- 1Xiyuan Hospital of China Academy of Chinese Medical Sciences, Beijing, China
- 2National Clinical Research Center for Cardiovascular Diseases of Traditional Chinese Medicine, Beijing, China
- 3Beijing University of Chinese Medicine, Beijing, China
Background: It remains controversial regarding the association between weight change and cardiovascular disease risk in older adults (aged ≥60 years). This study aimed to evaluate the association between weight change and the predicted 10-year atherosclerotic cardiovascular disease (ASCVD) risks in older adults.
Methods: This study used data from the National Health and Nutrition Examination Survey (NHANES). Older adults aged 60–79 years who were free of self-reported ASCVD at the time of the NHANES interview were included. Data were collected from January 1999 to December 2018 and analyzed in March 2022. We focused on the associations between weight change and the 10-year ASCVD risks with the percentage change in weight during short-term (1 year) and long-term (10 years), which categorized as moderate to high weight loss (≥10%), small weight loss (5.1–9.9%), stable weight (±5%), small weight gain (5.1–9.9%), and moderate to high weight gain (≥10%).
Results: The number of participants was 1,867 (mean age 67.49 years; 42.10% female) for the long-term interval (10 years) in our analysis, and 1894 for the short-term interval (1 years). We only observed an inverse association between long-term weight loss and the 10-year ASCVD risk in fully adjusted model (loss ≥ 10%: β = 2.52, 95%CI = 0.98, 4.05; loss 5.1% ~ 9.9%: β = 2.99, 95% CI = 1.30, 4.68), but all intervals of weight gain ≥5% were not significant associated with higher risk than stable weight. However, in the subgroup analyses, the association between long-term weight loss and the 10-year ASCVD risk was not significant in old-old (aged 75–79), obesity (BMI ≥ 35 kg/m2), intentional weight loss, moderate physical activity and diabetics.
Conclusion: Older adults (aged 60–79 years) with weight loss >5% over the past 10 years have excess predicted 10-year ASCVD risk. Our study supports the benefits of stable weight in promoting cardiovascular health in older adults.
1. Introduction
The increasing incidence of overweight and obesity among the aging population is a growing public health problem worldwide (1). Between 2007 and 2016, the proportion of obesity increased from 35.1 to 41.0% in older Americans, giving rise to a significant future burden on the U.S. healthcare systems (2). Substantial epidemiologic evidence indicates that excess body weight is associated with a higher risk of mortality, primarily due to atherosclerotic cardiovascular disease (ASCVD) (3, 4). It is not unexpected since obesity is clearly associated with most of the classical cardiovascular risk factors like hypertension, hyperlipidemia, and diabetes (5). However, whether losing weight could have a favor effect on decreasing cardiovascular events risk in older adults remains controversial.
Previous studies on the association between weight loss and long-term cardiovascular outcomes in older adults are limited. Although several studies have indicated that weight loss improved physical function and reduced frailty in obese older adults (6, 7). Increasing evidence suggested that weight loss was not uniformly associated with improved long-term survival (8). A meta-analysis reported that weight loss and weight gain were associated with a 59 and 10% increased risk of mortality respectively, suggesting an obesity paradox in older adults (9). In addition, the effect of weight loss among cardiovascular disease patients is also controversial (10). A meta-analysis of 35,335 patients (mean age 64 years) showed that, overall, weight loss was associated with a higher risk of cardiovascular events, but intentional weight loss was associated with improved outcomes (11). However, it remains unknown whether weight loss is associated with an increased risk of ASCVD events among older adults who are free of a prior heart attack or stroke. It is imperative to understand the health impact of long-term weight change on ASCVD risk in the general older population.
Therefore, the primary goal of this study was to examine the association between weight change and the 10-year predicted ASCVD risk in older U.S. adults (aged ≥60 years) using data from the 1999–2018 National Health and Nutrition Examination Survey (NHANES).
2. Methods
2.1. Database and study subjects
In this study, the data were obtained from the NHANES (1999–2018). This is an ongoing cross-sectional survey conducted by the National Center for Health Statistics (NCHS), designed to be representative of the U.S. non-institutionalized, civilian population. During a home interview, data are collected on demographic, socioeconomic, and health-related topics (including weight history). A separate examination collects standardized physical assessments and laboratory measurements. The survey obtained written informed consents from all participants prior to data collection. Methodological details about the NHANES are available at: www.cdc.gov/nchs/nhanes/.
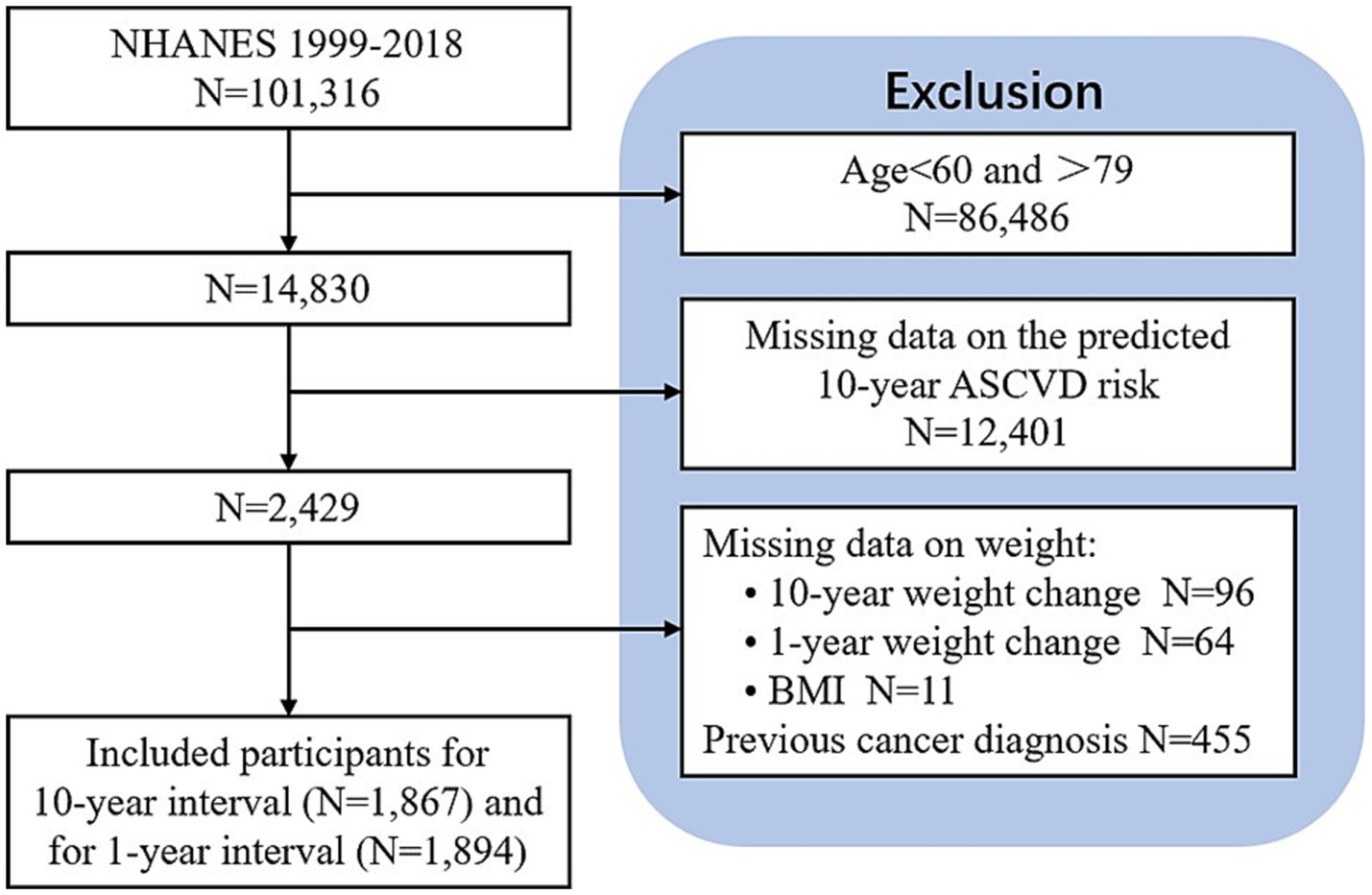
Older adults were defined as those of age 60 years and over (12). To estimate the 10-year ASCVD risk, the analytic sample was limited to 2,429 participants aged 60–79 years who were free of self-reported ASCVD at the beginning of the survey and met with high-density lipoprotein cholesterol (HDL-C) 20–100 mg/dL, total cholesterol (TC) 130–320 mg/dL, diastolic BP 30–140 mmHg and systolic BP 90–200 mmHg. After the exclusion of the participants with missing data on 10-year weight change (n = 96), 1-year weight change (n = 64) and BMI (n = 11), and those with a previous cancer diagnosis (n = 455), the number of participants included in the analysis was 1,867 for the long-term interval (10 years) and 1,894 for the short-term interval (1 years) (Figure 1).
2.2. Assessment of the predicted 10-year ASCVD risk
The primary outcome of this study was the 10-year ASCVD risk, defined as a first non-fatal myocardial infarction (MI), coronary heart disease (CHD) death, or fatal or non-fatal stroke over a 10-year period (13). According to the new pooled cohort equations (PCEs) introduced by the American College of Cardiology (ACC) and the American Heart Association (AHA) in 2013, the predictors used in estimating the 10-year risk of a first ASCVD event included age, sex, race, TC, HDL-C, treatment for hypertension, diabetes and current smoking status (13).
Data on age, sex, and race/ethnicity was obtained from the demographic questionnaire. The amount of TC (mg/dL) and HDL (mg/dL) was obtained from the laboratory file. Blood pressure was each calculated as the average of three readings. Participants self-reported currently smoking (yes, no), taking any blood pressure medications (yes, no), and had ever been told they had diabetes by a medical doctor (yes, no). Histories of diseases including CHD, MI, stroke, diabetes and cancer were ascertained through the question “Has a doctor or other health professional told you that you had diseases?”
2.3. Assessment of weight change
We used long-term (10 years) and short-term (1 year) weight change indicators according to the interval over which the change was assessed. The percentage change in weight was calculated from the difference between the present weight and the past weight, the specific formula was shown as followed:
where W refers to the present weight and W0 refers to their previous weight. All participants were asked to recall the weight 10 years ago or 1 year ago, and measured current weight in the NHANES examination. We classified the weight change into five categories: moderate-to-large weight loss (≥ 10%), small weight loss (5.1–9.9%), stable weight (± 5%), small weight gain (5.1–9.9%), and moderate-to-large weight gain (≥ 10%).
2.4. Assessment of covariates
The following covariates were included: age, sex, race, Body Mass Index (BMI), marital status, educational level, family income-to-poverty ratio, and physical activity. Marital status was categorized as married/partnered (married and living as married) and single/no partner (widowed, divorced, separated and never married). Educational level was classified as lower category (less than high school), intermediate category (high school graduate/GED, some college or AA degree) and higher category (college graduate or above). Physical activity was defined as sports, fitness and recreational activities, excluding work and transport activities. Physical activity was categorized as vigorous activity (cause large increases in breathing or heart rate), moderate activities (cause a small increase in breathing or heart rate) and none.
2.5. Statistical analysis
Categorical variables were expressed as frequency, and continuous variables were expressed as means ± standard deviations. Demographic and clinical data between the weight change groups were compared using the Kruskal-Wallis test and Fisher’s exact test. Multiple linear regression analyses were used to estimate the independent relationship between weight change and the predicted 10-year risk of ASCVD events. When calculating the relative ASCVD risk of each weight change category, we used the “stable weight” category as the reference. In addition to the relative 10-year ASCVD risk of each weight change category, we fit a smoothing spline curve to examine the non-linearity of weight change and the 10-year ASCVD risks. Moreover, we performed stratified analyses by age, sex, race/ethnicity, current BMI, intention to lose weight, physical activity, treatment for hypertension, diabetes and current smoking status.
Three models were constructed: Model 1 was adjusted for none; Model 2 was adjusted for sex, age, and race/ethnicity; Model 3 was adjusted for sex, age, race/ethnicity, body mass index, income-poverty ratio, physical activity, education level, and marital status. In the subgroup analysis, the model is not adjusted for the stratification variable itself.
We used multiple imputations, based on 5 replications and a chained equation approach method in the RMI procedure, to account for missing data. All statistical analyses were performed by using R version 3.4.3 (The R Foundation)1 and EmpowerStats software (X&Y solutions, Inc., Boston, MA)2 and Graphpad Prisma 8.3.0, with statistically significant set at p < 0.05.
3. Results
3.1. Characteristics
The description of sociodemographic and medical characteristics of the participants with long-term (10 years) weight change was presented in Table 1. A total of 1,867 older adults aged 60–79 years were enrolled in our analysis. Of all these participants, the mean age was 67.47 years (SD = 5.35), and 42.10% were female. For all participants, the mean predicted 10-year ASCVD risk was 23.21 (SD = 13.15). The mean BMI was 30.23 kg/m2 (SD = 6.21). The distribution of 10-year weight change was 27.05% for weight stable (± 5.0%), 13.87% for moderate-to-large weight loss (> − 10%), 10.18% for small weight loss (−5.1 to −9.9%), 13.93% for small weight gain (5.1~9.9%) and 34.98% for moderate-to-large weight gain (>10%). Among different groups of weight change, age, sex, race/ethnicity, BMI, income-poverty ratio, educational level, marital status, physical activity, smoker, diabetes, DBP, TC, and HDL were all significantly different (p < 0.05). Overall, older adults who had weight loss were more likely to be a racial/ethnic minority, single/no partner, and had lower income-to-poverty ratios and educational attainment, when compared to those with a stable weight. The descriptive statistics for the participants with short-term (1 year) weight change are shown in Supplementary material 1.

Table 1. Characteristics of study participants according to 10-year weight change patterns in National Health and Nutrition Examination survey, 1999–2018.
3.2. 10-year weight change and the predicted risk of ASCVD events
Results of multiple linear regression analyses of 10-year weight change and the 10-year risk of ASCVD events were displayed in Figure 2. Non-adjusted was displayed in Model 1 (Figure 2A), adjusted for age, sex, and race/ethnicity was displayed in Model 2 (Figure 2B), and adjusted for Model 2 plus BMI, income-poverty ratio, physical activity, education level, and marital status was displayed in Model 3 (Figure 2C). We observed a significant inverse association between weight change and the 10-year ASCVD risk.
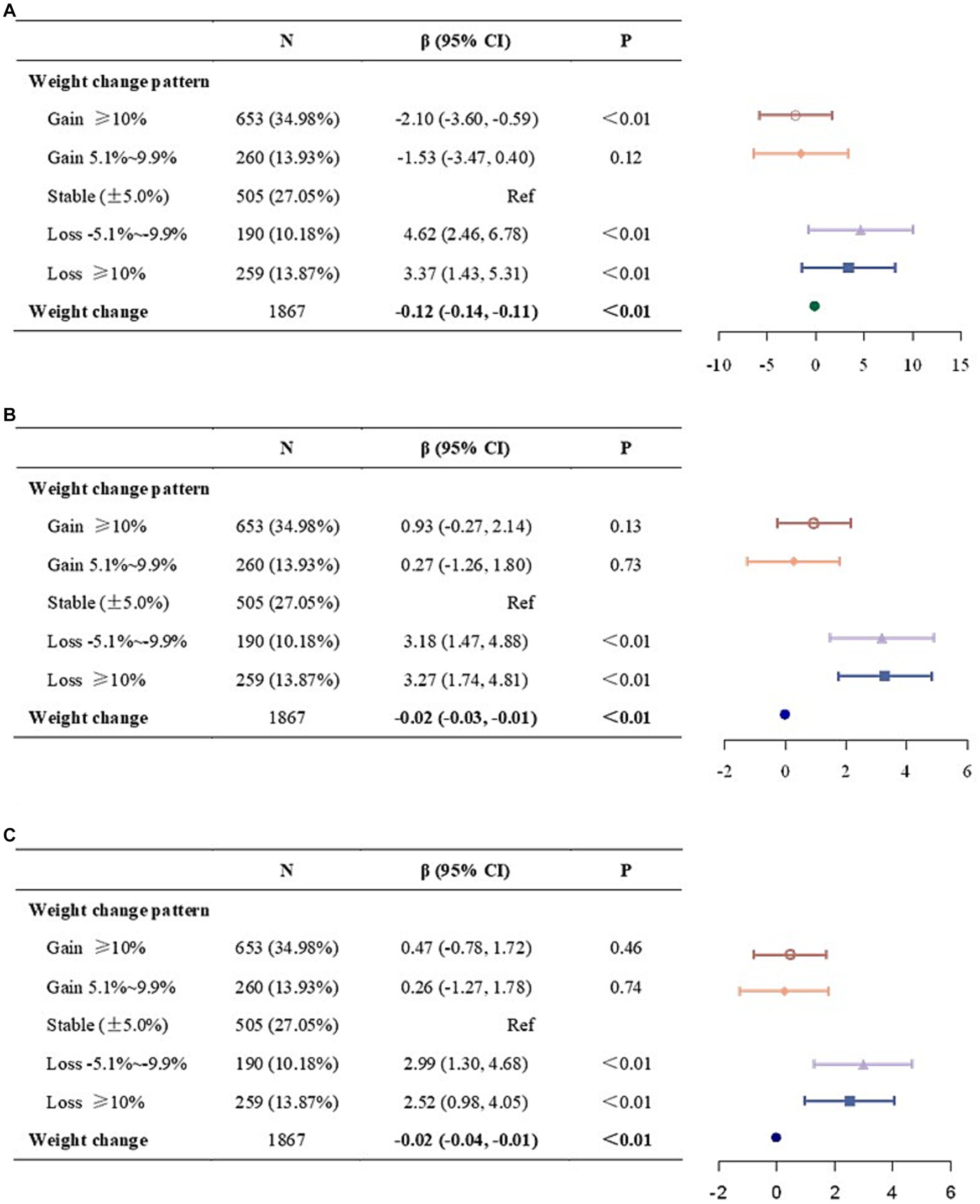
Figure 2. Association between 10-year weight change and the 10-year ASCVD risk. (A) Model 1, no covariates were adjusted. (B) Model 2, age, sex, and race/ethnicity were adjusted. (C) Model 3, age, sex, race/ethnicity, body mass index, income-poverty ratio, physical activity, education level, and marital status were adjusted. ASCVD, atherosclerotic cardiovascular disease; CI, confidence interval.
Similar results were found when weight change was divided into five categories. Compared to weight stable (± 5.0%), both moderate-to-large (≥ 10%) and small (−5.1% ~ −9.9%) weight loss was associated with a higher risk in Model 1 and Model 2. In fully adjusted model (Model 3), the significant association remained unchanged (loss≥10%: β = 2.52, 95%CI = 0.98, 4.05; loss 5.1% ~ 9.9%: β = 2.99, 95% CI = 1.30, 4.68). While neither Model 2 nor Model 3 found no significant association between the weight gain categories and the 10-year ASCVD risk, weight gain ≥10% was associated with lower risk in non-adjusted model (β = −2.10, 95% CI = −3.60, −0.59).
To check the dose–response relationship between continuous 10-year weight change (−9.9 to 9.9%) and the predicted 10-year risk of ASCVD events, we plotted the spline curves, as seen in Figure 3. This result confirmed the dose–response relationship was most pronounced in the link between weight loss and the 10-year ASCVD risk: greater weight loss was associated with higher 10-year ASCVD risk.
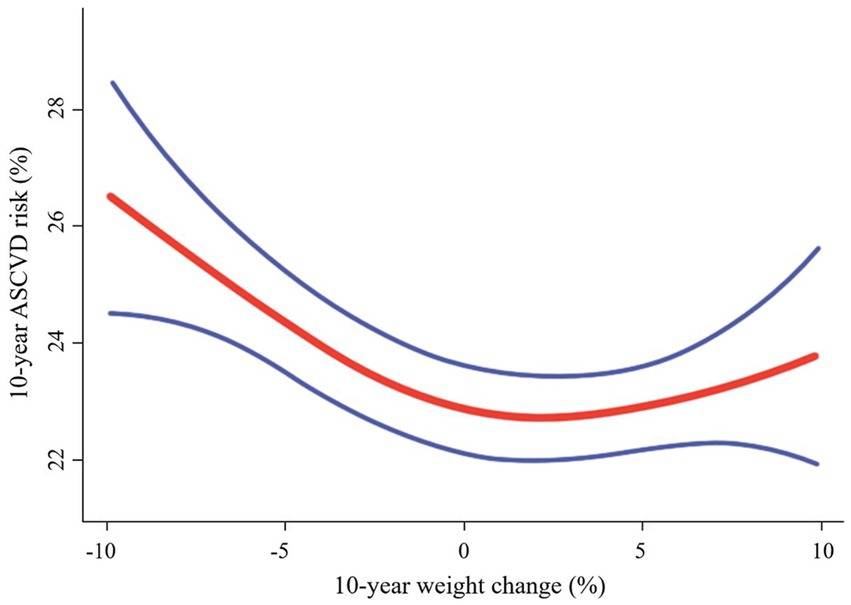
Figure 3. Correlation between 10-year weight change (−9.9 to 9.9%) and the 10-year ASCVD risk. Solid red line represents the smooth curve fit between variables. The area between two blue lined is expressed as a 95% CI. Age, sex, race/ethnicity, body mass index, income poverty ratio, physical activity, education level, and marital status were adjusted. ASCVD, atherosclerotic cardiovascular disease.
However, this was not the case for short-term weight change. Each category had no significant association with 10-year ASCVD risk, as seen in Supplementary material 2.
Table 2 presents the results stratified according to age, sex, race/ethnicity, BMI, physical activity, Intention to lose weight, treatment for hypertension, diabetes, and current smoking status. Compared to people with stable weight, it can be observed that people who lose weight may associate with a higher 10-year risk, no matter with ages (except for people aged ≥75 years) and sexes in Model 3. However, in the subgroup analyses, the association between weight loss and the 10-year ASCVD risk was non-significant in older adults who were obese (≥ 35 kg/m2), had intentional weight loss, and had moderate physical activity. In addition, moderate physical activity significantly decreases the 10-year ASCVD risk in older adults with moderate-to-large weight gain (β = −2.70, 95% CI = −4.97, −0.43). We also found that for diabetics, long-term weight change showed no significant association with the 10-year ASCVD risk. Subgroup analyses of short-term weight change and the 10-year ASCVD risk are presented in Supplementary material 3.
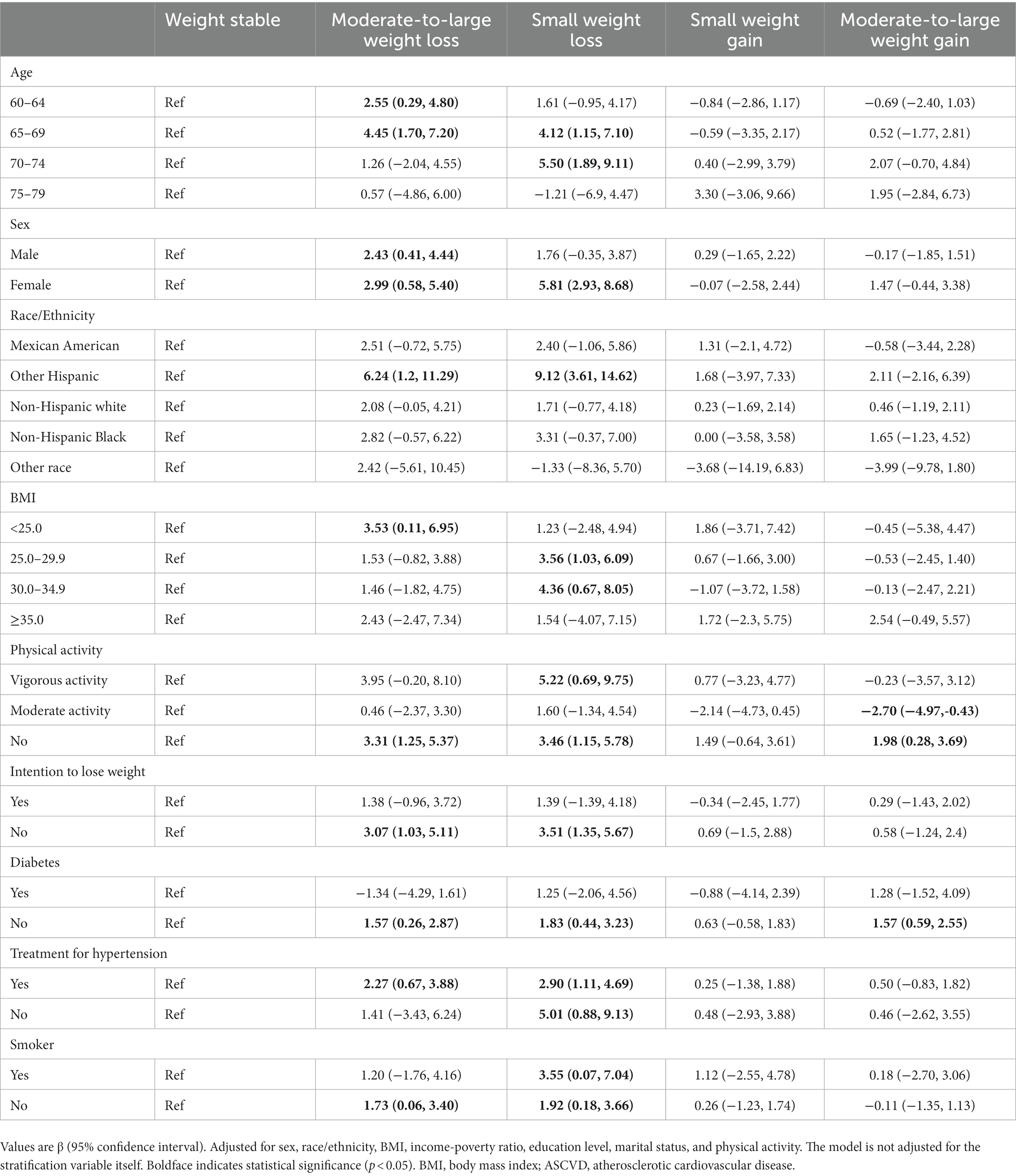
Table 2. Stratified analyses of the association between 10-year weight change and the 10-year ASCVD risk.
4. Discussion
The present study used a nationally representative sample of community-dwelling adults aged 60–79 years and assessed the risk of a first hard ASCVD event in the next 10 years according to the 2013 ACC/AHA equation. In this study, we found an inverse association between weight loss ≥5% and the predicted 10-year ASCVD risk in older adults, and no protective effect of weight gain.
Our results are generally in accordance with previous studies on the relationship between weight loss and cardiovascular and all-cause mortality in older adults. In a longitudinal observational cohort study conducted in the U.S. communities, weight loss of 5% or more in 3 years was associated with an increased risk of mortality in older adults (8). Likewise, community-dwelling older Japanese people with weight loss ≥5% in all terms was associated with a higher risk of all-cause mortality, not only in short-term (3 years), but also in medium-term (6–7 years) and long-term (12–13 years) (14). Moreover, a Tehran study of participants with type 2 diabetes aged ≥60 years without a history of cardiovascular disease and cancer at baseline has suggested that 3-year weight loss >5% was associated with an increased risk (marginally significant) of incident cardiovascular disease during more than 14 years of follow-up (15).
However, some previous studies reported conflicting results. For example, in a 12-month randomized controlled trial (RCT) of 164 obese older adults aged ≥65 years, there was a positive significant association between weight loss by exercise plus moderate caloric restriction and cardiometabolic risk (16). In addition, another RCT comprising 585 obese participants aged 60–80 years with hypertension found a favorable association between intentional weight loss (mean 4.4 kg) and reductions in the need for antihypertensive medication (17). This study also reported weight loss was not significantly associated with increased cardiovascular disease events during the first 2 years of follow-up (17), nor was all-cause mortality during over 12 years of follow-up (18).
In addition to the weight change calculated in different time intervals, the discrepancy between our study and previous ones may partly be related to current BMI and intention to lose weight. Indeed, our study indicated that the association between weight loss and the predicted 10-year risk was not significant in obesity (≥ 5 kg/m2) and intentional weight loss. This may be due to the fact that unintentional weight loss in older adults is usually reflect disease severity (e.g., in patients with advanced heart disease, lung disease or malignant disease) or underlying disease, and is particularly relevant to worsened outcomes (19). Cancer or malignancy, which is characterized by substantial weight loss during 1 year or less, accounts for 16–36% of organic causes of unintentional weight loss in older adults (20). However, our study showed that, an increased risk of a first ASCVD event was associated with weight loss within 10 years rather than 1 year. In addition, another possibility for discrepancy is the difference in the level of physical activity. The loss of muscle mass (21) and bone strength (22) that occurs with age, which contributes to disability and frailty in older adults (23, 24). Physical activity alone, without diet control, is not typically associated with significant weight loss and it can maintain lean body mass and muscle strength, improve cardiometabolic risk factors and physical function in older adults (7, 25, 26). However, because of the opposite effect observed in our study between vigorous and moderate intensity activity, further research is needed to clarify this issue.
A major strength of our study is the use of a nationally representative sample that represents the general U.S. adult population. Furthermore, with the comprehensive data collected in NHANES, a wide range of potential confounders including demographic, socioeconomic and lifestyle were able to be controlled.
As for the limitations. First, we used self-reported weight for the analysis, instead of measured weight, which may lead to the misclassification of weight change status. Secondly, we did not consider the fluctuation of body weight during the 10-year intervals. Third, weight lacks discriminatory power to differentiate between body fat and lean mass. Therefore, future research should investigate the same question using indicators of body composition to more fully understand the mechanisms linking weight changes to ASCVD risk to mortality risk. Fourthly, we failed to consider specific modalities of losing weight, such as intermittent fasting, low-calorie diets, more exercise or bariatric surgery, which might cause bias. Finally, this study was cross-sectional research, and it cannot demonstrate the causation but only the association. Further and prospective studies should be completed in the future.
5. Conclusion
In this study of U.S. adults 60–79 years of age, we found that weight loss >5% over 10 years was significantly associated with an increased the predicted 10-year ASCVD risk. Our study supports the benefits of stable weight in promoting cardiovascular health in older adults. However, further prospective studies are required to elucidate the effect of weight management in later life on decreasing ASCVD risk.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Ethics statement
The NHANES study was approved by the National Center for Health Statistics’ Ethics Review Board. The study was conducted in accordance with the local legislation and institutional requirements. All participants provided written informed consent (parental consent was obtained for those < 18 years).
Author contributions
YP: full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. YP and HL: concept and design. JL, FL, and WY: acquisition, analysis, and interpretation of data. LT, AL, and YW: drafting of the manuscript. YP and HQ: statistical analysis. LL and HQ: administrative, technical, and material support. CF: supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Center of China for Clinical Medical Research on Cardiovascular Diseases (No. CMC2022010).
Acknowledgments
We wish to thank National Center of China for Clinical Medical Research on Cardiovascular Diseases.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1183200/full#supplementary-material
Abbreviations
ASCVD, Atherosclerotic cardiovascular disease; NHANES, National Health and Nutrition Examination Survey; NCHS, National Center for Health Statistics; HDL-C, High-density lipoprotein cholesterol; TC, Total cholesterol; MI, Myocardial infarction; CHD, Coronary heart disease; PCEs, Pooled cohort equations; ACC, American College of Cardiology; AHA, American Heart Association; BMI, Body mass index; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; CI, Confidence interval; RCT, Randomized controlled trial.
Footnotes
References
1. Afshin, A , Forouzanfar, MH , Reitsma, MB , Sur, P , Estep, K , Lee, A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:13–27. doi: 10.1056/NEJMoa1614362
2. Hales, CM , Fryar, CD , Carroll, MD , Freedman, DS , and Ogden, CL . Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. (2018) 319:1723–5. doi: 10.1001/jama.2018.3060
3. Stevens, J , Cai, J , Pamuk, ER , Williamson, DF , Thun, MJ , and Wood, JL . The effect of age on the association between body-mass index and mortality. N Engl J Med. (1998) 338:1–7. doi: 10.1056/NEJM199801013380101
4. Angelantonio, E , Bhupathiraju, S , Wormser, D , Gao, P , Kaptoge, S , de Gonzalez, AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. (2016) 388:776–86. doi: 10.1016/S0140-6736(16)30175-1
5. Jensen, MD , Ryan, DH , Apovian, CM , Ard, JD , Comuzzie, AG , Donato, KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Obesity Society. Circulation. (2014) 129:S102–38. doi: 10.1161/01.cir.0000437739.71477.ee
6. Villareal, DT , Aguirre, L , Gurney, AB , Waters, DL , Sinacore, DR , Colombo, E, et al. Aerobic or resistance exercise, or both, in dieting obese older adults. N Engl J Med. (2017) 376:1943–55. doi: 10.1056/NEJMoa1616338
7. Batsis, JA , Gill, LE , Masutani, RK , Adachi-Mejia, AM , Blunt, HB , Bagley, PJ, et al. Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since 2005. J Am Geriatr Soc. (2017) 65:257–68. doi: 10.1111/jgs.14514
8. Newman, AB , Yanez, D , Harris, T , Duxbury, A , Enright, PL , Fried, LP, et al. Weight change in old age and its association with mortality. J Am Geriatr Soc. (2001) 49:1309–18. doi: 10.1046/j.1532-5415.2001.49258.x
9. Alharbi, TA , Paudel, S , Gasevic, D , Ryan, J , Freak-Poli, R , and Owen, AJ . The association of weight change and all-cause mortality in older adults: a systematic review and meta-analysis. Age Ageing. (2021) 50:697–704. doi: 10.1093/ageing/afaa231
10. Romero-Corral, A , Montori, VM , Somers, VK , Korinek, J , Thomas, RJ , Allison, TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. (2006) 368:666–78. doi: 10.1016/S0140-6736(06)69251-9
11. Pack, QR , Rodriguez-Escudero, JP , Thomas, RJ , Ades, PA , West, CP , Somers, VK, et al. The prognostic importance of weight loss in coronary artery disease: a systematic review and meta-analysis. Mayo Clin Proc. (2014) 89:1368–77. doi: 10.1016/j.mayocp.2014.04.033
12. World Health Organization . Technical advisory group for measurement, monitoring and evaluation of the UN decade of healthy ageing. Available at: https://www.who.int/groups/technical-advisory-group-for-measurement-monitoring-and-evaluation-of-the-un-decade-of-healthy-ageing (2022).
13. Goff, DCJ , Lloyd-Jones, DM , Bennett, G , Coady, S , D’Agostino, RB , Gibbons, R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. (2014) 129:S49–73. doi: 10.1161/01.cir.0000437741.48606.98
14. Murayama, H , Liang, J , Shaw, BA , Botoseneanu, A , Kobayashi, E , Fukaya, T, et al. Short-, medium-, and long-term weight changes and all-cause mortality in old age: findings from the National Survey of the Japanese elderly. J Gerontol A Biol Sci Med Sci. (2021) 76:2039–46. doi: 10.1093/gerona/glab052
15. Moazzeni, SS , Hizomi Arani, R , Deravi, N , Hasheminia, M , Khalili, D , Azizi, F, et al. Weight change and risk of cardiovascular disease among adults with type 2 diabetes: more than 14 years of follow-up in the Tehran lipid and glucose study. Cardiovasc Diabetol. (2021) 20:141. doi: 10.1186/s12933-021-01326-2
16. Ard, JD , Gower, B , Hunter, G , Ritchie, CS , Roth, DL , Goss, A, et al. Effects of calorie restriction in obese older adults: the CROSSROADS randomized controlled trial. J Gerontol A Biol Sci Med Sci. (2017) 73:glw237–80. doi: 10.1093/gerona/glw237
17. Whelton, PK , Appel, LJ , Espeland, MA , Applegate, WB , Ettinger, WHJ , Kostis, JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. (1998) 279:839–46. doi: 10.1001/jama.279.11.839
18. Brown, RE , and Kuk, JL . Consequences of obesity and weight loss: a devil's advocate position. Obes Rev. (2015) 16:77–87. doi: 10.1111/obr.12232
19. Alibhai, SM , Greenwood, C , and Payette, H . An approach to the management of unintentional weight loss in elderly people. CMAJ. (2005) 172:773–80. doi: 10.1503/cmaj.1031527
20. McMinn, J , Steel, C , and Bowman, A . Investigation and management of unintentional weight loss in older adults. BMJ. (2011) 342:d1732. doi: 10.1136/bmj.d1732
21. Newman, AB , Lee, JS , Visser, M , Goodpaster, BH , Kritchevsky, SB , Tylavsky, FA, et al. Weight change and the conservation of lean mass in old age: the health, aging and body composition study. Am J Clin Nutr. (2005) 82:872–8. doi: 10.1093/ajcn/82.4.872
22. Ensrud, KE , Vo, TN , Burghardt, AJ , Schousboe, JT , Cauley, JA , Taylor, BC, et al. Weight loss in men in late life and bone strength and microarchitecture: a prospective study. Osteoporos Int. (2018) 29:1549–58. doi: 10.1007/s00198-018-4489-6
23. Gill, LE , Bartels, SJ , and Batsis, JA . Weight Management in Older Adults. Curr Obes Rep. (2015) 4:379–88. doi: 10.1007/s13679-015-0161-z
24. Grabowski, DC , and Ellis, JE . High body mass index does not predict mortality in older people: analysis of the longitudinal study of aging. J Am Geriatr Soc. (2001) 49:968–79. doi: 10.1046/j.1532-5415.2001.49189.x
25. Brennan, AM , Standley, RA , Anthony, SJ , Grench, KE , Helbling, NL , DeLany, JP, et al. Weight loss and exercise differentially affect insulin sensitivity, body composition, cardiorespiratory fitness, and muscle strength in older adults with obesity: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. (2022) 77:1088–97. doi: 10.1093/gerona/glab240
Keywords: weight change, cardiovascular disease, NHANES, 10-year ASCVD risk, older adults
Citation: Peng Y, Li H, Liao F, Lu J, Yang W, Tan L, Lu A, Wei Y, Long L, Qu H and Fu C (2023) Association between weight change and the predicted 10-year risk for atherosclerosis cardiovascular disease among U.S. older adults: data from National Health and Nutrition Examination Survey 1999–2018. Front. Public Health. 11:1183200. doi: 10.3389/fpubh.2023.1183200
Edited by:
Basil Nwaneri Okeahialam, University of Jos, NigeriaReviewed by:
Anil Sirisena, Jos University Teaching Hospital, NigeriaKumar Ashish, CarolinaEast Medical Center, United States
Copyright © 2023 Peng, Li, Liao, Lu, Yang, Tan, Lu, Wei, Long, Qu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linzi Long, cWl4aWFuZzgzMDgwM0AxNjMuY29t; Hua Qu, aHVhX3F1QHllYWgubmV0; Changgeng Fu, ZnVjZ2JzQDE2My5jb20=
†These authors have contributed equally to this work
 Yuxuan Peng
Yuxuan Peng Hongzheng Li
Hongzheng Li Feifei Liao
Feifei Liao Jieming Lu1,2,3
Jieming Lu1,2,3 Wenwen Yang
Wenwen Yang Ling Tan
Ling Tan Linzi Long
Linzi Long Hua Qu
Hua Qu Changgeng Fu
Changgeng Fu