- 1Cicely Saunders Institute of Palliative Care, Policy, and Rehabilitation, King's College London, London, United Kingdom
- 2GKT School of Medical Education, King's College London, London, United Kingdom
- 3Wellcome Centre for Cultures and Environments of Health, University of Exeter, Exeter, United Kingdom
- 4Department of Health and Community Sciences, University of Exeter Medical School, Exeter, United Kingdom
- 5St Christopher's Hospice, London, United Kingdom
- 6End-of-Life Care Research Group, Vrije Universiteit Brussel, Brussels, Belgium
- 7Marie Curie Palliative Care Research Group, University College London, London, United Kingdom
Background: Public health palliative care views communities as an integral part of care delivery at the end of life. This community-provider partnership approach has the potential to improve end-of-life care for people who are dying and their carers.
Objective: To identify and appraise the current literature related to public health interventions that enable communities to support people who are dying and their carers.
Methods: A scoping review was conducted, applying Arksey and O'Malley's methods. Data was extracted and synthesized using narrative techniques, and results are reported using PRISMA guidelines.
Results: The search yielded 2,902 results. Eighteen met inclusion criteria and were included in the analysis. Interventions were categorized according to their target population: people with life-limiting illness (ex. facilitated social interaction, helplines and guided discussions about death and dying); carers (ex. social support mapping, psychoeducation, and community resource identification and facilitation); or dyads (ex. reminiscence activities, practical and emotional support from volunteers, online modules to bolster coping mechanisms). Public health palliative care approaches were delivered by key community stakeholders such as community health workers, volunteers, peer mentors, and pre-established support groups. Despite reported challenges in identifying appropriate tools to measure effectiveness, studies report improvement in quality of life, loneliness, social support, stress and self-efficacy.
Conclusion: We found that community-engaged palliative care interventions can lead to appreciable changes in various outcomes, though it was difficult to determine in which contexts this approach works best because of the dearth of contextual information reported. Based on the varied design and implementation strategies, it is clear that no one method for enhancing end of life care will benefit all communities and it is crucial to engage community members at all stages of the design and implementation process. Future research should be grounded in appropriate theory, describe contextual differences in these communities, and should specifically examine how demographics, resource availability, and social capital might impact the design, implementation, and results of public health palliative care interventions.
What is already known about this topic?
• Public health palliative care is a model of care that views communities as an integral part of care delivery at the end-of-life.
• Some people, like those in rural and coastal communities, people bound to their homes due to disability or transportation limitations, and those from historically underserved populations, might have palliative care needs that are difficult to meet with traditional services.
• Models of palliative care that include public health interventions have the potential to better serve the needs of groups that traditional services are unable to effectively meet.
What does this paper add?
• Though varied in targeted need and approach, each included intervention improved at least one aspect of care for people at the end of life and/or and their carers, demonstrating the utility of a public health palliative care approach in different settings. Despite this, few studies discussed the possible mechanisms of action leading to improved outcomes.
• There was marked heterogeneity in the studies' theoretical underpinnings, methods and outcomes of interest which emphasizes the diversity of the public health palliative care approach and how contextual factors such as demographics, resource availability and social capital likely impact success.
• This review demonstrates the wide number of actors beyond professional services who are involved in end-of-life care, including paid community members, trained volunteers, and peer support mentors.
• Contextual data was not reported consistently among included studies thus limiting our ability to make inferences about which types of approaches work for different communities and why.
Introduction
Palliative care is recognized by the World Health Organization as an essential health service under Universal Health Coverage (1, 2). However, globally only about 14% of people who would benefit from palliative care actually receive it (3). An estimated 56.8 million people around the world require palliative care each year, the majority of whom live in low- and middle-income countries (3). The need to correct the inequitable distribution of end-of-life care services is also evident in high-income countries, where lower socioeconomic position is associated with poorer outcomes in end-of-life care (4, 5). A more integrated approach between healthcare providers and the communities they serve is vital to bridge the gap between demand and supply (6).
Public health palliative care views communities as an integral part of care delivery at the end-of-life (7). The public health palliative care approach is informed by the five pillars for health promotion in the Ottawa Charter (8). It emphasizes the importance of health-centric public policy, supportive environments, community action, personal skill development, and health and social care services reoriented toward health promotion in order to improve the physical, mental, and social well-being of populations, including the context of life-limiting illness. This community-engaged approach has the potential to expand capacity and better serve groups such as rural and coastal communities, people living in economic poverty, people with disability or transportation limitations, and those with limited access to high-quality healthcare services (6). Furthermore, the COVID-19 pandemic shifted care into the home, accelerating new models of care delivery to meet needs beyond resource-limited health and social care institutions (9).
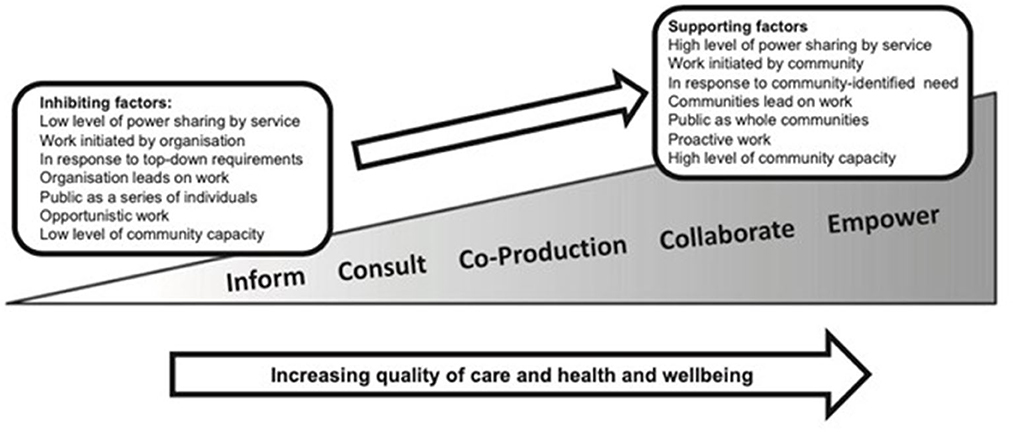
The level of community engagement in supporting the dying falls along a continuum ranging from information provision to consulting, co-producing, collaborating and finally empowerment (where communities lead the work) (10). The public health approach to palliative and end-of-life care ideally involves the input from members of the target community at every stage of design, implementation, and dissemination, thereby ensuring that services are relevant, people feel empowered and supported, with sustainable change. This ecological view of health acknowledges that traditional models of healthcare have limitations, and recognizes that community input is not only valuable, but essential in meeting health needs.
Previous large scale public health initiatives like the Neighborhood Network in Palliative Care in Kerala, India, and Compassionate Communities and Cities have demonstrated that a public health approach can increase the depth and breadth of a palliative and end-of-life care response for those who need it most (11, 12). Working in active partnership with key community stakeholders enables development of community driven support for people with palliative care needs within their networks and neighborhoods (13, 14). The identification and harnessing of community-specific assets with recognition of shared concerns may better reflect and serve the needs and wishes of ethnically and socially diverse populations than traditional service responses alone (10).
All along the spectrum of community engagement, public health palliative care approaches have been found to improve outcomes for both people with life-limiting illness and their carers, including improving quality of life (QoL), reducing fatigue and isolation, and increasing the size of caring networks (6). However, delivery of feasible, acceptable and effective public health palliative care programmes requires greater understanding of what might work, for whom and how, within differing social contexts, and application of robust methods to understand mechanisms and evaluate outcomes (15). This review aimed to identify and appraise the current literature related to public health interventions that enable communities to support people who are dying and their caregivers.
Methods
Design and research questions
A scoping review was undertaken in line with Arksey and O'Malley's methods (16); results were synthesized using narrative synthesis applying a public health palliative care framework (6). The search and screening results are reported according to the PRISMA guidelines.
The review sought to answer the following a priori research questions: (1) What are community needs to support those living with terminal illness? (2) What interventions have been developed and what are the theoretical models that underpin them? (3) What is the evidence for effectiveness? (4) What context-specific evidence is available for communities living with economic poverty? (5) What are the mechanisms of action? (6) What research methods are most appropriate to improve support in palliative care? (7) Which process and outcome measures are appropriate to evaluate the impact of these approaches?
The analysis was guided by Sallnow and colleagues' public health palliative care framework (6). In their 2016 systematic review (informed by the tenets of the Ottawa Charter), they explored current evidence at the cross-section of palliative care and public health, specifically seeking interventions in the Charter's community action pillar. For this review, we expanded our conceptualization of public health palliative care approaches to include the personal skill development pillar of the Ottawa Charter as well as community action, acknowledging the overlap that exists in practice. Therefore, we included interventions such as educational materials which had been created specifically for people at the end of life and/or their carers (provided that the materials had been created by or with input from community stakeholders). In their review, Sallnow and colleagues identified and described three main domains which the interventions targeted: “Making a practical difference, which describes the impact such work has on the immediate experiences of those facing the end of life and their carers; Individual learning and growth, which describes the journey of personal reflection, development and confidence that those involved in delivering the care embark on; and, Developing community capacity which refers to the impact of the work beyond the individuals involved, to the wider community where sustainable change can occur.” Based on this framework, we sought to assess the methods used in interventions to support the dying and their carers, understand their theoretical underpinnings, and begin to define the mechanism of action which could lead to an improvement in access to and quality of care.
Search strategy
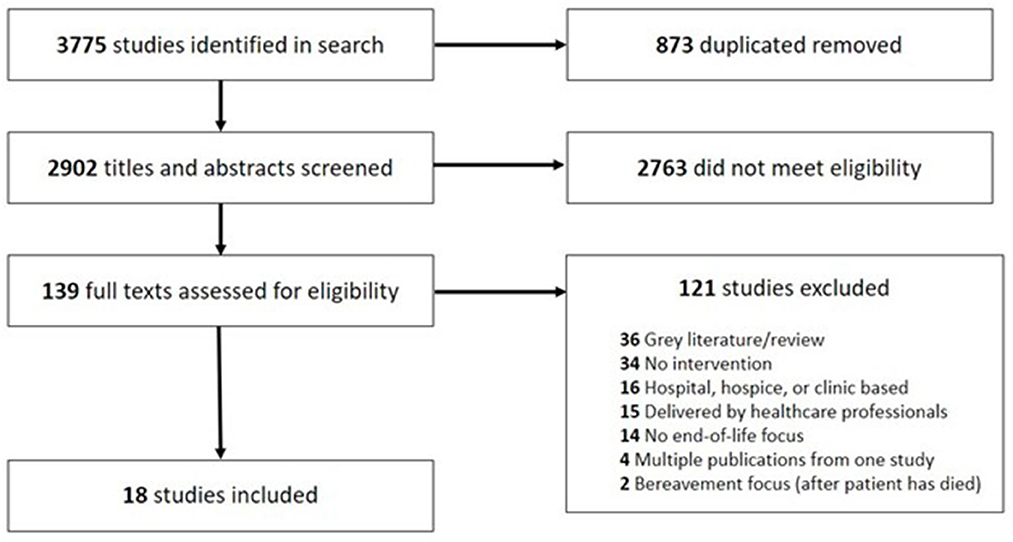
The search strategy is reported in Appendix 1. It was undertaken in September 2022, using the following databases: Medline, Embase, PsycInfo, Cumulative Index to Nursing and Allied Health Literature and Nursing and Allied Health Database. Additionally, we searched similar systematic reviews and publications about community engagement in palliative care for studies we might have missed in the database search. Identified publications were uploaded into Covidence and each assessed for relevance by at least two reviewers (AP, LW, AD, MI, MB). Discrepancies were discussed in weekly team meetings and resolved by consensus. Inclusion criteria were: (1) reporting the results of a public health palliative care intervention targeting the community action or personal skills domain of the Ottawa Charter, (2) the intervention aimed to directly improve the care of adults aged 18 or older at the end of life [within 1 year of dying (17)] and/or their carers, (3) outcomes focused on people at the end of life or their carers, (4) written in English language. Exclusion criteria were: (1) the intervention delivered in a healthcare setting (e.g., hospitals, hospices, skilled nursing facilities) or by healthcare professionals alone, (2) intervention was created with no community input or engagement, (3) outcomes that directly impact people at the end of life or their carers were not evaluated, (4) the intervention was aimed at bereaved individuals only, (5) the publication was a review or meta-analysis of existing literature, (6) full text was not available, or the publication was not peer reviewed (e.g., conference abstracts, gray literature). The full search and screening results are reported in a PRISMA flowchart (Figure 2).
Data extraction and analysis
In line with Arksey and O'Malley's methods (16), the study team extracted data on key aspects of the included studies' settings, designs, theoretical underpinnings, methods, outcome measures and results to address the review's research questions. We used narrative synthesis guided by Sallnow et al.'s public health palliative care framework to identify types of interventions that address the three domains of community-engaged end-of-life care (practical needs, personal growth, and community capacity), to assess the breadth of research on the topic, and to analyse similarities and differences between studies (6). Additionally, we mapped the level of community engagement involved in each of the studies based on Sallnow and Paul's spectrum of engagement in end-of-life care, seen in Figure 1 (10). We report relevant information from the selected publications according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (18).
Results
Search strategy
The search yielded 2,900 unique results, and two additional studies were identified from reference lists of other similar reviews and from expert consultation. Of those, 2,763 did not meet the eligibility criteria based on title and abstract screening. Subsequently, 139 full text articles were reviewed, and a further 121 did not meet the criteria for inclusion. In total, 18 studies were retained for analysis (see PRISMA flowchart in Figure 2).
Study characteristics
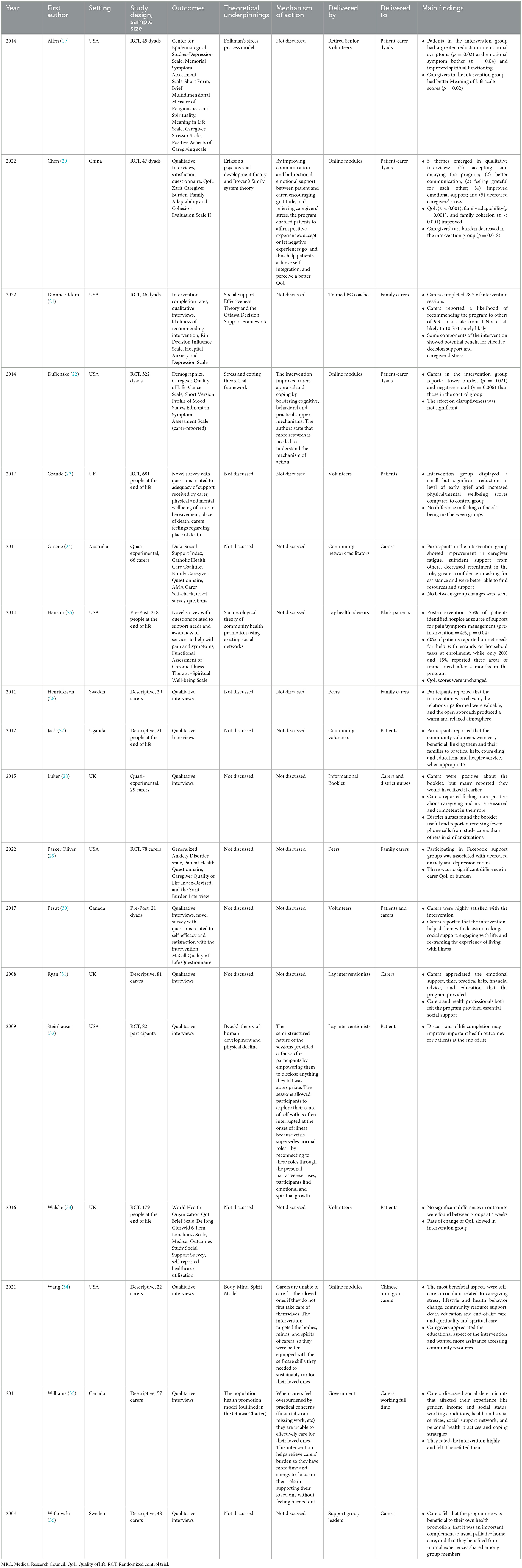
Study summaries are presented in Table 1. Nine studies were conducted in North America, 6 in Europe, 1 in Africa, 1 in Australia and 1 in Asia. Most (n = 12) were conducted in large metropolitan areas focusing mainly on urban communities. The majority of these community-based interventions targeted carers of patients with life limiting illness (n = 10), three to people at the end-of-life only, and five to dyads. In total, 1,641 patients and 867 carers participated in these intervention studies. In seven of the studies paid community members hired by the research team delivered the intervention, in six volunteers, and in a further five no person delivered the intervention. In the studies with no specified person delivering the intervention, educational materials (i.e., informational booklet, online modules, etc.) were created based on input from community stakeholders and were freely available for community members to utilize as needed. Most of the 18 retained studies were evaluated using randomized control trials (n = 8), six qualitative only, two quasi-experimental, and two pre-post designs.
In terms of reported contextual factors and demographic data, most studies (n = 16) reported age and sex of the participants. Nine reported marital status, six reported race and/or ethnicity, five highest level of education, four employment status, three living arrangements, two language proficiency, two religious affiliation, and one time since immigration. Two studies listed no demographic information about the participants. Four studies briefly described the catchment area for recruitment in terms of rurality and healthcare services available.
Included studies fell along the spectrum of community engagement seen in Figure 1 (10), from low levels of consultative engagement [educational materials that were created with community input then passively made available to those who might need it (20, 28)] to relatively high levels of collaborative engagement [researchers created training programs aimed at equipping volunteers with the skills they need to asses needs and then provide tailored support for people at the end of life and their carers (27, 30)]. No studies fell into the extremes of the spectrum, partly because we excluded studies that only informed participants without community engagement at any point in the intervention development.
Interventions focused on people at the end of life
Three of the 18 included studies reported the results of interventions explicitly aimed at supporting people who were dying (25, 32, 33). All aimed to address people's practical needs by providing psychological and social support from trained community volunteers. One targeted personal growth (32) and one addressed community capacity (25). Each approach lasted between 3 weeks and 2 months and were all held in-person. Descriptions of each of the studies and their main components are reported in Table 2. None of the three studies used the same outcome measures.
Hanson et al. developed a peer support group to help meet the practical, emotional and spiritual needs of African Americans with advanced cancer based on the socioecological theory of community health promotion using existing social networks. They measured outcomes using a novel survey of support needs and awareness of services to help with symptoms and the Functional Assessment of Chronic Illness Therapy–Spiritual Well-being Scale. After 2 months people reported less need for practical, emotional, and spiritual support, were more aware of hospice care but had no change in QoL (25). Informed by Byock's theory of human development and physical decline, Steinhauser et al. performed a three-armed RCT comparing a life completion discussion intervention with previously validated relaxation exercises or control. The results form a synopsis of what participants discussed in the three sessions but do not compare the groups in the discussion (32). This was the only study to discuss possible mechanisms of action, and they postulated that their intervention allowed people at the end of life to explore their sense of self and reconnect with their roles outside of illness, thus facilitating personal and spiritual growth. Walshe et al.'s study randomized 196 adults with a terminal diagnosis to receive a volunteer support intervention immediately or after a 4 week wait. They collected the World Health Organization QoL Brief Scale, De Jong Gierveld 6-item Loneliness Scale, Medical Outcomes Study Social Support Survey, and self-reported healthcare utilization from participants. While the intervention produced a positive shift in QoL, loneliness, and perceived social support scores these were not statistically significant (33).
To summarize, two of the three studies used quantitative methods to assess outcomes for people at the end of life [one used a novel survey (25) while the other used validated tools (33)]. One showed improvement in people's needs being met post-intervention (25), but neither showed a statistically significant increase in QoL. One study used qualitative interviews to determine patient satisfaction with the intervention (32). Patients in this study found the interviews to be beneficial in reflecting on their lives and accepting death which the authors stated may have improved their QoL.
Carer-facing interventions
Ten studies focused solely on carers' needs as the person they cared for approached the end-of-life (21, 23, 24, 26, 28, 29, 31, 34–36). Four approaches connected individual carers with trained community members employed by the research team (21, 23, 24, 31) while three joined multiple carers together to form small support groups (26, 29, 36). Three did not utilize interventionists and instead provided standardized support (online modules, information booklet, and government provided financial assistance) aimed at improving carers QoL and self-efficacy (28, 34, 35). All standardized support approaches were informed by community stakeholders and were freely available to community members to use as needed. Interventions lasted between one and 12 weeks and were implemented in a variety of formats, including in-person, online, and hybrid. To assess carer outcomes six studies used qualitative interviews (26, 28, 31, 34–36), two used quantitative methods [two validated tools (24, 29) and one a novel survey (23)], and one used mixed-methods (21). The studies that used validated tools chose the Rini Decision Influence Scale, Hospital Anxiety and Depression Scale, Duke Social Support Index, Catholic Health Care Coalition Family Caregiver Questionnaire, American Medical Association Carer Self-check.
Three of the 10 described the theories that underpinned them, including the Social Support Effectiveness Theory and the Ottawa Decision Support Framework (21), the Body-Mind-Spirit Model (34), and the population health promotion model (35). Two studies discussed possible mechanisms of action leading to improved outcomes. One cited improving physical and emotional well-being of carers allowing them to be better equipped to sustainably care for their loved one (34), and the other postulated that their intervention relieved the burden of practical concerns (financial strain, missing work, etc.,) thereby allowing more time and emotional energy for caring (35, 37). None of the studies that did not state a theoretical framework posited a mechanism of action.
All 10 interventions addressed at least one aspect of carers' practical needs, from psychological support and education about how to care for someone seriously ill or dying, to financial assistance. Six highlighted the importance of personal growth and encouraged participants to reflect on their experience and their own perceptions of death and dying (21, 23, 24, 26, 28, 29, 34). Five involved community capacity building, often in the form of peer support groups that could continue to meet after the person had died (26, 28, 29, 34, 36). None specifically focused on training community volunteers or activists to continue the program after the intervention study was complete.
As seen in Table 1, there was little overlap in the measures used to assess outcomes, so opportunities for comparison are limited. In all seven of the studies that employed qualitative interviews, carers were satisfied with the intervention and felt it substantially benefitted them. In the studies that used quantitative methods, researchers found that carers were likely to recommend the intervention (21), felt improved mental and physical well-being (21, 23, 29), had decreased anxiety and depression (21, 29), and decreased early grief after the patient had died (23).
Dyadic interventions
Five of the 18 included studies focused on patient-carer dyads (19, 20, 22, 27, 30). The dyadic interventions reported the highest level of community engagement in the development of the intervention and were the most comprehensive in addressing all three domains of the guiding framework. All five touched on at least one aspect within each of the three domains. All paid specific attention to the psychological needs of people at the end of life and their carers, aimed to improve knowledge about and acceptance of dying, and made efforts to embed sustainable change into community networks by bolstering volunteers and resources available to people facing the end of life and their carers. The duration range for dyadic interventions was wide, between 3 weeks and 1 year, and they were delivered in-person, over the phone, online or through apps designed with community input or moderated by community members.
Three of the five stated the theoretical framework that informed the study, including Folkman's stress process model (19), Erikson's psychosocial development theory and Bowen's family system theory (20), and the Stress and coping theoretical framework (22). Two discussed possible mechanisms of action (20, 22). One cited communication and bidirectional emotional support improvements as the key components of improved QoL (20), while the other asserted that the intervention helped improve carers' cognitive, behavioral and practical support mechanisms, thus improving their ability to cope with stressors (22).
Two of the studies evaluated outcomes using quantitative measures only (19, 22), two using mixed methods (20, 30), and one using qualitative methods only (27). There was almost no overlap in outcome measures. Those that used validated measures chose the Center for Epidemiological Studies-Depression Scale, the Memorial Symptom Assessment Scale-Short Form, the Brief Multidimensional Measure of Religiousness and Spirituality, the Meaning in Life Scale, the Caregiver Stressor Scale, the Positive Aspects of Caregiving scale, the Zarit Caregiver Burden scale, the Family Adaptability and Cohesion Evaluation Scale II, the Caregiver Quality of Life–Cancer Scale, the Short Version Profile of Mood States, the Edmonton Symptom Assessment Scale, and the McGill Quality of Life Questionnaire. All four studies using quantitative measures reported statistically significant positive outcomes for both patients and carers. Allen and colleagues reported decreased emotional symptoms and increased spiritual functioning (19). Chen and colleagues reported high satisfaction from both people at the end of life and carers and increased QoL and family cohesion (20). DuBenske and colleagues reported lower caregiving burden and negative mood in the intervention group compared with the control group (22). Finally, Pesut and colleagues reported increased confidence in decision making and perception of social support (30). The studies using qualitative methods similarly all reported positive experiences with the intervention and experiential reports of improved communication, psychosocial functioning and acceptance of death and dying (20, 27, 30).
Discussion
The purpose of this scoping review was to identify and appraise the current literature on public health palliative care interventions aimed at engaging community members in supporting people at the end of life and their carers. The interventions, their theoretical underpinnings, mechanisms of action, measurement strategies and results were heterogeneous. This emphasizes the wide range of interventions that comprise the public health palliative care approach and the importance of co-creating end-of-life care delivery strategies through community action and engagement to fit different contexts. Importantly, most successfully improved at least one aspect of care for people with life limiting illness and their carers, demonstrating the utility of this philosophy of care. This is supportive of the broader literature, which acknowledges the positive impact of engaging communities to improve health and well-being (6, 11, 38).
In terms of supporting people at the end of life and their carers, communities have wide ranging needs that are dependent on context, demographics, and social capital. These needs can be divided into the three distinct categories outlined in the guiding framework: practical needs, personal growth and community capacity (6). Support for practical needs, such as social interaction, symptom management, shopping and financial subsidies, were employed in all studies. For example, most included interventions involved social interaction with trained volunteers or peers in a similar situation and reported benefits for both people at the end of life and their carers. Six studies directed resources to bolstering social networks, while six provided participants with opportunities to interact with community members trained and paid by the research team and volunteers to discuss their needs and challenges. Older adults cite maintaining social well-being as more important to their overall health than their physical and cognitive state (39), however social support is often neglected in the care of older adults with debilitating conditions, leading to social isolation, decreased quality of life, and poorer health outcomes (40). Health professionals often do not have the skills or resources to support the social needs of people at the end of life and carers, nor are they the most appropriate people to do so. Building and supporting sustainable, community-based networks are a more appropriate response to these needs.
Personal growth needs, including education, training, and reflection to strengthen knowledge, skills and confidence around to death and dying, were identified and addressed in 12 of the 18 included studies. These needs were addressed with a range of strategies aimed at improving self-efficacy, such as reflection exercises, decision support coaching, and educational offerings about how to live with and support those with a terminal diagnosis. Death, dying, and loss are universal phenomena, yet strategies and resources to support people to learn and grow as they experience them, and to share this learning within their community networks, are often lacking (41). For both people at the end of life and carers, sharing these interpersonal reflections and experiences with others may provide alternative perspectives and, as found in this review, improved emotional functioning (19) and lower burden (22). Noonan et al. define the outcome of this accumulation of knowledge and skills that carers often develop through practice as ‘death literacy', and suggest that death literacy is a resource that strengthens the capacity of individuals and communities for future caring (42).
Lastly, opportunities to build community capacity, including the development of community activist networks, increasing social capital, and partnerships with professional institutions to embed sustainable change, represent an important facet to address community needs in end-of-life care. Eleven of the 18 included studies identified and addressed community capacity building as a need, most often in the form of developing a resource (i.e., educational modules, support groups, volunteer training programme) to be used by the community in perpetuity. Expanding community capacity to support equitable and sustainable end-of-life care is crucial in developing interventions that can continue even after the resources and workforce research teams offer are removed (43). The varied needs addressed in each of the studies supports the idea that public health palliative care approaches work best when they are locally generated in response to community needs and available resources (10).
Other than some similarities in the identified community needs, we found heterogeneity in almost all aspects of the design, implementation, and evaluation of the included intervention studies. Half (n = 8) of the publications reported a theoretical framework underpinning the approach taken, though none overlapped. Similarly, authors described differing mechanisms of action leading to improved outcomes in the five studies that reported on it. Interestingly, among the 10 studies that did not describe their theoretical underpinnings, none went on to discuss the mechanisms of action precipitating their outcomes, suggesting that grounding an intervention in a theoretical framework provided critical scaffolding to establish and test the mechanisms of action that are intended to lead to improved outcomes.
Additionally, studies fell all along the spectrum of community engagement (10) but were concentrated in the middle. In 13 of the 18 included studies, community members acted as agents to deliver the intervention, seven as paid members of the research team, and six as unpaid volunteers. Most studies demonstrated progress in consulting community stakeholders in the development of their intervention and co-creating solutions to identified problems, but nearly all fell short of collaborating with communities to promote shared-decision making in the development of new models of care to meet the needs of people at the end-of-life and their carers. None of the studies were considered to fall into the empowerment level of community engagement. While it is possible some aspects of community engagement were not detailed or that continuing efforts have not been reported, this has implications for the sustainability of the approaches. Particularly in burgeoning fields in which theoretical underpinnings are still being established and tested, as with public health palliative care, community engagement is vitally important for defining key concepts, community assets and needs, appropriate outcomes and sustainable solutions (44). Future research should focus on expanding sustainable community engagement approaches in order to more fully empower communities to identify needs and develop strategies to support people at the end of life.
Once needs were identified and interventions to address them were developed, research teams were tasked with developing evaluation strategies that examined key outcomes for people at the end of life and their carers while also acknowledging the importance of individual experiences and contextual nuance. Again, there was wide variability in the chosen outcome measurements which makes it difficult to conclude which methods are best in evaluating intervention efficacy in which contexts. Qualitative interviews were utilized in 14 studies and were the most common data collection method in evaluating the results and efficacy of the included interventions. Six studies used novel, unvalidated quantitative surveys aimed at eliciting satisfaction with the intervention or quality of care. Furthermore, among those that used validated, quantitative measures, few studies used common tools. QoL was measured using seven different tools across seven different studies (ex. Caregiver Quality of Life–Cancer Scale, McGill Quality of Life Questionnaire, World Health Organization Quality of Life Brief Scale), while caregiver burden was measured using four different tools across three different studies (ex. Caregiver Stressor Scale, Zarit Caregiver Burden, American Medical Association Carer Self-check). Many authors cited the lack of validated quantitative outcome measurement tools as a limitation.
The varied outcome measurement strategies represented in the field of included studies may reflect the differing priorities of the communities in which they were implemented. Defining outcomes that are meaningful to community members is as important as co-creating palliative care approaches that fit the community's needs. It is imperative that future research includes systematic evaluation of which measures are meaningful to community members and the co-creation of research strategies with community members to better fit their context. To do this, the WHO recommends beginning community-engaged health services development with exploratory data collection such as qualitative interviews, co-design workshops, or field observation designed to understand context (i.e., community infrastructure, social networks, existing services), encourage stakeholder engagement and buy-in, and identify shared goals and their corresponding outcome metrics (45).
The contextual information, including personal and environmental factors, that was reported varied widely between studies. In terms of personal factors, nearly all studies (n = 16) reported the age and sex of their participants, but other variables such as marital status, race and ethnicity, education level and employment status were collected less consistently. Environmental factors such as location, urbanicity, access to healthcare services, local infrastructure and transportation were rarely reported. Both personal factors (such as age, sex, race, ethnicity, socioeconomic status, education level, disease type or severity, political and religious ideations) and environmental factors (such as access to healthcare services and urbanicity) have been shown to affect engagement with end-of-life services and outcomes (5). As such, these variables have important implications for how interventions are developed and how their results should be interpreted. While an aim of this review was to examine who public health palliative care approaches work for, it was difficult to do so without detailed descriptions of each of the target communities. Understanding the demographic and socioeconomic context of a community is vitally important to designing appropriate end-of-life services that meet their needs. As the field of public health palliative care moves forward, researchers have an imperative to pay particular attention to these social and structural determinants, the context in which they are working, report personal and environmental variables that could impact uptake and examine associations with outcomes if possible. In doing so, we can gain a better understanding of who these approaches work for and in which contexts and move to tackle the significant inequity which exists currently.
As a matter of special interest, we hoped to focus attention on studies that specifically targeted rural and coastal communities or communities living in economic poverty. Rurality and economic status have been shown to impact access to and the delivery of in end-of-life care (4, 5). In this review, very few studies provided sufficient contextual information to determine whether or not their samples included people from these groups, and even fewer included related aims. The majority of studies took place in high-income countries (n = 16), and only a few reported any data related to the economic status of their participants such as highest level of education (n = 5) and employment status (n = 4). The only publication that had an in-depth discussion of economic status and its impact on the intervention was Jack and colleagues' 2011 report of community volunteers in two urban centers in Uganda (27). Here, they discussed the financial strain of the Ugandan population and the national health system and how that impacted the sustainability of the project. While public health and community-engaged palliative care can benefit people with life-limiting illness in all settings, this model of palliative care notably could benefit those living in rural and coastal communities and those in economic poverty who are less likely to receive appropriate palliative and end-of-life care (46). Included studies provided very little specific detail as to the relative economic status or rurality of the subject populations which make it difficult to determine which interventions and models of care would be most beneficial to this population.
Limitations
First, as the aim of this review was to identify publications that report the results of interventions aimed at fostering community engagement in end-of-life care, we only included studies that reported outcomes from people at the end-of-life or their carers. There are multiple public health palliative care initiatives, like the Neighborhood Network in Palliative Care in India and Compassionate Communities in Canada and Australia, that report community level or volunteer outcomes which fell out of the scope of this review (11, 37, 47). Secondly, we excluded gray literature, conference posters or abstracts without full-text publications, and non-peer reviewed literature. Lastly, there is potentially evidence published in languages other than English that we were unable to identify.
Conclusion
In this review, we aimed to gain a better understanding of existing public health palliative care approaches which captured individual outcomes to understand for whom and how they work, and how differing contexts might impact their design and delivery. We found that community-engaged palliative care interventions represent a strong opportunity for improving support at the end of life, and that engaging community members at various stages in the process can lead to appreciable changes in outcomes. There was marked heterogeneity in the studies' theoretical underpinnings, methods, outcomes of interest and results which suggests that this field is developing rapidly. Based on the varied design and implementation strategies and their collective success in improving outcomes, it is likely that different community engagement approaches will support public health palliative care approaches in different communities. Context is a crucial component in understanding community needs and how they might benefit from public health interventions. Future research should define contextual difference in these communities and should specifically examine how demographics, resource availability, and social capital might impact the design, implementation, and results of public health palliative care interventions. Defining these contextual differences and their impact, then adjusting community engagement strategies appropriately, public health approaches can better fit the needs of the communities in which they are situated.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
The review was designed and developed by LW-D, LH, KW, LS, and RH. The search was carried out by LW-D. AP, AD, LW-D, MI, and MB reviewed all items identified in the search and systematically decided which should be included in the final manuscript. All authors contributed to the writing of the manuscript and provided substantial edits to the final draft.
Funding
KW was supported by the Wellcome Centre for Cultures and Environments of Health (203109/Z/16/Z) and the National Institute for Health Research Applied Research Collaboration South West Peninsula (NIHR200167). AP was supported by Cicely Saunders International.
Conflict of interest
LS was employed by St Christopher's Hospice.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1180571/full#supplementary-material
References
1. Knaul FM, Farmer PE, Krakauer EL, De Lima L, Bhadelia A, Kwete XJ, et al. Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet. (2018) 391:1391–454. doi: 10.1016/S0140-6736(17)32513-8
2. Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, et al. Redefining palliative care-a new consensus-based definition. J Pain Symptom Manage. (2020) 60:754–64. doi: 10.1016/j.jpainsymman.2020.04.027
3. Sleeman KE, de Brito M, Etkind S, Nkhoma K, Guo P, Higginson IJ, et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Health. (2019) 7:e883–92. doi: 10.1016/S2214-109X(19)30172-X
4. Davies JM, Sleeman KE, Leniz J, Wilson R, Higginson IJ, Verne J, Maddocks M, Murtagh FEM. Socioeconomic position and use of healthcare in the last year of life: A systematic review and meta-analysis. PLoS Med. (2019) 16:e1002782. doi: 10.1371/journal.pmed.1002782
5. Nelson KE, Wright R, Peeler A, Brockie T, Davidson PM. Sociodemographic disparities in access to hospice and palliative care: an integrative review. Am J Hosp Palliat Care. (2021) 38:1378–90. doi: 10.1177/1049909120985419
6. Sallnow L, Richardson H, Murray SA, Kellehear A. The impact of a new public health approach to end-of-life care: a systematic review. Palliat Med. (2016) 30:200–11. doi: 10.1177/0269216315599869
7. Kellehear A. Health-promoting palliative care: Developing a social model for practice. Mortality. (1999) 4:75–82. doi: 10.1080/713685967
8. Potvin L, Jones C. Twenty-five years after the ottawa charter: the critical role of health promotion for public health. Public Health. (2011) 102:244–8. doi: 10.1007/BF03404041
9. Mitchell S, Maynard V, Lyons V, Jones N, Gardiner C. The role and response of primary healthcare services in the delivery of palliative care in epidemics and pandemics: a rapid review to inform practice and service delivery during the COVID-19 pandemic. Palliat Med. (2020) 34:1182–92. doi: 10.1177/0269216320947623
10. Sallnow L, Paul S. Understanding community engagement in end-of-life care: developing conceptual clarity. Crit Public Health. (2014) 25:231–8. doi: 10.1080/09581596.2014.909582
11. Sallnow L, Kumar S, Numpeli M. Home-based palliative care in Kerala, India: the neighbourhood network in palliative care. Prog Palliat Care. (2013) 18:14–7. doi: 10.1179/096992610X12624290276142
12. Quintiens B, D'Eer L, Deliens L, Van den Block L, Chambaere K, De Donder L, et al. Area-based compassionate communities: a systematic integrative review of existing initiatives worldwide. Palliat Med. (2022) 36:422–442. doi: 10.1177/02692163211067363
13. Mills J, Abel J, Kellehear A, Patel M. Access to palliative care: the primacy of public health partnerships and community participation. Lancet Public Health. (2021) 6:e791–2. doi: 10.1016/S2468-2667(21)00213-9
14. D'Eer L, Quintiens B, Van den Block L, Dury S, Deliens L, Chambaere K, et al. Civic engagement in serious illness, death, and loss: a systematic mixed-methods review. Palliat Med. (2022) 36:625–51. doi: 10.1177/02692163221077850
15. De Lima L, Pastrana T. Opportunities for palliative care in public health. Annu Rev Public Health. (2016) 37:357–74. doi: 10.1146/annurev-publhealth-032315-021448
16. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
17. Harding R, Higginson IJ. PRISMA: a pan-European co-ordinating action to advance the science in end-of-life cancer care. Eur J Cancer. (2010) 46:1493–501. doi: 10.1016/j.ejca.2010.01.035
18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
19. Allen RS, Harris GM, Burgio LD, Azuero CB, Miller LA, Shin HJ, et al. Can senior volunteers deliver reminiscence and creative activity interventions? Results of the legacy intervention family enactment randomized controlled trial. J Pain Symptom Manage. (2014) 48:590–601. doi: 10.1016/j.jpainsymman.2013.11.012
20. Chen YS, Sun LY, Xiao H, Zheng J, Lin X. Evaluation of a WeChat-based dyadic life review program for people with advanced cancer and family caregivers: a mixed-method feasibility study. Palliat Med. (2022) 36:498–509. doi: 10.1177/02692163211066736
21. Dionne-Odom JN, Wells RD, Guastaferro K, Azuero A, Hendricks BA, Currie ER, et al. An early palliative care telehealth coaching intervention to enhance advanced cancer family caregivers' decision support skills: the CASCADE pilot factorial trial. J Pain Symptom Manage. (2022) 63:11–22. doi: 10.1016/j.jpainsymman.2021.07.023
22. DuBenske LL, Gustafson DH, Namkoong K, Hawkins RP, Atwood AK, Brown RL, et al. CHESS improves cancer caregivers' burden and mood: results of an eHealth RCT. Health Psychol. (2014) 33:1261–72. doi: 10.1037/a0034216
23. Grande GE, Austin L, Ewing G, O'Leary N, Roberts C. Assessing the impact of a Carer Support Needs Assessment Tool (CSNAT) intervention in palliative home care: a stepped wedge cluster trial. BMJ Support Palliat Care. (2017) 7:326–34. doi: 10.1136/bmjspcare-2014-000829
24. Greene A, Aranda S, Tieman JJ, Fazekas B, Currow DC. Can assessing caregiver needs and activating community networks improve caregiver-defined outcomes? A single-blind, quasi-experimental pilot study: community facilitator pilot. Palliat Med. (2012) 26:917–23. doi: 10.1177/0269216311421834
25. Hanson LC, Green MA, Hayes M, Diehl SJ, Warnock S, Corbie-Smith G, et al. Circles of care: implementation and evaluation of support teams for African Americans with cancer. Health Educ Behav. (2014) 41:291–8. doi: 10.1177/1090198113512127
26. Henriksson A, Benzein E, Ternestedt BM, Andershed B. Meeting needs of family members of persons with life-threatening illness: a support group program during ongoing palliative care. Palliat Support Care. (2011) 9:263–71. doi: 10.1017/S1478951511000216
27. Jack BA, Kirton J, Birakurataki J, Merriman A. 'A bridge to the hospice': the impact of a Community Volunteer Programme in Uganda. Palliat Med. (2011) 25:706–15. doi: 10.1177/0269216310397566
28. Luker K, Cooke M, Dunn L, Lloyd-Williams M, Pilling M, Todd C. Development and evaluation of an intervention to support family caregivers of people with cancer to provide home-based care at the end of life: a feasibility study. Eur J Oncol Nurs. (2015) 19:154–61. doi: 10.1016/j.ejon.2014.09.006
29. Oliver DP, Washington KT, Benson J, White P, Oliver DC, Smith JB, et al. Facebook online support groups for hospice family caregivers of advanced cancer patients: protocol, facilitation skills and promising outcomes. J Soc Work End Life Palliat Care. (2022) 18:146–59. doi: 10.1080/15524256.2022.2046236
30. Pesut B, Duggleby W, Warner G, Fassbender K, Antifeau E, Hooper B, et al. Volunteer navigation partnerships: Piloting a compassionate community approach to early palliative care. BMC Palliat Care. (2017) 17:2. doi: 10.1186/s12904-017-0210-3
31. Ryan P, Howell V, Jones J, Hardy E. Lung cancer, caring for the caregivers. A qualitative study of providing pro-active social support targeted to the carers of patients with lung cancer. Palliat Med. (2008) 22:233–8. doi: 10.1177/0269216307087145
32. Steinhauser KE, Alexander SC, Byock IR, George LK, Tulsky JA. Seriously ill patients' discussions of preparation and life completion: an intervention to assist with transition at the end of life. Palliat Support Care. (2009) 7:393–404. doi: 10.1017/S147895150999040X
33. Walshe C, Dodd S, Hill M, Ockenden N, Payne S, Preston N, et al. How effective are volunteers at supporting people in their last year of life? A pragmatic randomised wait-list trial in palliative care (ELSA). BMC Med. (2016) 14:203. doi: 10.1186/s12916-016-0746-8
34. Wang Y, Liu M, Chi I. An evaluation of self-care and caregiving training curriculum content for Chinese immigrant caregivers: a participatory design approach. J Appl Gerontol. (2021) 40:1818–27. doi: 10.1177/0733464820987920
35. Williams AM, Eby JA, Crooks VA, Stajduhar K, Giesbrecht M, Vuksan M, et al. Canada's compassionate care benefit: is it an adequate public health response to addressing the issue of caregiver burden in end-of-life care? BMC Public Health. (2011) 11:335. doi: 10.1186/1471-2458-11-335
36. Witkowski A, Carlsson ME. Support group programme for relatives of terminally ill cancer patients. Support Care Cancer. (2004) 12:168–75. doi: 10.1007/s00520-003-0518-9
37. Librada-Flores S, Nabal-Vicuna M, Forero-Vega D, Munoz-Mayorga I, Guerra-Martin MD. Implementation models of compassionate communities andcompassionate cities at the end of life: a systematic review. Int J Environ Res Public Health. (2020) 17:6271. doi: 10.3390/ijerph17176271
38. O'Mara-Eves A, Brunton G, McDaid D, Oliver S, Kavanagh J, Jamal F, et al. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis. Public Health Res. (2013) 1. doi: 10.3310/phr01040
39. Ten Bruggencate T, Luijkx KG, Sturm J. To meet, to matter, and to have fun: the development, implementation, and evaluation of an intervention to fulfil the social needs of older people. Int J Environ Res Public Health. (2019) 16:2307. doi: 10.3390/ijerph16132307
40. Mehrabi F, Beland F. Effects of social isolation, loneliness and frailty on health outcomes and their possible mediators and moderators in community-dwelling older adults: a scoping review. Arch Gerontol Geriatr. (2020) 90:104119. doi: 10.1016/j.archger.2020.104119
41. Kellehear A. The end of death in late modernity: an emerging public health challenge. Crit Public Health. (2007) 17:71–9. doi: 10.1080/09581590601156365
42. Leonard R, Noonan K, Horsfall D, Kelly M, Rosenberg JP, Grindrod A, et al. Developing a death literacy index. Death Stud. (2022) 46:2110–22. doi: 10.1080/07481187.2021.1894268
43. Azeez A. Social capital and sustainable health care: an analysis of community based palliative care model of Kerala. Ind J Sustain Dev. (2015) 1. doi: 10.21863/ijsd/2015.1.1.001
44. Brunton G, Thomas J, O'Mara-Eves A, Jamal F, Oliver S, Kavanagh J. Narratives of community engagement: a systematic review-derived conceptual framework for public health interventions. BMC Public Health. (2017) 17:944. doi: 10.1186/s12889-017-4958-4
45. WHO. WHO Community Engagement Framework for Quality, People-Centred and Resilient Health Services. Geneva: WHO (2017).
46. Castleden H, Crooks VA, Schuurman N, Hanlon N. “It's not necessarily the distance on the map…”: using place as an analytic tool to elucidate geographic issues central to rural palliative care. Health Place Mar. (2010) 16:284–90. doi: 10.1016/j.healthplace.2009.10.011
Keywords: public health, palliative care, end-of-life, interventions, community engaged
Citation: Peeler A, Doran A, Winter-Dean L, Ijaz M, Brittain M, Hansford L, Wyatt K, Sallnow L and Harding R (2023) Public health palliative care interventions that enable communities to support people who are dying and their carers: a scoping review of studies that assess person-centered outcomes. Front. Public Health 11:1180571. doi: 10.3389/fpubh.2023.1180571
Received: 06 March 2023; Accepted: 05 July 2023;
Published: 26 July 2023.
Edited by:
Richard John Siegert, Auckland University of Technology, New ZealandReviewed by:
Gitismita Naik, All India Institute of Medical Sciences, Kalyani (AIIMS Kalyani), IndiaSuzie Xu Wang, Leeds Beckett University, United Kingdom
Samira Beiranvand, Ahvaz Jundishapur University of Medical Sciences, Iran
Copyright © 2023 Peeler, Doran, Winter-Dean, Ijaz, Brittain, Hansford, Wyatt, Sallnow and Harding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Peeler, YW5uYS5wZWVsZXJAa2NsLmFjLnVr
 Anna Peeler
Anna Peeler Alexandra Doran
Alexandra Doran Lee Winter-Dean
Lee Winter-Dean Mueed Ijaz2
Mueed Ijaz2