
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 18 July 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1165858
Background: There is improved access to Sever Acute Malnutrition management in Ethiopia; however, studies have revealed an alarming rate of defaulters’ poor recovery and deaths, emphasizing the importance of researching to identify major causes. As a result, the goal of this research is to identify treatment outcome determinants and associated factors in severely malnourished children aged 6–59 months admitted to public hospitals in Eastern Ethiopia’s stabilization centers.
Methods: This study used an institutional-based retrospective cohort study design with 712 children aged 6 to 59 months. Data was gathered using a Sever Acute Malnutrition registration logbook and patient charts. Participants were chosen at random from their respective healthcare facilities based on population proportion. Epi-data was entered and analyzed using STATA version 14. To identify associated factors, the Cox proportional hazard Ratio was calculated, and a p-value of 0.05 at the 95% confidence interval was considered statistically significant.
Results: This study revealed that only 70.65% (95% CI = 67.19, 73.88) of the children were cured while 17.84% defaulted from the management and 5.90% died. Children who did not have tuberculosis (AHR = 1.58, 95%CI:1.04, 2.40), anemia (AHR = 1.31, 95% CI:1.03, 1.68), Kwash dermatosis (AHR = 1.41, 95%CI:1.04, 1.91), or on NG-tube (AHR = 1.71, 95%CI:1.41, 2.08) were more likely to be cured from SAM.
Conclusion: This study discovered that the cure rate is extremely low and the defaulter rate is extremely high. As a result, intervention modalities that address the identified factor are strongly recommended to accelerate the rate of recovery in Eastern Ethiopia.
Severe acute malnutrition (SAM) is a nutritional deterioration identified by anthropometric indicators such as a WH/L -3Z score or MUAC 11.5 cm and/or the presence of nutritional edema (1, 2). Malnutrition remains a major public health issue worldwide, with 149.2(22%) million under-five children stunted, 45.4(6.7%) million under-five children wasted, and 38.9(5.7%) million children undernutrition. According to studies, more than half of all wasted children live in Southern Asia (SA) and Sub-Saharan Africa (SSA). In Africa, more than 12 million under-five children were wasted, of which 3 million were SAM (3). In addition, according to Ethiopian Mini-Demographic and Health Survey 2019 (Mini-EDHS 2019) reported that 7% of under-five children are wasted (4).
Even though SAM is a preventable cause of under-five children mortality and morbidity, children with SAM were nine times more likely to die compared to their counterparts (5). Thus, SAM is responsible for the deaths of 3.6 million children under the age of five worldwide, with 45–60% of these deaths occurring in low- and middle-income countries (LIMC) (6). Despite advances in child health and nutritional interventions (7), undernutrition was responsible for more than 28% of child deaths in Ethiopia (8).
Children with SAM and medical complications such as clinical signs of infection, severe edema and or anemia, metabolic disturbance, vomiting, hypothermia, dehydration, and poor appetite must be admitted to a stabilization center, according to the WHO protocol. According to the guidelines, they are primarily treated with F75 during stabilization and F100 or ready-to-use therapeutic foods (RUTF) during the transition, as well as other standard medications such as antibiotics, deworming, folic acid, and vitamin A.
A recent systematic review conducted in SSA and Ethiopia found that the recovery rate from SAM remains as low as 71.2 and 72.02%, respectively (9, 10). Other pocket studies in Ethiopia reported that the recovery rates ranged from 58.4% in the Bahir Dare referral Hospital to 70.4% in Yekatit 12 Ethiopian Hospitals (6, 11–15). Similarly, previous studies in Ethiopia also discovered that children’s socio-demographic and economic factors and baseline anthropometric characteristics, medical-related factors, adherence to the treatment protocol, duration of follow-up, and types of comorbidity on admission were the underlying determinants of treatment recovery (6, 11–15). However, to the knowledge of these researchers, there are no published studies that assessed the recovery rates from two regions of eastern Ethiopia among children admitted to stabilization centers. As a result, the main objective of this study was to identify the recovery rate and associated factors among under-five children with SAM admitted to public hospitals in Eastern Ethiopia’s stabilization centers.
This study was carried out at two public hospitals in East Hararghe Zone, Haramaya and Chelenko hospitals, as well as Hiwot-Fana specialized hospital in Harari Regional state, from December 10 to 30, 2021. Harar, located 525 kilometers east of Addis Abeba, served as the regional capital city of Harari as well as the East Hararghe Zone’s Zonal Administrative Center. Eastern Hararge zone is the most populous of the Oromia regional state’s 24 zones, with a total population of 3.7 million (16). There are six public hospitals, 121 health centers, and 548 health posts in this zone. The Harari Region of Ethiopia is one of nine regional states. There are a total of 232,000 people, with 116,928 men and 115,072 women. One military hospital, two public hospitals, one private hospital, and eight health centers are available.
An institutional retrospective cohort study was conducted among children aged 6 to 59 months who were admitted to randomly selected hospitals. The study population consisted of records of children aged 6–59 months admitted to stabilization centers in public hospitals in East Hararghe and Harari Region with the diagnosis of SAM. The study excluded records with missing or incorrect information.
The sample size was determined using Epi-info, Version 7.2, under the following assumptions: This study used anemia on admission as an exposure variable, with a 95% CI and a power of 80%. The percentages of recovery among the unexposed-to-anemia and exposed-to-anemia groups were 75.42 and 63%, respectively. Then a one-to-one ratio of unexposed to exposed, a 1.5 design effect, and 15% accounting for missing or incomplete data (11). As a result, the final sample size was 744.
In this study, a two-stage cluster sampling technique was used. All public hospitals in East Hararge Zone and Harari Regional State provide SAM inpatient care. Haramaya and Chelenko were chosen from the six East Hararge Zones of Oromia Regional State, and Hiwot-Fana specialized university hospital was chosen from two public hospitals in Harari Regional State. Each hospital had its sampling frame, and the registration log book was used to identify eligible SAM patients admitted to the chosen hospitals. Based on the number of patients seen in the previous 6 months, each hospital received a sample. Finally, eligible study subjects were chosen from each hospital using a systematic random sampling technique.
The checklist was created by combining the standard SAM management treatment protocol, the registration log book, and the SAM monitoring multi-chart. The checklist includes socio-demographics anthropometry (MUAC, weight, and height/length), presences or absences of edema, immunization status, medical diagnosis at admission, and treatment outcome of severe acute malnutrition were collected among the others (2) (Attached as supplement at the end of this manuscript).
Two supervisors and five data collectors (with BSc clinical Nurse practitioners) with SAM management experience were hired and given 2 days of training on data collection tools. The tool was tested on 5% of the sample size at a nearby public hospital with a comparable population before being included in the study. The pretest findings were discussed among supervisors, data collectors, and the principal investigator to ensure a better understanding of tools and procedures, and the final version was modified as a result. During data collection, the SAM registration log book, the children’s cards or folder, and the SAM monitoring multi-chart were all reviewed. Until the final data collection day, consistency and completeness were checked daily.
The data were double entered EPI Data after being cleaned, coded, and loaded into the Epi Data version 3.1 software and were exported and analyzed using STATA version 14.2 software. The study’s independent variables were described using descriptive statistics such as frequency distribution and percentage. To determine the relationship between the recovery rate and each independent variable, bivariable and multivariable Cox regression analyses were performed. Before running the Cox-proportional hazard, assumption tests were conducted for each variable using a log–log plot and the Schoenfeld residuals test (global test).To account for potential confounders, all variables with p-values less than 0.25 in the bivariable Cox regression analysis were identified and included in the multivariable model. The Cox-Snell plot was used to evaluate the overall fitness of the model. Finally, the AHR 95% confidence interval estimation was used to identify factors associated with recovery from severe acute malnutrition. The variable that shows statistical significance (p-vales < 0.05) in the multivariable analysis was considered statistically significant.
In this study, 712 children’s records were included in the analysis from a total sample size of 744, with a completeness rate of 96% and 32 records being incomplete and excluded. The majority of the children (55.34%) were males between the ages of 12 and 23 months (median age = 18 months), with 353 (49.58%) breastfeeding at the time of admission. 625 (87.78%) of the total study participants were admitted as new cases of SAM children, with 513 (72.05%) referred from a health facility. Malnutrition was classified as marasmus, Marasmic-Kwashiorkor, or kwashiorkor in 420 (58.99%), 163 (22.89%), and 129 (18.12%) cases, respectively. The mean weight and MUAC of children during admission were 7.12 kg (SD 2.25) and 11.25 kg (SD 1.31), respectively (Table 1).
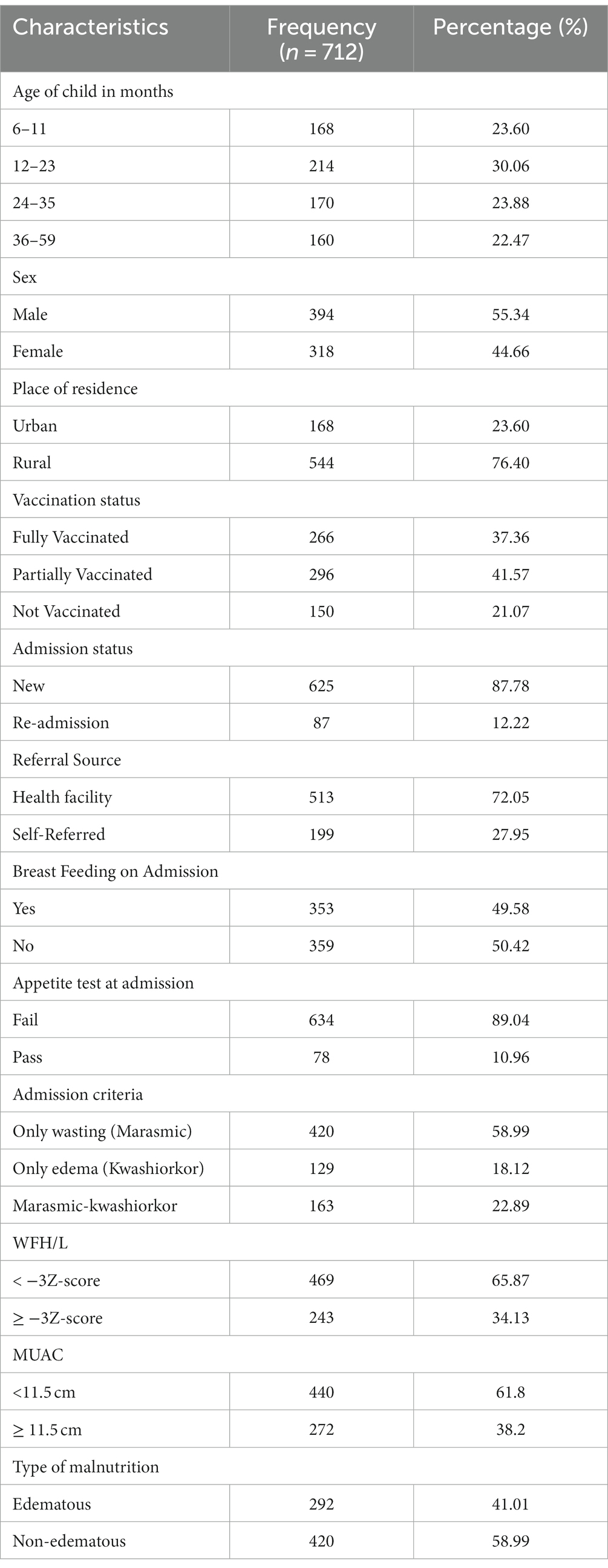
Table 1. Socio-demographic and characters of the children aged 6–59 months admitted to SC of selected public hospitals in East Hararghe Zone and Harari Region, Ethiopia.
Ampicillin, gentamycin, and ceftriaxone were administered intravenously to nearly all of the admitted children (97.05%). Furthermore, F-75 therapeutic milk was given to 89.33% of malnourished children, 74.02% were given F-100, and 208 (29.21%) were given plumpy nuts. Following admission, 37.64% of all admitted children were given Vitamin A supplements, and 40.45% were given Folic acid supplements. In comparison, only 5.34% of all children received blood during inpatient treatment, and 3.65% were resuscitated with IV fluid during inpatient waiting time. Almost half of SAM children (43.26%) have an NG tube during treatment. While 30.20% of the children were dewormed following their admission (Table 2).
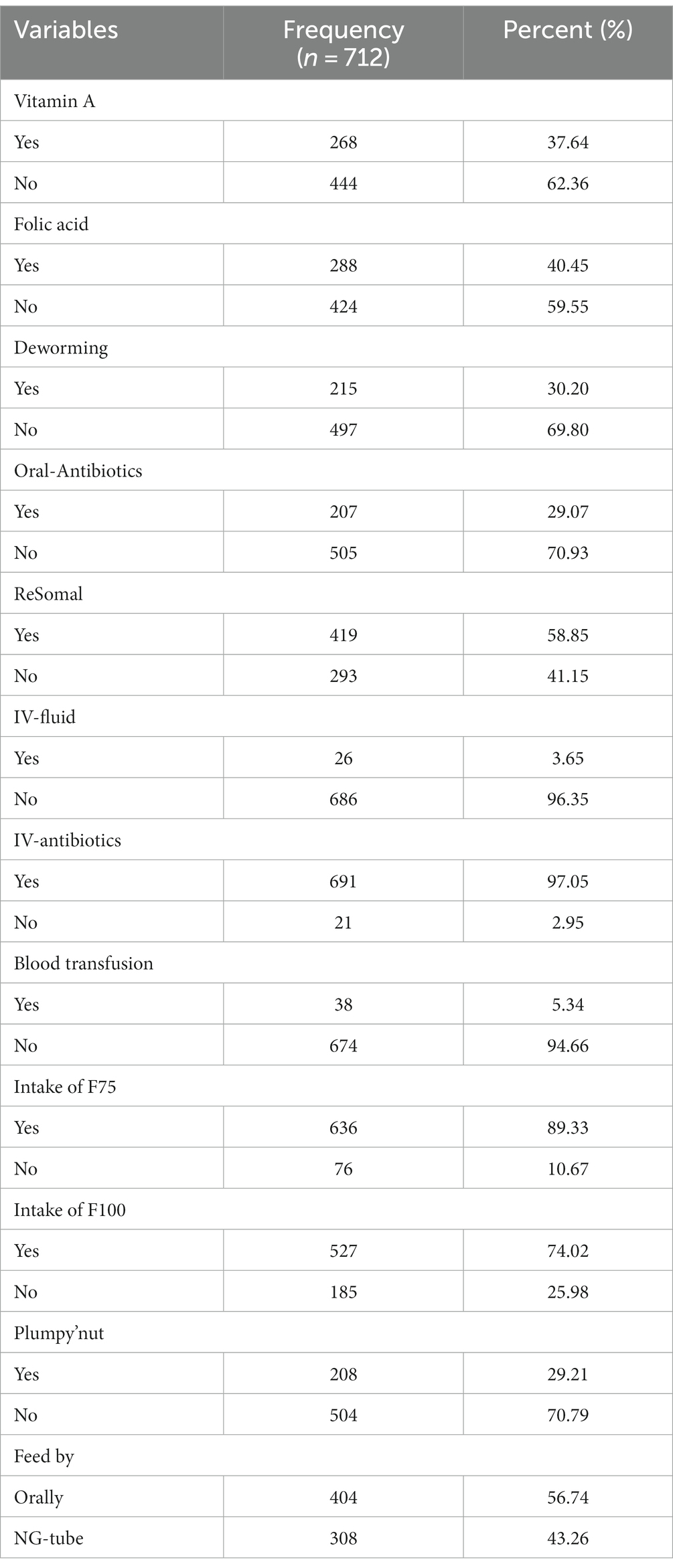
Table 2. Medication provision and mineral supplementation of SAM children aged 6–59 months admitted to SC of selected public hospitals in East Hararghe Zone and Harari Region, Ethiopia.
The majority (95.79%) of children admitted to the stabilization center had at least one type of co-morbidity while 44.38% of children were admitted with three or more. Among those with diagnosed comorbidity, 96.93% had marasmus-kwashiorkor, 97.38% had marasmus, and 89.15% had kwashiorkor at the time of admission. The most common co-morbidities were pneumonia (44.10%), diarrhea (62.64%), and anemia (18.68%; Table 3).
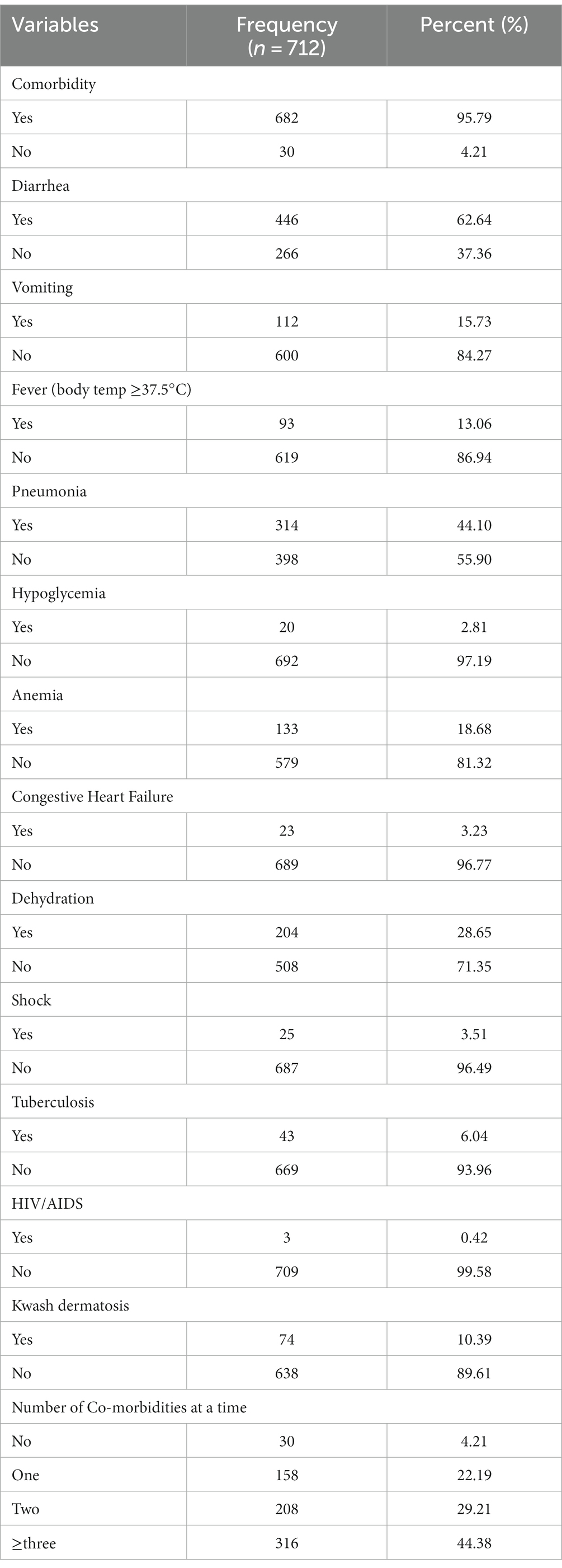
Table 3. Distribution of medical co-morbidity information on treatment outcomes of 6 to 59 months children with SAM admitted to SC of selected public hospitals in East Hararghe Zone and Harari Region, Ethiopia.
In this study, the recovery rate was 70.65% (95% CI: 67.19, 73.88), the death rate was 5.90% (95% CI: 4.39, 7.89), and the default rate was 17.84% (95% CI: 15.19, 20.83). Among those who recovered within 41 days, the median time to recovery was 11 days (95% CI:10, 12), and the incidence of recovery was 8.4 (95% CI: 7.6, 9.1) per 100 person-day observations. The average (SD) weight gain of a severely malnourished child was 13.65(9.2) g/kg/day. The mean (standard deviation) length of stay for recovered edematous and non-edematous children was 12.3(5.98) days and 11.6(5.47) days, with no statistically significant difference [p = 0.5626; 220 (75.34%)]. The overall performance of the hospitals, as well as their SPHERE indicators, are shown below (Table 4).
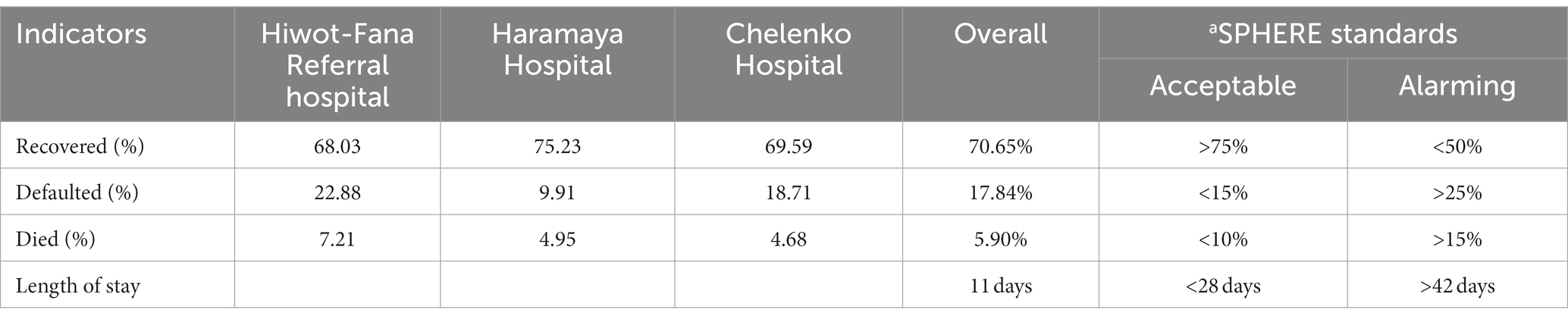
Table 4. Performance indicator of stabilization center of selected public hospitals in East Hararghe Zone and Harari Region, as compared to sphere project reference values/international standard.
In this analysis, 13 variables with p-values less than 0.25 were chosen for multivariable Cox regression. Referral source, vaccination status, admission status, vitamin A administration, fever, pneumonia, anemia, folic acid administration, tuberculosis, having an NG-tube during admission, dehydration during admission, presence with shock, and having Kwash dermatosis on admission are all included. After controlling for potential confounding effects on the outcome variable, factors such as the presence of anemia and tuberculosis during admission, Kwash dermatosis, and NG-tube placement during admission remained significantly associated with treatment recovery. As a result, children who did not have TB infection were 1.58 (AHR = 1.58, 95%CI: 1.04, 2.40) times more likely than those who did recover from SAM. Children aged 6–59 months who did not have an NG-tube during their admission had a 1.71 times higher chance of completing treatment than children who did (AHR = 1.71, 95%CI:1.41, 2.08). Furthermore, children who did not have anemia had a 1.31 (AHR = 1.31, 95% CI:1.03, 1.68) higher chance of recovering from SAM than those who did. Similarly, children who did not have Kwash dermatosis at the time of admission were 1.41 (AHR = 1.41, 95%CI:1.04, 1.91) times more likely than children who did recover from SAM (Table 5).
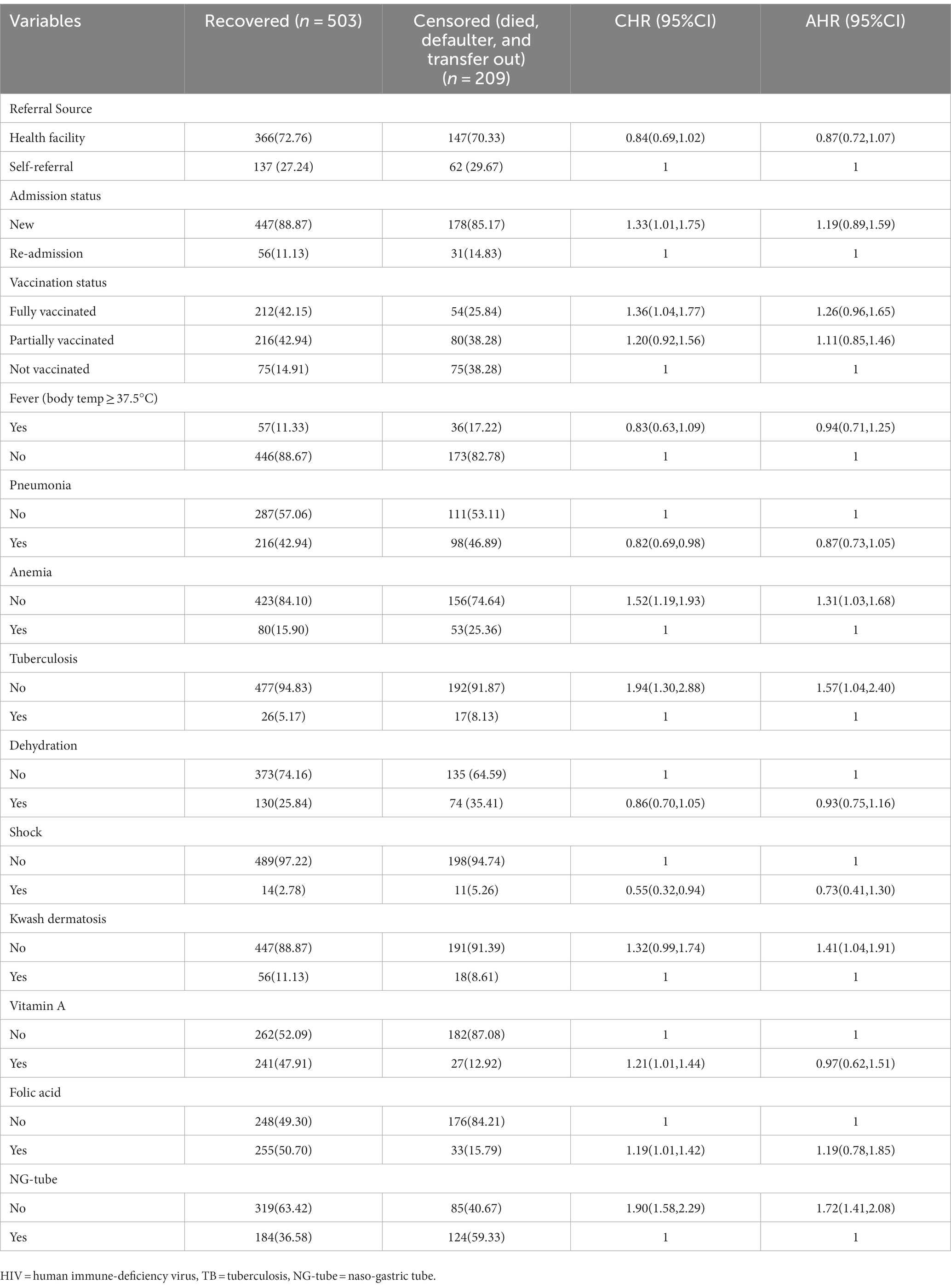
Table 5. Bivariable and multivariable Cox-regression analysis of factors associated with recovery among children admitted with SAM to SC of selected public hospitals in East Hararghe Zone and Harari Region, Ethiopia.
According to this study, 70.65% of children recovered, which falls short of the minimum acceptable international SPHERE standards (>75%) (1). However, the recovery rate in this study was similar to that of Yekatit 12 Hospital Medical College (70.4%) (15) and Lacor Hospital of Uganda (70.6%) (17), while higher than that of Bangladesh (55.7%) (18), Sudan (57.4%) (19), Nigeria (48.5%) (20). In contrast, the recovery rate of this study was lower than that of India (81%) (21), Wag Himra Zone, Northeast Ethiopia (80.4%) (22), Yirgalem Hospital (78%) (23), and Yekatit 12 Hospital (81.3%) (24). The reasons for the low recovery rate in this study compared to other studies could be attributed to an unacceptable higher defaulter rate, differences in socioeconomic status, quality of care provided for children, health-seeking behavior, and the availability and accessibility of therapeutic foods and medications.
Similarly, the default rate of this study was 17.84%, which was higher than the minimum acceptable international SPHERE standards (15%) (1). However, the default rate in this study was in line with Gondar University Comprehensive Specialized Hospital’s 17.79% (11), while higher than Zambia’s 17.2% (17), Pawe general hospital’s 16.52% (6), and Wag Himra Zone, Amhara National Regional State’s 8.2% (22). In contrast, the default rate of this study was lower than that of Bangladesh, which was 29.9% (18), Bahir Dar Felege Hiwot Referral Hospital, which was 21.7% (13), and Ayder referral hospital, which was 43.6% (25). Differences in study sitting, socioeconomic status, quality of care provided for children, health-seeking behavior, and availability and accessibility of therapeutic foods and medications are all possible reasons for the higher default rate in this study.
This study’s participants’ overall median nutritional recovery time was 11 days (IQR: 9–13). The findings are consistent with those of studies conducted in Pawe General Hospital, North West Ethiopia (6), Gonder referral hospitals (11), and Wag Himra Zone, Northeast Ethiopia (22), but they are lower than those of Pawe General Hospital (26), Hawassa Specialized (12). The disparity could be explained by differences in study settings, as some studies were conducted in referral and specialized hospitals where children with the most severe SAM cases are referred.
The presence of other comorbidities at admission greatly influences the prognosis of SAM. The humeral and cell-mediated immunity of children affected by SAM may be depressed and unable to protect children from infection, which may be attributable to the high prevalence of infection. In this study, for example, children who did not have tuberculosis were 1.58 times more likely to recover from SAM than those who did. This study was consistent with research done at Gondar Comprehensive Specialized Hospital (11), Benishangul-Gumuz, Pawi General Hospital (26), Jimma University (27), and Southern Ethiopia (12). Weight loss decreased appetite, and nutrient absorption may occur as a result of tuberculosis infection. This suggests that children with tuberculosis require a longer hospital stay because they have a greater nutritional crisis and require more nutrients than their peers (28).
In this study, we discovered that SAM children who did not have anemia had 1.31 times the chance of recovery as those who did. This finding was consistent with those from the WagHimra Zone in northeast Ethiopia (22), Jimma University Medical Center (27), Gondar Comprehensive Specialized Hospital (11), Nekemte Referral Hospital (14), and Pawi General Hospital (26). This is due to an increase in the prevalence of infection and an increased risk of heart failure in anemic children, resulting in a long time to cure (2).
According to a study conducted at Gondar, children without kwash-dermatosis had a higher probability of recovery (11). This is consistent with our study findings. The possibility is that children with kwash-dermatitis were more prone to infection and metabolic complications, as well as being edematous with more skin lesions, which led to more complications and a longer time to cure and poor appetites.
According to this study children without an NG tube had more likely to recover. A previous study also indicated that children admitted with complicated SAM and who were unable to feed orally were fed via NG tube were more at risk of poor treatment outcomes (29). This result was comparable to the findings of a study conducted in North Wet Ethiopia (6). The presence of an NG tube during admission may result in complications such as diarrhea, vomiting, lung aspiration, and electrolytic alterations, which will reduce the treatment cure rate (30).
The study’s limitations included the difficulty of determining the reliability of recorded data due to the nature of secondary data, as well as failure to address variables such as educational status, household wealth index, socioeconomic status, household family size, and child’s feeding practice that may affect treatment outcome.
This study found that the recovery rate was low with higher defaulter rate compared to the sphere standard guideline. Thus, prompt and timely management of tuberculosis, anemia, and kwash-dermatosis should be prioritized, as should reducing the use of NG tubes for feeding and medications after admission. Finally, we recommend additional research to determine the cause of this study’s low cure rate and high defaulter rate.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
This study’s methods were all carried out following the Helsinki Declaration-Ethical principle for medical research involving human subjects. Haramaya University’s Institutional Research Ethics and Review Committee (IRERC) provided an ethical approval letter with the reference number IHRERC/102/2021. Heads of hospitals provided informed written voluntary signed consent. Because the study was conducted through a review of records, no consent from study subjects is required. All personal identifiers were removed, and data was kept private and only used for the proposed study.
All authors made significant intellectual contributions to the study’s conception and design, as well as data acquisition, analysis, and interpretation. JA wrote the manuscript, which KR and TW reviewed for intellectual content. All authors contributed to the article and approved the submitted version.
We would like to express our heartfelt gratitude to Haramaya University for this research. Special thanks go to hospital administrators and their staff for their tremendous assistance during the data collection period. Finally, we would like to express our gratitude to all data collectors and supervisors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1165858/full#supplementary-material
AHR, Adjusted hazard ratio; CHR, Crude hazard ratio; CI, Confidence interval; EDHS, Demographic and Health Survey; FMOH, Federal ministry of health; HIV/AIDS, IV, intravenous; MUAC, mid-upper arm circumference; RUTF, Ready-to-use therapeutic foods; SAA, Sub-Saharan Africa; SA, Southern Asia; SAM, Severe acute malnutrition; SC, Stabilization center; SD, Standard deviation; NG, Nasogastric; WFH/L, Weight for height/length; WHO, World Health Organization.
1. Sphere Association. The sphere handbook: humanitarian charter and minimum standards in humanitarian response. In: Geneva. fourth ed. Sphere Association: Switzerland (2018). 2018.
2. WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: W.H. Organization (2013).
3. UNICEF/WHO/WBG. Levels and trends in child malnutrition: UNICEF/WHO/the World Bank Group joint child malnutrition estimates: Key findings of the 2021 edition. Geneva: World Health Organization (2021).
4. Central Statistical Agency (CSA) (2019). [Ethiopia] and ICF, Ethiopia Mini Demographic and Health Survey 2019. Addis Ababa, Ethiopia.
6. Bizuneh, FK, and Bekonjo, NE. Treatment cure rate and associated factors of sever acute malnutrition 6-59 month children treated in therapeutic Center in Pawe General Hospital: Nourth wet Ethiopia. J Nutri Med Diet Care. (2021) 7:51. doi: 10.23937/2572-3278/1510051
7. NIPN (2020). The National Nutrition Program (2016–2020) Progress analysis: Evidence for the upcoming Food and Nutrition Strategy Development, in National Information Platform for Nutrition (NIPN). NiPN-Ethiopia: Addis Ababa.
8. Central Statistical Agency (CSA) (2016). [Ethiopia] and ICF, Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia and Rockville, Maryland, USA: CSA and ICF.CSA.
9. Desyibelew, HD, Bayih, MT, Baraki, AG, and Dadi, AF. A systematic review and meta-analysis of observational studies. PLoS One. (2020) 15. doi: 10.1371/journal.pone.0229698
10. Yazew, KG, Kassahun, CW, Ewnetie, AW, Mekonen, HK, and Abagez, ES. Recovery rate and determinants of severe acute malnutrition children treatment in Ethiopia: a systematic review and meta-analysis. Access. (2019) 8:323. doi: 10.1186/s13643-019-1249-4
11. Wagnew, F, Dejenu, G, Eshetie, S, Alebel, A, Worku, W, and Abajobir, AA. Treatment cure rate and its predictors among children with severe acute malnutrition in Northwest Ethiopia: A retrospective record review. PLoS One. (2019) 14:14(2). doi: 10.1371/journal.pone.0211628
12. Fikrie, A, Alemayehu, A, and Gebremedhin, S. Treatment outcomes and factors affecting time-to-recovery from severe acute malnutrition in 6–59 months old children admitted to a stabilization center in southern Ethiopia: A retrospective cohort study. Ital J Pediatr. (2019) 45:46. doi: 10.1186/s13052-019-0642-x
13. Desyibelew, HD, Fekadu, A, and Woldie, H. Recovery rate and associated factors of children aaged6 to 59 months admitted with severe acute malnutrition at the in-patient unit of Bahir Dar Felege Hiwot referral hospital therapeutic feeding unite Northwest Ethiopia. PLoS One. (2017) 12:e0171020. doi: 10.1371/journal.pone.0171020
14. Mena, MB, Dedefo, MG, and Billoro, BB. Treatment outcome of severe acute malnutrition and its determinants among Pediatric patients in West Ethiopia. Int J Pediatr. (2018) 2018:1–7. doi: 10.1155/2018/8686501
15. Negussie, AS, and Tadesse, AW. Predictors of undesirable treatment outcomes of severe acute malnutrition among inpatient children in Addis Ababa, Ethiopia: a retrospective cohort study. Open Access. (2020) 20:20. doi: 10.1186/s12889-020-09645-x
16. CSA, POPULATION, and HOUSING CENSUS OF ETHIOPIA. (2007). Central Statistical Agency: Addis Ababa.
17. Mwanza, M, Okop, KJ, and Puoane, T. Evaluation of an outpatient therapeutic program for management of severe acute malnutrition in three districts of the eastern province. Zambia BMC Nutrition. (2016) 2:1–9.
18. Choudhury, Z, Chowdhury, D, Hoq, T, Begum, M, and Shamsul Alam, M. A comparative study between SAM with Edema and SAM without Edema and associated factors influencing treatment, outcome & recovery. American Journal of Pediatrics. (2020) 6:468–75. doi: 10.11648/j.ajp.20200604.24
19. Bilal, JA, Elsheikh, AE, Mahgoub, HM, and Adam, I. Poor adherence to the World Health Organisation guidelines of management of severe acute malnutrition in children 6 to 59 months of age at Kalakla Turkish Hospital in Khartoum, Sudan. Sudan. J Paediatr. (2018) 18:70
20. Aliyu, I, Ibrahim, HU, Idris, U, Michael, GC, Ibrahim, UA, Mohammed, A, et al. The clinical profile and outcome of children with acute malnutrition in a tertiary health center in north-West Nigeria: A 1-year retrospective review. J Clin Sci. (2020) 17:120. doi: 10.4103/jcls.jcls_55_19
21. Dhanalakshmi, K, and Devi, CG. The outcome of severe acute malnutrition children admitted to nutrition rehabilitation center of a tertiary level care hospital. Int J Contemp Pediatr. (2017) 4:801–3. doi: 10.18203/2349-3291.ijcp20171490
22. Tadesse, Z, Teshome, DF, Lakew, AM, Debalkie, G, and Gonete, KA. Time to nutritional recovery and its determinants among children aged 6 to 59 months with severe acute malnutrition admitted to stabilization centers of WagHimra zone, Northeast Ethiopia. Ecol Food Nutr. (2021) 60:751–64. doi: 10.1080/03670244.2021.1907746
23. Kabeta, A, and Bekele, G. Factors associated with treatment outcomes of under-five children with severe acute malnutrition admitted to therapeutic feeding unit of Yirgalem hospital. Clinics in Mother and Child Health. (2017) 14:2. doi: 10.4172/2090-7214.1000261
24. Kebede, MA, Teshome, GS, Fenta, FA, and Bantigegn, KA. Recovery time from severe acute malnutrition and associated factors among under-5 children in Yekatit 12 hospital, Addis Ababa, Ethiopia: a retrospective cohort study. EPHI. (2020) 42:e2020003.
25. Tirore, MG, Atey, TM, and Mezgebe, HB. Survival status and factors associated with treatment outcome of severely malnourished children admitted to Ayder referral hospital: a cross-sectional study. BMC Nutrition. (2017) 3:1–9. doi: 10.1186/s40795-017-0186-7
26. Wondim, A, Tigabu, B, and Kelkay, MM. Time to recovery from severe acute malnutrition and its predictors among admitted children aged 6-59 months at the therapeutic feeding Center of Pawi General Hospital, Northwest Ethiopia: A retrospective follow-up study. Int J Pediatr. (2020) 2020:9.
27. Adem, F, Edessa, D, Bayissa, B, Mohammed Hassen, M, and A Mohammed, M. Treatment outcomes and associated factors in hospitalised children with severe acute malnutrition: A prospective cohort study. Dove press. (2020) 11:235–43. doi: 10.2147/PHMT.S253396
28. WHO. Management of severe malnutrition: A manual for physicians and other senior health workers. Geneva: World Health Organization (1999).
29. Chamois, S, Golden, M, and Grellety, Y, (2007). Ethiopia Protocol for the management of Severe Acute Malnutrition (2007).
Keywords: treatment outcome, SAM with complication, east Hararghe, Ethiopia, retrospective study
Citation: Ahmed JA, Yusuf N, Wilfong T, Tukeni KN, Berhanu H and Roba KT (2023) Treatment outcomes among children admitted stabilization centers in Eastern Ethiopia: retrospective study. Front. Public Health 11:1165858. doi: 10.3389/fpubh.2023.1165858
Received: 14 February 2023; Accepted: 04 July 2023;
Published: 18 July 2023.
Edited by:
Edyta Łuszczki, University of Rzeszow, PolandReviewed by:
Olivier Mukuku, Institut Supérieur des Techniques Médicales de Lubumbashi, Democratic Republic of CongoCopyright © 2023 Ahmed, Yusuf, Wilfong, Tukeni, Berhanu and Roba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kedir Teji Roba, a2VkaXIudC5yb2JhQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.