- 1Institute of Medical Data Processing, Biometrics and Epidemiology (IBE), Faculty of Medicine, LMU Munich, Munich, Germany
- 2Pettenkofer School of Public Health, Munich, Germany
- 3Department of Psychosomatic Medicine and Psychotherapy, University Hospital, Technical University of Munich, Munich, Germany
- 4TUM School of Computation, Information and Technology, Technical University of Munich, Munich, Germany
- 5Institute of General Practice and Family Medicine, University Hospital of Ludwig-Maximilians-University Munich, Munich, Germany
Background: Community indicators may predict and influence individuals` mental health, and support or impede mental health management. However, there is no consensus on which indicators should be included in predictions, prognostic algorithms, or management strategies for community-based mental health promotion and prevention approaches. Therefore, this scoping review provides an overview of relevant community-level indicators for mental health in the general as well as risk populations in a European context.
Methods: We conducted a scoping review in the following electronic databases: PubMed, Embase, and PsycInfo. Eligible studies focused on context factors such as either the physical or social environment, reporting at least one mental health outcome and referring to a European population. Publications between 2012 and March 8, 2022 are considered.
Results: In total, the search yielded 12,200 identified records. After the removal of duplicates, 10,059 records were screened against the eligibility criteria. In total, 169 studies were included in the final analysis. Out of these included studies, 6% focused on pan-European datasets and 94% on a specific European country. Populations were either general or high-risk populations (56 vs. 44%, respectively) with depressive disorder as the main reported outcome (49%), followed by general mental health (33%) and anxiety (23%). Study designs were cross-sectional studies (59%), longitudinal (27%), and others (14%). The final set of indicators consisted of 53 indicators, which were grouped conceptually into 13 superordinate categories of community indicators. These were divided into the domains of the physical and social environment. The most commonly measured and reported categories of community indicators associated with mental health outcomes were social networks (n = 87), attitudinal factors toward vulnerable groups (n = 76), and the characteristics of the built environment (n = 56).
Conclusion: This review provides an evidence base of existing and novel community-level indicators that are associated with mental health. Community factors related to the physical and social environment should be routinely recorded and considered as influencing factors or potentially underestimated confounders. The relevance should be analyzed and included in clinical outcomes, data, monitoring and surveillance as they may reveal new trends and targets for public mental health interventions.
1. Introduction
Over the last decades, mental health impairments have imposed a high burden on society and health care systems across European countries and worldwide in terms of premature mortality, increased morbidity, and decreased quality of life (1). Before the COVID-19 pandemic, an average of one in nine adults had symptoms of psychological distress and one in six adults was diagnosed with a mental health condition, with varying prevalence across Europe (2). The Global Burden of Disease Study 2015 (3) showed that among all mental health conditions, depression and anxiety disorders are most prevalent. It further showed that mental disorders were among the most important contributors to years of life with disability (DALYs) in 2015.
To reduce the high prevalence and high burden imposed by mental health disorders, large scale and effective mental health promotion and prevention strategies are necessary. These strategies should aim at avoiding mental ill-health in the first place and at reducing the impacts of mental disorders on people’s lives. The importance of mental health promotion and prevention was underlined by an analysis of the Australian mental health strategy between 1992 and 2011: while the expenditure on mental health services, workforce, and treatments increased dramatically, the prevalence of depression and anxiety disorders remained high and even showed some increase at the same time. A possible explanation, among others, was that comprehensive and on-going mental health promotion and prevention interventions were missing in the strategy (4). This explanation is supported by findings such as that mental health promotion and prevention programs showing to strengthen protective factors for mental health but often target specific populations rather than the general population (5).
Communities (or herein also referred to as neighborhoods) qualify as ideal settings for mental health promotion and prevention strategies. Moreover, the WHO Comprehensive Plan of Action 2013–2020 demands the re-shaping of community and natural environments as central pillars for improving the mental health of the population. The WHO calls it “misplaced priorities” as 2/3 of the money spent in mental health is currently allocated to psychiatric hospitals instead of supporting other key factors such as communities. The advantages of community-based mental health care, however, are more fundamental, including increased accessibility, reduced stigmatization, better protected human rights, and improved outcomes (6). In communities, health messages are received in the immediate environment and are therefore powerful in influencing the individual’s health behavior and behavior change (7). As people are inextricably linked to their environment, and health promotion and prevention moved already beyond the clinical service provision, the community should be involved as an effective partner (8). As pointed out by the WHO, changes in the transforming field of mental health care are not happening fast enough, and community-level mental health services should be strengthened to serve people best with low threshold access (6). Moreover, community-level factors should be acknowledged as potential targets of intervention and support of treatment and management concepts of mental health disorders (9).
In the management of chronic diseases, the integration of the community and its resources is a central pillar as conceptualized, for instance, within the Chronic Care Model (10). To meet the requirements and incorporate the principles in the field of health promotion and prevention, Barr et al. (11) developed the Expanded Chronic Care Model (ECCM), which focuses on the social determinants of health and recognizes the importance of socio-economic factors as a key determinant to long-term success in the prevention and treatment of mental diseases (8). The ECCM provides a strategy to support high-quality healthcare services with policies and programs in the communities to reduce the impact on those who are ill, but also to help people to stay healthy (11). For example, ECCM-based chronic disease programs for hypertension and diabetes in Canada integrated community resources by strengthening community action (e.g., developing a community network on the condition, bringing services to marginalized groups, shifting decision-making to adapt to community needs and capacities, partnering with local businesses, and involving the non-profit sector to develop a strategic vision) (12, 13). In the mental health field, linking patients to community-based assets, such as community music, community exercise, museums/arts, libraries, and gardening is increasingly used and could be a promising intervention to reduce depression and anxiety (14). For example, horticultural therapy included tours of a botanical garden, learning about the species and how to cultivate, grow, and harvest them, combined with activities such as planting, arranging flowers, etc. (15, 16).Knowing the pertinent contributing factors and indicators for community mental health is essential for the development of successful mental health promotion and prevention interventions. However, there is currently no consensus or solid evidence base on which community indicators are the most relevant and should be included in monitoring, surveillance (predictions, prognostic algorithms), or management data collections. Factors of the physical environment include the built environment, which is defined most generally as “man-made infrastructure” such as buildings and streets (17), public transportation infrastructure, and recreational sites and structures among others (18). The social environment considers the sociodemographic composition of an area, as well as “the relationships, groups and social processes that exist between individuals” including social capital, social norms, safety, and poverty (19). Generaal et al. (20) showed that these socioeconomic, physical, and social community or neighborhood characteristics are associated with the prevalence and severity of depressive disorders. Particularly, social cohesion, a defining feature of a contextual unit with its core dimensions of social relation, identification with the social entity, and orientation toward a common good (21, 22) mediates the effects of environmental and built neighborhood characteristics on physical and mental health with a proportion between 10 and 23% (23). In addition, social capital and the strongly correlating concept of social justice, a central cornerstone of community psychology, have a strong impact on wellbeing and shows a high effect on life satisfaction on a national level (24). The citizen’s wellbeing is strongly related to their mattering and social environment in the community (25).
While much literature omits the definition of an indicator but focuses straight on its qualities, Kaye-Blake et al. (26) define an indicator as a “relevant variable, measurable over time and/or space that provides information on a larger phenomenon of interest and allows comparisons to be made.” Hence, community indicators quantify different aspects of community characteristics over time. The implementation and integration of health promotion principles into the prevention and management of mental health problems depends upon a good understanding of the specific social and physical indicators regarding the individual and its (health) context (11). Therefore, the aim of this scoping review is to:
1. Systematically identify relevant indicators that predict, explain, or monitor neighborhood/community characteristics that are relevant for mental health.
2. Assign the extracted indicators to core categories and possibly even deductively identify new core areas in field of mental health associated community characteristics.
3. Identify gaps in the field and new targets of interventions in community based (public) mental health.
2. Materials and methods
2.1. Study design
The methodological steps are structured according to the suggestions of the “Methodology for Joanna Briggs Institute Scoping Reviews” (27) and its update (28). This is on the basis of the framework for scoping reviews by Arksey and O` Malley (29) and consists of the following steps: (1) Identify the research question, (2) Identify relevant studies, (3) Select studies, (4) Chart the data, and (5) Collate, summarize, and report the results.
Additionally, we employed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) extension for Scoping Reviews Checklist (PRISMA-ScR Checklist) (30) as a guideline to develop this scoping review and the corresponding pre-registered study protocol. The study protocol was published in advance and can be viewed in the Open Science Framework at this link: https://osf.io/r6ngq.
2.2. Search strategy
We used the Population-Concept-Context (PCC) framework to build our search strategy and to guide the literature search considering: P (Population): general or high-risk community members/people living in a defined geographical area; C (Concept): community-level indicators/neighborhood characteristics, environmental determinants. C (Context): Mental health promotion and prevention in Europe (see Supplementary Table 1). For this paper, we focused on the term “community” in the sense of people living in a defined residential area, neighborhood, or town. For the sake of this work, we defined an indicator according to Kaye-Blake et al. (26) as a “relevant variable, measurable over time and/or space that provides information on a larger phenomenon of interest and allows comparisons to be made” and that is associated with the community’s mental health. But it was not the aim of this work to determine whether it fulfilled the criteria of a good indicator (quality appraisal) according to the current literature. To address heterogeneity regarding the healthcare, environmental and political systems, we only included studies that are based on European datasets. We conducted the search in three electronic databases (PubMed, Embase, and PsycInfo) on the March 8, 2022. The inclusion and exclusion criteria are described below. We chose the precise search terms according to the database used but all included title/abstract phrases such as “community,” “neighborhood,” “residential,” “environmental,” “indicators,” “characteristics,” “determinants,” “factors,” “mental health,” “depression,” “depressive disorders,” “anxiety,” and “mental disorders.” We give an example of the chosen keywords for our Medline search in the Supplementary Table 2. For the sake of completeness, we included a great variety of search terms to fully represent the topic. To account for the different types of evidence, we included quantitative and qualitative research. We excluded study protocols, case studies, conference abstracts, or gray literature.
2.3. Study selection with inclusion and exclusion criteria
To be included, the articles had to be (a) in English or German, (b) located in community or neighborhood, (c) focus on a European population, (d) focus on mental health outcomes, and (e) published between January 2012 and March 8, 2022 to retrieve recent publications and to depict current circumstances. Studies were excluded if they (a) were conducted in an institutional setting such as health care setting, school, workplace, or prison, (b) were occupation-related, (c) were COVID-19 related, (d) included the digital environment, such as social media platforms, online peer groups, and digital support systems as it cannot be geographically localized, (e) included medical interventions or health promoting activities (e.g., football training, mindfulness interventions) as these do not qualify as community indicator, and (f) included non-European data.
2.4. Data extraction process
All records retrieved in the electronic databases were merged using the Rayyan software. We deleted duplicates and the remaining records were first title and abstract screened, and then full-text screened against the inclusion and exclusion criteria. This process is shown in the PRISMA Flow Chart (Figure 1).
All records were distributed among the five reviewers (PS, KB, ADM, MK, and PRS) for screening using the Rayyan software. Twenty percent of the records from the title and abstract screen were double screened by two reviewers (PS, KB). Disagreements were resolved through discussion. The same five reviewers simultaneously conducted the full-text screen and data extraction.
For the data extraction, we developed a characterization matrix in an Excel spreadsheet, which comprised: first author, publication year, indicator(s), region(s), population, outcome measure(s), and study design (categorized as cross-sectional studies, longitudinal studies, and other study designs). In the data synthesis, we assigned the extracted indicators to either the physical or the social environment. If composite indicators were used in the studies, we extracted every single sub-indicator and regarded it as standalone indicator. We clustered conceptually similar indicators into superordinate indicator categories.
3. Results
3.1. Literature search
A total of 12.200 records were identified from the electronic databases. After removal of duplicates and records that did not meet the inclusion criteria, 169 studies were included in the final synthesis. Figure 1 gives an overview of the reasons for exclusion for each step of the screening process. The baseline characteristics of all studies are shown in the Table 1.
3.2. Characteristics of the included studies
The basic characteristics of the included studies are described in Table 1.
3.2.1. Study population
Of the included studies, 95 (56%) of the studies focused on the general population, while 74 studies (44%) targeted high-risk populations. High-risk populations included ethical/racial minorities (n = 36), sexual/gender minorities (n = 14), people with comorbidities (n = 10), and other special populations (n = 14), such as pregnant women, persons who experienced war, caregivers, terrorist attack survivors, and disaster victims. Adults were mainly researched (n = 141, 83%), while children (n = 10*, 6%) and adolescents (n = 19*, 11%) were less often represented (*double count for one study).
In this Europe-focused review, populations from following countries were most often under investigation: The United Kingdom (n = 53), the Netherlands (n = 23), Spain and Sweden (n = 15 each), Germany (n = 13), and other (n = 42). Eight studies included pan-European datasets with data from more than eight European countries.
3.2.2. Study outcomes
The most frequently reported outcomes were depressive symptoms/depression (n = 83, 49%), general mental health (n = 56, 33%), and anxiety disorders (n = 40, 23%). Other outcomes were well-being, psychological distress, post-traumatic stress disorder (PTSD), mood disorders, suicide/self-harm, schizophrenia, and “other” which includes health service use, any psychiatric disorder, substance abuse, intellectual disability, resilience, and loneliness. However, the study outcomes are independent of study design and statistical significance, but only based on being mentioned as such.
3.2.3. Study types
About 60% (n = 99) of the studies were cross-sectional studies, 27% (n = 46) were longitudinal studies, the remaining 24 studies (14%) were systematic reviews, qualitative studies, reviews, experimental studies, mixed methods studies, ecological studies, meta-analysis, and case–control studies.
3.3. Indicators and indicator categories
Of the included 169 studies, 53 indicators were identified and grouped conceptually into 13 indicator categories for mental health. These indicator categories again were assigned to either the physical or social environmental domain of community indicators. In the domain of the social environment, eight indicator categories with 36 indicators are described. In the domain of the physical environment, 17 indicators were grouped into five indicator categories. The most commonly investigated indicator categories are social networks (87 times), attitudinal factors toward vulnerable groups (76 times), built environment (56 times), deprivation (40 times), and security (34 times). Details on the division of the indicators regarding the two domains can be found in Table 2.
3.3.1. Composite indicators
Composite indicators combine a set of individual indicators into a single index (197). To account for the distinct aspects of the neighborhood, 11 studies used composite indices/indicators to depict either the social or physical environment, or both in the context of mental health. The composite indicators measure neighborhood quality (137), neighborhood composition (51), neighborhood usability (60), social disadvantage (32, 33), community resources accessibility index (61), community-level alcohol environment (B (143).), ecological assets (45), neighborhood characteristics (91), and post-migration living difficulties (172). Among these composite indicators, the most frequently used were “access to services” (n = 4) and “neighborhood deprivation” (n = 3).
3.3.2. Indicator categories by outcomes
Regarding general mental health, social networks (n = 25), discrimination (n = 24), built environment (n = 18), deprivation (n = 15), and violence (n = 6) were most studied. For depression, the most common indicators were social networks (n = 30), discrimination (n = 28), built environment (n = 23), deprivation (n = 13), pollution (n = 10), and violence (n = 9). Similarly, regarding anxiety disorders, the most frequently investigated indicator categories were discrimination (n = 17), social networks (n = 13), violence (n = 6), deprivation (n = 5), built environment (n = 5), and pollution (n = 3). The other mental health conditions were most investigated regarding social networks (n = 13), built environment (n = 7) and violence (n = 7), discrimination (n = 4), and urbanization and policy (each n = 3).
3.3.3. Indicator categories by population
The identified indicators in the included studies vary by population. The most frequently investigated categories in the general population were social networks (n = 41), built environment (n = 38), deprivation (n = 19), security (n = 16), and pollution (n = 15), while in the high-risk-population attitudinal factors toward vulnerable groups (n = 51) and social network (n = 31) were by far the most important indicator categories (see Table 3).
Table 3. Number of occurrences of the indicator categories by risk and age group displayed in different blue shades according to frequency.
3.3.4. Indicator categories by special groups
Attitudinal factors toward vulnerable groups and social networks are most commonly researched in ethnical/racial and sexual/gender minorities. For people with comorbidities, attitudinal factors toward vulnerable groups were frequently investigated. “Comorbid patients” where defined as those with diagnosed epilepsy, HIV, schizophrenia, depression, mental health problems, borderline, intellectual impairment, anxiety/somatoform disorder, or obesity. In this population group, attitudinal factors toward vulnerable groups were most researched. Social networks were the most often investigated indicator category in “Other population” such as adults who experienced war, caregivers, pregnant women, survivors of terrorist attacks, disaster victims, mothers, and persons after bereavement (see Table 4).
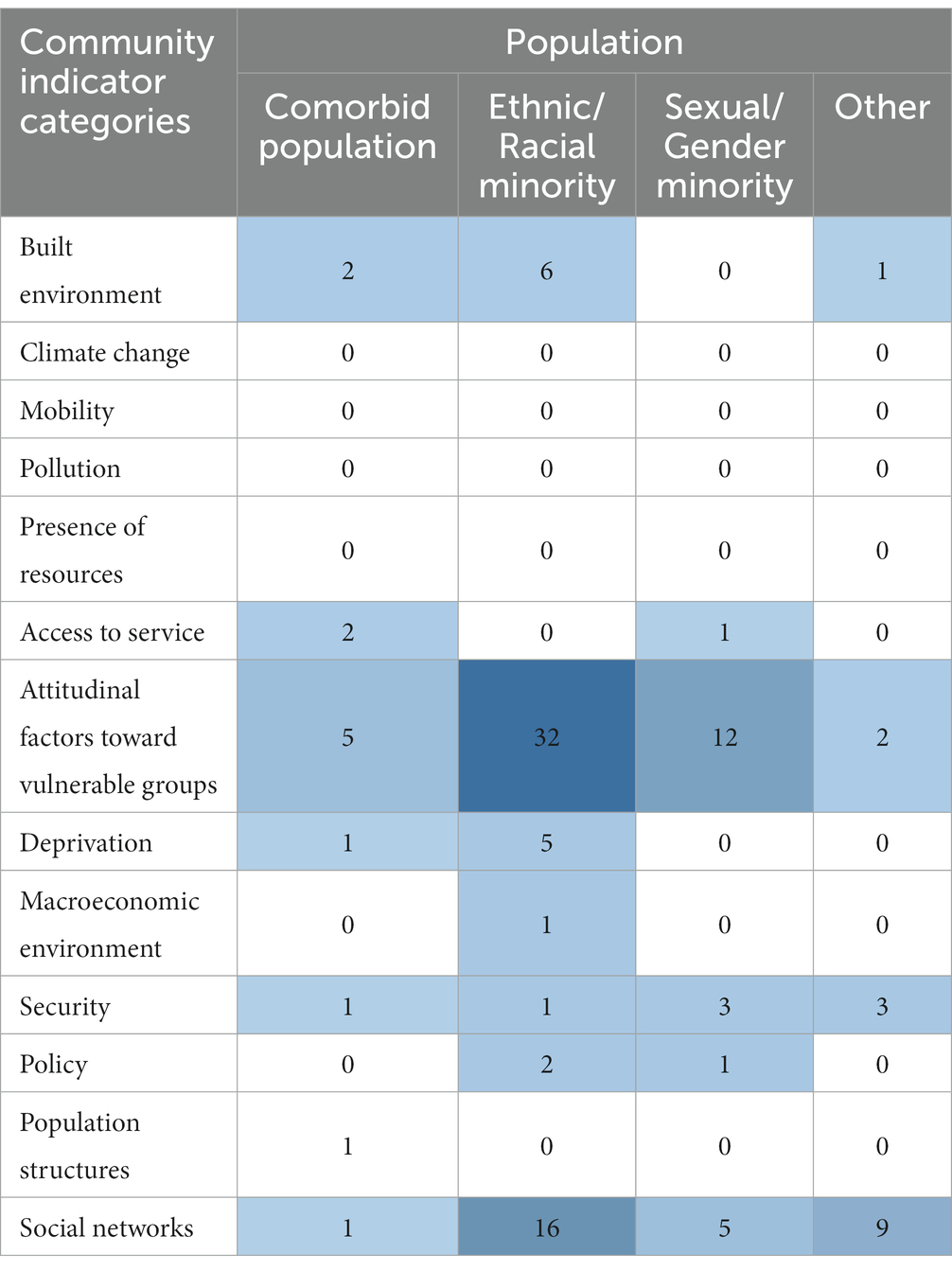
Table 4. Number of occurrences of the indicator categories in the identified studies by special groups displayed in different blue shades according to frequency.
4. Discussion
4.1. Summary of main findings
With this scoping review, we aim at providing a framework for relevant community indicators and public mental health measures in general and high-risk populations with a focus on Europe. We identified 53 community indicators that were clustered into 13 indicator categories, divided into the domains of physical and social environment. In comparison to the physical environment, the domain of the social environment has been studied more frequently. Overall, the indicator categories social networks, attitudinal factors toward vulnerable groups, and the built environment were the most frequently discussed topics. Pollution, mobility, presence of resources, and climate change, as well as population structure, macroeconomic environment, and policies were highlighted as new in terms of not yet being part of or under consideration for mental health surveillance. Many of the identified indicators and indicator categories are not yet part of existing monitoring systems but complement the picture of those indicators that should be included in the biopsychosocial models of disease in the future.
The understanding of mental health as a multi-faceted concept is translated into the latest WHO’s Comprehensive Mental Health Action Plan’s recommendation to gather “at least a core set of mental health indicators” every 2 years in a national Mental Health Surveillance (MHS) (198). There, environmental factors such as national policies, social protection, living standards, working conditions, and community social support are addressed and call for a multi-sectorial approach in the management and prevention of mental health disorders. Such indicator sets that cover a wide range of personal, social, and physical aspects are valuable to communities to monitor the community’s characteristics and needs, and to act appropriately with adequate mental health promotion and prevention strategies (199). Despite the importance of community-level indicators, the German Robert Koch Institute found them to be underrepresented in current surveillances and communicated it as a gap to be filled (200).
The community-level indicators range in a wide field of important areas and were structured by identifying the 13 superordinate indicator categories. As the indicators are extracted from exclusively scientific studies, we cannot make statements whether routinely monitored data are widely available. As most indicators were extracted from different studies, we cannot assume that there are existing databases for the individual indicator nor that there is a consensus on how it is operationalized.
The International classification of functioning, disability, and health (ICF) endorsed by the World Health Assembly for the international use (WHO) in 2001, is an important framework for the description of health and health related status of an individual in its specific context with a unified and standard language (201). With the adoption of the ICF, the understanding of functioning and disability has changed fundamentally (202). Individuals are not seen as unrelated entities anymore, but the individual’s functioning and health condition seen as in constant interaction with contextual factors such as social surroundings (202). In this classification, context factors are divided into personal and environmental factors, where the latter form the physical, social, and attitudinal environment in which people live and conduct their lives (201, 203). While the social and attitudinal environments are widely discussed in the identified literature, the categories of the physical environment are less well investigated.
The concept of environmental factors is generally based on the sociophysical context, which is understood as the observation that health is affected by the social and physical environment. The term sociophysical context is often not clearly defined in literature but shows overlaps with the concepts of community and neighborhood. In a broader sense, the place of residence with its specific environment affects the community members´ health condition through either direct (e.g., air pollution) or indirect factors (e.g., access to health care and social services) (136). Environmental factors could explain the repeated observation of health outcome differences across geographic areas (204). The growing interest in the contributing aspects of the community and neighborhood on the health status and lives of its residents urges the academic community to clearly define these terms in their research (205).
The domain of the social environment, especially the indicator category of social network, is well represented in this scoping review. The social network, which in various operationalizations comprises social capital, social cohesion, trust, community connectedness, peer and social support, is increasingly regarded as relevant (136). These indicators are believed to be mental health-related neighborhood/community factors, although the observed associations in the literature may be confounded by genetic or other environmental factors (206).
The lack of consensus on comparable measures of the social environment and the difficulties in obtaining them, makes the comparisons of the social environment complicated (204). For example, the definition and measurement of social capital shows great heterogeneity, ranging from individual to neighborhood-level measures. To obtain valid measures of social capital, proxy indicators such as voter turnout (81), or survey data (41, 64, 164, 191) are commonly used. The indicator category of social networks is also listed in the RKI scoping review (200) and in the ICF (201) expressing its relevance.
The indicators of discrimination, minority stress, stigma and racism were assigned to the superordinate topic “attitudinal factors toward vulnerable people” and represent the attitudinal environment. In the ICF, attitudinal factors are described as observable consequences of customs, ideologies, values, and norms influencing both individual behavior and social life at all levels (201, 203). This affects individuals in their personal and professional lives, as well as societal attitudinal factors and social norms. In the identified studies, attitudinal factors toward vulnerable groups were most studied in high-risk groups, mainly in ethnic/racial and sexual/gender minorities. Discrimination is associated with a higher cumulative risk of negative long-term effects on mental health (207). The RKI identified stigma, self-stigma and anti-stigma movements, discrimination, discrimination due to mental health problems, and perceived legitimacy of discrimination of people with mental disorders as six relevant indicators for a future national MHS (200). This is of enormous importance as heterogeneous communities are advised to create an inclusive and supportive environment to prevent mental illness in the first place (207). This goes in line with the recommendation provided in the ECCM.
In the prevention and health promotion oriented ECCM (11), the newly introduced categories in the domain of community resources and policies include the creation of supportive environments, building healthy public policies and strengthening community action. The identified indicators can support the ECCM by providing measures to indicate the direction of action but also enrich the ECCM toward an Extended Chronic Mental Care Model. As indicators rely on continuous good quality data, a “broadly-based information system to include community data beyond the health care system” is needed and also suggested by ECCM (11). Routinely collected data can provide an integrated picture to fully understand the communities´ context and needs to inform policy makers, municipalities, and stakeholders. It is worth noticing that many community indicators in the identified literature were assessed based on primary data. Routinely collected data on the physical and social environment is often not available, which imposes a barrier to monitoring.
Factors in the physical environment that had been proven to impact people’s health include harmful substances (e.g., air pollution), access to health-related resources and the built environment (204, 208). The indicator category of the built environment was most frequently discussed in the reviewed literature (n = 41). It comprises the indicators: built neighborhood environment, access to and quality of housing, green and blue space, attractiveness, and indoor sunlight opportunity. Of these, green and blue spaces were studied most frequently and their association with mental health is getting more attention. Still, the physical environment domain is less frequently researched compared to the social environment in the context of mental health. It was neglected for a long time but meanwhile there is growing evidence for its contribution to mental health (209).
Several studies documented the effects of elements of the physical environment (e.g., exposure to harmful substances in the air/air pollution) on somatic diseases, especially cardiovascular and respiratory morbidity (204, 210–213). Specific disease-related mechanisms had been identified by which these exposures affect inflammatory, autonomic, and vascular processes (204, 210, 213). These processes can also influence mental health and the initiation of mental disease (214, 215).
The built environment can influence mental health directly or indirectly by affecting psychosocial and behavioral processes (209). Such processes that are known to be linked to mental health are for example personal control (e.g., over noise and crowded homes), social support (e.g., great distance and residence and high-traffic volume streets is associated with reduced social interaction) as well as restoration and recovery from fatigue and stress (e.g., by the presence of natural elements). These hypotheses and the growing amount of literature underpinning them stress the need to include physical environment indicators in population mental health surveillances. Also, the ICF considers the built environment in the chapter “Natural environment and human-made changes to environment.” Among the methodological challenges to estimate the association between the physical environment and mental health are the self-selection of individuals into settings, inadequate environmental measurements, poor exposure assessment and over-reliance on self-reported indicators (209).
In this review, the distribution of community-level indicators and the representation of populations varied among the identified studies. While high-risk populations were commonly studied under the aspect of attitudinal factors toward vulnerable groups and social networks, the indicator categories of the general population were distributed more evenly between social networks, built environment, security, deprivation, and pollution. Adults were more frequently studied than children and adolescents (n = 141 vs. n = 28, respectively). For the age group <19 years, there are only few studies available, which could be regarded as a major “gap” as the average onset of mental health disorders is at the age of 14.5 years (216). Primary prevention and early intervention programs can alter the course of mental health disorders and improve outcomes at the same time (217, 218). Mental health promotion and prevention achieves its optimal benefits when young people are targeted at the time of or even before onset of mental health problems (216).
In high-risk populations, minority groups, followed by patients with comorbidities, were most frequently studied (n = 85 and n = 13, respectively). Despite the known association between physical disease and depression, this did not translate into the amount of literature identified. This lack is surprising, as especially in the development and severity of cardiovascular disease, social (219) and environmental (220) aspects are known risk factors. Also, only a few studies on post-partum women, another risk group for the development of mental disorders, were included despite a prevalence of up to 15% of depression in this group (221). The exclusion of post-partum women may be due to the strict exclusion criteria as this group is mainly investigated in a clinical setting.
Many of the identified community indicators are not included in existing surveillance and monitoring systems, possibly because they are either novel, continue to be unrecognized, or face operationalization challenges. Up to now, the physical environment was less recognized as relevant for public mental health. In particular, climate change, and pollution is receiving more attention due to the collective crisis awareness. In this review, the focus is on the community setting, which results in only two studies on climate change and mental health despite rapidly growing body of literature (222). Nonetheless, we emphasize that climate change and the associated climate emergency and its relation to mental health should be picked up in future research. Climate change will continue to contribute to more natural disasters in the future which may impact people’s wellbeing to a large degree and affect a greater proportion of the population (223). Climate change and pollution must be addressed on a community level by low-threshold interventions (e.g., by planting more trees against heat, noise, and pollution) but also on a national and global level.
Given the constant interaction and exposure of the individual to features of the social and physical environment, even minor changes can have a significant impact on population health. Communities can act as facilitators for mental health promotion and prevention and may therefore significantly support the efforts of the mental health care sector.
4.2. Limitations and future research
Applying state-of-the-art methodology, this scoping review also comes with its limitations: First, the terms “community” and “neighborhood” are often insufficiently defined in studies and therefore the authors had to make explicit decisions about what a person perceives as their area of residence. In this review, we refer to the community as people living in the same geographical area, which is clearly just one core element of a community. As most patients with mental health problems are treated in primary care settings and one central pillar of the Chronic Care Model concept are community resources, we were interested in seeing which community factors can add to the management of mental health problems. As we focus on geographical communities, we neglected communities that were beyond spatial boundaries such as online communities. Hence, we also explicitly excluded studies with a digital focus, which may in turn offer additional factors that might have been excluded.
Second, scoping reviews are not intended to provide in-depth information on the included studies, nor do they provide information on the relationship or correlation between each indicator and mental health. As we report the frequency of published papers with the mentioned indicators, a publication and researcher bias should be taken into account. And it is very possible that there is more data available or accessible for certain indicators than for others without meaning that the frequency of investigations reflects the importance or relevance of an indicator. No methodological quality appraisal of the included studies was conducted, which limits the implications for practice. Further studies should conduct a more extensive research on the identified indicator categories. With this scoping review, we point to community indicators, which have been of interest in previous studies and direct us to new fields for future research. Within the scope of spin-off projects, it will be necessary to hone in on the key domains, identify standardized tools within these areas, and evaluate their applicability, implementation, value, and usage within the context of community mental health approaches.
Third, due to the strict exclusion criteria, especially regarding the location as we were focusing only on the European context, some indicators could not (e.g., disasters and terrorism) or just to a limited degree (e.g., climate change) be represented in the final synthesis.
Fourth, the literature search was limited to three databases, so we could probably not cover the entire breadth of community settings.
This scoping review provides the first collection of community-level indicators that may influence public mental health. More research is needed to evaluate the operationalization, contribution and the prognostic relevance of each indicator on mental health and should be routinely included in mental health surveillance systems as cofounders. Further, relevant community-level indicators should be considered in the management and prevention of mental disorders.
4.3. Conclusion
This scoping review covers a comprehensive set of community indicators, some of which are already well known as contributing factors to mental health, and others whose importance has recently gained more attention and may reveal latest trends in key areas. It complements the picture of community factors that should be represented in the biopsychosocial models of disease, and should also be routinely collected in surveillance systems to investigate their importance and role as a confounding factor. Future research should, on the one hand focus more on children and adolescents as this is the time when mental health promotion and prevention should start, and on the other hand on emerging new fields such as climate change.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
POKAL-group
The following doctoral students are as well members of the POKAL-Group: Jochen Vukas, Puya Younesi, Feyza Gökce, Victoria von Schrottenberg, Petra Schönweger, Hannah Schillock, Jonas Raub, Philipp Reindl-Spanner, Lisa Hattenkofer, Lukas Kaupe, Carolin Haas, Julia Eder, Vita Brisnik, Constantin Brand and Katharina Biersack.
Author contributions
PS and CJ-S defined and developed the study question, protocol, and search strategy. PS, A-FM, KB, PR-S, and MK performed title, abstract, and full-text screening, as well as data extraction. Attachments and figures were composed by PS and A-FM. The manuscript was commented by MK, KB, A-FM, BP, JG, PH, HK, and CD-J. The manuscript was finally drafted by PS and finalized by PS and CJ-S. All authors contributed to the article and approved the submitted version.
Funding
The Research Training Group “PrediktOren und Klinische Ergebnisse bei depressiven ErkrAnkungen in der hausärztLichen Versorgung” (POKAL, DFG-GRK 2621; Predictors and Clinical Outcomes of Depressive Disorders in Primary Care) POKAL is a member of the German Research Foundation (DFG) and has developed the comprehensive qualification concept that aims to effectively support both health care providers and stakeholders and improve the future treatment of depression in primary care. The focus is on depression as the most common diagnosis.
Acknowledgments
The authors would like to thank the POKAL-Study group that consists of the following principle investigators: Tobias Dreischulte, Peter Falkai, Jochen Gensichen, Peter Henningsen, Markus Bühner, Caroline Jung-Sievers, Helmut Krcmar, Karoline Lukaschek, Gabriele Pitschel-Walz and Antonius Schneider.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1188494/full#supplementary-material
References
1. Arias-de la Torre, J, Vilagut, G, Ronaldson, A, Serrano-Blanco, A, Martín, V, Peters, M, et al. Prevalence and variability of current depressive disorder in 27 European countries: a population-based study. Lancet Public Health. (2021) 6:e729–38. doi: 10.1016/S2468-2667(21)00047-5
3. Vos, T, Allen, C, Arora, M, Barber, RM, Brown, A, Carter, A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
4. Jorm, AF. Why hasn’t the mental health of Australians improved? The need for a national prevention strategy. Aust N Z J Psychiatry. (2014) 48:795–801. doi: 10.1177/0004867414546387
5. Muñoz, RF, Cuijpers, P, Smit, F, Barrera, AZ, and Leykin, Y. Prevention of major depression. Annu Rev Clin Psychol. (2010) 6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040
6. World Health Organization (2022). World mental health report: Transforming mental health for all. Available at: https://www.who.int/news/item/17-06-2022-who-highlights-urgent-need-to-transform-mental-health-and-mental-health-care
7. Stoto, M. A., Behrens, R., and Rosemont, C. (1990). Health Promotion and Disease Prevention in Community Settings.
8. Glasgow, RE, Tracy Orleans, C, and Wagner, EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. (2001) 79:579–612. doi: 10.1111/1468-0009.00222
9. Allen, J, Balfour, R, Bell, R, and Marmot, M. Social determinants of mental health. Int Rev Psychiatry. (2014) 26:392–407. doi: 10.3109/09540261.2014.928270
10. Bauer, MS, Weaver, K, Kim, B, Miller, C, Lew, R, Stolzmann, K, et al. The collaborative chronic care model for mental health conditions: from evidence synthesis to policy impact to scale-up and spread. Med Care. (2019) 57:S221–7. doi: 10.1097/MLR.0000000000001145
11. Barr, VJ, Robinson, S, Marin-Link, B, Underhill, L, Dotts, A, Ravensdale, D, et al. The expanded chronic care model: an integration of concepts and strategies from population health promotion and the chronic care model. Hosp Q. (2003) 7:73–82. doi: 10.12927/hcq.2003.16763
12. Campbell, NRC, Lackland, DT, Lisheng, L, Zhang, X-H, Nilsson, PM, Redburn, KA, et al. The world hypertension league challenges hypertension and cardiovascular organizations to develop strategic plans for the prevention and control of hypertension. J Clin Hypertens. (2015) 17:325–7. doi: 10.1111/jch.12557
13. Delon, S, and Mackinnon, B. Alberta’s systems approach to chronic disease management and prevention utilizing the expanded chronic care model. Healthc Q. (2009) 13:98–104. doi: 10.12927/HCQ.2009.21106
14. Buechner, H., Toparlak, S. M., Ostinelli, E. G., Shokraneh, F., Nicholls-Mindlin, J., Cipriani, A., et al. (2023). Community interventions for anxiety and depression in adults and young people: a systematic review. Aust N Z J Psychiatry doi: 10.1177/00048674221150362 (Epub ahead of print).
15. Makizako, H, Tsutsumimoto, K, Doi, T, Makino, K, Nakakubo, S, Liu-Ambrose, T, et al. Exercise and horticultural programs for older adults with depressive symptoms and memory problems: a randomized controlled trial. J Clin Med. (2019) 9. doi: 10.3390/jcm9010099
16. Vujcic, M, Tomicevic-Dubljevic, J, Grbic, M, Lecic-Tosevski, D, Vukovic, O, and Toskovic, O. Nature based solution for improving mental health and well-being in urban areas. Environ Res. (2017) 158:385–92. doi: 10.1016/j.envres.2017.06.030
17. Saelens, BE, and Handy, SL. Built environment correlates of walking: a review. Med Sci Sports Exerc. (2008) 40:S550–66. doi: 10.1249/MSS.0B013E31817C67A4
18. Khair, N, Mohd Ali, H, and Juhari, NH. Assessment of physical environment elements in public low-cost housing. J Teknol. (2015) 74:23–9. doi: 10.11113/JT.V74.4519
19. Suglia, SF, Shelton, RC, Hsiao, A, Wang, YC, Rundle, A, and Link, BG. Why the neighborhood social environment is critical in obesity prevention. J Urban Health. (2016) 93:206. doi: 10.1007/s11524-015-0017-6
20. Generaal, E, Hoogendijk, EO, Stam, M, Henke, CE, Rutters, F, Oosterman, M, et al. Neighbourhood characteristics and prevalence and severity of depression: pooled analysis of eight Dutch cohort studies. Br J Psychiatry. (2019) 215:468–75. doi: 10.1192/bjp.2019.100
21. Oberndorfer, M, Dorner, TE, Leyland, AH, Grabovac, I, Schober, T, Sramek, L, et al. The challenges of measuring social cohesion in public health research: a systematic review and ecometric meta-analysis. SSM Popul Health. (2022) 17:101028. doi: 10.1016/j.ssmph.2022.101028
22. Schiefer, D, and Van Der Noll, J. The essentials of social cohesion: A literature review. Soc Indic Res. (2016) 132:579–603. doi: 10.1007/s11205-016-1314-5
23. Kress, S, Razum, O, Zolitschka, KA, Breckenkamp, J, Sauzet, O, and Sauzet, O. Does social cohesion mediate neighbourhood effects on mental and physical health? Longitudinal analysis using German socio-economic panel data. BMC Public Health. (2020) 20:1043. doi: 10.1186/s12889-020-09149-8
24. Di Martino, S, and Prilleltensky, I. Happiness as fairness: the relationship between national life satisfaction and social justice in EU countries. J Commun Psychol. (2020) 48:1997–2012. doi: 10.1002/jcop.22398
25. Prilleltensky, I. Psychosocial intervention meaning-making, mattering, and thriving in community psychology: from co-optation to amelioration and transformation. Psychosoc Interv. (2014) 23:151–4. doi: 10.1016/j.psi.2014.07.008
26. Kaye-Blake, W., Smith, M., and Stirrat, K. (2017). Signs to look for: Criteria for developing and selecting fit for purpose indicators. Available at: https://www.researchgate.net/publication/322491574_Signs_to_look_for_Criteria_for_developing_and_selecting_fit_for_purpose_indicators
27. Peters, M., Godfrey, C. M., Mcinerney, P., and Soares, C. B. (2015). Methodology for JBI scoping reviews pharmacy workforce view project tonsillectomy view project. Available at: https://www.researchgate.net/publication/294736492
28. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthes. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
29. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
30. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
31. Abebe, DS, Lien, L, and Hjelde, KH. What we know and don’t know about mental health problems among immigrants in Norway. J Immigr Minor Health. (2014) 16:60–7. doi: 10.1007/s10903-012-9745-9
32. Adriaanse, M, Veling, W, Doreleijers, T, and van Domburgh, L. The link between ethnicity, social disadvantage and mental health problems in a school-based multiethnic sample of children in the Netherlands. Eur Child Adolesc Psychiatry. (2014) 23:1103–13. doi: 10.1007/s00787-014-0564-5
33. Adriaanse, M, Doreleijers, T, Domburgh, L, and Veling, W. Factors associated with psychiatric symptoms and psychiatric disorders in ethnic minority youth. Eur Child Adolesc Psychiatry. (2016) 25:1067–79. doi: 10.1007/s00787-016-0829-2
34. Ahnquist, J, Wamala, SP, and Lindstrom, M. Social determinants of health – a question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc Sci Med. (2012) 74:930–9. doi: 10.1016/j.socscimed.2011.11.026
35. Aichberger, MC, Bromand, Z, Rapp, MA, Yesil, R, Montesinos, AH, Temur-Erman, S, et al. Perceived ethnic discrimination, acculturation, and psychological distress in women of Turkish origin in Germany. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1691–700. doi: 10.1007/s00127-015-1105-3
36. Almquist, YB, Östberg, V, Rostila, M, Edling, C, and Rydgren, J. Friendship network characteristics and psychological well-being in late adolescence: exploring differences by gender and gender composition. Scand J Public Health. (2014) 42:146–54. doi: 10.1177/1403494813510793
37. Astell-Burt, T, Mitchell, R, and Hartig, T. The association between green space and mental health varies across the lifecourse a longitudinal study. J Epidemiol Community Health. (2014) 68:578–83. doi: 10.1136/jech-2013-203767
38. Bailey, J, Taylor, L, Kingston, P, and Watts, G. Older adults and “scams”: evidence from the mass observation archive. J Adult Protect. (2021) 23:57–69. doi: 10.1108/JAP-07-2020-0030
39. Bakic, H, and Ajdukovic, D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. (2019) 10:1614821. doi: 10.1080/20008198.2019.1614821
40. Bakic, H, and Ajdukovic, D. Resilience after natural disasters: the process of harnessing resources in communities differentially exposed to a flood. Eur J Psychotraumatol. (2021) 12:1891733. doi: 10.1080/20008198.2021.1891733
41. Bamford, J, Klabbers, G, Curran, E, Rosato, M, and Leavey, G. Social capital and mental health among black and minority ethnic groups in the UK. J Immigr Minor Health. (2021) 23:502–10. doi: 10.1007/s10903-020-01043-0
42. Baranyi, G, Sieber, S, Pearce, J, Cheval, B, Dibben, C, Kliegel, M, et al. A longitudinal study of neighbourhood conditions and depression in ageing European adults: do the associations vary by exposure to childhood stressors? Prevent Med. (2019) 126:105764. doi: 10.1016/j.ypmed.2019.105764
43. Barratt, C, Green, G, and Speed, E. Mental health and houses in multiple occupation. J Public Ment Health. (2015) 14:107–17. doi: 10.1108/JPMH-11-2013-0070
44. Barriuso-Lapresa, L, Hernando-Arizaleta, L, and Rajmil, L. Social inequalities in mental health and health-related quality of life in children in Spain. Pediatrics. (2012) 130:e528–35. doi: 10.1542/peds.2011-3594
45. Bastos, AM, Faria, C, Moreira, E, Morais, D, Melo-de-Carvalho, JM, and Paul, MC. The importance of neighborhood ecological assets in community dwelling old people aging outcomes: a study in northern Portugal. Frontiers in aging. Neuroscience. (2015) 7:156. doi: 10.3389/FNAGI.2015.00156/BIBTEX
46. Borsch, AS, de Montgomery, CJ, Gauffin, K, Eide, K, Heikkilä, E, and Smith Jervelund, S. Health, education and employment outcomes in young refugees in the Nordic countries: a systematic review. Scand J Public Health. (2019) 47:735–47. doi: 10.1177/1403494818787099
47. Botchkovar, EV, Antonaccio, O, and Hughes, LA. Neighbourhood disorder, collective sentiments and personal strain: bringing neighbourhood context into general strain theory. Br J Criminol. (2018) 58:455–77. doi: 10.1093/bjc/azx023
48. Castaneda, AE, Rask, S, Koponen, P, Suvisaari, J, Koskinen, S, Härkänen, T, et al. The association between discrimination and psychological and social well-being: a population-based study of Russian, Somali and Kurdish migrants in Finland. Psychol Dev Soc. (2015) 27:270–92. doi: 10.1177/0971333615594054
49. Cecil, CAM, Viding, E, Barker, ED, Guiney, J, and McCrory, EJ. Double disadvantage: the influence of childhood maltreatment and community violence exposure on adolescent mental health. J Child Psychol Psychiatry. (2014) 55:839–48. doi: 10.1111/jcpp.12213
50. Chaves, C, Castellanos, T, Abrams, M, and Vazquez, C. The impact of economic recessions on depression and individual and social well-being: the case of Spain (2006–2013). Soc Psychiatry Psychiatr Epidemiol. (2018) 53:977–86. doi: 10.1007/s00127-018-1558-2
51. Cramer, S, Losert, C, Schmau, M, and Kilian, R. Associations between community characteristics and psychiatric admissions in an urban area. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1797–808. doi: 10.1007/S00127-013-0667-1
52. Cramm, JM, van Dijk, HM, and Nieboer, AP. Het belang van sociale cohesie en sociaal kapitaal in de buurt voor het welzijn van ouderen = the importance of neighborhood social cohesion and social capital for the well being of older adults in the community. Tijdschr Gerontol Geriatr. (2013) 44:50–8. doi: 10.1007/s12439-013-0010-z
53. Curtis, S, Pain, R, Fuller, S, Khatib, Y, Rothon, C, Stansfeld, SA, et al. Neighbourhood risk factors for common mental disorders among young people aged 10-20 years: a structured review of quantitative research. Health Place. (2013) 20:81–90. doi: 10.1016/j.healthplace.2012.10.010
54. Dabbagh, N, Johnson, S, King, M, and Blizard, R. Muslim adolescent mental health in the UK: an exploratory cross-sectional school survey. Int J Cult Ment Health. (2012) 5:202–18. doi: 10.1080/17542863.2011.594246
55. de Freitas, D, Fonseca Fernandes-Jesus, M, Ferreira, PD, Coimbra, S, Teixeira, PM, de Moura, A, et al. Psychological correlates of perceived ethnic discrimination in Europe: a meta-analysis. Psychol Violence. (2018) 8:712–25. doi: 10.1037/vio0000215
56. de Vries, S, van Dillen, SME, Groenewegen, PP, and Spreeuwenberg, P. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc Sci Med. (2013) 94:26–33. doi: 10.1016/j.socscimed.2013.06.030
57. Delaruelle, K, Walsh, SD, Dierckens, M, Deforche, B, Kern, MR, Currie, C, et al. Mental health in adolescents with a migration background in 29 European countries: the buffering role of social capital. J Youth Adolesc. (2021) 50:855–71. doi: 10.1007/s10964-021-01423-1
58. Derdikman-Eiron, R, Hjemdal, O, Lydersen, S, Bratberg, GH, and Indredavik, MS. Adolescent predictors and associates of psychosocial functioning in young men and women: 11 year follow-up findings from the Nord-Trøndelag health study. Scand J Psychol. (2013) 54:95–101. doi: 10.1111/sjop.12036
59. Dewaele, A, Van Houtte, M, and Vincke, J. Visibility and coping with minority stress: a gender-specific analysis among lesbians, gay men, and bisexuals in Flanders. Arch Sex Behav. (2014) 43:1601–14. doi: 10.1007/s10508-014-0380-5
60. Domènech-Abella, J, Mundó, J, Leonardi, M, Chatterji, S, Tobiasz-Adamczyk, B, Koskinen, S, et al. Loneliness and depression among older European adults: the role of perceived neighborhood built environment. Health Place. (2020) 62:102280. doi: 10.1016/j.healthplace.2019.102280
61. Donisi, V, Tedeschi, F, Percudani, M, Fiorillo, A, Confalonieri, L, De Rosa, C, et al. Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Res. (2013) 209:691–8. doi: 10.1016/j.psychres.2013.02.031
62. Economou, M, Souliotis, K, Peppou, LE, Agapidaki, I, Tzavara, C, and Stefanis, CN. Major depression in Cyprus amid financial crisis: prevalence and correlates. Int J Cult Ment Health. (2018) 11:255–67. doi: 10.1080/17542863.2017.1364283
63. Economou, M, Madianos, M, Peppou, LE, Souliotis, K, Patelakis, A, and Stefanis, C. Cognitive social capital and mental illness during economic crisis: a nationwide population-based study in Greece. Soc Sci Med. (2014) 100:141–7. doi: 10.1016/j.socscimed.2013.11.006
64. Elliott, J, Gale, CR, Parsons, S, and Kuh, D. Neighbourhood cohesion and mental wellbeing among older adults: a mixed methods approach. Soc Sci Med. (2014) 1982:44–51. doi: 10.1016/J.SOCSCIMED.2014.02.027
65. Engemann, K, Pedersen, CB, Arge, L, Tsirogiannis, C, Mortensen, PB, and Svenning, J-C. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proc Nat Acad Sci USA. (2019) 116:5188–93. doi: 10.1073/pnas.1807504116
66. Engemann, K, Pedersen, CB, Agerbo, E, Arge, L, Børglum, AD, Erikstrup, C, et al. Association between childhood green space, genetic liability, and the incidence of schizophrenia. Schizophr Bull. (2020) 46:1629–37. doi: 10.1093/schbul/sbaa058
67. Essers, E, Pérez-Crespo, L, Foraster, M, Ambrós, A, Tiemeier, H, and Guxens, M. Environmental noise exposure and emotional, aggressive, and attention-deficit/hyperactivity disorder-related symptoms in children from two European birth cohorts. Environ Int. (2022) 158:106946. doi: 10.1016/j.envint.2021.106946
68. Ettema, D, and Schekkerman, M. How do spatial characteristics influence well-being and mental health? Comparing the effect of objective and subjective characteristics at different spatial scales. Travel Behav Soc. (2016) 5:56–67. doi: 10.1016/j.tbs.2015.11.001
69. Finegan, M, Firth, N, and Delgadillo, J. Adverse impact of neighbourhood socioeconomic deprivation on psychological treatment outcomes: the role of area-level income and crime. Psychother Res. (2020) 30:546–54. doi: 10.1080/10503307.2019.1649500
70. Fone, D, White, J, Farewell, D, Kelly, M, John, G, Lloyd, K, et al. Effect of neighborhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol Med. (2014) 44:2449–60. doi: 10.1017/S0033291713003255
71. Forsman, AK, Nyqvist, F, Schierenbeck, I, Gustafson, Y, and Wahlbeck, K. Structural and cognitive social capital and depression among older adults in two nordic regions. Aging Ment Health. (2012) 16:771–9. doi: 10.1080/13607863.2012.667784
72. Foy, AAJ, Morris, D, Fernandes, V, and Rimes, KA. LGBQ+ adults’ experiences of improving access to psychological therapies and primary care counselling services: informing clinical practice and service delivery. Cogn Behav Therap. (2019) 12:E42. doi: 10.1017/S1754470X19000291
73. Freitas, DF, D’Augelli, AR, Coimbra, S, and Fontaine, AM. Discrimination and mental health among gay, lesbian, and bisexual youths in Portugal: the moderating role of family relationships and optimism. J GLBT Fam Stud. (2016) 12:68–90. doi: 10.1080/1550428X.2015.1070704
74. Friborg, O, Sørlie, T, and Hansen, KL. Resilience to discrimination among indigenous Sami and non-Sami populations in Norway: the SAMINOR2 study. J Cross-Cult Psychol. (2017) 48:1009–27. doi: 10.1177/0022022117719159
75. Gaum, PM, Gube, M, Esser, A, Schettgen, T, Quinete, N, Bertram, J, et al. Depressive Symptoms After PCB Exposure: Hypotheses for Underlying Pathomechanisms via the Thyroid and Dopamine System. Int. J. Environ. Res. Public Health. (2019) 16:950. doi: 10.3390/ijerph16060950
76. Generaal, E, Timmermans, EJ, Dekkers, JEC, Smit, JH, and Penninx, BWJH. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol Med. (2019) 49:149–61. doi: 10.1017/S0033291718000612
77. Gnan, GH, Rahman, Q, Ussher, G, Baker, D, West, E, and Rimes, KA. General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. J Youth Stud. (2019) 22:1393–408. doi: 10.1080/13676261.2019.1581361
78. Gonzales-Inca, C, Pentti, J, Stenholm, S, Suominen, S, Vahtera, J, and Käyhkö, N. Residential greenness and risks of depression: Longitudinal associations with different greenness indicators and spatial scales in a Finnish population cohort. Health Place. (2022) 74:102760. doi: 10.1016/j.healthplace.2022.102760
79. Gubbels, JS, Kremers, SPJ, Droomers, M, Hoefnagels, C, Stronks, K, Hosman, C, et al. The impact of greenery on physical activity and mental health of adolescent and adult residents of deprived neighborhoods: a longitudinal study. Health Place. (2016) 40:153–60. doi: 10.1016/j.healthplace.2016.06.002
80. Hackett, RA, Steptoe, A, and Jackson, SE. Sex discrimination and mental health in women: a prospective analysis. Health Psychol. (2019) 38:1014–24. doi: 10.1037/hea0000796
81. Hamano, T, Li, X, Lönn, SL, Nabika, T, Sundquist, J, and Sundquist, K. Is familial risk for depression confounded by individual and familial socioeconomic factors and neighborhood environmental factors? A 7-year follow-up study in Sweden. Psychiatry Res. (2018) 266:30. doi: 10.1016/j.psychres.2018.05.041
82. Hansen, KL, and Sørlie, T. Ethnic discrimination and psychological distress: a study of Sami and non-Sami populations in Norway. Transcult Psychiatry. (2012) 49:26–50. doi: 10.1177/1363461511433944
83. Hatch, SL, Gazard, B, Williams, DR, Frissa, S, Goodwin, L, and Hotopf, M. Discrimination and common mental disorder among migrant and ethnic groups: findings from a South East London community sample. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:689–701. doi: 10.1007/s00127-016-1191-x
84. Helsen, V, Enzlin, P, and Gijs, L. Mental health in transgender adults: the role of proximal minority stress, community connectedness, and gender nonconformity. Psychol Sex Orientat Gend Divers. (2021) 4:466–477. doi: 10.1037/sgd0000530
85. Hüfner, K, Ower, C, Kemmler, G, Vill, T, Martini, C, Schmitt, A, et al. Viewing an alpine environment positively affects emotional analytics in patients with somatoform, depressive and anxiety disorders as well as in healthy controls. BMC Psychiatry. (2020) 20:385. doi: 10.1186/s12888-020-02787-7
86. Igde, E, Heinz, A, Schouler-Ocak, M, and Rössler, W. Depressive und somatoforme Störungen bei türkeistämmigen Personen in Deutschland = depressive and somatoform disorders in persons with a Turkish migration background in Germany. Nervenarzt. (2019) 90:25–34. doi: 10.1007/s00115-018-0602-5
87. Ikram, UZ, Snijder, MB, Fassaert, TJL, Schene, AH, Kunst, AE, and Stronks, K. The contribution of perceived ethnic discrimination to the prevalence of depression. Eur J Pub Health. (2015) 25:243–8. doi: 10.1093/eurpub/cku180
88. Infurna, MR, Giannone, F, Guarnaccia, C, Lo Cascio, M, Parzer, P, and Kaess, M. Environmental factors that distinguish between clinical and healthy samples with childhood experiences of abuse and neglect. Psychopathology. (2015) 48:256–63. doi: 10.1159/000435959
89. Jackson, SE, Hackett, RA, Grabovac, I, Smith, L, and Steptoe, A. Perceived discrimination, health and wellbeing among middle-aged and older lesbian, gay and bisexual people: a prospective study. PLoS One. (2019) 14:e0216497. doi: 10.1371/journal.pone.0216497
90. Junghans, C, and Jones, M. Consent bias in research: how to avoid it. Heart. (2007) 93:1024–5. doi: 10.1136/hrt.2007.120113
91. Jonsson, KR, Vartanova, I, and Södergren, M. Ethnic variations in mental health among 10-15-year-olds living in England and Wales: the impact of neighbourhood characteristics and parental behaviour. Health Place. (2018) 51:189–99. doi: 10.1016/j.healthplace.2018.03.010
92. Källström, Å, Hellfeldt, K, Howell, KH, Miller-Graff, LE, and Graham-Bermann, SA. Young adults victimized as children or adolescents: relationships between perpetrator patterns, poly-victimization, and mental health problems. J Interpers Violence. (2020) 35:2335–57. doi: 10.1177/0886260517701452
93. Kendrick, K, Jutengren, G, and Stattin, H. The protective role of supportive friends against bullying perpetration and victimization. J Adolesc. (2012) 35:1069–80. doi: 10.1016/j.adolescence.2012.02.014
94. Klaperski, S, Koch, E, Hewel, D, Schempp, A, and Müller, J. Optimizing mental health benefits of exercise: the influence of the exercise environment on acute stress levels and wellbeing. Mental Health Prevent. (2019) 15:200173. doi: 10.1016/j.mhp.2019.200173
95. Knott, CS, Panter, J, Foley, L, and Ogilvie, D. Changes in the mode of travel to work and the severity of depressive symptoms: a longitudinal analysis of UK biobank. Prevent Med. (2018) 112:61–9. doi: 10.1016/j.ypmed.2018.03.018
96. Kreski, NT, Park, SH, Safren, SA, Goedel, WC, Morganstein, JG, Chaix, B, et al. Is neighborhood safety associated with depression symptoms, anxiety symptoms, and psychological distress among gay, bisexual, and other men who have sex with men? J Gay Lesbian Mental Health. (2018) 22:243–60. doi: 10.1080/19359705.2018.1463583
97. Kritsotakis, G, Vassilaki, M, Melaki, V, Georgiou, V, Philalithis, AE, Bitsios, P, et al. Social capital in pregnancy and postpartum depressive symptoms: a prospective mother–child cohort study (the Rhea study). Int J Nurs Stud. (2013) 50:63–72. doi: 10.1016/j.ijnurstu.2012.08.012
98. Kunst, M, and Van Wilsem, J. Trait impulsivity and change in mental health problems after violent crime victimization: a prospective analysis of the Dutch longitudinal internet studies for the social sciences database. J Interpers Violence. (2013) 28:1642–56. doi: 10.1177/0886260512468320
99. Lafferty, A, Duryae, EL, Martin, R, Moseley, L, Wafford, M, McIntire, DD, et al. A prospective study of social needs associated with mental health among mothers living in poverty. Am J Obstet Gynecol. (2022) 226:S593–4. doi: 10.1016/j.ajog.2021.11.979
100. Lakeman, R, McGowan, P, MacGabhann, L, Parkinson, M, Redmond, M, Sibitz, I, et al. A qualitative study exploring experiences of discrimination associated with mental-health problems in Ireland. Epidemiol Psychiatr Sci. (2012) 21:271–9. doi: 10.1017/S2045796012000017
101. Landstedt, E, Almquist, YB, Eriksson, M, and Hammarström, A. Disentangling the directions of associations between structural social capital and mental health: longitudinal analyses of gender, civic engagement and depressive symptoms. Soc Sci Med. (2016) 163:135–43. doi: 10.1016/j.socscimed.2016.07.005
102. Lanfredi, M, Zoppei, S, Ferrari, C, Bonetto, C, Van Bortel, T, Thornicroft, G, et al. Self-stigma as a mediator between social capital and empowerment among people with major depressive disorder in Europe: the ASPEN study. Eur Psychiatry. (2015) 30:58–64. doi: 10.1016/j.eurpsy.2014.06.002
103. Latham, RM, Kieling, C, Arseneault, L, Botter-Maio Rocha, T, Beddows, A, Beevers, SD, et al. Childhood exposure to ambient air pollution and predicting individual risk of depression onset in UK adolescents. J Psychiatr Res. (2021) 138:60–7. doi: 10.1016/j.jpsychires.2021.03.042
104. Lecerof, SS, Stafström, M, Westerling, R, and Östergren, P-O. Does social capital protect mental health among migrants in Sweden? Health Promot Int. (2016) 31:644–52. doi: 10.1093/heapro/dav048
105. Lee, EJ, Keyes, K, Bitfoi, A, Mihova, Z, Pez, O, Yoon, E, et al. Mental health disparities between Roma and non-Roma children in Romania and Bulgaria. BMC Psychiatry. (2014) 14. doi: 10.1186/s12888-014-0297-5
106. Levecque, K, and Van Rossem, R. Depression in Europe: does migrant integration have mental health payoffs? A cross-national comparison of 20 European countries. Ethn Health. (2015) 20:49–65. doi: 10.1080/13557858.2014.883369
107. Lindström, M, and Rosvall, M. Marital status, social capital, economic stress, and mental health: a population-based study. Soc Sci J. (2012) 49:339–42. doi: 10.1016/j.soscij.2012.03.004
108. Lindström, M, and Giordano, GN. The 2008 financial crisis: changes in social capital and its association with psychological wellbeing in the United Kingdom—a panel study. Soc Sci Med. (2016) 153:71–80. doi: 10.1016/j.socscimed.2016.02.008
109. Llorente, JM, Oliván-Blázquez, B, Zuñiga-Antón, M, Masluk, B, Andrés, E, García-Campayo, J, et al. Variability of the prevalence of depression in function of sociodemographic and environmental factors: ecological model. Front Psychol. (2018) 9:2182. doi: 10.3389/fpsyg.2018.02182
110. Magallares, A, Morales, JF, and Rubio, MÁ. Group identification, discrimination and psychological health in an obese sample. Int J Psychol Psycholog Therap. (2014) 14:421–31.
111. Magallares, A, Bolaños-Rios, P, Ruiz-Prieto, I, de Valle, P, Irles, JA, and Jáuregui-Lobera, I. The mediational effect of weight self-stigma in the relationship between blatant and subtle discrimination and depression and anxiety. Span J Psychol. (2017) 20. doi: 10.1017/sjp.2017.1
112. Mangalore, R, and Knapp, M. Income-related inequalities in common mental disorders among ethnic minorities in England. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:351–9. doi: 10.1007/s00127-011-0345-0
113. Markkula, N, Härkänen, T, Nieminen, T, Peña, S, Mattila, AK, Koskinen, S, et al. Prognosis of depressive disorders in the general population– results from the longitudinal Finnish health 2011 study. J Affect Disord. (2016) 190:687–96. doi: 10.1016/j.jad.2015.10.043
114. Jessye, MM, Coleman, JRI, Breen, G, and Vassos, E. Association between genetic risk for psychiatric disorders and the probability of living in urban settings. JAMA Psychiat. (2021) 78:1355–64. doi: 10.1001/jamapsychiatry.2021.2983
115. McEachan, RRC, Prady, SL, Smith, G, Fairley, L, Cabieses, B, Gidlow, C, et al. The association between green space and depressive symptoms in pregnant women: moderating roles of socioeconomic status and physical activity. J Epidemiol Community Health. (2016) 70:253–9. doi: 10.1136/jech-2015-205954
116. McGorrian, C, Hamid, NA, Fitzpatrick, P, Daly, L, Malone, KM, and Kelleher, C. Frequent mental distress (FMD) in Irish travellers: discrimination and bereavement negatively influence mental health in the all Ireland traveller health study. Transcult Psychiatry. (2013) 50:559–78. doi: 10.1177/1363461513503016
117. Mears, M, Brindley, P, Jorgensen, A, and Maheswaran, R. Population-level linkages between urban greenspace and health inequality: the case for using multiple indicators of neighbourhood greenspace. Health Place. (2020) 62. doi: 10.1016/j.healthplace.2020.102284
118. Mewes, R, Asbrock, F, and Laskawi, J. Perceived discrimination and impaired mental health in Turkish immigrants and their descendents in Germany. Compr Psychiatry. (2015) 62:42–50. doi: 10.1016/j.comppsych.2015.06.009
119. Missinne, S, and Bracke, P. Depressive symptoms among immigrants and ethnic minorities: a population based study in 23 European countries. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:97–109. doi: 10.1007/s00127-010-0321-0
120. Mock-Muñoz de Luna, CJ, Vitus, K, Torslev, MK, Krasnik, A, and Jervelund, SS. Ethnic inequalities in child and adolescent health in the Scandinavian welfare states: The role of parental socioeconomic status - a systematic review. Scand. J. Public Health. (2019) 47:679–89. doi: 10.1177/1403494818779853
121. Mölsä, M, Kuittinen, S, Tiilikainen, M, Honkasalo, M-L, and Punamäki, R-L. Mental health among older refugees: the role of trauma, discrimination, and religiousness. Aging Ment Health. (2017) 21:829–37. doi: 10.1080/13607863.2016.1165183
122. Motoc, I, Timmermans, EJ, Deeg, D, Penninx, BWJH, and Huisman, M. Associations of neighbourhood sociodemographic characteristics with depressive and anxiety symptoms in older age: results from a 5-wave study over 15 years. Health Place. (2019) 59. doi: 10.1016/j.healthplace.2019.102172
123. Mueller, MAE, Flouri, E, and Kokosi, T. The role of the physical environment in adolescent mental health. Health Place. (2019) 58:102153. doi: 10.1016/j.healthplace.2019.102153
124. Mueller, MAE, and Flouri, E. Neighbourhood greenspace and children’s trajectories of self-regulation: findings from the UK millennium cohort study. J Environ Psychol. (2020) 71:101472. doi: 10.1016/j.jenvp.2020.101472
125. Müller, LRF, Gossmann, K, Schmid, RF, Rosner, R, and Unterhitzenberger, J. A pilot study on ecological momentary assessment in asylum-seeking children and adolescents resettled to Germany: investigating compliance, post-migration factors, and the relation between daily mood, sleep patterns, and mental health. PLoS One. (2021) 16:e0246069. doi: 10.1371/journal.pone.0246069
126. Nesterko, Y, Seidel, N, Brähler, E, and Claesmer, H. Depression und Angst bei älteren russischstammigen Menschen mit jüdischem Hintergrund in Deutschland: Wie wirken sich Diskriminierung und Religiosität aus? = Depression and anxiety in elderly Jews from the former Soviet Union in Germany: The role of discrimination and religiosity. Psychiatr Prax. (2014) 41:76–81. doi: 10.1055/s-0033-1349647
127. Newbury, J, Arseneault, L, Caspi, A, Moffitt, TE, Odgers, CL, and Fisher, HL. Why are children in urban neighborhoods at increased risk for psychotic symptoms? Findings from a UK longitudinal cohort study. Schizophr Bull. (2016) 42:1372–83. doi: 10.1093/schbul/sbw052
128. Newbury, JB, Stewart, R, Fisher, HL, Beevers, S, Dajnak, D, Broadbent, M, et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: retrospective cohort study. Br J Psychiatry. (2021) 219:678–85. doi: 10.1192/bjp.2021.119
129. Nilsen, LG, Thoresen, S, Wentzel-Larsen, T, and Dyb, G. Trust after terror: institutional trust among young terror survivors and their parents after the 22nd of July terrorist attack on Utøya Island, Norway. Front Psychol. (2019) 10:2819. doi: 10.3389/fpsyg.2019.02819
130. Nimmo-Smith, V, Brugha, TS, Kerr, MP, McManus, S, and Rai, D. Discrimination, domestic violence, abuse, and other adverse life events in people with epilepsy: population-based study to assess the burden of these events and their contribution to psychopathology. Epilepsia. (2016) 57:1870–8. doi: 10.1111/epi.13561
131. Noordzij, JM, Beenackers, MA, Oude Groeniger, J, Timmermans, E, Chaix, B, Doiron, D, et al. Green spaces, subjective health and depressed affect in middle-aged and older adults: a cross-country comparison of four European cohorts. J Epidemiol Community Health. (2021) 75:470–6. doi: 10.1136/jech-2020-214257
132. Nyqvist, F, Forsman, AK, and Cattan, M. A comparison of older workers’ and retired older people’s social capital and sense of mastery. Scand J Public Health. (2013) 41:792–8. doi: 10.1177/1403494813498005
133. Oppedal, B, and Idsoe, T. The role of social support in the acculturation and mental health of unaccompanied minor asylum seekers. Scand J Psychol. (2015) 56:203–11. doi: 10.1111/sjop.12194
134. Østergaard, SD, Waltoft, BL, Mortensen, PB, and Mors, O. Environmental and familial risk factors for psychotic and non-psychotic severe depression. J Affect Disord. (2013) 147:232–40. doi: 10.1016/j.jad.2012.11.009
135. Papagavriel, K, Jones, R, Sheehan, R, Hassiotis, A, and Ali, A. The association between loneliness and common mental disorders in adults with borderline intellectual impairment. J Affect Disord. (2020) 277:954–61. doi: 10.1016/j.jad.2020.09.005
136. Putrik, P, de Vries, NK, Mujakovic, S, van Amelsvoort, L, Kant, I, Kunst, AE, et al. Living environment matters: relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J Commun Health Publ Health Promot Dis Prev. (2015) 40:47–56. doi: 10.1007/s10900-014-9894-y
137. Ram, B, Shankar, A, Nightingale, CM, Giles-Corti, B, Ellaway, A, Cooper, AR, et al. Comparisons of depression, anxiety, well-being, and perceptions of the built environment amongst adults seeking social, intermediate and market-rent accommodation in the former London Olympic athletes’ village. Health Place. (2017) 48:31–9. doi: 10.1016/j.healthplace.2017.09.001
138. Rask, S, Elo, IT, Koskinen, S, Lilja, E, Koponen, P, and Castaneda, AE. The association between discrimination and health: findings on Russian, Somali and Kurdish origin populations in Finland. Eur J Pub Health. (2018) 28:898–903. doi: 10.1093/eurpub/cky100
139. Recio, P, Molero, F, Silván-Ferrero, P, and Nouvilas-Pallejà, E. Perceived discrimination and emotional distress among family caregivers of children with physical disabilities: the mediational role of affiliate stigma and self-efficacy. Am J Orthop. (2021) 91:367–74. doi: 10.1037/ort0000534
140. Reinhard, E, Courtin, E, van Lenthe, FJ, and Avendano, M. Public transport policy, social engagement and mental health in older age: a quasi-experimental evaluation of free bus passes in England. J Epidemiol Community Health. (2018) 72:361–8. doi: 10.1136/jech-2017-210038
141. Riglin, L, Hammerton, G, Heron, J, Collishaw, S, Arseneault, L, Thapar, AK, et al. Developmental contributions of schizophrenia risk alleles and childhood peer victimization to early-onset mental health trajectories. Am J Psychiatry. (2019) 176:36–43. doi: 10.1176/appi.ajp.2018.18010075
142. Rimes, KA, Shivakumar, S, Ussher, G, Baker, D, Rahman, Q, and West, E. Psychosocial factors associated with suicide attempts, ideation, and future risk in lesbian, gay, and bisexual youth: the youth chances study. Crisis. (2019) 40:83–92. doi: 10.1027/0227-5910/a000527
143. Roberts, B, Murphy, A, Chikovani, I, Makhashvili, N, Patel, V, and McKee, M. Individual and community level risk-factors for alcohol use disorder among conflict-affected persons in Georgia. PLoS One. (2014) 9:e98299. doi: 10.1371/journal.pone.0098299
144. Roberts, S, Arseneault, L, Barratt, B, Beevers, S, Danese, A, Odgers, CL, et al. Exploration of NO₂ and PM25 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. (2019) 272:8–17. doi: 10.1016/j.psychres.2018.12.050
145. Roberts, H, van Lissa, C, and Helbich, M. Perceived neighbourhood characteristics and depressive symptoms: potential mediators and the moderating role of employment status. Soc Sci Med. (2021) 268:113533. doi: 10.1016/j.socscimed.2020.113533
146. Roccato, M, and Russo, S. Right-wing authoritarianism, societal threat to safety, and psychological distress. Eur J Soc Psychol. (2017) 47:600–10. doi: 10.1002/ejsp.2236
147. Rocha, K, Pérez, K, Rodríguez-Sanz, M, Obiols, JE, and Borrell, C. Perception of environmental problems and common mental disorders (CMD). Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1675–84. doi: 10.1007/s00127-012-0474-0
148. Romani, A, Mazzoli, F, Ristori, J, Cocchetti, C, Cassioli, E, Castellini, G, et al. Psychological wellbeing and perceived social acceptance in gender diverse individuals. J Sex Med. (2021) 18:1933–44. doi: 10.1016/j.jsxm.2021.08.012
149. Rothon, C, Goodwin, L, and Stansfeld, S. Family social support, community “social capital” and adolescents’ mental health and educational outcomes: a longitudinal study in England. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:697–709. doi: 10.1007/s00127-011-0391-7
150. Ruijsbroek, A, Mohnen, SM, Droomers, M, Kruize, H, Gidlow, C, Gražulevičiene, R, et al. Neighbourhood green space, social environment and mental health: an examination in four European cities. Int J Public Health. (2017) 62:657–67. doi: 10.1007/s00038-017-0963-8
151. Sáez, G, Valor-Segura, I, and Expósito, F. Interpersonal sexual objectification experiences: psychological and social well-being consequences for women. J Interpers Violence. (2019) 34:741–62. doi: 10.1177/0886260516645813
152. Sangster Jokić, C, and Bartolac, A. Iskustvo stresa i mentalno zdravlje osoba s tjelesnim invaliditetom: Perspektiva manjinskog stresa = the stress experience and mental health among persons with physical disabilities: a minority stress perspective. Socijalna Psihijatrija. (2018) 46:26–57. doi: 10.24869/spsih.2018.26
153. Sariaslan, A, Larsson, H, D’Onofrio, B, Långström, N, Fazel, S, and Lichtenstein, P. Does population density and neighborhood deprivation predict schizophrenia? A nationwide Swedish family-based study of 24 million individuals. Schizophr Bull. (2015) 41:494–502. doi: 10.1093/schbul/sbu105
154. Sattler, MC, Färber, T, Traußnig, K, Köberl, G, Paier, C, Dietz, P, et al. Cross-sectional association between active commuting and perceived commuting stress in Austrian adults: results from the HOTway study. Ment Health Phys Act. (2020) 19:100356. doi: 10.1016/j.mhpa.2020.100356
155. Sattler, FA, and Zeyen, J. Intersecting identities, minority stress, and mental health problems in different sexual and ethnic groups. Stigma Health. (2021) 6:457–66. doi: 10.1037/sah0000340
156. Saville, CWN. Ecological social capital does not predict geographical variance in increases in depression following the 2008 financial crisis. Br J Psychol. (2021) 112:163–79. doi: 10.1111/bjop.12448
157. Scandurra, C, Amodeo, AL, Valerio, P, Bochicchio, V, and Frost, DM. Minority stress, resilience, and mental health: a study of Italian transgender people. J Soc Issues. (2017) 73:563–85. doi: 10.1111/josi.12232
158. Schnittker, J. Religion, social integration, and depression in Europe: evidence from the European social survey. Soc Sci Med. (2020) 267:112376. doi: 10.1016/j.socscimed.2019.112376
159. Schrier, AC, Peen, J, de Wit, MAS, van Ameijden, EJC, Erdem, Ö, Verhoeff, AP, et al. Ethnic density is not associated with psychological distress in Turkish-Dutch, Moroccan-Dutch and Surinamese-Dutch ethnic minorities in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1557–67. doi: 10.1007/s00127-014-0852-x
160. Schubert, M, Hegewald, J, Freiberg, A, Starke, KR, Augustin, F, Riedel-Heller, SG, et al. Behavioral and emotional disorders and transportation noise among children and adolescents: a systematic review and Meta-analysis. Int J Environ Res Public Health. (2019) 16:3336. doi: 10.3390/ijerph16183336
161. Schunck, R, Reiss, K, and Razum, O. Pathways between perceived discrimination and health among immigrants: evidence from a large national panel survey in Germany. Ethn Health. (2015) 20:493–510. doi: 10.1080/13557858.2014.932756
162. Sevillano, V, Basabe, N, Bobowik, M, and Aierdi, X. Health-related quality of life, ethnicity and perceived discrimination among immigrants and natives in Spain. Ethn Health. (2014) 19:178–97. doi: 10.1080/13557858.2013.797569
163. Signoretta, PE, Buffel, V, and Bracke, P. Mental wellbeing, air pollution and the ecological state. Health Place. (2019) 57:82–91. doi: 10.1016/j.healthplace.2019.03.003
164. Simons, M, Lataster, J, Reijnders, J, Peeters, S, Janssens, M, and Jacobs, N. Bonding personal social capital as an ingredient for positive aging and mental well-being a study among a sample of Dutch elderly. Aging Ment Health. (2020) 24:2034–42. doi: 10.1080/13607863.2019.1650887
165. Singh, GK, Siahpush, M, Azuine, RE, and Williams, SD. Increasing area deprivation and socioeconomic inequalities in heart disease, stroke, and cardiovascular disease mortality among working age populations, United States, 1969-2011. Int J MCH AIDS. (2015) 3:119–33.
166. Slotman, A, Snijder, MB, Ikram, UZ, Schene, AH, and Stevens, GWJM. The role of mastery in the relationship between perceived ethnic discrimination and depression: the HELIUS study. Cult Divers Ethn Minor Psychol. (2017) 23:200–8. doi: 10.1037/cdp0000113
167. Smith, R, Drennan, V, Mackenzie, A, and Greenwood, N. The impact of befriending and peer support on family carers of people living with dementia: a mixed methods study. Arch Gerontol Geriatr. (2018) 76:188–95. doi: 10.1016/j.archger.2018.03.005
168. Smith, DM, Wang, SB, Carter, ML, Fox, KR, and Hooley, JM. Longitudinal predictors of self-injurious thoughts and behaviors in sexual and gender minority adolescents. J Abnorm Psychol. (2020) 129:114–21. doi: 10.1037/abn0000483
169. Sørensen, T, Kleiner, R, Ngo, P, Sørensen, A, and Bøe, N. From sociocultural disintegration to community connectedness dimensions of local community concepts and their effects on psychological health of its residents. Psychiatry J. (2013) 2013:1–13. doi: 10.1155/2013/872146
170. Spahlholz, J, Pabst, A, Riedel-Heller, SG, and Luck-Sikorski, C. Coping with perceived weight discrimination: testing a theoretical model for examining the relationship between perceived weight discrimination and depressive symptoms in a representative sample of individuals with obesity. Int J Obes. (2016) 40:1915–21. doi: 10.1038/ijo.2016.164
171. Stathopoulou, T, Avrami, L, Mouriki, A, Cavounidis, J, and Kostaki, A. Self-reported depression among migrant and native populations in Greece in times of crisis. Eur J Pub Health. (2018) 28:32–7. doi: 10.1093/eurpub/cky205
172. Steel, JL, Dunlavy, AC, Harding, CE, and Theorell, T. The psychological consequences of pre-emigration trauma and post-migration stress in refugees and immigrants from Africa. J Immigr Minor Health. (2017) 19:523–32. doi: 10.1007/s10903-016-0478-z
173. Stepanikova, I, and Kukla, L. Is perceived discrimination in pregnancy prospectively linked to postpartum depression? Exploring the role of education. Matern Child Health J. (2017) 21:1669–77. doi: 10.1007/s10995-016-2259-7
174. Stojanovski, K, Zhou, S, King, E, Gjorgjiovska, J, and Mihajlov, A. An application of the minority stress model in a non-Western context: discrimination and mental health among sexual and gender minorities in Macedonia. Sex Res Soc Policy. (2018) 15:367–76. doi: 10.1007/s13178-017-0299-4
175. Stronks, K, Şekercan, A, Snijder, M, Lok, A, Verhoeff, AP, Kunst, AE, et al. Higher prevalence of depressed mood in immigrants’ offspring reflects their social conditions in the host country: the HELIUS study. PLoS One. (2020) 15:e0234006. doi: 10.1371/journal.pone.0234006
176. Swanson, V, Sharpe, T, Porteous, C, Hunter, C, and Shearer, D. Indoor annual sunlight opportunity in domestic dwellings may predict well-being in urban residents in Scotland. Ecopsychology. (2016) 8:121–30. doi: 10.1089/eco.2015.0059
177. Tan, S-Y, and Haining, R. Crime victimization and the implications for individual health and wellbeing: a Sheffield case study. Soc Sci Med. (2016) 167:128–39. doi: 10.1016/j.socscimed.2016.08.018
178. Taylor, LK, Merrilees, CE, Cairns, E, Shirlow, P, Goeke-Morey, M, and Cummings, EM. Risk and resilience: the moderating role of social coping for maternal mental health in a setting of political conflict. Int J Psychol. (2013) 48:591–603. doi: 10.1080/00207594.2012.658055
179. Thomas, F. The role of natural environments within women’s everyday health and wellbeing in Copenhagen, Denmark. Health Place. (2015) 35:187–95. doi: 10.1016/j.healthplace.2014.11.005
180. Thoresen, S, Birkeland, MS, Wentzel-Larsen, T, and Blix, I. Loss of trust may never heal institutional trust in disaster victims in a long-term perspective: associations with social support and mental health. Front Psychol. (2018) 9:1204. doi: 10.3389/fpsyg.2018.01204
181. Timmins, L, Rimes, KA, and Rahman, Q. Minority stressors, rumination, and psychological distress in monozygotic twins discordant for sexual minority status. Psychol Med. (2018) 48:1705–12. doi: 10.1017/S003329171700321X
182. van den Berg, M, van Poppel, M, van Kamp, I, Andrusaityte, S, Balseviciene, B, Cirach, M, et al. Visiting green space is associated with mental health and vitality: a cross-sectional study in four European cities. Health Place. (2016) 38:8–15. doi: 10.1016/j.healthplace.2016.01.003
183. van den Berg, MM, van Poppel, M, van Kamp, I, Ruijsbroek, A, Triguero-Mas, M, Gidlow, C, et al. Do physical activity, social cohesion, and loneliness mediate the association between time spent visiting green space and mental health? Environ Behav. (2019) 51:144–66. doi: 10.1177/0013916517738563
184. Verelst, A, Spaas, C, Pfeiffer, E, Devlieger, I, Kankaapää, R, Peltonen, K, et al. Social determinants of the mental health of young migrants. European. J Health Psychol. (2022) 29:61–73. doi: 10.1027/2512-8442/a000097
185. Vilhjalmsdottir, A, Gardarsdottir, RB, Bernburg, JG, and Sigfusdottir, ID. Neighborhood income inequality, social capital and emotional distress among adolescents: a population-based study. J Adolesc. (2016) 51:92–102. doi: 10.1016/j.adolescence.2016.06.004
186. Voci, A, Hadziosmanovic, E, Cakal, H, Veneziani, CA, and Hewstone, M. Impact of pre-war and post-war intergroup contact on intergroup relations and mental health: evidence from a Bosnian sample. Peace Conflict. (2017) 23:250–9. doi: 10.1037/pac0000222
187. Weimann, H, Rylander, L, Albin, M, Skärbäck, E, Grahn, P, Östergren, P-O, et al. Effects of changing exposure to neighbourhood greenness on general and mental health: a longitudinal study. Health Place. (2015) 33:48–56. doi: 10.1016/j.healthplace.2015.02.003
188. White, MP, Alcock, I, Wheeler, BW, and Depledge, MH. Would you be happier living in a greener urban area? A fixed-effects analysis of panel data. Psychol Sci. (2013) 24:920–8. doi: 10.1177/0956797612464659
189. Wickham, S, Shryane, N, Lyons, M, Dickins, T, and Bentall, R. Why does relative deprivation affect mental health? The role of justice, trust and social rank in psychological wellbeing and paranoid ideation. J Public Ment Health. (2014) 13:114–26. doi: 10.1108/JPMH-06-2013-0049
190. Wiginton, JM, Murray, S, Kall, M, Maksut, JL, Augustinavicius, J, Delpech, V, et al. HIV-related stigma and discrimination in health care and health-related quality of life among people living with HIV in England and Wales: a latent class analysis. Stigma Health. (2021). doi: 10.1037/sah0000299
191. Wind, TR, and Komproe, IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med. (2012) 75:1715–20. doi: 10.1016/j.socscimed.2012.06.032
192. Wothge, J, and Niemann, H. Gesundheitliche Auswirkungen von Umgebungslärm im urbanen Raum Einleitung. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. (2020) 63:987–96. doi: 10.1007/s00103-020-03178-9
193. Wu, Y-T, Prina, AM, Jones, A, Barnes, LE, Matthews, FE, and Brayne, C. Micro-scale environment and mental health in later life: results from the cognitive function and ageing study II (CFAS II). J Affect Disord. (2017) 218:359–64. doi: 10.1016/j.jad.2017.05.001
194. Wypych, M, and Bilewicz, M. Psychological toll of hate speech: the role of acculturation stress in the effects of exposure to ethnic slurs on mental health among Ukrainian immigrants in Poland. Cult Divers Ethn Minor Psychol. (2022) 31. doi: 10.1037/cdp0000522
195. Ye, J, Wen, Y, Sun, X, Chu, X, Li, P, Cheng, B, et al. Socioeconomic deprivation index is associated with psychiatric disorders: an observational and genome-wide gene-by-environment interaction analysis in the UK biobank cohort. Biol Psychiatry. (2021) 89:888–95. doi: 10.1016/j.biopsych.2020.11.019
196. Zhou, S, King, EJ, Gjorgiovska, J, Mihajlov, A, and Stojanovski, K. Self-concealment, discrimination, and mental health in Macedonia: disparities experienced by sexual and gender minorities. Glob Public Health. (2019) 14:1075–86. doi: 10.1080/17441692.2018.1560484
198. World Health Organization (2013a). Comprehensive mental health action plan 2013-2030. Available at: https://www.who.int/publications/i/item/9789240031029
199. Durch, J. S., Bailey, L. A., and Stoto, M. A. Institute of Medicine (US) Committee on Using Performance Monitoring to Improve Community Health. Improving Health in the Community: A Role for Performance Monitoring. Eds. Durch JS, Bailey LA, Stoto MA, editors. (1997) Washington (DC): National Academies Press (US).
200. Peitz, D, Kersjes, C, Thom, J, Hoelling, H, and Mauz, E. Indicators for public mental health: a scoping review. Front Public Health. (2021) 9:714497. doi: 10.3389/FPUBH.2021.714497
201. World Health Organization (2001). International classification of functioning, disability and health World Health Organization Geneva ICF ii WHO library cataloguing-in-publication data international classification of functioning, disability and health: ICF.
202. Martins, AI, Queirós, A, Cerqueira, M, Rocha, N, and Teixeira, A. The international classification of functioning, disability and health as a conceptual model for the evaluation of environmental factors. Proced Comp Sci. (2012) 14:293–300. doi: 10.1016/j.procs.2012.10.033
203. World Health Organization (2013b). How to use the ICF: A practical manual for using the international classification of functioning, disability and health (ICF) exposure draft for comment. 1–122.
204. National Research Council (US). Institute of Medicine (US). U.S. Health in International Perspective: Shorter Lives, Poorer Health. Eds. Woolf SH, and Aron L. Washington (DC): National Academies Press (US) (2013).
205. Siordia, C, and Saenz, J. What is a “neighborhood”? Definition in studies about depressive symptoms in older persons. J Frailty Aging. (2013) 2:153. doi: 10.14283/jfa.2013.23
206. Cohen-Cline, H, Beresford, SAA, Barrington, W, Matsueda, R, Wakefield, J, and Duncan, GE. Associations between social capital and depression: a study of adult twins. Health Place. (2018) 50:162–7. doi: 10.1016/j.healthplace.2018.02.002
207. Wallace, S, Nazroo, J, and Bécares, L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. Am J Public Health. (2016) 106:1294. doi: 10.2105/AJPH.2016.303121
209. Evans, GW. The built environment and mental health. J Urban Health. (2003) 80:536–55. doi: 10.1093/jurban/jtg063
210. Brook, RD, Rajagopalan, S, Pope, CA, Brook, JR, Bhatnagar, A, Diez-Roux, AV, et al. Particulate matter air pollution and cardiovascular disease. Circulation. (2010) 121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1
211. Laumbach, RJ, and Kipen, HM. Respiratory health effects of air pollution: update on biomass smoke and traffic pollution. J Allergy Clin Immunol. (2012) 129:3–11. doi: 10.1016/j.jaci.2011.11.021
212. Mustafić, H, Jabre, P, Caussin, C, Murad, MH, Escolano, S, Tafflet, M, et al. Main air pollutants and myocardial infarction. JAMA. (2012) 307:713. doi: 10.1001/jama.2012.126
213. Tzivian, L. Outdoor air pollution and asthma in children. J Asthma. (2011) 48:470–81. doi: 10.3109/02770903.2011.570407
214. Halaris, A. Inflammation-associated co-morbidity between depression and cardiovascular disease. Curr Top Behav Neurosci. (2016) 31:45–70. doi: 10.1007/7854_2016_28
215. Hayley, S, Hakim, AM, and Albert, PR. Depression, dementia and immune dysregulation. Brain. (2021) 144:746–60. doi: 10.1093/brain/awaa405
216. Solmi, M, Radua, J, Olivola, M, Croce, E, Soardo, L, Salazar de Pablo, G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2022) 27:281–95. doi: 10.1038/s41380-021-01161-7
217. Correll, CU, Galling, B, Pawar, A, Krivko, A, Bonetto, C, Ruggeri, M, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, Meta-analysis, and Meta-regression. JAMA Psychiat. (2018) 75:555–65. doi: 10.1001/jamapsychiatry.2018.0623
218. Fusar-Poli, P, Correll, CU, Arango, C, Berk, M, Patel, V, and Ioannidis, JPA. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry. (2021) 20:200–21. doi: 10.1002/wps.20869
219. Kawachi, I, Colditz, GA, Ascherio, A, Rimm, EB, Giovannucci, E, Stampfer, MJ, et al. A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J Epidemiol Community Health. (1996) 50:245–51. doi: 10.1136/jech.50.3.245
220. Cosselman, KE, Navas-Acien, A, and Kaufman, JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. (2015) 12:627–42. doi: 10.1038/nrcardio.2015.152
221. Pearlstein, T, Howard, M, Salisbury, A, and Zlotnick, C. Postpartum depression. Am J Obstet Gynecol. (2009) 200:357. doi: 10.1016/j.ajog.2008.11.033
222. Charlson, F, Ali, S, Benmarhnia, T, Pearl, M, Massazza, A, Augustinavicius, J, et al. Climate change and mental health: a scoping review. Int J Environ Res Public Health. (2021) 18:4486. doi: 10.3390/ijerph18094486
Keywords: public mental health, community indicators, neighborhood, mental health promotion and prevention, scoping review
Citation: Schoenweger P, Kirschneck M, Biersack K, Di Meo A-F, Reindl-Spanner P, Prommegger B, Ditzen-Janotta C, Henningsen P, Krcmar H, Gensichen J and Jung-Sievers C (2023) Community indicators for mental health in Europe: a scoping review. Front. Public Health. 11:1188494. doi: 10.3389/fpubh.2023.1188494
Edited by:
Elisa Harumi Kozasa, Hospital Israelita Albert Einstein, BrazilReviewed by:
Ottar Ness, Norwegian University of Science and Technology, NorwayRachel Dale, University for Continuing Education Krems, Austria
Copyright © 2023 Schoenweger, Kirschneck, Biersack, Di Meo, Reindl-Spanner, Prommegger, Ditzen-Janotta, Henningsen, Krcmar, Gensichen and Jung-Sievers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Petra Schoenweger, cGV0cmEuc2Nob2Vud2VnZXJAaWJlLm1lZC51bmktbXVlbmNoZW4uZGU=
 Petra Schoenweger
Petra Schoenweger Michaela Kirschneck
Michaela Kirschneck Katharina Biersack
Katharina Biersack Anna-Francesca Di Meo1,2
Anna-Francesca Di Meo1,2 Philipp Reindl-Spanner
Philipp Reindl-Spanner Claudia Ditzen-Janotta
Claudia Ditzen-Janotta Peter Henningsen
Peter Henningsen Caroline Jung-Sievers
Caroline Jung-Sievers