- 1Tohoku Medical Megabank Organization, Tohoku University, Sendai, Japan
- 2Graduate School of Medicine, Tohoku University, Sendai, Japan
- 3Department of Health and Social Behavior, School of Public Health, The University of Tokyo, Tokyo, Japan
- 4Department of Disaster Public Health, International Research Institute of Disaster Science, Tohoku University, Sendai, Japan
Introduction: Health literacy (HL) can be regarded as a key element of non-pharmaceutical interventions used in emergency responses. The present study aimed to determine the associations of combinations of general HL and COVID-19-related HL with COVID-19 protective behaviors and healthy lifestyle behaviors.
Methods: A questionnaire survey was conducted from December 2020 to January 2021 among residents in Japanese metropolitan areas. Valid responses were received from 1,443 residents. The levels of HL were categorized into four groups: low level in both HLs (reference), high level in general HL only, high level in COVID-19-related HL only, and high level in both HLs. The total scores of eight COVID-19 protective behaviors were dichotomized into low and high adherence. Healthy lifestyle behaviors included healthy and balanced diet, adequate sleep, and regular exercise. Poisson regression analyses were conducted to examine the associations between the HL groups and high adherence to COVID-19 protective behaviors.
Results: High level in COVID-19-related HL only was associated with high adherence to COVID-19 protective behaviors [prevalence ratio (PR), 1.25; 95% confidence interval (CI), 1.09–1.45], while high level in general HL only was associated with healthy and balanced diet (PR, 1.49; 95% CI, 1.04–2.13), adequate sleep (PR, 1.46; 95% CI, 1.02–2.10), and regular exercise (PR, 2.00; 95% CI, 1.29–3.13). High level in both HLs showed the highest prevalence of high adherence to COVID-19 protective behaviors and healthy lifestyle behaviors.
Conclusion: These findings indicate that COVID-19-related HL and general HL can both be considered to enhance protective behaviors.
Introduction
Since the beginning of the coronavirus disease 2019 (COVID-19) pandemic, governments have implemented both pharmaceutical and non-pharmaceutical measures to curb the spread of the virus (1). While efforts to develop pharmaceutical interventions for COVID-19 are under way, non-pharmaceutical interventions still play an important role in the control of the pandemic (2–4). Therefore, promoting motivation and adherence to non-pharmaceutical preventive behavioral recommendations presents an important public health challenge. In addition, healthy lifestyle behaviors play an important role in maintaining physical and mental health during the COVID-19 pandemic, as well as during ordinary times (5, 6).
Health literacy (HL) can be regarded as a key element of non-pharmaceutical interventions used in emergency responses (7, 8). HL has been defined as people’s knowledge, motivation, and competence to access, understand, appraise, and apply health information to make judgements and decisions in everyday life concerning healthcare, disease prevention, and health promotion to maintain or improve their quality of life (9). Therefore, HL is critical for informed decision-making and empowers people and communities (10). There is accumulating evidence that people with higher levels of HL are more likely to adhere to COVID-19 protective behaviors (11–20). However, these studies focused mainly on general HL. This type of HL may be inadequate for assessing responses to the COVID-19 pandemic because HL is context-dependent and therefore requires different forms of cognitive processing (21). It is possible that people with generally acceptable HL skills may still face HL challenges in certain contexts. To the best of our knowledge, no studies have examined the associations between combinations of general HL and COVID-19-related HL and COVID-19 protective behaviors. Furthermore, it remains unclear whether HL is differently associated with COVID-19 protective behaviors and healthy lifestyle behaviors.
Considering the above circumstances, we aimed to determine the associations of combinations of general HL and COVID-19-related HL with COVID-19 protective behaviors and healthy lifestyle behaviors in Japan. Unlike other countries, Japan has relied heavily on voluntary behavioral changes and cooperation, because the public health measures implemented by the Japanese government to mitigate COVID-19 do not have penalties for non-adherence. Therefore, we hypothesized that HL is a key determinant of adherence to COVID-19 protective behaviors.
Materials and methods
Study population
Data were obtained from the Japanese Study of Stratification, Health, Income, and Neighborhood (J-SHINE), which has been described elsewhere (22). The first-wave survey was conducted in four municipalities in and around the greater Tokyo metropolitan area between October 2010 and February 2011. Among 13,920 residents aged 25–50 years who were probabilistically selected from the residential registry in each of these four municipalities, survey staff members were able to contact 8,408 residents and received valid responses from 4,317 residents. The survey participants were re-contacted in 2012 and 2017 (the second and third waves) (23). The fourth-wave survey was conducted between December 2020 and January 2021 (24). Among 1,638 residents who responded, 97.0% responded online and 3.0% responded offline. We analyzed 1,443 participants with no missing values for any variables used in the analyses. The Research Ethics Committee of The University of Tokyo, Graduate School of Medicine approved the survey procedure of the J-SHINE (Approval No. 3073). The J-SHINE Data Management Committee approved the secondary use of the data, with personally identifiable information deleted to ensure confidentiality.
General HL and COVID-19-related HL
General HL was measured using the Communicative and Critical Health Literacy (CCHL) scale for the first-wave questionnaire (25). This scale was developed and validated in Japan to assess communicative and critical HL (26). Communicative HL refers to the capacity to collect necessary and appropriate information to support one’s actions and communicate the information to others, while critical HL refers to one’s capacity to critically evaluate the quality of available information and select appropriate information for use in decision-making (26). Participants were asked whether they could do the following: collect health-related information from various sources; extract the information they want; understand and communicate the obtained information; consider the credibility of the information; and make decisions based on the information, in the context of health issues. Each item was rated on a five-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The scores of these five responses were summed and divided by the number of items to determine a total score (theoretical range: 1–5), with higher scores indicating greater HL (25). The Cronbach’s alpha value of the scale was 0.83, and this was not improved by the deletion of any specific item.
COVID-19-related HL was measured based on the questionnaire in the “Survey tool and guidance” edited by the World Health Organization Regional Office for Europe included in the fourth-wave survey (27). Participants were asked how easy or difficult they found it to: find the information they need related to COVID-19; understand information about what to do if they think they have COVID-19; judge if the information about COVID-19 in the media is reliable; understand restrictions and recommendations of authorities regarding COVID-19; follow the recommendations on how to protect themselves from COVID-19; understand recommendations about when to stay at home from work/school, and when not to; and understand recommendations about when to engage in social activities, and when not to. Each item was rated on a five-point Likert scale, ranging from 1 (very difficult) to 5 (very easy). The scores of these seven responses were summed and divided by the number of items to determine a total score (theoretical range: 1–5), with higher scores indicating greater HL. The Cronbach’s alpha value of the scale was 0.85, and this was not improved by the deletion of any specific item. According to the process-knowledge model of HL (21), HL can be synergistically acquired through processing capacity and knowledge. Furthermore, knowledge can offset limitations in processing capacity. We can argue that the general HL measure we relied on (CCHL) measures the perceived capacity for processing health information rather than knowledge. In contrast, the context-specific HL measure we adopted (COVID-19-related HL) measures domain-specific knowledge and the capacity to process the optimal responses for controlling COVID-19 infection. Adopting this theory frame, we could then hypothesize that high scores in COVID-19-related HL (specific knowledge-based HL) would result in a marked likelihood of adoption of COVID-19 protective behavior, regardless of the level of general HL (processing capacity-based HL). In contrast, high general HL is likely to be associated with non-specific healthy lifestyle behaviors.
HL was categorized into four groups, after dichotomizing each HL by the median score (25): low level in both HLs (low general HL and low COVID-19-related HL; reference), high level in general HL only (high general HL and low COVID-19-related HL), high level in COVID-19-related HL only (low general HL and high COVID-19-related HL), and high level in both HLs (high general HL and high COVID-19-related HL).
COVID-19 protective behaviors
Participants were asked whether they had performed the COVID-19 protective behaviors during the past 1 month, based on the protective measures against COVID-19 recommended by the World Health Organization: wearing a mask outside their home; staying at home as much as possible; avoiding gatherings; avoiding the use of public transportation; regularly and thoroughly cleaning their hands with an alcohol-based hand rub or washing them with soap and water; covering their mouth and nose with their bent elbow or tissue when they cough or sneeze; disinfecting surfaces frequently, especially those that are regularly touched; and maintaining at least a 2 m distance between themselves and others when outdoors. Each item was rated on a five-point Likert scale as never (1), almost never (2), sometimes (3), almost always (4), or always (5). The scores of these eight responses were summed and divided by the number of items to determine a total score (theoretical range: 1–5), with higher scores indicating adherence to more protective behaviors. The Cronbach’s alpha value of the scale was 0.77, and this was not improved by the deletion of any specific item. High adherence to total protective behaviors was defined as a total score greater than the median score of 4.
Healthy lifestyle behaviors
Three types of health-related behaviors were measured: healthy and balanced diet, adequate sleep, and regular exercise (5). Each item was rated on a five-point Likert scale as never, almost never, sometimes, almost always, or always. Responses to each item were dichotomized as low adherence (never, almost never, sometimes, almost always) and high adherence (always) to healthy lifestyle behaviors.
Covariates
As covariates, we chose age, sex, education level (high school or lower, college, university or higher), annual household income (≤4.99, 5.00–9.99, ≥10.00 million Japanese yen, unknown/refusal), work status (working, not working), self-rated health, and psychological distress. Self-rated health was measured using the question “How would you describe your health during the past 1 month?” Responses were dichotomized as good health (excellent, very good, good) and poor health (fair, poor) for the purposes of analysis. Psychological distress was measured using the K6 scale, which comprises six items assessing depressive moods and anxiety during the past 1 month on a five-point Likert scale ranging from 0 (none of the time) to 4 (all the time) (28, 29). A cut-off score of 5 was used to identify psychological distress (29, 30).
Statistical analysis
The characteristics of the participants were compared between the HL groups using the chi-square test. Poisson regression analyses with robust variance estimators were conducted to examine the associations between the HL groups and high adherence to COVID-19 protective behaviors. Prevalence ratios (PRs) and 95% confidence intervals (CIs) were calculated after adjustment for covariates. Low level in both HLs was set as the reference category. Similar analyses were conducted for healthy lifestyle behaviors.
All analyses were conducted with Stata 16.0 (StataCorp LP, College Station, TX, United States). For all analyses, a two-tailed p-value <0.05 was considered statistically significant.
Results
Table 1 shows the characteristics of the participants. The prevalences of the HL groups were 35.8% for low level in both HLs, 15.1% for high level in general HL only, 26.1% for high level in COVID-19-related HL only, and 23.0% for high level in both HLs. Participants with high level in both HLs were more likely to be men, be highly educated, and have higher income, and less likely to have psychological distress.
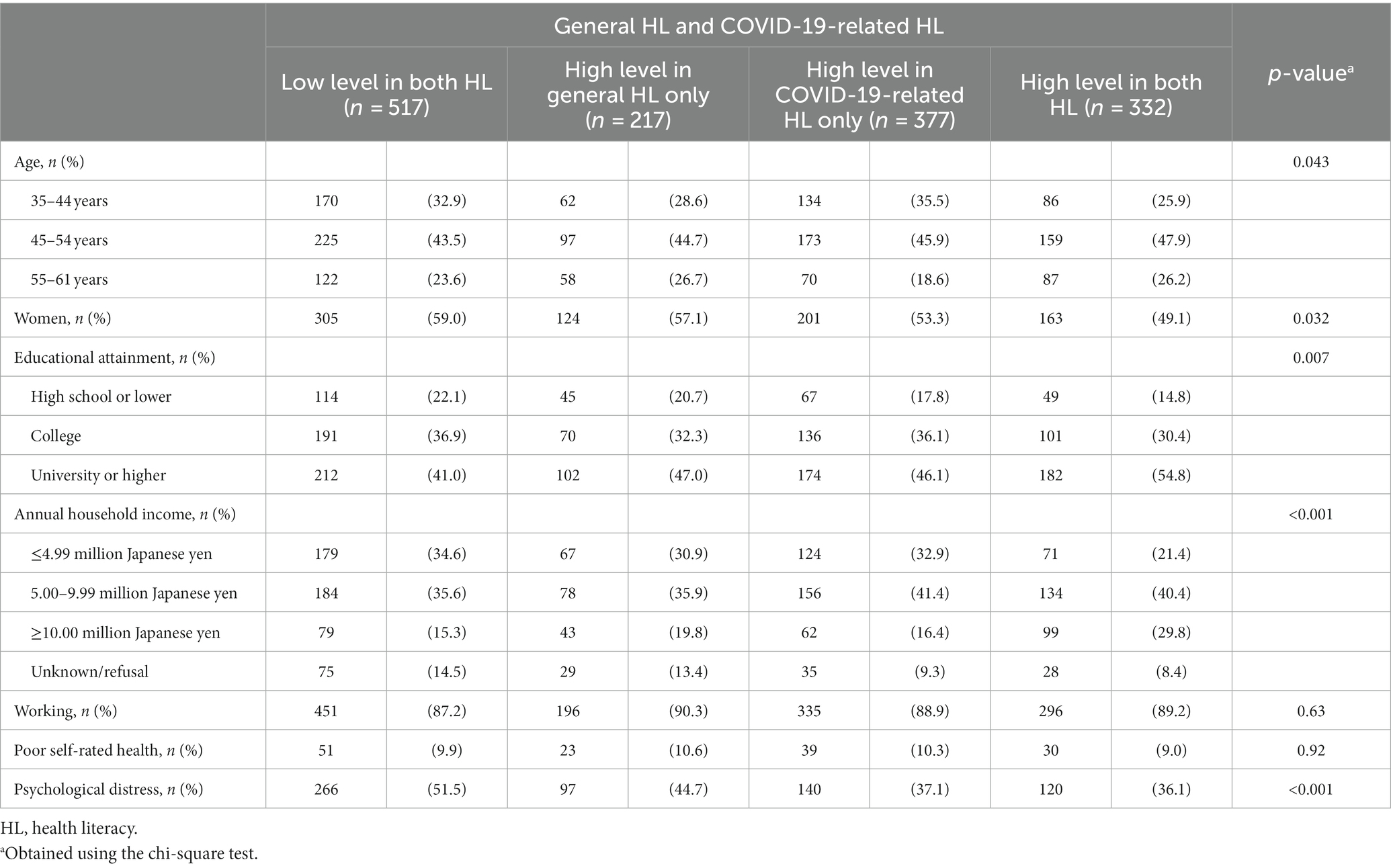
Table 1. Characteristics of participants: the Japanese Study of Stratification, Health, Income, and Neighborhood (J-SHINE).
Table 2 presents the associations between combinations of general HL and COVID-19-related HL and high adherence to COVID-19 protective behaviors. High level in COVID-19-related HL only, but not high level in general HL only, was associated with high adherence to COVID-19 protective behaviors; the multivariate-adjusted PRs were 1.25 (95% CI, 1.09–1.45) and 1.11 (95% CI, 0.93–1.34), respectively. High level in both HLs was associated with high adherence to COVID-19 protective behaviors; the multivariate-adjusted PR was 1.29 (95% CI, 1.11–1.50). Female sex, low income, and non-working status were associated with high adherence to COVID-19 protective behaviors, while age, education, self-rated health, and psychological distress were not associated with adherence to COVID-19 protective behaviors.
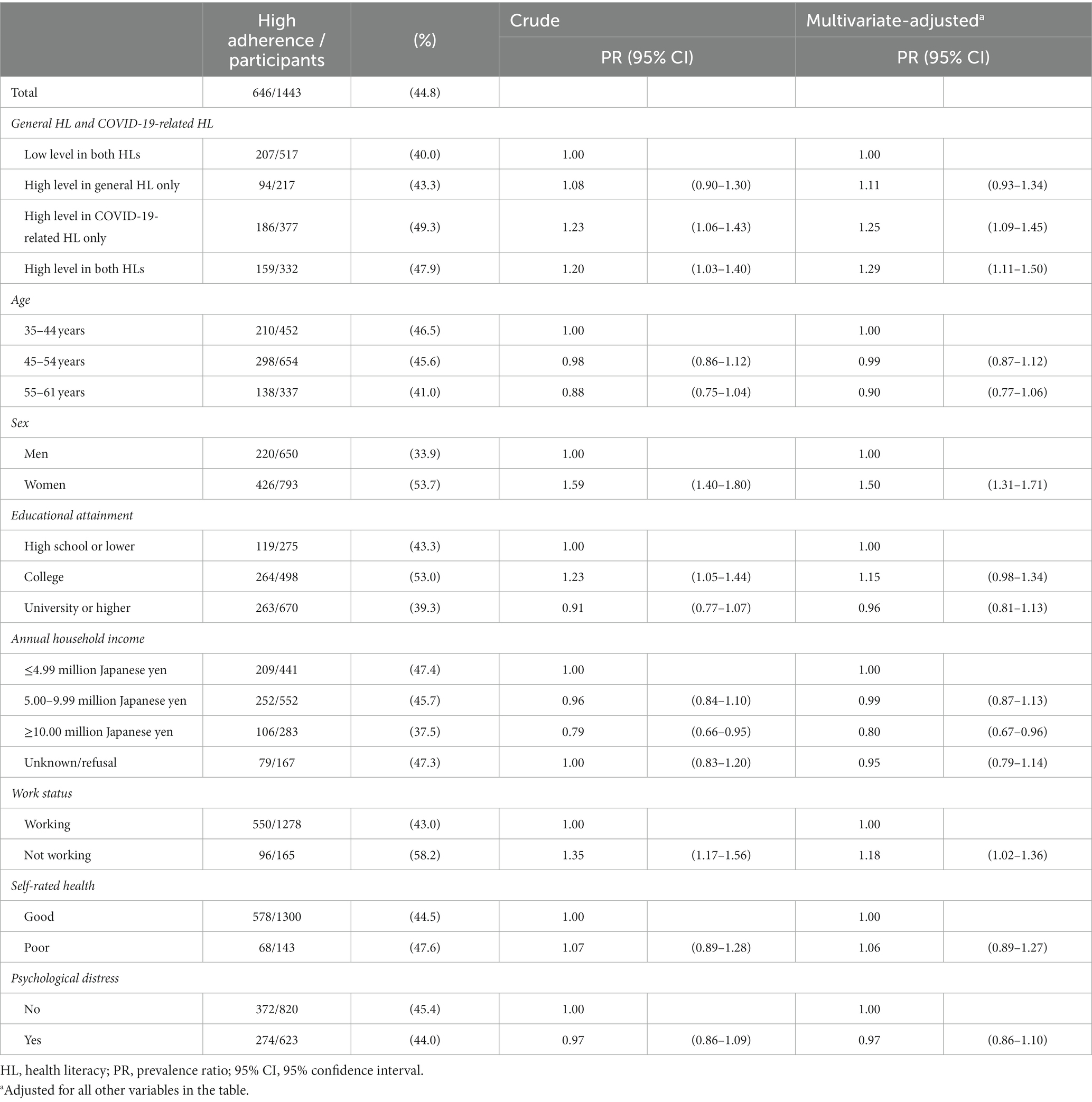
Table 2. Associations between combinations of general HL and COVID-19-related HL and high adherence to COVID-19 protective behaviors.
Table 3 presents the associations between combinations of general HL and COVID-19-related HL and healthy lifestyle behaviors. High level in general HL only, but not high level in COVID-19-related HL only, was associated with healthy and balanced diet; the multivariate-adjusted PRs were 1.49 (95% CI, 1.04–2.13) and 1.33 (95% CI, 0.97–1.81), respectively. High level in both HLs was associated with healthy and balanced diet; the multivariate-adjusted PR was 2.09 (95% CI, 1.57–2.79). High level in general HL only, but not high level in COVID-19-related HL only, was associated with adequate sleep; the multivariate-adjusted PRs were 1.46 (95% CI, 1.02–2.10) and 1.29 (95% CI, 0.94–1.76), respectively. High level in both HLs was associated with adequate sleep; the multivariate-adjusted PR was 1.83 (95% CI, 1.36–2.47). High level in general HL only, high level in COVID-19-related HL only, and high level in both HLs were associated with regular exercise; the multivariate-adjusted PRs were 2.00 (95% CI, 1.29–3.13), 1.57 (95% CI, 1.04–2.37), and 1.82 (95% CI, 1.21–2.75), respectively. Psychological distress was associated with low adherence to all three healthy lifestyle behaviors.
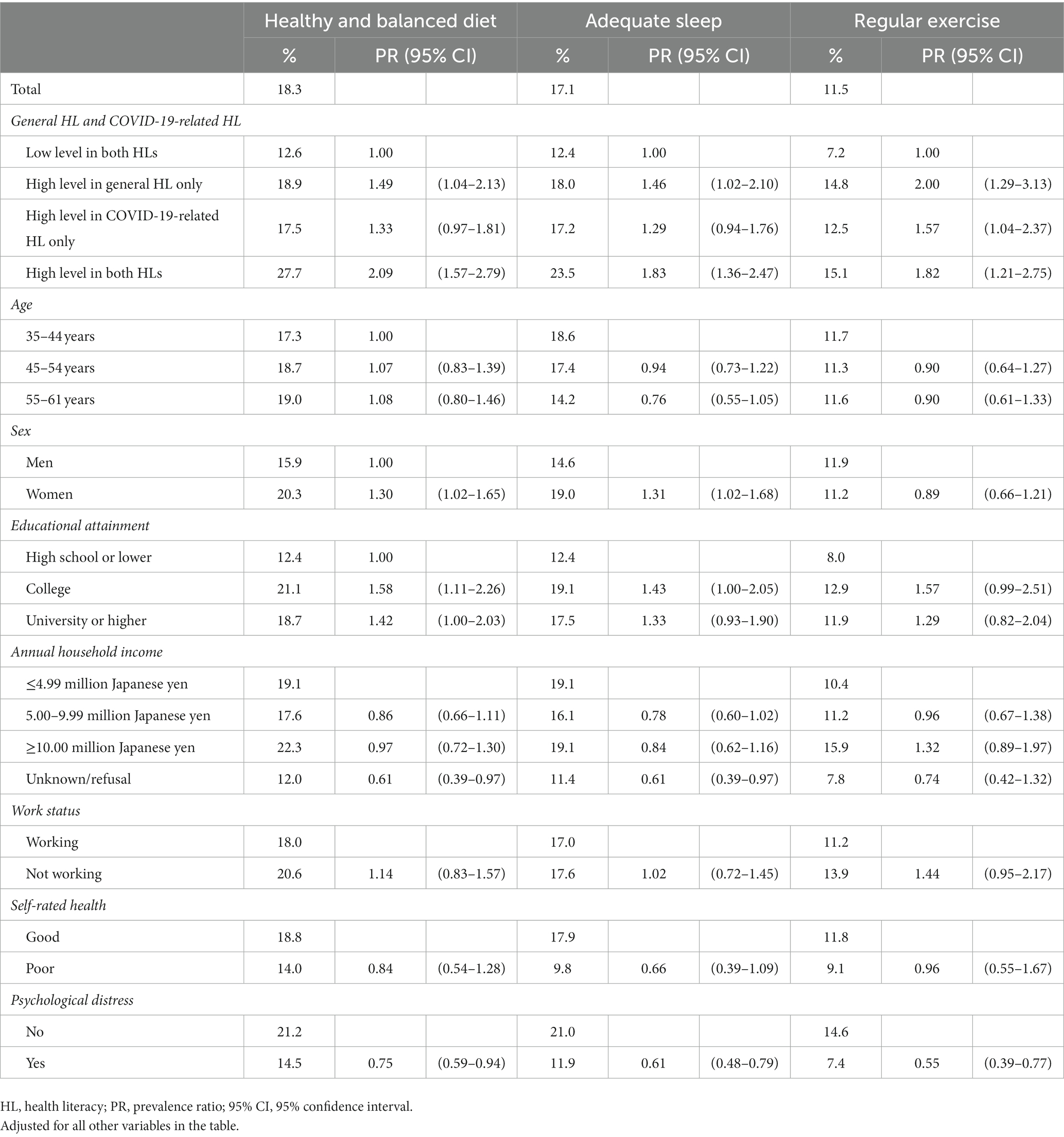
Table 3. Associations between the combination of general HL and COVID-19-related HL and healthy lifestyle behaviors.
Discussion
The present study examined the associations of combinations of general HL and COVID-19-related HL with COVID-19 protective behaviors and healthy lifestyle behaviors in Japan. High level in COVID-19-related HL only was associated with high adherence to COVID-19 protective behaviors, while high level in general HL only was associated with healthy and balanced diet, adequate sleep, and regular exercise.
High level in COVID-19-related HL only and high level in both HLs were associated with high adherence to COVID-19 protective behaviors. The situation during a newly emerging pandemic is typically characterized by urgency of actions, but is challenged by uncertain scientific knowledge and a high degree of complexity at all levels of action (31). Although the understanding of COVID-19 and its control are improving, there remains scientific uncertainty regarding many characteristics of the COVID-19 pandemic. Furthermore, COVID-19 is the first pandemic in history in which technology and social media are being used on a massive scale to keep people safe, informed, productive and connected (32). The technology we rely on to stay connected and informed is enabling and amplifying an infodemic—an overabundance of information—that continues to undermine the global response and jeopardizes measures to control the pandemic (32, 33). Therefore, it is a major challenge for individuals to integrate this sea of information into their personal behavioral actions (34). One review concluded that research should attempt to develop HL instruments that measure COVID-19-related HL (35). However, there are only a few COVID-19-related HL instruments (36, 37). One web-based study in Japan showing the association between high general HL measured by the Japanese version of the 47-item European health literacy survey questionnaire (HLS-EU-Q47) (38, 39) and COVID-19 protective behaviors stated that the assessment of HL may be inadequate to assess responses to pandemics caused by new viruses or infodemics because it may reflect the ability to cope with common diseases (16). One study found that domain-general and domain-specific abilities can influence the processing of information and subsequent adoption of behaviors distinctively (21). The present study showed that high level in COVID-19-related HL only, but not high level in general HL only, was associated with high adherence to COVID-19 protective behaviors. These findings indicate that general HL is insufficient for adherence to COVID-19 protective behaviors, whereas COVID-19-related HL is helpful in promoting adherence to COVID-19 protective behaviors even among individuals with low levels of general HL. Given this advantage of knowledge-based HL, it is speculated that optimal design of health messages is very important for supporting recipients’ comprehension of health information sufficiently to result in positive behavioral responses (40). Indeed, since the early phase of the COVID-19 pandemic, the Japanese government has used the following campaign slogan: “avoid the three Cs,” namely closed spaces with poor ventilation, crowded places with many people nearby, and close-contact settings such as close-range conversation. These clear messages regarding prevention of COVID-19 may partly explain the association between high level in COVID-19-related HL only and high adherence to COVID-19 protective behaviors.
High level in general HL only and high level in both HLs were associated with healthy lifestyle behaviors. Our finding is consistent with the finding of one study showing that high HL measured by the CCHL scale was associated with healthy lifestyles such as regular eating patterns and weekly exercise (25). It has been repeatedly reported that people with high HL are able to adequately understand and utilize health information in a way that protects and improves their health (41). High HL improves the health choices of individuals and their opportunities for certain health-related behaviors (42). The CCHL scale used in the present study explicitly attempts to assess critical HL in terms of information appraisal and ask respondents the extent to which they consider the reliability, validity, credibility and applicability of health information (25, 43). The present study also showed that high level in both HLs had the highest prevalences of high adherence to healthy lifestyle behaviors. Healthy lifestyle behaviors have been recommended since the start of the COVID-19 pandemic, because these behaviors affect the ability of the body to prevent, fight, and recover from infections and the stay-home request forces people to change their lifestyles (5). HL, as a social vaccine, acts as a means to understand and apply culturally appropriate and socially sensitive information about required protective behaviors to support the COVID-19 strategies of governments and health authorities (7). The combination of general HL and COVID-19-related HL can efficiently promote adherence to healthy lifestyle behaviors.
During the COVID-19 pandemic, concerns have repeatedly been raised about potential long-term damage to mental health (44). The present study showed associations between higher levels of HL and high adherence to COVID-19 protective behaviors as well as healthy lifestyle behaviors, even after adjustment for psychological distress. These findings indicate that the association between HL and adherence to protective behaviors cannot be explained by mental health alone. The present study further showed that psychological distress was associated with low adherence to healthy lifestyle behaviors, but not with adherence to COVID-19 protective behaviors. Different approaches are needed to promote adherence to COVID-19 protective behaviors and healthy lifestyle behaviors.
Participants with high level in both HLs were more likely to be men, be highly educated, and have higher income, and less likely to have psychological distress. Higher educational attainment is a strong precursor to higher general HL (45), which further leads to higher income status, especially in Japan, where education is a major factor affecting social stratification among men as bread winners, while women are less likely to undertake higher education (university bachelor’s degree or higher) (46). A higher level of general HL is reportedly associated with lower perceived risk of infection, higher compliance with appropriate protective behaviors, and lower risk of anxiety during the pandemic, even after adjusting for COVID19-specific knowledge (14).
The present findings have implications for promoting protective behaviors against COVID-19. Although vaccination delivery and roll-out have been in progress since 2021 in Japan, it is still possible to contract COVID-19 and spread it to others after being vaccinated. Therefore, people should continue to adhere to COVID-19 protective behaviors to keep themselves and others healthy. The observed associations of HL with COVID-19 protective behaviors and healthy lifestyle behaviors highlight the importance of HL for pandemic prevention and health maintenance. Because HL can be improved by education, it may be important to implement educational interventions during ordinary times, thus facilitating people to develop transferable skills in accessing, understanding, analyzing, and applying health information (47). However, it remains unclear how COVID-19-related HL can be improved. Therefore, governments and health authorities need to provide information on COVID-19 based on the level of COVID-19-related HL and also enhance general HL during ordinary times.
The present study has several limitations. First, the response rate was low. The participants of the J-SHINE survey in the first wave were comparable with the vital statistics of the target population in terms of age, sex, and educational attainment (22). However, the participants of the J-SHINE survey in the fourth wave were more likely to be older, be women, and highly educated than those who participated in the first wave but not in the fourth wave. Second, general HL was measured about 10 years before the COVID-19 pandemic. HL can change over time (48, 49), and one study showed that general HL declined significantly from immediately before the COVID-19 pandemic to 1 year later (47). However, the present study showed that high general HL was associated with healthy lifestyle behaviors, which is consistent with previous findings in Japan (25). Third, the reliability and validity of the questionnaire for COVID-19-related HL have not been verified. However, this questionnaire was adapted from validated questions (39). Fourth, the COVID-19 protective behaviors were self-reported, which is a source of uncertainty because participants may be influenced by social desirability bias.
In conclusion, the present study found that high level in COVID-19-related HL only was associated with high adherence to COVID-19 protective behaviors, while high level in general HL only was associated with healthy lifestyle behaviors. High level in both HLs showed the highest prevalence of high adherence to COVID-19 protective behaviors and healthy lifestyle behaviors. These findings indicate that consideration of both general HL and COVID-19-related HL could be useful for public health interventions to promote COVID-19 protective behaviors and maintain healthy lifestyle behaviors, with consequent preparation for possible future pandemics and public health crises.
Data availability statement
The datasets presented in this article are not readily available because of ethical consideration under written consent with the survey respondents. Requests to access the datasets should be directed to the last author.
Ethics statement
The Research Ethics Committee of The University of Tokyo, Graduate School of Medicine approved the survey procedure of the J-SHINE (Approval No. 3073). The J-SHINE Data Management Committee approved the secondary use of the data, with personally identifiable information deleted to ensure confidentiality. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KM conceived the study, performed the statistical analysis, and drafted the manuscript as the principal author. SK and HH provided advice regarding critically important intellectual content and helped to draft the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The J-SHINE survey was supported by a Grant-in-Aid for Scientific Research on Innovative Areas (grant number, 21119002) and a Grant-in-Aid for Scientific Research (A) (grant number, 18H04070) from the Ministry of Education, Culture, Sports, Science and Technology, Japan, and by a research grant from the Ministry of Health, Labour and Welfare, Japan (grant number, H27-Lifestyle-ippan-002). This work was supported by a Grant-in-Aid for Early-Career Scientists (grant number, 18K17397) and a Grant-in-Aid for Scientific Research (C) (grant number, 21K10490) from the Ministry of Education, Culture, Sports, Science and Technology, Japan. The funding sources played no role in study design, the collection, analysis and interpretation of data, the writing of the articles, or the decision to submit it for publication.
Acknowledgments
The authors thank the J-SHINE Data Management Committee for approving secondary use of the data. The authors also thank the reviewers for their valuable and insightful comments, which have improved the manuscript substantially.
Conflict of interest
KM is an employee of the Ministry of Education, Culture, Sports, Science and Technology, Japan.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hale, T, Angrist, N, Goldszmidt, R, Kira, B, Petherick, A, Phillips, T, et al. A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nat Hum Behav. (2021) 5:529–38. doi: 10.1038/s41562-021-01079-8
2. Bavel, JJV, Baicker, K, Boggio, PS, Capraro, V, Cichocka, A, Cikara, M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. (2020) 4:460–71. doi: 10.1038/s41562-020-0884-z
3. Jalloh, MF, Nur, AA, Nur, SA, Winters, M, Bedson, J, Pedi, D, et al. Behaviour adoption approaches during public health emergencies: implications for the COVID-19 pandemic and beyond. BMJ Glob Health. (2021) 6:e004450. doi: 10.1136/bmjgh-2020-004450
4. Yeoh, EK, Chong, KC, Chiew, CJ, Lee, VJ, Ng, CW, Hashimoto, H, et al. Assessing the impact of non-pharmaceutical interventions on the transmissibility and severity of COVID-19 during the first five months in the Western Pacific Region. One Health. (2021) 12:100213. doi: 10.1016/j.onehlt.2021.100213
5. World Health Organization . Advice for the public: coronavirus disease (COVID-19). (2020). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. (Accessed April 19, 2023).
6. GBD 2017 Risk Factor Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
7. Okan, O, Messer, M, Levin-Zamir, D, Paakkari, L, and Sørensen, K. Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot Int. (2023) 38:daab197. doi: 10.1093/heapro/daab197
8. Paakkari, L, and Okan, O. COVID-19: health literacy is an underestimated problem. Lancet Public Health. (2020) 5:e249–50. doi: 10.1016/S2468-2667(20)30086-4
9. Sørensen, K, Van den Broucke, S, Fullam, J, Doyle, G, Pelikan, J, Slonska, Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80
10. Nutbeam, D, and Muscat, DM. Health promotion glossary 2021. Health Promot Int. (2021) 36:1578–98. doi: 10.1093/heapro/daaa157
11. An, L, Bacon, E, Hawley, S, Yang, P, Russell, D, Huffman, S, et al. Relationship between coronavirus-related eHealth literacy and COVID-19 knowledge, attitudes, and practices among US adults: web-based survey study. J Med Internet Res. (2021) 23:e25042. doi: 10.2196/25042
12. Fukuda, Y, Ando, S, and Fukuda, K. Knowledge and preventive actions toward COVID-19, vaccination intent, and health literacy among educators in Japan: an online survey. PLoS One. (2021) 16:e0257552. doi: 10.1371/journal.pone.0257552
13. Guo, Z, Zhao, SZ, Guo, N, Wu, Y, Weng, X, Wong, JY, et al. Socioeconomic disparities in eHealth literacy and preventive behaviors during the COVID-19 pandemic in Hong Kong: cross-sectional study. J Med Internet Res. (2021) 23:e24577. doi: 10.2196/24577
14. Hermans, L, Van den Broucke, S, Gisle, L, Demarest, S, and Charafeddine, R. Mental health, compliance with measures and health prospects during the COVID-19 epidemic: the role of health literacy. BMC Public Health. (2021) 21:1365. doi: 10.1186/s12889-021-11437-w
15. McCaffery, KJ, Dodd, RH, Cvejic, E, Ayrek, J, Batcup, C, Isautier, JM, et al. Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Res Pract. (2020) 30:30342012. doi: 10.17061/phrp30342012
16. Nakayama, K, Yonekura, Y, Danya, H, and Hagiwara, K. COVID-19 preventive behaviors and health literacy, information evaluation, and decision-making skills in Japanese adults: cross-sectional survey study. JMIR Form Res. (2022) 6:e34966. doi: 10.2196/34966
17. Patil, U, Kostareva, U, Hadley, M, Manganello, JA, Okan, O, Dadaczynski, K, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. college students: implications for interventions. Int J Environ Res Public Health. (2021) 18:3301. doi: 10.3390/ijerph18063301
18. Rodon, C, Chin, J, and Chevalier, A. Assessing COVID-19 health literacy (CoHL) and its relationships with sociodemographic features, locus of control and compliance with social distancing rules during the first lockdown in France. Health Educ Res. (2022) 37:143–54. doi: 10.1093/her/cyac009
19. Sánchez-Arenas, R, Doubova, SV, González-Pérez, MA, and Pérez-Cuevas, R. Factors associated with COVID-19 preventive health behaviors among the general public in Mexico city and the state of Mexico. PLoS One. (2021) 16:e0254435. doi: 10.1371/journal.pone.0254435
20. Wong, JYH, Wai, AKC, Zhao, S, Yip, F, Lee, JJ, Wong, CKH, et al. Association of individual health literacy with preventive behaviours and family well-being during COVID-19 pandemic: mediating role of family information sharing. Int J Environ Res Public Health. (2020) 17:8838. doi: 10.3390/ijerph17238838
21. Chin, J, Morrow, DG, Stine-Morrow, EA, Conner-Garcia, T, Graumlich, JF, and Murray, MD. The process-knowledge model of health literacy: evidence from a componential analysis of two commonly used measures. J Health Commun. (2011) 16:222–41. doi: 10.1080/10810730.2011.604702
22. Takada, M, Kondo, N, and Hashimoto, H, J-SHINE Data Management Committee. Japanese study on stratification, health, income, and neighborhood: study protocol and profiles of participants. J Epidemiol. (2014) 24:334–44. doi: 10.2188/jea.JE20130084
23. Takagi, D, Yokouchi, N, and Hashimoto, H. Smoking behavior prevalence in one’s personal social network and peer’s popularity: a population-based study of middle-aged adults in Japan. Soc Sci Med. (2020) 260:113207. doi: 10.1016/j.socscimed.2020.113207
24. Fujii, K, and Hashimoto, H. Socio-psychological factors associated with anticipated stigma toward COVID-19: a cross-sectional study in Japan. BMC Public Health. (2023) 23:1245. doi: 10.1186/s12889-023-16159-9
25. Ishikawa, H, Nomura, K, Sato, M, and Yano, E. Developing a measure of communicative and critical health literacy: a pilot study of Japanese office workers. Health Promot Int. (2008) 23:269–74. doi: 10.1093/heapro/dan017
26. Nutbeam, D . Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
27. World Health Organization. Regional Office for Europe . Survey tool and guidance: rapid, simple, flexible behavioural insights on COVID-19. (2020). Available at: https://apps.who.int/iris/handle/10665/333549 (Accessed August 5, 2023).
28. Kessler, RC, Andrews, G, Colpe, LJ, Hiripi, E, Mroczek, DK, Normand, SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. (2002) 32:959–76. doi: 10.1017/S0033291702006074
29. Furukawa, TA, Kawakami, N, Saitoh, M, Ono, Y, Nakane, Y, Nakamura, Y, et al. The performance of the Japanese version of the K6 and K10 in the world mental health survey Japan. Int J Methods Psychiatr Res. (2008) 17:152–8. doi: 10.1002/mpr.257
30. Sakurai, K, Nishi, A, Kondo, K, Yanagida, K, and Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci. (2011) 65:434–41. doi: 10.1111/j.1440-1819.2011.02236.x
31. Abel, T, and McQueen, D. Critical health literacy in pandemics: the special case of COVID-19. Health Promot Int. (2021) 36:1473–81. doi: 10.1093/heapro/daaa141
32. World Health Organization . WHO public health research agenda for managing infodemics. Geneva: World Health Organization (2021).
33. Zarocostas, J . How to fight an infodemic. Lancet. (2020) 395:676. doi: 10.1016/S0140-6736(20)30461-X
34. Abel, T, and McQueen, D. Critical health literacy and the COVID-19 crisis. Health Promot Int. (2020) 35:1612–3. doi: 10.1093/heapro/daaa040
35. Matterne, U, Egger, N, Tempes, J, Tischer, C, Lander, J, Dierks, ML, et al. Health literacy in the general population in the context of epidemic or pandemic coronavirus outbreak situations: rapid scoping review. Patient Educ Couns. (2021) 104:223–34. doi: 10.1016/j.pec.2020.10.012
36. Falcón, M, Rodríguez-Blázquez, C, Fernández-Gutiérrez, M, Romay-Barja, M, Bas-Sarmiento, P, and Forjaz, MJ. Measuring COVID-19 health literacy: validation of the COVID-19 HL questionnaire in Spain. Health Qual Life Outcomes. (2022) 20:138. doi: 10.1186/s12955-022-02050-5
37. Okan, O, Bollweg, TM, Berens, EM, Hurrelmann, K, Bauer, U, and Schaeffer, D. Coronavirus-related health literacy: a cross-sectional study in adults during the COVID-19 infodemic in Germany. Int J Environ Res Public Health. (2020) 17:5503. doi: 10.3390/ijerph17155503
38. Nakayama, K, Osaka, W, Togari, T, Ishikawa, H, Yonekura, Y, Sekido, A, et al. Comprehensive health literacy in Japan is lower than in Europe: a validated Japanese-language assessment of health literacy. BMC Public Health. (2015) 15:505. doi: 10.1186/s12889-015-1835-x
39. Sørensen, K, Van den Broucke, S, Pelikan, JM, Fullam, J, Doyle, G, Slonska, Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European health literacy survey questionnaire (HLS-EU-Q). BMC Public Health. (2013) 13:948. doi: 10.1186/1471-2458-13-948
40. Chin, J, Payne, B, Gao, X, Conner-Garcia, T, Graumlich, JF, Murray, MD, et al. Memory and comprehension for health information among older adults: distinguishing the effects of domain-general and domain-specific knowledge. Memory. (2015) 23:577–89. doi: 10.1080/09658211.2014.912331
41. Berkman, ND, Sheridan, SL, Donahue, KE, Halpern, DJ, and Crotty, K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
42. Abel, T . Cultural capital in health promotion In: DV McQueen, I Kickbusch, and L Potvin, editors. Health and modernity: the role of theory in health promotion. New York: Springer (2007). 41–71.
43. Chinn, D . Critical health literacy: a review and critical analysis. Soc Sci Med. (2011) 73:60–7. doi: 10.1016/j.socscimed.2011.04.004
44. COVID-19 Mental Disorders Collaborators . Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
45. Stormacq, C, Van den Broucke, S, and Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot Int. (2019) 34:e1–e17. doi: 10.1093/heapro/day062
46. Murakami, K, Ohkubo, T, and Hashimoto, H. Distinct association between educational attainment and overweight/obesity in unmarried and married women: evidence from a population-based study in Japan. BMC Public Health. (2017) 17:903. doi: 10.1186/s12889-017-4912-5
47. Ishikawa, H, Kato, M, and Kiuchi, T. Declines in health literacy and health-related quality of life during the COVID-19 pandemic: a longitudinal study of the Japanese general population. BMC Public Health. (2021) 21:2180. doi: 10.1186/s12889-021-12092-x
48. Nutbeam, D, McGill, B, and Premkumar, P. Improving health literacy in community populations: a review of progress. Health Promot Int. (2018) 33:901–11. doi: 10.1093/heapro/dax015
Keywords: COVID-19, health literacy, healthy lifestyle behaviors, Japan, protective behaviors
Citation: Murakami K, Kuriyama S and Hashimoto H (2023) General health literacy, COVID-19-related health literacy, and protective behaviors: evidence from a population-based study in Japan. Front. Public Health. 11:1208815. doi: 10.3389/fpubh.2023.1208815
Edited by:
Graça S. Carvalho, University of Minho, PortugalReviewed by:
Jessie Chin, University of Illinois at Urbana-Champaign, United StatesAngela M. Goins, University of Houston–Downtown, United States
Copyright © 2023 Murakami, Kuriyama and Hashimoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keiko Murakami, bWtlaWtvLXRreUB1bWluLmFjLmpw
 Keiko Murakami
Keiko Murakami Shinichi Kuriyama
Shinichi Kuriyama Hideki Hashimoto3
Hideki Hashimoto3