- Department of Sociology, HeDeRa (Health and Demographic Research), Ghent University, Ghent, Belgium
Introduction: The use of psychotropics, such as benzodiazepine receptor agonists (BzRAs), among working-age adults in Belgium has shown educational differences. However, it is unclear how work status plays a role in this relationship. Therefore, this research aims to investigate whether work status explains observed educational differences in BzRA use. In addition, considering medicalisation processes, where non-medical factors, such as work status, are increasingly associated with medical mental health care-seeking behavior, this research also aims to investigate whether work status explains observed educational differences in BzRA use, regardless of mental health status.
Methods: Data are obtained from the Belgian Health Interview Survey (BHIS). Four successive waves are covered: 2004, 2008, 2013, and 2018. The weighted data represent a sample of 18,547 Belgian respondents aged 18 to 65 years old. Poisson regression models are used to analyze the research aims. Time evolutions are plotted using marginal means postestimation.
Results: The average use of BzRAs shows a slight decline over the waves studied (2004 = 5.99, 2008 = 5.88, 2013 = 5.33, 2018 = 4.31). Educational and work status differences in BzRA use are observed, regardless of mental health status. Individuals with longer education report lower use compared to individuals with shorter education, and individuals who are unemployed, (pre-)retired, or sick or disabled report higher use compared to employed individuals. Furthermore, work status acts as a mediator, partially explaining educational differences in BzRA use, regardless of mental health status.
Discussion: Work-related uncertainty leads to increased prescribing and medication use, regardless of mental health. Medicalisation and pharmaceuticalisation processes detach social problems from their social roots and treat them as personal failures. The marginalization of the social roots of unemployment, sick leave and involuntary (pre-)retirement has led to a personalization of responsibility. Negative feelings arising from such work statuses may cause isolated, non-specific symptoms for which medical treatment is sought.
Introduction
Benzodiazepine receptor agonists (BzRAs), which include benzodiazepines and Z-products, are widely prescribed for the treatment of anxiety, nervousness and sleep problems (1–5). While BzRAs can have initial beneficial anxiolytic and sedative effects, their use also leads to risks of developing tolerance, dependence, withdrawal symptoms and severe adverse effects, such as impaired cognitive functioning and driving skills and an increased risk of falls and hip fractures (6, 7). These risks already appear after 2 to 4 weeks of use and are particularly elevated among long-term users (8).
For over two decades, the Belgian Federal Service of Public Health has launched awareness campaigns to decrease anxiolytic-sedative consumption in Belgium (9). Reports and studies that followed have mainly focused on BzRA use by older Belgians (65+ years) (10–12). Hence, it is also important to examine other understudied age groups, such as working-age adults, who are especially prone to experience daily mental stressors from multiple life domains, such as work and personal life. These stressors, along with work-life spillover effects, may influence BzRA use (13, 14).
Recent Belgian studies on the use of psychotropics, like benzodiazepines, Z-products and antidepressants, have shown clear educational differences in use among working-age adults, with these differences persisting over time (15, 16). These educational differences in use may be partially attributed to differences in work status. Education is the most important mechanism of labor market allocation in credential societies and strongly influences work status (17). However, while work status is a crucial factor to consider when analyzing BzRA use among working-age adults, no prior empirical studies, to the best of our knowledge, have examined this. Therefore, this research aims to explore the mediating role of work status in relation to BzRA use.
Mostly, researchers assume that individuals with shorter education are more at risk of using BzRAs because they are less likely to have a favorable and stable work status, with an increased risk of unemployment and involuntary (pre-)retirement (18–22), which may cause mental health complaints. Studies have already shown that unemployed individuals are more likely to experience poor mental health, and to make greater use of mental health care, including taking antidepressants (23, 24). Unemployed individuals also have a higher chance of substance abuse (25), and pre-retirement as well, relates to higher levels of mental distress (26).
However, we argue that work status may also mediate the relationship between education and the use of BzRAs independently of mental health complaints, due to medicalisation processes. According to Conrad (27) medicalisation is a social process in which normal biological processes or behaviors are increasingly described, accepted and treated as medical problems, leading to increased attention for- and growing consumption of medical treatments. Given these medicalisation processes, non-medical factors, such as work status, are increasingly associated with medical mental health care-seeking behavior (27). Work status is increasingly viewed as a personal responsibility, whereas ‘not being employed' is seen as an individually caused situation (28, 29), with all the negative mental health consequences this may entail.
The purpose of this study is to describe trends in BzRA use among working-age adults in Belgium and to assess (1) to what extent work status explains observed educational differences in BzRA use, and (2) to what extent work status explains observed educational differences in BzRA use, regardless of mental health status. We assume that work status differences in BzRA use, irrespective of mental health status, provide indications of medicalisation. To answer these research questions, data from the Belgian Health Interview Survey (BHIS) covering a wide time span (2004–2018) are used to analyze evolutions in education and work status and differences in BzRA use.
Methods
Sample
The Belgian Health Interview Survey (BHIS) is a repeated cross-sectional survey coordinated by Sciensano, the Scientific Institute of Public Health of the federal Belgian State. Four successive waves are covered: 2004, 2008, 2013, and 2018. Households and their members are selected from the National Register following a multi-stage stratified sampling procedure. Information is collected through face-to-face interviews, as well as through a self-administered questionnaire. After pooling the data and omitting cases with missing values, the final sample includes 18,547 Belgian respondents of working age between 18 and 65 years old (2004 = 5,045 respondents, 2008 = 4,412 respondents, 2013 = 4,076 respondents, 2018 = 5,014 respondents). The waves are well balanced in terms of gender distribution (ratio men/women: 2004 = 49.42/50.58, 2008 = 49.09/50.91, 2013 = 48.77/51.23, 2018 = 49.68/50.32). The average age of respondents across the waves is slightly older, with a mean of 44 years old ( = 43.40, = 43.56, = 44.51, = 45.60). Information on respondent selection criteria and data cleaning are available in Appendix 1a, as well as more information on general sample characteristics (see Appendix 1b).
Variables
Dependent variable
The dependent variable ‘benzodiazepine receptor agonists (BzRA) use' measures the use of benzodiazepines and/or Z-products in the past 24 h.1 Respondents were asked to show the medicines that they had used in the past 24 h, and the interviewer indicated on a list whether the medicines belonged to a specific Anatomical Therapeutic Chemical (ATC) category, which is an internationally accepted classification system for medicines (30). The computed variable consists of two categories: 0 = no BzRA use in the past 24 h, 1 = BzRA use in the past 24 h.
Independent variable
Education is measured as the highest level of education completed and is recoded into three categories according to the International Standard Classification of Education (ISCED) of 2011 (31): 1 = shorter education (pre-primary or primary education), 2 = intermediate education (lower- and upper secondary education) and 3 = longer education (post-secondary or tertiary education) [ref.cat].
Mediation variable
Work status is recoded into five categories: 1 = employed [ref.cat], 2 = unemployed, 3 = non-employed (consisting of two items; housekeeping without benefits and family worker), 4 = sick or disabled and 5 = (pre-)retired. Being sick or disabled is added as a separate category due to a known association with BzRA use (32, 33).
Covariate variables
Several other important variables are considered: household income is recoded into four categories: 1 = low income (1st and 2nd quintile), 2 = medium income (3rd and 4th quintile), 3 = high income (5th quintile) [ref.cat] and 4 = information missing. Gender (0 = man) and country of birth (0 = Belgium) are included as dichotomous variables. Age is recoded into three categories: 1 = 18-34 years old [ref.cat], 2 = 35–49 years old, 3 = 50–65 years old as well as urbanization: 1 = cities-agglomerates [ref.cat], 2=urban-suburban, 3=rural and region: 1 = Flanders [ref.cat], 2 = Brussels, 3 = Wallonia. Wave is incorporated as a categorical variable: 1 = 2004 [ref.cat], 2 = 2008, 3 = 2013, 4 = 2018. GP-contact in the past twelve months (0 = no) and regular GP (0 = no) are added as dichotomous variables along with frequency of social contact (0 = less than once a week). Household composition consists of three categories: 1 = single or one parent household [ref.cat], 2 = couple with or without children living in the household, 3 = another household composition.
This study includes three variables to account for mental health status, namely the presence of depression complains, anxiety complaints and sleeping complaints. Depression complaints (0 = no) is operationalized as a dichotomous variable based on the Patient Health Questionnaire (PHQ-9) (34), which assesses depression symptoms experienced over the past 2 weeks. Additional details on the operationalization of depression complaints are provided in Appendix 2a. Similarly, anxiety complaints is operationalized as a dichotomous variable (0 = no) based on the Generalized Anxiety Disorder questionnaire (GAD-7) (35), which measures anxiety symptoms over the past 2 weeks. Further information on the operationalization of anxiety complaints is available in Appendix 2b. Lastly, a metric variable is included to measure sleeping complaints, specifically, “loss of sleep over worry” experienced in the past 2 weeks.
Statistical procedure
Prevalence rates of BzRA use are calculated using weighted proportions and are stratified by wave and education, as well as wave and work status. Prevalence rates of work status are also reported stratified by education, as well as prevalence rates of BzRA use, stratified by work status and education. After conducting bivariate statistics, four Poisson regression models are estimated. The models estimate incidence rate ratios (IRRs), Z-scores and their corresponding P-values. The first two models are tested without the mental health variables added, with one model without work status included and one model with work status included. The next two models are tested with the mental health variables added, again with one model without work status included and one model with work status included. To concentrate on the mediating effect of work status, we control for several variables that are both related to education and BzRA use (such as income, GP contact, social contact, and so on). Additionally, the results of the tested models are plotted, using marginal means postestimations. Analyses are weighted for survey sampling and non-participation bias and are conducted with SPSS 28 and STATA 15.
Results
Bivariate results presented in Table 1 indicate that individuals with longer education (2.92%) use BzRAs less frequently compared to those with intermediate (6.22%) and shorter education (12.54%). The results also reveal that employed individuals (2.60%) use them the least, while unemployed individuals (7.48%) use them more often than non-employed individuals (6.51%). (Pre-)retired individuals (11.17%) use BzRAs more frequently than those in the previous work status categories. Notably, individuals who are sick or disabled (31.38%) use them significantly more frequently. The results also show a significant decline in use over the observed period (2004 = 5.99%; 2018 = 4.31%). The differences in use based on education and work status remain consistent across the waves. However, in terms of the education gradient, the differences in the last wave are less pronounced due to the sharp decline in use by the shorter educated.
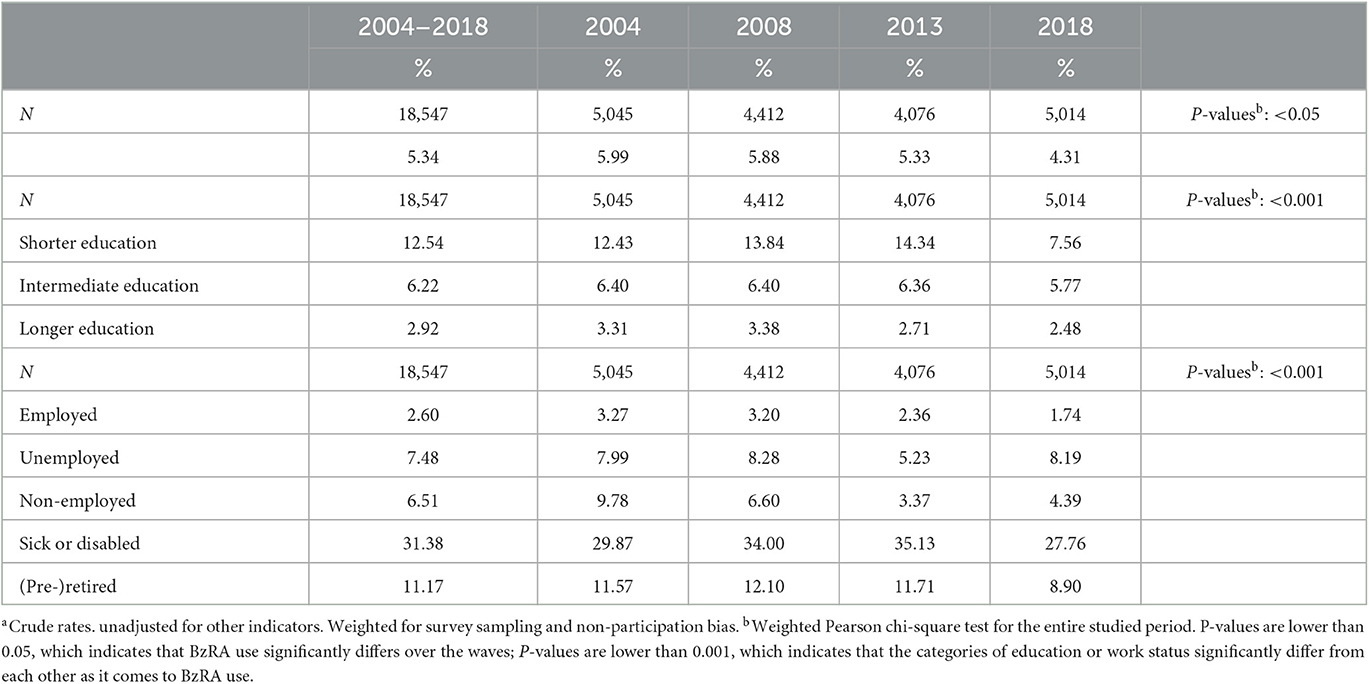
Table 1. Weighted proportionsa of BzRA use in the past 24 h, according to wave, stratified by education and work status.
The results in Table 2 indicate that individuals with longer education (87.31%) are more likely to be employed compared to those with intermediate (67.91%) and shorter education (38.18%). Moreover, individuals with shorter education are more likely to be unemployed, non-employed, (pre-)retired, or sick or disabled than those with intermediate and longer education. Therefore, significant educational differences exist in work status. Regarding BzRA use among different work status categories stratified by education, significant educational differences are observed within the work status categories. In the employed category, individuals with longer education (1.94%) use fewer BzRAs compared to those with shorter education (5.18%), and comparable results are found for the other categories, with major differences. For example, in the non-employed category, individuals with shorter education (10.79%) use them significantly more than those with longer education (1.33%).
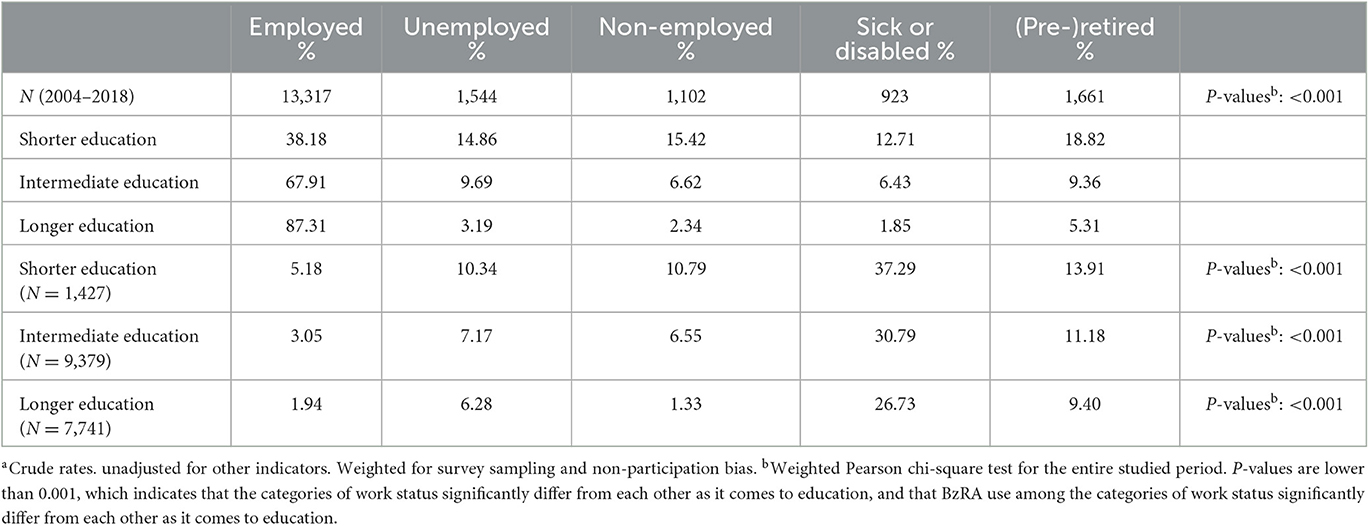
Table 2. Weighted proportionsa of work status, stratified by education; and weighted proportionsa of BzRA use in the past 24 h according to work status, stratified by education.
The Poisson regression results in model 1a (see Table 3) confirm a significant association between education and the use of BzRAs. Specifically, individuals with shorter (IRR 2.15, P < 0.001) and intermediate education (IRR 1.63, P < 0.001) report higher use rates than those with longer education. These educational differences remain significant in model 1b, which includes work status as a covariate. However, the Z-scores of the different education categories decline, suggesting a mediating effect of work status (Z-scores of model 1a compared to model 1b: shorter education = 5.56/3.60, intermediate education = 4.71/2.97). In addition, work status is significantly related to BzRA use, irrespective of education. Specifically, unemployed (IRR 1.89, P < 0.001) and (pre-)retired individuals (IRR 2.13, P < 0.001) use them significantly more than employed individuals. There is no significant difference in use between non-employed (IRR 1.28, P = 0.128) and employed individuals. Sick or disabled individuals (IRR 5.83, P < 0.001) use them significantly more than employed individuals, which is not surprising given their health status.

Table 3. Weighted IRRs, Z-scores, and corresponding P-values of BzRA use in the past 24 h according to education, work status and the covariates.
In model 2a, which includes the mental health variables, education remains significantly associated with BzRA use, with the same interpretation as in model 1a. In model 2b, where work status is included, educational differences remain significant, but the Z-scores indicate a decline in the strength of the associations between the education categories and BzRA use (Z-scores of model 2a compared to model 2b: shorter education = 4.25/3.06, intermediate education = 3.78/2.58). This again suggests that the observed educational differences in use are partially related to differences in work status, and independent from mental health status. Furthermore, significant differences in use according to work status remain, suggesting that the impact of work status on BzRA use is subject to medicalisation processes.
Regarding the covariates, it is noteworthy that there is a significant income gradient in BzRA use, with individuals from households with a lower income having higher use rates than those from households with a higher income. However, differences in mental health status explain this gradient completely, as evidenced by model 2b. In addition, men, non-Belgians and younger working-age adults report lower levels of BzRA use. Conversely, individuals living in Brussels or Wallonia tend to use them more than those residing in Flanders. Moreover, single people and those with infrequent social contact have higher use rates compared to those in relationships or with more frequent social contact. Having a regular GP and recent GP contact are also associated with higher use rates. In 2018, the most recent wave, BzRA use was significantly lower than in 2004 in Model 1a and Model 1b. In Model 2a and Model 2b, this trend already started from 2013 onwards. Additionally, depression-, anxiety- and sleeping complaints are strongly associated with higher use rates.
Figures 1–6 display Poisson regression graphs depicting trends over time. The graphs reveal that the addition of work status (model 1a and model 2a compared to model 1b and model 2b) reduces educational differences, suggesting that work status mediates this relationship. When comparing model 2a&b to model 1a&b, inclusion of the mental health variables results in decreased inequalities and highlights the general declining trend in BzRA use. However, the graph of model 2b still displays differences in use based on individuals' work status, regardless of their education or mental health status.
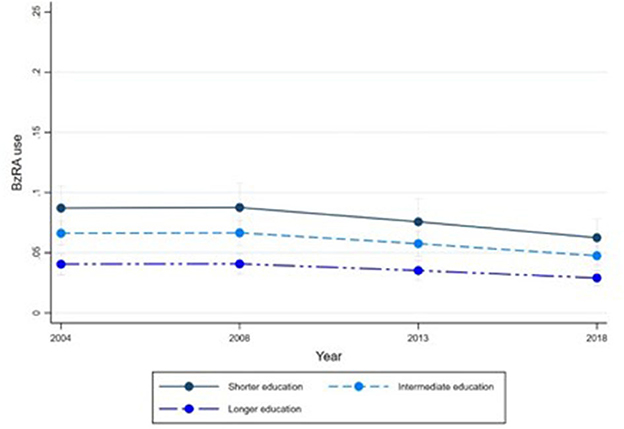
Figure 1. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 1 (see Table 3). Model 1a (Education, before including work status).
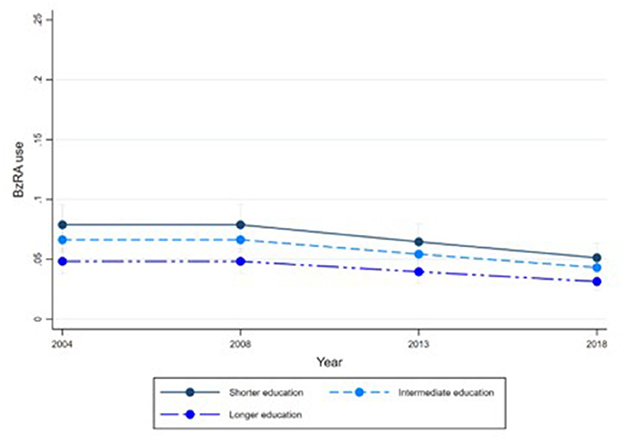
Figure 2. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 1 (see Table 3). Model 1b (Education, after including work status).
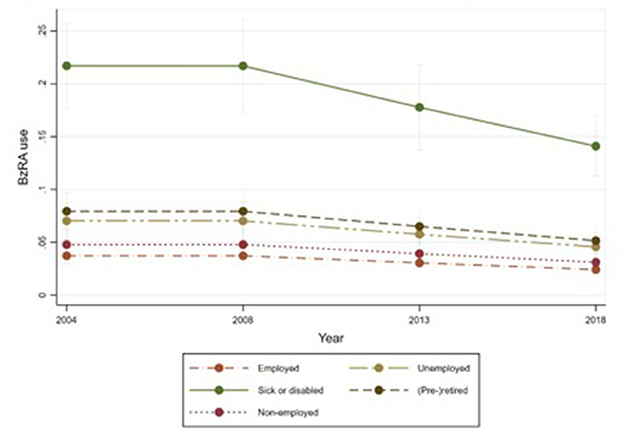
Figure 3. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 1 (see Table 3). Model 1b (Work status, controlled for education).
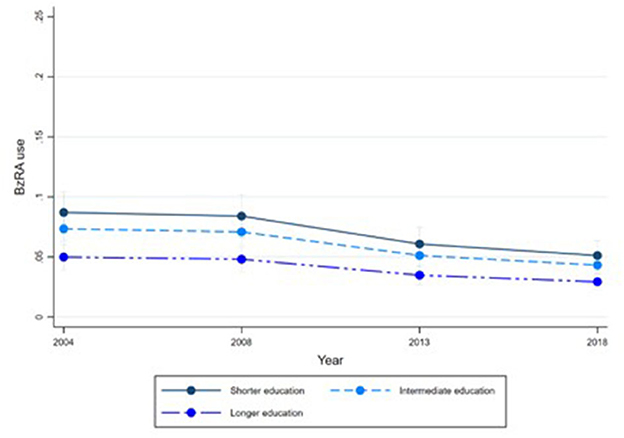
Figure 4. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 2 (see Table 3). Model 2a (Education, before including work status).
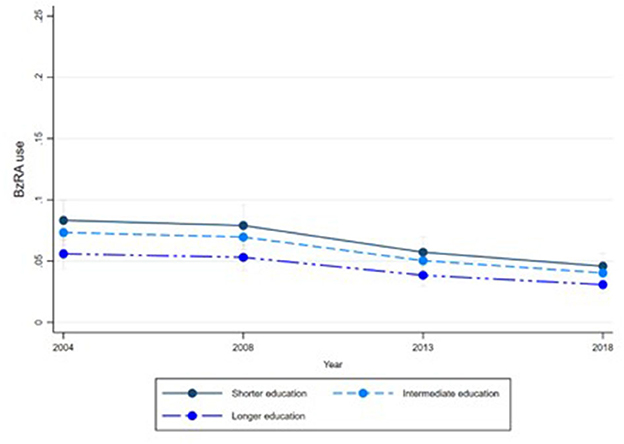
Figure 5. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 2 (see Table 3). Model 2b (Education, after including work status).
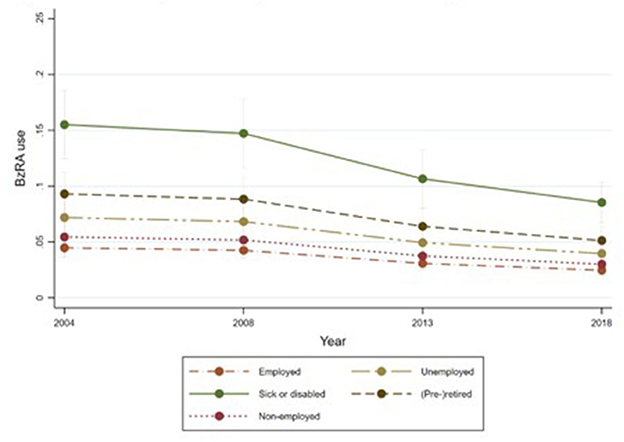
Figure 6. BzRA use in the past 24 h according to education and work status, stratified by wave, weighted prevalence (min.-max.:0–1) for Model 2 (see Table 3). Model 2b (Work status, controlled for education).
Discussion
Our study reveals several important findings. Firstly, work status acts as a mediator, partially explaining educational differences in BzRA use, even after accounting for mental health status. We found that individuals who are unemployed, (pre-)retired, or sick or disabled, regardless of their mental health status, exhibit higher levels of use than employed individuals. This aligns with previous research, which suggests that work-related uncertainty may lead to increased prescribing and medication use, regardless of mental health (36–39). Medicalisation and pharmaceuticalisation processes tend to detach social problems from their social roots and treat them as personal failures (40, 41). The marginalization of the social roots of unemployment, sick leave and pre-retirement has led to a personalization of responsibility. Negative feelings, including stress and self-stigma, arising from such work statuses may cause isolated, non-specific symptoms for which medical treatment is sought, including psychotropics like BzRAs (28).
Secondly, we found that even after taking into account mental health status, part of the educational differences in BzRA use remain unexplained, as work status only partially mediates the relationship. This finding is consistent with a recent Belgian study, which highlights the role of education as a socialization mechanism in explaining differences in mental health care use, rather than allocation mechanisms (16). The study suggests that education plays a significant role in influencing mental health care use, as it enhances non-material resources such as knowledge and social competences that may impact health care use (17). Socialization mechanisms contribute to creating social inequalities, as individuals with longer education are more likely to choose ‘effective' treatment options (42, 43), or in the case of BzRAs, to neglect ‘non-effective' options, due to their awareness of potential side- and withdrawal effects. Moreover, longer educated individuals also tend to adopt a certain ‘health identity' (44).
Furthermore, we observe an overall declining trend in BzRA use, which is an important pattern, especially when the mental health variables are taken into account. This suggests that non-need-based use is decreasing over time, possibly due to numerous prevention campaigns and federal government initiatives aimed at raising awareness of the side- and withdrawal effects of these medications (7, 9, 45). However, despite this trend, overconsumption remains a significant problem, with a large group of individuals continuing to use them daily on a long-term basis (10, 46). Studies indicate that while GPs are aware of the issues of overconsumption and long-term use, they often struggle to support their patients in stopping their use (39, 47, 48). In fact, research suggests that GPs find it hard to take initiative to change their chronic prescribing behavior (39, 49). Therefore, although a declining trend is visible, future research should focus on (inequalities in) the prevalence and incidence of long-term BzRA use and how it evolves over time, as well as strategies to address their long-term use.
Our study also reveals some expected findings, such as the relationship between mental health complaints and BzRA use. Specifically, higher levels of complaints are associated with higher levels of use. However, it is important to note that the use of BzRAs does not necessarily eliminates all complaints, suggesting a sub-optimal relationship between use and mental health. This could be because they are not true ‘medicines' but rather medication that enable individuals to function socially despite complaints (50). In addition, our study finds a positive association between higher levels of BzRA use and more frequent GP visits, which is expected given that GPs often prescribe these medications (48). However, this association could also highlight the presence of a GP-medication nexus that is not necessarily connected to the level of patient's complaints or their social context. Instead, it may be a result of GPs being ‘locked' into a particular mode of treatment (51, 52).
Two limitations of this study also need to be addressed. The first limitation concerns the measurement of the dependent variable BzRA use. Respondents were asked to present the medicines they had used in the past 24 h, and the interviewer then matched these to appropriate ATC codes on a list. Although the interviewer verified the medicines, respondents may not have shown all the medicines they had used, especially for stigmatized medicines such as BzRAs (53, 54). Longer educated individuals may be particularly aware of the stigma surrounding psychotropic medication use, including the potential risks of use (55), which could affect their willingness to disclose BzRA use to the interviewer. Since the question was part of a general module on the use of medicines, unrelated to the issue of mental health, the potential impact of self-report bias may be limited. Nevertheless, the reported rates probably underestimate the consumption of BzRAs. Furthermore, obtaining more information about the medication use would have been beneficial, including whether BzRAs were used to treat specific symptoms or diagnoses and whether they were used infrequently or frequently. The second limitation concerns the lack of comprehensive work-related information in the BHIS. It would have been interesting to include more detailed information on working conditions and work arrangements, related to the psychosocial quality of labor, which are associated with both education (56) and mental health care use (57, 58).
To end, some findings of this study require further investigation. For example, the higher use of BzRAs among older working-age adults beyond their (mental) health status and social position. Future research may investigate how their higher use is related to their GP contact. It may be possible that the increased use is not solely due to the age or cohort of the users (59), but also to the age or cohort of the GPs who are prescribing the medications (60). This finding highlights the need to understand the factors contributing to the prescribing practices of GPs.
Another finding that deserves consideration is the lower level of BzRA use among non-Belgians. For individuals from neighboring countries, the lower use could be explained by the fact that GPs play a less central role in those countries, with the exception of France, resulting in lower use of psychotropics (61). In Belgium and France, there is a low rate of referral to mental health specialists and a low rate of mental health specialist consultations. In contrast, in the Netherlands there is a high rate of referral and non-medical mental health care use. For individuals from non-neighboring countries, this may be due to their underrepresentation in ambulatory health care, which could be caused by cultural-specific barriers such as language barriers or differences in preferences and health care seeking behavior (62–64). Barriers can also occur at the level of health care providers, where patients from non-neighboring countries are treated differently, which is described as provider bias (65, 66).
Lastly, our study also indicates regional disparities in BzRA use, with higher levels of use observed in Brussels and Wallonia, even after adjusting for socio-demographic and composition factors. In Belgium, the competences for health care, including mental health care and health promotion, are decentralized, with the federal government retaining only certain competences (67). This decentralization, combined with the multiple communities with different traditions and behavioral patterns that make up Belgium, might contribute to the regional differences in use. However, future research is needed to gain a more comprehensive understanding of the factors driving these regional differences.
Conclusion
In conclusion, work status plays a crucial role in explaining educational differences in BzRA use, regardless of mental health status. This indicates that non-medical factors, such as work status, are medicalized and associated with medical mental health care-seeking behavior. Health care providers should be cautious while prescribing BzRAs and consider non-medical factors that may influence a patient's decision to seek medical treatment. Given the potential risks of BzRA use and the possibility of non-medical underlying reasons, health care providers should prioritize non-pharmacological treatment options. Therefore, it is essential for health care providers to educate their patients on the potential risks of BzRA use and the importance of non-pharmacological therapies.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data will not be deposited since its subject to a contract with Sciensano (The Scientific Institute of public health of the federal Belgian State). Requests to access these datasets should be directed to https://www.sciensano.be/en/node/55737/health-interview-survey-microdata-request-procedure.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
LC designed the study, had primary responsibility for the writing and editing of the manuscript, and performed the data analysis. KD, PB, and MC critically reviewed the manuscript. All authors gave final approval for the article to be published.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1191151/full#supplementary-material
Footnotes
1. ^Following ATC level four classes were included: N03AE, N04BA, N05CD and N05CF.
References
1. Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiatry. (2015) 72:136–42. doi: 10.1001/jamapsychiatry.2014.1763
2. Markota M, Rummans TA, Bostwick JM, Lapid MI. Benzodiazepine use in older adults: dangers, management, and alternative therapies. Mayo Clin Proc. (2016) 91:1632–9. doi: 10.1016/j.mayocp.2016.07.024
3. Jorm AF, Grayson D, Creasey H, Waite L, Broe GA. Long-term benzodiazepine use by elderly people living in the community. Aust N Z J Public Health. (2000) 24:7–10. doi: 10.1111/j.1467-842X.2000.tb00715.x
4. Kirby M, Denihan A, Bruce I, Radic A, Coakley D, Lawlor BA. Benzodiazepine use among the elderly in the community. Int J Geriatr Psychiatry. (1999) 14:280–4.
5. Barbee JG. Memory, benzodiazepines, and anxiety: integration of theoretical and clinical perspectives. J Clin Psychiatry. (1993) 54:86–101.
6. Petrovic M, Mariman A, Warie H, Afschrift M, Pevernagie D. Is there a rationale for prescription of benzodiazepines in the elderly? review of the literature. Acta Clinica Belgica. (2003) 58:27–36. doi: 10.1179/acb.2003.58.1.004
7. BENZONET: Perception habitual habitual use and cessation of BENZOdiazepines: a multi-method NETnography (BELSPO) [press release]. Ghent University (2021).
8. Oude Voshaar RC, Couvee JE, van Balkom AJ, Mulder PG, Zitman FG. Strategies for discontinuing long-term benzodiazepine use: meta-analysis. Br J Psychiatry. (2006) 189:213–20. doi: 10.1192/bjp.189.3.213
9. Federal Public Service (FPS). Slaap- en kalmeerpillen [Sleeping pills and tranquilizers]. (2019). Available online at: https://www.health.belgium.be/en/node/23214
10. Pétein C, Spinewine A, Henrard S. Trends in benzodiazepine receptor agonists use and associated factors in the Belgian general older population: analysis of the Belgian health interview survey data. Ther Adv Psychopharmacol. (2021) 11:20451253211011874. doi: 10.1177/20451253211011874
11. Azermai M, Elseviers M, Petrovic M, Van Bortel L, Stichele RV. Geriatric drug utilisation of psychotropics in Belgian nursing homes. Hum Psychopharmacol. (2011) 26:12–20. doi: 10.1002/hup.1160
12. Verhoeven V, Hartmann ML, Wens J, Sabbe B, Dieleman P, Tsakitzidis G, et al. Happy pills in nursing homes in Belgium: a cohort study to determine prescribing patterns and relation to fall risk. J Clin Gerontol Geriatr. (2014) 5:53–7. doi: 10.1016/j.jcgg.2013.12.001
13. Grzywacz JG, Almeida DM, McDonald DA. Work–family spillover and daily reports of work and family stress in the adult labor force. Fam Relat. (2002) 51:28–36. doi: 10.1111/j.1741-3729.2002.00028.x
14. Perreault M, Power N. Work-life balance as a personal responsibility: the impact on strategies for coping with interrole conflict. J Occup Sci. (2021) 30:160–74. doi: 10.1080/14427591.2021.1894596
15. Colman L, Delaruelle K, Bracke P. The stratified medicalisation of mental health symptoms: educational inequalities in the use of psychotropic medication in Belgium. Soc Psychiatry Psychiatr Epidemiol. (2022) 58:833–42. doi: 10.1007/s00127-022-02283-1
16. Colman L, Delaruelle K, Bracke P. The socialization power of education: approaching the social gradient in treatment for self-reported depression in Belgium between 2004 and 2018. (2022) (Unpublished).
17. Mirowsky J, Ross CE. Education, learned effectiveness and health. London Rev Educ. (2005). doi: 10.1080/14748460500372366
18. Groot W, van den Brink HM. “What does education do to our health? Measuring the effect of education on health and civic engagement,” in Proceedings of the Copenhagen symposium. Paris: OECD (2006).
19. Lynch SM. Explaining life course and cohort variation in the relationship between education and health: the role of income. J Health Soc Behav. (2006) 47:324–38. doi: 10.1177/002214650604700402
20. Ross CE, Wu C-l. The links between education and health. Am Soc Rev. (1995) 60:719–45. doi: 10.2307/2096319
21. Shultz KS, Morton KR, Weckerle JR. The influence of push and pull factors on voluntary and involuntary early retirees' retirement decision and adjustment. J Vocat Behav. (1998) 53:45–57. doi: 10.1006/jvbe.1997.1610
22. Radl J. Labour market exit and social stratification in Western Europe: the effects of social class and gender on the timing of retirement. Eur Sociol Rev. (2013) 29:654–68. doi: 10.1093/esr/jcs045
23. Buffel V, Dereuddre R, Bracke P. Medicalization of the uncertainty? an empirical study of the relationships between unemployment or job insecurity, professional care seeking, and the consumption of antidepressants. Eur Soc Rev. (2015) 31:446–59. doi: 10.1093/esr/jcv004
24. Virtanen M, Kivimäki M, Ferrie JE, Elovainio M, Honkonen T, Pentti J, et al. Temporary employment and antidepressant medication: a register linkage study. J Psychiatr Res. (2008) 42:221–9. doi: 10.1016/j.jpsychires.2006.12.005
25. Henkel D. Unemployment and substance use: a review of the literature (1990-2010). Curr Drug Abuse Rev. (2011) 4:4–27. doi: 10.2174/1874473711104010004
26. Doshi JA, Cen L, Polsky D. Depression and retirement in late middle-aged US workers. Health Serv Res. (2008) 43:693–713. doi: 10.1111/j.1475-6773.2007.00782.x
27. Conrad P. Medicalization and social control. Annu Rev Sociol. (1992) 18:209–32. doi: 10.1146/annurev.so.18.080192.001233
28. Holmqvist M. Medicalization of unemployment: individualizing social issues as personal problems in the Swedish welfare state. Work Employ Soc. (2009) 23:405–21. doi: 10.1177/0950017009337063
29. Janlert U. Unemployment as a disease and diseases of the unemployed. Scand J Work Environ Health. (1997) 23:79–83.
30. Nahler G. Anatomical therapeutic chemical classification system (ATC). In: Dictionary of Pharmaceutical Medicine. Vol. 160. (2009) p. 174. doi: 10.1007/978-3-211-89836-9_64
31. Unesco Institute for Statistics,. International standard classification of education: ISCED 2011. Comparative Social Research (2012). Available online at: https://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf
32. Fride Tvete I, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. (2015) 33:252–9. doi: 10.3109/02813432.2015.1117282
33. Rizvi SJ, Cyriac A, Grima E, Tan M, Lin P, Gallaugher LA, et al. Depression and employment status in primary and tertiary care settings. Can J Psychiatry. (2015) 60:14–22. doi: 10.1177/070674371506000105
34. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
35. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
36. Buffel V. Mental Health and Mental Health Care Use of the Unemployed: A Multilevel Study Into the Medicalization of Unemployment in Europe. Ghent University (2016).
37. Buffel V, Beckfield J, Bracke P. The institutional foundations of medicalization: a comparative approach to medicalizing unemployment. J Health Soc Behav. (2017) 58:272–90. doi: 10.1177/0022146517716232
38. van de Straat V, Buffel V, Bracke P. Medicalization of sleep problems in an aging population: a longitudinal cross-national study of medication use for sleep problems in older European adults. J Aging Health. (2018) 30:816–38. doi: 10.1177/0898264317696775
39. Sirdifield C, Anthierens S, Creupelandt H, Chipchase SY, Christiaens T, Siriwardena AN. General practitioners' experiences and perceptions of benzodiazepine prescribing: systematic review and meta-synthesis. BMC Fam Pract. (2013) 14:1–13. doi: 10.1186/1471-2296-14-191
40. Bendelow G. Sociological Aspects of the Emotions. The SAGE handbook of mental health and illness (2011). p. 67–79. doi: 10.4135/9781446200988.n4
41. Williams SJ, Martin P, Gabe J. The pharmaceuticalisation of society? a framework for analysis. Sociol Health Illn. (2011) 33:710–25. doi: 10.1111/j.1467-9566.2011.01320.x
42. Link BG, Phelan J. Social conditions as fundamental causes of health inequalities. Handbook Med Sociol. (2010) 6:17. doi: 10.2307/j.ctv16h2n9s.4
43. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. (1995) 80–94. doi: 10.2307/2626958
44. Greenhalgh T, Wessely S. ‘Health for me': a sociocultural analysis of healthism in the middle classes. Br Med Bull. (2004) 69:197–213. doi: 10.1093/bmb/ldh013
45. Donoghue J, Lader M. Usage of benzodiazepines: a review. Int J Psychiatry Clin Pract. (2010) 14:78–87. doi: 10.3109/13651500903447810
46. Kiridis SJ, Sawchik J, Maenhaut N, Sabbe M, Wuillaume F, Hamdani J. Survey on the Use of Benzodiazepines Z-drugs to Treat Insomnia in Belgium. (2022). Available online at: https://www.fagg.be/sites/default/files/BZRA_study_report_2020_DEF_21.06.2022_0.pdf
47. Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. (2009) 23:19–34. doi: 10.2165/0023210-200923010-00002
48. Coteur K, Van Nuland M, Vanmeerbeek M, Henrard G, Anthierens S, Van den Broeck K, et al. Effectiveness of a blended care programme for the discontinuation of benzodiazepine use for sleeping problems in primary care: study protocol of a cluster randomised trial, the Big Bird trial. BMJ Open. (2020) 10:e033688. doi: 10.1136/bmjopen-2019-033688
49. Ellen VL, Anthierens S, van Driel ML, Sutter AD, Branden Evd, Christiaens T. ‘Never change a winning team': GPs' perspectives on discontinuation of long-term antidepressants. Scand J Prim Health Care. (2021) 39:533–42. doi: 10.1080/02813432.2021.2006487
50. Kennedy KM, O'Riordan J. Prescribing benzodiazepines in general practice. Br J Gen Pract. (2019) 69:152–3. doi: 10.3399/bjgp19X701753
51. Anthierens S, Habraken H, Petrovic M, Christiaens T. The lesser evil? initiating a benzodiazepine prescription in general practice: a qualitative study on GPs' perspectives. Scand J Prim Health Care. (2007) 25:214–9. doi: 10.1080/02813430701726335
52. Department of Health and Social Care. Good for you, good for us, good for everybody: A plan to reduce overprescribing to make patient care better and safer, support the NHS, and reduce carbon emissions. DHSC London (2021).
53. Rogers A, Pilgrim D, Brennan S, Sulaiman I, Watson G, Chew-Graham C. Prescribing benzodiazepines in general practice: a new view of an old problem. Health. (2007) 11:181–98. doi: 10.1177/1363459307074693
54. Liebrenz M, Gehring M-T, Buadze A, Caflisch C. High-dose benzodiazepine dependence: a qualitative study of patients' perception on cessation and withdrawal. BMC Psychiatry. (2015) 15:1–12. doi: 10.1186/s12888-015-0493-y
55. Wong K, Bartlett D-J, Saini B. Benzodiazepine use risk: understanding patient specific risk perceptions and medication beliefs. Res Social Adm Pharm. (2019) 15:1317–25. doi: 10.1016/j.sapharm.2018.12.007
56. Rahkonen O, Laaksonen M, Martikainen P, Roos E, Lahelma E. Job control, job demands, or social class? the impact of working conditions on the relation between social class and health. J Epidemiol Community Health. (2006) 60:50–4. doi: 10.1136/jech.2005.035758
57. van Daalen G, Willemsen TM, Sanders K, van Veldhoven MJ. Emotional exhaustion and mental health problems among employees doing “people work”: the impact of job demands, job resources and family-to-work conflict. Int Arch Occup Environ Health. (2009) 82:291–303. doi: 10.1007/s00420-008-0334-0
58. Virtanen M, Honkonen T, Kivimäki M, Ahola K, Vahtera J, Aromaa A, et al. Work stress, mental health and antidepressant medication findings from the Health 2000 Study. J Affect Disord. (2007) 98:189–97. doi: 10.1016/j.jad.2006.05.034
59. Straand J, Rokstad K. General practitioners' prescribing patterns of benzodiazepine hypnotics: are elderly patients at particular risk for overprescribing? Scand J Prim Health Care. (1997) 15:16–21. doi: 10.3109/02813439709043423
60. Dybwad T, Kjølsrød L, Eskerud J, Laerum E. Why are some doctors high-prescribers of benzodiazepines and minor opiates? a qualitative study of GPs in Norway. Fam Pract. (1997) 14:361–8. doi: 10.1093/fampra/14.5.361
61. Kovess-Masfety V, Alonso J, Brugha TS, Angermeyer MC, Haro JM, Sevilla-Dedieu C. Differences in lifetime use of services for mental health problems in six European countries. Psychiatr Serv. (2007) 58:213–20. doi: 10.1176/ps.2007.58.2.213
62. Miranda J, Cooper LA. Disparities in care for depression among primary care patients. J Gen Intern Med. (2004) 19:120–6. doi: 10.1111/j.1525-1497.2004.30272.x
63. Jaeger FN, Pellaud N, Laville B, Klauser P. The migration-related language barrier and professional interpreter use in primary health care in Switzerland. BMC Health Serv Res. (2019) 19:1–10. doi: 10.1186/s12913-019-4164-4
64. Brisset C, Leanza Y, Rosenberg E, Vissandjée B, Kirmayer LJ, Muckle G, et al. Language barriers in mental health care: a survey of primary care practitioners. J Immigr Minor Health. (2014) 16:1238–46. doi: 10.1007/s10903-013-9971-9
65. Duveau C, Wets C, Delaruelle K, Demoulin S, Dauvrin M, Lepièce B, et al. Unintentional discrimination against patients with a migration background by general practitioners in mental health management: an experimental study. Adm Policy Ment Health Ment Health Serv Res. (2023) 50:450–60. doi: 10.1136/jech-2022-SSMabstracts.44
66. Ceuterick M, Bracke P, Van Canegem T, Buffel V. Assessing provider bias in general practitioners' assessment and referral of depressive patients with different migration backgrounds: Methodological insights on the use of a video-vignette study. Community Ment Health J. (2020) 56:1457–72. doi: 10.1007/s10597-020-00590-y
Keywords: benzodiazepines, education, employment, health inequities, medicalization, mental health, psychotropic drugs
Citation: Colman L, Delaruelle K, Bracke P and Ceuterick M (2023) Trends in the use of benzodiazepine receptor agonists among working-age adults in Belgium from 2004 to 2018. Front. Public Health 11:1191151. doi: 10.3389/fpubh.2023.1191151
Received: 21 March 2023; Accepted: 30 May 2023;
Published: 15 June 2023.
Edited by:
Adriana Mihai, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, RomaniaReviewed by:
Saeid Komasi, Mind GPS Institute, IranAvarvaroaei Isabela, Emergency County Hospital Targu Mures, Romania
Copyright © 2023 Colman, Delaruelle, Bracke and Ceuterick. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa Colman, bGlzYS5jb2xtYW5AdWdlbnQuYmU=
 Lisa Colman
Lisa Colman Katrijn Delaruelle
Katrijn Delaruelle Piet Bracke
Piet Bracke Melissa Ceuterick
Melissa Ceuterick