
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 05 June 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1194779
This article is part of the Research Topic School-based nutrition and physical activity interventions among children and adolescents View all 14 articles
Background: Schools provide a favorable setting for health education, however, the most effective school-based exercise mode for improving physical fitness remains unclear. This network meta-analysis was designed to assess and rank the comparative efficacy of six exercise modalities on physical fitness indicators in a school-based setting.
Methods: An online search of the Web of Science, PubMed, SPORTDiscus, and Scopus databases was conducted. Randomized and quasi-randomized controlled trials were considered. Outcomes included measures of anthropometry and body composition, muscular fitness, and cardiorespiratory fitness. Data were pooled with a random effects model using the frequentist framework.
Results: A total of 66 studies with 8,578 participants (48% girls) were included. High-intensity interval training was the most effective intervention reducing body mass index (mean difference (MD) = −0.60 kg·m−2, 95% confidence interval (95%CI) = −1.04 to −0.15, p = 0.009), elevating VO2max (MD = 3.59 mL·kg−1·min−1, 95% CI = 2.45 to 4.74, p < 0.001), and 20-meter sprint performance (MD = −0.35 s, 95% CI = −0.55 to −0.14, p = 0.001). Aerobic training had the highest probability of reducing waist circumference (standardized mean difference (SMD) = −0.60, 95% CI = −0.88 to −0.32, p < 0.001). Active video games emerged as a promising modality for improving countermovement jump (MD = 2.43 cm, 95% CI = 0.06 to 4.80, p = 0.041) and shuttle running performance (SMD = 0.86, 95% CI = 0.29 to 1.43, p = 0.003). Strength training was the best exercise mode for improving standing long jump performance (SMD = 1.03, 95% CI = 0.07 to 1.98, p = 0.035) while combined training was rated the first for decreasing body fat percent (MD = −2.56%, 95% CI = −4.73 to −0.40, p = 0.022) and increasing push-up repetitions (SMD = 3.59, 95% CI = 0.81 to 6.37, p = 0.012).
Conclusion: School-based exercise interventions have multiple effects on physical fitness. The findings of this study will help to inform physical education teachers and coaches how best to deliver exercise programs in a school setting. Since the study was limited by the original research, the conclusions will require further verification using high-quality randomized controlled trials.
Systematic Review Registration: PROSPERO, Identifier: CRD42023401963.
Physical fitness (PF) is a valuable health marker. Maintaining satisfactory PF status in children and adolescents reduces the risk of obesity (1), cardiovascular disease (2), and diabetes (3) in adulthood. Indeed, approximately 80% of children and adolescents suffer from these health conditions because they are engaged in an insufficient level of physical activity (PA) (4–6). As a result, exercise intervention and PF promotion among children and adolescents have become a major focus of public health research. Schools are favorable setting for PF promotion (7) because they offer this age group a high amount active time during the school day (8). The school environment provides an equitable sociocultural environment for exercise behavior using various PF promotion programs (9). Studies have reported the impact of particular school-based interventions on health-related PF (10, 11). A recent systematic review found that school-based neuromuscular training is effective at increasing strength (12). Two systematic reviews with meta-analyses involving 11 and 35 randomized controlled trials (RCTs) found that high-intensity interval training (HIIT) in school contributes to greater improvement in muscular and aerobic fitness (13, 14). However, these pairwise meta-analyses only compared one type of exercise to regular physical education (PE) lessons. While one meta-analysis attempted to evaluate the impact of school-based PF promotion programs on obesity prevention (15), it still failed to assess the superiority of the diverse exercise types. Overall, the evidence needed to measure the comparative effectiveness of multiple school-based exercise treatments on PF remains limited.
Recently, gamified exercises with higher attractiveness have been embedded in school-based PA programs to enhance students’ enjoyment (16). One meta-analysis reported favorable results for active video games (AVGs) on body mass index (BMI) reduction in children and adolescents (17). Likewise, game-based exercise (GB) including small-side ball games in recreational sports and aerobic exercise performed with game patterns, attracts researchers’ attention. A previous review found that small-side football ball games had a similar effect as interval running on PF (18). However, whether these novel exercise programs are superior to other modalities remains unclear. Thus, AVGs and GB conducted in school were included in the comparison.
No systematic review has integrated and assessed the effects of various exercise treatments on anthropometry and body composition, muscular fitness (MF), and cardiorespiratory fitness (CRF) outcomes, concentrating exclusively among children and adolescents in school-based settings. This review used network meta-analysis (NMA), a newly recommended analysis tool in the field of PA and health promotion (19), to (1) evaluate the comparative efficacy of six exercise treatments performed in the school environment on anthropometry and body composition, MF and CRF and (2) construct an effectiveness hierarchy. Unlike pairwise meta-analysis, NMA is able to comparative multiple interventions as an intermediary for indirect comparisons even in the absence of direct comparative evidence. NMA also ranks probable success of each intervention.
The study follows the relevant PRISMA checklist (20). The study protocol was registered prospectively in PROSPERO (registration code: CRD42023401963).
A comprehensive computerized search of the Web of Science, PubMed, SPORTDiscus, and Scopus database was performed from inception until February 2023. The retrieval strategy was conducted using the PICOS tool: (P) Population: children and adolescents; (I) Intervention: active video games (AVGs), game-based exercise (GB), high-intensity interval training (HIIT), aerobic training (AT), strength training (ST), and combined aerobic and strength training (CT; Table 1); (C) Comparator: regular physical activity or physical education; (O) Outcomes: anthropometry and body composition, muscular fitness (MF), and cardiorespiratory fitness (CRF); (S) Study type: randomized controlled trials (RCTs) or quasi-RCTs. The detailed search algorithms are shown in Supplementary Table S1. Reference lists of the included studies and previous reviews were scanned for articles that met the eligibility criteria.
The inclusion criteria for this systematic review and NMA were as follows: (1) peer-reviewed original research with full text in English over the past 20 years (January 2003 to February 2023); (2) study participants were children and adolescents aged 4–18 years of age enrolled in full-time or part-time education; (3) at least one exercise type, including AVGs, GB, HIIT, AT, ST, or CT, was employed in a school setting (intra-PE, or extra-PE during school hours); (4) anthropometry and body composition [body mass index (BMI), body fat percent (BF%), and waist circumference (WC)], MF [standing long jump (SLJ), countermovement jump (CMJ), push-ups, and 20-meter sprint (20-m sprint)], and/or CRF (shuttle running (SR), and VO2max) were used as outcomes; and (5) the intervention lasted at least 4 weeks. Both RCTs and quasi-RCTs were included given the difficulty of implementing RCTs in school settings. The inclusion of only RCTs may have led to the omission of relevant information. Participants with injuries or chronic or acute diseases, participants who were youth athletes, reviews and meta-analyses, studies lacking the required outcomes, or studies that were unable to identify implementation setting were excluded.
Two independent authors (JW and YY) screened the literature based on the inclusion and exclusion criteria and read the full text to assess their eligibility. Any disagreements were handled by adjudications from other team members. The following data were extracted from eligible articles and recorded in EXCEL: (1) first author and publication year; (2) participant demographics (e.g., sample size, sex, and mean age); (3) intervention characteristics (exercise type, duration frequency, time in school); and (4) outcomes. EndNote X9 was used to consolidate and remove duplicates. If the same trial was published more than once, the most recent or more complete study was selected.
Two authors (JW and YY) independently assessed the risk of bias (ROB) using the following seven dimensions from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 tool (21): (1) randomized sequence generation; (2) treatment allocation concealment; (3) blinding of participants; (4) blinding of personnel; (5) incomplete outcome data; (6) selective reporting; and (7) other sources of bias. Eligible studies were divided into high risk (≥4), medium risk (3), and low risk (≤2) of bias based on the frequency of high-risk items. By default, all studies were classified as high ROB in the “blinding of participants” dimension since it is difficult to achieve participant blinding during exercise intervention protocols in school settings. Thus, this domain was not counted toward the overall score.
All outcomes involved in this study were continuous variables, so the mean and standard deviations (SDs) were extracted from the included studies. Mean differences (MDs) were obtained by directly extracting or subtracting the mean at the post-training vs. pre-training. The unreported standard deviation difference was imputed according to the formula provided in the Cochrane Handbook (Supplementary Figure S37) (22). Standardized mean differences (SMDs) were applied when different evaluation methods or scales were used to measure the same indicator. When multiple posttests (e.g., multiple follow-ups) occurred, data measured immediately after the intervention were extracted. If multiple variations of the same interventions or different population subgroups were compared in an included study, the respective outcomes were pooled using the formula provided in Supplementary Figure S37 (22).
Statistical analyses were conducted using STATA 16.0 software. Heterogeneity was assessed using I2 statistic. Values of I2 ≤ 25, 25% < I2 ≤ 50, 50% < I2 ≤ 75%, and I2 > 75% represented no significant heterogeneity, low heterogeneity, medium heterogeneity, and high heterogeneity, respectively. A random-effects frequentist framework-based NMA was used to calculate pooled estimates and 95% confidence intervals (CI) (23). Network plots were created to visually demonstrate the geometry of various treatments. Each node corresponded to a certain treatment, and the node size represented the sample size. The lines linking the nodes indicated the direct head-to-head comparisons between interventions, and the line thickness between nodes represented the number of included studies. The Wald test and node splitting methods were used to evaluate global and local inconsistencies, respectively. The surface under the cumulative ranking curve (SUCRA) shows the ranking probability of each intervention. The larger the SUCRA value, which ranges from 0 to 100%, the more significant the intervention effect. Network funnel plots were generated to identify whether publication bias was caused by any small sample studies. To examine robustness, sensitivity analyses were performed by eliminating individual studies separately to evaluate the impact of each study on the overall heterogeneity.
A total of 2,296 studies were obtained by a preliminary search of the databases, and an additional 25 studies were obtained from existing systematic reviews. After removing duplicate studies and screening titles and abstracts, 241 studies were carefully read, of which 66 studies were finally included. A flowchart of the selection process is shown in Figure 1.
Basic information about the eligible studies is shown in Supplementary Table S3. These included studies were conducted in North America (n = 3), South America (n = 3), Europe (n = 38), Asia (n = 13), Oceania (n = 7), and Africa (n = 2). A total of 8,578 children and adolescents (48% girls) with a mean age of 13.6 ± 4.3 were included in the 66 studies. Nine studies recruited only girls, eight studies recruited only boys, and the remaining 49 recruited both boys and girls. Fourteen studies focused on overweight or obese children and adolescents.
A total of 3,486 participants (1,685 girls) were included in the control group (CON) group that participated in regular physical activity (PA) or physical education (PE), 426 participants (171 girls) were included in the active video games (AVGs) group (24–31), 1,670 participants (803 girls) were included in the game-based exercise (GB) group (32–42), 1,085 participants (522 girls) were included in the high-intensity interval training (HIIT) group (36, 37, 43–65), 1,005 participants (462 girls) were included in the strength training (ST) group (41, 66–82), 599 participants (300 girls) were included in the aerobic training (AT) group (49, 53, 56, 61, 62, 66, 76, 83–87), and 307 participants (197 girls) were included in the combined aerobic and strength training (CT) group (68–71, 76, 88, 89). Interventions lasted on average of 13.9 ± 9.6 weeks and ranged from 4 to 50 weeks, with 73% of studies lasting less than 12 weeks. The average number of sessions per week was 2.7 ± 0.8. Twenty-three interventions were conducted intra-PE, 38 were conducted extra-PE, and five occurred both intra- and extra-PE.
A summary of risk of bias (ROB) evaluation results is shown in Supplementary Table S2. Ten studies had high a ROB, 38 had a moderate ROB, and the remaining 18 had a low ROB. For each individual ROB item, 48 studies had a high random sequence generation. Only two studies demonstrated a low ROB in allocation concealment, while four mentioned blinding of research personnel. Seven studies had a high ROB due to incomplete outcome data and 36 studies had unclear ROB from selective reporting. Five studies had a high risk of other bias. Table 2 presents the ROB results in each intervention.
Three anthropometry and body composition [body mass index (BMI; kg·m−2), waist circumference (WC), and body fat percent (BF; %) measurements, four muscular fitness (standing long jump (SLJ), countermovement jump (CMJ; cm), push-up, and 20-meter sprint (20-m sprint; s)] measurements, and two cardiorespiratory fitness [shuttle running (SR), VO2max; mL·kg−1·min−1)] measurements were included in the network meta-analysis (NMA). The geometry of different interventions for each outcome is shown in Figure 2. Each node represents one type of exercise treatment, while node size represents the sample size used in the intervention. The lines between two nodes indicate direct comparisons between the exercise types, with thicker lines indicating that more studies were included. Additional information about the contribution plots of comparative evidence is available in Supplementary Figures S1–S9. Global inconsistency testing was not significant (all Wald test statistic p values >0.5). Homoplastically, the results of local inconsistency testing using the node splitting method showed that each direct and indirect comparison among estimates was coincident for all outcomes (all p-values > 0.5; Supplementary Tables S4–S12). Forest plots with 95% CI are displayed in Supplementary Figures S10–S18. The comparative effects of each exercise type is shown in Figures 3A–I. Funnel plots evaluating publication bias are available in Supplementary Figures S19–S27. Supplementary Figures S28–S36 describes the surface under the cumulative ranking curve for all interventions. Larger SUCRA values, represent a higher probability that a treatment will be effective. Using the SUCRA value and mean rank of all exercise types were sorted (Table 3). Besides, due to the limitation of original studies, hand grip strength and sit-ups were not able to form a complete loop in NMA. Therefore, they were excluded.
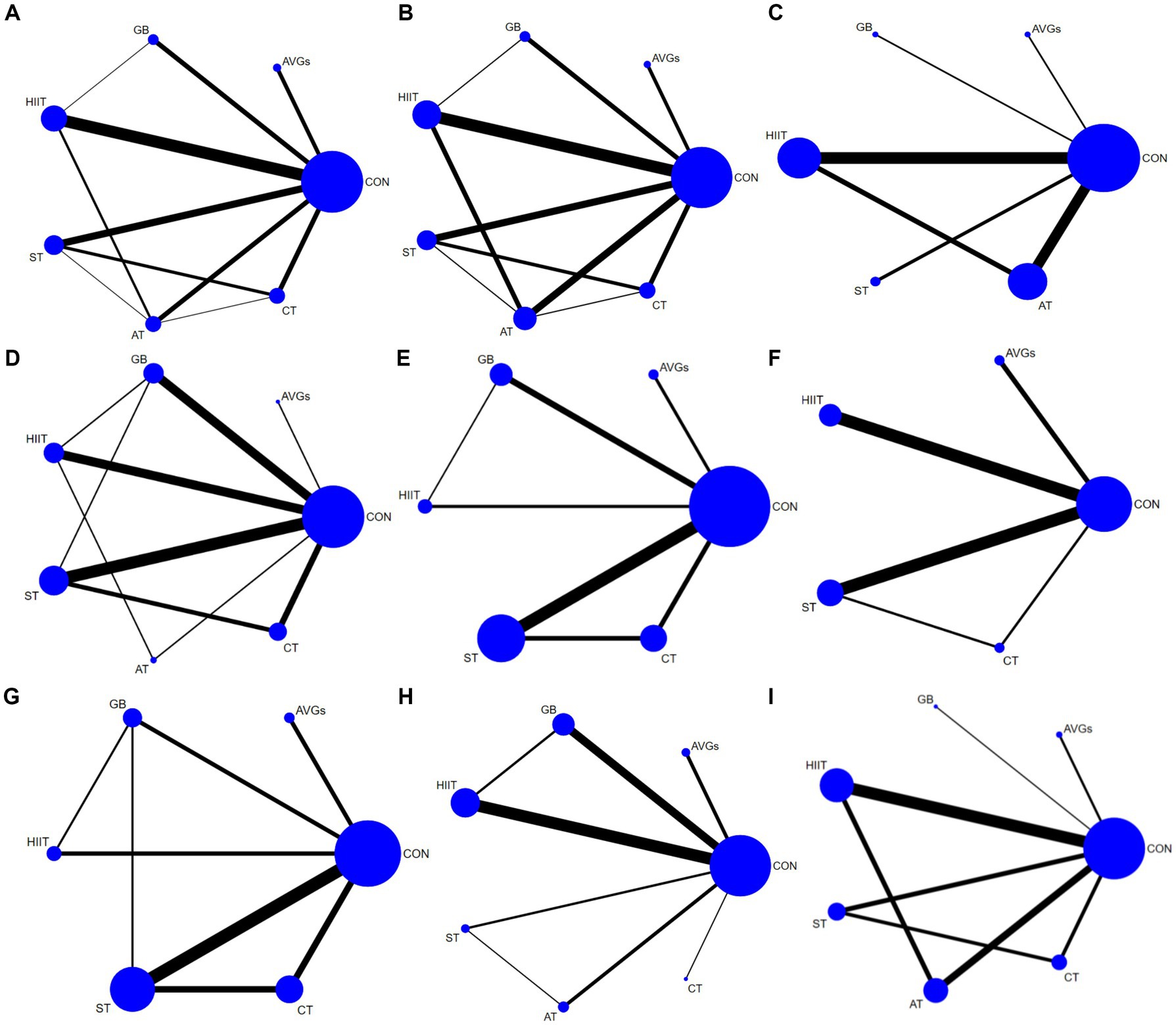
Figure 2. Network plots for outcome comparisons. The node size represented the sample size corresponding to the intervention, and the line thickness between nodes represented the number of included studies. (A) BMI, (B) body fat percent, (C) waist circumference, (D) standing long jump, (E) countermovement jump, (F) push-ups, (G) 20-m sprint, (H) shuttle running, and (I) VO2max.
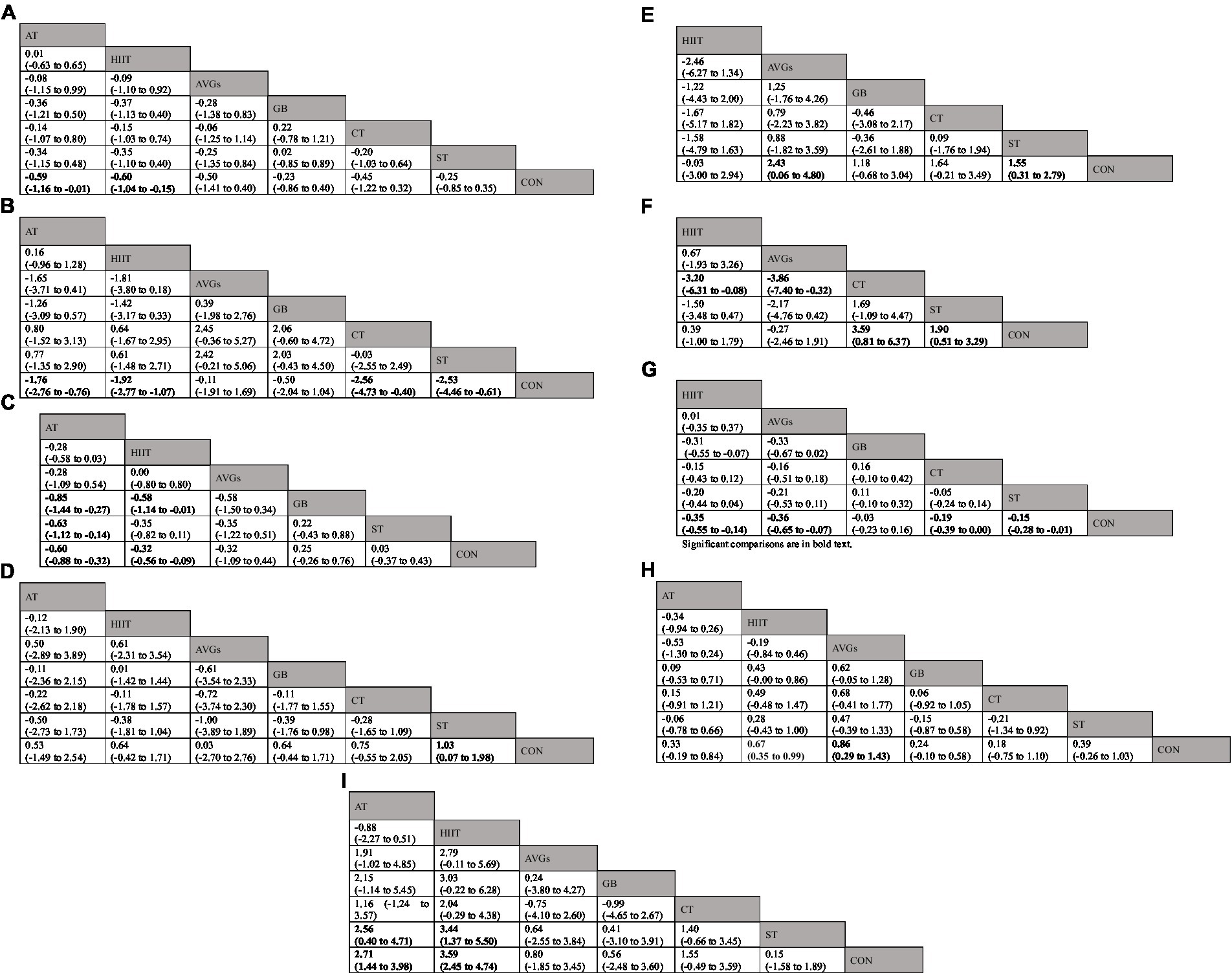
Figure 3. League table of comparative effectiveness results for (A) BMI [kg·m−2], (B) body fat percent [%], (C) waist circumference, (D) standing long jump, (E) countermovement jump [cm], (F) push-ups, (G) 20-m sprint [s], (H) shuttle running, (I) VO2max [mL·kg−1·min−1]. Significant comparisons are in bold text. Each cell presents an SMD/MD with a 95%CI. For A–C,G, lower negative SMD/MD values indicate positive effects on PF. Thus, a negative SMD/MD supports the upper-left intervention. For D–F,H,I, higher positive SMD/MD values indicate positive effects on PF. Thus, a positive SMD/MD supports the upper-left intervention, and a negative SMD/MD supports the lower-right intervention. 95%CI = 95%confidence interval; AT, aerobic training; HIIT, high-intensity interval training; AVGs, active video games; GB, game-based exercise; CT, combined aerobic and strength training; ST, strength training; CON, control group; SMD, standardized mean difference; MD, mean difference.
Forty studies involving 4,841 participants and all six exercise types reported BMI. Overall effects indicated that school-based exercise interventions can effectively reduce BMI (MD = −0.39 kg·m−2, 95% CI = −0.62 to −0.15, p = 0.001). Compared with CON, AT (MD = −0.59 kg·m−2, 95% CI = −1.16 to −0.01, p = 0.043) and HIIT (MD = −0.60 kg·m−2, 95% CI = −1.04 to −0.15, p = 0.009) significantly reduced BMI while AVGs (MD = −0.50 kg·m−2, 95% CI = −1.41 to 0.40, p = 0.275), GB (MD = −0.23 kg·m−2, 95% CI = −0.86 to 0.40, p = 0.475), ST (MD = −0.25 kg·m−2, 95% CI = −0.85 to 0.35, p = 0.418), and CT (MD = −0.45 kg·m−2, 95% CI = −1.22 to 0.32, p = 0.255) had no significant impact on BMI (Figure 3A; Supplementary Figure S10). HIIT had the highest probability (SUCRA = 72.6%) of being the most treatment for lowering BMI (Table 3; Supplementary Figure S28).
Thirty studies involving 3,332 participants and all six exercise types included BF%. Overall effects indicated that school-based exercise interventions can effectively reduce BF% (MD = −1.78%, 95% CI = −2.38 to −1.17, p < 0.001). Compared with CON, CT (MD = −2.56%, 95% CI = −4.73 to −0.40, p = 0.022), ST (MD = −2.53%, 95% CI = −4.46 to −0.61, p = 0.011), HIIT (MD = −1.92%, 95% CI = −2.77 to −1.07, p < 0.001), and AT (MD = −1.76%, 95% CI = −2.76 to −0.76, p < 0.001) significantly reduced BF% (Figure 3B; Supplementary Figure S11). CT was the most effective intervention for BF% reduction (SUCRA = 81.0%; Table 3; Supplementary Figure S29). Compared with CON, AVGs (MD = −0.11%, 95% CI = −1.91 to 1.69, p = 0.909), and GB (MD = −0.50%, 95% CI = −2.04 to 1.04, p = 0.534) had no significant impact on BF% (Figure 3B; Supplementary Figure S11).
Sixteen studies involving 1,073 participants and five exercise modalities in addition to CT explored the effects of exercise on waist circumference. Overall effects indicated that school-based exercise interventions can effectively reduce WC (SMD = −0.31, 95% CI = −0.52 to −0.10, p = 0.004). Compared with CON, HIIT (SMD = −0.32, 95% CI = −0.56 to −0.09, p = 0.007) and AT (SMD = −0.60, 95% CI = −0.88 to −0.32, p < 0.001) significantly reduced WC (Figure 3C; Supplementary Figure S12). AT had the highest probability (SUCRA = 94.2%) of reducing WC (SUCRA = 94.2%; Table 3; Supplementary Figure S30). Compared with CON, AVGs (SMD = −0.32, 95% CI = −1.09 to 0.44, p = 0.405), GB (SMD = 0.25, 95% CI = −0.26 to 0.76, p = 0.333), and ST (SMD = 0.03, 95% CI = −0.37 to 0.43, p = 0.887) had no significant impact on WC (Figure 3C; Supplementary Figure S12).
Twenty-two studies involving 4,185 participants and all six interventions reported the effects of multiple exercise modes on SLJ. Overall effects indicated that school-based exercise interventions can effectively improve SLJ (SMD = 0.63, 95% CI = 0.38 to 0.89, p < 0.001). Compared with CON, ST (SMD = 1.03, 95% CI = 0.07 to 1.98, p = 0.035) significantly improved SLJ while AVGs (SMD = 0.03, 95% CI = −2.70 to 2.76, p = 0.983), GB (SMD = 0.64, 95% CI = −0.44 to 1.71, p = 0.245), HIIT (SMD = 0.64, 95% CI = −0.42 to 1.71, p = 0.234), AT (SMD = 0.53, 95% CI = −1.49 to 2.54, p = 0.607), and CT (SMD = 0.75, 95% CI = −0.55 to 2.05, p = 0.258) had no significant impact on SLJ (Figure 3D; Supplementary Figure S13). ST had the highest probability of improving SLJ (SUCRA = 74.6%; Table 3; Supplementary Figure S31).
Fifteen studies involving 934 participants and five exercise modalities other than AT examined the effects of various exercise treatments on CMJ. Overall effects indicated that school-based exercise interventions can effectively improve CMJ (MD = 1.22 cm, 95% CI = 0.27 to 2.18, p = 0.012). Compared with CON, AVGs (MD = 2.43 cm, 95% CI = 0.06 to 4.80, p = 0.041) and ST (MD = 1.55 cm, 95% CI = 0.31 to 2.79, p = 0.014) significantly improved CMJ while GB (MD = 1.18 cm, 95% CI = −0.68 to 3.04, p = 0.212), HIIT (MD = −0.03 cm, 95% CI = –3.00 to 2.94, p = 0.983), and CT (MD = 1.64 cm, 95% CI = −0.21 to 3.49, p = 0.083) had no significant impact on CMJ (Figure 3E; Supplementary Figure S14). AVGs had the highest probability of improving CMJ (SUCRA = 81.9%; Table 3; Supplementary Figure S32).
Twelve studies involving 1,557 participants and four interventions in addition to AT and GB assessed the effects of diverse exercise regimens on push-up ability. Overall effects indicated that school-based exercise interventions can effectively improve push-up ability (SMD = 1.14, 95% CI = 0.35 to 1.93, p = 0.005). Compared with CON, CT (SMD = 3.59, 95% CI = 0.81 to 6.37, p = 0.012) and ST (SMD = 1.90, 95% CI = 0.51 to 3.29, p = 0.007) significantly improved push-up ability while AVGs (SMD = −0.27, 95% CI = −2.46 to 1.91, p = 0.806) and HIIT (SMD = 0.39, 95% CI = −1.00 to 1.79, p = 0.581) had no significant impact on SLJ (Figure 3F; Supplementary Figure S15). CT had the highest probability of improving push-up ability (SUCRA = 96.0%; Table 3; Supplementary Figure S33).
Ten studies involving 1,059 participants reported the effects of five exercise modalities on 20-m sprint performance. Overall effects indicated that school-based exercise interventions can effectively improve 20-m sprint performance (MD = −0.17 s, 95% CI = −0.24 to −0.10, p < 0.001). Compared with CON, HIIT (MD = −0.35 s, 95% CI = −0.55 to −0.14, p = 0.001), AVGs (MD = −0.36 s, 95% CI = −0.65 to −0.07, p = 0.016), ST (MD = −0.15 s, 95% CI = −0.28 to −0.01, p = 0.035), and CT (MD = −0.19 s, 95% CI = −0.39 to 0.00, p = 0.047) significantly advanced the 20-m sprint performance while GB (MD = −0.03 s, 95% CI = −0.23 to 0.16, p = 0.729) had no significant impact on 20-m sprint performance (Figure 3G; Supplementary Figure S16). HIIT had the highest possibility of improving participant 20-m sprint ability (SUCRA = 85.6%; Table 3; Supplementary Figure S34).
Twenty-three studies involving 3,927 participants explored the impact of all six exercise types on SR. Overall effects indicated that school-based exercise interventions can effectively improve SR performance (SMD = 0.44, 95% CI = 0.29 to 0.59, p < 0.001). Compared with CON, AVGs (SMD = 0.86, 95% CI = 0.29 to 1.43, p = 0.003) and HIIT (SMD = 0.67, 95% CI = 0.35 to 0.99 p < 0.001) significantly advanced SR while GB (SMD = 0.24, 95% CI = −0.10 to 0.58, p = 0.170), ST (SMD = 0.39, 95% CI = −0.26 to 1.03, p = 0.238), AT (SMD = 0.33, 95% CI = −0.19 to 0.84, p = 0.210), and CT (SMD = 0.18, 95% CI = −0.75 to 1.10, p = 0.710) had no significant impact on (Figure 3H; Supplementary Figure S17). AVGs had the highest probability of improving SR (SUCRA = 89.1%; Table 3; Supplementary Figure S35).
Twenty-one studies involving 2,842 participants reported the effects of all six treatments on VO2max. Overall effects indicated that school-based exercise interventions can effectively improve VO2max (MD = 2.50 mL·kg−1·min−1, 95% CI = 1.78 to 3.22, p < 0.001). Compared with CON, HIIT (MD = 3.59 mL·kg−1·min−1, 95% CI = 2.45 to 4.74, p < 0.001) and AT (MD = 2.71 mL·kg−1·min−1, 95% CI = 1.44 to 3.98, p < 0.001) significantly improved VO2max while AVGs (MD = 0.80 mL·kg−1·min−1, 95% CI = −1.85 to 3.45, p = 0.428), GB (MD = 0.56 mL·kg−1·min−1, 95% CI = −2.48 to 3.60, p = 0.669), ST (MD = 0.15 mL·kg−1·min−1, 95% CI = −1.58 to 1.89, p = 0.370), and CT (MD = 1.55 mL·kg−1·min−1, 95% CI = −0.49 to 3.59, p = 0.054) had no significant impact on VO2max (Figure 3I; Supplementary Figure S18). Overall, HIIT had the highest probability of increasing VO2max (SUCRA = 96.5%; Table 3; Supplementary Figure S36).
To the best of our current knowledge, it is the first network meta-analysis (NMA) to compare the effects of school-based exercise modalities for physical fitness (PF) promotion among young students. High-intensity interval training (HIIT) was the most effective intervention reducing body mass index (BMI), and elevating VO2max, and 20-meter sprint (20-m sprint) performance. Aerobic training (AT) had the highest probability of reducing waist circumference (WC) while active video games (AVGs) emerged as a promising modality for improving countermovement jump (CMJ)and shuttle running (SR). Strength training (ST) was the best exercise for standing long jump (SLJ). Of the six interventions discussed, combined aerobic and strength training (CT) was most effective at lowering body fat percent (BF%) and increasing push-up repetitions.
BMI, total body fat, and abdominal adiposity are important predictors of cardiometabolic risk among youth. A recent systematic review used pairwise meta-analysis to assess the effects of HIIT (MD = −1.66 kg·m−2) and moderate-intensity continuous training (MD = −2.37 kg·m−2) on pediatric BMI and found no significant differences between the two exercises (90). While these findings were similar to those reported by the current study, the effects provided by this NMA were smaller, possibly due to differences in participant demographics. While the review focused exclusively on obese children, the current study did not make a strict distinction between overweight and normal weight participants. Exercise tends to have a greater impact on the body composition of obese or overweight children than those of normal weight (91).
One study found that exercise had a greater impact on BF% than BMI (92). This may be because a decrease in BMI can correlate with both weight loss and an increase in height caused by the natural growth of children and adolescents. In addition, because it is the most metabolically hazardous tissue, body fat serves as a valuable health measure of exercise intervention assessments. However, there is limited evidence showing that school-based exercise programs can reduce student BF%. A recent meta-analysis summarized the effect of a school-based HIIT program on BF% and found a pooled effect size of −1.7% (13). The current NMA went one step further by evaluating different exercise types. In addition to HIIT, AT, ST, and CT also lowered BF% of children and adolescents, a finding consistent with a previous NMA that compared the effects of five exercise types on the PF of adults (93). Although the current NMA found that CT was the best exercise mode for reducing body fat, HIIT was more efficient. Additional research is needed to compare the effect of CT and HIIT on fat loss.
In addition to total body fat, abdominal adiposity correlates closely with all-cause mortality (94). WC is often used as an indicator of abdominal adiposity and serves as a warning of potential health risks. For example, the risk of cardiovascular disease increases by 2% for each 1 cm increase in WC (95). While prior studies have suggested that HIIT does not significantly decrease WC in adolescents (96), more recent evidence contradicts these results (97). Similarly, this study found that HIIT and AT were effective at reducing WC in youth.
Surprisingly, while prior studies showed that AVGs significantly reduced BMI and BF% in children and adolescents, the current study found that school-based AVGs did not have a significant impact on participant anthropometry and body composition (98, 99). Differences in environmental factors may explain this inconsistency. While the articles included in this NMA study were exclusively conducted in schools, other reviews incorporated home or laboratory settings that were more beneficial to AVGs programs. Thus, more high-quality RCTs are needed to explore the influences of school-based AVGs on anthropometry and body composition.
Maximum muscular strength, muscular power, and endurance are potentially correlated with cardiovascular variables and the future health of children and adolescents (100). One prior review found that school-based interventions have a small-to-moderate effect on muscular fitness (101), which is congruent with the results of the current study. However, distinct from the strength exercise guidelines (102), this NMA suggested that ST had a relatively small impact on muscular fitness (MF). The development of muscle strength involves both neuromuscular adaptation and muscle hypertrophy. Thus, to improve MF through ST, a detailed assessment of training prescription (i.e., frequency, load, volume, and duration) should be conducted. However, it can be difficult to develop in-school exercise programs that strictly following the prescription when there is a high number of students. In addition, there is variation in the efficacy of different ST modes. Compared with bodyweight training, for example, plyometric training has a greater impact on CMJ and SLJ (103). Unfortunately, the use of specialized plyometric training in school settings was not assessed in this review. Some teachers also oppose school-based ST due to their limited experience and qualifications or low confidence in the training plans (104), further limiting the benefits of this intervention.
Of note, the current NMA found that AVGs are an innovative exercise mode with the highest possibility of increasing vertical jump performance. Compared to regular physical activity (PA) or physical education (PE), AVGs led to statistically significant and clinically important changes in CMJ. Since the exercise intensity of most commercial AVGs (e.g., Xbox Kinect, Wii, PlayStation) cannot reach the minimum threshold needed to stimulate growth in muscle strength (27), it is probable that the increase in CMJ performance caused by AVGs may be related to elevated locomotor skills rather than muscle strength. Two previous reviews support this inference, revealing that AVGs had a small but statistically significant effects on the fundamental motor skills of young people (105, 106). However, the disadvantages of AVGs are obvious as well. Since the sensors embedded in exergames are unable to precisely track human movement, skill-specific motor learning cannot be guided. This explains why the effect size reported in these reviews was smaller than that observed in a previous meta-analysis of foundational motor skill (FMS) interventions presented in real-life situations (107).
Push-ups provide a simple and valid muscular endurance test for the upper body. Higher push-up capacity relates to a lower incidence of cardiovascular disease events (108). The current NMA found that CT was the most promising exercise treatment for enhancing push-ups. While this supports the findings of other studies, limited data have been collected in the school environment. One randomized controlled trial (RCT) compared the effects of a 22-week CT to ST and AT alone on obese adolescents, and CT was shown to have a superior impact on muscle endurance (109). The current study also found that HIIT had no effect on push-ups, which is inconsistent with previous reports. For example, Eather et al. reported 4.0 repetition (95% CI: 1.2 to 6.8) push-up changes in favor of a HIIT program in the university setting (110). This discrepancy may stem from differences in the HIIT content. Indeed, push-up capacity only increases when relevant upper body motions are involved in the HIIT prescription.
HIIT had the highest possibility of improving participant 20-m sprint performance. This finding generally coincides with previous studies on the effect of HIIT and ST on sprint running (111, 112). The main factors that contribute to sprint performance are anaerobic power and leg muscle strength. Recent studies suggest that specialized HIIT and ST are the key to modifying these factors (113, 114), with running-based HIIT and velocity-based ST showing relatively higher efficacy. Running-based HIIT employs stretch-shortening cycle (SSC) actions that involve the sequential assortment of eccentric and concentric muscle actions. SSC improves concentric power output, which increases maximal running speed (115). Velocity-based ST tends to improve strength and power via neural mechanisms (116).
CRF has a positive impact on physical and mental health (117) and academic performance (118) in teenagers, and physical exercise is recommended as a cost-effective tool to sustain CRF (119). The current study found that AVGs and HIIT were most effective at improving shuttle running and VO2max respectively. The impact of AVGs was strongly impacted by the intervention arrangements used in each study. Due to governmental restrictions associated with the COVID-19 pandemic, regular daily PA was reduced for participants in the CON and their performance in shuttle running decreased significantly (26), leading to an unexpected gap between the experimental and CON groups. Without this interference, our calculations suggest that HIIT has a superior impact on shuttle running and VO2max, a result consistent with several pairwise meta-analyses (120–122). These improvements could be related to exercise-induced advantageous mitochondrial adaptations as well as an increase in blood capillarization, oxidative enzyme activity, and oxygen transport to the muscular system (123).
The strengths of this study include the following: (1) a considerable sample size (n = 8,578) of children and adolescents that provided enough power to identify statistically significant mean differences; (2) the incorporation of two emerging exercise interventions (AVGs and game-based exercise) that catered to the latest trends; and (3) the use of strict eligibility criteria to ensure that data were extracted from high-quality literature.
The study limitations are as follows: (1) low methodological quality of the included studies, with only 18 using random sequence generation methods and two mentioning whether allocation concealment was performed. Unclear allocation concealment may exaggerate study results and increase heterogeneity in meta-analysis; (2) the small number of AVGs studies may have reduced the robustness of the results and biased comparisons; (3) the failure to conduct detailed subgroup analysis for intra- and extra-PE interventions, making it difficult to explore the heterogeneity among studies.
This systematic review using NMA suggested that except for GB, school-based exercise interventions were associated with an improvement in PF among children and adolescents. Based on these findings, we recommend integrating HIIT into PE classes and adding AT and ST to extracurricular activities. It is encouraged that exergaming systems be introduced into primary and secondary schools to improve student exercise enjoyment and PF. However, because the school-based exercise interventions evaluated by this study were applied to different populations (e.g., boys, girls, students of normal weight or overweight) and were largely affected by PE teachers, additional high quality RCTs are needed to explore the influence of teacher and student-related factors on the effectiveness of various exercise interventions.
JW and YY contributed to study design, literature research, data extraction, risk of bias assessment, and drafting of the manuscript. HY and LL made substantial contributions to risk of bias assessment and data analysis. YC was a significant manuscript reviser. YS played important role in concept and design. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1194779/full#supplementary-material
PF, Physical fitness; PA, Physical activity; AVGs, Active video games; GB, Game-based exercise; HIIT, High-intensity interval training; ST, Strength training; AT, Aerobic training; CT, Combined aerobic and strength training; CON, Control group; RCTs, Randomized controlled trials; BMI, Body mass index; BF%, Body fat percent; WC, Waist circumference; SLJ, Standing long jump; CMJ, Countermovement jump; SR, Shuttle running; 20-m sprint, 20-meter sprint; MF, Muscular fitness; CRF, Cardiorespiratory fitness; NMA, Network meta-analysis; PE, Physical education.
1. Hills, AP, Andersen, LB, and Byrne, NM. Physical activity and obesity in children. Br J Sports Med. (2011) 45:866–70. doi: 10.1136/bjsports-2011-090199
2. Smith, JJ, Eather, N, Morgan, PJ, Plotnikoff, RC, Faigenbaum, AD, and Lubans, DR. The health benefits of muscular fitness for children and adolescents: a systematic review and meta-analysis. Sports Med. (2014) 44:1209–23. doi: 10.1007/s40279-014-0196-4
3. Dwyer, T, Magnussen, CG, Schmidt, MD, Ukoumunne, OC, Ponsonby, AL, Raitakari, OT, et al. Decline in physical fitness from childhood to adulthood associated with increased obesity and insulin resistance in adults. Diabetes Care. (2009) 32:683–7. doi: 10.2337/dc08-1638
4. Tapia-Serrano, MA, Sevil-Serrano, J, Sánchez-Miguel, PA, López-Gil, JF, Tremblay, MS, and García-Hermoso, A. Prevalence of meeting 24-hour movement guidelines from pre-school to adolescence: a systematic review and meta-analysis including 387,437 participants and 23 countries. J Sport Health Sci. (2022) 11:427–37. doi: 10.1016/j.jshs.2022.01.005
5. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet child Adolesc. Health. (2020) 4:23–35. doi: 10.1016/S2352-4642(19)30323-2
6. Sénéchal, M, Hebert, JJ, Fairchild, TJ, Møller, NC, Klakk, H, and Wedderkopp, N. Vigorous physical activity is important in maintaining a favourable health trajectory in active children: the CHAMPS study-DK. Sci Rep. (2021) 11:19211. doi: 10.1038/s41598-021-98731-0
7. Sun, C, Pezic, A, Tikellis, G, Ponsonby, AL, Wake, M, Carlin, JB, et al. Effects of school-based interventions for direct delivery of physical activity on fitness and cardiometabolic markers in children and adolescents: a systematic review of randomized controlled trials. Obes Rev. (2013) 14:818–38. doi: 10.1111/obr.12047
8. Fox, KR, Cooper, A, and McKenna, J. The school and promotion of children’s health-enhancing physical activity: perspectives from the United Kingdom. J Teach Phys Educ. (2004) 23:338–58. doi: 10.1123/jtpe.23.4.338
9. Love, R, Adams, J, and van Sluijs, EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev. (2019) 20:859–70. doi: 10.1111/obr.12823
10. Pozuelo-Carrascosa, DP, García-Hermoso, A, Álvarez-Bueno, C, Sánchez-López, M, and Martinez-Vizcaino, V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: a meta-analysis of randomised controlled trials. Br J Sports Med. (2018) 52:1234–40. doi: 10.1136/bjsports-2017-097600
11. Minatto, G, Barbosa Filho, VC, Berria, J, and Petroski, EL. School-based interventions to improve cardiorespiratory fitness in adolescents: systematic review with Meta-analysis. Sports Med. (2016) 46:1273–92. doi: 10.1007/s40279-016-0480-6
12. Lin, J, Zhang, R, Shen, J, and Zhou, A. Effects of school-based neuromuscular training on fundamental movement skills and physical fitness in children: a systematic review. PeerJ. (2022) 10:e13726. doi: 10.7717/peerj.13726
13. Duncombe, SL, Barker, AR, Bond, B, Earle, R, Varley-Campbell, J, Vlachopoulos, D, et al. School-based high-intensity interval training programs in children and adolescents: a systematic review and meta-analysis. PLoS One. (2022) 17:e0266427. doi: 10.1371/journal.pone.0266427
14. Bauer, N, Sperlich, B, Holmberg, HC, and Engel, FA. Effects of high-intensity interval training in school on the physical performance and health of children and adolescents: a systematic review with Meta-analysis. Sports Med Open. (2022) 8:50. doi: 10.1186/s40798-022-00437-8
15. Podnar, H, Jurić, P, Karuc, J, Saez, M, Barceló, MA, Radman, I, et al. Comparative effectiveness of school-based interventions targeting physical activity, physical fitness or sedentary behaviour on obesity prevention in 6- to 12-year-old children: a systematic review and meta-analysis. Obes Rev. (2021) 22:e13160. doi: 10.1111/obr.13160
16. Gao, Z, and Chen, S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Obes Rev. (2014) 15:676–91. doi: 10.1111/obr.12164
17. Oliveira, CB, Pinto, RZ, Saraiva, BTC, Tebar, WR, Delfino, LD, Franco, MR, et al. Effects of active video games on children and adolescents: a systematic review with meta-analysis. Scand J Med Sci Sports. (2020) 30:4–12. doi: 10.1111/sms.13539
18. Hill-Haas, SV, Dawson, B, Impellizzeri, FM, and Coutts, AJ. Physiology of small-sided games training in football: a systematic review. Sports Med. (2011) 41:199–220. doi: 10.2165/11539740-000000000-00000
19. Su, X, McDonough, DJ, Chu, H, Quan, M, and Gao, Z. Application of network meta-analysis in the field of physical activity and health promotion. J Sport Health Sci. (2020) 9:511–20. doi: 10.1016/j.jshs.2020.07.011
20. Hutton, B, Salanti, G, Caldwell, D, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analysis of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
21. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. Cochrane statistical methods group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
22. Higgins, J, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, M, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester (UK): John Wiley & Sons (2019).
24. Lau, PW, Wang, JJ, and Maddison, R. A randomized-controlled trial of school-based active videogame intervention on Chinese Children's aerobic fitness, physical activity level, and psychological correlates. Games Health J. (2016) 5:405–12. doi: 10.1089/g4h.2016.0057
25. Liang, Y, Lau, PWC, Jiang, Y, and Maddison, R. Getting active with active video games: a quasi-experimental study. Int J Environ Res Public Health. (2020) 17:7984. doi: 10.3390/ijerph17217984
26. Ketelhut, S, Roglin, L, Martin-Niedecken, AL, Nigg, CR, and Ketelhut, K. Integrating regular exergaming sessions in the Exer cube into a school setting increases physical fitness in elementary school children: a randomized controlled trial. J Clin Med. (2022) 11:1570. doi: 10.3390/jcm11061570
27. Comeras-Chueca, C, Villalba-Heredia, L, Perez-Lasierra, JL, Marín-Puyalto, J, Lozano-Berges, G, Matute-Llorente, Á, et al. Active video games improve muscular fitness and motor skills in children with overweight or obesity. Int J Environ Res Public Health. (2022) 19:2642. doi: 10.3390/ijerph19052642
28. Ye, S, Lee, JE, Stodden, DF, and Gao, Z. Impact of exergaming on Children's motor skill competence and health-related fitness: a quasi-experimental study. J Clin Med. (2018) 7:261. doi: 10.3390/jcm7090261
29. Comeras-Chueca, C, Villalba-Heredia, L, Perez-Lasierra, JL, Lozano-Berges, G, Matute-Llorente, A, Vicente-Rodriguez, G, et al. Effect of an active video game intervention combined with multicomponent exercise for cardiorespiratory fitness in children with overweight and obesity: randomized controlled trial. JMIR Serious Games. (2022) 10:e33782. doi: 10.2196/33782
30. Chen, H, and Sun, H. Effects of active videogame and sports, play, and active recreation for kids physical education on Children's health-related fitness and enjoyment. Games Health J. (2017) 6:312–8. doi: 10.1089/g4h.2017.0001
31. Lau, PW, Wang, G, and Wang, JJ. Effectiveness of active video game usage on body composition, physical activity level and motor proficiency in children with intellectual disability. J Appl Res Intellect Disabil. (2020) 33:1465–77. doi: 10.1111/jar.12774
32. Petrusic, T, Trajkovic, N, and Bogataj, S. Twelve-week game-based school intervention improves physical fitness in 12-14-year-old girls. Front Public Health. (2022) 10:831424. doi: 10.3389/fpubh.2022.831424
33. Trajkovic, N, Lazic, A, Trkulja-Petkovic, D, Barišić, V, Milić, V, Nikolić, S, et al. Effects of after-school volleyball program on body composition in overweight adolescent girls. Children. (2021) 9:21. doi: 10.3390/children9010021
34. Trajkovic, N, Pajek, M, Sporis, G, Petrinović, L, and Bogataj, Š. Reducing aggression and improving physical fitness in adolescents through an after-school volleyball program. Front Psychol. (2020) 11:2081. doi: 10.3389/fpsyg.2020.02081
35. Trajkovic, N, Madic, DM, Milanovic, Z, Mačak, D, Padulo, J, Krustrup, P, et al. Eight months of school-based soccer improves physical fitness and reduces aggression in high-school children. Biol Sport. (2020) 37:185–93. doi: 10.5114/biolsport.2020.94240
36. Cvetkovic, N, Stojanovic, E, Stojiljkovic, N, Nikolić, D, Scanlan, AT, and Milanović, Z. Exercise training in overweight and obese children: recreational football and high-intensity interval training provide similar benefits to physical fitness. Scand J Med Sci Sports. (2018) 28:18–32. doi: 10.1111/sms.13241
37. Larsen, MN, Nielsen, CM, Ørntoft, C, Randers, MB, Helge, EW, Madsen, M, et al. Fitness effects of 10-month frequent Low-volume ball game training or interval running for 8-10-year-old school children. Biomed Res Int. (2017) 2017:2719752. doi: 10.1155/2017/2719752
38. Latorre-Roman, PA, Mora-Lopez, D, and Garcia-Pinillos, F. Effects of a physical activity programme in the school setting on physical fitness in preschool children. Child Care Health Dev. (2018) 44:427–32. doi: 10.1111/cch.12550
39. Krustrup, P, Hansen, PR, Nielsen, CM, Larsen, MN, Randers, MB, Manniche, V, et al. Structural and functional cardiac adaptations to a 10-week school-based football intervention for 9-10-year-old children. Scand J Med Sci Sports. (2014) 24:4–9. doi: 10.1111/sms.12277
40. Skoradal, MB, Purkhús, E, Steinholm, H, Olsen, MH, Ørntoft, C, Larsen, MN, et al. "FIFA 11 for health" for Europe in the Faroe Islands: effects on health markers and physical fitness in 10- to 12-year-old schoolchildren. Scand J Med Sci Sports. (2018) 28:8–17. doi: 10.1111/sms.13209
41. Larsen, MN, Nielsen, CM, Helge, EW, Madsen, M, Manniche, V, Hansen, L, et al. Positive effects on bone mineralisation and muscular fitness after 10 months of intense school-based physical training for children aged 8-10 years: the FIT FIRST randomised controlled trial. Br J Sports Med. (2018) 52:254–60. doi: 10.1136/bjsports-2016-096219
42. Ryom, K, Christiansen, SR, Elbe, AM, Aggestrup, CS, Madsen, EE, Madsen, M, et al. The Danish "11 for health" program raises health knowledge, well-being, and fitness in ethnic minority 10- to 12-year-olds. Scand J Med Sci Sports. (2022) 32:138–51. doi: 10.1111/sms.14057
43. Camacho-Cardenosa, A, Brazo-Sayavera, J, Camacho-Cardenosa, M, Marcos-Serrano, M, Timón, R, and Olcina, G. Effects of high intensity interval training on fat mass parameters in adolescents. Rev Esp Salud Publica. (2016) 90:e1–9.
44. Cao, M, Tang, Y, and Zou, Y. Integrating high-intensity interval training into a school setting improve body composition, cardiorespiratory fitness and physical activity in children with obesity: a randomized controlled trial. J Clin Med. (2022) 11:5436. doi: 10.3390/jcm11185436
45. Delgado-Floody, P, Espinoza-Silva, M, Garcia-Pinillos, F, and Latorre-Román, P. Effects of 28 weeks of high-intensity interval training during physical education classes on cardiometabolic risk factors in Chilean schoolchildren: a pilot trial. Eur J Pediatr. (2018) 177:1019–27. doi: 10.1007/s00431-018-3149-3
46. Martin, R, Buchan, DS, Baker, JS, Young, J, Sculthorpe, N, and Grace, FM. Sprint interval training (SIT) is an effective method to maintain cardiorespiratory fitness (CRF) and glucose homeostasis in Scottish adolescents. Biol Sport. (2015) 32:307–13. doi: 10.5604/20831862.1173644
47. Martin-Smith, R, Buchan, DS, Baker, JS, Macdonald, MJ, Sculthorpe, NF, Easton, C, et al. Sprint interval training and the school curriculum: benefits upon cardiorespiratory fitness, physical activity profiles, and Cardiometabolic risk profiles of healthy adolescents. Pediatr Exerc Sci. (2019) 31:296–305. doi: 10.1123/pes.2018-0155
48. Martinez-Vizcaino, V, Soriano-Cano, A, Garrido-Miguel, M, Cavero-Redondo, I, Medio, EP, Madrid, VM, et al. The effectiveness of a high-intensity interval games intervention in schoolchildren: a cluster-randomized trial. Scand J Med Sci Sports. (2022) 32:765–81. doi: 10.1111/sms.14113
49. Meng, C, Yucheng, T, Shu, L, and Yu, Z. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: a randomized controlled trial. BMC Pediatr. (2022) 22:112. doi: 10.1186/s12887-021-03079-z
50. Alonso-Fernández, D, Fernández-Rodríguez, R, Taboada-Iglesias, Y, and Gutiérrez-Sánchez, A. Impact of a HIIT protocol on body composition and VO2max in adolescents. Sci Sports. (2019) 34:341–7. doi: 10.1016/j.scispo.2019.04.001
51. Bogataj, Š, Trajković, N, Cadenas-Sanchez, C, and Sember, V. Effects of school-based exercise and nutrition intervention on body composition and physical fitness in overweight adolescent girls. Nutrients. (2021) 13:238. doi: 10.3390/nu13010238
52. Costigan, SA, Eather, N, Plotnikoff, RC, Taaffe, DR, Pollock, E, Kennedy, SG, et al. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: a pilot randomized controlled trial. Prev Med Rep. (2015) 2:973–9. doi: 10.1016/j.pmedr.2015.11.001
53. Martínez, SR, Ríos, LJC, Tamayo, IM, Almedia, LG, López-Gomez, MA, and Jara, CC. An after-school, high-intensity, interval physical activity programme improves health-related fitness in children. Motriz Revista de Educação Física. (2016) 22:359–67. doi: 10.1590/S1980-6574201600040022
54. Engel, FA, Wagner, MO, Schelhorn, F, Deubert, F, Leutzsch, S, Stolz, A, et al. Classroom-based Micro-sessions of functional high-intensity circuit training enhances functional strength but not cardiorespiratory fitness in school children-a feasibility study. Front Public Health. (2019) 7:291. doi: 10.3389/fpubh.2019.00291
55. Lambrick, D, Westrupp, N, Kaufmann, S, Stoner, L, and Faulkner, J. The effectiveness of a high-intensity games intervention on improving indices of health in young children. J Sports Sci. (2016) 34:190–8. doi: 10.1080/02640414.2015.1048521
56. Baquet, G, Gamelin, FX, Mucci, P, Thévenet, D, Van Praagh, E, and Berthoin, S. Continuous vs. interval aerobic training in 8- to 11-year-old children. J Strength Cond Res. (2010) 24:1381–8. doi: 10.1519/JSC.0b013e3181d1575a
57. Baquet, G, Guinhouya, C, Dupont, G, Nourry, C, and Berthoin, S. Effects of a short-term interval training program on physical fitness in prepubertal children. J Strength Cond Res. (2004) 18:708–13. doi: 10.1519/13813.1
58. Gamelin, FX, Baquet, G, Berthoin, S, Thevenet, D, Nourry, C, Nottin, S, et al. Effect of high intensity intermittent training on heart rate variability in prepubescent children. Eur J Appl Physiol. (2009) 105:731–8. doi: 10.1007/s00421-008-0955-8
59. Leahy, AA, Eather, N, Smith, JJ, Hillman, CH, Morgan, PJ, Plotnikoff, RC, et al. Feasibility and preliminary efficacy of a teacher-facilitated high-intensity interval training intervention for older adolescents. Pediatr Exerc Sci. (2019) 31:107–17. doi: 10.1123/pes.2018-0039
60. McNarry, MA, Winn, CON, Davies, GA, Eddolls, WTB, and Mackintosh, KA. Effect of high-intensity training and asthma on the VO2 kinetics of adolescents. Med Sci Sports Exerc. (2020) 52:1322–9. doi: 10.1249/MSS.0000000000002270
61. Racil, G, Ben Ounis, O, Hammouda, O, Kallel, A, Zouhal, H, Chamari, K, et al. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. (2013) 113:2531–40. doi: 10.1007/s00421-013-2689-5
62. Racil, G, Coquart, JB, Elmontassar, W, Haddad, M, Goebel, R, Chaouachi, A, et al. Greater effects of high-compared with moderate-intensity interval training on cardio-metabolic variables, blood leptin concentration and ratings of perceived exertion in obese adolescent females. Biol Sport. (2016) 33:145–52. doi: 10.5604/20831862.1198633
63. Harris, N, Warbrick, I, Atkins, D, Vandal, A, Plank, L, and Lubans, DR. Feasibility and provisional efficacy of embedding high-intensity interval training into physical education lessons: a pilot cluster-randomized controlled trial. Pediatr Exerc Sci. (2021) 33:186–95. doi: 10.1123/pes.2020-0255
64. Jurić, P, Dudley, DA, and Petocz, P. Does incorporating high intensity interval training in physical education classes improve fitness outcomes of students? A cluster randomized controlled trial. Prev Med Rep. (2023) 32:102127. doi: 10.1016/j.pmedr.2023.102127
65. Cataldi, S, Francavilla, VC, Bonavolonta, V, De Florio, O, Carvutto, R, De Candia, M, et al. Proposal for a fitness program in the school setting during the COVID 19 pandemic: effects of an 8-week cross fit program on psychophysical well-being in healthy adolescents. Int J Environ Res Public Health. (2021) 18:3141. doi: 10.3390/ijerph18063141
66. Cohen, DD, Sandercock, GR, Camacho, PA, Otero-Wandurraga, J, Romero, SMP, Marín, RDPM, et al. The SIMAC study: a randomized controlled trial to compare the effects of resistance training and aerobic training on the fitness and body composition of Colombian adolescents. PLoS One. (2021) 16:e0248110. doi: 10.1371/journal.pone.0248110
67. Yoshimoto, T, Takai, Y, Fukunaga, Y, Fujita, E, Yamamoto, M, and Kanehisa, H. Effects of school-based squat training in adolescent girls. J Sports Med Phys Fitness. (2016) 56:678–83.
68. Alves, AR, Marta, CC, Neiva, HP, Izquierdo, M, and Marques, MC. Concurrent training in prepubescent children: the effects of 8 Weeks of strength and aerobic training on explosive strength and VO2max. J Strength Cond Res. (2016) 30:2019–32. doi: 10.1519/JSC.0000000000001294
69. Santos, A, Marinho, DA, Costa, AM, Izquierdo, M, and Marques, MC. The effects of concurrent resistance and endurance training follow a specific detraining cycle in young school girls. J Hum Kinet. (2011) 29A:93–103. doi: 10.2478/v10078-011-0064-3
70. Dorgo, S, King, GA, Candelaria, NG, Bader, JO, Brickey, GD, and Adams, CE. The effects of manual resistance training on fitness in adolescents. J Strength Cond Res. (2009) 23:2287–94. doi: 10.1519/JSC.0b013e3181b8d42a
71. Santos, AP, Marinho, DA, Costa, AM, Izquierdo, M, and Marques, MC. The effects of concurrent resistance and endurance training follow a detraining period in elementary school students. J Strength Cond Res. (2012) 26:1708–16. doi: 10.1519/JSC.0b013e318234e872
72. Kennedy, SG, Smith, JJ, Morgan, PJ, Peralta, LR, Hilland, TA, Eather, N, et al. Implementing resistance training in secondary schools: a cluster randomized controlled trial. Med Sci Sports Exerc. (2018) 50:62–72. doi: 10.1249/MSS.0000000000001410
73. Eather, N, Morgan, PJ, and Lubans, DR. Improving health-related fitness in adolescents: the cross fit teens randomised controlled trial. J Sports Sci. (2016) 34:209–23. doi: 10.1080/02640414.2015.1045925
74. Zhao, M, Liu, S, Han, X, Li, Z, Liu, B, Chen, J, et al. School-based comprehensive strength training interventions to improve muscular fitness and perceived physical competence in Chinese male adolescents. Biomed Res Int. (2022) 2022:7464815–14. doi: 10.1155/2022/7464815
75. Muehlbauer, T, Gollhofer, A, and Granacher, U. Sex-related effects in strength training during adolescence: a pilot study. Percept Mot Skills. (2012) 115:953–68. doi: 10.2466/06.10.30
76. Alves, AR, Marta, CC, Neiva, HP, Izquierdo, M, and Marques, MC. Effects of order and sequence of resistance and endurance training on body fat in elementary school-aged girls. Biol Sport. (2017) 34:379–84. doi: 10.5114/biolsport.2017.69826
77. Lubans, DR, Sheaman, C, and Callister, R. Exercise adherence and intervention effects of two school-based resistance training programs for adolescents. Prev Med. (2010) 50:56–62. doi: 10.1016/j.ypmed.2009.12.003
78. Granacher, U, Goesele, A, Roggo, K, Wischer, T, Fischer, S, Zuerny, C, et al. Effects and mechanisms of strength training in children. Int J Sports Med. (2011) 32:357–64. doi: 10.1055/s-0031-1271677
79. Winwood, PW, and Buckley, JJ. Short-term effects of resistance training modalities on performance measures in male adolescents. J Strength Cond Res. (2019) 33:641–50. doi: 10.1519/JSC.0000000000001992
80. Marta, C, Alves, AR, Esteves, PT, Casanova, N, Marinho, D, Neiva, HP, et al. Effects of suspension versus traditional resistance training on explosive strength in elementary school-aged boys. Pediatr Exerc Sci. (2019) 31:473–8. doi: 10.1123/pes.2018-0287
81. Robinson, KJ, Lubans, DR, Mavilidi, MF, Hillman, CH, Benzing, V, Valkenborghs, SR, et al. Effects of classroom-based resistance training with and without cognitive training on Adolescents' cognitive function, on-task behavior, and muscular fitness. Front Psychol. (2022) 13:811534. doi: 10.3389/fpsyg.2022.811534
82. Velez, A, Golem, DL, and Arent, SM. The impact of a 12-week resistance training program on strength, body composition, and self-concept of Hispanic adolescents. J Strength Cond Res. (2010) 24:1065–73. doi: 10.1519/JSC.0b013e3181cc230a
83. Sun, MX, Huang, XQ, Yan, Y, Li, BW, Zhong, WJ, Chen, JF, et al. One-hour after-school exercise ameliorates central adiposity and lipids in overweight Chinese adolescents: a randomized controlled trial. Chin Med J. (2011) 124:323–9.
84. van der Fels, IMJ, Hartman, E, Bosker, RJ, de Greeff, JW, de Bruijn, AGM, Meijer, A, et al. Effects of aerobic exercise and cognitively engaging exercise on cardiorespiratory fitness and motor skills in primary school children: a cluster randomized controlled trial. J Sports Sci. (2020) 38:1975–83. doi: 10.1080/02640414.2020.1765464
85. Tan, S, Chen, C, Sui, M, Xue, L, and Wang, J. Exercise training improved body composition, cardiovascular function, and physical fitness of 5-year-old children with obesity or Normal body mass. Pediatr Exerc Sci. (2017) 29:245–53. doi: 10.1123/pes.2016-0107
86. Walther, C, Gaede, L, Adams, V, Gelbrich, G, Leichtle, A, Erbs, S, et al. Effect of increased exercise in school children on physical fitness and endothelial progenitor cells: a prospective randomized trial. Circulation. (2009) 120:2251–9. doi: 10.1161/CIRCULATIONAHA.109.865808
87. Song, JK, Stebbins, CL, Kim, TK, Kim, HB, Kang, HJ, and Chai, JH. Effects of 12 weeks of aerobic exercise on body composition and vascular compliance in obese boys. J Sports Med Phys Fitness. (2012) 52:522–9.
88. Cohen, DD, Carreño, J, Camacho, PA, Otero, J, Martinez, D, Lopez-Lopez, J, et al. Fitness changes in adolescent girls following in-school combined aerobic and resistance exercise: interaction with birthweight. Pediatr Exerc Sci. (2022) 34:76–83. doi: 10.1123/pes.2021-0034
89. Wong, PC, Chia, MY, Tsou, IY, Wansaicheong, GK, Tan, B, Wang, JC, et al. Effects of a 12-week exercise training programme on aerobic fitness, body composition, blood lipids and C-reactive protein in adolescents with obesity. Ann Acad Med Singap. (2008) 37:286–93. doi: 10.47102/annals-acadmedsg.V37N4p286
90. Liu, J, Zhu, L, and Su, Y. Comparative effectiveness of high-intensity interval training and moderate-intensity continuous training for Cardiometabolic risk factors and cardiorespiratory fitness in childhood obesity: a Meta-analysis of randomized controlled trials. Front Physiol. (2020) 11:214. doi: 10.3389/fphys.2020.00214
91. Utesch, T, Dreiskämper, D, Naul, R, and Geukes, K. Understanding physical (in-) activity, overweight, and obesity in childhood: effects of congruence between physical self-concept and motor competence. Sci Rep. (2018) 8:5908. doi: 10.1038/s41598-018-24139-y
92. Millstein, RA . Measuring outcomes in adult weight loss studies that include diet and physical activity: a systematic review. J Nutr Metab. (2014) 2014:421423. doi: 10.1155/2014/421423
93. Batrakoulis, A, Jamurtas, AZ, Metsios, GS, Perivoliotis, K, Liguori, G, Feito, Y, et al. Comparative efficacy of 5 exercise types on Cardiometabolic health in overweight and obese adults: a systematic review and network Meta-analysis of 81 randomized controlled trials. Circ Cardiovasc Qual Outcomes. (2022) 15:e008243. doi: 10.1161/CIRCOUTCOMES.121.008243
94. Van Gaal, LF, Mertens, IL, and De Block, CE. Mechanisms linking obesity with cardiovascular disease. Nature. (2006) 444:875–80. doi: 10.1038/nature05487
95. de Koning, L, Merchant, AT, Pogue, J, and Anand, SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. (2007) 28:850–6. doi: 10.1093/eurheartj/ehm026
96. Costigan, SA, Eather, N, Plotnikoff, RC, Taaffe, DR, and Lubans, DR. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. (2015) 49:1253–61. doi: 10.1136/bjsports-2014-094490
97. Yarizadeh, H, Eftekhar, R, Anjom-Shoae, J, Speakman, JR, and Djafarian, K. The effect of aerobic and resistance training and combined exercise modalities on subcutaneous abdominal fat: a systematic review and Meta-analysis of randomized clinical trials. Adv Nutr. (2021) 12:179–96. doi: 10.1093/advances/nmaa090
98. Ho, RS, Chan, EK, Liu, KK, and Wong, SH. Active video game on children and adolescents' physical activity and weight management: a network meta-analysis. Scand J Med Sci Sports. (2022) 32:1268–86. doi: 10.1111/sms.14176
99. Gao, Z, Zeng, N, McDonough, DJ, and Su, X. A systematic review of active video games on Youth's body composition and physical activity. Int J Sports Med. (2020) 41:561–73. doi: 10.1055/a-1152-4959
100. García-Hermoso, A, Ramírez-Campillo, R, and Izquierdo, M. Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and Meta-analysis of longitudinal studies. Sports Med. (2019) 49:1079–94. doi: 10.1007/s40279-019-01098-6
101. Villa-González, E, Barranco-Ruiz, Y, García-Hermoso, A, and Faigenbaum, AD. Efficacy of school-based interventions for improving muscular fitness outcomes in children: a systematic review and meta-analysis. Eur J Sport Sci. (2023) 23:444–59. doi: 10.1080/17461391.2022.2029578
102. Stricker, PR, Faigenbaum, AD, and McCambridge, TM, COUNCIL ON SPORTS MEDICINE AND FITNESS. Resistance training for children and adolescents. Pediatrics. (2020) 145:e20201011. doi: 10.1542/peds.2020-1011
103. Peitz, M, Behringer, M, and Granacher, U. A systematic review on the effects of resistance and plyometric training on physical fitness in youth—what do comparative studies tell us? PLoS One. (2018) 13:e0205525. doi: 10.1371/journal.pone.0205525
104. Nathan, N, Elton, B, Babic, M, McCarthy, N, Sutherland, R, Presseau, J, et al. Barriers and facilitators to the implementation of physical activity policies in schools: a systematic review. Prev Med. (2018) 107:45–53. doi: 10.1016/j.ypmed.2017.11.012
105. Oppici, L, Stell, FM, Utesch, T, Woods, CT, Foweather, L, and Rudd, JR. A skill acquisition perspective on the impact of exergaming technology on foundational movement skill development in children 3-12 years: a systematic review and Meta-analysis. Sports Med Open. (2022) 8:148. doi: 10.1186/s40798-022-00534-8
106. Liu, W, Zeng, N, McDonough, DJ, and Gao, Z. Effect of active video games on healthy Children's fundamental motor skills and physical fitness: a systematic review. Int J Environ Res Public Health. (2020) 17:8264. doi: 10.3390/ijerph17218264
107. Tompsett, C, Sanders, R, Taylor, C, and Cobley, S. Pedagogical approaches to and effects of fundamental movement skill interventions on health outcomes: a systematic review. Sports Med. (2017) 47:1795–819. doi: 10.1007/s40279-017-0697-z
108. Yang, J, Christophi, CA, Farioli, A, Baur, DM, Moffatt, S, Zollinger, TW, et al. Association between push-up exercise capacity and future cardiovascular events among active adult men. JAMA Netw Open. (2019) 2:e188341. doi: 10.1001/jamanetworkopen.2018.8341
109. Alberga, AS, Prud'homme, D, Sigal, RJ, Goldfield, GS, Hadjiyannakis, S, Phillips, P, et al. Effects of aerobic training, resistance training, or both on cardiorespiratory and musculoskeletal fitness in adolescents with obesity: the HEARTY trial. Appl Physiol Nutr Metab. (2016) 41:255–65. doi: 10.1139/apnm-2015-0413
110. Eather, N, Riley, N, Miller, A, Smith, V, Poole, A, Vincze, L, et al. Efficacy and feasibility of HIIT training for university students: the Uni-HIIT RCT. J Sci Med Sport. (2019) 22:596–601. doi: 10.1016/j.jsams.2018.11.016
111. McQuilliam, SJ, Clark, DR, Erskine, RM, and Brownlee, TE. Free-weight resistance training in youth athletes: a narrative review. Sports Med. (2020) 50:1567–80. doi: 10.1007/s40279-020-01307-7
112. Behm, DG, Young, JD, Whitten, JHD, Reid, JC, Quigley, PJ, Low, J, et al. Effectiveness of traditional strength vs. power training on muscle strength, power and speed with youth: a systematic review and Meta-analysis. Front Physiol. (2017) 8:423. doi: 10.3389/fphys.2017.00423
113. de Oliveira-Nunes, SG, Castro, A, Sardeli, AV, Cavaglieri, CR, and MPT, C-M. HIIT vs. SIT: what is the better to improve V˙O2max? A systematic review and Meta-analysis. Int J Environ Res Public Health. (2021) 18:13120. doi: 10.3390/ijerph182413120
114. McKinlay, BJ, Wallace, P, Dotan, R, Long, D, Tokuno, C, Gabriel, DA, et al. Effects of plyometric and resistance training on muscle strength, explosiveness, and neuromuscular function in Young adolescent soccer players. J Strength Cond Res. (2018) 32:3039–50. doi: 10.1519/JSC.0000000000002428
115. Cormie, P, McGuigan, MR, and Newton, RU. Changes in the eccentric phase contribute to improved stretch-shorten cycle performance after training. Med Sci Sports Exerc. (2010) 42:1731–44. doi: 10.1249/MSS.0b013e3181d392e8
116. Liao, KF, Wang, XX, Han, MY, Li, LL, Nassis, GP, and Li, YM. Effects of velocity based training vs. traditional 1RM percentage-based training on improving strength, jump, linear sprint and change of direction speed performance: a systematic review with meta-analysis. PLoS One. (2021) 16:e0259790. doi: 10.1371/journal.pone.0259790
117. Lema-Gómez, L, Arango-Paternina, CM, Eusse-López, C, Petro, J, Petro-Petro, J, López-Sánchez, M, et al. Family aspects, physical fitness, and physical activity associated with mental-health indicators in adolescents. BMC Public Health. (2021) 21:2324. doi: 10.1186/s12889-021-12403-2
118. Santana, CCA, Azevedo, LB, Cattuzzo, MT, Hill, JO, Andrade, LP, and Prado, WL. Physical fitness and academic performance in youth: a systematic review. Scand J Med Sci Sports. (2017) 27:579–603. doi: 10.1111/sms.12773
119. Raghuveer, G, Hartz, J, Lubans, DR, Takken, T, Wiltz, JL, Mietus-Snyder, M, et al. Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association. Circulation. (2020) 142:e101–18. doi: 10.1161/CIR.0000000000000866
120. Gripp, F, Nava, RC, Cassilhas, RC, Esteves, EA, Magalhães, COD, Dias-Peixoto, MF, et al. HIIT is superior than MICT on cardiometabolic health during training and detraining. Eur J Appl Physiol. (2021) 121:159–72. doi: 10.1007/s00421-020-04502-6
121. Menz, V, Marterer, N, Amin, SB, Faulhaber, M, Hansen, AB, and Lawley, JS. Functional vs. running Low-volume high-intensity interval training: effects on VO2max and muscular endurance. J Sports Sci Med. (2019) 18:497–504.
122. Martland, R, Mondelli, V, Gaughran, F, and Stubbs, B. Can high-intensity interval training improve physical and mental health outcomes? A meta-review of 33 systematic reviews across the lifespan. J Sports Sci. (2020) 38:430–69. doi: 10.1080/02640414.2019.1706829
Keywords: adolescents, school-based exercise, physical fitness, children, network meta-analysis
Citation: Wu J, Yang Y, Yu H, Li L, Chen Y and Sun Y (2023) Comparative effectiveness of school-based exercise interventions on physical fitness in children and adolescents: a systematic review and network meta-analysis. Front. Public Health. 11:1194779. doi: 10.3389/fpubh.2023.1194779
Received: 27 March 2023; Accepted: 18 May 2023;
Published: 05 June 2023.
Edited by:
Shooka Mohammadi, University of Malaya, MalaysiaReviewed by:
Ai Kah Ng, University of Malaya, MalaysiaCopyright © 2023 Wu, Yang, Yu, Li, Chen and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin Wu, NTIyMTEwMDAwMTdAc3R1LmVjbnUuZWR1LmNu; Youping Sun, eXBzdW5AdHl4eC5lY251LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.