVID-19 severity (3–5). Older individuals, as well as those of any age with co-morbidities, such as hypertension and diabetes, have exhibited a poorer prognosis (6). Individuals with chronic obstructive pulmonary disease (COPD) or other respiratory illnesses are at a greater risk for severe illness and have been associated with hospitalization and intensive care unit (ICU) admissions (7). Tobacco smoke comprises over 7,000 chemicals, including 69 compounds known to be carcinogenic and other harmful chemicals such as hydrogen cyanide, carbon monoxide, and ammonia (8). Tobacco use including smoking is associated with increased severity/progression of disease, mortality, and hospitalized COVID-19 patients (9–11). Secondhand smoke (SHS) is a combination of tobacco smoke exhaled by smokers during the smoking of cigarettes, bidi, hookah, etc., and smoke produced from the burning ends of these products. Thirdhand smoke is a residue from firsthand and SHS on clothes, furniture, and household surfaces (12). SHS is responsible for approximately 1.2 million deaths globally each year (13). Adults who are exposed to SHS have increased rates of coronary heart disease, stroke, and lung cancer; additionally, babies born to mothers who smoke are more likely to die of sudden infant death syndrome (SIDS), prematurity, low birth weight, and other conditions (14, 15). Moreover, it is a fact that smokers are less aware of the ill effects of SHS when compared to smokers (16). Exposure to SHS is an established causal risk factor for cardiovascular disease (CVD) and chronic lung disease (17) and may also be a risk factor for COVID-19 severity, either by contributing to the development of these underlying conditions or by triggering inflammation and upregulation of angiotensin-converting enzyme 2 (ACE-2) receptors, which facilitate the entry of COVID-19 into cells (5). However, a lack of SHS surveillance makes it difficult to quantify any potential relationship or to make evidence-informed recommendations about the effects of SHS exposure on COVID-19 incidence or severity (5). Numerous studies have evaluated the role of tobacco in COVID-19 infection, severity, and mortality but missed the opportunity to assess the role of SHS (18). Thus, this study has been planned to study SHS as an independent risk factor for COVID-19 infection, severity, mortality, and other co-morbidities. With this background, we conducted a case–control study to determine the association of COVID-19 severity with SHS exposure SHS and to evaluate the relationship between the clinical-social profile of COVID-19 patients and exposure to SHS (19).
After obtaining approval from the Institutional Ethics Committee, this case–control study was conducted retrospectively by choosing persons with COVID-19 admitted and non-admitted from multiple sites across India (Figure 1).
All the cases were ≥ 18 years of age for both sexes and were from rural as well as urban areas. We evaluated the exposure to SHS in our study, comparing severe COVID-19 patients as cases and mild and moderate COVID-19 patients as controls. The recruited cases were laboratory-confirmed COVID-19 patients with severe manifestations between 1 January 2020 and 28 February 2022. The cases were contacted and traced from the inpatient records available in the study sites. The control group participants in this research study were frequently matched to the cases based on gender, age at the time of recruitment, and neighborhood-matched control selection was done with each case to minimize ecologic variability. Active smokers, individuals with incomplete COVID-19 diagnosis information, and those who did not provide consent were excluded from both the case and control groups.
After obtaining written consent, trained interviewers conducted face-to-face interviews with all participants using a questionnaire that covered topics such as past and current exposure to SHS, demographic details, lifestyle habits (including alcohol consumption), and both occupational and home exposure to SHS. Participants self-reported exposure to SHS was assessed by asking whether anyone who had ever lived in their household was a smoker, either currently or in the past (such as parents, grandparents, siblings, or others), and if so, whether they regularly smoked in the home during their lifetime. Similar questions were asked about the regular smoking habits of others in the household during the participant's childhood. The participants were also asked to provide information about their age at the time of exposure to SHS and the number of active smokers in their households.
• Secondhand smoke: SHS is the combination of smoke from the burning end of a cigarette, and the smoke breathed out by smokers (20).
• COVID-infected cases: A person with laboratory confirmation of COVID-19 infection (RT PCR Positive), irrespective of clinical signs and symptoms.
• Severe COVID-19: The severity of COVID-19 was defined as patients admitted with COVID-19 having SpO2 <90% on room air at sea level or COVID-19 Reporting and Data System (CO-RADS) on Chest Computed Tomography 4 or more at the time of admission. Patients with COVID-19 were considered to have severe illness if they have SpO2 <94% on room air at sea level, PaO2/FiO2 <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50%. These patients may experience rapid clinical deterioration (21, 22).
• Mild/Moderate COVID-19: Patients who were diagnosed with COVID-19 but have not shown signs of severe COVID-19.
• Smoking: Current Smoker user is an adult who has smoked 100 cigarettes in his or her lifetime and currently smokes cigarettes (until the COVID-19 illness). A former smoker user was an adult who had smoked at least 100 cigarettes in his or her lifetime but who had quit smoking at the time of the interview. Never smoker was an adult who has never smoked, or who has smoked less than 100 cigarettes in his or her lifetime (23).
• SHS exposure at Home: Exposure at home was estimated for non-smokers who reported anyone smoking inside his/her home (that excludes areas outside, such as patios, balconies, gardens, etc., that are not fully enclosed). SHS was taken to be present (“Yes”) if the response to the question “How often does anyone smoke inside your home?” was “more than or equal to once in the last 1 month” (24).
• SHS exposure at the workplace: This was assessed for the respondents who work outside of the home and who usually work indoors or both indoors and outdoors. SHS is defined as the percentage of respondents who reported someone smoking at least in indoor workplaces in the past 30 days before the survey. SHS was considered to be present (“Yes”) if the response to the question “During the past 30 days- did anyone smoke in indoor areas where you work?” was affirmative (24).
Statistical analysis was performed using IBM SPSS Statistics Software (version 26; IBM, New York, USA). Quantitative data were presented as mean with standard deviation (SD) and counting data were presented as the percentage of the total unless otherwise specified. The comparisons of the quantitative data were statistically evaluated using the parametric or non-parametric test, according to the distribution which was assessed by the Shapiro–Wilk test.
We used independent t-tests to measure the differences between the two groups (cases vs. controls) for continuous variables and Pearson's chi-square to test the correlations between the study groups for categorical parameters. We used binary logistic regression models to test correlations between the study groups and SHS exposure variables with adjustments for significant and potential confounders. The p-value of 5% or less was considered statistically significant. The data were analyzed using SPSS version 24 (SPSS Inc., Chicago, IL, USA).
The sample size was calculated using Epi-info version 7. Three Fleiss with continuity correction formula calculated the required sample size with a two-sided significance level (1-alpha) 95% and 0.80% Power (1-beta, % chance of detecting). With a controls/cases ratio of 1 and an odds ratio of 1.3, a total of 1,132 individuals are needed for the study, comprising 566 individuals in both the cases and control. The required sample size calculated using Fleiss or Fleiss with continuity correction formula was 1,070 and 1,132 persons, respectively. A minimum sample size of 1,250 individuals was determined for the study.
This research adheres to rigorous ethical standards, including obtaining approval from the Institutional Human Ethics Committee (IHEC) with the number IHEC/AIIMS-GKP/BMR/105/2022 at AIIMS Gorakhpur. Confidentiality, informed consent, participant wellbeing, and data protection were prioritized throughout the study.
A total of 672 cases of severe COVID-19 and 681 controls of mild and moderate COVID-19 were recruited in this study. The socio-demographic data and other characteristics among cases and controls were compared using the chi-square test, as shown in Table 1. Participants who were above 30 years of age were significantly associated with severe COVID-19 compared to mild/moderate COVID-19, i.e., 81.4% (547/672) vs. 69.3% (472/672) (P < 0.001). Similarly, among other demographic variables, married individuals and illiterate were significantly associated with severe COVID-19 illness with a p-value of <0.001 and 0.02, respectively. Among the clinical characteristics, those with BMI ≥23.0, RBS ≥200, systolic blood pressure ≥140, and diastolic blood pressure ≥90 at the time of the interview were found to be significantly associated with severe COVID-19 illness. Also, it was found that among the severe cases, the history of vaccination was less frequent compared to the controls, i.e., 7.5% (42/563) vs. 21.5% (123/571) (P < 0.001).
It was also found that exposure to SHS was comparatively more among participants with severe COVID-19 illness (cases) when compared to participants with moderate and mild COVID-19 illness (controls), i.e., 51.2% (344/672) vs. 27.6% (147/681) (P < 0.001). Similarly, the participants with severe COVID-19 illness reported more frequent exposure to secondhand smoking at the workplace compared to participants with mild and moderate COVID-19 illness, i.e., 15.5% (111/672) vs. 9.0% (61/681) (P < 0.001), as shown in Table 2.
To control all potential confounders, logistic regression analysis was performed, and it was observed that the adjusted odds ratio (AOR) for SHS exposure at home was 3.03 (CI 95%: 2.29–4.02) compared to mild/moderate COVID-19, while SHS exposure at the workplace had odds of 2.19 (CI 95%: 1.43–3.35) compare to control, i.e., mild/moderate illness. The COVID vaccination and BMI <23 were shown to be protective with an odds ratio of 0.24 (0.15–0.36) and 0.51 (0.38–0.71), respectively. Furthermore, other variables, such as systolic blood pressure and history of COVID-19 vaccination, also had a significant association with severe COVID-19 illness when compared to mild and moderate illness (p-value of < 0.01) (Table 3).
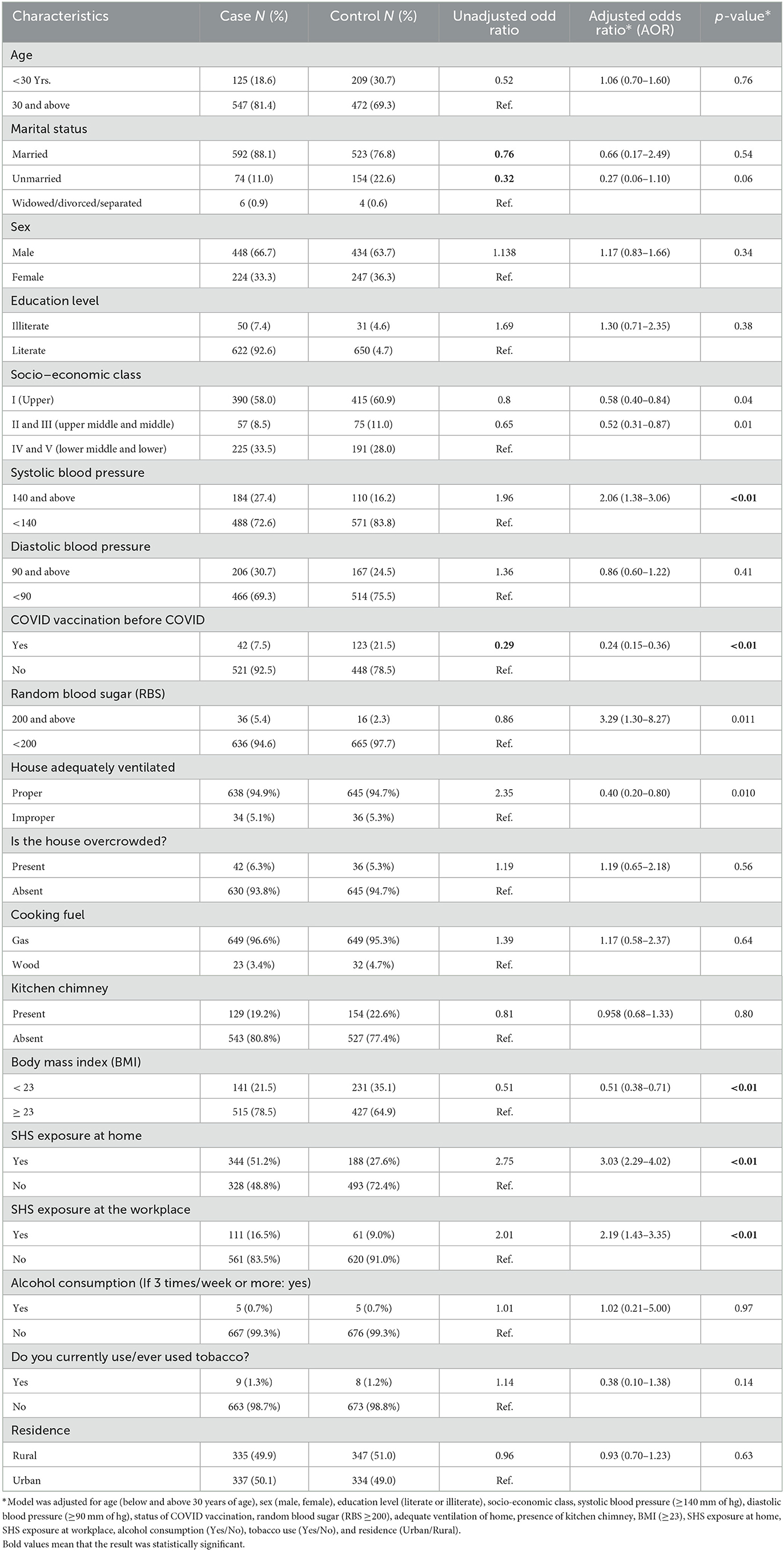
Table 3. Association of SHS exposure and other characteristics with case and control using logistic regression analysis.
In this case–control study, after controlling all confounders related to socio-demographic and clinic-social characteristics, we found that those who had severe COVID-19 illness had 3.03 times greater odds of being exposed to SHS at their home when compared to controls. Also, the exposure to SHS at the workplace was 2.19 times greater among participants with severe COVID-19 illness compared to participants with mild and moderate COVID-19 illness. Furthermore, it was also noticed that participants who were severely ill with COVID-19, when compared to participants with mild and moderate illness due to the same were less likely to have a previous history of COVID-19 vaccination.
To the best of our knowledge, this study is the first to associate secondhand exposure with the severity of COVID. Our study demonstrated secondhand smoking as an independent risk factor for severe COVID illness. Our research results were also consistent with other studies in Asian countries where the level of tobacco exposure at home and in the environment was high (8–13). Also, as mentioned in WHO's Global estimate of the burden of disease from SHS (25), 9% of the global lower respiratory tract infection risk could be attributed to SHS. In addition, our study's findings somewhat align with those of a study performed by Jasper V. Been et al. (26), on exposure to SHS and reduction in hospitalization due to lower respiratory tract infection. Similarly, a study by Flouris et al. (27) also claims that even 1-h exposure to SHS produces deleterious effects on our lung membrane, resulting in exaggerated respiratory tract infection symptoms. Other factors that were found to be associated with severe COVID-19 illness are BMI >23 kg/m2 and systolic blood pressure of 140 mm of hg or above. Some previous literature also suggests some other factors that are independently related/associated with the severity of COVID-19 illness such as obesity, low education level, and diet. Albashir AAD (28) mentioned in his study that the most common characteristics of those hospitalized due to severe COVID-19 illness were diabetes, chronic lung disease and cardiovascular disease, and obesity is a well-known risk factor for these diseases. One of the key points of his study was that obesity is a strong independent risk factor for hospitalization in COVID-19 and increases the need for critical care and invasive mechanism (28, 29). It is also found in other studies, in addition to factors such as diabetes, diet, and nutrient intake, such as supplementation with omega-3 fatty acids and fish consumption (30, 31).
The strengths of this study were that we recorded and controlled environmental factors, vaccination status, and clinical characteristics in our analysis, thus eliminating the major confounders. Neighborhood matching was made for the selection of controls thus minimizing ecological bias along with age and sex.
The limitations of this study were as follows: First, SHS exposure was estimated through face-to-face interviews; it was neither possible to measure nicotine levels in hair nor to measure cotinine in urine to determine tobacco exposure. Second, as this study was conducted during the COVID-19 lockdown, SHS exposure at social events could not be recorded. Third, due to the retrospective nature of case–control studies, the questionnaires were administered after the COVID-19 illness occurred, and therefore bias cannot be excluded. Finally, we cannot collect all possible confounders for the severity of COVID-19, as it is a memory bias. More studies using biomarkers and quantifying SHS exposure in the future are needed to confirm this finding. The results of this study suggest that cumulative exposure to secondhand cigarette smoke is an independent risk factor for hospital admission from COVID-19.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Ethical Committee, AIIMS Gorakhpur Similar ethical permission was obtained from all the other sites before the commencement of data collection. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Conceptualization: SKi, VS, OB, and UV. Data curation and investigation: SKi, UV, RK, PA, PB, CS, and CM. Formal analysis: UV, OB, and GM. Supervision: SKi, VS, OB, UV, CM, SG, GM, and PM. Validation: SKi, UV, RK, PA, PB, CS, CM, GM, PM, and SG. Writing—original draft: UV, VS, OB, RK, PA, and PB. Writing—review and editing: SKi, UV, CS, CM, SG, GM, and PM. All authors contributed to the article and approved the submitted version.
Dr. D.K. Srivastava (Professor and HoD, Department of Community Medicine, Baba Raghav Das Medical College Gorakhpur, Uttar Pradesh, India), Dr. Anuj Mundra (Department of Community Medicine, Mahatma Gandhi Institute of Medical Sciences, Sevagram, Maharashtra, India), Dr. Amey Dhatrak (Department of Community Medicine, Mahatma Gandhi Institute of Medical Sciences, Sevagram, Maharashtra, India), Dr. Mahendra Singh Gehlot (Department of Community and Family Medicine, All India Institute of Medical Sciences, Rishikesh, Uttrakhand, India), Dr. Yogesh Bahurupi (Department of Community and Family Medicine, All India Institute of Medical Sciences, Rishikesh, Uttrakhand, India), Dr. Santosh Kumar Nirala (Department of Community and Family Medicine, All India Institute of Medical Sciences, Patna, Bihar, India), Dr. Mahendra Pratap Singh (Department of Community Medicine and Family Medicine, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India), and Mr. Arvind Kumar Jaiswal (Department of Community Medicine and Family Medicine, All India Institute of Medical Sciences, Gorakhpur, Uttar Pradesh, India).
This study was funded by the Campaign for Tobacco-Free Kids. The Campaign for Tobacco-Free Kids is a leading organization working to reduce tobacco use and its devastating health and economic consequences in the United States and around the world.
We thank the families who participated in this study for contributing their time and expertise. We are also grateful to Campaign for Tobacco-Free Kids, USA, for supporting the study.
VS was employed by Campaign for Tobacco-Free Kids. OB was employed by Global Health Advocacy Incubator.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/ (accessed December 12, 2022).
2. World Health Organization Coronavirus Disease (COVID-19) Pandemic. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed December 12, 2022).
3. World Health Organization World health Organisation Statement: Tobacco Use and COVID-19 2020. Geneva: World Health Organization.
4. Centers for Disease Control and Prevention. Coronavirus Disease 2019: People With 21 Certain Medical Conditions 2020. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medicalconditions.html#smoking (accessed December 12, 2022).
5. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80. doi: 10.1016/j.cell.2020.02.052
6. Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. (2020) 14:303–10. doi: 10.1016/j.dsx.2020.04.004
7. Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J Med Virol. (2020) 92:1915–21. doi: 10.1002/jmv.25889
8. National Cancer Institute. Harms of Cigarette Smoking and Health Benefits of Quitting. Available online at: https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/cessation-fact-sheet (accessed December 12, 2022).
9. RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol. (2021) 93:1045–56. doi: 10.1002/jmv.26389
10. Baker J, Krishnan N, Abroms LC, Berg CJ. The impact of tobacco use on COVID outcomes: a systematic review. J Smok Cessat. (2022) 20:2022. doi: 10.1155/2022/5474397
11. World Health Organization. Available online at: https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19 (accessed December 12, 2022).
12. Garg S, Sharma AD. Secondhand smoke: an unintended public health concern. Indian Community Fam Med. (2022) 8:81–5. doi: 10.4103/ijcfm.ijcfm_64_22
13. WHO statement: Tobacco Use COVID-19. (2020). Available online at: https://www.who.int/news/item/11-05-2020-who-statement-tobacco-use-and-covid-19
14. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. Geneva: World Health Organization (2008).
15. Öberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to secondhand smoke: a retrospective analysis of data from 192 countries. Lancet. (2011) 377:139–46. doi: 10.1016/S0140-6736(10)61388-8
16. Lee SR, Cho AR, Lee SY, Cho YH, Park EJ, Kim YJ, et al. Secondhand smoke knowledge, sources of information, and associated factors among hospital staff. PLoS ONE. (2019) 14:e0210981. doi: 10.1371/journal.pone.0210981
17. Office on Smoking and Health. Publications and Reports of the Surgeon General. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention (US), (2006).
18. Klein JD, Resnick EA, Chamberlin ME, Kress EA. Secondhand smoke surveillance and COVID-19: a missed opportunity. Tob Control. (2021) 32:265–6. doi: 10.1136/tobaccocontrol-2021-056532
19. Klein JD, Chamberlin ME, Kress EA, Geraci MW, Rosenblatt S, Boykan R, et al. Asking the right questions about secondhand smoke. Nicotine Tob Res. (2021) 23:57–62. doi: 10.1093/ntr/ntz125
20. Centers for Disease Control and Prevention. Data and statistics. Centers for Disease Control and Prevention (2022). Available online at: https://www.cdc.gov/tobacco/data_statistics/index.html (accessed December 17, 2022).
21. Clinical Management Protocol for COVID-19 - Goi RSS. Available online at: https://www.mohfw.gov.in/pdf/ClinicalManagementProtocolforCOVID19.pdf (accessed December 19, 2022).
22. Indian Council of Medical Research. Delhi ICMRN. Indian Council of Medical Research, New Delhi. Available online at: https://www.icmr.gov.in/pdf/covid/techdoc/COVID_Clinical_Management_14012022.pdf (accessed December 19, 2022).
23. Centers for Disease Control and Prevention. NHIS - Adult Tobacco Use - Glossary. Centers for Disease Control and Prevention (2017). Available online at: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm (accessed December 10, 2022).
24. Verma M, Kathirvel S, Das M, Aggarwal R, Goel S. Trends and patterns of secondhand smoke exposure amongst the non-smokers in India-A secondary data analysis from the Global Adult Tobacco Survey (GATS) I andamp; II. PLoS ONE. (2020) 15:e0233861. doi: 10.1371/journal.pone.0233861
25. Oberg M, Jaakkola MS, Prüss-Üstün A, Peruga A, Woodward A, World Health Organization. Global Estimate of the Burden of Disease From Secondhand Smoke. Available online at: https://apps.who.int/iris/handle/10665/44426 (accessed December 19, 2022).
26. Been JV, Millett C, Lee JT, van Schayck CP, Sheikh A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections. Eur Respir J. (2015) 46:697–706. doi: 10.1183/09031936.00014615
27. Flouris AD, Koutedakis Y. Immediate and short-term consequences of secondhand smoke exposure on the respiratory system. Curr Opin Pulm Med. (2011) 17:110–5. doi: 10.1097/MCP.0b013e328343165d
28. Albashir AA. The potential impacts of obesity on COVID-19. Clin Med. (2020) 20:e109. doi: 10.7861/clinmed.2020-0239
29. CDC Covid-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. Morb Mortal Weekly Rep. (2020) 69:382–6. doi: 10.15585/mmwr.mm6913e2
30. Zapata B R, Müller JM, Vásquez JE, Ravera F, Lago G, Cañón E, et al. Omega-3 index and clinical outcomes of severe covid-19: preliminary results of a cross-sectional study. Int J Environ Res Public Health. (2021) 18:7722. doi: 10.3390/ijerph18157722
Keywords: secondhand smoke, COVID-19, smoking, vaccination, substance abuse
Citation: Kishore S, Shah V, Bera OP, Venkatesh U, Kakkar R, Aggarwal P, Bhardwaj P, Singh CM, Maliye C, Garg S, Menon GR, Misra P, Kishore Verma S and the COVID SHS Study Group (2023) Risk of secondhand smoke exposure and severity of COVID-19 infection: multicenter case–control study. Front. Public Health 11:1210102. doi: 10.3389/fpubh.2023.1210102
Received: 24 April 2023; Accepted: 05 July 2023;
Published: 03 August 2023.
Edited by:
Mohammad Javad Mohammadi, Ahvaz Jundishapur University of Medical Sciences, IranReviewed by:
Muriel Ramirez Santana, Universidad Católica del Norte, ChileCopyright © 2023 Kishore, Shah, Bera, Venkatesh, Kakkar, Aggarwal, Bhardwaj, Singh, Maliye, Garg, Menon, Misra, Kishore Verma and the COVID SHS Study Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: U. Venkatesh, dmVua2F0ZXNoMjAwN21iYnNAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.