- 1Department of Cardiology, First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China
- 2Department of Emergency, The First Affiliated Hospital of Harbin Medical University, Harbin, China
- 3School of Computer Science and Technology, Harbin Institute of Technology, Harbin, China
- 4School of Information and Computer Engineering, Northeast Forestry University, Harbin, Heilongjiang, China
- 5School of Computer Science and Technology, Harbin Institute of Technology, Weihai, Shandong, China
- 6Department of Cardiology, Harbin Second Hospital, Harbin, China
- 7Department of Medical Record, The Second Affiliated Hospital of Harbin Medical University, Harbin, China
- 8Department of Obstetrics and Gynecology, First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China
Background: Air pollution and severe weather conditions can adversely affect cardiovascular disease emergencies. Nevertheless, it remains unclear whether air pollutants and low ambient temperature can trigger the occurrence of acute aortic dissection (AAD) in cold regions.
Methods: We applied a retrospective analysis to assess the short-term effects of air pollution and ambient temperature on the occurrence of AAD in Harbin, China. A total of 564 AAD patients were enrolled from a major hospital in Harbin between January 1, 2017, and February 5, 2021. Weather condition data and air pollutant concentrations, including fine particulate matter smaller than 10 μm (PM10) and 2.5 μm in diameter (PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), and ozone (O3), were collected every day. Conditional logistic regressions and correlation analysis were applied to analyze the relationship of environmental and atmospheric parameters with AAD occurrence at lags of 0 to 7 days. Specifically, we appraised the air quality index, CO, NO2, SO2, O3, PM10, PM2.5, temperature, dew point temperature, atmospheric pressure, and cloud amount.
Results: A total of 1,496 days at risk were assessed, of which 564 patients developed AAD. Specifically, AAD did not occur on 1,043 (69.72%) days, while 1 or more cases occurred on 453 (30.28%) days. Several pollution and weather predictors for AAD were confirmed by multilevel modeling. The air quality index (p = 0.0012), cloud amount (p = 0.0001), and concentrations of PM2.5 (p = 0.0004), PM10 (p = 0.0013), NO2 (p = 0.0007) and O3 (p = 0.0001) predicted AAD as early as 7 days before the incident (lag of 7 days) in the study period. However, only concentrations of the air pollutants NO2 (p = 0.0468) and O3 (p = 0.011) predicted the occurrence of AAD after the COVID-19 outbreak. Similar predictive effects were observed for temperature, dew point temperature, and atmospheric pressure (all p < 0.05) on all days.
Conclusion: The risk of AAD is closely related to air pollution and weather characteristics in Harbin. While causation was not determined, the impact of air pollutants on the risk of AAD was reduced after the COVID-19 outbreak.
Introduction
Acute aortic dissection (AAD) is the most common medical emergency in aortic diseases and is caused by tearing of the lining of the aorta. If left untreated, the mortality rate in the first 24 h after the onset of aortic dissection increases by 1 to 2% per hour (1, 2). According to the 2010 Global Burden of Disease (GBD) data, the total global mortality rate for aortic aneurysms and AAD increased by 0.29 per 100,000 from 1990 to 2010. Specifically, the mortality rate increased from 2.49 per 100,000 inhabitants to 2.78 per 100,000 inhabitants (3). Therefore, it is particularly important to ascertain potential risk factors for AAD to improve prevention. The public health relevance of a precipitating factor depends on two perspectives: the relative risk of the individual and the prevalence of the precipitating factor in the population (4). The relative risk factors of individuals for AAD include arterial hypertension, bicuspid aortic valve, coarctation of the aorta, and Turner syndrome (5–8). Although the relative risk of AAD is small for a given individual precipitating environmental factors can affect the entire population and have a major public health influence.
Studies have found that the incidence of AAD is significantly associated with the season and is highest in winter and lowest in summer (9–14). In addition, the incidence of AAD is higher in cold regions than in tropical regions. Such seasonal and regional differences indicate that ambient temperature and meteorological variables may be significant environmental risk factors for AAD (15). In addition, the independent and joint effects of ambient weather characteristics and pollution on subsequent AAD risk remain unclear (16, 17). To the best of our knowledge, no studies have examined ambient temperature and air pollutants as underlying risk factors for AAD. Additionally, few studies have assessed time-lag patterns of the impacts of temperature and air pollutants on the incidence of AAD at the individual level in cold regions. Such research could improve early intervention for AAD. Since the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, the global healthcare system has faced unprecedented challenges. COVID-19 has an important impact on the incidence, management and outcome of many cardiovascular diseases (18), among which AAD is a serious but underestimated problem (19). During the COVID-19 pandemic, it has been reported that the surgical volume of acute type A aortic dissection has decreased by 30% (20). A recent study has reported that the COVID-19 has significantly reduced the number of admissions to AAD throughout the year or part of the time, and the in-hospital mortality rate of AAD has increased compared with the pre-pandemic period (21). However, no studies have assessed the effects of population behavior on the occurrence of AAD after the COVID-19 outbreak in China.
Therefore, drawing on data from a regionwide registry in Northeast China, we aimed to determine the influence of meteorological factors, including ambient temperature and air pollutants, on the risk of AAD occurrence in a cold region. In this region, the heating period lasts for 6 months, and the minimum temperature in winter is even lower to −20°C, these conditions may heighten the risk of AAD in the days following particular pollutant and weather variations. Furthermore, the relevant factors for AAD before and after the COVID-19 outbreak would also be explored in this study.
Materials and methods
This was a retrospective analysis of anonymized data from the emergency department of the First Affiliated Hospital of Harbin Medical University, the largest heart disease center in Heilongjiang Province, China. Data were collected between January 1, 2017, and February 5, 2021. Specifically, patients with AAD were identified in a retrospective manner by examining hospital admission diagnosis records and surgical and echocardiographic databases. A diagnosis of AAD was verified through computed tomography with arterial contrast, magnetic resonance imaging, or echocardiography. All emergency admissions with a new episode of AAD met the eligibility criteria. The exclusion criteria were as follows: (1) traumatic AAD, (2) iatrogenic aortic disease secondary to previous cardiac surgery or interventional repair, (3) unidentified AAD with no evidence on multidetector computed tomography scans or echocardiography, (4) subacute and chronic aortic dissection, or (5) not living in this cold region. The numbers of daily AAD cases were entered in a database containing data on local weather and pollution acquired from the China Integrated Meteorological Information Service System (CIMISS), provided by the China Meteorological Data Service Center. These meteorological conditions and air pollutants data were sourced from 31 national meteorological observation stations within 200 kilometers around Harbin, including 2 base stations, 10 basic stations, and 19 general stations. All included patients lived in a cold region to minimize climatic variation among study regions. This study was approved by the Ethics Committee of the First Affiliated Hospital of Harbin Medical University, and the procedures were carried out according to the approved guidelines.
Data on the following environmental contaminants were systematically collected several times a day: fine particulate matter [i.e., with a mean aerodynamic diameter < 2.5 μm (PM2.5)] and particulate matter with a mean aerodynamic diameter ≥ 2.5 μm and < 10 μm (PM10), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), and ozone (O3). All concentrations are expressed as μm/m3. Data on these pollutants were collected every 3 h throughout the region and minimum, maximum, average, and change values were recorded. At the same time, we systematically collected the following weather characteristics: temperature (°C), dew point temperature, atmospheric pressure, and cloud amount. Similarly, we collected minimum, maximum, average, and variation values for all of the above weather characteristics (except cloud amount) every 3 h. Our explicit objective was to assess the impacts of pollution and weather characteristics on AAD occurrence on the same day as well as 1, 2, 3, 5, and 7 days later.
Categorical variables are presented as counts and percentages. Continuous variables are presented as the mean ± standard deviation as well as the median and quartiles. Binary logistic regression analyzes were used to determine odds ratios (ORs) and their 95% confidence intervals (CIs). The independent variables in logistic regression models included air quality index, PM2.5, PM10, sulfur dioxide, nitrogen dioxide, ozone, carbon monoxide, temperature, dew point temperature, atmospheric pressure, cloud amount. The effect of COVID-19 outbreak on the relationship between climate state and AAD occurrence was analyzed with interaction and stratified analysis by logistic regression models. We used a 4-knot restricted cubic spline (RCS) to flexibly simulate the correlations of temperature, PM2.5, and PM10 with AAD. The median of each measure was set as the reference. A p value <0.05 was considered statistically significant. Computations were performed with SAS 9.4 (SAS Inc., Cary, N.C., United States) and R 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
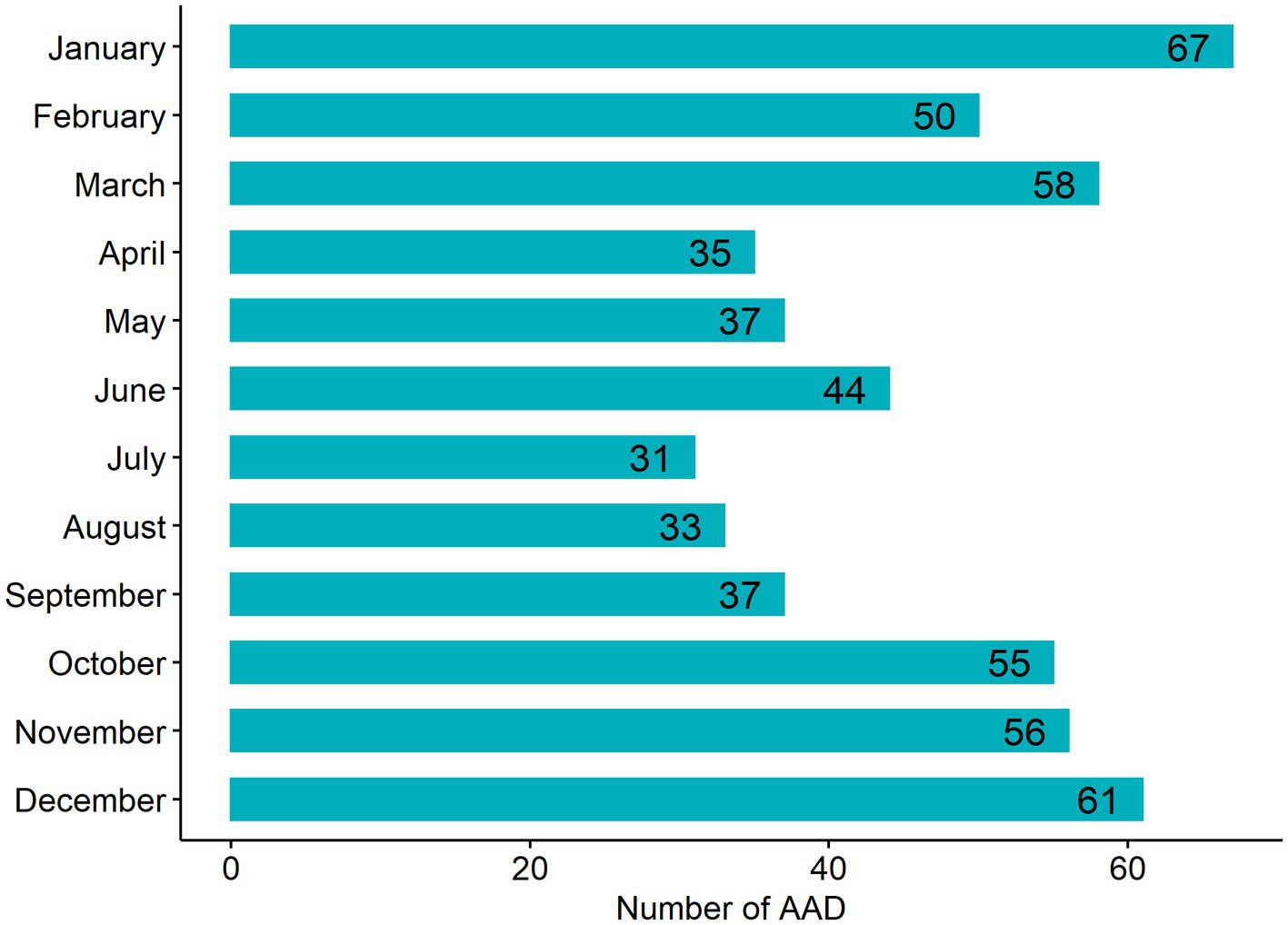
A total of 1,496 days of risk assessment were included, of which 564 cases (53.37% Stanford type A) of AAD were identified (Table 1). Specifically, there were 1,043 (69.72%) days without an AAD occurrence, 360 (24.06%) days with 1 case, 79 (5.28%) days with 2 cases, and 14 (0.94%) days with three or more cases. Descriptive analysis shows that the quartile variation is large, indicating substantial changes in pollution and weather characteristics. The numbers of AAD cases in each month from 2017 to 2021 in the cold region are shown in Figure 1. As shown in the figure, the AAD case numbers were relatively low in summer and relatively high in winter. In particular, the occurrence of AAD varied greatly between the indoor heating period and nonheating period in the cold region.
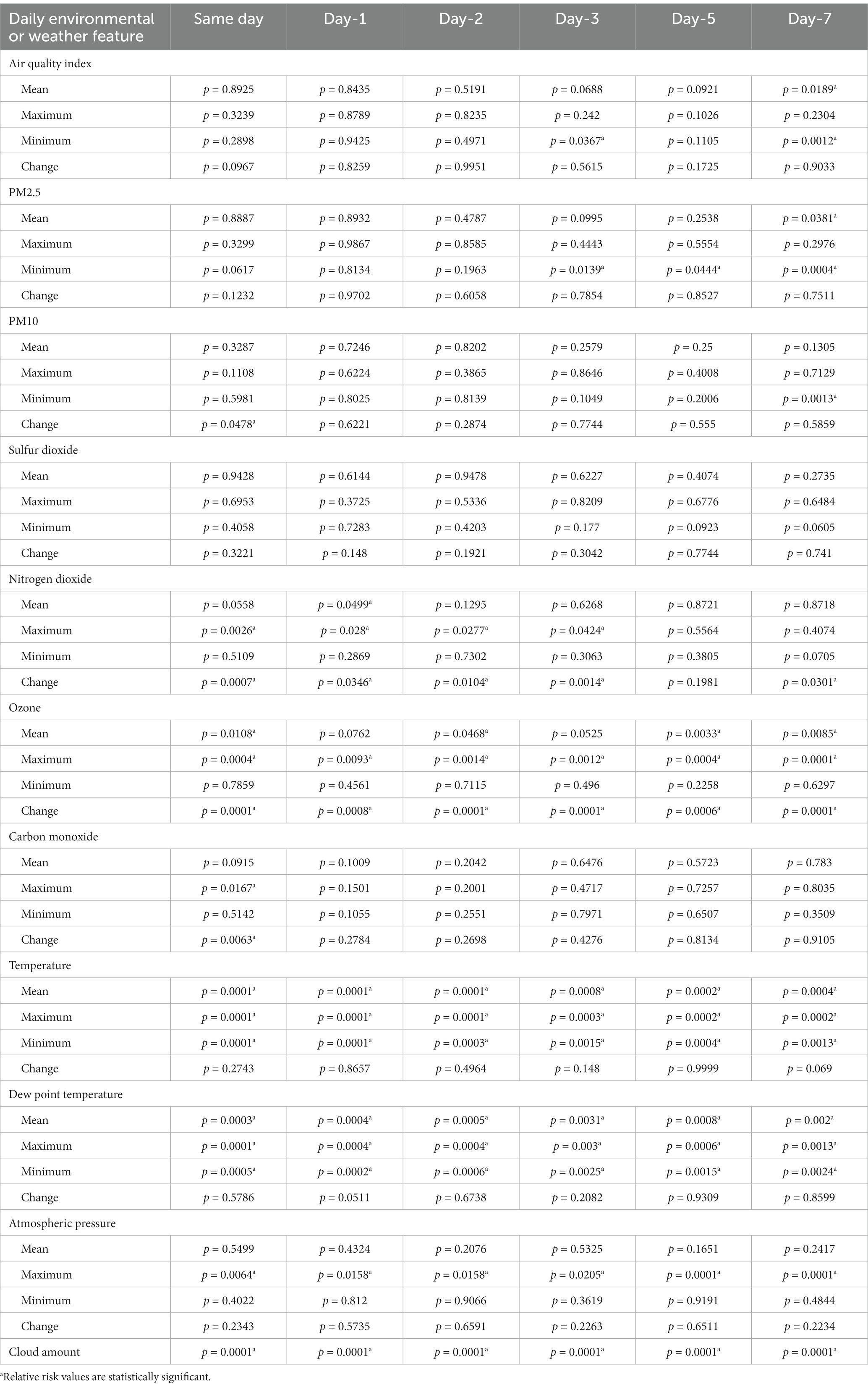
Logistic regression models were performed to identify several pollutants and weather characteristics associated with AAD occurrence (Table 2 and Figure 2). These predictors either originated on the same day or the days before AAD occurrence. The air quality index (p = 0.0012), cloud amount (p = 0.0001), and concentrations of PM2.5 (p = 0.0004), PM10 (p = 0.0013), NO2 (p = 0.0007) and O3 (p = 0.0001) predicted AAD occurrence at lags of 0 to 7 days. Similarly, temperature, dew point temperature, and atmospheric pressure (all p < 0.05) significantly predicted AAD occurrence. Notably, temperature, dew point temperature, and O3 were negatively correlated with the risk of AAD occurrence; days with low temperature, low dew point temperature, and low O3 concentration were associated with a higher risk of AAD occurrence at lags of 0 to 7 days.
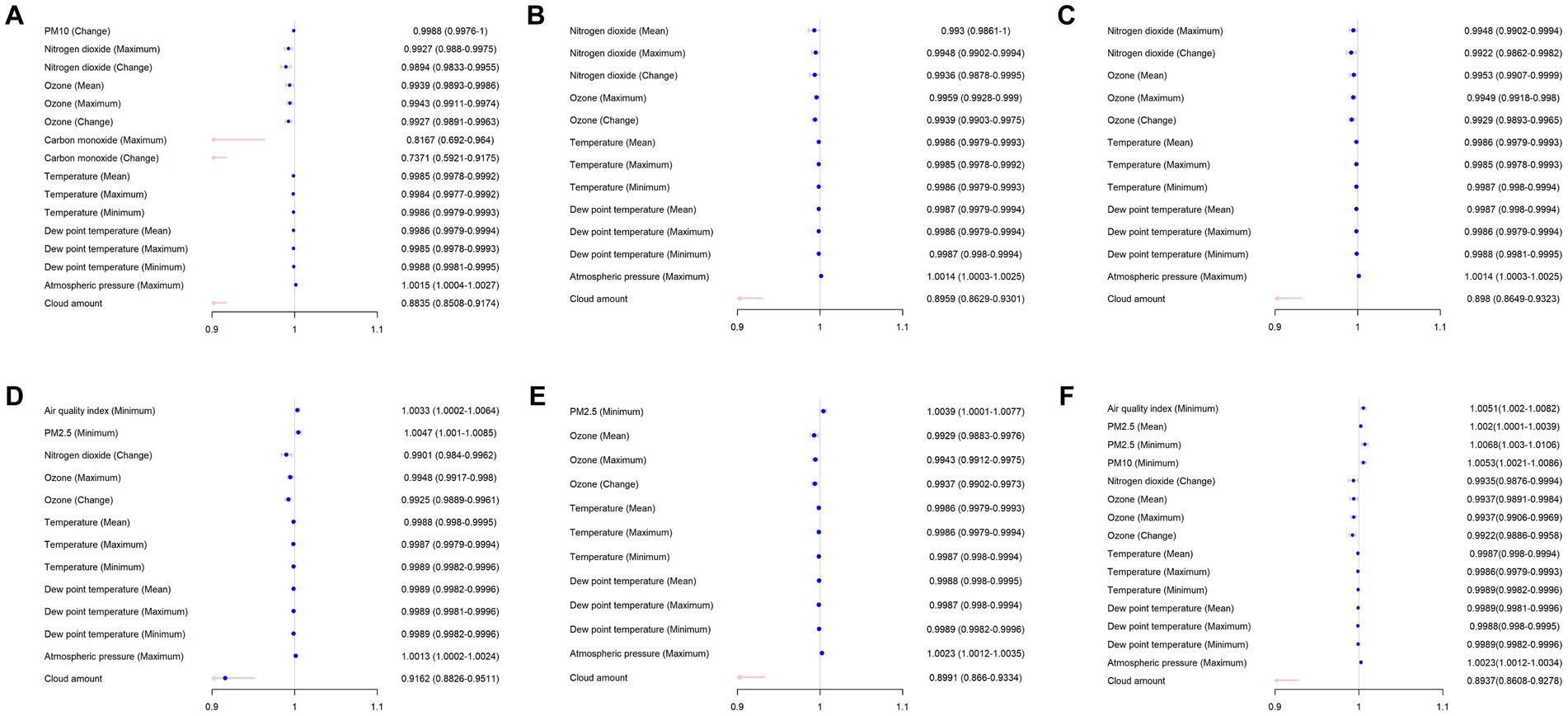
Figure 2. Logistic regression analysis of environmental and weather feature associated with AAD occurrence. The day of onset: (A) same day, (B) one day before (day – 1), (C) two days before (day – 2), (D) three days before (day – 3), (E) five days before (day – 5), and (F) seven days before (day – 7).
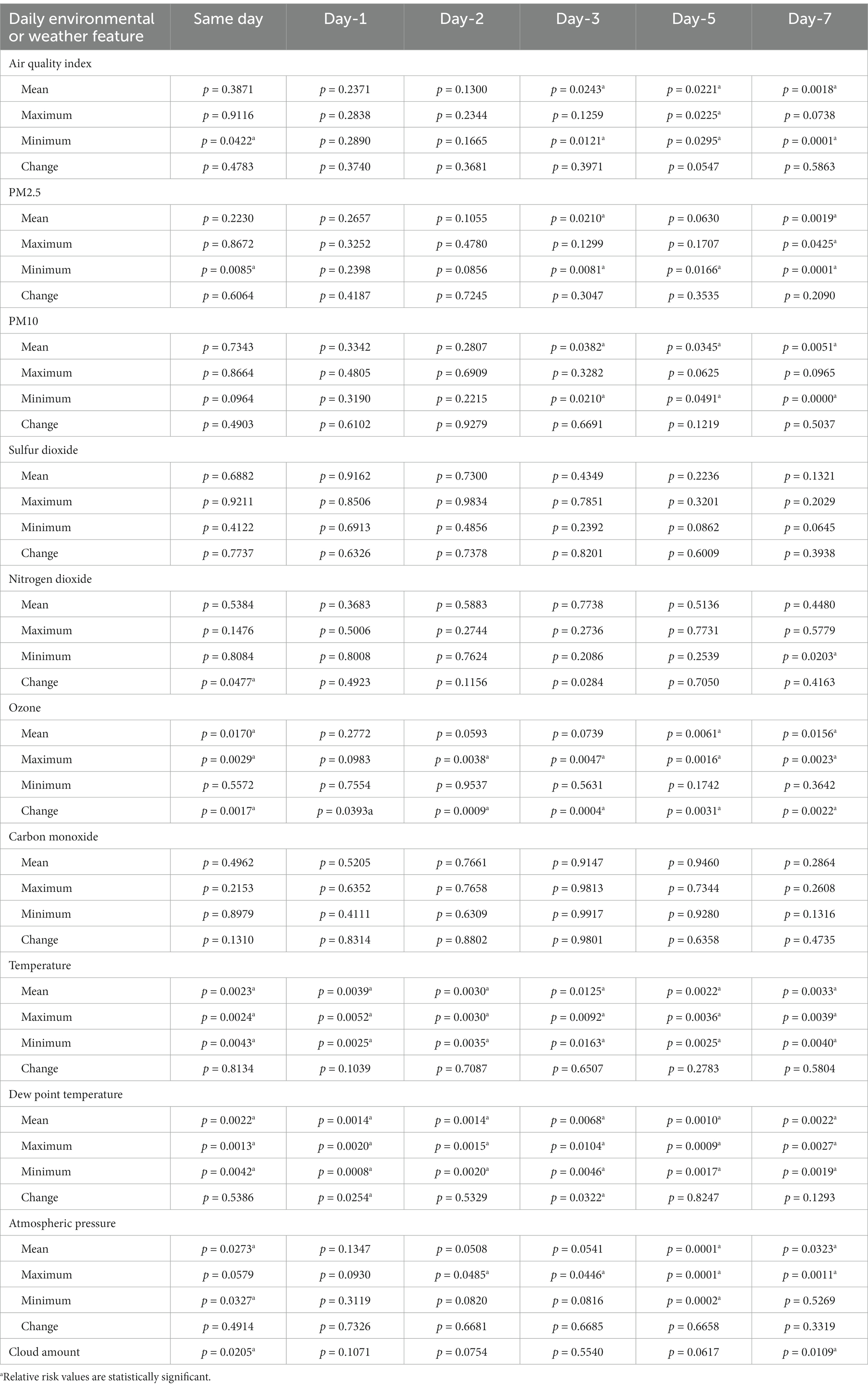
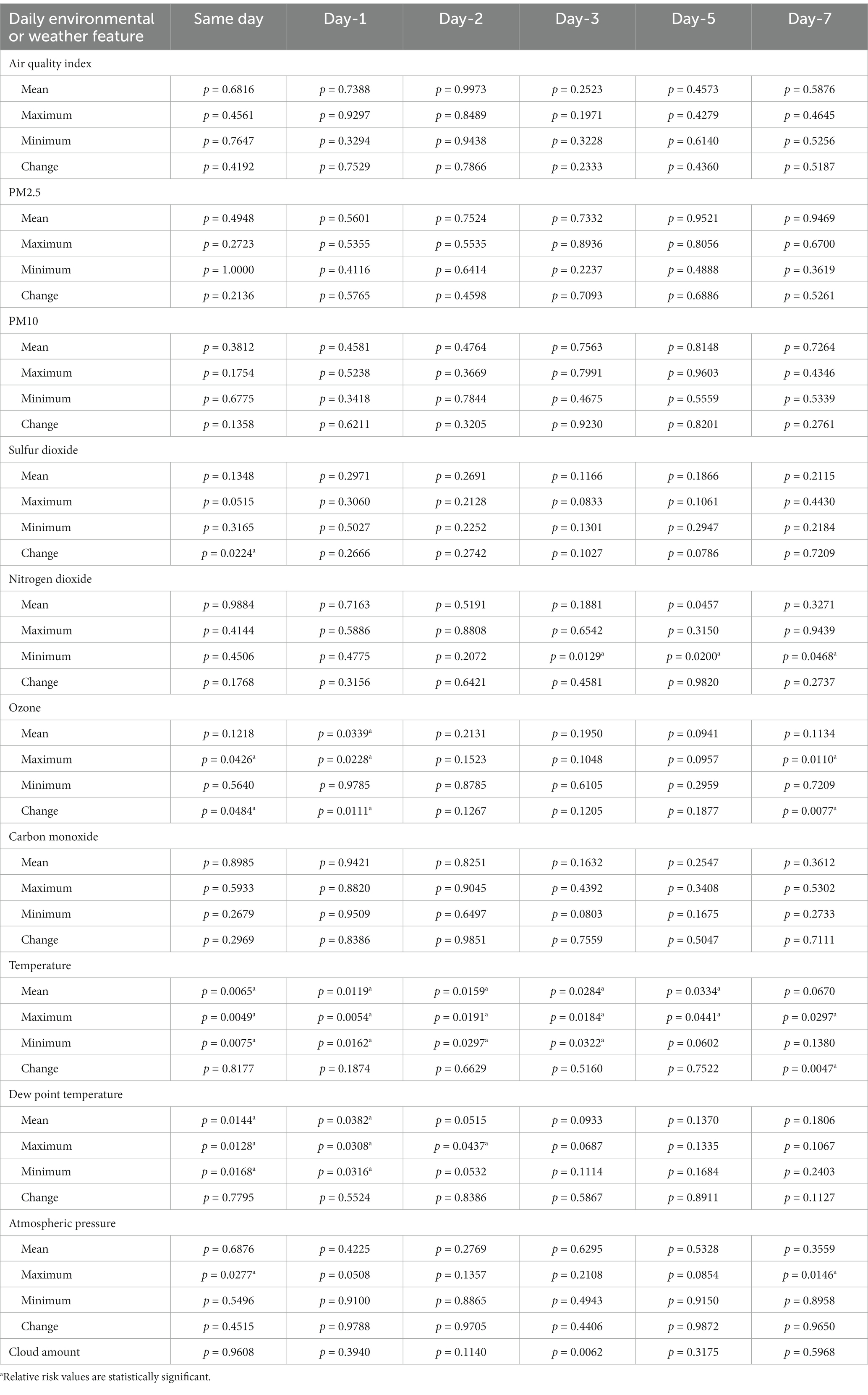
The interactions analyzes showed that the relationship between climate state and AAD occurrence was affected by COVID-19 outbreak (Supplementary Table S1). Subgroup analyzes were then conducted based on whether COVID-19 outbreak (Tables 3, 4 and Figure 3). In the days before the COVID-19 outbreak, the concentrations of pollutants performed a predictive ability significantly on the same day or the days before AAD occurrence. Interestingly, in the days after the COVID-19 outbreak, only concentrations of NO2 (p = 0.0468) and O3 (p = 0.011) predicted AAD occurrence as early as 7 days before the event. Temperature, dew point temperature, and atmospheric pressure also exhibited obvious event correlations.
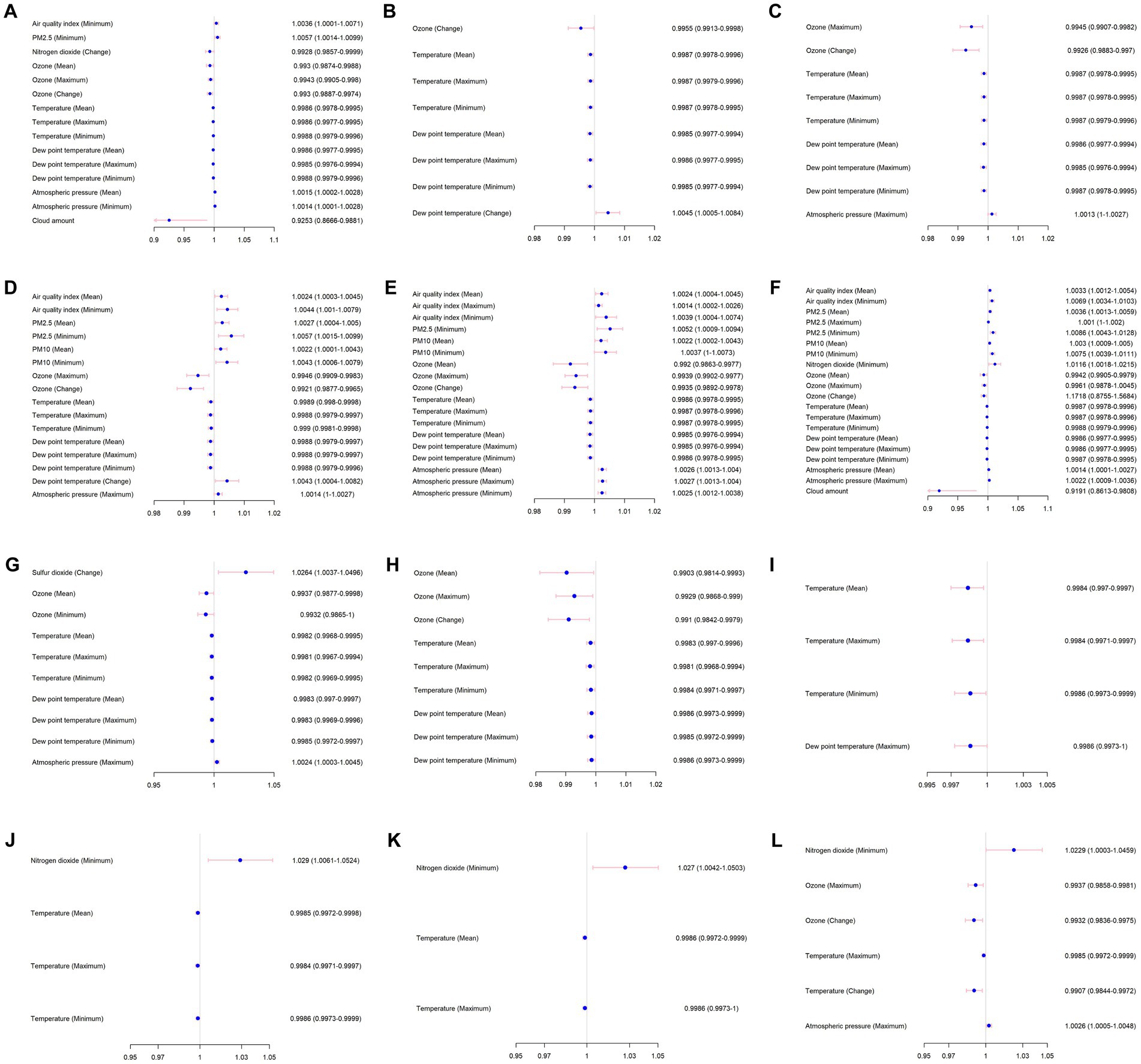
Figure 3. Stratified analysis for COVID-19 outbreak of environmental and weather feature associated with AAD occurrence. The day of onset: (A) same day, before February 1, 2020, (B) one day before (day – 1), before the COVID-19 outbreak, (C) two days before (day – 2), before the COVID-19 outbreak, (D) three days before (day – 3), before the COVID-19 outbreak, (E) five days before (day – 5), before the COVID-19 outbreak, and (F) seven days before (day – 7), before the COVID-19 outbreak. (G) same day, after the COVID-19 outbreak, (H) one day before (day – 1), after the COVID-19 outbreak, (I) two days before (day – 2), after the COVID-19 outbreak, (J) three days before (day – 3), after the COVID-19 outbreak, (K) five days before (day – 5), after the COVID-19 outbreak, and (L) seven days before (day – 7), after the COVID-19 outbreak.
As shown in Figure 4, RCS were used to flexibly model and visualize the correlations of the mean temperature, mean PM2.5, and mean PM10 with AAD risk. Generally, the correlations were curved rather than linear, indicating the presence of significant quadratic terms and thus the need for visual inspection of quadratic prediction plots. Notably, although there was not a nonlinear relationship between temperature and AAD risk, these variables were significantly related (p < 0.05). The median temperature of the mean (6.99°C) was chosen as a reference of RCS in all days. The median temperature of the mean (7.11°C) was chosen as a reference of RCS in days before the COVID-19 outbreak. The median temperature of the mean (6.33°C) was chosen as a reference of RCS in days after the COVID-19 outbreak. The results from RCS showed that as the mean temperature increases, the risk of AAD decreases actually (Figures 4A,D,G).
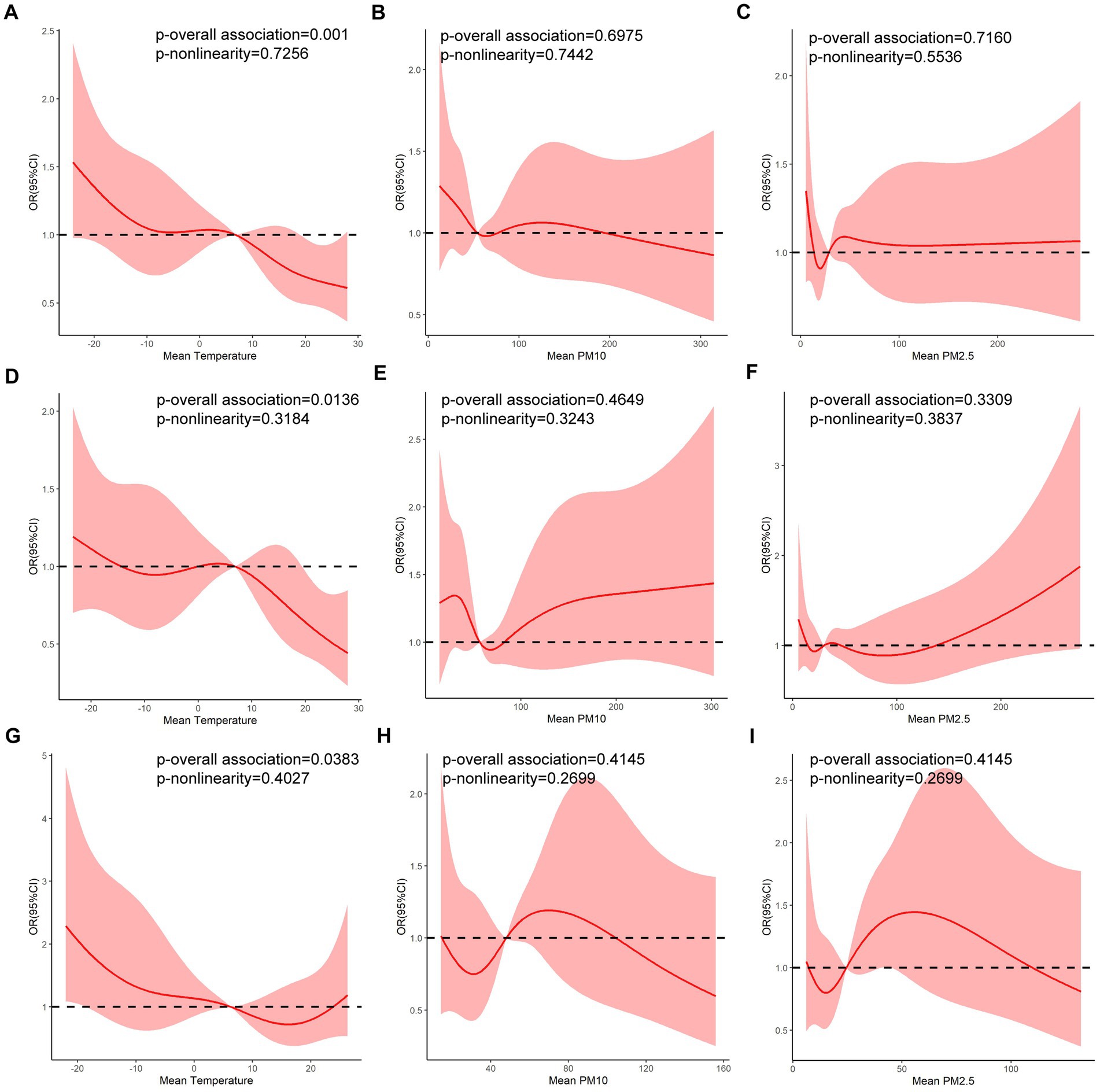
Figure 4. Relationships of mean temperature, mean PM10 concentration and mean PM2.5 concentration with the risk of AAD occurrence for all days, days prior to the COVID-19 outbreak and days after the COVID-19 outbreak. (A) Mean temperature: all days. (B) PM10 concentration: all days. (C) PM2.5 concentration: all days. (D) Mean temperature: before the COVID-19 outbreak. (E) PM10 concentration: before the COVID-19 outbreak. (F) PM2.5 concentration: before the COVID-19 outbreak. (G) Mean temperature: after the COVID-19 outbreak. (H) PM10 concentration: after the COVID-19 outbreak. (I) PM2.5 concentration: after the COVID-19 outbreak (The red solid line is the mean risk estimate, and the red areas are their 95% confidence intervals).
Discussion
In this research, a regionwide retrospective study was conducted in Harbin, a large city with the highest latitude and lowest temperatures in Northeast China. Harbin’s climate is characterized by short, cool summers and long, cold winters (22, 23). In addition, the heating period lasts for half a year, during which the outdoor air quality is frequently poor, likely due to fossil fuel combustion for heating, industrial discharge, automobile exhaust, or burning straw in nearby rural areas (24). The impacts of these significant climatic conditions and environmental factors on the occurrence of AAD has not been evaluated previously. Indeed, to the best of our knowledge, this is the first study to examine the effects of daily ambient temperature and air pollutants on the risk of AAD occurrence; additionally, it is the first study to evaluate the influence of the COVID-19 pandemic on the relationship between air pollution and AAD risk in a cold region.
Regarding meteorological indicators, we observed that a drop in temperature was associated with an increased risk of later AAD, with lags of 0 to 7 days. Indicators of this drop in temperature included the daily maximum, minimum, and average temperatures, but did not include the daily temperature change. This association between low temperatures and AAD risk (with lags of 0 to 7 days) was detected even with a long heating period during winter in cold regions. This result aligns with previous findings of associations between low ambient temperature and a high risk of acute cardiovascular incidents, such as acute coronary syndrome, heart failure, hypertension, and stroke (25–29). In addition, the risk of AAD increased with lower ambient temperature to a greater extent than the risks of the cardiovascular events listed above. Regarding the mechanisms by which low temperature can affect AAD risk, there are numerous biological responses to low temperatures, such as increased blood pressure, haemodynamic changes, vasoconstriction in small vessels, behavioral changes, or onset of suboptimal health conditions (13, 15). Nevertheless, there is little evidence of the underlying biological mechanisms of the relationship between low temperatures and an increased risk of AAD.
Dew point temperature had a similar effect on AAD risk as temperature. Dew point temperature is related to the water vapour content (i.e., humidity) in the air; that is, the lower the dew point temperature is, the lower the water vapour content and the lower the relative humidity (30). In this study, we found that a low dew point temperature was associated with a higher risk of later AAD, with lags of 0 to 7 days. Although the underlying mechanism remains unclear, this correlation is also supported by the fact that colder, drier air in winter is associated with a high incidence of AAD in cold regions. On the other hand, it may also indicate that the incidence of AAD in dry inland regions is significantly higher than that in humid coastal regions (31).
Regarding air pollutants, we found that short-term exposure to high concentrations of air pollutants was associated with later AAD risk, with lags of 3 to 7 days. In brief, our results indicate that the risk of AAD is strongly associated with several pollutants and weather characteristics. Our current study was unable to directly investigate the causality of this relationship. However, we found that the following predictors of AAD changed before AAD onset: concentrations of PM2.5, PM10, NO2, O3, and CO. These indicators changed drastically as early as 7 days before AAD onset. Increased values of these indicators (other than O3) were significantly associated with increased risk of AAD. However, apart from the negative correlation of O3 with AAD onset, the risk of AAD was difficult to predict in the short term with pollutant concentrations (i.e., lags varied from 0 to 2 days), especially AQI as a comprehensive indicator.
Fine particulate matter (PM2.5) is the most important air pollutant. It is considered the single greatest environmental threat to human health worldwide. Acute cardiovascular events mainly include coronary heart disease, acute myocardial infarction, heart failure, cardiac arrest, hypertension, arrhythmia, and stroke, and according to numerous epidemiological studies, short-term exposure to PM2.5 is prominently associated with increased risk of occurrence (1, 4, 32, 33). PM2.5 exposure and AAD onset are correlated; moreover, this relationship is also biologically credible. PM2.5 exposure increases blood pressure and can thus promote the occurrence of AAD. However, there is a paucity of epidemiological research on the latent risks of AAD associated with PM2.5 exposure.
Although the relationship between O3 and the occurrence and mortality of cardiovascular diseases is still controversial (34, 35), our results showed that the occurrence of AAD increases with the decreased in O3 concentration. Interestingly, results of studies have varied regarding the chronic effects of O3 exposure on cardiovascular mortality. There is no clear “safe” threshold for O3 exposure in terms of cardiovascular mortality. Long-term exposure to O3 is linked to an increased risk of death from cardiovascular disease, ischemic heart disease, and stroke (36, 37). A prior investigation revealed that short-term exposure to O3 is linked to higher mortality in those who have previously been hospitalized for acute myocardial infarction (38). In the atmosphere, O3 efficiently shields UV rays and safeguards human health; it is typically found approximately 30 kilometers above the ground. However, sufficient light (strong radiation), high temperatures, and low humidity cause photochemical reactions, leading to O3 pollution that harms human health and the ecosystem. Although studies have found that O3 exposure is associated with cardiovascular mortality (35, 39), the underlying biological mechanism is still unclear. In conclusion, the risk of AAD was inversely related to temperature, dew point temperature, and air pressure, as mentioned previously. In other words, days that were colder, drier, and had lower air pressures, lower O3 concentrations, and heavier pollution had a higher risk of AAD.
In addition, after the COVID-19 outbreak, the predictive power of pollutant concentrations on the occurrence of AAD was reduced. The study period lasted 1 year. Except for SO2 and O3, the pollutants were essentially not associated with the occurrence of AAD, with lags of 0 to 7 days. This may be because people were required to wear masks during the COVID-19 pandemic, which reduced the risk of AAD caused by inhalation of air pollutants. Research has not yet investigated whether wearing masks (N95 masks or even general surgical masks) could prevent cardiovascular emergencies. This may indicate a new avenue for prevention of AAD. Meanwhile, people’s exercise range has been constrained during the COVID-19 preventive and control period, dramatically limiting outdoor activities and vigorous exercise. These characteristics lessen the effect of outdoor air pollution on the occurrence of AAD, and intensive exercise’s effect on blood pressure and heart rate also contributes to the condition’s development.
Strengths and limitations
To the best of our knowledge, this is the first study to explore the impact of daily ambient temperature and air pollutants on the risk of AAD under low-temperature weather conditions. In this study, we offered novel and convincing evidence in a cold region (Harbin, China), which revealed that short-term exposure to air pollution and low temperatures was linked to an increased risk of AAD. Our findings identify modifiable environmental risk factors for AAD occurrence, which would be useful for AAD prevention, as AAD is a life-threatening cardiovascular emergency.
Due to some limitations, our results should be interpreted with caution. First, this study had a single-center retrospective design, and therefore inevitably included selection bias. Second, there may have been measurement errors due to the collection of meteorological and air pollution data from outdoor monitoring stations. Finally, the interference of indoor temperature and air pollutants was not considered. These factors may be the main causes of cardiovascular emergencies. Most health impacts are due to indoor air pollutants, which can enter a room in various ways from the outdoors (40); therefore, even people who stay indoors most of the time may still be affected by air pollutants.
Conclusion
The risk of AAD is closely related to air pollution and weather characteristics in Harbin. While causation was not determined, the impact of air pollutants on the risk of AAD was reduced after the COVID-19 outbreak.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TS and YuS designed the study, handled data analysis and interpretation, and drafted the manuscript. YZ, ZQ, SP, ZW, BS, JD, JL, KD, MW, YaS, JC, and HoZ participated in the gathering of data, its analysis and interpretation, and its critical examination for key intellectual elements. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Heilongjiang Postdoctoral Research Foundation (LBH-Q20110) and the Scientific Research Fund of the First Affiliated Hospital of Harbin Medical University (HYD2020YQ0004, 2020M20, 2020M08).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1172532/full#supplementary-material
References
1. Mussa, FF, Horton, JD, Moridzadeh, R, Nicholson, J, Trimarchi, S, and Eagle, KA. Acute aortic dissection and intramural hematoma: a systematic review. JAMA. (2016) 316:754–63. doi: 10.1001/jama.2016.10026
2. Nienaber, CA, and Clough, RE. Management of acute aortic dissection. Lancet. (2015) 385:800–11. doi: 10.1016/S0140-6736(14)61005-9
3. Lim, SS, Vos, T, Flaxman, AD, Danaei, G, Shibuya, K, Adair-Rohani, H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8
4. Biondi-Zoccai, G, Frati, G, Gaspardone, A, Mariano, E, Di Giosa, AD, Bolignano, A, et al. Impact of environmental pollution and weather changes on the incidence of ST-elevation myocardial infarction. Eur J Prev Cardiol. (2021) 28:1501–7. doi: 10.1177/2047487320928450
5. Carlson, M, Airhart, N, Lopez, L, and Silberbach, M. Moderate aortic enlargement and bicuspid aortic valve are associated with aortic dissection in turner syndrome: report of the international turner syndrome aortic dissection registry. Circulation. (2012) 126:2220–6. doi: 10.1161/CIRCULATIONAHA.111.088633
6. Eleid, MF, Forde, I, Edwards, WD, Maleszewski, JJ, Suri, RM, Schaff, HV, et al. Type a aortic dissection in patients with bicuspid aortic valves: clinical and pathological comparison with tricuspid aortic valves. Heart. (2013) 99:1668–74. doi: 10.1136/heartjnl-2013-304606
7. Dong, N, Piao, H, Li, B, Xu, J, Wei, S, and Liu, K. Poor management of hypertension is an important precipitating factor for the development of acute aortic dissection. J Clin Hypertens (Greenwich). (2019) 21:804–12. doi: 10.1111/jch.13556
8. Li, Y, Ji, C, Zhang, J, and Han, Y. The effect of ambient temperature on the onset of acute Stanford type B aortic dissection. Vasa. (2016) 45:395–401. doi: 10.1024/0301-1526/a000555
9. Mehta, RH, Manfredini, R, Hassan, F, Sechtem, U, Bossone, E, Oh, JK, et al. International registry of acute aortic dissection I. Chronobiological patterns of acute aortic dissection. Circulation. (2002) 106:1110–5. doi: 10.1161/01.cir.0000027568.39540.4b
10. Ma, WG, Li, B, Zhang, W, Sarkar, AEH, Tufail, R, Peterss, S, et al. Chronologic and climatic factors of acute aortic dissection: study of 1642 patients in two continents. Ann Thorac Surg. (2020) 110:575–81. doi: 10.1016/j.athoracsur.2019.11.013
11. Benouaich, V, Soler, P, Gourraud, PA, Lopez, S, Rousseau, H, and Marcheix, B. Impact of meteorological conditions on the occurrence of acute type a aortic dissections. Interact Cardiovasc Thorac Surg. (2010) 10:403–6. doi: 10.1510/icvts.2009.219873
12. Xia, L, Huang, L, Feng, X, Xiao, J, Wei, X, and Yu, X. Chronobiological patterns of acute aortic dissection in Central China. Heart. (2020) 107:320–5. doi: 10.1136/heartjnl-2020-317009
13. Chen, J, Gao, Y, Jiang, Y, Li, H, Lv, M, Duan, W, et al. Low ambient temperature and temperature drop between neighbouring days and acute aortic dissection: a case-crossover study. Eur Heart J. (2022) 43:228–35. doi: 10.1093/eurheartj/ehab803
14. Mehta, RH, Manfredini, R, Bossone, E, Fattori, R, Evagelista, A, Boari, B, et al. International registry of acute aortic dissection I. the winter peak in the occurrence of acute aortic dissection is independent of climate. Chronobiol Int. (2005) 22:723–9. doi: 10.1080/07420520500179605
15. Zhang, Q, Peng, L, Hu, J, Li, H, Jiang, Y, Fang, W, et al. Low temperature and temperature decline increase acute aortic dissection risk and burden: a nationwide case crossover analysis at hourly level among 40, 270 patients. Lancet Reg Health West Pac. (2022) 28:100562. doi: 10.1016/j.lanwpc.2022.100562
16. Xie, N, Zou, L, and Ye, L. The effect of meteorological conditions and air pollution on the occurrence of type a and B acute aortic dissections. Int J Biometeorol. (2018) 62:1607–13. doi: 10.1007/s00484-018-1560-0
17. Chen, J, Lv, M, Yao, W, Chen, R, Lai, H, Tong, C, et al. Association between fine particulate matter air pollution and acute aortic dissections: a time-series study in Shanghai. China Chemosphere. (2020) 243:125357. doi: 10.1016/j.chemosphere.2019.125357
18. Mazaherpour, H, Soofian, M, Farahani, E, Masfari Farahani, F, Ghaznavi Rad, E, Mazaherpour, S, et al. Frequency of cardiovascular complications and its association with prognosis of COVID-19 patients. Biomed Res Int. (2021) 2021:7073348–6. doi: 10.1155/2021/7073348
19. Ramandi, A, Akbarzadeh, MA, Khaheshi, I, and Khalilian, MR. Aortic dissection and Covid-19; a comprehensive systematic review. Curr Probl Cardiol. (2023) 48:101129. doi: 10.1016/j.cpcardiol.2022.101129
20. Arnaoutakis, GJ, Wallen, TJ, Desai, N, Martin, TD, Thourani, VH, Badhwar, V, et al. Outcomes of acute type a aortic dissection during the COVID-19 pandemic: an analysis of the Society of Thoracic Surgeons database. J Card Surg. (2022) 37:4545–51. doi: 10.1111/jocs.17085
21. Yamamoto, T, Harada, K, Yoshino, H, Nakamura, M, Kobayashi, Y, Yoshikawa, T, et al. Impact of the COVID-19 pandemic on incidence and mortality of emergency cardiovascular diseases in Tokyo. J Cardiol. (2023) 82:134–9. doi: 10.1016/j.jjcc.2023.01.001
22. Nie, TZ, Yuan, R, Liao, SH, Zhang, ZX, Gong, ZP, Zhao, X, et al. Characteristics of potential evapotranspiration changes and its climatic causes in Heilongjiang Province from 1960 to 2019. Agriculture-Basel. (2022) 12. doi: 10.3390/agriculture12122017
23. Yu, X, Xia, L, Xiao, J, Zheng, J, Xu, N, Feng, X, et al. Association of Daily Mean Temperature and Temperature Variability with Onset Risks of acute aortic dissection. J Am Heart Assoc. (2021) 10:e020190. doi: 10.1161/JAHA.120.020190
24. Wang, L, Deng, JR, Yang, LJ, Yu, TR, Yao, YL, and Xu, DW. Dynamic analysis of particulate pollution in haze in Harbin city. Northeast China Open Geosci. (2021) 13:1656–67. doi: 10.1515/geo-2020-0327
25. Ishikawa, K, Niwa, M, and Tanaka, T. Difference of intensity and disparity in impact of climate on several vascular diseases. Heart Vessel. (2012) 27:1–9. doi: 10.1007/s00380-011-0206-5
26. Li, N, Ma, J, Liu, F, Zhang, Y, Ma, P, Jin, Y, et al. Associations of apparent temperature with acute cardiac events and subtypes of acute coronary syndromes in Beijing, China. Sci Rep. (2021) 11:15229. doi: 10.1038/s41598-021-94738-9
27. Chen, R, Jiang, Y, Hu, J, Chen, H, Li, H, Meng, X, et al. Hourly air pollutants and acute coronary syndrome onset in 1.29 million patients. Circulation. (2022) 145:1749–60. doi: 10.1161/CIRCULATIONAHA.121.057179
28. Wang, M, Zhou, T, Song, Y, Li, X, Ma, H, Hu, Y, et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK biobank. Eur Heart J. (2021) 42:1582–91. doi: 10.1093/eurheartj/ehaa1031
29. Lian, H, Ruan, Y, Liang, R, Liu, X, and Fan, Z. Short-term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int J Environ Res Public Health. (2015) 12:9068–88. doi: 10.3390/ijerph120809068
30. Nguyen, JL, and Dockery, DW. Daily indoor-to-outdoor temperature and humidity relationships: a sample across seasons and diverse climatic regions. Int J Biometeorol. (2016) 60:221–9. doi: 10.1007/s00484-015-1019-5
31. Tang, X, Lu, K, Liu, X, Jin, D, Jiang, W, Wang, J, et al. Incidence and survival of aortic dissection in urban China: results from the National Insurance Claims for epidemiological research (NICER) study. Lancet Reg Health West Pac. (2021) 17:100280. doi: 10.1016/j.lanwpc.2021.100280
32. Sun, Z, Chen, C, Xu, D, and Li, T. Effects of ambient temperature on myocardial infarction: a systematic review and meta-analysis. Environ Pollut. (2018) 241:1106–14. doi: 10.1016/j.envpol.2018.06.045
33. Wang, R, Liu, J, Qin, Y, Chen, Z, Li, J, Guo, P, et al. Global attributed burden of death for air pollution: demographic decomposition and birth cohort effect. Sci Total Environ. (2023) 860:160444. doi: 10.1016/j.scitotenv.2022.160444
34. Rich, DQ, Balmes, JR, Frampton, MW, Zareba, W, Stark, P, Arjomandi, M, et al. Cardiovascular function and ozone exposure: the Multicenter ozone study in old Er subjects (MOSES). Environ Int. (2018) 119:193–202. doi: 10.1016/j.envint.2018.06.014
35. Zhang, J, Chen, Q, Wang, Q, Ding, Z, Sun, H, and Xu, Y. The acute health effects of ozone and PM (2.5) on daily cardiovascular disease mortality: a multi-center time series study in China. Ecotoxicol Environ Saf. (2019) 174:218–23. doi: 10.1016/j.ecoenv.2019.02.085
36. Niu, Y, Zhou, Y, Chen, R, Yin, P, Meng, X, Wang, W, et al. Long-term exposure to ozone and cardiovascular mortality in China: a nationwide cohort study. Lancet Planet Health. (2022) 6:e496–503. doi: 10.1016/S2542-5196(22)00093-6
37. Yin, P, Brauer, M, Cohen, AJ, Wang, H, Li, J, Burnett, RT, et al. The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990-2017: an analysis for the global burden of disease study 2017. Lancet Planet Health. (2020) 4:e386–98. doi: 10.1016/S2542-5196(20)30161-3
38. Bero Bedada, G, Raza, A, Forsberg, B, Lind, T, Ljungman, P, Pershagen, G, et al. Short-term exposure to ozone and mortality in subjects with and without previous cardiovascular disease. Epidemiology. (2016) 27:663–9. doi: 10.1097/EDE.0000000000000520
39. Mirowsky, JE, Carraway, MS, Dhingra, R, Tong, H, Neas, L, Diaz-Sanchez, D, et al. Ozone exposure is associated with acute changes in inflammation, fibrinolysis, and endothelial cell function in coronary artery disease patients. Environ Health. (2017) 16:126. doi: 10.1186/s12940-017-0335-0
Keywords: weather, environment, temperature, pollution, acute aortic dissection, COVID-19
Citation: Zhang H, Yin L, Zhang Y, Qiu Z, Peng S, Wang Z, Sun B, Ding J, Liu J, Du K, Wang M, Sun Y, Chen J, Zhao H, Song T and Sun Y (2023) Short-term effects of air pollution and weather changes on the occurrence of acute aortic dissection in a cold region. Front. Public Health. 11:1172532. doi: 10.3389/fpubh.2023.1172532
Edited by:
Mohammad Javad Mohammadi, Ahvaz Jundishapur University of Medical Sciences, IranReviewed by:
Antonella Bodini, National Research Council (CNR), ItalyNagisa Morikawa, Kurume University, Japan
Marzieh Sadeghian, Ahvaz Jundishapur University of Medical Sciences, Iran
Copyright © 2023 Zhang, Yin, Zhang, Qiu, Peng, Wang, Sun, Ding, Liu, Du, Wang, Sun, Chen, Zhao, Song and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Song, c2h1dGlhbzE5ODFAc2luYS5jb20=; Yuhui Sun, eXVodWlfc3VuQHZpcC4xNjMuY29t
†These authors have contributed equally to this work
 Haiyu Zhang1†
Haiyu Zhang1† Zhaowen Qiu
Zhaowen Qiu Jianrui Ding
Jianrui Ding Tao Song
Tao Song Yuhui Sun
Yuhui Sun