- 1Fujian Provincial Center for Disease Control and Prevention, Fuzhou, Fujian, China
- 2Department of Preventive Medicine and Health Education, School of Public Health, Institute of Health Communication, Key Lab of Public Health Safety of Ministry of Education, Fudan University, Shanghai, China
- 3School of Journalism and Communication/National Media and Experimental Teaching Center, Jinan University, Guangzhou, China
- 4Duke Global Health Institute, Duke University, Durham, NC, United States
- 5Fudan Development Institute, Fudan University, Shanghai, China
Introduction: Human papillomavirus (HPV) infection, an important pathogenic factor for cervical cancer, can be prevented by the HPV vaccine. Health care provider (HCP) recommendations contribute to improve HPV vaccination coverage. The aim of this study was to assess the frequency of HCP recommendations for HPV vaccination and associated factors.
Methods: From Nov 8 to Dec 6 in 2018, a cross-sectional study was conducted through online questionnaires among HCPs (n = 1,371) from hospitals in three large cities in China (Shanghai, Guangzhou, and Shenzhen). Data on demographic characteristics, the frequency of HPV vaccination recommendations, HPV knowledge and related attitudes were collected through the questionnaires.
Results: Among 1,371 participants, only 30.2% reported that they frequently recommended HPV vaccination. Multivariate analyses indicated that female sex, being employed in obstetrics or gynecology departments and community health service centers, and having higher self-reported and actual knowledge of HPV were factors associated with a higher recommendation frequency. Factors including a self-perceived non-obligation to provide recommendations and difficulties in discussing sexual topics were significantly correlated with less frequent recommendations. Employment in a community health service center (OR = 2.068, 95% CI: 1.070–3.999) was the strongest factor associated with the frequency of HCPs’ recommendations for HPV vaccination.
Discussion: The frequency of HCPs’ recommendations for HPV vaccination in China was much lower than that in many developed countries. To enhance the recommendation frequency, medical institutions should help HCPs gain more knowledge of HPV and master communication skills. At the same time, the government should take measures to enhance the accessibility of HPV vaccines. The media should help to alleviate people’s concerns and encourage them to face up sexual health.
1. Introduction
As the fourth most common cancer among women, cervical cancer is estimated to have caused 342,000 deaths globally and 59,060 deaths in China in 2020 (1, 2). Two types of human papillomavirus (HPV) (16 and 18) are responsible for almost 50% of high-grade cervical pre-cancers (1). To protect people from high-risk or oncogenic HPV infection, vaccination against HPV is the primary preventive comprehensive cervical cancer control measure in the global strategy (3). However, as of 2020, the estimated full-series cumulative HPV vaccination coverage rate was only 2.24% among females between 9 and 45 years old in China (4), while the global coverage rate of the final HPV dose was estimated at 15% (5). There seems to be a vast distance for HPV vaccination coverage in China to keep up with global coverage.
There have been great challenges in HPV vaccination since the vaccine was approved in mainland of China in 2016. First, as a preventive treatment, HPV vaccination was not covered by health insurance in most cases (6, 7). Additionally, the costs of HPV vaccines in China are high for the public (7), ranging from RMB 987 (2vHPV, Cecolin) to RMB 3910 (9vHPV, Gardasil®9), which raises questions about their cost-effectiveness (7, 8). Even so, HPV vaccine supplies are inadequate. Sometimes people have to wait for a long time, even up to 2 years, to make an online appointment for vaccination (7, 9). In addition, HPV vaccination has been culturally constructed as an indicator of females’ sexual morality to some extent in China. It is sometimes seen as encouragement for promiscuity and a necessity for those engaged in promiscuous sexual activities (8).
As opinion leaders on the topic of health, health care providers (HCPs) play an important role in HPV vaccination (10). Females who received a strong recommendation from an HCP were 4 times more likely to receive the HPV vaccine than those who received a weak recommendation (11). However, too strong HPV vaccine recommendation may also have negative effects on the patient vaccination rate. If HCPs show too much enthusiasm in their recommendations, patients might be suspicious of their motives, especially when the HPV vaccine is self-paid and expensive (8).
To date, although many studies have explored HCPs’ willingness to recommend HPV vaccines in China (12–14), the frequency of recommendation has rarely been considered. Compared with recommendation intentions, the actual recommendation frequency is a better measure of HCPs’ recommendation behaviors, reflecting the comprehensive influence of the environment, HCP abilities and doctor–patient communication.
Factors influencing HCPs’ recommendations are complicated. The existing studies in China have mainly focused on the impact of HCPs’ knowledge on recommendations (12–14). However, the influences of other factors, such as difficulty communicating with patients regarding sexual topics and whether HCPs realize that recommending vaccinations is their responsibility, remain unknown. Understanding and improving HCPs’ communication, particularly with regard to recommendations for HPV vaccination, has both theoretical and practical significance. Our study aimed to assess the frequency of HCPs’ recommendations for HPV vaccination and explore its related factors. These findings are expected to provide guidance for targeted measures that could enhance the frequency of HCPs’ recommendations for HPV vaccination, which is imperative to increasing HPV vaccination coverage in China.
2. Materials and methods
2.1. Study design and implementation
This multicenter cross-sectional study was conducted in Shanghai, Guangzhou, and Shenzhen, China. All of these cities are located in coastal areas with advanced economies and superior medical resources. The rapid development in Shanghai, as China’s economic and trade center, made new health policies and products more acceptable. Before the HPV vaccine was officially approved in mainland of China, HPV vaccination was already available in Hong Kong and Macao, which are geographically close to Shenzhen and Guangzhou. Thus, HCPs in Shanghai, Shenzhen and Guangzhou might have more communication regarding HPV and vaccination than those in other cities in China. The selection of these three cities could help us investigate more factors related to HCPs’ recommendations for HPV vaccination.
Purposive sampling was used in this study. We chose 13 third-class general hospitals in the three cities (4 in Shanghai, 6 in Shenzhen, and 3 in Guangzhou). In addition, we chose 4–6 districts in each city. Maternal and child hospitals in each district were invited to participate in our study. Community health centers in each city were purposively selected, with an average of approximately 10, covering the different geographic locations and representing the different economic levels of the city. In total, we selected 20 maternal and child health hospitals, 29 community health centers and 13 general hospitals.
Physicians and nurses who worked in obstetrics and gynecology, preventive health care, pediatrics and general medicine departments in the above institutions were mainly invited to the survey. Females between 9 and 45 years old were the target people for HPV vaccination. Consultation regarding HPV vaccination was mainly provided by gynecologists and pediatricians. Besides, HPV vaccine is usually provided by community health service centers, while preventive health care and general medicine departments were the important departments in HPV vaccination administration. Thus, we selected HCPs from these departments for they were more closely related to HPV vaccination.
So far, there is no similar research in China. Although there are more than a dozen foreign literatures on this topic, the results of other countries may not be applicable considering the unique social background of China. Therefore, the proportion of frequent vaccination recommendations in HCPs is estimated at 50% to achieve the most conservative sample size. Assuming an alpha error of 5%, an allowable error of 0.04, and a 70% response rate, the target minimum sample size is calculated to be 858. To ensure that the minimum sample size was reached, we planned to obtain at least 15 providers from each institution. For institutions with fewer than 15 HCPs, all eligible HCPs were invited to participate in the survey.
This study was conducted through online anonymous questionnaires by the Wenjuanxing platform (a popular online survey platform in China, available at: https://www.wjx.cn/app/survey.aspx) from November 8 to December 6 in 2018. Each participating hospital had a contact person. After receiving the online questionnaire link from the study team, the contact person sent the link to each participant. During the survey period, the HCPs who received the link could open the questionnaire and complete the survey. In total, 1,616 HCPs were invited for the survey, and 1,396 (86.4%) questionnaires were returned. Questionnaires were identified valid if they: (1) Took more than 2 min to complete the survey; (2) The question about common sense was answered correctly (Question: What is the capital of China? Correct answer: Beijing); (3) No obvious conflicts between the answers. After information sorting and cleaning, 25 (1.8%) participants were excluded in the current study. We used the STROBE cross sectional reporting guidelines to make sure that our study included all the items needed for survey reporting (Supplementary material 1) (15). This study was approved by the institutional review board of the School of Public Health, Fudan University (IRB#2018-04-0677-B).
2.2. Measures
There were totally 32 questions in the questionnaire, which could be divided into four sections including demographic information, frequency of HPV vaccine recommendation, knowledge of HPV and attitudes toward HPV-related topics (Supplementary material 2).
2.2.1. Frequency of HPV vaccine recommendations
The frequency of HPV vaccine recommendations was measured by the following question: “How often have you recommended HPV vaccination for age-appropriate patients in the past 3 months?” The response options included (1) never, (2) seldom, (3) sometimes, (4) usually and (5) always. For our analyses, we dichotomized the responses, combining the “usually” and “always” responses (frequent recommendation of HPV vaccines) versus the combination of all other responses (infrequent recommendation of HPV vaccines) (16, 17).
2.2.2. Covariates
Demographic information, knowledge of HPV and attitudes toward different HPV-related topics were measured as covariates. The demographic information included sex, age, occupation (physician, nurse), department (obstetrics and gynecology, preventive health care, pediatrics, general medicine and others), title (primary, intermediate, senior), hospital type (community health service center, maternal and child hospital, general hospital), and city (Shanghai, Guangzhou, Shenzhen).
Knowledge of HPV included actual and self-reported knowledge. The actual knowledge refers to one’s knowledge of HPV and HPV vaccine in actual. It was measured by 10 HPV-related questions; every question was multiple-choice, and there was only one correct answer. The actual knowledge score was calculated by summing the number of correct responses to the questions. The self-reported knowledge is how much the HCPs think themselves know about HPV, cervical cancer and HPV vaccine. We designed three questions to assess self-reported knowledge of HPV, cervical cancer and HPV vaccination. Detailed information on the survey questions is shown in the Supplementary material 2 (Section III).
Based on a literature review and considering the Chinese context and general views from a previous discussion with HCPs, we formulated eight items on attitudes toward different HPV-related topics. These topics encompass HCPs’ self-perceived lack of obligation to recommend vaccines, apprehensions about being perceived as pushy salespeople, beliefs that their patients face a low risk of HPV infection and related diseases, skepticism towards the HPV vaccine, and difficulty in discussing sensitive sexual topics. Detailed information on the related survey questions, variable descriptions and processing is shown in the Supplementary material 2 (Section IV).
2.2.3. Concerns and difficulties in discussing HPV/sexual topics with patients
Difficulty in discussing HPV/sexual topics with patients or parents of young patients may decrease the frequency of HCPs’ recommendations for HPV vaccination. For HCPs who reported having discussions with patients or parents of young patients about HPV vaccines, two additional probing questions were asked regarding patients’ concerns about HPV vaccines and the difficulties in discussing sexual topics with parents of young patients (Supplementary material 2, Section V).
2.3. Statistical analysis
Frequencies and proportions are reported for HCPs’ HPV vaccine recommendations. The median and interquartile ranges (IQR) are reported for the knowledge of HPV and the attitudes toward different HPV-related topics. The Chi-square tests was used to explore the association between demographic characteristics and HPV recommendation frequency. Internal consistency reliability was assessed by calculating Cronbach’s α coefficient for self-reported knowledge of HPV, low risk of infection/disease and skepticism regarding the HPV vaccine. Multivariate logistic regression analyses were performed to assess the association between the potential influencing factors and the frequency of HPV vaccine recommendations after controlling for related characteristic covariates. Adjusted odds ratios (ORs) and their 95% confidence intervals (CIs) were used to quantify the effects. IBM SPSS software version 20.0 (SPSS, Inc., Chicago, Illinois, US) was used to carry out all analyses. All tests were two-sided, and p < 0.05 was considered statistically significant.
3. Results
3.1. Descriptive statistics
3.1.1. Demographic characteristics and HPV vaccine recommendation frequency
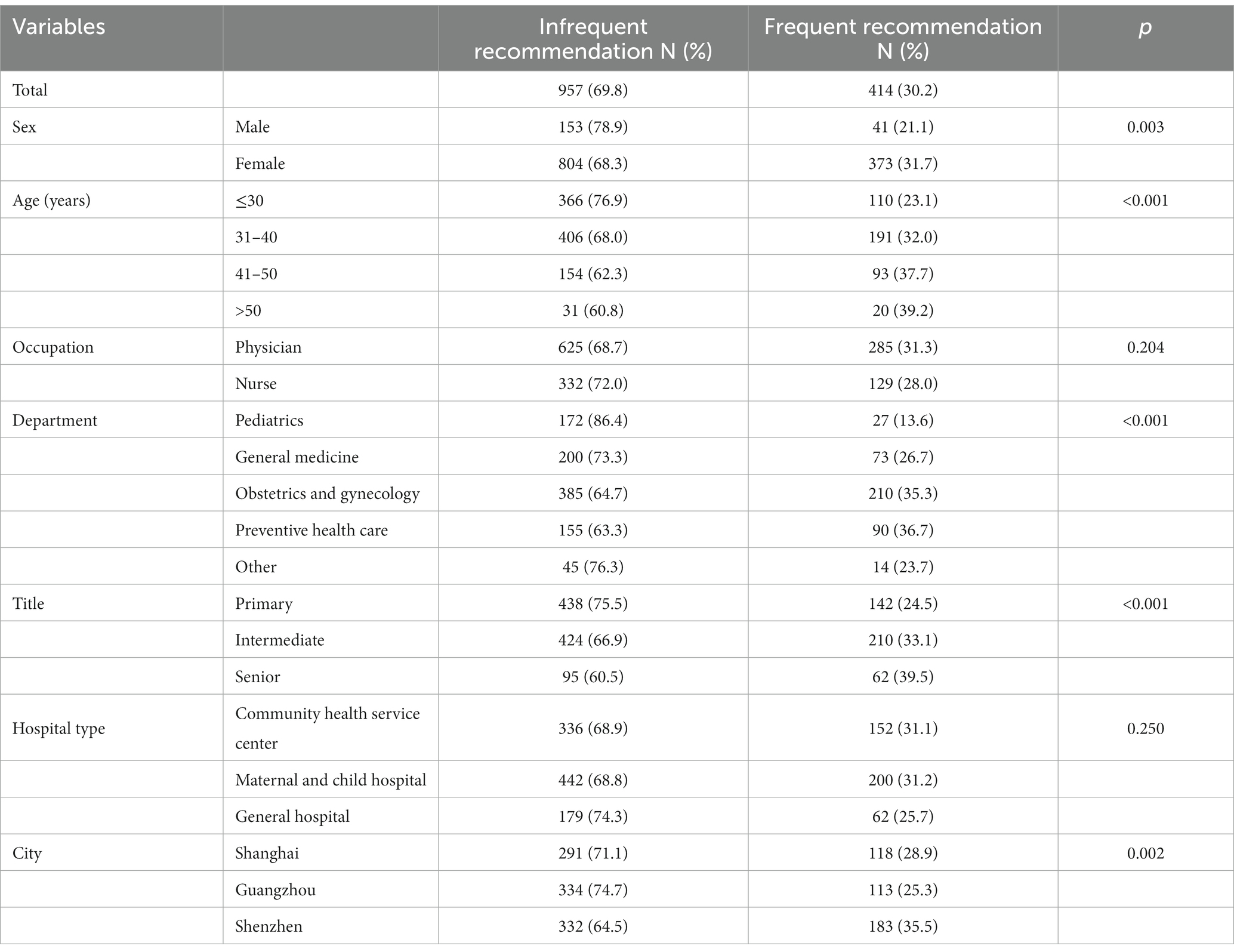
Among 1,616 HCPs who were invited, 1,396 (86.4%) participated the survey with 1,371 (98.2%) valid questionnaires. Among those valid participants, 1,177 were female (85.8%), and 194 were male (14.2%), with an average age of 34.9 ± 8.0 years. The occupations of the participants were physicians (66.4%) and nurses (33.6%). Almost half of the participants (43.4%) worked in obstetrics and gynecology departments, and 17.9% worked in preventive health care departments. Most participants’ titles were primary (42.3%) and intermediate (46.2%). A total of 46.8% of the participants worked in maternal and child hospitals, and 35.6% worked in community health service centers (Table 1).
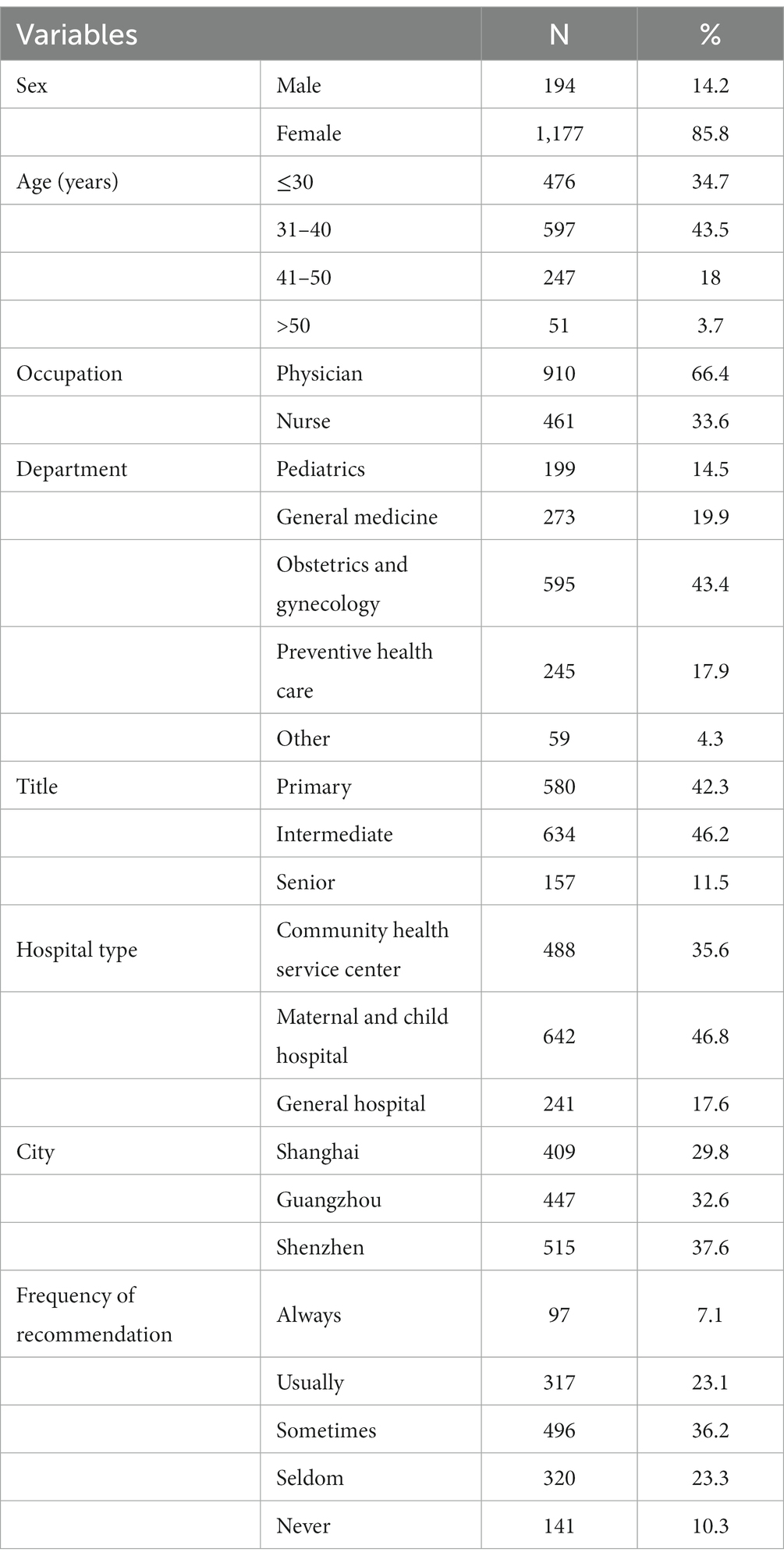
Table 1. Demographic information and the frequency of recommending HPV vaccination among participants.
The number of participants who never, seldom and sometimes recommended HPV vaccination to their patients was 141 (10.3%), 320 (23.3%) and 496 (36.2%), respectively, and all of them were categorized as infrequently recommending HPV vaccination (957, 69.8%). A total of 23.1% of the participants reported that they usually recommend HPV vaccines, and 7.1% reported always recommending HPV vaccines; all of them were categorized as frequently recommending HPV vaccines (414, 30.2%) (Table 1). The univariate analysis showed that gender, age, city of the HCPs, departments as well as their working titles were associated with the frequency of HPV vaccine recommendation (Table 2).
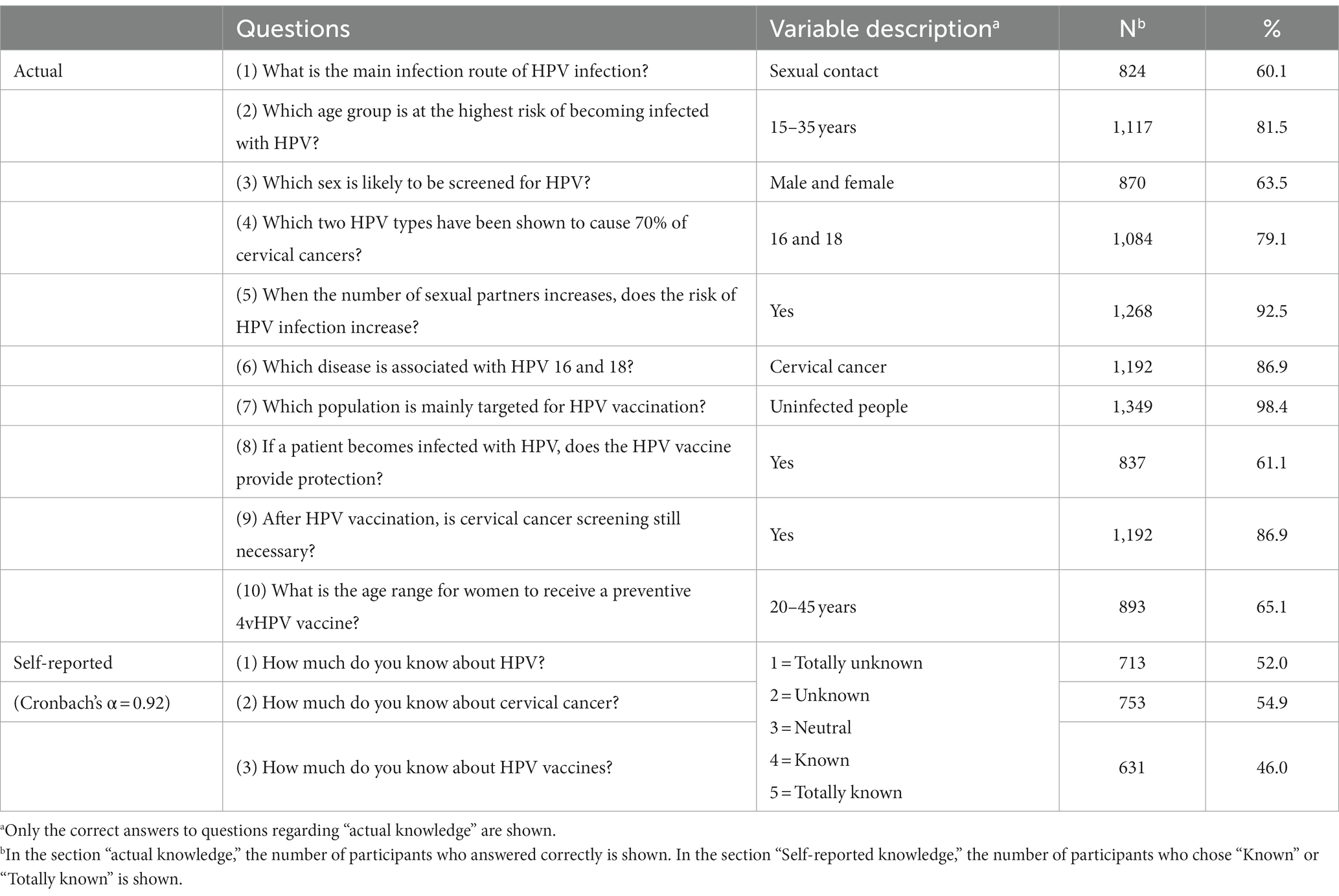
3.1.2. Knowledge of HPV
For the knowledge of HPV, the actual HPV knowledge score ranged from 0 to 10 points, with a median score of 8.00 (IQR: 7.00–9.00). The self-reported knowledge of HPV score ranged from 1 to 5 points, with a median score of 3.33 (IQR: 2.67–4.00). The Cronbach’s α coefficient of the self-reported knowledge of HPV was 0.92. The description of the rate of each answer for actual and self-reported HPV knowledge was as following (Table 3).
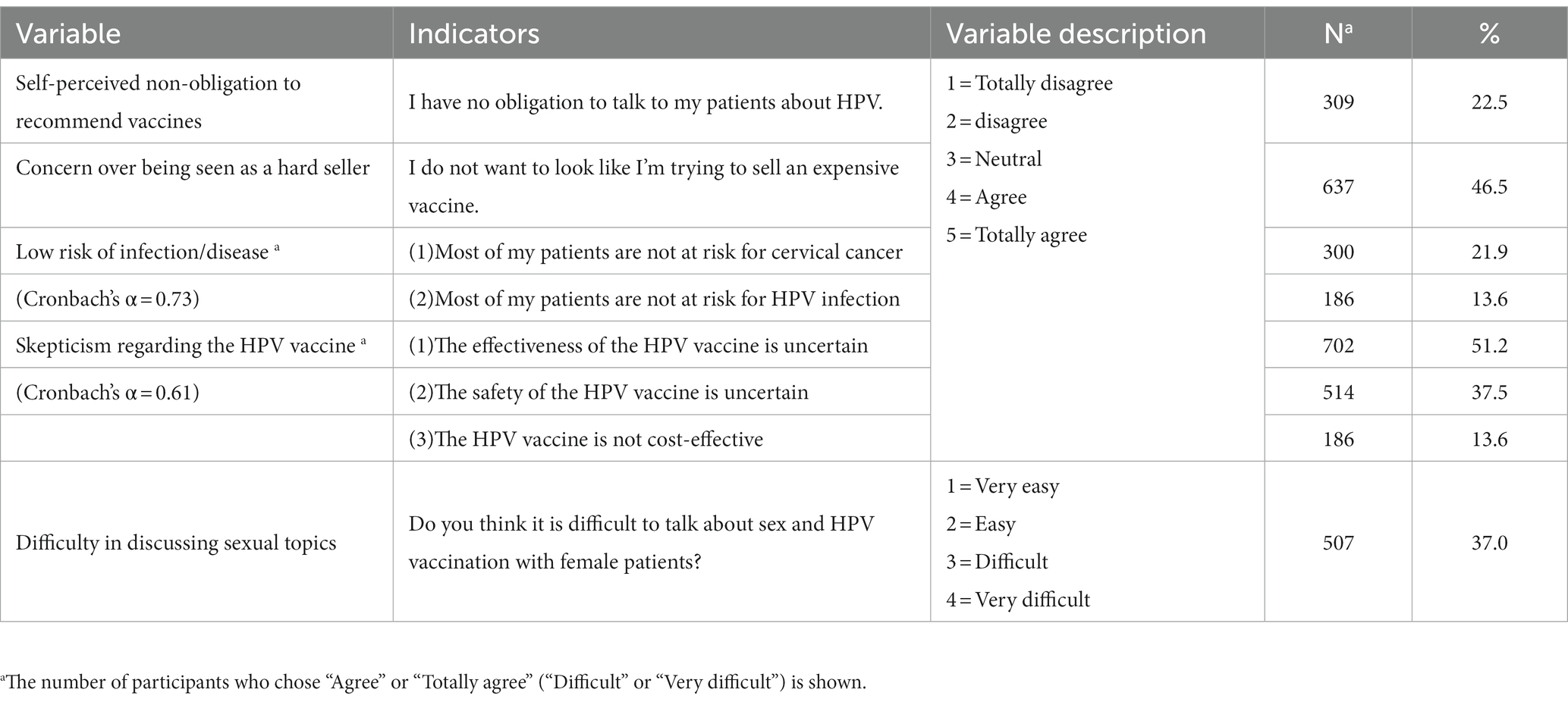
3.1.3. Attitudes toward different HPV-related topics
Apart from difficulty in communicating regarding sexual topics (scores ranging from 1 to 4), the scores of the other variables ranged from 1 to 5 (Table 4). The median score of perceived non-obligation to recommend vaccines was 3.00 (IQR: 2.00–3.00); the median score of concern over being seen as a hard seller was 3.00 (IQR: 3.00–4.00); and the median score for low risk of infection/disease was 2.50 (IQR: 2.00–3.00). Skepticism regarding the HPV vaccine had a median score of 3.00 (IQR: 2.67–3.33). The median score of difficulty in discussing sexual topics was 2.00 (IQR: 1.00–3.00). The Cronbach’s α coefficient of both of low risk of infection/disease and skepticism regarding the HPV vaccine was higher than 0.60.
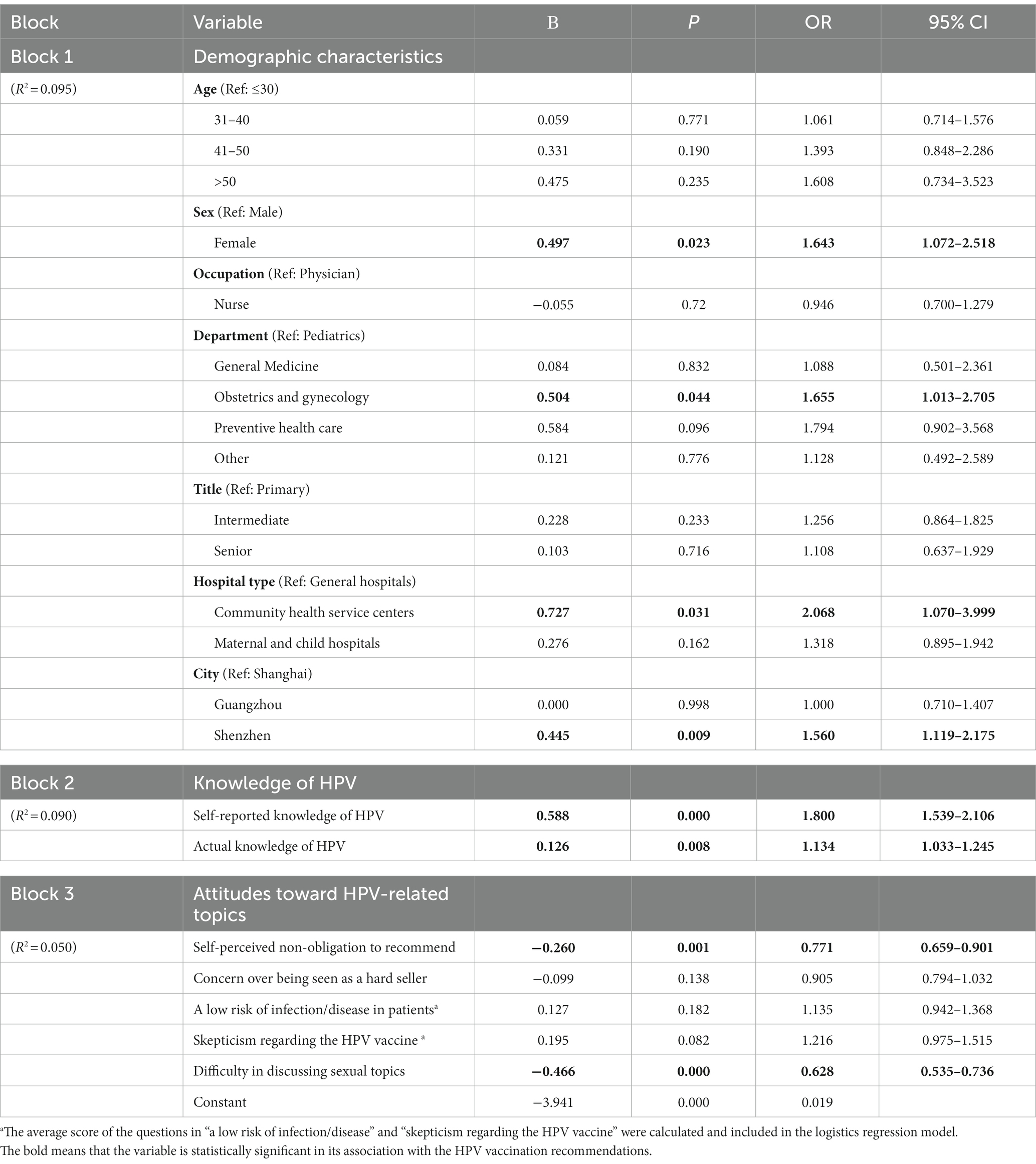
3.2. Association of the frequency of HPV vaccine recommendations with influencing factors
With infrequent HPV vaccination recommendation as a reference, logistic regression analyses revealed the following (Table 5): Comparing to male HCPs, female HCPs were more likely to recommend HPV vaccines to their patients (OR = 1.643, 95% CI: 1.072–2.518); HCPs working in obstetrics and gynecology departments (OR = 1.655, 95% CI: 1.013–2.705) recommended HPV vaccination more frequently than those working in pediatric departments. Compared to general hospitals, in community health service centers, the intention to frequently recommend HPV vaccination was higher (OR = 2.068, 95% CI: 1.070–3.999). HCPs who worked in Shenzhen were more likely to recommend HPV vaccine than HCPs in Shanghai (OR = 1.560, 95% CI: 1.119–2.175).
Knowledge and attitude of HCPs also influenced the frequency of recommendations. Participants who had higher self-reported and actual knowledge of HPV recommended HPV vaccination more frequently (OR = 1.800, 95% CI: 1.539–2.106; OR = 1.134, 95% CI: 1.033–1.245). In contrast, for HCPs who perceived no obligation to recommend vaccination (OR = 0.771, 95% CI: 0.659–0.901) or experienced difficulty in discussing sexual topics with their patients (OR = 0.628, 95% CI: 0.535–0.736), the frequency of recommendation decreased. The total Nagelkerke R2 of this logistic regression was 0.235.
3.3. Concerns and difficulties in discussing HPV/sexual topics with patients
Many HCPs thought that their patients worried about the efficacy (37.5%) and safety (32.5%) of the HPV vaccine. In addition, 13.7% of the participants claimed that it was difficult for patients to receive HPV vaccines. The majority of participants found that parents of young patients were unwilling to start a sex-related conversation with their children (63.5%). A total of 38.0% of the participants thought that parents regarded sexually transmitted diseases (STDs) as rarely occurring in children. More detailed information was listed in Table 6.
4. Discussion
This study is among the first studies that evaluated the frequency of HCPs’ recommendations for HPV vaccination in China. Moreover, we verified the association of HCPs’ knowledge of HPV and attitudes toward various HPV-related topics with their recommendations for HPV vaccination. All of the above findings provided in-depth evidence explaining the low prevalence of frequent recommendations for HPV vaccination. The findings also provide theoretical evidence for exploring approaches to enhance the frequency of HPV vaccine recommendations by Chinese HCPs and achieve high HPV vaccination coverage to realize the goal of “zero” cervical cancer cases.
In this study, less than one-third of Chinese HCPs frequently recommended HPV vaccination, which is much lower than the recommendation (always or usually) made by HCPs in the United States (79.0%) and France (72.4%) (16, 17). With HPV vaccines having been approved for more than 10 years, the low frequency of HCPs’ recommendations in China is a cause for public health concern. However, in a prior national survey with only two answer options (willing and unwilling), 94.8% of the Chinese HCPs claimed that they were willing to recommend HPV vaccination to their patients (14), indicating the large gap between willingness and actual recommendations which further highlights the importance of exploring factors that influence recommendations.
According to our findings, female HCPs were more likely than male HCPs to frequently recommend HPV vaccination in China. Because female HCPs may pay more attention to cervical cancer as a women’s health issue, they may be more flexible in dealing with sexual health issues (18, 19). In terms of departments, the frequency of recommendations made by obstetrician-gynecologists is higher than that of pediatricians because obstetrician-gynecologists not only know the potential health effects of HPV infection but also take responsibility for offering primary health care services for women of childbearing age (20, 21). Ensuring frequent recommendations by both obstetricians-gynecologists and pediatricians is equally essential, as girls aged between 9 and 15 years old are an important target population for HPV vaccination. To achieve a higher frequency of HPV vaccination recommendations, more attention should also be paid to male HCPs, especially those who work in pediatric departments.
Knowledge of HPV played a key role in the low frequency of HPV vaccine recommendations (12, 22), which was also the most powerful block in our logistic regression model. Both actual and self-reported HPV knowledge could enhance the recommendation intentions of HCPs (12, 23–25). The actual knowledge of HPV reflected whether an HCP knew the risks of HPV infection and the protective effect of the HPV vaccine. In a previous study, the low knowledge level was the primary reason for unwillingness to recommend HPV vaccination in Western China (12). The self-reported knowledge reflected self-efficacy that HCPs believe themselves having enough knowledge to discuss with their patients about HPV vaccine (26). In addition, HCPs with higher self-reported knowledge could communicate the benefits of the HPV vaccine clearly and confidently and address their patients’ doubts regarding the HPV vaccine (27). Thus, it is necessary to provide HCPs with HPV-related training to improve not only their actual knowledge but also their self-reported knowledge, which is essential to increase their self-efficacy in discussing relevant topics with patients.
According to the WHO strategy, every HCP has the duty to ensure that women and adolescents receive the health services they need, including HPV vaccination (3). It is an HCP’s obligation to recommend the HPV vaccine to their patients (28, 29). However, almost one quarter (22.5%) of the HCPs still agreed with the viewpoint that “they had no obligation to talk to their patients about HPV.” Consultations with doctors in China mainly involved discussions regarding disease and treatment methods rather than preventive measures (8). This could partly be attributed to the lack of preventive medicine knowledge in clinical education (30). Previous studies indicated that the proportion of preventive medicine curricula, such as HPV vaccines, was insufficient in current clinical medicine training programs, which led to HCPs’ poor awareness of disease prevention (30, 31).
According to HCPs, one of the concerns patients have about HPV vaccines in China is the accessibility of vaccines. Because Shenzhen is the nearest city to Hong Kong, it is convenient for people in Shenzhen to go to Hong Kong to get HPV vaccination. Thus, HCPs in Shenzhen were more likely to recommend vaccine. As one important source of HPV vaccine supplements, the frequency of HCPs’ recommendations in community health service centers was higher than that of HCPs in general hospitals. Only HCPs in preventive health care department were permitted to prescribe the vaccine for their patients in China (32). The vaccine supply was derailed between general medicine and vaccination departments. In addition, approximately half of the participants stated that they did not want to seem like a hard seller of HPV vaccines, especially when the costs of vaccines were very high. Patients have to wait for a long time and pay a high price for the HPV vaccine (7, 33). The low frequency of HCPs’ recommendations may be partly due to the time and financial cost of the vaccine.
In view of the sex symbolic meaning of the HPV vaccine, difficulty in communication with patients regarding sexual topics is also a barrier (8). Sexuality is a sensitive and private topic related to moral and culture in China, whereas traditionally, people can only obtain limited education related to sex from family members and school (34, 35). Individuals from conservative social backgrounds often perceive sex as shameful or guilt-inducing, leading them to avoid open discussions on this topic (36). When talking about sex with someone from a conservative social background, especially children and their parents, HCPs may fear offending their patients and avoid talking about HPV-related topics (24, 25, 36, 37). The “unwillingness to start a sex-related discussion with children” and “vaccination is a social stigma associated with STDs” became the main reasons for the difficulties in discussing sexual topics with parents of young patients. Furthermore, HCPs may assume that young people from a conservative social background are less likely to engage in high-risk sexual behaviors and therefore have a lower risk of HPV exposure (24). Thus, they may think that it is not necessary to recommend HPV vaccination (38). In fact, the number of people who have high-risk sexual behaviors such as multiple sexual partners is increasing and their age is getting younger in China (39). This underscores the fact that minors are also at high risk of HPV infection (39–41).
The frequency of HCPs’ recommendations played an important role in HPV vaccination coverage. First, medical institutions should hold regular training to increase HCPs’ knowledge of HPV and help them realize their responsibility in practicing clinical preventive medicine, including recommending HPV vaccination to patients. The preventive medicine curriculum in clinical medicine training programs needs to be strengthened to promote the concept of putting prevention first and the integrated development of preventive medicine and clinical medicine (30, 31).
To cope with the difficulties in communicating with patients regarding HPV/sexual topics, the “provider-driven” and “bundling” recommendation styles were suggested by the Centers for Disease Control and Prevention (CDC) and the American Academy of Family Physicians (AAFP), respectively (42–44). These recommendation styles require the HCPs to inform patients that they should receive the HPV vaccine at an appropriate age and bundle the HPV vaccine with routine immunization (45). In addition, regardless of prior exposure to HPV and sexual activity, HCPs should be reminded to provide recommendations for all patients of appropriate age, not just those perceived to be “at risk” (29, 44).
To enhance the accessibility of HPV vaccines, the range of institutions that have the right to supply HPV vaccines should be expanded, not just community health centers. The American College of Obstetricians and Gynecologists (ACOG) suggested that the HPV vaccine could be stocked and administered by clinicians in clinics when feasible (29). This will make HCPs take part in vaccination deeply, not just as advisors. For children, a school-based HPV vaccine recommendation system with the cooperation of HCPs may be suitable and effective (46). In addition, expanding access to HPV vaccination is also essential. Possible solutions include single-dose vaccination, low-cost domestic vaccines, and co-administration with other vaccines for adolescents (47). Whether the domestic HPV vaccine should be included in the publicly funded Expanded Program on Immunization (EPI) requires more cost-effectiveness tests in China (33).
The media plays an important role in recommending HPV vaccination to the public. More information about the HPV and HPV vaccine should be delivered to the public through media. The effectiveness and safety of HPV vaccines have become the greatest concerns of patients. The media could track and provide real-time data about the effectiveness and safety of HPV vaccines to alleviate the concerns of the public. Moreover, the media should also call for people to face up sexual health topics and promote correct sexual health education, especially for those from a conservative social background and those having active sexual behaviors (48), which could help reduce the difficulties for HCPs in communication regarding sexual topics.
There are still a few limitations in this study. First, as a cross-sectional study, the causal relationship between the frequency of recommendations and associated factors remains uncertain. Second, the participants in this study were mostly from developed cities within China which is different from other cities in China and other countries in terms of cultures and health policy. The sample may not be representative of HCPs throughout China, and the results may overestimate the frequency of recommendations. Furthermore, all data collected in this study were self-reported and the HPV recommendation frequency was measured in subjective terms which may generate information bias. Further research may use longitudinal approaches and more objective measures across the country to explore factors influencing the frequency of recommendations in China.
5. Conclusion
In conclusion, our study showed that the frequency of HCPs’ recommendations for HPV vaccination is relatively low in China. This could be partly attributed to the lack of HCPs’ knowledge of HPV and HPV vaccine. The difficulty in discussing sexual topics and the sense of having no obligation to recommend vaccines are also barriers to HCPs’ recommendations. It is essential to enhance HCPs’ knowledge of HPV and help them master the skills to communicate with patients about sexual health and HPV vaccination. The government should take measures to enhance the accessibility of HPV vaccines. The media should provide accurate information about the vaccines to alleviate people’s concerns and encourage them to face up sexual health topics.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the institutional review board of the School of Public Health, Fudan University (IRB#2018-04-0677-B).
Author contributions
PZ and FW designed and organized the study. PZ, FW, YM, and LZ performed the survey. YZ and YM undertook the data analysis and interpretation, supervised by PZ, and wrote the manuscript. PZ, FW, JL, and AA reviewed and commented on the manuscript. All authors have read and agreed to this version of the manuscript.
Funding
This research was funded by Project HOPE of the “Cervical Cancer/HPV Prevention Education Program” and the project “Advocacy Activities Design to Improve Health Literacy of New Media among Shanghai Teenagers,” commissioned by the Shanghai Audio-Visual Education Museum.
Acknowledgments
We would like to thank the study communities and data collectors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1203610/full#supplementary-material
References
1. World Health Organization. Cervical cancer. E. coli (2022): Available at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed March 15, 2022).
2. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–9. doi: 10.3322/caac.21660
3. World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. E. coli (2020). Available at: https://www.who.int/publications/i/item/9789240014107 (accessed March 15, 2022).
4. Yifan, S, Xiaoxue, L, Zundong, Y, Wenzhou, Y, Lei, C, Lingsheng, C, et al. Human papillomavirus vaccine coverage among the 9-45-year-old female population of China in 2018-2020. Chin J Vacc Immun. (2021) 27:570–5. doi: 10.19914/j.CJVI.2021101
5. Bruni, L, Saura-Lázaro, A, Montoliu, A, Brotons, M, Alemany, L, Diallo, MS, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev Med. (2021) 144:106399. doi: 10.1016/j.ypmed.2020.106399
6. Wei, L, Xie, X, Liu, J, Qiao, Y, Zhao, F, Wu, T, et al. Elimination of cervical Cancer: challenges promoting the HPV vaccine in China. Indian J Gynecol Oncol. (2021) 19:51. doi: 10.1007/s40944-021-00536-6
7. Yin, Y. HPV vaccination in China needs to be more cost-effective. Lancet (London, England). (2017) 390:1735–6. doi: 10.1016/s0140-6736(17)32606-5
8. Siu, JY, Fung, TKF, and Leung, LH. Social and cultural construction processes involved in HPV vaccine hesitancy among Chinese women: a qualitative study. Int J Equity Health. (2019) 18:147. doi: 10.1186/s12939-019-1052-9
9. Data Blog of Netease. Nowadays, there is a two-year waiting list for the HPV vaccine. E coli (2021) Available at: https://www.huxiu.com/article/404675.html?f=member_article. (accessed April 5, 2023).
10. Hernandez, ND, Daley, EM, Young, L, Kolar, SK, Wheldon, C, Vamos, CA, et al. HPV vaccine recommendations: does a health care provider's gender and ethnicity matter to unvaccinated Latina college women? Ethn Health. (2019) 24:645–1. doi: 10.1080/13557858.2017.1367761
11. Rosenthal, SL, Weiss, TW, Zimet, GD, Ma, L, Good, MB, and Vichnin, MD. Predictors of HPV vaccine uptake among women aged 19-26: importance of a physician's recommendation. Vaccine. (2011) 29:890–5. doi: 10.1016/j.vaccine.2009.12.063
12. Ma, J, Zhang, X, Wang, W, Zhang, R, Du, M, Shan, L, et al. Knowledge of HPV, its vaccines, and attitudes toward HPV vaccines among obstetrician-gynecologists, pediatricians and immunization services providers in Western China. Hum Vaccin Immunother. (2022) 18:1–7. doi: 10.1080/21645515.2021.1962150
13. Chen, S, Mei, C, Huang, W, Liu, P, Wang, H, Lin, W, et al. Human papillomavirus vaccination related knowledge, and recommendations among healthcare providers in southern China: a cross-sectional survey. BMC Womens Health. (2022) 22:169. doi: 10.1186/s12905-022-01728-8
14. Xu, X, Wang, Y, Liu, Y, Yu, Y, Yang, C, Zhang, Y, et al. A nationwide post-marketing survey of knowledge, attitudes and recommendations towards human papillomavirus vaccines among healthcare providers in China. Prev Med. (2021) 146:106484. doi: 10.1016/j.ypmed.2021.106484
15. Von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surgery (London, England). (2014) 12:1495–9. doi: 10.1016/j.ijsu.2014.07.013
16. Finney Rutten, LJ, St Sauver, JL, Beebe, TJ, Wilson, PM, Jacobson, DJ, Fan, C, et al. Association of both consistency and strength of self-reported clinician recommendation for HPV vaccination and HPV vaccine uptake among 11- to 12-year-old children. Vaccine. (2017) 35:6122–8. doi: 10.1016/j.vaccine.2017.09.056
17. Collange, F, Fressard, L, Pulcini, C, Sebbah, R, Peretti-Watel, P, and Verger, P. General practitioners' attitudes and behaviors toward HPV vaccination: a French national survey. Vaccine. (2016) 34:762–8. doi: 10.1016/j.vaccine.2015.12.054
18. Haley, N, Maheux, B, Rivard, M, and Gervais, A. Sexual health risk assessment and counseling in primary care: how involved are general practitioners and obstetrician-gynecologists? Am J Public Health. (1999) 89:899–2. doi: 10.2105/ajph.89.6.899
19. Riedesel, JM, Rosenthal, SL, Zimet, GD, Bernstein, DI, Huang, B, Lan, D, et al. Attitudes about human papillomavirus vaccine among family physicians. J Pediatr Adolesc Gynecol. (2005) 18:391–8. doi: 10.1016/j.jpag.2005.09.004
20. Dempsey, AF, Pyrzanowski, J, Brewer, S, Barnard, J, Sevick, C, and O'Leary, ST. Acceptability of using standing orders to deliver human papillomavirus vaccines in the outpatient obstetrician/gynecologist setting. Vaccine. (2015) 33:1773–9. doi: 10.1016/j.vaccine.2015.02.044
21. Mazzoni, S, Brewer, S, Durfee, J, Pyrzanowski, J, Barnard, J, Dempsey, AF, et al. Patient perspectives of obstetrician-gynecologists as primary care providers. J Reprod Med. (2017) 62:3–8.
22. Nilsen, K, Aasland, OG, and Klouman, E. The HPV vaccine: knowledge and attitudes among public health nurses and general practitioners in northern Norway after introduction of the vaccine in the school-based vaccination programme. Scand J Prim Health Care. (2017) 35:387–5. doi: 10.1080/02813432.2017.1358433
23. Lin, C, Mullen, J, Smith, D, Kotarba, M, Kaplan, SJ, and Tu, P. Healthcare providers’ vaccine perceptions, hesitancy, and recommendation to patients: A systematic review. Vaccines (Basel). (2021) 9:713. doi: 10.3390/vaccines9070713
24. Abi Jaoude, J, Khair, D, Dagher, H, Saad, H, Cherfan, P, Kaafarani, MA, et al. Factors associated with human papilloma virus (HPV) vaccine recommendation by physicians in Lebanon, a cross-sectional study. Vaccine. (2018) 36:7562–7. doi: 10.1016/j.vaccine.2018.10.065
25. Aldossri, M, Okoronkwo, C, Dodd, V, Manson, H, and Singhal, S. Determinants of dentists' readiness to assess HPV risk and recommend immunization: a transtheoretical model of change-based cross-sectional study of Ontario dentists. PLoS One. (2021) 16:e0247043. doi: 10.1371/journal.pone.0247043
26. Presser, BE, Katz, ML, Shoben, AB, Moore, D, Ruffin, MT, Paskett, ED, et al. Effects of an education intervention about HPV self-testing for healthcare providers and staff. J Cancer Education. (2018) 33:954–9. doi: 10.1007/s13187-017-1164-0
27. González Cano-Caballero, M, Gil García, E, Garrido Peña, F, and Cano-Caballero Galvez, MD. Opinions of Andalusian primary health care professionals. An Sist Sanit Navar. (2018) 41:27–34. doi: 10.23938/assn.0126
28. Brown, V. Immunization for midlife women. Menopause (New York, NY). (2022) 29:1204–9. doi: 10.1097/gme.0000000000002024
29. The American College of Obstetricians and Gynecologists (ACOG). Human papillomavirus vaccination: ACOG Committee opinion summary, number 809. Obstet Gynecol. (2020) 136:435–6. doi: 10.1097/aog.0000000000004001
30. Shi, HY, Wang, SZ, Yang, XJ, Lin, L, and Hu, JY. Preventive medicine curriculum system in training program of clinical medicine in the era of healthy China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. (2020) 41:1155–9. doi: 10.3760/cma.j.cn112338-20200104-00009
31. Wen, Y, Pan, XF, Zhao, ZM, Chen, F, Fu, CJ, Li, SQ, et al. Knowledge of human papillomavirus (HPV) infection, cervical cancer, and HPV vaccine and its correlates among medical students in Southwest China: a multi-center cross-sectional survey. Asian Pac J Cancer Prev. (2014) 15:5773–9. doi: 10.7314/apjcp.2014.15.14.5773
32. China's State Council. Opinions of the general Office of the State Council on further strengthening the Administration of Vaccine Circulation and Vaccination. (2017).
33. Luo, Y, He, H, Tang, X, Wang, S, Zhang, J, Wu, T, et al. Cost-effectiveness of 2-dose human papillomavirus vaccination for 12-year-old girls in Zhejiang Province: implications for China's expanded program on immunization. Hum Vaccin Immunother. (2020) 16:1623–9. doi: 10.1080/21645515.2019.1711299
34. Callaghan, T, Motta, M, Sylvester, S, Lunz Trujillo, K, and Blackburn, CC. Parent psychology and the decision to delay childhood vaccination. Soc Sci Med. (2019) 238:112407. doi: 10.1016/j.socscimed.2019.112407
35. Dai, Z. What have we missed?: the knowledge of and access to the HPV vaccine and sex education in China. Health Commun. (2020) 35:96–8. doi: 10.1080/10410236.2018.1545168
36. Tsai, YF. Nurses' facilitators and barriers for taking a sexual history in Taiwan. Appl Nurs Res. (2004) 17:257–4. doi: 10.1016/j.apnr.2004.09.011
37. Hosking, YP, Cappelli, D, Donly, K, and Redding, S. HPV Vaccination and the role of the pediatric dentist: survey of graduate program directors. Pediatr Dent. (2017) 39:383–389.
38. Suryadevara, M, Handel, A, Bonville, CA, Cibula, DA, and Domachowske, JB. Pediatric provider vaccine hesitancy: an under-recognized obstacle to immunizing children. Vaccine. (2015) 33:6629–34. doi: 10.1016/j.vaccine.2015.10.096
39. Zhao, FH, Tiggelaar, SM, Hu, SY, Xu, LN, Hong, Y, Niyazi, M, et al. A multi-center survey of age of sexual debut and sexual behavior in Chinese women: suggestions for optimal age of human papillomavirus vaccination in China. Cancer Epidemiol. (2012) 36:384–10. doi: 10.1016/j.canep.2012.01.009
40. Zhao, R, Zhang, L, Fu, X, Su, C, and Zhang, Y. Sexual and reproductive health related knowledge, attitude and behavior among senior high school and college students in 11 provinces and municipalities of China. Chin J Public Health. (2019) 35:1330–8.
41. Yuan, Y, Ruan, F, Liu, Y, Wu, L, Pan, M, Ye, Z, et al. Prevalence of and factors associated with unintended pregnancies among sexually active undergraduates in mainland China. Reprod Health. (2022) 19:165. doi: 10.1186/s12978-022-01461-3
42. Richman, AR, Torres, E, Wu, Q, Eldridge, D, and Lawson, L. HPV vaccine recommendation practices of current and future physicians in North Carolina: an exploratory study. Health Educ Res. (2022) 37:213–6. doi: 10.1093/her/cyac016
43. The American Academy of Family Physicians (AAFP). Human Papillomavirus Vaccine (HPV) Available at: https://www.aafp.org/family-physician/patient-care/prevention-wellness/immunizations-vaccines/disease-pop-immunization/human-papillomavirus-vaccine-hpv.html#recommendations (accessed April 5, 2023).
44. Gilkey, MB, and McRee, AL. Provider communication about HPV vaccination: a systematic review. Hum Vaccin Immunother. (2016) 12:1454–68. doi: 10.1080/21645515.2015.1129090
45. Jacobson, RM, St Sauver, JL, Griffin, JM, MacLaughlin, KL, and Finney Rutten, LJ. How health care providers should address vaccine hesitancy in the clinical setting: evidence for presumptive language in making a strong recommendation. Hum Vaccin Immunother. (2020) 16:2131–5. doi: 10.1080/21645515.2020.1735226
46. Vorsters, A, Arbyn, M, Baay, M, Bosch, X, de Sanjosé, S, Hanley, S, et al. Overcoming barriers in HPV vaccination and screening programs. Papillomavirus Res (Amsterdam, Netherlands). (2017) 4:45–53. doi: 10.1016/j.pvr.2017.07.001
47. Oberlin, AM, Rahangdale, L, Chinula, L, Fuseini, NM, and Chibwesha, CJ. Making HPV vaccination available to girls everywhere. Int J Gynaecol Obstet. (2018) 143:267–76. doi: 10.1002/ijgo.12656
Keywords: vaccine recommendation frequency, HPV vaccine, health care provider, knowledge of HPV, vaccine accessibility, communication difficulty
Citation: Mao Y, Zhao Y, Zhang L, Li J, Abdullah AS, Zheng P and Wang F (2023) Frequency of health care provider recommendations for HPV vaccination: a survey in three large cities in China. Front. Public Health. 11:1203610. doi: 10.3389/fpubh.2023.1203610
Edited by:
Italo F. Angelillo, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Benjamin E. Ansa, Augusta University, United StatesVincenza Sansone, University of Campania Luigi Vanvitelli, Italy
Copyright © 2023 Mao, Zhao, Zhang, Li, Abdullah, Zheng and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pinpin Zheng, enBpbnBpbkBzaG11LmVkdS5jbg==; Fan Wang, d2FuZ2ZhbjUxMkAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Yimeng Mao
Yimeng Mao Yuchen Zhao
Yuchen Zhao Lingyun Zhang
Lingyun Zhang Jie Li3
Jie Li3 Abu S Abdullah
Abu S Abdullah Pinpin Zheng
Pinpin Zheng Fan Wang
Fan Wang