
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 26 June 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1179755
 Julan Xiao1,2
Julan Xiao1,2 Lili Liu3
Lili Liu3 Yueming Peng2,4
Yueming Peng2,4 Yi Wen1,2
Yi Wen1,2 Xia Lv2,5
Xia Lv2,5 Lijun Liang2,4
Lijun Liang2,4 Yi Fan2,4
Yi Fan2,4 Jie Chen2,6
Jie Chen2,6 Yanru Chen2,7
Yanru Chen2,7 Hongying Hu2,4
Hongying Hu2,4 Weisi Peng2,4
Weisi Peng2,4 Haiyan Wang2,4
Haiyan Wang2,4 Weixiang Luo2,4*
Weixiang Luo2,4*Introduction: Frontline nurses fighting against the epidemic were under great psychological stress. However, there is a lack of studies assessing the prevalence rates of anxiety, depression, and insomnia among frontline nurses after the full liberalization of COVID-19 in China. This study demonstrates the impact of the full liberalization of COVID-19 on the psychological issues and the prevalence rate and associated factors of depressive symptoms, anxiety, and insomnia among frontline nurses.
Methods: A total of 1766 frontline nurses completed a self-reported online questionnaire by convenience sampling. The survey included six main sections: the 9-item Patient Health Questionnaire (PHQ-9), the 7-item Generalized Anxiety Disorder (GAD-7), the 7-item Insomnia Severity Index (ISI), the 10-item Perceived Stress Scale (PSS-10), sociodemographic information, and work information. Multiple logistic regression analyses were applied to identify the potential significantly associated factors for psychological issues. The study methods were compliant with the STROBE checklist.
Results: 90.83% of frontline nurses were infected with COVID-19, and 33.64% had to work while infected COVID-19. The overall prevalence of depressive symptoms, anxiety and insomnia among frontline nurses was 69.20%, 62.51%, and 76.78%, respectively. Multiple logistic analyses revealed that job satisfaction, attitude toward the current pandemic management, and perceived stress were associated with depressive symptoms, anxiety, and insomnia.
Conclusions: This study highlighted that frontline nurses were suffering from varying degrees of depressive symptoms, anxiety, and insomnia during full liberalization of COVID-19. Early detection of mental health issues and preventive and promotive interventions should be implemented according to the associated factors to prevent a more serious psychological impact on frontline nurses.
Coronavirus disease 2019 (COVID-19) is a rapidly spreading disease with high infectivity and high morbidity and mortality rates worldwide caused by severe acute respiratory syndrome-novel coronavirus-2 (SARS-CoV-2) (1). The pandemic has caused a global threat to health and life. By the end of April 2020, approximately 90,000 health care workers worldwide were infected, and more than 600 nurses died (2). As such, nurses who care for COVID-19 patients are at a high risk of infection. To combat COVID-19, in affected countries such as China, measures have been implemented to prevent the spread of the virus, such as quarantine, daily nucleic acid testing, temperature screening and screening of patients with COVID-19, and setting up fever clinics and isolation units in many hospitals (3). On December 27, 2022, the National Health Commission of the People's Republic of China issued a circular on further optimizing prevention and control measures against COVID-19 and suddenly adopted a policy of full liberalization, called daily nucleic acid testing or temperature screening of patients with COVID-19 infection. In a very short time, most people, whether they were medical staff or the general population, were infected. There was a lack of preparation for defeating COVID-19 due to sudden full liberalization, and nurses faced challenges and difficulties such as the huge increase in the number of critically ill COVID-19 patients. Many nurses were infected and had to work while ill, and nursing work stress increased. Nurses were physically and psychologically exhausted from intensive, heavy workloads and long-term usage of personal protective equipment (4, 5).
Nurses consitute the largest proportion of hospital health care professionals (6), spend more time caring for patients than other health care workers, and play an essential role in the treatment, care, and control of patients during disease outbreaks, disasters, and emergency situations (5, 7). In addition, nurses have the closest proximity to COVID-19 patients worldwide. Previous research has shown that frontline health care providers have a high risk of mental health conditions during the COVID-19 pandemic, mainly fear, anxiety, depression, and insomnia. Approximately 91.2% of 1,837 nurses working in Wuhan, China, showed fear of infection and death as well as fear of nosocomial spreading to their loved ones (8). A systematic review and meta-analysis of global health care professionals showed that the pooled prevalence of psychological problems for anxiety, depression, and distress was 40%, 37%, and 37%, respectively (9). A cross-sectional study reported that the prevalence of anxiety, depression, insomnia, and nonspecific distress symptoms in Chinese frontline health care workers was 44.6%, 50.4%, 34.0%, and 71.5%, respectively (10). Therefore, it is necessary to pay special attention to the psychological health of frontline nurses.
Nurses were at the forefront of defeating the pandemic and were therefore at risk of developing high levels of stress and physical and psychological depletion. They were affected by a variety of stressors in their workplaces because they were confronted with a complex psychological conflict between their responsibility, dedication, and mission as nurses to provide health and care for patients with a very dangerous virus and their right to protect themselves from the virus (8, 11). After the sudden full liberalization of COVID-19, nurses experienced acute and exacerbated stress (e.g., more COVID-19 patients, direct exposure to diseases, longer workload and work shifts, and high rates of infection by COVID-19), whereas there was a shortage of resources (e.g., a lack of protective equipment, insufficient facilities, insufficient nursing staff, lack of training or experience in caring for seriously ill COVID-19 patients) (12). In a systematic review of the psychology of frontline health care staff caring for COVID-19 patients, the prevalence of stress was 45% (13). Stress is the most common issue and an integral part of human life. Hospital staff in charge of admitting and directly caring for COVID-19 patients were subjected to pressure that adversely impacted their health and job satisfaction (13). Stress can increase anxiety and depression, jeopardize physical, mental, and social health, and even lead to suicidal thoughts (14). More importantly, poor psychological health among nurses not only has been linked to negative outcomes such as psychological distress, depression, anxiety, and burnout but also hinders professional performance, in turn leading to the deterioration of the quality of patients' care (12). Thus, frontline nurses should maintain excellent physical and psychological health.
Nurses working during the global pandemic were physically and psychologically exhausted and experienced severe anxiety, depression, and stress. However, there is a lack of studies exploring anxiety, depression, perceived stress, and sleep disorders among nurses during the sudden full liberalization of COVID-19 in China. In particular, most medical staffs were also infected during this specific period. In addition to psychological health problems, some physical symptoms and manifestations of the virus, such as pain, fatigue, cough, expectoration, sore throat, and weakness, caused additional workload to health care systems.
This study aims to determine the prevalence rates of anxiety, depression, and insomnia among frontline nurses during the full liberalization of COVID-19 in Shenzhen, China, and to explore significantly associated factors and protective measures to provide a theoretical basis for the early identification and intervention of negative emotions for these professionals. We hypothesize that perceived stress, job satisfaction, turnover intention, attitude toward current pandemic management, and perceived health status are associated with the risk of depression, anxiety, and insomnia. To our knowledge, this is the first study to determine the prevalence of mental health issues after the full liberalization of COVID-19. Consequently, our study will make a positive contribution to the literature on organizing preventive mental health services and help plan emergency responses to future infectious disease outbreaks.
This was a multicenter cross-sectional study conducted from December 27, 2022, to January 7, 2023, in six tertiary hospitals in Shenzhen. Convenience sampling was used for the recruitment strategy, and 1,833 nurses volunteered to participate. The online questionnaire was shared via “Wenjuan Xing,” a professional questionnaire survey platform that is widely used in China (15). The online survey was first disseminated through an instant messaging system, the WeChat group, to nursing managers at Shenzhen hospitals, who were encouraged to pass it on to other frontline nurses at Shenzhen hospitals. The inclusion criteria for participants were as follows: (1) nurses aged 18 and above; (2) normal language expression and understanding and the ability to understand the investigation content and cooperate with the research; and (3) the ability to give voluntary informed consent. The exclusion criteria were (1) history of mental illness and (2) serious physical diseases. Screening criteria included a response time of fewer than 200 s (16) to complete the survey and the deletion of incomplete or repeated answers. The target simple size of participants was determined using the formula N = P(1 – P)/d2, in which α = 0.05 and Zα = 1.96, and the estimated acceptable margin of error for proportion d was 3%. The proportion of health care professionals with psychological comorbidities was estimated at 40%, based on a previous study of COVID-19 outbreak (9). Given the 35% attrition rate, the final sample size calculation of at least 1,333 completed questionnaires from participants. While reviewing the participants' data, 67 nurses completed the questionnaire in <200 s or had missing data. In total, 1,766 frontline nurses completed the questionnaire (response rate of 96.34%).
This study was conducted in Shenzhen, which is one of the highest-income cities in China. All investigators received unified training on the questionnaire survey. The unified guidance on the questionnaire explained the purpose and completion method of this research. Each question was a mandatory item and could only be answered once by the same IP address. In addition, the nurses were told that the survey could be stopped at any time, and anonymity would be guaranteed. The online questionnaire began with informed consent. Frontline nurses needed to read the informed consent and chose the “agree” option to begin filling out the questionnaire; otherwise, the questionnaire could not be completed. To test the feasibility and suitability of the questionnaire, online pilot test including 15 frontline nurses was conducted. The nurses who participated were also asked for advice on questionnaire modification. Pilot test data were not used for the final statistics. The trained authors of this article distributed the final version of the questionnaires to the frontline nurses for data collection.
A general information questionnaire (created by the authors in line with the literature) included two parts. The first part collected data on the participants' gender, age, educational background, working years, marital status, income per year, staff type, professional technical titles, night shifts per month, hospital type, and hospital department. The second part included job satisfaction, turnover intention, COVID-19 vaccination status, infection with COVID-19, working status, and compared with the outbreak period, the attitude toward the current epidemic.
The 10-item Perceived Stress Scale (PSS-10) is based on the theory of psychological stress and was developed in 1983 by Cohen et al. (17). The PSS-10 is used to measure how stressful an individual perceives events in daily life. The scale has previously shown good reliability and validity (17). The PSS-10 is a 10-item self-report scale; six items measure crisis perception and four items measure coping ability. Each item is rated on a 5-point Likert-type scale ranging from 0 indicating “never” to 4 indicating “very often.” The total score on the PSS-10 ranges from 0 to 40. Higher scores indicate that the individual's perceived stress level is high. In the current study, the Cronbach's alpha for the PSS-10 was 0.72, the Guttman Split-Half Coefficient was 0.88.
The severity of depression was assessed using the 9-item Patient Health Questionnaire (PHQ-9), which is a self-report validated screening instrument for use among patients and general populations. The questionnaire is based on the nine symptoms of depression in the US Diagnostic Standard for Mental Illness (DSM-IV) (18). Participants rate their experiences in the past 2 weeks, scoring each item from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day). Total scores on the PHQ-9 range from 0 (not at all) to 27 (extremely severe depression) (19), the higher the score, the more obvious the state of depression. Regarding severity, PHQ-9 comprises five categories as follows: minimal/no depression (0–4), mild depression (5–9), moderate depression (10–14), or severe depression (15–21) (20). In our study, the Cronbach's alpha for the PHQ-9 was 0.93.
We used the 7-item Generalized Anxiety Disorder (GAD-7) to evaluate the severity of anxiety, which is a self-rated scale with good reliability and validity (21). Each item was scored based on a 4-point Likert scale, where 0 and 3 points indicated “never” and “almost every day,” respectively. Higher scores indicated higher exposure to anxiety. The total scores are categorized as follows: minimal/no anxiety (0–4), mild anxiety (5–9), moderate anxiety (10–14), or severe anxiety (15–21). Cronbach's alpha in the present study was 0.97.
The 7-item Insomnia Severity Index (ISI) was used to evaluate the severity of insomnia in the past week. The ISI is a measure of insomnia severity that has been shown to be valid and reliable. The total scores are categorized as follows: normal (0–7), subthreshold (8–14), moderate insomnia (15–21), or severe insomnia (22–28) (22). Cronbach's alpha of the scale was 0.93 in this study.
Data were analyzed with SPSS version 26.0. Descriptive statistics, including frequencies and central tendencies, were calculated to characterize the sample's demographic profile. Binary and multiple logistic regression analyses were performed to explore the potential factors influencing depression, anxiety and insomnia after the sudden full liberalization of COVID-19. Perceived stress was divided into four groups using quartiles, indicating the position of the score in the sample. The first quartile was 0–25%, the second was 25%−50%, the third was 50%−75%, and the fourth was 75%−100%. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were obtained from the logistic regression models. P < 0.05 was considered statistically significant.
This study was in line with ethical principles, and the contents of the questionnaire didn't involve private and sensitive topics such as names. More importantly, the research was approved by the ethics committee of Shenzhen People's Hospital (Approval No. LL-KY-2022004-01). All samples were given information about introducing the study and notified about their own right to withdraw at any time, and informed consent was sought from all eligible participants, which illustrated that they had understood the study in its entirety.
The demographic characteristics of the 1,766 participants are summarized in Table 1. Most of the participants (n = 1,694, 95.92%) were female, and the majority (n = 1,342, 75.99%) were younger than 40 years of age. A total of 30.81% (n = 544) of respondents had <5 years of work experience, while 45.36% (n = 801) reported working in hospitals for more than 10 years. A total of 81.99% (n = 1,448) of the sample were employed as contract staff with a primary title (n = 1,092, 61.83%). More than half of the nurses (n = 1,000, 56.63%) were married.
Regarding the characteristics of the nurses' working situations, 30.69% (n = 542) of nurses had no night shifts, while 13.59% (n = 240) had 11 or more night shifts per month. The majority (n = 1,476, 83.58%) stated that they worked in general hospitals. Among the frontline nurses, 4.3% (n = 76) worked in the emergency department and 3.34% (n = 59) in the intensive care unit (ICU); 48.47% (n = 856) were satisfied with their current nursing work, and only 16.54% (n = 292) were not satisfied with their work. Furthermore, 37.66% (n = 665) had turnover intentions. Overall, 90.83% (n = 1,604) were infected with COVID-19, and 33.64% (n = 594) had to work while infected COVID-19, while 68.74% (n = 1,214) did not accept their return to duty as soon as a fever was not present after infection.
The prevalence rates of depression, anxiety, and insomnia in the survey sample are shown in Table 2. The overall prevalence of depressive symptoms, anxiety and insomnia among frontline nurses was 69.20%, 62.51%, and 76.78%, respectively. Specifically, the participants indicated mild (n = 538, 30.46%), moderate (n = 352, 19.93%), and severe (n = 332, 18.80%) depressive symptoms. Similarly, the participants reported mild (n = 637, 36.07%), moderate (n = 143, 8.10%), and severe (n = 324, 18.35%) anxiety. The majority of the nurses reported mild (n = 745, 42.19%) and moderate (n = 443, 25.08%) insomnia (Figure 1).
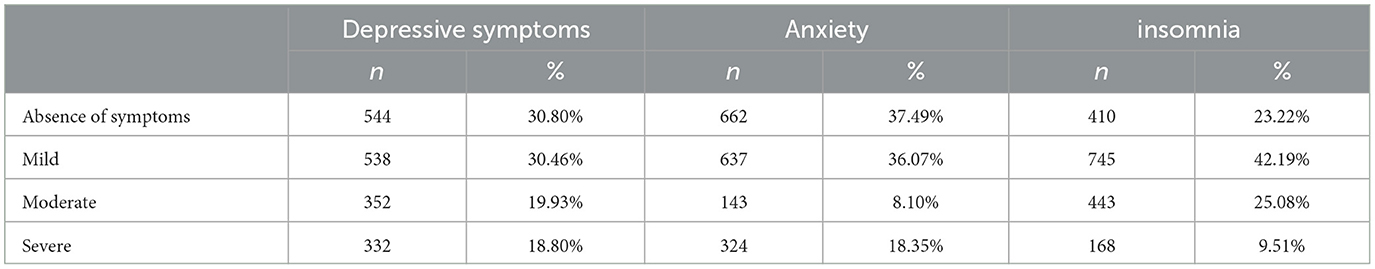
Table 2. Prevalence of depressive symptoms, anxiety and insomnia among nurses during the early open up phase of the COVID-19 pandemic.
The results from the binary logistic regression analysis are presented in Table 3. Nurses with a primary technical title and intermediate nurses had a higher level of depression than those with a senior title. Nurses who were single (OR, 1.58; 95% CI, 1.12–2.22), had 11 or more night shifts per month (OR, 1.70; 95% CI, 1.08–2.67), had turnover intentions (OR, 1.69; 95% CI, 1.29–2.21) were at greater risk of depression. Nurses were dissatisfied or had neutral satisfaction with their current nursing work were at greater risk of depression than those who were satisfied. A negative attitude toward the current pandemic management and nurses with higher total PSS-10 scores also had a higher risk of depression.
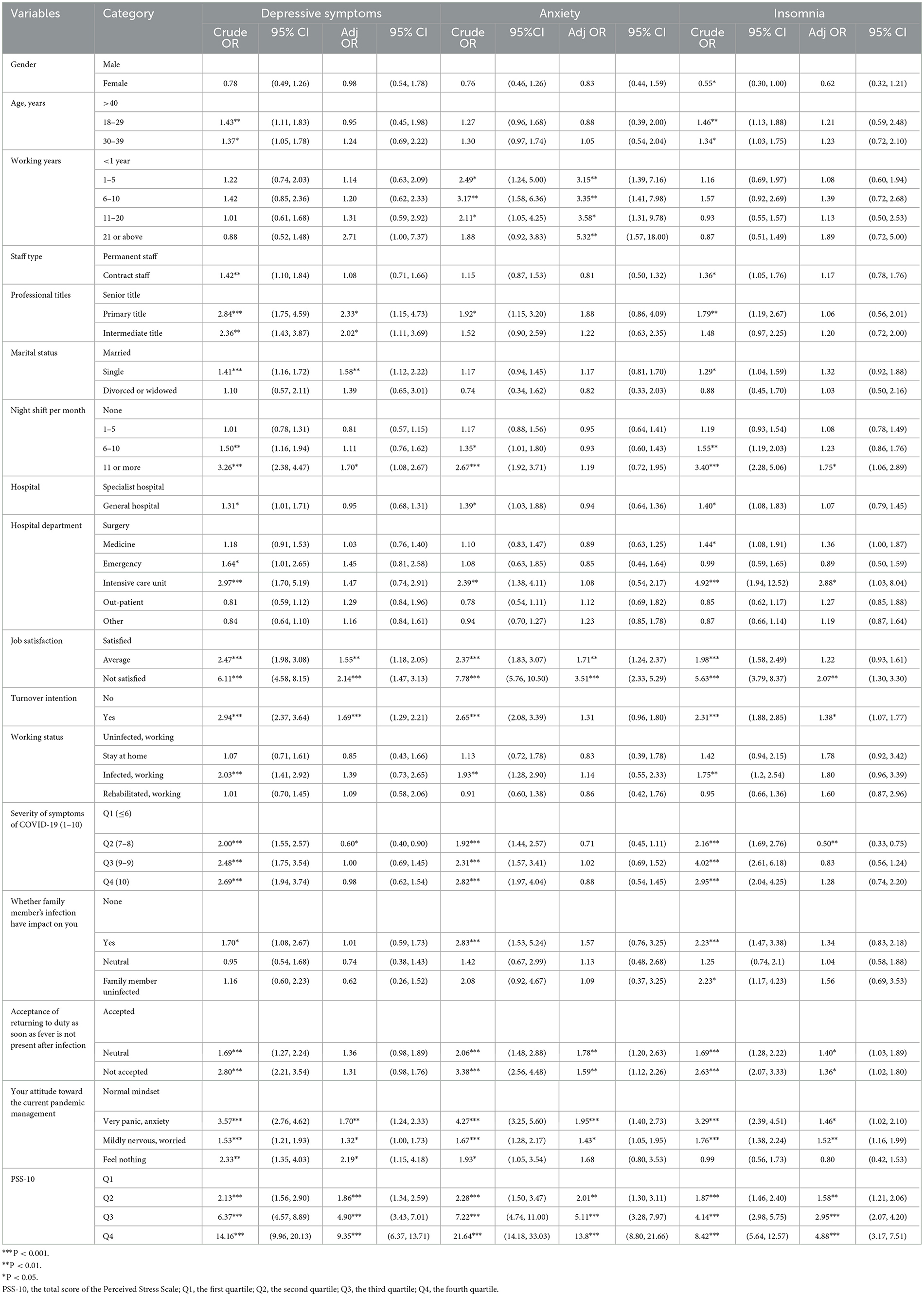
Table 3. Binary logistic regression analysis of the factors associated with depressive symptoms, anxiety and insomnia.
Longer working years increased the risk of anxiety. Nurses who were dissatisfied (OR, 3.51; 95% CI, 2.33–5.29) and average (OR, 1.71; 95% CI, 1.24–2.37) with their current nursing work had a higher level of anxiety than those who were satisfied. Those who had a lack of acceptance (OR, 1.59; 95% CI, 1.12–2.26) or felt neutral (OR, 1.78; 95% CI, 1.20–2.63) about returning to duty as soon as fever was not present after infection were also at greater risk of anxiety than those who accepted this. A negative attitude toward the current pandemic management and nurses with higher total PSS-10 scores also had an increased risk of anxiety (Table 3).
The factor significantly associated with insomnia was turnover intention (OR, 1.38; 95% CI, 1.07–1.77). Nurses with 11 or more night shifts per month (OR, 1.75; 95% CI, 1.06–2.89) were at greater risk of developing insomnia than those without night shifts. The insomnia risk was higher among those working in the ICU (OR, 2.88; 95% CI, 1.03–8.04). Nurses who were dissatisfied (OR, 2.07; 95% CI, 1.30–3.30) with their current work had a higher level of insomnia than those who were satisfied. Nurses who did not accept (OR, 1.36; 95% CI, 1.02–1.80) or felt neutral (OR, 1.40; 95% CI, 1.03–1.89) about returning to duty as soon as fever was not present after infection also had a higher level of insomnia than those who accepted this. A negative attitude toward the current pandemic management and nurses with higher total PSS-10 scores also had a higher risk of insomnia (Table 3).
To the best of our knowledge, the current study represents the first attempt to examine frontline nurses' epidemiology and correlates of psychological health during the full liberalization of COVID-19 in China using a multicenter large-scale cross-sectional design. The strengths of this survey included the multicentered sampling, the large sample size, and the use of standardized evaluation tools for depression, anxiety, perceived stress and insomnia. We conducted our research in six hospitals with large-scale treatment of COVID-19 patients, which made our sample relatively representative of frontline nurses.
In this study, it was determined that the majority of respondents were female, were aged <40 years, were married, had bachelor's degrees, worked in general hospitals with a primary technical title, and had a working period between 1 and 20 years. Moreover, the present study identified certain independent significantly associated factors associated with depressive symptoms, anxiety, and insomnia among China frontline nurses. Our research was conducted during the critical period of full liberalization of the pandemic in China, from the COVID-19 pandemic in December 2019 to the current stage in January 2023, which was China's first phase of comprehensive epidemic liberalization. Moreover, the study targeted participants in Shenzhen, China, which is a large population and high-income region in China. Consequently, our findings might have certain implications and reference value for frontline nurses in regions and countries currently experiencing the full liberalization of COVID-19.
Our study revealed that a significantly high proportion of frontline nurses were afflicted with depressive symptoms (69.20%), anxiety (62.51%), and insomnia (76.78%). In the survey, ~38.73% nurses showed moderate to severe depressive symptoms, 26.45% had moderate to severe anxiety, and 34.59% had moderate to severe insomnia. Frontline nurses revealed more severe psychological symptoms on all measurements.
Most previous studies concentrated on nurses' psychological health at the early stage of the COVID-19 pandemic, when the psychological impacts of COVID-19 on nurses were already apparent. A cross-sectional study using the same scales as our study demonstrated that the prevalence of depression, anxiety, and insomnia among frontline health care workers in China exposed to COVID-19 was 50.4%, 44.6%, and 34.0% (10), respectively, which was lower than that in the present study. Approximately 43.61% of frontline nurses in emergency departments treating COVID-19 patients experienced depression (23). In research during the severe acute respiratory syndrome (SARS) outbreak, a previous infectious disease, 38.5% of nurses working in high-risk situations showed psychological symptoms (24). Compared to the Singapore and India study populations during the COVID-19 outbreak, our cohort showed a higher prevalence rate of moderate to severe depressive symptoms (38.73 vs. 5.30%) and anxiety (26.45 vs. 8.72%) (25). However, compared to the previous Chinese study population, our research indicated a higher prevalence rate of depressive symptoms (38.73 vs. 16.51%) and a slightly lower rate of anxiety (26.45 vs. 28.83%) (26). A systematic review, meta-analysis and meta regression of subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic confirmed that all the countries reported significant sleep impairment and subclinical insomnia, except for Asia (27). Indeed, the reason may be that these countries registered the highest number of deaths from COVID-19 in the world. Previous research hypothesized that countries with a more severe pandemic situation showed greater levels of stress that may impact on sleep quality (28), which may explain that a significantly high proportion of Chinese frontline nurses were afflicted with insomnia (76.78%) during the full liberalization of COVID-19. Thus, public health emergencies, whether SARS or COVID-19, lead to a strong psychological impact on health care professionals, especially frontline nurses (29). However, compared with these findings, the incidence of depressive symptoms, anxiety, and insomnia in frontline nurses in our study was particularly high. This phenomenon may be attributed to the stage of sudden full liberalization control of COVID-19, which caused a rapid increase in admissions and presentations to hospitals and consequently increased the workload of nurses. In addition, nurses working as frontline health care professionals who had direct involvement with COVID-19 patients were an independent significantly associated factor for all psychological health symptoms (10). Overall, 90.83% of frontline nurses in our study were infected with COVID-19, and 33.64% had to work with COVID-19-infected patients. A previous study demonstrated that the most commonly reported physical symptoms of COVID-19 were headache (31.90%), throat pain (33.55%), anxiety (26.71%), lethargy (26.60%), and insomnia (20.97%) (25). There is a bidirectional significant association between the prevalence of physical symptoms and psychological issues, where uncomfortable physical symptoms exacerbate psychological issues and vice versa (25). Furthermore, despite being infected with COVID-19, frontline nurses still have to work, which poses a threat to their mental health. Among all health care professionals, frontline nurses have been the main force in fighting against public health crises and emergencies, and their psychological health is crucial. These results highlight the requirement for early identification and the significance of effectively assessing and treating milder or moderate symptoms before they turn into more severe and complex mental health issues.
This study revealed that frontline nurses with primary or intermediate technical titles had a higher level of depression than those with senior technical titles, which agrees with previous findings (10). A possible contributing factor was that 61.83% of frontline nurses had primary technical titles and 31.94% had intermediate titles, indicating that many nurses had fewer years of work experience (10), and particularly lacked experience caring for COVID-19 patients and critically ill patients, compared with seniors. Another possible reason may be that nurses with lower technical titles had increased odds of mental health issues and PTSD during the period of caring for the sharply increasing number of positive patients (15). Therefore, this population should be given special attention to reduce depressive symptoms.
Our results indicated that depressive symptoms and insomnia were related to night shifts per month; frontline nurses with 11 or more night shifts per month were more likely to develop depressive symptoms and insomnia than those without night shifts. Some previous studies have demonstrated that rotating night shift work may produce circadian disruption, sleep disturbances, and health behavioral changes (30), resulting in an increased risk of chronic diseases (31, 32) psychological disorders (33), cognition impairment and mortality (34). Excess night shift work is a significant health concern that may result in the deteriorating overall health of frontline nurses (35), which may explain why frequently rotating night shift work was associated with more depression and insomnia during the special period of full liberalization control of COVID-19.
This study showed that turnover intention, job satisfaction, current working status, attitude toward current pandemic management, and perceived stress scores were associated with frontline nurses' depression, anxiety, and insomnia. During the full liberalization control of COVID-19, frontline nurses, who made enormous efforts by risking their lives in emergency departments, intensive isolation units, intensive care units, and COVID-19 patient wards, demonstrated their commitment and responsibility to their profession and their patients. Nurses who treated COVID-19-positive patients tended to be exposed to the highest risk of virus infection due to their close, frequent contact with patients and intensive work. Nurses constantly suffer from stressful situations that lead to emotional exhaustion while managing the complex care and treatment processes of COVID-19 patients. Particularly during the special period of full liberalization control of COVID-19, working for a long time in a hectic environment with a high level of stress and increasing workload caused nurses to experience burnout more rapidly (36). Moreover, the incompatibility between the ideal expectations of the nursing profession and the situations encountered in real life gives rise to turnover intention and dissatisfaction with current nursing work (37). The number of nurses reporting turnover intention was notably higher in nurses assigned to COVID-19 hospitals than in those assigned to non-COVID-19 hospitals (38, 39). Nurses who were at greater risk of being infected were more likely to quit their job and the profession (40). This result is in accordance with international studies which shown that caring for infected patients itself may significantly contribute to negative emotions and psychological distress, leading to reduced job satisfaction and increased turnover (41). The long duration of uncertainty during sudden public events such as emergencies and/or disasters also affects the stress level of individuals (36).
Our study highlighted that higher stress levels were a significantly associated factor that influenced nurses' mental health. The acceptance of returning to duty as soon as a high fever was not present after infection was an essential significantly associated factor associated with anxiety and insomnia. This finding was consistent with previous studies (15). Frontline nurses constantly face a number of work-related stressors, including but not limited to heavy workloads, long work hours, meeting patients' requirements, and irregular working schedules (42). Previous studies have noted that the ongoing stress faced by these health care professionals can have negative effects on their psychological wellbeing (42), especially when they face a greater threat of public emergencies. It is widely understood that perceived stress is linked to psychological status; nurses who suffer from perceived stress are more inclined to develop depressive symptoms, anxiety, insomnia, and health-related concerns. Due to the large number of infection cases, frontline nurses worried about becoming infected through asymptomatic transmission (43), a lack of effective treatment, and stigmatization (44). In this study, 90.83% of frontline nurses were infected with COVID-19, and 33.64% had to work while infected COVID-19. It was confirmed that COVID-19 affects all human body systems physiopathologically, especially the immune and respiratory systems, which also results in negative psychological effects (45). Thus, during the health crises of full liberalization control of COVID-19, nurses may have had no fever and went to work after contracting the virus, but they may have had cough, sputum, and sore throat. Nurses who experienced physical discomfort due to COVID-19 might not have sufficient time to become better adjusted to caring for affected patients and may have become more concerned about personal and family health during full liberalization control.
Furthermore, the insomnia risk was higher among frontline nurses working in the ICU. The ICU is a constantly changing, highly regulated workplace for patients in critical situations. In addition, excessive workload, shift work, resuscitation and death are proven significantly associated factors for insomnia (46). Consistent with a previous study (10), our research revealed that longer working years increased the risk of anxiety, which was possibly related to the fact that nurses with longer working experience were routinely assigned to treat and care for more patients and/or more severe patients in hospitals in Shenzhen, further increasing their anxiety. Consequently, this population should be given special attention to reduce symptom severity.
This study has limitations in the generalization of the results. First, the cross-sectional nature of the study merely provided information at one time point and was unable to interpret causality. Second, the lack of follow-up data on frontline nurses' psychological health made it difficult to understand their mental health status over time. Third, the participants completed the questionnaires using the Wenjuanxing application and mobile devices, which might result in self-selection bias. Fourth, The study's sample was limited to six hospitals in Shenzhen, China. While this region represents a high-income and large population area, which may limit the generalizability of the findings to other contexts or time periods. Finally, the psychological variable measures in this study were based on a self-report questionnaire. Accordingly, longitudinal studies and prospective controlled studies are suggested for future studies to provide more in-depth and useful information about the psychological health of frontline nurses, both in China and in other parts of the world.
Our findings demonstrate that frontline nurses were suffering from varying degrees of depressive symptoms, anxiety, and insomnia during full liberalization of COVID-19. Job satisfaction, attitude toward current pandemic management, and perceived stress were associated with depressive symptoms, anxiety, and insomnia. Furthermore, frontline nurses with 11 or more night shifts per month and turnover intentions were associated with higher depressive symptoms and insomnia. Nurses who did not accept their return to duty as soon as high fever was not present after infection were associated with higher anxiety and insomnia. Therefore, it is essential for hospitals and health care institutions to implement early and effective psychosocial support and intervention for nurses to prevent the further impact of the full liberalization of COVID-19.
This is the first study to examine frontline nurses' epidemiology and correlates of psychological health during the full liberalization of COVID-19 in China using a multicenter, large-scale, cross-sectional design. This study highlighted that frontline nurses suffered from varying degrees of depressive symptoms, anxiety, and insomnia. Early screening and preventive and promotive interventions are required to prevent a more serious psychological impact on frontline nurses.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Shenzhen People's Hospital (Approval No. LL-KY-2022004-01). The patients/participants provided their written informed consent to participate in this study.
JX and WL designed and managed the study. LLiu, YP, and YW developed the methodology. XL, YF, LLia, JC, YC, HH, WP, and HW were responsible for the questionnaire survey of frontline nurses in Shenzhen and data acquisition. JX and LLiu analyzed the statistics. JX, WL, and LLiu wrote the first draft of the manuscript. All authors revised the manuscript, meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and read and approved the final manuscript.
This study was supported by the Shenzhen Peoples' Hospital and Young and Middle-aged Research Fund Project (grant number SYHL2021–N0006).
We are grateful to all the frontline nurses who took their time to participate in the study, especially those subjects who provided our study with essential information about their feelings, supporting us to complete the survey.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I. COVID-19 pandemia and public and global mental health from the perspective of global health securit. Psychiatr Danub. (2020) 32:6–14. doi: 10.24869/psyd.2020.6
2. Dawn News,. Fighting on the Front Line, at Least 253 Healthcare Workers Infected with Covid- 19 in Pakistan. (2020). Available online at: https://www.dawn.com/news/1551853/fighting-onthe-front-line-at-least-253-healthcare-workers-infected-with-covid-19-in-pakistan-so-far (acccessed January 14, 2023).
3. National Health Commission of the People's Republic of China. A Circular on Further Optimizing and Implementing the Prevention and Control Measures of the Novel Coronavirus Outbreak. (2023). Available online at: http://www.nhc.gov.cn/xcs/zhengcwj/202212/8278e7a7aee34e5bb378f0e0fc94e0f0.shtml (acccessed January 14, 2023).
4. Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. (2020) 8:e790–8. doi: 10.1016/S2214-109X(20)30204-7
5. Doo EY, Kim M, Lee S, Lee SY, Lee KY. Influence of anxiety and resilience on depression among hospital nurses: a comparison of nurses working with confirmed and suspected patients in the COVID-19 and non-COVID-19 units. J Clin Nurs. (2021) 30:1990–2000. doi: 10.1111/jocn.15752
6. United States Bureau of Labor Statistics. Occupational Outlook Handbook: Registered Nurses. (2023). Available online at: https://www.bls.gov/ooh/healthcare/registered-nurses.htm (acccessed January 15, 2023).
7. Labrague LJ, de Los Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. (2021) 29:395–403. doi: 10.1111/jonm.13168
8. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. (2020) 24:100424. doi: 10.1016/j.eclinm.2020.100424
9. Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
10. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
11. Kim Y. Nurses' experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control. (2018) 46:781–7. doi: 10.1016/j.ajic.2018.01.012
12. Lorente L, Vera M, Peiró T. Nurses' stressors and psychological distress during the COVID-19 pandemic: the mediating role of coping and resilience. J Adv Nurs. (2021) 77:1335–44. doi: 10.1111/jan.14695
13. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. doi: 10.1186/s12960-020-00544-1
14. Kapur N, Ibrahim S, While D, Baird A, Rodway C, Hunt IM, et al. Mental health service changes, organisational factors, and patient suicide in England in 1997-2012: a before-and-after study. Lancet Psychiatry. (2016) 3:526–34. doi: 10.1016/S2215-0366(16)00063-8
15. Zheng R, Zhou Y, Fu Y, Xiang Q, Cheng F, Chen H, et al. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: a cross-sectional study. Int J Nurs Stud. (2021) 114:103809. doi: 10.1016/j.ijnurstu.2020.103809
16. Trauzettel-Klosinski S, Dietz K, IReST Study Group. Standardized assessment of reading performance: the New International Reading Speed Texts IReST. Invest Ophthalmol Vis Sci. (2012) 53:5452–61. doi: 10.1167/iovs.11-8284
17. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
18. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders patient health questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
20. Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
21. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
22. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
23. An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. (2020) 276:312–5. doi: 10.1016/j.jad.2020.06.047
24. Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
25. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
26. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
27. Scarpelli S, Zagaria A, Ratti PL, Albano A, Fazio V, Musetti A, et al. Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: a systematic review, meta-analysis and meta-regression. Sleep Med. (2022) 100:89–102. doi: 10.1016/j.sleep.2022.07.012
28. Gardani M, Bradford DRR, Russell K, Allan S, Beattie L, Ellis JG, et al. A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Med Rev. (2022) 61:101565. doi: 10.1016/j.smrv.2021.101565
29. Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. (2020) 29:4217–26. doi: 10.1111/jocn.15454
30. Kervezee L, Kosmadopoulos A, Boivin DB. Metabolic and cardiovascular consequences of shift work: the role of circadian disruption and sleep disturbances. Eur J Neurosci. (2020) 51:396–412. doi: 10.1111/ejn.14216
31. Wu QJ, Sun H, Wen ZY, Zhang M, Wang HY, He XH, et al. Shift work and health outcomes: an umbrella review of systematic reviews and meta-analyses of epidemiological studies. J Clin Sleep Med. (2022) 18:653–62. doi: 10.5664/jcsm.9642
32. Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, et al. Association between rotating night shift work and risk of coronary heart disease among women. JAMA. (2016) 315:1726–34. doi: 10.1001/jama.2016.4454
33. Torquati L, Mielke GI, Brown WJ, Burton NW, Kolbe-Alexander TL. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health. (2019) 109:e13–20. doi: 10.2105/AJPH.2019.305278
34. Jørgensen JT, Karlsen S, Stayner L, Hansen J, Andersen ZJ. Shift work and overall and cause-specific mortality in the Danish nurse cohort. Scand J Work Environ Health. (2017) 43:117–26. doi: 10.5271/sjweh.3612
35. Shi H, Huang T, Schernhammer ES, Sun Q, Wang M. Rotating night shift work and healthy aging after 24 years of follow-up in the nurses' health study. JAMA Netw Open. (2022) 5:e2210450. doi: 10.1001/jamanetworkopen.2022.10450
36. Murat M, Köse S, Savaşer S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30:533–43. doi: 10.1111/inm.12818
37. Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. (2020) 123:9–20. doi: 10.1016/j.jpsychires.2019.12.015
38. Kim YJ, Lee SY, Cho JH. A study on the job retention intention of nurses based on social support in the Covid-19 situation. Sustainability. (2020) 12:7276. doi: 10.3390/su12187276
39. Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int. (2021) 28:8791–801. doi: 10.1007/s11356-020-11235-8
40. Goh YS, Ow Yong QYJ, Chen TH, Ho SHC, Chee YIC, Chee TT. The impact of COVID-19 on nurses working in a University Health System in Singapore: a qualitative descriptive study. Int J Ment Health Nurs. (2021) 30:643–52. doi: 10.1111/inm.12826
41. Lavoie-Tremblay M, Gélinas C, Aubé T, Tchouaket E, Tremblay D, Gagnon MP, et al. Influence of caring for COVID-19 patients on nurse's turnover, work satisfaction and quality of care. J Nurs Manag. (2022) 30:33–43. doi: 10.1111/jonm.13462
42. Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of australian nurses. Int J Environ Res Public Health. (2018) 16:61. doi: 10.3390/ijerph16010061
43. Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
44. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
45. Badahdah A, Khamis F, Al Mahyijari N, Al Balushi M, Al Hatmi H, Al Salmi I, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry. (2021) 67:90–5. doi: 10.1177/0020764020939596
Keywords: anxiety, depression, insomnia, nurses, full liberalization of COVID-19
Citation: Xiao J, Liu L, Peng Y, Wen Y, Lv X, Liang L, Fan Y, Chen J, Chen Y, Hu H, Peng W, Wang H and Luo W (2023) Anxiety, depression, and insomnia among nurses during the full liberalization of COVID-19: a multicenter cross-sectional analysis of the high-income region in China. Front. Public Health 11:1179755. doi: 10.3389/fpubh.2023.1179755
Received: 04 March 2023; Accepted: 01 June 2023;
Published: 26 June 2023.
Edited by:
Federico Salfi, University of L'Aquila, ItalyReviewed by:
Nida Zahid, Aga Khan University, PakistanCopyright © 2023 Xiao, Liu, Peng, Wen, Lv, Liang, Fan, Chen, Chen, Hu, Peng, Wang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weixiang Luo, bHVvd2VpeGlhbmc2ODhAMTI2LmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.