
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health , 04 May 2023
Sec. Disaster and Emergency Medicine
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1180511
The coronavirus disease of 2019 (COVID-19) pandemic, directly and indirectly, affected the emergency medical care system and resulted in worse out-of-hospital cardiac arrest (OHCA) outcomes and epidemiological features compared with those before the pandemic. This review compares the regional and temporal features of OHCA prognosis and epidemiological characteristics. Various databases were searched to compare the OHCA outcomes and epidemiological characteristics during the COVID-19 pandemic with before the pandemic. During the COVID-19 pandemic, survival and favorable neurological outcome rates were significantly lower than before. Survival to hospitalization, return of spontaneous circulation, endotracheal intubation, and use of an automated external defibrillator (AED) decreased significantly, whereas the use of a supraglottic airway device, the incidence of cardiac arrest at home, and response time of emergency medical service (EMS) increased significantly. Bystander CPR, unwitnessed cardiac arrest, EMS transfer time, use of mechanical CPR, and in-hospital target temperature management did not differ significantly. A subgroup analysis of the studies that included only the first wave with those that included the subsequent waves revealed the overall outcomes in which the epidemiological features of OHCA exhibited similar patterns. No significant regional differences between the OHCA survival rates in Asia before and during the pandemic were observed, although other variables varied by region. The COVID-19 pandemic altered the epidemiologic characteristics, survival rates, and neurological prognosis of OHCA patients.
Review registration: PROSPERO (CRD42022339435).
Worldwide out-of-hospital cardiac arrest (OHCA) has a reported incidence of 55–88 per 100,000, and is an important national health problem that has a high mortality rate if not treated properly (1–6). The International Liaison Committee on Resuscitation reported that emergency medical service (EMS)-treated OHCA and bystander CPR increased steadily (7). As OHCA onset is difficult to predict and occurs in places other than hospitals, various social and medical components are required in the treatment process (8). In the past 40 years, the survival rate of OHCA patients worldwide has been improving, and the factors that influenced this improved survival include rapid recognition of patients by bystanders, bystander CPR, rapid EMS response, and the use of AEDs (8–10). Moreover, post-OHCA survival may be affected by the characteristics of the emergency medical care system in regions and countries where the cardiac arrest has occurred (1, 3).
Coronavirus disease of 2019 (COVID-19) first emerged in December 2019 and spread globally; on March 11, 2020, a pandemic was declared by the World Health Organization (WHO) (11). By October 2022, approximately 600 million people worldwide had been diagnosed with COVID-19, which resulted in approximately 6.5 million deaths (12). Paramedics were equipped with personal protective equipment and took additional steps to prepare ambulances for dispatch to access emergency patients at risk of infection, which contributed to delays in dispatch (13). Moreover, hospitals faced difficulties in securing isolation spaces and beds for critical care, which led to patient-capacity restrictions that affected the medical care for not only patients with fevers but also non-COVID-19 emergency patients (14–17). In the early days of the pandemic, the healthcare system was unprepared to face the pandemic, and the majority of medical resources were concentrated on the care of COVID-19 patients, which resulted in a collateral impact on the outcomes of various other conditions. Hospitalizations and mortality rates increased for patients with acute myocardial infarction and ischemic stroke, complication rates in patients with acute peritonitis increased, and time to surgery was delayed (14–16). The incidence and mortality rates of OHCA, which has a very high fatality rate when immediate appropriate treatment is not given, have also increased (18, 19). In addition, the desire to “social distance” may have led to a decrease in EMS or hospital utilization in serious cases.
Several previous observational studies and meta-analyses have reported the incidence rate, epidemiological characteristics, and prognosis of OHCA patients during the pandemic compared with the pre-COVID-19 pandemic period (20–23). Shockable rhythms, automatic external defibrillator application use, and endotracheal intubation use were reported to have decreased, whereas EMS reaction time, arrest-at-home frequency, and use of supraglottic airways were reported to have increased (20–23). Treatment-induced return of spontaneous circulation (ROSC), survival to admission, survival to discharge, 30-day survival, and favorable neurological outcomes all had poor results during the pandemic (20–23). The pandemic had a significant impact on the survival and neurological prognosis of OHCA patients. However, as the COVID-19 pandemic continues, meta-analyses of the entire pandemic period that do not evaluate the effects of each period and region can potentially distort the results.
The medical system experienced a decrease in the care of various other diseases due to the focus on COVID-19 treatments at the beginning of the pandemic. The development of therapeutics and vaccines, the reduction in deadly COVID-19 subvariants, the change in the dominant variant, and the improved awareness of the general population and medical staff, who initially suffered panic and fear, have led to improvements to the emergency medical care system (24, 25).
As the emergency medical care system improved over time and adapted to different regional changes, a targeted, stratified, and refined meta-analysis is necessary to address the knowledge gap that exists despite the existing meta-analyses. The purpose of this review is to examine the most recent trends of change in epidemiological factors, prehospital factors, and outcomes for OHCA affected by the COVID-19 pandemic.
This systematic review and meta-analysis were performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (26). The review protocol was registered in The International Prospective Register of Systematic Reviews (PROSPERO; CRD42022339435).
The participants were adult OHCA patients (age ≥18 years) from before and after the start of the COVID-19 pandemic period. The survival rate was the primary outcome, and the secondary endpoint was comprised of the factors that are associated with each stage of the survival chain and good neurological prognoses (Supplementary Table S1).
In October 2022, PubMed, EMBASE, Cochrane Library, bioRxiv, and medRxiv databases were searched to identify relevant studies. In addition, the reference lists of previous meta-analyses were reviewed to identify and include any missing studies. Analyzable studies were manually searched on Google Scholar.
An extensive search based on the two keywords, “COVID-19 pandemic” and “out-of-hospital cardiac arrest,” as well as the related MeSH terms and Embase subject headings, was conducted. The search strategies that were used for each database search are described in Supplementary Table S2.
Duplicated references were excluded using the bibliographic management program (Endnote 20; Clarivate Analytics, Philadelphia, PA, United States) based on the title, author, and year of publication. Two researchers independently checked the titles and abstracts of the articles to implement the primary exclusion. The full-text articles were subsequently extracted and reviewed, and a second exclusion was carried out. Through the consensus of two reviewers, the studies were selected for inclusion in the final analysis. If there was a disagreement about the studies to be included, the final decision was made after seeking the opinion of an expert in the field.
The exclusion criteria were as follows: the absence of comparative data between the time of the COVID-19 pandemic and the preceding period; the primary result was missing; studies that used redundant data; and review articles, case reports, editorials, commentaries, meta-analyses, animal studies, and molecular biology studies.
Finally, retrospective observational studies in OHCA patients aged 18 years and older that presented variables associated with prognosis and the chain of survival after cardiac arrest and compared the time of the COVID-19 pandemic with the preceding period were included in this systematic review and meta-analysis.
Data extraction was conducted independently after a sufficient discussion by two researchers; if there was disagreement, the decision was made by a majority vote that incorporated the opinion of a third expert. The information provided in the studies was extracted as objectively and reliably as possible and included the following details: study information (randomly assigned study number, author name, year of publication, country where the study was conducted), research method (study design), study subjects (total number of participants, study period, age, sex), survival discharge rate, neurological prognosis, 30-day survival rate, rate of survival to hospital admission, target body temperature treatment, spontaneous circulation recovery rate, tracheal intubation, use of glottal gastric airway, CPR performed using mechanical CPR, automatic external defibrillator use, witness CPR, unwitnessed cardiac arrest, shock required rhythm, cardiac arrest at home, EMS response time, and EMS transport time. The EMS response time was defined as the time it took for the paramedic to make contact with the patient after the cardiac arrest was first reported to the emergency agency. The EMS transport time was defined as the time it took from the cardiac arrest site to the arrival at the medical institution.
Data on the EMS response time and EMS transport time were collected as the mean and standard deviation as a continuity variable, and in studies where the data were presented as the median and quartiles, these were converted to the mean and standard deviation (27).
A quality assessment of the included studies was performed to determine whether the studies were conducted appropriately for the stated purpose. The studies included in this meta-analysis were non-randomized clinical trials (NRCT) and were evaluated using the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) (28). ROBINS-I consists of seven areas: (1) bias due to confounding, (2) bias in study subject selection, (3) bias in the classification of interventions during interventions, assessed to identify pre-intervention confounding, (4) bias due to the deviation from the intended intervention, (5) bias due to missing values, (6) bias in measuring intervention outcomes, and (7) bias in the selection of reported study outcomes to assess post-intervention bias.
This meta-analysis investigated the epidemiological characteristics and outcomes of OHCA during the COVID-19 pandemic compared with that of before the pandemic. Individual and pooled statistics were calculated as the odds ratio (OR) and mean difference with a 95% confidence interval (CI). The random-effects model was used to determine the pooled outcome from the included studies, based on the diversity of the medical system according to the nation, region, and study period. We estimated the proportion of inter-study inconsistency using the I2 statistic to assess the heterogeneity. We considered I2 values of 25%, 50%, and 75% as low, moderate, and high heterogeneity, respectively (29).
Subgroup analyses were conducted according to the study period (with the first wave-only versus with sequential wave periods with and without the first wave) and regional (Asia, Europe, and the United States and Australia). Emergency care systems had different tendencies in the first wave compared with the subsequent waves of the COVID-10 pandemic. Previous studies have shown that there were lower severity and mortality rates in COVID-19 patients after the first wave due to changes in the system (30–33). In the subgroup analysis in this study, studies that analyzed only the first wave and those that included the subsequent wave periods were separately analyzed. However, in the group of studies including subsequent wave periods, data from the first wave were included. The first wave was from March to June 2020, according to the WHO’s COVID-19 incidence graph. In addition, there were differences in the prevalence of the COVID-19 pandemic by country and region due to a combination of healthcare systems and social and cultural factors in response to the COVID-19 pandemic. Stratified analyses were performed on the studies by categorizing and grouping them into Asia, Europe, and the United States and Australia.
We performed the meta-analysis using R (version 4.0.0, The R Foundation for Statistical Computing, Vienna, Austria), with the packages “meta” (version 4.11-0) and “metaphor” (version 2.1-0). A p-value less than 0.05 was considered statistically significant. Publication bias was assessed using a funnel plot. Asymmetry of the funnel plot was an indicator of bias.
A total of 4,715 articles were searched from five databases, and eight were identified through manual searches. In total, 4,723 articles were found. After excluding duplicate searches by title, author, and year of publication, 3,902 articles were subjected to primary exclusion based on a review of the title and abstract. Sixty-six articles were identified to be potentially related to the research topic and underwent a full-text review for secondary exclusion. A total of 18 documents were excluded during the secondary exclusion review for the following reasons: the type of study met the exclusion criteria (9 cases: reviews), the study did not compare data from before the COVID-19 pandemic (4 studies), the results of the studies were inconsistent with the objectives of this study (3 studies compared myocardial infarction and in-hospital cardiac arrest), overlapping participants (one study whose authors used the same sample in subsequent studies with overlapping variables), and inadequate information about the comparison or control group (one study did not have relevant data on the comparison of the COVID-19 pandemic with the pre-pandemic period). Finally, 48 articles were included in this systematic review and meta-analysis (Figure 1) (13, 34–80).
The main characteristics and basic patient characteristics from the 48 studies included in this systematic review and meta-analysis are described in Table 1. The timing of COVID-19 in the included studies is presented in Supplementary Figure S1.
Thirty-four studies only included data from the first wave of COVID-19, and fourteen studies included data from the second and subsequent waves of COVID-19. Studies were grouped into four regional categories: fourteen studies conducted in the Republic of Korea, Japan, Thailand, Taiwan, and Singapore were grouped in the Asia group; nine studies were conducted in Europe; and the remain studies were classified into the United States and Australia group. The study by Lim et al. compared OHCAs during and before the COVID-19 pandemic in Singapore and Atlanta, United States, the data from these two locations were collected and analyzed separately (58).
The risk of bias was assessed using ROBINS-I for the 49 studies included in this systematic review and meta-analysis (Supplementary Figures S2, S3). Bias occurred mainly before the intervention (domains 1 and 2) and during the intervention (domain 3). Domain 1 was assessed as low risk of bias if the patient’s baseline, disease, history, and predefined confounding factors were presented clearly and as moderate or high risk when this information was not provided. Only 7 of the 48 studies were rated as low risk. The risk of bias (domain 3) of intervention was assessed as low if the duration of the intervention was presented with clear criteria and moderate if this was not presented. In addition, when 2020 was included in the control period or if no clear classification criteria were proposed, the risk was rated as moderate or high. For the post-intervention (domains 4–7) items, all the studies were assessed as low risk.
A total of 26 studies showed a statistically significant reduction in live discharge rates during the COVID-19 pandemic (OR, 0.66; 95% CI, 0.56–0.76; I2 = 59%; Figure 2A). Spontaneous circulatory recovery rates decreased significantly during the COVID-19 pandemic in 33 studies (OR, 0.71; 95% CI, 0.64–0.79; I2 = 79%; Figure 2B). Survival to hospital admission rates decreased significantly during the COVID-19 pandemic in 22 studies (OR, 0.63; 95% CI, 0.56–0.71; I2 = 88%; Figure 2C). Seven studies showed a statistically significant reduction in 30-day survival during the COVID-19 pandemic (OR, 0.66; 95% CI, 0.46–0.95; I2 = 72%; Figure 2D). Neurological prognoses were significantly worse during the COVID-19 pandemic in 15 studies (OR, 0.73; 95% CI, 0.63–0.84; I2 = 49%; Figure 2E).
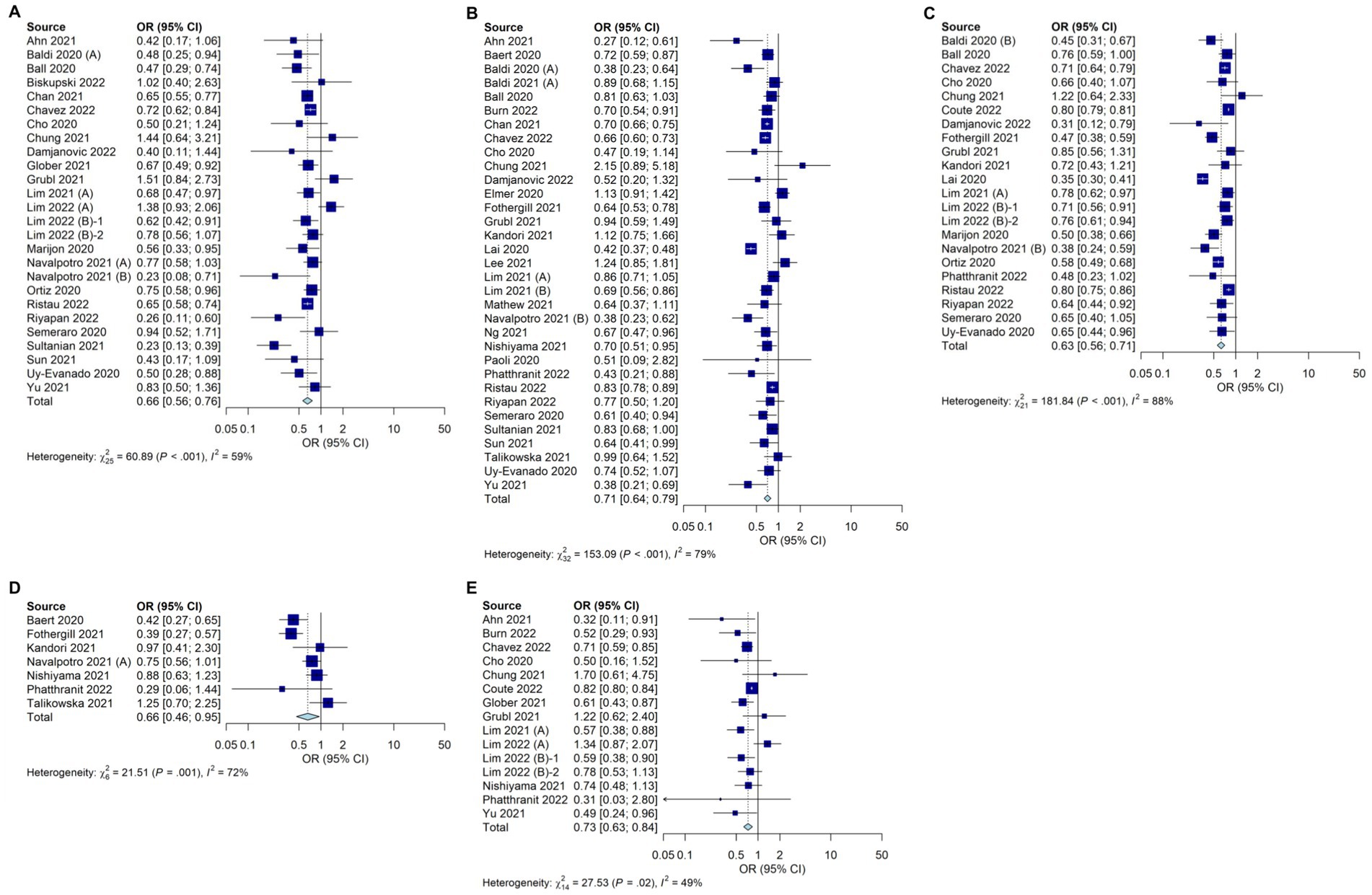
Figure 2. Forest plot depicting the outcomes of OHCA during the COVID-19 pandemic compared with those before the pandemic. (A) Live discharge rates (B) Spontaneous circulatory recovery rates (C) Survival to hospital admission rates (D) 30-day survival (E) Neurological prognoses.
The incidence of cardiac arrest at home was increased significantly during the COVID-19 pandemic in 30 studies (OR, 1.39; 95% CI, 1.24–1.56; I2 = 87%; Figure 3A). The use of AEDs was significantly decreased during the COVID-19 pandemic in 26 studies (Figure 3B; OR, 0.79; 95% CI, 0.69–0.90; I2 = 74%) and the rhythm of shock needs was not significantly different in 38 studies, which depicted a trend that differed from previous meta-analyses (Figure 3C; OR, 0.89; 95% CI, 0.79–1.01; I2 = 85%). The number of unwitnessed cardiac arrests did not differ significantly between during the COVID-19 pandemic and before the COVID-19 period in 38 studies (Figure 3D; OR, 0.98; 95% CI, 0.92–1.05; I2 = 73%). The rate of bystander CPR being performed did not differ significantly between during the COVID-19 pandemic and before the COVID-19 pandemic in 44 studies (Figure 3E; OR, 0.95; 95% CI, 0.88–1.04; I2 = 83%).
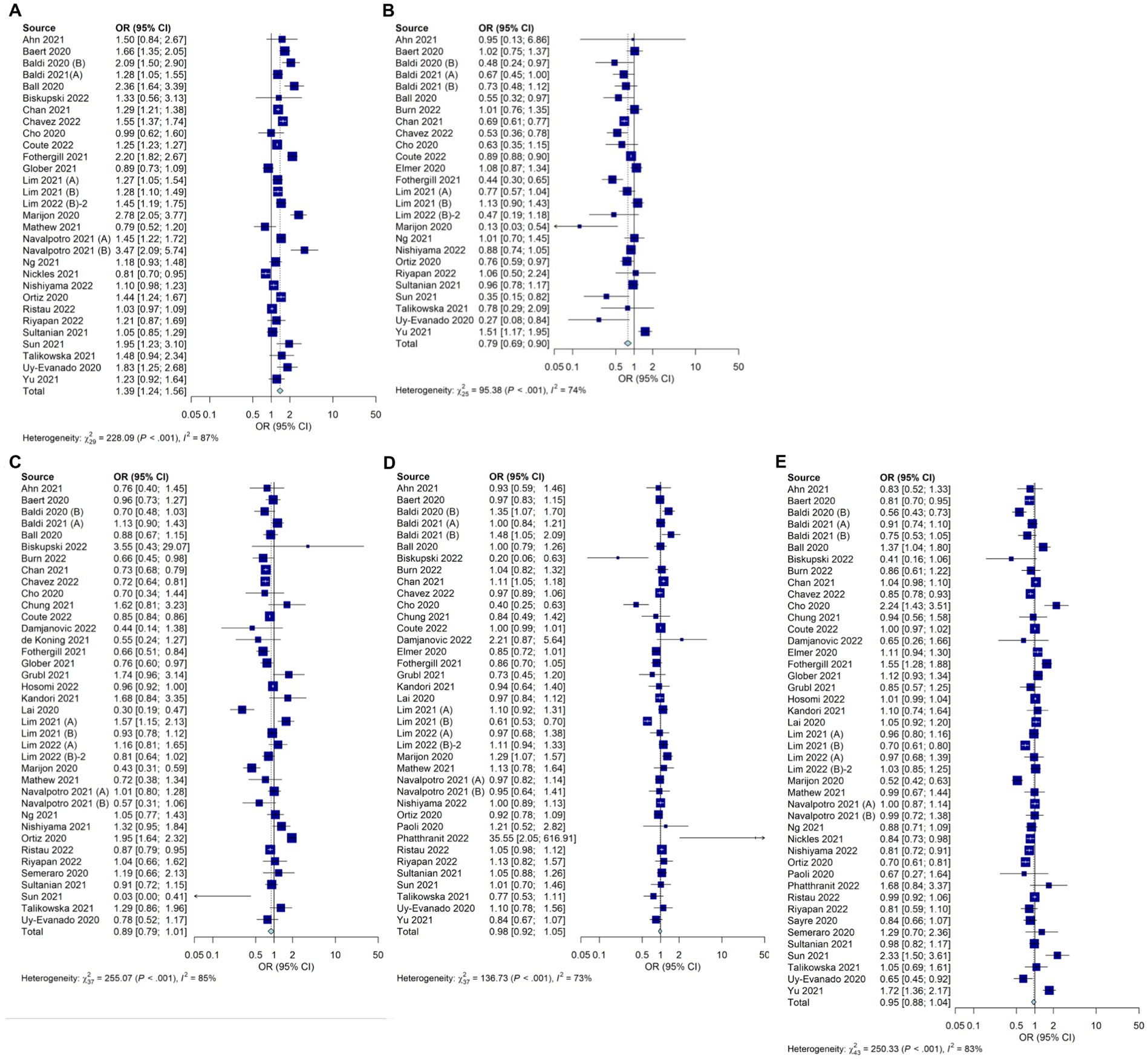
Figure 3. Forest plot depicting the epidemiologic factors of OHCA during the COVID-19 pandemic compared with those before the pandemic. (A) Incidence of cardiac arrest at home (B) Use of AEDs (C) Rhythm of shock needs (D) Number of unwitnessed cardiac arrests (E) Rate of bystander CPR.
The EMS response time was significantly longer during the COVID-19 pandemic in 30 studies (mean difference, 1.40; 95% CI, 0.79–2.02; I2 = 98%; Figure 4A). There was no significant difference in the EMS transport time in four studies (mean difference, 0.78; 95% CI, −0.06 to 1.62; I2 = 77%; Figure 4B). The use of supraglottal airway devices increased significantly during the pandemic in 12 studies (Figure 4C; OR, 1.69; 95% CI, 1.22–2.34; I2 = 97%), whereas endotracheal intubation, as analyzed in 18 studies, decreased significantly (Figure 4D; OR, 0.51; 95% CI, 0.38–0.68; I2 = 97%). Data on CPR with mechanical CPR devices were included in eight studies and did not differ significantly between during the COVID-19 pandemic and before the COVID-19 pandemic (Figure 4E; OR, 1.36; 95% CI, 0.85–2.19; I2 = 89%). Prehospital spontaneous circulatory recovery rates were significantly reduced during the COVID-19 pandemic in 27 studies (OR, 0.70; 95% CI, 0.61–0.79; I2 = 81%; Figure 4F).

Figure 4. Forest plot depicting the prehospital factors of OHCA during the COVID-19 pandemic compared with those before the pandemic. (A) EMS response time (B) EMS transport time (C) Use of supraglottal airway devices (D) Endotracheal intubation (E) CPR with mechanical CPR devices (F) Prehospital spontaneous circulatory recovery rates.
There was no significant difference in the target body temperature treatment between during the COVID-19 pandemic and before the COVID-19 pandemic in seven studies (OR, 0.64; 95% CI, 0.37–1.10; I2 = 52%; Supplementary Figure S4).
The entire analysis was divided into studies that included studies with first wave data only (A) and studies with sequential wave periods with and without the first wave (B), both of which showed a significant reduction in the survival discharge rates compared with the pre-pandemic period (OR, 0.63; 95% CI, 0.51–0.77; I2 = 64% and OR, 0.69; 95% CI, 0.63–0.75; I2 = 44%, respectively; Table 2; Supplementary Figure S5). Spontaneous circulatory recovery rates decreased significantly in (A) and (B) compared with the pre-pandemic periods (OR, 0.66; 95% CI, 0.58–0.75; I2 = 78% and OR, 0.83; 95% CI, 0.71–0.98; I2 = 74%, respectively; Table 2; Supplementary Figure S5). Survival to hospital admission and favorable neurological prognosis rates decreased significantly in (A) and (B) compared with the pre-pandemic period [(A) OR, 0.56; 95% CI, 0.48–0.66; I2 = 79% and OR, 0.72; 95% CI, 0.56–0.93; I2 = 50%, respectively; (B) OR, 0.78; 95% CI, 0.74–0.82; I2 = 30% and OR, 0.74; 95% CI, 0.63–0.87; I2 = 49%, respectively; Table 2; Supplementary Figure S5].
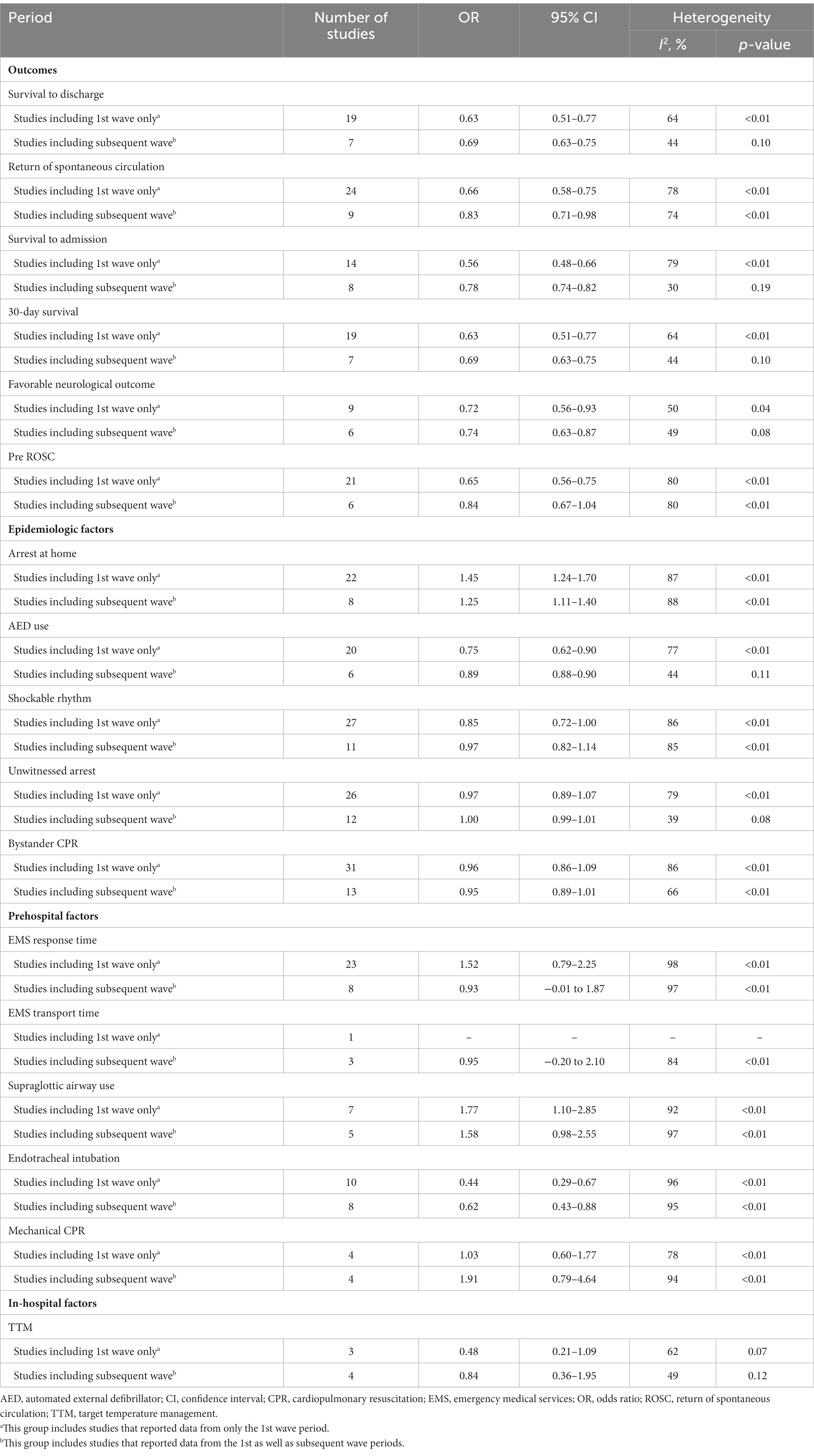
Table 2. Subgroup analysis according to the inclusion period following the early outbreak period: comparison of outcomes during the COVID-19 pandemic versus before the pandemic.
Furthermore, the incidence of cardiac arrest at home showed the same trend, with the same significant increase in (A) and (B), compared with the pre-pandemic period (OR, 1.45; 95% CI, 1.24–1.70; I2 = 87% and OR, 1.25; 95% CI, 1.11–1.40; I2 = 88%, respectively; Table 2; Supplementary Figure S6). The use of automatic external defibrillators decreased significantly in (A) and (B) compared with that of the pre-pandemic period (OR, 0.75; 95% CI, 0.62–0.90; I2 = 77% and OR, 0.89; 95% CI, 0.88–0.90; I2 = 44%, respectively; Table 2; Supplementary Figure S6).
The EMS response time increased significantly in period (A) compared with before the pandemic; however, no significant difference between period (B) and the pandemic period was observed (mean difference, 1.52; 95% CI, 0.79–2.25; I2 = 98% and OR, 0.93; 95% CI, −0.01 to −1.87; I2 = 97%, respectively; Table 2; Supplementary Figure S7). The use of supraglottal airway devices increased significantly in period (A) compared with before the pandemic, although this did not significantly differ from that in period (B) (OR, 1.77; 95% CI, 1.10–2.85; I2 = 92% and OR, 1.58; 95% CI, 0.98–2.55; I2 = 97%, respectively; Table 2; Supplementary Figure S7). Endotracheal intubation significantly decreased in (A) and (B) compared with before the pandemic (OR, 0.44; 95% CI, 0.29–0.67; I2 = 96% and OR, 0.62; 95% CI, 0.43–0.88; I2 = 95%, respectively; Table 2; Supplementary Figure S7). The spontaneous circulatory recovery rate at the prehospital stage decreased significantly in period (A) compared with the pre-pandemic period, whereas period (B) did not significantly differ compared with the pre-pandemic period (OR, 0.65; 95% CI, 0.56–0.75; I2 = 80% and OR, 0.84; 95% CI, 0.67–1.04; I2 = 80%, respectively; Table 2; Supplementary Figure S7).
Target temperature management in the hospital stage did not significantly differ in period (A) of period (B) compared with the pre-pandemic pandemic (OR, 0.48; 95% CI, 0.21–1.09; I2 = 62% and OR, 0.84; 95% CI, 0.36–1.95; I2 = 49%, respectively; Table 2; Supplementary Figure S8).
Survival discharge rates decreased significantly during the COVID-19 pandemic in Europe and the United States, whereas no significant difference was detected in Asia (OR 0.61, 95% CI 0.43–0.85, I2 = 71%, OR 0.69, 95% CI 0.62–0.76, I2 = 0%, and OR 0.71, 95% CI 0.49–1.02, I2 = 0%, respectively; Table 3; Supplementary Figure S9). In Asia, Europe, and North America, the total spontaneous recovery and survival hospitalization rates decreased significantly during the COVID-19 pandemic (ROSC: OR 0.73, 95% CI 0.57–0.93, I2 = 67%; OR 0.69, 95% CI 0.60–0.81, I2 = 61%; and OR 0.68, 95% CI 0.55–0.84, I2 = 90%, respectively. Survival to admission: OR 0.73, 95% CI 0.64–0.83, I2 = 0%; OR 0.56, 95% CI 0.46–0.68, I2 = 85%; and OR 0.63, 95% CI 0.46–1.86, I2 = 96%, respectively; Table 3; Supplementary Figure S9). The neurological prognosis in Asia and the United States significantly worsened during the COVID-19 pandemic (OR 0.69, 95% CI 0.50–0.95, I2 = 54%, and OR 0.74, 95% CI 0.65–0.85, I2 = 45%, respectively; Table 3; Supplementary Figure S9).
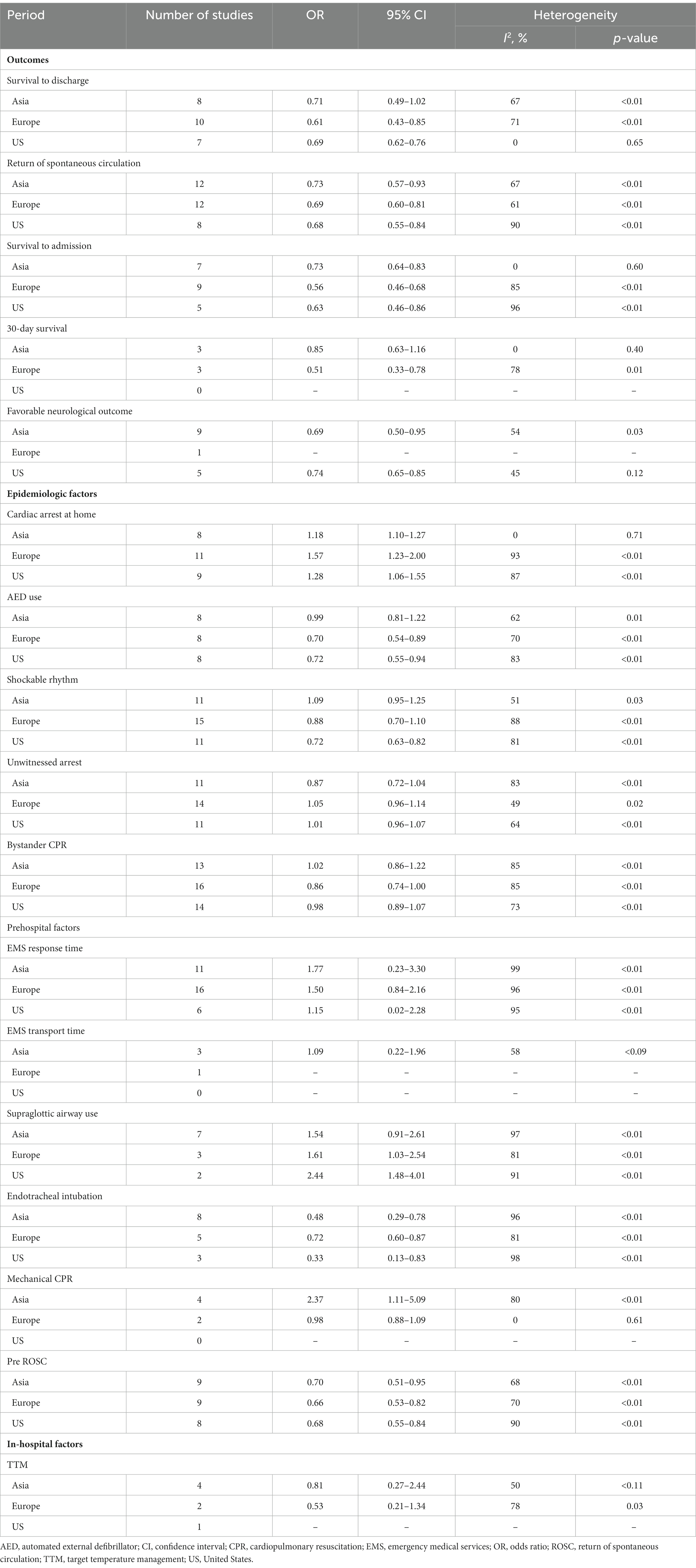
Table 3. Region-wise comparison of the data on survival analysis during the COVID-19 pandemic with before the pandemic.
In Asia, Europe, and North America, the number of cardiac arrests at home significantly increased during the COVID-19 pandemic (OR 1.18, 95% CI 1.10–1.27, I2 = 0%; OR 1.57, 95% CI 1.23–2.00, I2 = 93%; and OR 1.28, 95% CI 1.06–1.55, I2 = 0%, respectively; Table 3; Supplementary Figure S10). In all three regions, the EMS response times were significantly longer during the COVID-19 pandemic (mean difference 1.77, 95% CI 0.23–3.30, I2 = 99%; mean difference 1.50, 95% CI 0.84–2.16, I2 = 96%; and mean difference 1.15, 95% CI 0.02–2.28, I2 = 95%, respectively; Table 3; Supplementary Figure S10).
In Europe and the United States, the use of supraglottal airway devices significantly increased during the pandemic, whereas in Asia, the use did not significantly differ (OR 1.61, 95% CI 1.03–2.54, I2 = 81%; OR 2.44, 95% CI 1.48–4.01, I2 = 91%; and OR 1.54, 95% CI 0.91–2.61, I2 = 97%, respectively; Table 3; Supplementary Figure S11). In Asia, Europe, and the United States, endotracheal intubation rates significantly decreased during the COVID-19 pandemic (OR 0.48, 95% CI 0.29–0.78, I2 = 0%; OR 0.72, 95% CI 0.60–0.87, I2 = 0%; and OR 0.33, 95% CI 0.13–1.83, I2 = 98%, respectively; Table 3; Supplementary Figure S11). Prehospital spontaneous circulatory recovery rates significantly decreased during the COVID-19 pandemic (OR 0.70, 95% CI 0.51–0.95, I2 = 68%; OR 0.66, 95% CI 0.53–0.82, I2 = 70%; and OR 0.68, 95% CI 0.55–0.84, I2 = 90%, respectively; Table 3; Supplementary Figure S11).
In Europe and Asia, target temperature management in the hospital stage did not significantly differ compared with the pre-pandemic pandemic (OR, 0.53; 95% CI, 0.21–1.34; I2 = 78% and OR, 0.81; 95% CI, 0.27–2.44; I2 = 50%, respectively; Table 3; Supplementary Figure S12).
The ROSC and prehospital ROSC showed asymmetric funnel plots for the variables that were assessed in this study from more than ten studies (Supplementary Figure S13).
The COVID-19 pandemic greatly impacted the survival chain of OHCA patients at each stage of the survival chain. This review analyzed the latest studies comparing OHCA during the pandemic with pre-pandemic periods and included subgroup analyses based on region and time. A meta-analysis of 48 studies showed significant reductions in survival discharge and 30-day survival rates during the pandemic. Previous studies after the first wave also showed reduced survival to discharge rates (20, 22, 23). A regional analysis showed significant reductions in the United States and Europe but not in Asia, where there was no significant difference in survival rates during the pandemic. This review is clinically significant as it provides a detailed analysis of the pandemic’s impact on OHCA patients, considering the latest studies and regional and time-specific characteristics. However, previous studies only analyzed data from the early pandemic period, so ongoing research is needed to fully understand the pandemic’s impact on OHCA patients. The findings of this review underscore the importance of a coordinated response to maintain the survival chain of OHCA patients during pandemics.
Previous research has shown that the impact of the COVID-19 pandemic on cardiac arrest can be categorized into direct and indirect effects (81). Direct factors include hypoxia induced by the respiratory disease itself, inflammatory reactions (cytokine storms, thrombosis, myocarditis, and arrhythmias), pulmonary embolism caused by thrombosis, acute coronary syndrome, and drug-induced arrhythmias (81–84). Suggested indirect factors include social lockdown and distancing measures, home quarantine, the reopening of the health care system, reduction of emergency testing and skills, overloading of the emergency and hospital systems, wearing of personal protective equipment, reduction in hospital staffing, delays in care, and more frequent situations of being at risk when alone (20, 23, 81). These factors are closely related to the number of initial COVID-19 cases, and it can be assumed that the impact on the health system and OHCA was lower because the number of COVID-19 patients in Asia and the Republic of Korea was relatively low compared with Europe and North America during the initial pandemic period. In the Republic of Korea, the initial increase in cases showed a different trend than the United States and Europe, indicating that the OHCA survival rate during the pandemic and pre-pandemic period was not significantly different (19).
Depending on the region and country, policies related to the COVID-19 pandemic have shown different approaches (85–87). Several countries sought to prevent the spread of the virus by implementing strict lockdowns to block the inflow and transmission from the beginning of the COVID-19 pandemic and surveillance and tracing strategies of the infected and suspected patients by utilizing IT technology (85, 86, 88). In particular, Asian countries, such as the Republic of Korea and Japan, tried to contain the entry and spread of COVID-19 through stronger controls in the early stages of the outbreak (88). These approaches led to more available medical resources that could afford to operate relatively efficiently, resulting in a lower impact of the COVID-19 pandemic on OHCA (19, 89).
As in a previous meta-analysis, there was a significant increase in cardiac arrests at home, which can be explained by the fact that more people were in quarantine during the COVID-19 pandemic and time spent at home increased due to strong social distancing (90). The increase in cardiac arrest at home is related to other variables. In the subgroup analysis of this study, except in Asia, the use of AEDs decreased significantly during the COVID-19 pandemic. Since AEDs are mostly installed in public places, a significant increase in cardiac arrest at home would also reduce the likelihood of their application. Leung et al. noted that the use of AEDs in public places might have been reduced as governmental social distancing and activity restrictions limited access to public places (91). Nishiyama et al. showed that the number of AED applications decreased during the first wave of the COVID-19 pandemic but increased in the subsequent waves (68). Even those who were able to apply an AED and perform CPR did not know how to respond to cardiac arrest patients in a pandemic-like situation, reducing the rate of CPR performance. The implementation of AEDs increased with the publication of guidelines recommending active treatment by the public. Therefore, the dissemination of clear guidelines from authorized institutions to general citizens may improve the active treatment of OHCA patients (68).
Willingness to perform CPR varied in studies on witnessed OHCA. While some studies reported decreased willingness due to COVID-19, others found no change (92, 93). Fear of infection may make witnesses hesitant, but the increase in OHCA at home may have increased opportunities for family members to provide CPR with less resistance to infection. In addition, unlike previous meta-analyses that showed a decrease in shockable rhythms during the pandemic (20–23), this study found no significant difference compared to the pre-pandemic period. The reduced fatality rate of COVID-19 patients may have led to a decrease in OHCA patients, which is not significantly different from the pre-pandemic period. The fatality rate peaked in April 2020 at 7.71% but gradually declined to 5.21% by July 1, 2020, and is continuing to decrease since then (94). The decline in the fatality rate may have led to a decrease in OHCA patients and shockable rhythms. These findings suggest that the impact of the pandemic on OHCA patients is multifaceted and related to both direct and indirect factors, as well as the timing and fatality rate of COVID-19.
The use of endotracheal intubation decreased significantly during the COVID-19 pandemic across all subgroups, while the use of supraglottic airway devices increased significantly in most subgroups in this study. Meanwhile, CPR with mechanical CPR devices increased significantly in the subgroup analysis of Asia. Temporary resuscitation guidelines were issued by the ILCOR, the American Heart Association, and the European Resuscitation Committee for cardiac arrest patients with suspected or confirmed COVID-19, aiming to reduce the risk of infection for rescuers and the number of rescuers involved in resuscitation (95–97). The guidelines recommend the use of personal protective equipment, the most skilled rescuer attempting tracheal intubation, the use of a video laryngoscope to be considered whenever possible, and supraglottal airway devices use if tracheal intubation is not possible. This study showed a decrease in endotracheal intubation during the COVID-19 pandemic, with an increase in the use of supraglottal airway devices. While guidelines do not suggest avoiding intubation, some regions had protocols that prioritized the use of supraglottal airway devices (34, 51, 67). Rapid transport without intubation has also been recommended in some studies (73). The risk of infection during intubation may not be significantly higher when wearing personal protective equipment, but endotracheal intubation may have been avoided at front-line rescue sites due to a lack of studies on the risk of infection during intubation in the early stages of the pandemic.
The regional subgroup analyses, excluding Asia, showed no significant difference in CPR using mechanical CPR devices during the COVID-19 pandemic. A total of ten studies were included in the analysis of CPR using mechanical CPR devices, with six studies showing significant results. Among them, a significant increase in CPR with mechanical CPR devices during the COVID-19 pandemic was reported in three studies (34, 57, 71), and a significant decrease was reported in the other studies (13, 78, 98). Talikowska et al. noted that the increase in the number of patients who stopped CPR in the field could be explained by the desire to follow local protocols, and a decrease in the number of people who required CPR using mechanical CPR devices (78). The two studies by Baldi et al. did not provide a specific explanation; however, there was no significant difference in the interruption of rescue by paramedics, and therefore, an explanation due to other factors is needed (13, 98). Even before the COVID-19 pandemic, the region had a relatively low rate of CPR applications using mechanical CPR devices compared with other regions. However, the number of samples was small, and it is possible that these results were due to problems with the distribution of automatic CPR devices or the adaptation of field crews. The American Heart Association and the European Resuscitation Committee recommend CPR using mechanical CPR devices to minimize the risk of infection during CPR (95–97). Furthermore, the Korean Society of Emergency Medicine recommends CPR using a mechanical CPR device if possible (99). In Asia, including the Republic of Korea, these guidelines may have been well reflected, suggesting an increase in CPR using mechanical CPR devices. Over the duration of the study, Ahn et al. suggested that CPR was performed before these guidelines were issued, but regional protocols reflected these aspects in advance (34). In the Republic of Korea, the continuous supply of mechanical CPR devices since 2014 and the ability of paramedics to use mechanical CPR devices without medical guidance may have led to an increase in CPR using mechanical CPR devices due to the ease of reflecting the above guidelines (57).
During the COVID-19 pandemic, an increase in the number of OHCA and the influx of OHCA in people with COVID-19 could be expected to have an impact on the rate of targeted body temperature treatment; however, the results of this analysis did not show a significant difference. There are no guidelines for targeted body temperature treatment for patients with confirmed or suspected COVID-19, but since droplets are generally not produced during the process of targeted body temperature treatment, it appears that front-line medical staff actively implemented targeted body temperature treatment in consideration of the benefits of the treatment. The frequency of percutaneous coronary intervention reported by Ahn et al., Riyapan et al., and Phattharapornjaroen et al. and the frequency of emergency coronary angiography reported by Sultanian et al. did not show significant differences before and during the COVID-19 pandemic. Therefore, it can be assumed that the impact of the COVID-19 pandemic on the hospital-stage treatments of OHCA patients may be low; however, interpretation is limited because meta-analyses were not performed due to the small number of studies (34, 71, 73, 76).
The following limitations of this review need to be noted. First, there was a lack of information about underlying conditions, such as patients’ medical history or cerebral performance category (CPC) scores before cardiac arrest, resulting in confounding bias. Second, this study did not differentiate between confirmed and non-confirmed COVID-19 cases. Since COVID-19 cases can be a factor in cardiac arrest, the failure to analyze these studies without differentiating them may cause biases when comparing the COVID-19 pandemic period to the previous period. Third, this review was based on data from 16 countries and did not include studies from Africa and South America. In addition, the European studies focused on Western European countries, and the North American and other studies only included studies conducted in the United States and Australia. These limitations make it difficult to generalize the results of this study to races and countries worldwide. Fourth, this study conducted a meta-analysis considering the timing of the epidemic and the epidemic region as factors that influenced the pattern of the COVID-19 pandemic. In addition, the introduction of COVID-19 vaccines and major virus subvariants may have significantly changed the pandemic pattern, but none of the included studies conducted a meta-analysis on this topic. Finally, this is a systematic review and meta-analysis based on previously published non-randomized controlled studies and has a limited ability to reflect overall trends. Additionally, insignificant or negative research results are not always published, which can lead to bias.
The COVID-19 pandemic has had a significant impact on the epidemiology and outcomes of OHCA patients. This review identified changes, such as an increase in cardiac arrests at home, a decrease in the use of AED, a decrease in endotracheal intubation, and an increase in the use of supraglottal airway devices. Unlike previous reviews, we noted a decrease in shockable rhythms. The impact of the pandemic on OHCA patients varied regionally, likely due to differences in health systems and resources. Some countries showed no significant differences in OHCA survival and neurological prognosis compared to before the pandemic, possibly due to a less explosive increase in COVID-19 cases and the absence of a complete collapse of the emergency medical care system. In the event of future infectious disease pandemics, the experiences and lessons learned globally from the pandemic will enable early recognition of factors that can negatively impact OHCA survival, improving the prognosis for OHCA patients and the effectiveness of the response.
JK and CA developed the concept and drafted the manuscript. JK, CA, and YP performed the data analysis. JK and MW performed data acquisition. CA and YP performed the statistical analysis. All authors contributed to the article and approved the submitted version.
Corredpondence (CA) have been supported by National Research Foundation of Korea (NRF) grant that was funded by the Korean Government (MSIT; 2021R1G1A1091336).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1180511/full#supplementary-material
AED, automated external defibrillator; CI, confidence interval; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest; OR, odds ratio; ROSC, return of spontaneous circulation; TTM, target temperature management.
1. Yan, S, Gan, Y, Jiang, N, Wang, R, Chen, Y, Luo, Z, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. (2020) 24:61. doi: 10.1186/s13054-020-2773-2
2. Tsao, CW, Aday, AW, Almarzooq, ZI, Alonso, A, Beaton, AZ, Bittencourt, MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. (2022) 145:e153–639. doi: 10.1161/CIR.0000000000001052
3. Berdowski, J, Berg, RA, Tijssen, JG, and Koster, RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. (2010) 81:1479–87. doi: 10.1016/j.resuscitation.2010.08.006
4. Luc, G, Baert, V, Escutnaire, J, Genin, M, Vilhelm, C, Di Pompéo, C, et al. Epidemiology of out-of-hospital cardiac arrest: a French national incidence and mid-term survival rate study. Anaesth Crit Care Pain Med. (2019) 38:131–5. doi: 10.1016/j.accpm.2018.04.006
5. Xu, F, Zhang, Y, and Chen, Y. Cardiopulmonary resuscitation training in China: current situation and future development. JAMA Cardiol. (2017) 2:469–70. doi: 10.1001/jamacardio.2017.0035
6. Korea Centers for Disease Control and Prevention. (2020) Sudden cardiac arrest survey statistics (2022). Available at: https://www.kdca.go.kr/injury/biz/injury/recsroom/statsSmMain.do (Accessed March 5, 2023).
7. Nishiyama, C, Kiguchi, T, Okubo, M, Alihodžić, H, Al-Araji, R, Baldi, E, et al. Three-year trends in out-of-hospital cardiac arrest across the world: second report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. (2023) 186:109757. doi: 10.1016/j.resuscitation.2023.10975
8. Ong, MEH, Perkins, GD, and Cariou, A. Out-of-hospital cardiac arrest: prehospital management. Lancet. (2018) 391:980–8. doi: 10.1016/S0140-6736(18)30316-7
9. Gräsner, JT, Herlitz, J, Tjelmeland, IBM, Wnent, J, Masterson, S, Lilja, G, et al. European resuscitation council guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. (2021) 161:61–79. doi: 10.1016/j.resuscitation.2021.02.007
10. Panchal, AR, Bartos, JA, Cabañas, JG, Donnino, MW, Drennan, IR, Hirsch, KG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2020) 142:S366–468. doi: 10.1161/CIR.0000000000000916
11. World Health Organization. Director-General’s opening remarks at the media briefing on COVID-19. (2020). Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-mediabriefing-on-covid-19---11-march-2020 (Accessed November 29, 2022).
12. World Health Organization. Coronavirus (COVID-19) dashboard. (2022). Available at: https://covid19.who.int/ (Accessed October 12, 2022).
13. Baldi, E, Sechi, GM, Mare, C, Canevari, F, Brancaglione, A, Primi, R, et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. (2020) 41:3045–54. doi: 10.1093/eurheartj/ehaa508
14. De Rosa, S, Spaccarotella, C, Basso, C, Calabrò, MP, Curcio, A, Filardi, PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. (2020) 41:2083–8. doi: 10.1093/eurheartj/ehaa409
15. Tejada Meza, H, Lambea Gil, Á, Saldaña, AS, Martínez-Zabaleta, M, Juez, PR, Martínez, EL, et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in north-west Spain. Int J Stroke. (2020) 15:755–62. doi: 10.1177/1747493020938301
16. Fallani, G, Lombardi, R, Masetti, M, Chisari, M, Zanini, N, Cattaneo, GM, et al. Urgent and emergency surgery for secondary peritonitis during the COVID-19 outbreak: an unseen burden of a healthcare crisis. Updat Surg. (2021) 73:753–62. doi: 10.1007/s13304-020-00943-y
17. Kim, JH, Ahn, C, and Namgung, M. Comparative evaluation of the prognosis of septic shock patients from before to after the onset of the COVID-19 pandemic: a retrospective single-center clinical analysis. J Pers Med. (2022) 12:103. doi: 10.3390/jpm12010103
18. Sung, CW, Lu, TC, Fang, CC, Huang, CH, Chen, WJ, Chen, SC, et al. Impact of COVID-19 pandemic on emergency department services acuity and possible collateral damage. Resuscitation. (2020) 153:185–6. doi: 10.1016/j.resuscitation.2020.06.021
19. Kim, JH, Ahn, C, and Namgung, M. Epidemiology and outcome of out-of-hospital cardiac arrests during the COVID-19 pandemic in South Korea: a systematic review and meta-analyses. Yonsei Med J. (2022) 63:1121–9. doi: 10.3349/ymj.2022.0339
20. Lim, ZJ, Ponnapa Reddy, M, Afroz, A, Billah, B, Shekar, K, and Subramaniam, A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: a systematic review and meta-analysis. Resuscitation. (2020) 157:248–58. doi: 10.1016/j.resuscitation.2020.10.025
21. Masuda, Y, Teoh, SE, Yeo, JW, Tan, DJH, Jimian, DL, Lim, SL, et al. Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: a systematic review and meta-analysis. Sci Rep. (2022) 12:800. doi: 10.1038/s41598-021-04749-9
22. Teoh, SE, Masuda, Y, Tan, DJH, Liu, N, Morrison, LJ, Ong, MEH, et al. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: a systematic review and meta-analysis. Ann Intensive Care. (2021) 11:169. doi: 10.1186/s13613-021-00957-8
23. Bielski, K, Szarpak, A, Jaguszewski, MJ, Kopiec, T, Smereka, J, Gasecka, A, et al. The influence of COVID-19 on out-hospital cardiac arrest survival outcomes: an updated systematic review and meta-analysis. J Clin Med. (2021) 10:5573. doi: 10.3390/jcm10235573
24. Chung, HS, Lee, DE, Kim, JK, Yeo, IH, Kim, C, Park, J, et al. Revised triage and surveillance protocols for temporary emergency department closures in tertiary hospitals as a response to COVID-19 crisis in Daegu Metropolitan City. J Korean Med Sci. (2020) 35:e189. doi: 10.3346/jkms.2020.35.e189
25. Kaushik, M, Agarwal, D, and Gupta, AK. Cross-sectional study on the role of public awareness in preventing the spread of COVID-19 outbreak in India. Postgrad Med J. (2021) 97:777–81. doi: 10.1136/postgradmedj-2020-138349
26. Liberati, A, Altman, DG, Tetzlaff, J, Mulrow, C, Gøtzsche, PC, Ioannidis, JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
27. Wan, X, Wang, W, Liu, J, and Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
28. Sterne, JA, Hernán, MA, Reeves, BC, Savović, J, Berkman, ND, Viswanathan, M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
29. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
30. Saito, S, Asai, Y, Matsunaga, N, Hayakawa, K, Terada, M, Ohtsu, H, et al. First and second COVID-19 waves in Japan: a comparison of disease severity and characteristics. J Infect. (2021) 82:84–123. doi: 10.1016/j.jinf.2020.10.033
31. Rajatanavin, N, Tuangratananon, T, Suphanchaimat, R, and Tangcharoensathien, V. Responding to the COVID-19 second wave in Thailand by diversifying and adapting lessons from the first wave. BMJ Glob Health. (2021) 6:e006178. doi: 10.1136/bmjgh-2021-006178
32. Oladunjoye, O, Gallagher, M, Wasser, T, Oladunjoye, A, Paladugu, S, and Donato, A. Mortality due to COVID-19 infection: a comparison of first and second waves. J Community Hosp Intern Med Perspect. (2021) 11:747–52. doi: 10.1080/20009666.2021.1978154
33. Dorrucci, M, Minelli, G, Boros, S, Manno, V, Prati, S, Battaglini, M, et al. Excess mortality in Italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Front Public Health. (2021) 9:669209. doi: 10.3389/fpubh.2021.669209
34. Ahn, JY, Ryoo, HW, Cho, JW, Kim, JH, Lee, SH, and Jang, TC. Impact of the COVID-19 outbreak on adult out-of-hospital cardiac arrest outcomes in Daegu, South Korea: an observational study. Clin Exp Emerg Med. (2021) 8:137–44. doi: 10.15441/ceem.21.008
35. Baert, V, Jaeger, D, Hubert, H, Lascarrou, JB, Debaty, G, Chouihed, T, et al. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: registry-based study. Scand J Trauma Resusc Emerg Med. (2020) 28:119. doi: 10.1186/s13049-020-00813-x
36. Baldi, E, Auricchio, A, Klersy, C, Burkart, R, Benvenuti, C, Vanetta, C, et al. Out-of-hospital cardiac arrests and mortality in Swiss cantons with high and low COVID-19 incidence: a nationwide analysis. Resusc Plus. (2021) 6:100105. doi: 10.1016/j.resplu.2021.100105
37. Baldi, E, Caputo, ML, Auricchio, A, Vanetta, C, Cresta, R, and Benvenuti, C. A quantitative assessment of the contribution of “citizen first responder” in the adult out-of-hospital chain of survival during COVID-19 pandemic. Resuscitation. (2021) 166:41–2. doi: 10.1016/j.resuscitation.2021.07.024
38. Baldi, E, Sechi, GM, Mare, C, Canevari, F, Brancaglione, A, Primi, R, et al. Treatment of out-of-hospital cardiac arrest in the COVID-19 era: a 100 days experience from the Lombardy region. PLoS One. (2020) 15:e0241028. doi: 10.1371/journal.pone.0241028
39. Ball, J, Nehme, Z, Bernard, S, Stub, D, Stephenson, M, and Smith, K. Collateral damage: hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. (2020) 156:157–63. doi: 10.1016/j.resuscitation.2020.09.017
40. Biskupski, P, Heraud, SO, Khalil, M, Horoub, A, Maqsood, M, Ong, K, et al. Out-of-hospital cardiac arrest before and during the COVID-19 pandemic in the South Bronx. medRxiv (2022). doi: 10.1101/2022.06.08.22276169
41. Burns, TA, Touzeau, C, Kaufman, BT, Butsch, AL, Vesselinov, R, and Stone, RM. Decreases in out of hospital cardiac arrest (OHCA) outcome metrics persist when known COVID patients are excluded from analysis. Am J Emerg Med. (2022) 51:64–8. doi: 10.1016/j.ajem.2021.09.083
42. Chan, PS, Girotra, S, Tang, Y, Al-Araji, R, Nallamothu, BK, and McNally, B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. (2021) 6:296–303. doi: 10.1001/jamacardio.2020.6210
43. Chavez, S, Huebinger, R, Chan, HK, Gill, J, White, L, Mendez, D, et al. The impact of COVID-19 on incidence and outcomes from out-of-hospital cardiac arrest (OHCA) in Texas. Am J Emerg Med. (2022) 57:1–5. doi: 10.1016/j.ajem.2022.04.006
44. Cho, JW, Jung, H, Lee, MJ, Lee, SH, Lee, SH, Mun, YH, et al. Preparedness of personal protective equipment and implementation of new CPR strategies for patients with out-of-hospital cardiac arrest in the COVID-19 era. Resusc Plus. (2020) 3:100015. doi: 10.1016/j.resplu.2020.100015
45. Chung, H, Namgung, M, Lee, DH, Choi, YH, and Bae, SJ. Effect of delayed transport on clinical outcomes among patients with cardiac arrest during the coronavirus disease 2019 pandemic. Australas Emerg Care. (2021) 25:241–6. doi: 10.1016/j.auec.2021.11.006
46. Coute, RA, Nathanson, BH, Kurz, MC, and Mader, TJ, CARES Surveillance Group. Estimating the impact of the COVID-19 pandemic on out-of-hospital cardiac arrest burden of disease in the United States. J Am Coll Emerg Physicians Open. (2022) 3:e12811. doi: 10.1002/emp2.12811
47. Damjanovic, D, Pooth, J-S, Steger, R, Boeker, M, Steger, M, Ganter, J, et al. Observational study on implications of the COVID-19-pandemic for cardiopulmonary resuscitation in out-of-hospital cardiac arrest: qualitative and quantitative insights from a model region in Germany. BMC Emerg Med. (2022) 22:85. doi: 10.1186/s12873-022-00628-2
48. de Koning, ER, Boogers, MJ, Bosch, J, de Visser, M, Schalij, MJ, and Beeres, SLMA. Emergency medical services evaluations for chest pain during first COVID-19 lockdown in Hollands-Midden, the Netherlands. Neth Heart J. (2021) 29:224–9. doi: 10.1007/s12471-021-01545-y
49. Elmer, J, Okubo, M, Guyette, FX, and Martin-Gill, C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. (2020) 156:282–3. doi: 10.1016/j.resuscitation.2020.08.127
50. Fothergill, RT, Smith, AL, Wrigley, F, and Perkins, GD. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc Plus. (2021) 5:100066. doi: 10.1016/j.resplu.2020.100066
51. Glober, NK, Supples, M, Faris, G, Arkins, T, Christopher, S, Fulks, T, et al. Out-of-hospital cardiac arrest volumes and characteristics during the COVID-19 pandemic. Am J Emerg Med. (2021) 48:191–7. doi: 10.1016/j.ajem.2021.04.072
52. Grübl, T, Plöger, B, Sassen, MC, Jerrentrup, A, Schieffer, B, and Betz, S. Out-of-hospital cardiac arrest during lockdown: effects of the infection prevention measures during the first wave of SARS-CoV-2 pandemic. Notf Rett Med. (2021) 24:1, 1–6. German, 6. doi: 10.1007/s10049-021-00932-7
53. Hosomi, S, Zha, L, Kiyohara, K, Kitamura, T, Irisawa, T, Ogura, H, et al. Survival following an out-of-hospital cardiac arrest in Japan in 2020 versus 2019 according to the cause. Acute Med Surg. (2022) 9:e777. doi: 10.1002/ams2.777
54. Kandori, K, Okada, Y, Ishii, W, Narumiya, H, and Iizuka, R. Evaluation of a revised resuscitation protocol for out-of-hospital cardiac arrest patients due to COVID-19 safety protocols: a single-center retrospective study in Japan. Sci Rep. (2021) 11:12985. doi: 10.1038/s41598-021-92415-5
55. Lai, PH, Prezant, DJ, Lancet, EA, Weiden, MD, Webber, MP, Zeig-Owens, R, et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. (2020) 5:1154–63. doi: 10.1001/jamacardio.2020.2488
56. Lee, N-J, Yang, J-C, and Moon, J-d. Collateral damage of emergency medical services due to COVID-19. Korean J Emerg Med Serv. (2021) 25:189–200. doi: 10.14408/KJEMS.2021.25.3.189
57. Lim, D, Park, SY, Choi, B, Kim, SH, Ryu, JH, Kim, YH, et al. The comparison of emergency medical service responses to and outcomes of out-of-hospital cardiac arrest before and during the COVID-19 pandemic in an area of Korea. J Korean Med Sci. (2021) 36:e255. doi: 10.3346/jkms.2021.36.e255
58. Lim, KT, Ahn, KO, Park, JH, Park, CH, Lim, J, and Lee, K. Bystander cardiopulmonary resuscitation in public locations before and after the coronavirus disease 2019 pandemic in the Republic of Korea. Am J Emerg Med. (2022) 56:271–4. doi: 10.1016/j.ajem.2021.07.012
59. Lim, SL, Kumar, L, Saffari, SE, Shahidah, N, Al-Araji, R, Ng, QX, et al. Management of out-of-hospital cardiac arrest during COVID-19: a tale of two cities. J Clin Med. (2022) 11:5177. doi: 10.3390/jcm11175177
60. Lim, SL, Shahidah, N, Saffari, SE, Ng, QX, Ho, AFW, Leong, BSH, et al. Impact of COVID-19 on out-of-hospital cardiac arrest in Singapore. Int J Environ Res Public Health. (2021) 18:3646. doi: 10.3390/ijerph18073646
61. Marijon, E, Karam, N, Jost, D, Perrot, D, Frattini, B, Derkenne, C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. (2020) 5:e437–43. doi: 10.1016/S2468-2667(20)30117-1
62. Mathew, S, Harrison, N, Chalek, AD, Gorelick, D, Brennan, E, Wise, S, et al. Effects of the COVID-19 pandemic on out-of-hospital cardiac arrest care in Detroit. Am J Emerg Med. (2021) 46:90–6. doi: 10.1016/j.ajem.2021.03.025
63. Navalpotro-Pascual, J-M, Monge-Martín, D, González-León, M-J, Neria, F, Peinado-Vallejo, F, Alonso-Blas, C, et al. Impact of different waves of COVID-19 on emergency medical services and out-of-hospital cardiopulmonary arrest in Madrid, Spain. Res Sq. (2021). doi: 10.21203/rs.3.rs-944651/v1
64. Navalpotro-Pascual, JM, Pérez, CF, Vallejo, FAP, Moya, AC, Cuesta, YM, Isabel, BM, et al. Caseload and cardiopulmonary arrest management by an out-of-hospital emergency service during the COVID-19 pandemic. Emergencias. (2021) 33:100–6. Spanish.
65. Ng, QX, Lee, EZH, Tay, JAM, and Arulanandam, S. Impact of COVID-19 ‘circuit-breaker’ measures on emergency medical services utilisation and out-of-hospital cardiac arrest outcomes in Singapore. Emerg Med Australas. (2021) 33:149–51. doi: 10.1111/1742-6723.13668
66. Nickles, AV, Oostema, A, Allen, J, O’Brien, SL, Demel, SL, and Reeves, MJ. Comparison of out-of-hospital cardiac arrests and fatalities in the metro Detroit area during the COVID-19 pandemic with previous-year events. JAMA Netw Open. (2021) 4:4. doi: 10.1001/jamanetworkopen.2020.32331
67. Nishiyama, C, Kiyohara, K, Iwami, T, Hayashida, S, Kiguchi, T, Matsuyama, T, et al. Influence of COVID-19 pandemic on bystander interventions, emergency medical service activities, and patient outcomes in out-of-hospital cardiac arrest in Osaka City, Japan. Resusc Plus. (2021) 5:100088. doi: 10.1016/j.resplu.2021.100088
68. Nishiyama, C, Kiyohara, K, Kitamura, T, Hayashida, S, Maeda, T, Kiguchi, T, et al. Impact of the COVID-19 pandemic on prehospital intervention and survival of patients with out-of-hospital cardiac arrest in Osaka City, Japan. Circ J. (2022) 86:1579–85. doi: 10.1253/circj.CJ-22-0040
69. Ortiz, F, Fernández del Valle, P, Knox, EC, Jiménez Fábrega, X, Navalpotro Pascual, JM, Mateo Rodríguez, I, et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. (2020) 157:230–40. doi: 10.1016/j.resuscitation.2020.09.037
70. Paoli, A, Brischigliaro, L, Scquizzato, T, Favaretto, A, and Spagna, A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the province of Padua, Northeast Italy. Resuscitation. (2020) 154:47–9. doi: 10.1016/j.resuscitation.2020.06.031
71. Phattharapornjaroen, P, Nimnuan, W, Sanguanwit, P, Atiksawedparit, P, Phontabtim, M, and Mankong, Y. Characteristics and outcomes of out-of-hospital cardiac arrest patients before and during the COVID-19 pandemic in Thailand. Int J Emerg Med. (2022) 15:46. doi: 10.1186/s12245-022-00444-2
72. Ristau, P, Wnent, J, Gräsner, J-T, Fischer, M, Bohn, A, Bein, B, et al. Impact of COVID-19 on out-of-hospital cardiac arrest: a registry-based cohort-study from the German resuscitation registry. PLoS One. (2022) 17:e0274314. doi: 10.1371/journal.pone.0274314
73. Riyapan, S, Chantanakomes, J, Roongsaenthong, P, Tianwibool, P, Wittayachamnankul, B, Supasaovapak, J, et al. Impact of the COVID-19 outbreak on out-of-hospital cardiac arrest management and outcomes in a low-resource emergency medical service system: a perspective from Thailand. Int J Emerg Med. (2022) 15:26. doi: 10.1186/s12245-022-00429-1
74. Sayre, MR, Barnard, LM, Counts, CR, Drucker, CJ, Kudenchuk, PJ, Rea, TD, et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander cardiopulmonary resuscitation. Circulation. (2020) 142:507–9. doi: 10.1161/CIRCULATIONAHA.120.048951
75. Semeraro, F, Gamberini, L, Tartaglione, M, Iarussi, B, Descovich, C, Picoco, C, et al. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: system response to preserve performances. Resuscitation. (2020) 157:1–2. doi: 10.1016/j.resuscitation.2020.09.032
76. Sultanian, P, Lundgren, P, Strömsöe, A, Aune, S, Bergström, G, Hagberg, E, et al. Cardiac arrest in COVID-19: characteristics and outcomes of in-and out-of-hospital cardiac arrest. A report from the Swedish registry for cardiopulmonary resuscitation. Eur Heart J. (2021) 42:1094–106. doi: 10.1093/eurheartj/ehaa1067
77. Sun, C, Dyer, S, Salvia, J, Segal, L, and Levi, R. Worse cardiac arrest outcomes during the COVID-19 pandemic in Boston can be attributed to patient reluctance to seek care. Health Aff. (2021) 40:886–95. doi: 10.1377/hlthaff.2021.00250
78. Talikowska, M, Ball, S, Tohira, H, Bailey, P, Rose, D, Brink, D, et al. No apparent effect of the COVID-19 pandemic on out-of-hospital cardiac arrest incidence and outcome in Western Australia. Resusc Plus. (2021) 8:100183. doi: 10.1016/j.resplu.2021.100183
79. Uy-Evanado, A, Chugh, HS, Sargsyan, A, Nakamura, K, Mariani, R, Hadduck, K, et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol. (2021) 7:6–11. doi: 10.1016/j.jacep.2020.08.010
80. Yu, JH, Liu, CY, Chen, WK, Yu, SH, Huang, FW, Yang, MT, et al. Impact of the COVID-19 pandemic on emergency medical service response to out-of-hospital cardiac arrests in Taiwan: a retrospective observational study. Emerg Med J. (2021) 38:679–84. doi: 10.1136/emermed-2020-210409
81. Bharmal, M, DiGrande, K, Patel, A, Shavelle, DM, and Bosson, N. Impact of coronavirus disease 2019 pandemic on cardiac arrest and emergency care. Heart Fail Clin. (2023) 19:231–40. doi: 10.1016/j.hfc.2022.08.009
82. Ippolito, M, Catalisano, G, Marino, C, Fucà, R, Giarratano, A, Baldi, E, et al. Mortality after in-hospital cardiac arrest in patients with COVID-19: a systematic review and meta-analysis. Resuscitation. (2021) 164:122–9. doi: 10.1016/j.resuscitation.2021.04.025
83. Poissy, J, Goutay, J, Caplan, M, Parmentier, E, Duburcq, T, Lassalle, F, et al. Pulmonary embolism in patients with COVID-19: awareness of an increased prevalence. Circulation. (2020) 142:184–6. doi: 10.1161/CIRCULATIONAHA.120.047430
84. Siripanthong, B, Nazarian, S, Muser, D, Deo, R, Santangeli, P, Khanji, MY, et al. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. (2020) 17:1463–71. doi: 10.1016/j.hrthm.2020.05.001
85. Rozanova, L, Temerev, A, and Flahault, A. Comparing the scope and efficacy of COVID-19 response strategies in 16 countries: an overview. Int J Environ Res Public Health. (2020) 17:9421. doi: 10.3390/ijerph17249421
86. Chen, H, Shi, L, Zhang, Y, Wang, X, Jiao, J, Yang, M, et al. Response to the COVID-19 pandemic: comparison of strategies in six countries. Front Public Health. (2021) 9:708496. doi: 10.3389/fpubh.2021.708496
87. Lau, LL, Hung, N, and Wilson, K. COVID-19 response strategies: considering inequalities between and within countries. Int J Equity Health. (2020) 19:137. doi: 10.1186/s12939-020-01254-9
88. Cha, V. Asia’s COVID-19 lessons for the west: public goods, privacy, and social tagging. Wash Q. (2020) 43:1–18. doi: 10.1080/0163660X.2020.1770959
89. Lu, N, Cheng, KW, Qamar, N, Huang, KC, and Johnson, JA. Weathering COVID-19 storm: successful control measures of five Asian countries. Am J Infect Control. (2020) 48:851–2. doi: 10.1016/j.ajic.2020.04.021
90. Thu, TPB, Ngoc, PNH, Hai, NM, and Tuan, LA. Effect of the social distancing measures on the spread of COVID-19 in 10 highly infected countries. Sci Total Environ. (2020) 742:140430. doi: 10.1016/j.scitotenv.2020.140430
91. Leung, KHB, Alam, R, Brooks, SC, and Chan, TCY. Public defibrillator accessibility and mobility trends during the COVID-19 pandemic in Canada. Resuscitation. (2021) 162:329–33. doi: 10.1016/j.resuscitation.2021.01.008
92. Grunau, B, Bal, J, Scheuermeyer, F, Guh, D, Dainty, KN, Helmer, J, et al. Bystanders are less willing to resuscitate out-of-hospital cardiac arrest victims during the COVID-19 pandemic. Resusc Plus. (2020) 4:100034. doi: 10.1016/j.resplu.2020.100034
93. Howell, S, Nehme, Z, Eastwood, K, Battaglia, T, Buttery, A, and Bray, J. The impact of COVID-19 on the Australian public’s willingness to perform hands-only CPR. Resuscitation. (2021) 163:26–7. doi: 10.1016/j.resuscitation.2021.03.034
94. Data OWi. (2022). Case fatality rate of COVID-19. Available at: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-03-14.2020-12-29&facet=none&pickerSort=asc&pickerMetric=location&hideControls=true&Interval=Cumulative&Relative+to+Population=false&Color+by+test+positivity=tr (Accessed November 30, 2022).
95. Perkins, GD, Morley, PT, Nolan, JP, Soar, J, Berg, K, Olasveengen, T, et al. International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. (2020) 151:145–7. doi: 10.1016/j.resuscitation.2020.04.035
96. Edelson, DP, Sasson, C, Chan, PS, Atkins, DL, Aziz, K, Becker, LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. (2020) 141:e933–43. doi: 10.1161/CIRCULATIONAHA.120.047463
97. Nolan, JP, Monsieurs, KG, Bossaert, L, Böttiger, BW, Greif, R, Lott, C, et al. European resuscitation council COVID-19 guidelines executive summary. Resuscitation. (2020) 153:45–55. doi: 10.1016/j.resuscitation.2020.06.001
98. Baldi, E, Sechi, GM, Mare, C, Canevari, F, Brancaglione, A, Primi, R, et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. (2020) 383:496–8. doi: 10.1056/NEJMc2010418
99. Korean Society of Emergency Medicine. (2020). Recommendations of in-hospital CPR for COVID-19 Available at: https://emergency.or.kr/bbs/notice/2108 (Accessed November 30, 2022).
Keywords: out-of-hospital cardiac arrest, COVID-19, meta-analysis, survival, epidemioloy
Citation: Kim JH, Ahn C, Park Y and Won M (2023) Comparison of out-of-hospital cardiac arrests during the COVID-19 pandemic with those before the pandemic: an updated systematic review and meta-analysis. Front. Public Health. 11:1180511. doi: 10.3389/fpubh.2023.1180511
Received: 06 March 2023; Accepted: 11 April 2023;
Published: 04 May 2023.
Edited by:
Simone Savastano, San Matteo Hospital Foundation (IRCCS), ItalyReviewed by:
Enrico Baldi, San Matteo Hospital Foundation (IRCCS), ItalyCopyright © 2023 Kim, Ahn, Park and Won. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiwon Ahn, Y2FobkBjYXUuYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.