- 1Ningbo Yinzhou No.2 Hospital, Ningbo, China
- 2Fenghua District Center for Disease Control and Prevention, Ningbo, China
- 3Ningbo Municipal Center for Disease Control and Prevention, Ningbo, China
- 4Zhejiang Provincial Center for Disease Control and Prevention, Hangzhou, China
Background: Myopia is an increasingly serious public concern, particularly among primary school students. The prevalence of myopia and its influencing factors in primary school pupils in Eastern China during the COVID-19 pandemic had not been explored.
Methods: A randomly clustered sampling method was performed, and selected pupils from grade 1 to grade 3 in 15 primary schools in the Fenghua District of Zhejiang Province were included and given myopia screening and uniform questionnaire survey 1 year later.
Results: A total of 4,213 students completed the myopia screening and questionnaire survey. Myopia was diagnosed in 1,356 pupils, with a myopia incidence of 32.19%. The spherical equivalent (SE) refraction of the included pupils decreased on average by 0.50 ± 2.15 D 1 year later. The myopia rate was positively correlated with the increase of grade, in which the myopia rate among grade 3 students was the highest at 39.69%. The myopia rate among female students was higher than that among male students. Students residing in urban areas had a higher myopia rate than in rural areas. Maintaining an near work distance ≥33 cm was a significant protective factor (OR = 0.84, 95% CI: 0.74–0.96). Students with two myopic parents had a higher risk of myopia (OR = 1.61, 95% CI: 1.34–1.92).
Conclusion: During the COVID-19 pandemic, the myopia rate among early primary school students in Eastern China was high. More attention and implementation of interventions from health and education departments, such as training the development of good eye behavior, should be considered to strengthen the intervention of myopia in primary school students.
1. Introduction
In recent years, the prevalence of myopia has increased markedly and rapidly, resulting in a serious burden among the general population (1–6). Its prevalence in East Asian countries, particularly in the Chinese population, is the highest (7). The prevalence of myopia among senior high school students has reached 80% in China, and that there is a trend of increasingly younger age at diagnosis (8, 9). Moreover, meta-analysis results have shown that the myopia rate among primary students in China was 22.53% during 1989–2014, whereas it has increased to 38.92% during 2018–2020, implying an increasing challenge for myopia's interventions (10, 11). Individuals who developed myopia during childhood were prone to developing high myopia, which could increase the risk of macular degeneration, retinal detachment, glaucoma, and cataract (12–15). These complications might further cause low vision and even blindness. Thus, how to curb children's myopia effectively has become an important issue of public health.
School-age children and adolescents have been seriously affected by the worldwide outbreak of COVID-19 from the end of 2019. Due to the indispensable quarantine measures required during the outbreak, children had less opportunities for outdoor activities, which inevitably implied increased time involved in online learning and other online activities (16). Previous studies have reported that the amount of time spent in outdoor activities and the amount of time spent reading at a close distance were two main factors that strongly influence myopia (17, 18). Although COVID-19 had no direct influence on myopia, it might have had an indirect effect via these factors, and therefore could have contributed to the prevalence of myopia. Hence, assessing these factors in Chinese children during COVID-19 pandemic was worth investigating.
The aim of this study was to explore myopia prevalence in primary school pupils in Eastern China during the COVID-19 pandemic. Fenghua district of Zhejiang Province was selected as the site to examine the potential influencing factors that would be helpful for the development of positive intervention for prevent myopia in this special group.
2. Materials and methods
In this study, Fenghua district was selected as the study site. Fenghua district is located in the coastal area of East China. It is between 29°25′ and 29°47′ north latitude, and 121°03′ and 121°46′ east longitude, and covers a land area of 1,277 km2. There are eight communities and four towns under the jurisdiction of Fenghua District, with 577,505 permanent residents. In Fenghua district, there are 30 primary schools, with nearly 30,271 pupils from grade 1 to 6.
2.1. Respondents
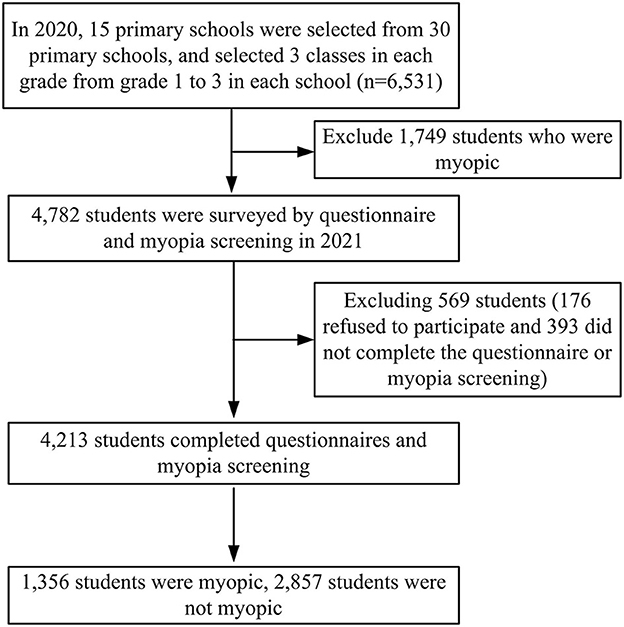
A randomly clustered sampling method was used in this study in 2020. Firstly, 30 random numbers were assigned to 30 primary schools. Then, by randomly drawing 15 numbers, the specific numbers corresponding to schools were obtained. Subsequently, the same method was used to select 3 classes in each grade from grade 1 to 3 in each school. A total of 6,531 students were considered initially. From these students, 1,749 students who were already myopic prior to the study were excluded; thus, 4,782 students were included as research subjects. Questionnaires and myopia screening were carried out among these students 1 year later. Among the 4,782 included students, 4,213 students completed both the questionnaire survey and the myopia screening, with a completion rate of 88.10% (569 students were excluded: 176 refused to participate and 393 did not complete the questionnaire survey or myopia screening). The baseline data of SE refraction for the general characteristics of included participants in 2020 was presented in the Supplementary material 1. The electronic questionnaire included items on demographic characteristics, parent's myopia status, near work distance, average outdoor activity time, time spent in homework, average time spent on electronic device, and average sleep duration (Supplementary material 2). It was delivered using the student health management platform (SHMP) of Fenghua District. By scanning a QR code on this platform, students would complete the survey along with their parents by using mobile phones or other electronic equipment. The details of this process are shown in Figure 1.
2.2. Definitions
Myopia screening included an uncorrected distance visual acuity (UDVA) examination and refractive examination. The UDVA examination employed a standard logarithmic visual acuity chart, in which students were examined in the order of the right eye first, followed by the left eye, with an eye mask on the alternate eye, at a distance of 5 meters from the visual acuity chart. The results were recorded to one decimal place. Additionally, refractive examination was performed by means of a computer refractometer under non-cycloplegic conditions, and the average value of three measurements by a local ophthalmologist was taken. The combination of measurement indexes included spherical refraction and cylindrical refraction. Spherical equivalent refraction (SE) was calculated as spherical refraction + 1/2 cylindrical refraction. The criteria for myopia were set as UDVA < 5.0 and SE < −0.5 D. If a single eye was denoted as myopic, the participant was identified as having myopia.
2.3. Ethics statement
This study was approved by the ethics committee of Ningbo Yinzhou No.2 hospital. A standard informed consent section describing the research target was presented at the beginning of the electronic questionnaire. All personal information in this study was kept confidential as required and the research process complied with the Declaration of Helsinki.
2.4. Statistical analysis
Quantitative data are presented as mean (standard deviation). Considering the high correlation between the SE of the left eye and the right eye in students (r = 0.84), only the SE of the right eye was analyzed in this study. The SE among students with different variables were compared by t-test or analysis of variance. The chi-square test was used to evaluate factors influencing students' myopia. The variables with statistically significant differences were further considered in a multivariate logistic regression analysis. P < 0.05 was considered as indicating a statistically significant difference. All data were analyzed by using R v4.0.5 software (https://www.r-project.org/).
3. Results
3.1. The general epidemiological characteristics of myopia among students
In 2020, based on the principles of sampling and inclusion, a total of 4,782 pupils were recruited in this study. One year later, 4,213 pupils had ultimately completed the questionnaire and myopia screening, including 2,228 male students (52.88%) and 1,985 female students (47.12%). The myopia rate in students with different characteristics is shown in Table 1. The distribution of pupils overall, from grade 1 to grade 3, was as follows: 1,236 (29.34%) in grade 1, 1,609 (38.19%) in grade 2, and 1,368 (32.47%) in grade 3. There were 2,658 (63.09%) students residing in urban areas and 1,555 (36.91%) students residing in rural areas. Among 4,213 pupils, myopia was found in 1,356 students, constituting a myopia incidence of 32.19% with 95% CI 30.78%-33.60% (males: 30.66% and females: 33.90%, which was statistically significantly different; P < 0.01). Furthermore, the myopia rate showed a significant increasing trend with the increase in grade level (P < 0.01). The students living in urban areas had a higher myopia rate than did those in rural areas (P < 0.01). Students whose near work distance ≥33 cm had a comparatively lower myopia rate than those with a near work distance <33 cm (P < 0.01). Moreover, students whose parents had myopia appeared to have a higher risk of myopia progression (P < 0.01).

Table 1. The comparison of myopia incidence among students with different characteristics in Fenghua District.
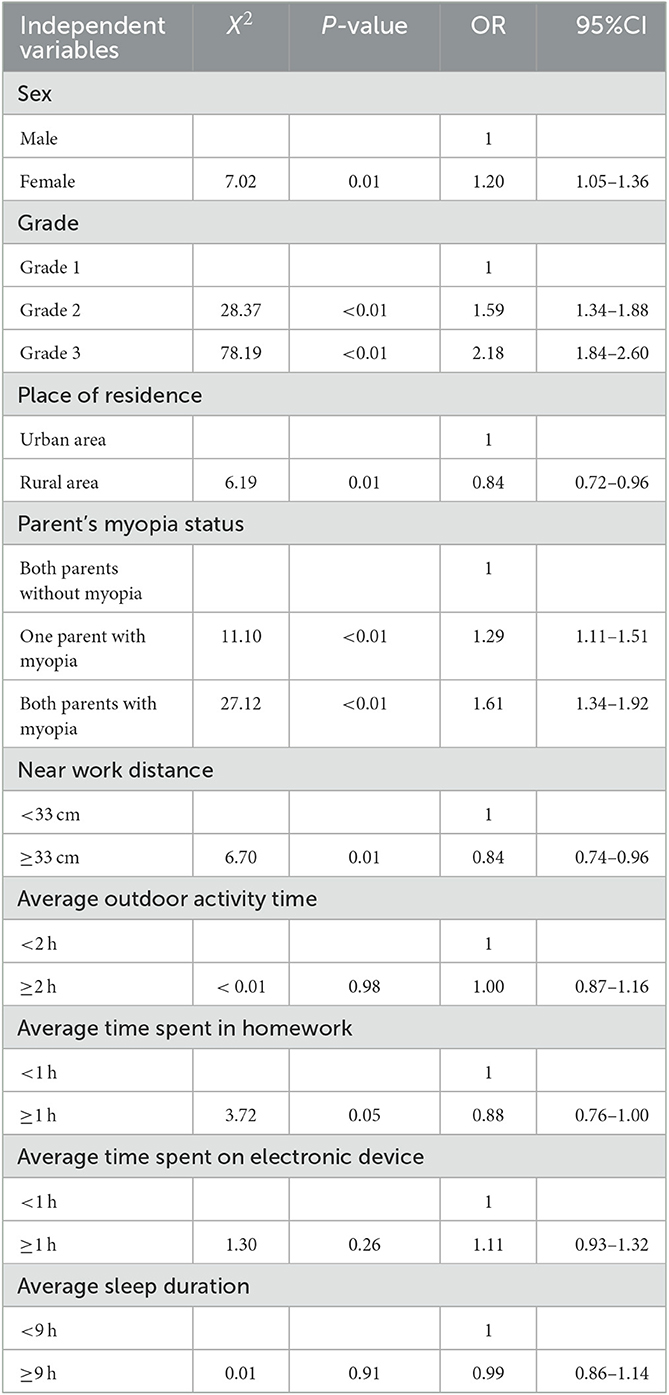
3.2. Multivariate analysis of factors influencing myopia among primary school students
The factors that were identified as significantly influencing myopia in univariate analysis, including place of residence, parent's myopia status, sex, grade, and near work distance, were considered in the multivariate logistic regression analysis (Table 2). The myopia rate of the grade 3 students was found to be 2.18 times than that of grade 1 students. Students whose parents had myopia showed a higher risk of myopia occurrence [odds ratio (OR) = 1.61, 95% confidence interval (CI): 1.34–1.92], while near work distance ≥33 cm was a protective factor against myopia development (OR = 0.84, 95% CI: 0.74–0.96). Female had a higher risk of myopia progression than male. Students living in rural areas had a lower risk of myopia than those living in urban areas.
3.3. The change value in spherical equivalent of pupils
During the study period, the pupils' SE of the right eye decreased with an average of 0.50 D, in which the variation of SE was 0.47 D in males and 0.52 D in females. By analyzing the differences in the three grades, we found a maximum variation (0.57 D) in students in grade 3. Differences in the SE of students with different characteristics are displayed in Table 3.
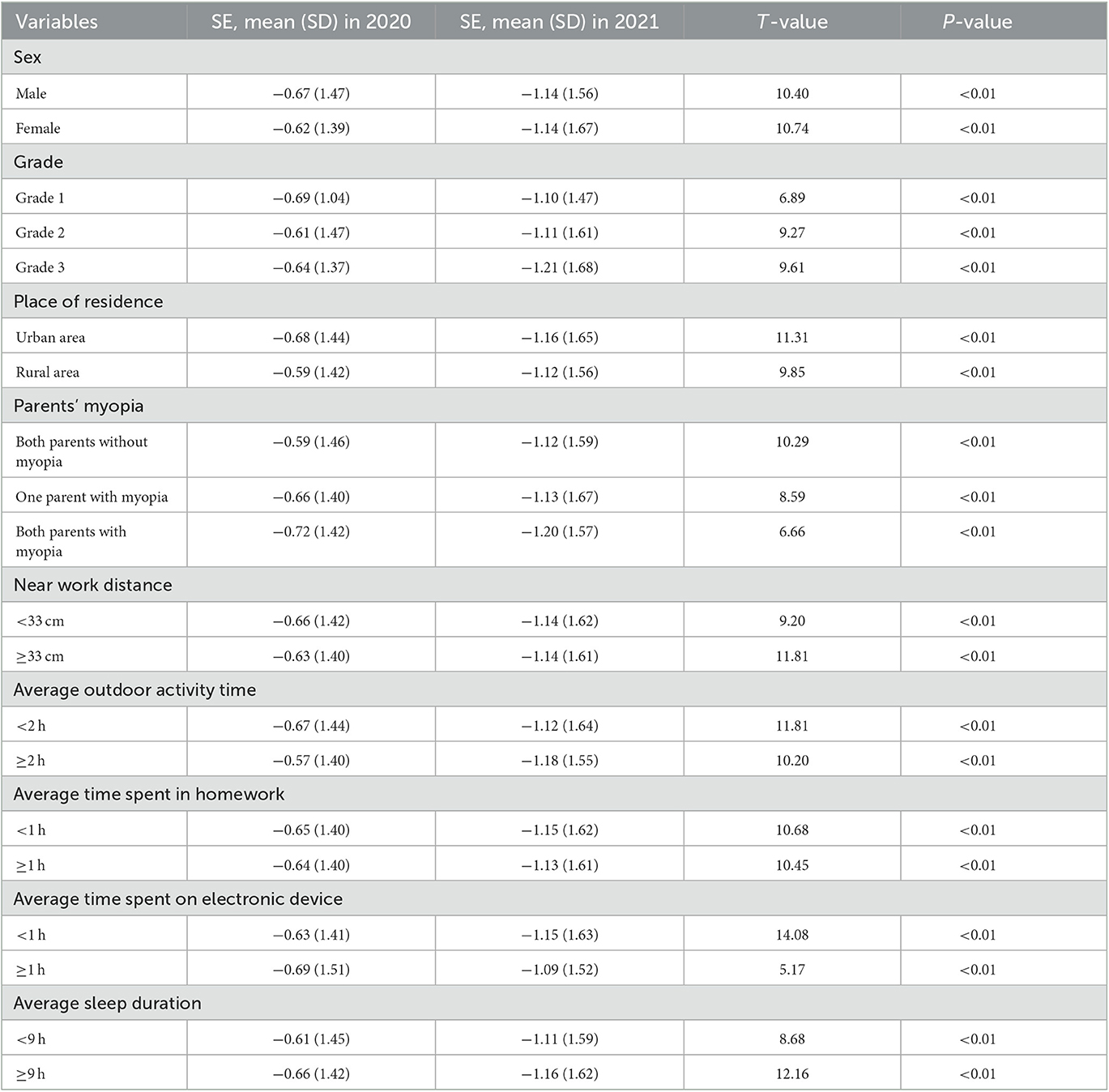
Table 3. The comparison of right eye's spherical equivalent of students with different characteristics between 2020 and 2021.
4. Discussion
In recent years, the problem of myopia has increasingly received attention, given the increase in the myopia rate among younger students (2, 19–21). Our study showed that 32.19% of pupils were newly diagnosed with myopia, while the SE of pupils from grades 1 to 3 decreased by a mean of 0.50 D during the COVID-19 pandemic after a 1-year follow-up. One previous study performed in the Shanxi Province of China identified that the rate of myopia development of pupils in grades 1 to 3 was 20.05% within half a year during the COVID-19 pandemic (22). Another study in the Shanghai area reported that the SE among students aged 7–12 years decreased by an average of 0.59 D between April 2019 and May 2020 (23). Similarly, one investigation in Beijing showed that the SE of students aged between 8 and 10 years decreased by 0.60 D in 1 year during the COVID-19 pandemic (24). A meta-analysis of eight studies assessed the change in adolescent myopia development and compared the visual acuity before and after the COVID-19 pandemic. The review found a 0.41 D reduction in SE, which implied a negative effect of the pandemic on adolescent vision development (25). Simultaneously, studies in Turkey, Spain, and India reported similar conclusion (26–28). Although no strict before and after comparisons were performed in our study, the results were in line with other contemporary studies above, implying that an increased risk of myopia during the COVID-19 pandemic.
According to the findings of our investigation, the risks of myopia in students whose parents both had myopia and that of those who had one parent diagnosed with myopia were 1.61 and 1.29 times higher than those whose parents were both without myopia, respectively, indicating that myopia is influenced by genetic factor. A previous study analyzed the data of 15,316 students aged between 6 and 18 years in 19 schools in China, and concluded that the adjusted OR value of students whose parents both had myopia was 2.83, as compared to those whose parents both were without myopia (29). A multivariate analysis of factors affecting myopia, conducted in 16,771 students aged between 7 and 18 years in Beijing, concluded that the occurrence of myopia was positively correlated with parents' myopia status, with an OR value of 1.35 (30). Therefore, students with a single parent or both parents suffering from myopia should be treated as target groups of myopia prevention.
Our investigation demonstrated that a near work distance ≥33 cm is a potential protective factor for myopia. The cohort study conducted in Taipei followed 10,743 children aged 9 to 11 years over 2 years. They found that students with a near work distance >30 cm had significantly less myopic progression (31). Two other studies show that shorter working distance is related to higher incidence of myopia (32, 33). Therefore, one of the vital interventions is to develop good eye habits and conscious eye care behaviors.
As primary school age is a crucial period for myopia prevention, it would be appropriate that schools and parents should work together to guide students to develop good eye habits. Myopia among female students is higher than that among male students, which may be due to girls' shorter outdoor activity time, and consequent longer time for study (19, 34). Therefore, additional attention should be paid to female primary school students for myopia prevention and control. Additionally, the increased learning burden and increased time spent on studying could also explain the positive correlation between the myopia rate and increasing grade levels. Hence, it is necessary to persist in and reinforce interventions.
Our investigation also demonstrated that the myopia rate among pupils in urban areas is higher than that in rural areas, which was consistent with the data from other studies conducted in Shanxi province, Wuhan city and so on (35, 36). This difference might be attributable to potential differences in education pressure. Students in urban areas face higher academic pressure from school and family than students in rural areas, while students in rural areas have more opportunities to enjoy outdoor time. Moreover, electronic devices are increasingly popularized in urban areas, and better financial conditions in urban families are accompanied by a higher frequency of using electronic devices such as mobile phones and computers (37). Thus, decreasing the academic burden, encouraging more physical training and outdoor activity, and reducing the utilization of electronic devices in school children remain a priority.
Our study survey found no statistically significant correlation between daily outdoor time and myopia, which conflicted with other findings. One follow-up study in Britain showed that the longer the outdoor activity time of 3–9-year-old children, the lower the myopia prevalence was by the time these children grew up to be 10–15 years of age (38). Besides, another study illustrated that outdoor activity time was negatively correlated with the occurrence of myopia in both 6-year and 12-year age groups (39). In China, a cohort study in Guangdong Province presented that reduced outdoor activity was related to preschool myopia among 1–3-year-old children (40). The other cohort study in northeast China revealed that 20 min of additional outdoor activity every morning and every afternoon could obviously reduce the myopia levels in the intervention group (41). Given the potential home quarantine for all participants and the limited follow-up time, the effect of daily outdoor time might not be easily observed in our study. Nevertheless, we advocate for ensuring sufficient outdoor time to protect the eyesight of teenagers effectively.
Previous study demonstrated that students spend about 4.37 h/day on electronic device during periods of COVID-19 isolation, showing a positive relationship between myopia development and its used time (24). However, our finding did not identify an obvious association between electronic device use and myopia occurrence, which might be contributed to the cancellation of online education during our survey, that may cause the bias for this variable. Considering an increasing association between the used time of electronic device and myopia occurrence, it was still suggested that a wide health education should be performed among patients to reduce electronic device use in pupils.
SE was not only one of the indicators of myopia, but was also an evaluation index for hyperopia reserve. With appropriate hyperopia reserve, the occurrence of myopia among pupils, particularly those in low grades, could be slowed down. Although we did not perform a comparison in our study group, our results showed a mean difference of 0.5 D from grade 2 to grade 3 pupils, whereas this was only 0.31 D among the same age group in the Guangzhou study that was conducted before the COVID-19 pandemic (42). This implied that the risk of developing myopia was greater among students during the COVID-19 epidemic. Thus, health education and target interventions should be emphasized among primary school children to ensure that they have an adequate hyperopia reserve. This will undoubtedly benefit the prevention and control of myopia.
Some limitations of the study should be noted. First, since the diopter examination in the myopia screening was not performed under cycloplegic conditions, the observed myopia rate and the real rate may have differed. Second, we did not collect data on myopia before 2020, which might limit further analysis of the change trend before and after COVID-19.
5. Conclusion
In this study, the myopia rate among primary school students in Eastern China was high during the COVID-19 pandemic. The myopia rate among female students was higher than that among male students, and that among students living in urban areas was higher than that among students living in rural areas. Additionally, students with near work distance <33 cm, and those who had parents with myopia, were at greater risk of developing myopia. Thus, further attention and implementation of interventions, such as development of good eye habits, from health and education departments, are needed particularly in primary school students.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Ningbo Yinzhou No.2 hospital. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
SH: writing—original draft, methodology, software, and funding acquisition. FS: data collection, investigation implementation, validation, formal analysis, and supervision. FZ: investigation implementation, software, and formal analysis. QG: supervision and methodology. KL: writing—review and editing and conceptualization. WF: visualization, software, conceptualization, funding acquisition, and supervision. DC: methodology and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Social Development Scientific Research Project of Fenghua District (201904401), the Science and Technology Plan Project of Ningbo (2022S077), the Natural Science Foundation of Ningbo (202003N4295), and General Health Foundation of Zhejiang Province (2021KY1067).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1167379/full#supplementary-material
References
1. Ma Y, Wen Y, Zhong H, Lin S, Liang L, Yang Y, et al. Healthcare utilization and economic burden of myopia in urban China: a nationwide cost-of-illness study. J Glob Health. (2022) 12:11003. doi: 10.7189/jogh.12.11003
2. Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. (2020) 20:27. doi: 10.1186/s12886-019-1220-0
3. Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modeling. Ophthalmology. (2019) 126:338–46. doi: 10.1016/j.ophtha.2018.10.029
4. Wang SK, Guo Y, Liao C, Chen Y, Su G, Zhang G, et al. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. (2018) 136:1017–24. doi: 10.1001/jamaophthalmol.2018.2658
5. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
7. Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. (2016) 100:882–90. doi: 10.1136/bjophthalmol-2015-307724
8. Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ. (2018) 361:k2022. doi: 10.1136/bmj.k2022
9. Dong YH, Liu HB, Wang ZH, Yang ZP, Xu RB, Yang ZG, et al. [Prevalence of myopia and increase trend in children and adolescents aged 7-18 years in Han ethnic group in China, 2005-2014]. Zhonghua Liu Xing Bing Xue Za Zhi. (2017) 38:583–7. doi: 10.3760/cma.j.issn.0254-6450.2017.05.005
10. Kang ZF, Tao FF, Jing J, Xu XM, Su LY. A meta-analysis for prevalence of myopia among Chinese teenagers. J Clin Ophthalmol. (2016) 05:395–9.
11. Liu C, Liu WL, Wang J, He MM. Meta analysis of myopia prevalence among primary and secondary school students in China from 2018–2020. Occup Health. (2021) 22:3145–48. doi: 10.13329/j.cnki.zyyjk.2021.0780
12. Annechien EG. Haarman CAEJ: The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. (2020) 4:49. doi: 10.1167/iovs.61.4.49
13. Verhoeven VJ, Wong KT, Buitendijk GH, Hofman A, Vingerling JR, et al. Visual consequences of refractive errors in the general population. Ophthalmology. (2015) 122:101–9. doi: 10.1016/j.ophtha.2014.07.030
14. Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P: Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. (2014) 157:9–25. doi: 10.1016/j.ajo.2013.08.010
15. Richter GM, Torres M, Choudhury F, Azen SP, Varma R. Risk factors for cortical, nuclear, posterior subcapsular, and mixed lens opacities: the Los Angeles Latino Eye Study. Ophthalmology. (2012) 119:547–54. doi: 10.1016/j.ophtha.2011.09.005
16. Cyril KA, Raju A, Luthra G, Shahbaz M, Almatooq H, Foucambert P, et al. The impact of the COVID-19 pandemic on myopia progression in children: a systematic review. Cureus. (2022) 14:e28444. doi: 10.7759/cureus.28444
17. Karthikeyan SK, Ashwini DL, Priyanka M, Nayak A, Biswas S. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: an overview of systematic reviews and meta-analyses. Indian J Ophthalmol. (2022) 70:728–39. doi: 10.4103/ijo.IJO_1564_21
18. Gajjar S, Ostrin LA. A systematic review of near work and myopia: measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol. (2022) 100:376–87. doi: 10.1111/aos.15043
19. Xu L, Zhuang Y, Zhang G, Ma Y, Yuan J, Tu C, et al. Design, methodology, and baseline of whole city-million scale children and adolescents myopia survey (CAMS) in Wenzhou, China. Eye Vis. (2021) 8:31. doi: 10.1186/s40662-021-00255-1
20. Xiang ZY, Zou HD. Recent epidemiology study data of myopia. J Ophthalmol. (2020) 2020:4395278. doi: 10.1155/2020/4395278
21. Wang J, Li Y, Zhao Z, Wei N, Qi X, Ding G, et al. School-based epidemiology study of myopia in Tianjin, China. Int Ophthalmol. (2020) 40:2213–22. doi: 10.1007/s10792-020-01400-w
22. Ma FF, Luo H, Zhao GH, Luo XL. The prevalence and progression of myopia in elementary school students in Shanxi Province, China during the COVID-19 pandemic. Semin Ophthalmol. (2022) 37:756–66. doi: 10.1080/08820538.2022.2087474
23. Ma M, Xiong S, Zhao S, Zheng Z, Sun T, Li C. COVID-19 home quarantine accelerated the progression of myopia in children aged 7 to 12 years in China. Invest Ophthalmol Vis Sci. (2021) 62:37. doi: 10.1167/iovs.62.10.37
24. Ma D, Wei S, Li SM, Yang X, Cao K, Hu J, et al. Progression of myopia in a natural cohort of Chinese children during COVID-19 pandemic. Graefes Arch Clin Exp Ophthalmol. (2021) 259:2813–20. doi: 10.1007/s00417-021-05305-x
25. Watcharapalakorn A, Poyomtip T, Tawonkasiwattanakun P. Coronavirus disease 2019 outbreak and associated public health measures increase the progression of myopia among children and adolescents: evidence synthesis. Ophthalmic Physiol Opt. (2022) 42:744–52. doi: 10.1111/opo.12976
26. Aslan F, Sahinoglu-Keskek N. The effect of home education on myopia progression in children during the COVID-19 pandemic. Eye. (2022) 36:1427–32. doi: 10.1038/s41433-021-01655-2
27. Mohan A, Sen P, Peeush P, Shah C, Jain E. Impact of online classes and home confinement on myopia progression in children during COVID-19 pandemic: Digital eye strain among kids (DESK) study 4. Indian J Ophthalmol. (2022) 70:241–5. doi: 10.4103/ijo.IJO_1721_21
28. Alvarez-Peregrina C, Martinez-Perez C, Villa-Collar C, Andreu-Vazquez C, Ruiz-Pomeda A, Sanchez-Tena MA. Impact of COVID-19 Home Confinement in Children's Refractive Errors. Int J Environ Res Public Health. (2021) 18:5347. doi: 10.3390/ijerph18105347
29. Lim LT, Gong Y, Ah-Kee EY, Xiao G, Zhang X, Yu S: Impact of parental history of myopia on the development of myopia in mainland china school-aged children. Ophthalmol Eye Dis. (2014) 6:31–5. doi: 10.4137/OED.S16031
30. You QS, Wu LJ, Duan JL, Luo YX, Liu LJ Li X, Gao Q, et al. Factors associated with myopia in school children in China: the Beijing childhood eye study. PLoS One. (2012) 7:e52668. doi: 10.1371/journal.pone.0052668
31. Huang PC, Hsiao YC, Tsai CY, Tsai DC, Chen CW, Hsu CC, et al. Protective behaviours of near work and time outdoors in myopia prevalence and progression in myopic children: a 2-year prospective population study. Br J Ophthalmol. (2020) 104:956–61. doi: 10.1136/bjophthalmol-2019-314101
32. Yao L, Qi LS, Wang XF, Tian Q, Yang QH, Wu TY, et al. Refractive change and incidence of myopia among a group of highly selected senior high school students in China: a prospective study in an aviation cadet prerecruitment class. Invest Ophthalmol Vis Sci. (2019) 60:1344–52. doi: 10.1167/iovs.17-23506
33. Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, Mitchell P. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. (2008) 49:2903–10. doi: 10.1167/iovs.07-0804
34. Zhang Y, Zhou GX, Miao C, Shi YF. Prevalence of myopia in school students in Yuyao, Zhejiang. Dis Surveil. (2021) 12:1347–50. doi: 10.3784/jbjc.202101190031
35. Wang H, Zhang X, Huo J, Hou L, Meng Y, Zhang Y, et al. Analysis on the status quo and risk factors of myopia among primary school students from grade 4 to grade 6 in Shanxi Province. Chin J Health Educ. (2022) 6:483–90. doi: 10.16168/j.cnki.issn.1002-9982.2022.06.001
36. Shi MD, Wand HJ, Wu Y, Wang X, Wu XM. Analysis on current situation and influencing factors of myopia among primary and middle school students in Wuhan City in 2019. Occup Health. (2022) 38:534–7. doi: 10.13329/j.cnki.zyyjk.2022.0138
37. Yuan XL, Liu KQ, Wang YY, Xu T, Zheng XG, Yang ZY, et al. Relationship between screen time and myopia in children aged 11–14 years in China. Chin J School Health. (2022) 43:333–7. doi: 10.16835/j.cnki.1000-9817.2022.03.004
38. Shah RL, Huang Y, Guggenheim JA, Williams C. Time Outdoors at Specific Ages During Early Childhood and the Risk of Incident Myopia. Invest Ophthalmol Vis Sci. (2017) 58:1158–66. doi: 10.1167/iovs.16-20894
39. French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. (2013) 120:2100–8. doi: 10.1016/j.ophtha.2013.02.035
40. He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. (2015) 314:1142–8. doi: 10.1001/jama.2015.10803
41. Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun eye care study. BMC Ophthalmol. (2015) 15:73. doi: 10.1186/s12886-015-0052-9
Keywords: COVID-19, primary school, influencing factor, myopia, pupil
Citation: Huang S, Shen F, Zhou F, Gong Q, Liu K, Feng W and Cen D (2023) Myopia in elementary school students in Eastern China during the COVID-19 pandemic. Front. Public Health 11:1167379. doi: 10.3389/fpubh.2023.1167379
Received: 16 February 2023; Accepted: 30 May 2023;
Published: 21 June 2023.
Edited by:
Amir Almasi-Hashiani, Arak University of Medical Sciences, IranReviewed by:
Jun Jiang, Wenzhou Medical University, ChinaAzim Siraj Azimuddin, Ministry of Health, Brunei
Copyright © 2023 Huang, Shen, Zhou, Gong, Liu, Feng and Cen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kui Liu, a2xpdUBjZGMuemouY24=; Wei Feng, Zmhmd2hoeHgxMTExQDE2My5jb20=; Dong Cen, Y2VuZG9uZzIwMDJAMTI2LmNvbQ==
 Shuaishuai Huang
Shuaishuai Huang Fanhan Shen2
Fanhan Shen2 Qinghai Gong
Qinghai Gong Kui Liu
Kui Liu