
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 19 October 2023
Sec. Public Health Policy
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1148277
 Chenhao Yu1†
Chenhao Yu1† Yun Xian1†
Yun Xian1† Tiantian Jing1
Tiantian Jing1 Mayangzong Bai1
Mayangzong Bai1 Xueyuan Li2
Xueyuan Li2 Jiahui Li3
Jiahui Li3 Huigang Liang4*
Huigang Liang4* Guangjun Yu1,5*
Guangjun Yu1,5* Zhiruo Zhang1*
Zhiruo Zhang1*Objective: The objective of this study is to explore the association between patient-centered care (PCC) and inpatient healthcare outcomes, including self-reported physical and mental health status, subjective necessity of hospitalization, and physician-induced demand behaviors.
Methods: A cross-sectional survey was conducted to assess patient-centered care among inpatients in comprehensive hospitals through QR codes after discharge from September 2021 to December 2021 and had 5,222 respondents in Jiayuguan, Gansu. The questionnaire included a translated 6-item version of the PCC questionnaire, physician-induced behaviors, and patients' sociodemographic characteristics including gender, household registration, age, and income. Logistic regression analyses were conducted to assess whether PCC promoted self-reported health, the subjective necessity of hospitalization, and decreased physician-induced demand. The interactions between PCC and household registration were implemented to assess the effect of the difference between adequate and inadequate healthcare resources.
Results: PCC promoted the patient's self-reported physical (OR = 4.154, p < 0.001) and mental health (OR = 5.642, p < 0.001) and subjective necessity of hospitalization (OR = 6.160, p < 0.001). Meanwhile, PCC reduced physician-induced demand in advising to buy medicines outside (OR = 0.415, p < 0.001), paying at the outpatient clinic (OR =0.349, p < 0.001), issuing unnecessary or repeated prescriptions and medical tests (OR = 0.320, p < 0.001), and requiring discharge and readmitting (OR = 0.389, p < 0.001).
Conclusion: By improving health outcomes for inpatients and reducing the risk of physician-induced demand, PCC can benefit both patients and health insurance systems. Therefore, PCC should be implemented in healthcare settings.
The WHO advocates for patient-centered care (PCC) in healthcare (1), taking into account patients' perspectives and psychological and interpersonal effects during treatment (2). Despite different definitions of PCC (3), the core of achieving PCC is to inform and involve patients in healthcare (4). The involvement of patients shifts the focus of healthcare from the disease to the patient, which promotes the wellbeing of the patients (2).
PCC has been shown to improve healthcare outcomes for a variety of chronic diseases, including depression and anxiety disorder (5–7), cardiovascular risk management (8–11), diabetes (12–15), and addictive behavior (16). The benefits of PCC include improved patient engagement, which can lead to better treatment outcomes and lower costs. PCC also allows for the integration of multidisciplinary team engagement and nutrient management, which can play a greater role in chronic disease management (17–20).
However, some studies have found that PCC does not have a significant impact on health status. For example, Spall et al. (21) found that PCC treatment did not decrease the readmission rate of heart failure patients. Ma et al. (22) also found that PCC improved the self-efficacy of patients diagnosed with diabetes, but the health status remained the same as the control group.
These findings suggest that the impact of PCC on health status may vary depending on the patient population. For example, PCC may be more effective for patients with psychological conditions, such as anxiety or depression. It is also possible that the heterogeneity of patients in randomized controlled trials (RCTs) has limited the ability to detect a significant effect of PCC on health status. For example, RCTs may exclude patients who are most likely to benefit from PCC, such as the older adult (21, 23).
Overall, the evidence on the impact of PCC on health status is mixed. Therefore, it is still essential to study the association between PCC and health status, as well as the subjective necessity of healthcare utilization in the population. Considering that the role of PCC is realized through all aspects of patients' daily lives, we focus on patients' self-reported health status and subjective necessity of hospitalization. These indicators are not only convenient to collect but also they are reliable in predicting patients' behaviors (24, 25).
Under the World Trade Organization (WTO) framework, the social cost of healthcare must also be considered (26). Some studies of PCC in populations have focused on the cost of treatment, which has led to contradictory findings about the financial effects of PCC.
For example, Liang et al. (23) reviewed PCC in oncology care and found that PCC reduced the utilization of inpatient care and cost. However, the overall positive effects were not statistically significant. Kohler et al. (27) also found that PCC promoted healthcare utilization in primary care and emergency care. David et al. (28) proposed that the contradictory findings may be due to the heterogeneity of patient populations. They found that PCC had differential effects on different patient populations.
From the perspective of information asymmetry between patients and physicians (29), the patient-centered approach can help to reduce information asymmetry between patients and physicians, which can lead to more effective healthcare.
In a patient-centered approach, the physician provides the patient with more information about their treatment plan and disease. This helps to fill the information gap between the patient and physician (2), which can lead to better decision-making. Hence, a patient-centered approach can help to reduce physician-induced demand and patients' self-interested behaviors. Physician-induced demand occurs when a physician orders unnecessary tests or procedures because they believe the patient will want them.
According to the regulations of Chinese healthcare insurance, we focus on four potential healthcare insurance violation behaviors, i.e., advising to buy medicines outside, paying at the outpatient clinic, issuing unnecessary or repeating prescriptions and medical tests, and requiring discharge and readmitting. We focus on these behaviors due to two main reasons. First, physicians may have a financial incentive to do so. They may have an interesting relationship with a specific pharmacy, and they may receive kickbacks or other benefits for referring patients to that pharmacy. Second, physicians may be motivated by performance metrics. The proportion of medicines that are prescribed by a physician is often used as a key performance indicator (KPI). If a physician wants to improve the KPI, they may be tempted to advise patients to buy medicines outside of the hospital, even if it is not in the best interests of the patient. Meanwhile, the average length of hospital stay is also a KPI; hence the physician may be tempted to advise patients to pay at the outpatient clinic and require discharge and readmitting.
Focusing on the expense caused by physician-induced demand has two advantages over direct comparison of expense. On one hand, healthcare expenses can vary due to the patient's physical condition and diagnosis techniques, which makes it difficult to compare expenses between different patients directly (23). Moreover, the expense caused by physician-induced demand can be identified by the specific behaviors prohibited by regulation, which avoids the need for a direct comparison of expenses. On the other hand, reducing physician-induced demand is a more critical issue in the sustainability of healthcare insurance (30). Therefore, we focus on whether PCC can reduce the expense caused by healthcare insurance fraud.
In summary, this study explored whether PCC could promote patients' self-reported health status and subjective necessity of hospitalization and reduce physician-induced demand.
The study was conducted in the secondary and tertiary hospitals of Jiayuguan, a prefecture-level city in northwestern Gansu province in China, with 312,000 residents. To keep the representativeness of the sample, this study includes the inpatients of the tertiary (tertiary referral) and secondary (regional or district) comprehensive hospitals in Jiayuguan.
This study distributed questionnaires among inpatients (n = 5,222) by posting QR codes. The survey of the study was implemented from September 2021 to December 2021. The incomplete questionnaires were removed (n = 23). Research ethics approval was obtained from Shanghai Jiao Tong University School of Medicine (protocol code STUPN-202203). All participants were given informed consent before the study began.
A translated version of the 6-item patient-centered care scale developed by Keating et al. (31) was used to assess patient-centered care. The scale uses a five-point Likert scale, ranging from 1 (never) to 5 (always), to assess the degree to which patients agree with statements about their care. One item, “Does your physician take enough time to answer your questions?” was deleted from the scale for two reasons. First, nurses spend more time communicating directly with hospitalized patients, so the communication between patients and physicians may compete with the communication between patients and nurses (32, 33). Second, Cronbach's alpha of the scale increased from 0.53 to 0.88 after this item was deleted, and the item had a very low correlation with the other items (detailed in Figure 1). The average score was used to reflect the level of PCC perceived by the patient, with higher scores representing higher PCC. The 6-item scale was also implemented in the supplementary document to improve the robustness of the study (see details in Supplementary Tables 1, 2).
The self-reported health status was assessed using three questions: “How would you rate your current physical/mental health?” and “How much do you think your hospitalization is necessary?” The questions were answered on a scale of 1 (absolutely disagree/very bad) to 5 (absolutely agree/very good). The participants were inpatients, and the questionnaires were collected when they were filling discharge procedures. Therefore, the self-reported health status can be used to measure the effect of healthcare.
To assess the physician-induced demand (34), we have collected information about whether the physician performed the following behaviors which had been prohibited by regulations, i.e., advising to buy medicines outside, paying at the outpatient clinic, issuing unnecessary or repeated prescriptions and medical tests, and requiring discharge and readmitting.
The control variables include the types of household registration (0 = agricultural household registration, 1 = non-agricultural household registration) that would not only indirectly affect the occupation or work sector but also affect the type of medical insurance for inpatients, gender (0 = male, 1 = female), age, education status (0 = did (or not) finish primary school, 1 = junior high school, 2 = high school or secondary school, 3 = college, 4 = undergraduate, 5 = master degree, and 6 = doctoral degree), marital status (0 = unmarried, 1 = married, 2 = divorced, and 3 = widowed), and average yearly income (0 = lower than 2800 Yuan, 1 = 2,801–10,000 Yuan, 2 = 10,001–30,000 Yuan, 3 = 30,001–100,000 Yuan, 4 = 100,001–300,000 Yuan, and 5 = more than 300,001 Yuan).
Multiple logistic regressions were implemented to estimate the effect of PCC. We used health status and perceived necessity to healthcare utilization as binary variables, with a value of 1 indicating a response of >3 (35). To account for the group characteristics of different hospitals during data collection, we controlled for the random effect from different hospitals and used a robust cluster estimator (36) grouping with the hospital. All statistical analyses were performed in R 4.1.1 with the packages psych 2.2.9 and RMS 6.4-0.
The socioeconomic status of participants is presented in Table 1. The majority of participants were female (52.4%) and urban residents (76.1%). The mean age was 48.76 years old. Most participants had an annual income of <100,000 yuan. Only 6.7% of participants did not have government-provided healthcare insurance.
Table 2 presents the association between PCC and health status. Based on the identification, PCC played as a protective factor for self-reported physical health status (OR = 4.154, p < 0.001) and self-reported mental health status (OR =5.642, p < 0.001). PCC also promotes the patient's subjective necessity of hospitalization (OR =6.160, p < 0.001).
We found that household registration status had different effects on the three outcomes. This led us to estimate whether household registration status interacted with patient-centered care (PCC). As shown in Figure 2 and columns (4–6) of Table 2, we found that when the mean score of PCC was above 4, the self-reported physical and mental health of urban residents was lower than those of agricultural household registration individuals.
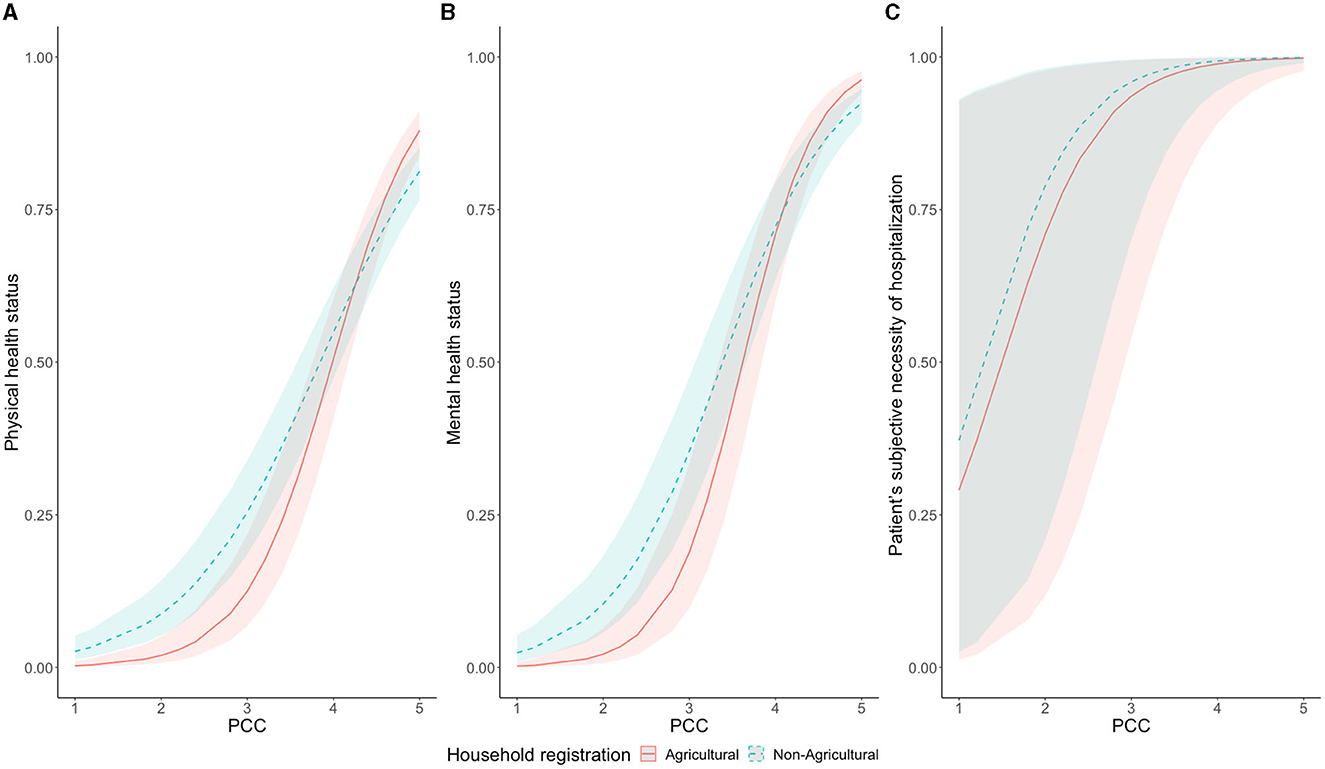
Figure 2. The interaction relationship between PCC and PHS (A) and MHS (B) and PSN (C). PHS, Physical health status; MHS, Mental health status; PSN, Patients' subjective necessity of hospitalization; PCC, Patient-centered care.
Table 3 shows the association between PCC and physician-induced demand. A higher PCC score was associated with a lower probability of physician-induced demand. Notably, the role of PCC was close and sufficient in all four healthcare insurance violations. From the perspective of comparing the scale of coefficients, PCC could prevent physicians from issuing unnecessary or repeated prescriptions and medical tests (OR = 0.320, p < 0.001), which was most relevant to physician self-interest. We also found that marital status could change physician behavior. Married patients had a higher opportunity to be advised to buy medicines outside (OR = 1.385, p < 0.001) or to pay at the outpatient clinic (OR = 3.221, p < 0.001), which were usually done by the spouse of the patient.
This study conducted a large population survey on inpatients in Jiayuguan to explore the association between patient-centered care (PCC), patients' self-reported health status, subjective necessity of hospitalization, and physician-induced demand. The study found that PCC was associated with improved self-reported health status (ps < 0.001) and reduced physician-induced demand (ps < 0.001). These findings provide new evidence on the controversy about the effect of PCC on health status improvement and asymmetric information between physicians and patients.
Unlike previous studies that focused on how to formulate a PCC plan and its effects (37–39), our study provides a macro perspective on the effect of PCC. We found that PCC can generally improve patients' health status and their subjective necessity of hospitalization. Based on the numerous samples from Jiayuguan, we can predict that the association between health status and PCC can be generalized to different types of diseases. Furthermore, our results suggest that PCC can benefit not only chronic diseases but also other diseases by engaging patients in their healthcare plan and providing them with more information and emotional support. As the number of patients with multiple diseases increases due to aging and younger chronic diseases, healthcare orientation needs to shift from disease-centered to patient-centered (40).
PCC is also regarded as a key tool to reduce health disparities (41–43). Considering the large gap in GDP per capita between Jiayuguan and Gansu Province, we tested the different effects of PCC among different socioeconomic status (SES) levels. We used household registration as a moderator to distinguish between high SES and low SES. We found that although PCC can still improve the self-reported physical health and mental health of inpatients, the effect was reduced in the group of non-agricultural household registration. This difference could be caused by the curse effect of education (44) in healthcare, where those with a higher health literacy or better access to medical resources may rank a worse treatment effect during self-report. For inpatients with non-agricultural household registration, due to past prejudices (45), over-care patients are regarded as a kind of palliative care, which leads to the effect of PCC being lower than in inpatients with agricultural household registration.
Considering the epidemiological trend of chronic diseases (46–48) and the current situation of unbalanced medical resources, we believe that providing PCC education in medical education will become an important tool to face future challenges.
The development of PCC has been criticized by some people for the potential of physicians or hospitals to treat patients as consumers (49), taking advantage of asymmetric information to induce unnecessary medical services (50). However, the evidence on whether PCC reduces physician-induced demand is mixed. We believe that the contradictory findings in previous studies are likely due to two factors (23): (1) the treatment plan for a given patient is highly individualized and (2) the treatment methods available to patients can vary depending on the medical technology available. To address these factors, we have focused on a typical identification of four specific behaviors regulated by medical regulations in China.
From the perspective of healthcare expense, this study provided empirical evidence to support that the PCC plan leads to fewer physician-induced demand behaviors that have already been listed in the regulation and fewer unnecessary expenses. According to the asymmetric information framework, we used the core concept of patient-centered care—involving patients to participate in treatment decisions—to explain the reason why PCC relates to fewer health insurance violations. Moreover, the protective effect of PCC is very sufficient.
In 2021, medical insurance violation funds reached 23.418 billion yuan (51). Incorporating PCC into medical education and practice can improve patient wellbeing and the sustainability of medical insurance. However, the requirement and education of PCC may lead to job burnout (52) for physicians. To solve this, in the short term, the savings of expenses from PCC can be used to expand welfare and job resources for physicians. This can be done through incentive plans that reward physicians for promoting communication and hard work (53). Moreover, in the long term, forming a patient-centered organizational culture (54) and providing psychological safety and perceived organizational support (55) can also be effective methods to promote PCC in practice.
Although the identification of the protective effect of PCC has used Chinese medical regulation, we can still predict that the contradiction of PCC in physician-induced demand and medical expense could be excavated further by eliminating the expense from technological innovation. Our result is consistent with the long-term research on the effect of the Affordable Care Act in the United States (56). Hence, we could predict that PCC would have a generalized effect on reducing physician-induced demand among different countries; however, short-term effects are easily concealed, and its long-term effects need to be identified.
Based on the above discussion, we believe that future research can further proceed from the following three aspects. First, the psychological mechanism for interpreting the reason why PCC would promote mental and physical health status and the patient's subjective necessity of hospitalization would excavate the causation of benefits from PCC. Second, exploring more efficient communication methods based on patient-centered care to promote the feasibility of outpatient is essential. Third, exploring the way to reduce the side-effects of PCC as a job demand from the organizational aspect would promote physicians' wellbeing and make PCC practical.
Although a large survey has been conducted, and we have indicated the association, the mechanism by which PCC reduces asymmetric information between patients and physicians is still worth further exploration.
Additionally, although this study has conducted a large survey of PCC, we cannot guarantee that endogeneity will be eliminated completely. These endogeneities may be caused by the selection of sampling cities and the degree of patient cooperation in the random sampling process. Additionally, whether there are differences between inpatients and outpatients will also affect the generalizability of the results of this study.
This study provides evidence that patient-centered care (PCC) is an effective and beneficial approach for inpatients in comprehensive hospitals. It shows that PCC can improve patients' physical and mental wellbeing, increase their subjective necessity of hospitalization, and reduce unnecessary or inappropriate medical interventions by physicians. The study also suggests that PCC can have different effects depending on the availability of healthcare resources in different regions. Therefore, PCC should be promoted and tailored to the local context and needs of the patients. These findings call for strengthening PCC research and evidence, underpinning practice, policy, and system transformation. Adopting PCC would provide not only better healthcare but also cost-effective healthcare, which would advance the development of the performance of the healthcare system facing the aging population and tight budget.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Shanghai Jiao Tong University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CY, YX, HL, GY, and ZZ: study design and implementation. CY and HL: methodology. TJ, XL, JL, and MB: data curation. CY and YX: analysis, validation, and writing—original draft preparation. CY, YX, JL, TJ, and MB: discussion. HL, GY, and ZZ: supervision. All authors contributed to the article and approved the submitted version.
The authors would like to thank all the study participants and investigators for data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1148277/full#supplementary-material
1. Lehman BJ, David DM, Gruber JA. Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Soc Pers Psychol Compass. (2017) 11:e12328. doi: 10.1111/spc3.12328
2. Santana MJ, Manalili K, Jolley RJ, Zelinsky S, Quan H, Lu M. How to practice person-centred care: a conceptual framework. Health Expect. (2018) 21:429–40. doi: 10.1111/hex.12640
3. Håkansson Eklund J, Holmström IK, Kumlin T, Kaminsky E, Skoglund K, Höglander J, et al. “Same same or different? “A review of reviews of person-centered and patient-centered care. Patient Educ Counsel. (2019) 102:3–11. doi: 10.1016/j.pec.2018.08.029
4. Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff. (2010) 29:1489–95. doi: 10.1377/hlthaff.2009.0888
5. Schwedt TJ, Hentz JG, Sahai-Srivastava S, Murinova N, Spare NM, Treppendahl C, et al. Patient-centered treatment of chronic migraine with medication overuse: a prospective, randomized, pragmatic clinical trial. Neurology. (2022) 98:e1409–21. doi: 10.1212/WNL.0000000000200117
6. Bayliss EA, Ellis JL, Shoup JA, Zeng C, McQuillan DB, Steiner JF. Association of patient-centered outcomes with patient-reported and ICD-9–based morbidity measures. Annal Family Med. (2012) 10:126–33. doi: 10.1370/afm.1364
7. Pinho LG de, Lopes MJ, Correia T, Sampaio F, Arco HR, Mendes A, et al. Patient-centered care for patients with depression or anxiety disorder: an integrative review. J Pers Med. (2021) 11:776. doi: 10.3390/jpm11080776
8. Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, et al. Home-based cardiac rehabilitation: a scientific statement from the American association of cardiovascular and pulmonary rehabilitation, the American heart association, and the American college of cardiology. Circulation. (2019) 140:663. doi: 10.1161/CIR.0000000000000663
9. Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W, et al. Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol. (2020) 75:1523–34. doi: 10.1016/j.jacc.2020.01.052
10. Kuipers SJ, Cramm JM, Nieboer AP. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv Res. (2019) 19:13. doi: 10.1186/s12913-018-3818-y
11. Iturralde E, Sterling SA, Uratsu CS, Mishra P, Ross TB, Grant RW. Changing results—engage and activate to enhance wellness: a randomized clinical trial to improve cardiovascular risk management. J Am Heart Assoc. (2019) 8:e014021. doi: 10.1161/JAHA.119.014021
12. Morton RL, Sellars M. From patient-centered to person-centered care for kidney diseases. Clin J Am Soc Nephrol. (2019) 14:623–5. doi: 10.2215/CJN.10380818
13. Seiglie J, Platt J, Cromer SJ, Bunda B, Foulkes AS, Bassett IV, et al. Diabetes as a risk factor for poor early outcomes in patients hospitalized with COVID-19. Diabetes Care. (2020) 43:2938–44. doi: 10.2337/dc20-1506
14. McTigue KM, Wellman R, Nauman E, Anau J, Coley RY, Odor A, et al. Comparing the 5-year diabetes outcomes of sleeve gastrectomy and gastric bypass: the national patient-centered clinical research network (PCORNet) bariatric study. JAMA Surg. (2020) 155:e200087. doi: 10.1001/jamasurg.2020.0087
15. Kornelius E, Chiou JY, Yang YS, Lu YL, Peng CH, Huang CN. The diabetes shared care program and risks of cardiovascular events in type 2 diabetes. Am J Med. (2015) 128:977–85. doi: 10.1016/j.amjmed.2015.03.025
16. Davis EL, Kelly PJ, Deane FP, Baker AL, Buckingham M, Degan T, et al. The relationship between patient-centered care and outcomes in specialist drug and alcohol treatment: a systematic literature review. Subst Abuse. (2020) 41:216–31. doi: 10.1080/08897077.2019.1671940
17. Bosserman LD, Cianfrocca M, Yuh B, Yeon C, Chen H, Sentovich S, et al. Integrating academic and community cancer care and research through multidisciplinary oncology pathways for value-based care: a review and the city of hope experience. J Clin Med. (2021) 10:188. doi: 10.3390/jcm10020188
18. Tunzi L, Funk T, Brown T, Findlay M, Bauer J. Optimal frequency of individualised nutrition counselling in patients with head and neck cancer receiving radiotherapy: a systematic review. J Hum Nutri Diet. (2022) 35:223–33. doi: 10.1111/jhn.12919
19. Findlay M, Bauer JD, Dhaliwal R, de van der Schueren M, Laviano A, Widaman A, et al. Translating evidence-based guidelines into practice—are we getting it right? A multi-centre prospective international audit of nutrition care in patients with foregut tumors (INFORM). Nutrients. (2020) 12:3808. doi: 10.3390/nu12123808
20. Findlay M, Rankin NM, Shaw T, White K, Boyer M, Milross C, et al. Best evidence to best practice: implementing an innovative model of nutrition care for patients with head and neck cancer improves outcomes. Nutrients. (2020) 12:1465. doi: 10.3390/nu12051465
21. Van Spall HGC, Lee SF, Xie F, Oz UE, Perez R, Mitoff PR, et al. Effect of patient-centered transitional care services on clinical outcomes in patients hospitalized for heart failure: the PACT-HF randomized clinical trial. JAMA. (2019) 321:753–61. doi: 10.1001/jama.2019.0710
22. Ma RCW, Xie F, Lim CKP, Lau ESH, Luk AOY, Ozaki R, et al. A randomized clinical trial of genetic testing and personalized risk counselling in patients with type 2 diabetes receiving integrated care -The genetic testing and patient empowerment (GEM) trial. Diabetes Res Clin Pract. (2022) 189:109969. doi: 10.1016/j.diabres.2022.109969
23. Liang H, Tao L, Ford EW, Beydoun MA, Eid SM. The patient-centered oncology care on healthcare utilization and cost: a systematic review and meta-analysis. Health Care Manage Rev. (2020) 45:364. doi: 10.1097/HMR.0000000000000226
24. Reychav I, Beeri R, Balapour A, Raban DR, Sabherwal R, Azuri J. How reliable are self-assessments using mobile technology in healthcare? The effects of technology identity and self-efficacy. Comput Hum Behav. (2019) 91:52–61. doi: 10.1016/j.chb.2018.09.024
25. D'Addario L, Kuo T, Robles B. Do knowledge about sodium, health status by self-report, and having hypertension predict sodium consumption behaviors among Southern California hospital employees? Transl Behav Med. (2021) 11:1254–63. doi: 10.1093/tbm/ibaa148
27. Kohler RE, Goyal RK, Lich KH, Domino ME, Wheeler SB. Association between medical home enrollment and health care utilization and costs among breast cancer patients in a state medicaid program. Cancer. (2015) 121:3975–81. doi: 10.1002/cncr.29596
28. David G, Saynisch PA, Smith-McLallen A. The economics of patient-centered care. J Health Econ. (2018) 59:60–77. doi: 10.1016/j.jhealeco.2018.02.012
29. Blomqvist Å. The doctor as double agent: Information asymmetry, health insurance, and medical care. J Health Econ. (1991) 10:411–32. doi: 10.1016/0167-6296(91)90023-G
30. Fei Y, Fu Y, Yang D, Hu C. Research on the formation mechanism of health insurance fraud in China: from the perspective of the tripartite evolutionary game. Front Public Health. (2022) 10:930120. doi: 10.3389/fpubh.2022.930120
31. Keating NL, Green DC, Kao AC, Gazmararian JA, Wu VY, Cleary PD. How are patients' specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians? J Gen Intern Med. (2002) 17:29–39. doi: 10.1046/j.1525-1497.2002.10209.x
32. Lusk JM, Fater K. A concept analysis of patient-centered care. Nursing Forum. (2013) 48:89–98. doi: 10.1111/nuf.12019
33. Slatore CG, Hansen L, Ganzini L, Press N, Osborne ML, Chesnutt MS, et al. Communication by nurses in the intensive care unit: qualitative analysis of domains of patient-centered care. Am J Crit Care. (2012) 21:410–8. doi: 10.4037/ajcc2012124
34. Fang H, Lei X, Shi J, Yi X. Physician-Induced Demand: Evidence from China's Drug Price Zero-Markup Policy. National Bureau of Economic Research (2021).
35. Fang J, Liu L, Fang P. What is the most important factor affecting patient satisfaction – a study based on gamma coefficient. Pat Pref Adh. (2019) 13:515–25. doi: 10.2147/PPA.S197015
36. Cameron AC, Gelbach JB, Miller DL. Robust inference with multiway clustering. J Bus Econ Stat. (2011) 29:238–49. doi: 10.1198/jbes.2010.07136
37. Cardel MI, Newsome FA, Pearl RL, Ross KM, Dillard JR, Miller DR, et al. Patient-centered care for obesity: how health care providers can treat obesity while actively addressing weight stigma and eating disorder risk. J Acad Nutr Diet. (2022) 122:1089–98. doi: 10.1016/j.jand.2022.01.004
38. Mason AN. The most important telemedicine patient satisfaction dimension: patient-centered care. Telemed e-Health. (2022) 28:1206–14. doi: 10.1089/tmj.2021.0322
39. Kosowicz L, Tran K, Khanh TT, Dang TH, Pham VA, Kim HTT, et al. Lessons for Vietnam on the use of digital technologies to support patient-centered care in low- and middle-income countries in the Asia-pacific region: scoping review. J Med Int Res. (2023) 25:e43224. doi: 10.2196/43224
40. Chen X, Giles J, Yao Y, Yip W, Meng Q, Berkman L, et al. The path to healthy ageing in China: a Peking university–lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
41. Doubova SV, Martinez-Vega IP, Infante-Castañeda C, Aranda-Flores CE, Knaul FM, Pérez-Cuevas R. Social inequalities in supportive care needs and quality of patient-centered care of cancer patients in Mexico. Supp Care Cancer. (2021) 29:1355–67. doi: 10.1007/s00520-020-05615-6
42. Mitchell JA, Williams EDG, Li Y, Tarraf W. Identifying disparities in patient-centered care experiences between non-Latino white and black men: results from the 2008-2016 medical expenditure panel survey. BMC Health Serv Res. (2020) 20:495. doi: 10.1186/s12913-020-05357-5
43. Wilkerson L, Fung CC, May W, Elliott D. Assessing patient-centered care: one approach to health disparities education. J Gen Intern Med. (2010) 25:86–90. doi: 10.1007/s11606-010-1273-5
44. O'Malley AJ, Zaslavsky AM, Elliott MN, Zaborski L, Cleary PD. Case-mix adjustment of the CAHPS® hospital survey. Health Serv Res. (2005) 40:2162–81. doi: 10.1111/j.1475-6773.2005.00470.x
45. Hu HH Qi Q, Yang CH. Analysis of hospital technical efficiency in China: Effect of health insurance reform. China Econ Rev. (2012) 23:865–77. doi: 10.1016/j.chieco.2012.04.008
46. Writing committee of the report on cardiovascular health and diseases in china. Report on cardiovascular health and diseases in China 2021: an updated summary. Biomed Environ Sci. (2022) 35:573–603. doi: 10.3967/bes2022.079
47. Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA. (2021) 326:2498–506. doi: 10.1001/jama.2021.22208
48. Tu WJ, Xue Y, Nie D. The prevalence and treatment of diabetes in China From 2013 to 2018. JAMA. (2022) 327:1706. doi: 10.1001/jama.2022.3014
49. Gusmano MK, Maschke KJ, Solomon MZ. Patient-centered care, yes; patients as consumers, no. Health Aff. (2019) 38:368–73. doi: 10.1377/hlthaff.2018.05019
50. Lee C. Optimal medical treatment under asymmetric information. J Health Econ. (1995) 14:419–41. doi: 10.1016/0167-6296(95)00012-7
51. National Healthcare Security Administration. Statistical Data of the National Medical Security Administration 2021 Statistical Bulletin on the Development of National Medical Security. Hong Kong: National Healthcare Security Administration (2021).
52. Rajamohan S, Porock D, Chang YP. Understanding the relationship between staff and job satisfaction, stress, turnover, and staff outcomes in the person-centered care nursing home arena. J Nurs Scholar. (2019) 51:560–8. doi: 10.1111/jnu.12488
53. Yu C, Li X, Liang H, Zhang Z, Fang D. The effects of monetary incentives on physicians' effort and patient satisfaction: understanding the links between monetary incentives and physicians' effort. Int J Environ Res Public Health. (2022) 19:13075. doi: 10.3390/ijerph192013075
54. Wick EC, Galante DJ, Hobson DB, Benson AR, Lee KK, Berenholtz SM, et al. Organizational culture changes result in improvement in patient-centered outcomes: implementation of an integrated recovery pathway for surgical patients. J Am Coll Surg. (2015) 221:669–77. doi: 10.1016/j.jamcollsurg.2015.05.008
55. Li J, Li S, Jing T, Bai M, Zhang Z, Liang H. Psychological safety and affective commitment among Chinese hospital staff: the mediating roles of job satisfaction and job burnout. Psychol Res Behav Manag. (2022) 15:1573–85. doi: 10.2147/PRBM.S365311
Keywords: patient-centered care, physician-induced demand, charge and fees, healthcare expense, healthcare insurance sustainability
Citation: Yu C, Xian Y, Jing T, Bai M, Li X, Li J, Liang H, Yu G and Zhang Z (2023) More patient-centered care, better healthcare: the association between patient-centered care and healthcare outcomes in inpatients. Front. Public Health 11:1148277. doi: 10.3389/fpubh.2023.1148277
Received: 19 January 2023; Accepted: 19 September 2023;
Published: 19 October 2023.
Edited by:
Rosaria Indah, Syiah Kuala University, IndonesiaReviewed by:
Monika Elisabeth Finger, Swiss Paraplegic Research, SwitzerlandCopyright © 2023 Yu, Xian, Jing, Bai, Li, Li, Liang, Yu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huigang Liang, aGxpYW5nMUBtZW1waGlzLmVkdQ==; Guangjun Yu, Z3VhbmdqdW55dUBjdWhrLmVkdS5jbg==; Zhiruo Zhang, emhhbmd6aGlydW9Ac2p0dS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.