
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 25 April 2023
Sec. Planetary Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1143751
This article is part of the Research TopicClimate and Health Education: Defining the Needs of Society in a Changing ClimateView all 14 articles
Aim: The climate and ecological crises are considered fundamental threats to human health. Healthcare workers in general and doctors in particular can contribute as change agents in mitigation and adaptation. Planetary health education (PHE) aims to harness this potential. This study explores perspectives among stakeholders involved in PHE at German medical schools on the characteristics of high-quality PHE and compares them to existing PHE frameworks.
Methods: In 2021, we conducted a qualitative interview study with stakeholders from German medical schools involved in PHE. Three different groups were eligible: faculty members, medical students actively involved in PHE, and study deans of medical schools. Recruitment was performed through national PHE networks and snowball sampling. Thematic qualitative text analysis according to Kuckartz was used for the analysis. Results were systematically compared to three existing PHE frameworks.
Results: A total of 20 participants (13 female) from 15 different medical schools were interviewed. Participants covered a wide range of professional backgrounds and experience in PHE education. The analysis revealed ten key themes: (1) Complexity and systems thinking, (2) inter- and transdisciplinarity, (3) ethical dimension, (4) responsibility of health professionals, (5) transformative competencies including practical skills, (6) space for reflection and resilience building, (7) special role of students, (8) need for curricular integration, (9) innovative and proven didactic methods, and (10) education as a driver of innovation. Six of our themes showed substantial overlap with existing PHE frameworks. Two of our themes were only mentioned in one of the frameworks, and two others were not explicitly mentioned. Few important elements of the frameworks did not emerge from our data.
Conclusions: In the light of increased attention regarding the connections of the climate and ecological crises and health, our results can be useful for anyone working toward the integration of planetary health into medical schools' and any health professions' curricula and should be considered when designing and implementing new educational activities.
The climate crisis has been called the most significant threat to human health in the twenty-first century (1). It is one important element of a planetary health (PH) perspective, others include biodiversity loss, global social injustice, limits to growth (2) and the risk of civilization collapse via nuclear conflict. Effects of the climate and other environmental crises on human health worldwide can already be observed (3). These health impacts vary by region. Prevalent risks in Western Europe, including Germany, include extreme weather events, such as heat waves and flooding. Moreover, a rise in disease burden through allergies and changes in occurrence of certain infectious diseases linked to the climate crisis are observed (4–6), as are negative mental health effects, especially for young people (7, 8). The interdependence of human health and wellbeing and planetary ecosystems is at the core of the emerging concept of PH, which has been defined as “the health of human civilization and the state of the natural systems on which it depends” (9). Achieving PH requires a profound transformation of all areas of human activities, for example the energy, mobility and agri-food systems. At the same time, adaptation to the already occurring (health) impacts of the changes in planetary ecosystems is required. Education can play an important role in this regard when it “includes knowledge transfer to raise awareness of certain realities, critical analysis to understand the complexities underlying these realities, and experiential exposure to connect to these realities” (10, 11).
The health (care) sector plays a specific and important role in the mitigation of and adaptation to the unfolding planetary crises: On the one hand, it contributes to the climate and ecological crises by generating 4.4% of the global greenhouse emissions and a high resource use (12). On the other hand, it has to respond to changing disease burdens caused by these crises (3). This implies that the education of health professionals needs to be adapted so that they become equipped with the knowledge and skills they need to address these health impacts. Additionally, it has been suggested that health professionals can play an important role as change agents in driving the transformative societal changes needed to mitigate the climate and ecological crises (13, 14). Health professionals belong to the most trusted of all professional groups in society (15) and the medical professional ethos demands care for individual and population health, including that of future generations (16). In Germany, the duty to maintain natural living conditions is explicitly mentioned in the medical professional code (17).
Planetary health education (PHE) aims to “equip people with the necessary knowledge, skills and values, as well as a sense of self-confidence and self-efficacy in the face of multiple environmental and social crises, in order to collectively achieve the necessary transformation of societal activities for planetary health” [own translation (18)]. Within medical education, it cannot be expected for all students to become experts for PH topics, but it is crucial to get a general understanding of the most important aspects as well as (further) develop values aligned with planetary health in their professional identity formation.
Several conceptual frameworks, detailed road maps, and principles for PHE have recently been developed. The Association of Medical Education in Europe (AMEE) has laid out in its “Consensus Statement: Planetary health and education for sustainable healthcare” (19) examples of learning activities, opportunities, and possible assessment modes as well as a road map and targets for implementing PHE. Further conceptual frameworks that define the scope and aims of PHE are the 12 “Cross-cutting principles for planetary health education” (20) and “A framework to guide planetary health education” (21).
Although the integration of PHE into the medical curriculum has been demanded repeatedly, including by medical students in Germany and globally, the integration of PHE into medical education and the monitoring of these processes remains insufficient (22–27). Like in other countries, such as the UK (28), previous studies show that that the majority of German students is not yet familiar with the PH concept, but would like to learn more about PH and consider it relevant to their studies (29). While a growing number of curricular and extracurricular educational activities is being implemented at several institutions, including nationwide lecture series (11), the experience of stakeholders involved or interested in PHE at German medical schools has, to our knowledge, not yet been explored. The opinion of the stakeholders of what characterizes high-quality PHE could inform the process of integrating PHE into medical education in Germany.
The aim of our study therefore is to explore the insights into the characteristics of high-quality PHE of a broad range of stakeholders - educators, students as educators and study deans - who are involved in PHE at German medical faculties. We also assess whether our findings are related to existing PHE frameworks.
This qualitative interview study is a component (substudy C, see Supplementary material S1) of the mixed methods study: Planetary Health in Medical Education in Germany (PlanetMedEd). The aim of the PlanetMedEd study is to comprehensively investigate and explore the current state and diverse perspectives of the potential ways forward for PHE at German medical schools. Further components include a nationwide student survey and a systematic overview of PHE initiatives including a systematic web search. Results of these components will be published elsewhere.
Three groups were eligible for participation in this study: Educators, students as educators (18 years and older), and study deans who were involved in PHE or were interested in establishing PHE at their institution. Participants were recruited via the contact list of the PHE working group (30) of the German Alliance on Climate Change and Health (KLUG e.V.) and through snowball sampling. Some individuals were recruited in alumni and student groups within the Master in Medical Education (MME-D) programme at Heidelberg University. In addition, results of the web search conducted as part of the PlanetMedEd study (Substudy A) were also used to identify eligible individuals.
We conducted interviews between June and September 2021 via the Zoom® video-conferencing software or via telephone based on a semi-structured interview guide (see Supplementary material S2). Additionally, sociodemographic data (gender identification, age in categories, academic background, and profession) as well as further professional qualifications and activities or expertise considered relevant for PHE by the interviewees were collected to allow contextualization of the qualitative findings. The transcripts were completely anonymized and contained no personal or third-person information that would allow tracing any identities. Data on sociodemographic characteristics were only collected for contextualization and are presented in aggregated categories.
Data were collected jointly by JS (doctoral thesis student) and E-MS-S (MD, MScIH, experienced in PHE and implementation research). JS conducted 4 interviews alone. Both researchers were present in 13 interviews and took turns in conducting the interviews and note-taking. The interviews were audio-recorded and transcribed verbatim. The same two authors (E-MS-S, JS) were involved in the coding process. Thematic qualitative text analysis with a content-structuring approach according to Kuckartz was performed in MAX-QDA 2020 (31). For the current study, we deductively grouped data into main categories adapted from the main interview questions (see Figure 1), then we inductively developed sub-categories within the first main category on PHE characteristics.
Figure 1. Overview of the main questions based on the semi-structured interview guide of the PlanetMedEd qualitative substudy C.
The process of inductively developing sub-categories included the following steps: After familiarizing ourselves with the data, we first created sub-categories independently for three randomly selected interviews. We then compared and discussed these sub-categories. As an intermediate analysis step, case summaries were created for each interview to create a better overview of the data. A detailed system of sub-categories was then created based on all interviews and was discussed several times in the research team for completeness and consistency before it was applied to the entire text material. We performed several iterations to adjust the sub-category system.
In a second analysis step, we compared the categories developed in this way with three existing frameworks for PHE: With the “Cross-cutting principles for PHE” by Stone et al. (20), with “A Framework to guide PHE” by Guzmán et al. (21), and with the “AMEE consensus statement: Planetary health and education for sustainable healthcare” by Shaw et al. (19). For this purpose, E-MS-S, JS, and KW (MD, experienced in PHE and qualitative research) independently assessed whether our categories corresponded to elements in the central figures of each framework. Any discrepancies were resolved through discussion. In this step, we did not aim to compare the three frameworks with each other or to explore in depth how our sub-categories corresponded to the content of the entire text body supporting each framework. We rather aimed to broadly compare them in order to assess whether our data could provide new aspects that were not yet covered in the existing frameworks, or if central themes were covered in the frameworks that were not mentioned by our study participants. As guidance for a comprehensible presentation of the study conduct, the checklist presented in the Consolidated criteria for reporting qualitative research (COREQ) guideline (32) was used (see Supplementary material S3).
The audio files were transcribed anonymously directly from the recorder and then deleted. Data storage and analysis took place on password-protected computers, in anonymized form and in accordance with the privacy policy.
The ethics committee of the University Hospital of Würzburg approved the conduct of the study (file number 20210312-01). All participants were provided with study information sheets and provided written informed consent.
A total of 30 potential participants were identified and contacted, of which 20 individuals agreed to participate and were interviewed in 17 interviews (3 interviews were conducted jointly with 2 participants from one university). The interviews lasted between 13 and 43 min, with an average duration of 31 min.
Participants reported a broad range of professional and academic backgrounds. Eleven participants were faculty members, seven were students actively involved in PHE, and two were study deans. Activity in several networks such as the German Alliance on Climate Change and Health or Health for Future and other experiences were reported as relevant to their PHE expertise or interest (Table 1).
Ten main themes emerged (Table 2). The categories and examples of verbatim translations are listed in Table 3. The complete coding framework can be found at Supplementary material S4, verbatim supplement (VS) VS1-142 in Supplementary material S5, S6.
Many participants stressed the importance of a solid foundation of factual knowledge that takes the complexity of the topic into account and at the same time introduces a perspective of systems thinking. The participants perceived fundamental challenges in developing a curriculum that covers the broad range of topics on PH and also discusses them in depth (VS1-3).
“Factual knowledge” (VS7) on climate and environmental changes, knowledge on environmental factors as health determinants, such as urban planning and the psychosocial environment and a historical context of the development of human societies to date were considered important (VS4). Students should be enabled to understand and classify the multiple complex interrelationships of the system and the interaction of these interrelationships with human health (VS17-19) as well as to consider patients in their entire environment (VS19). This eclipses the classical medical curriculum by far (VS15).
An integral part of PHE is to bring different disciplines together and to teach and learn together (VS21, VS24-26). This concerns different professional groups and disciplines in the health sector (VS27), but also “the inclusion of other groups and members of society that have not been classically considered by us so far” (VS29). For example, interdisciplinary lectures might include lectures by geographers and space researchers (VS30).
An ethical discussion of issues such as gender-based discrimination, racism, sexism, capitalism (VS35), and modern medical treatments and their impact on the environment (VS34) should be included. “Social justice” in terms of a “global justice perspective” (VS40, VS39) and the different regional impacts of environmental change also need to be discussed (VS38, VS41). Students should consider and reflect the principles they see as the basis of society (VS36). “Think globally and act locally” (VS46) represents an important principle here.
Other areas mentioned were individual consumption habits, including those of the students themselves, for example with regard to air travel and meat consumption, including weighing the impacts and learning how to make difficult consumption choices (VS43, VS44).
A reflection of one's own position in society as well as options for action or even agency, including the role of a change agent as a healthcare professional, should be part of PHE (VS48-50, VS53). Health professionals should develop a “sense of duty and responsibility” (VS55), and be aware of their social role-model function (VS54). This does not only mean the education of patients about PH issues, but also considers the sustainability aspects of one's own medical practice, financial investments, and mobility (VS51). This requires addressing questions of the (professional) attitude of “medical students as critical citizens” (VS59, VS60).
By acquiring knowledge about possible actions and reflecting about their own options for action, students themselves can become change agents and can gain confidence in their own agency (VS61-63, VS65-67), motivating the implementation of own ideas (VS68). Excursions with practical experience can be helpful in this regard, for instance a visit of a sustainable farm (VS64).
Science competencies, including searching, finding, correctly classifying, and evaluating sources of scientific evidence is relevant in order to be able to communicate knowledge properly and also to apply it to one's own actions (VS69-71). Thereby, it can also be part of PHE to acquire and practice communicative skills (VS72) by talking to other groups of society, for example in schools and nursing homes to support transformation within communities (VS73).
Learners need enough space for guided and unguided reflection inside and outside the classroom, to reflect and discuss freely and to share frustrating experiences (VS74-76). This is important to question one's own behavior and values, to promote “systemic thinking, critical thinking” to “broaden the horizon” (VS80), and to reflect on the learning journey (VS78, VS79, VS81, VS82). International and intercultural “long-term social relationships” (VS83) can also create changes in perspective and motivation. PHE also needs to incorporate resilience building for learners as they are confronted with dire future scenarios (VS75).
In the best case, PHE ties in with the real life of students (VS85) and takes up topics that students themselves suggest or are currently concerned with (VS84, VS86). It is also necessary to “take the students seriously, with their questions and concerns, ideas, and suggestions” (VS76). In the development of educational activities, students play an important role because they add a different perspective and have often already dealt with many topics more intensively than (older) lecturers themselves. Students and lecturers can learn from each other (VS88-90). Students can also act as promoters for the implementation of PHE at their universities (VS91).
Extracurricular implementation of PHE is currently clearly predominant (VS93). Many interviewees called for the integration of PHE as a transversal theme into the entire curriculum (VS95, VS101, VS103). Lecturers of different subjects should repeatedly refer to PH within the core medical curriculum by enriching classical medical knowledge with related PH topics (VS96, VS107). PH aspects should not be presented in a disjointed manner, but “build on each other” in a coherent framework throughout the course of medical studies (VS106). In this context, PHE should not be just “an add-on” in the curriculum, but “touches the core of medical studies',” and it corresponds to a “great interest and a great need of the students” (VS99).
Most participants in extracurricular and elective classes or courses are often already sensitized to the topic. Curricular teaching, however, reaches all students, even those who have not yet dealt with topics of PH (VS107).
Interview participants suggested a wide range of didactic methods in PHE, both innovative and proven. Many suggested combining classroom teaching and blended-learning concepts (VS113, VS114). More discussion and interaction and less “multiple choice” knowledge is required (VS72, VS115, VS117, VS118). Teaching should be interdisciplinary to address the diversity of PH (VS21). Lecture formats would be most appropriate for basic knowledge and best embedded in a broader curriculum with additional seminars in small groups (VS126). Training of communicative competencies, with simulation patients (VS124), problem-oriented learning cases (VS120, VS125, VS128), constructive solution finding with experts (VS129), and excursions with practical relevance (VS64, VS130, VS131), were also mentioned. Examination formats in PHE could include essays on a self-selected topic (VS133, VS136), interviews in group work with various stakeholders (VS123), and a subsequent report that analyzes and reflects on a patient's care environment in group work (VS135). The assessment methods and their evaluation require more time and effort, but promote gaining “a deeper understanding” (VS136, VS135).
The overarching concept of PH and its mediation through PHE holds the possibility of driving innovative teaching and research in the field so that each faculty member engages with the connection between his or her own discipline and PH. Educators can develop an awareness of the concept of PH and its complex interrelationships beyond their discipline (VS17, VS142). The goal is “a complete mindset change of the teaching staff” so that PHE is addressed by them in various educational courses (VS137). In this way, the topic could be highlighted also among students, colleagues, and people beyond the medical professions (VS87, VS138-140).
When comparing each of the three frameworks for PHE [(19–21), see Table 4] with our ten themes, we found that six of our themes (1.-5.,10.) overlap with two or all three frameworks. We found that two themes (6. and 9.) overlap only with the AMEE Consensus Statement. For two (7. and 8.) of our themes, we did not find a clearly mentioned equivalent in any of the three frameworks. Additionally, we found aspects in the three frameworks, such as “harmony or interconnection with nature” and “indigenous place-based perspectives,” that did not emerge in the interviews.
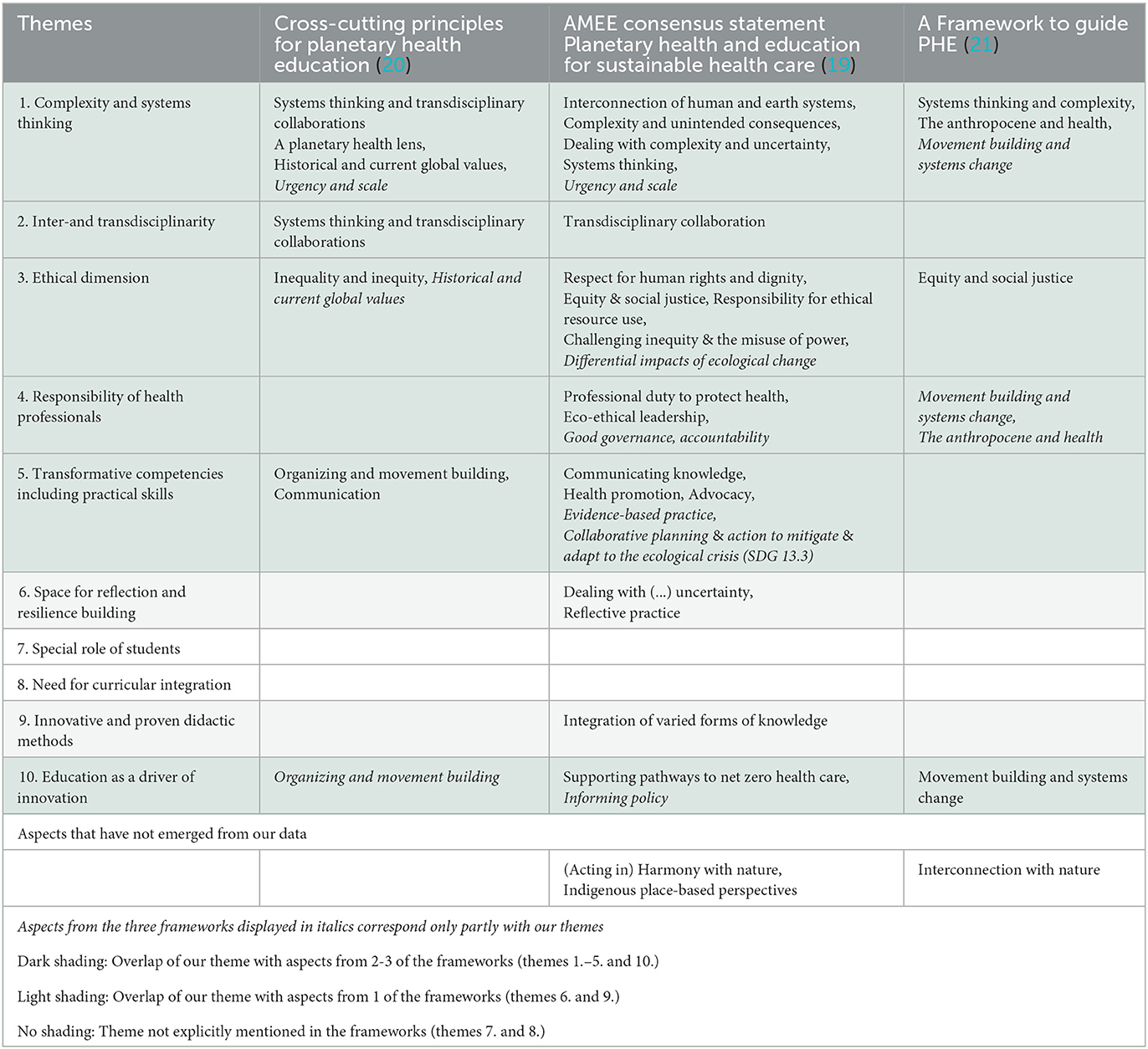
Table 4. Comparison of our ten themes with three international frameworks for planetary health education.
To the very best of our knowledge, this study conducted with a large variety of stakeholders at 15 medical schools across Germany is the first study in the German-speaking context that explores high-quality characteristics of PHE through qualitative interviews. Participants reported diverse professional and personal backgrounds, in line with the transdisciplinarity often highlighted in the context of PH (33). Of the ten characteristics we identified, six overlap with two to three existing international frameworks for PHE.
Complexity and systems thinking refers to the climate and other environmental crises as examples of so-called (super-)wicked problems that pose particular difficulties to public policy, mainly owing to being the emergent outcome of multiple interactions between natural and social systems in what are called complex systems (34, 35). Methods for training students in systems thinking include complex systems mapping (36, 37). Important paradigms that should form part of systems thinking in the context of PHE include the social (and other) determinants of health (38). An approach to understand the complex interrelationships between human health, social and economic factors and the environment can be the doughnut model (39). In medical education it can also be beneficial to explore analogies between the human body as a system of complex systems and the natural complex systems to appreciate the importance of systems thinking for tackling problems and finding solutions.
Inter- and transdisciplinary approaches are highlighted as essential but often lack conceptual clarity at least in relation to the public health workforce (40). Achieving profound changes for PH, such as decarbonizing health care systems, requires collaboration of different professional groups and stakeholders (33).
The ethical dimension includes aspects of equity and social justice in a global perspective (41–43) and questions of climate justice (44). Equally important are questions of ethical resource use in the health sector, with many open questions of implementation that need to be addressed in practice and teaching. Learners can take on an important role of pushing for reflection of current practice in resource waste in their clinical placements.
Regarding the responsibility of health professionals, part of the PHE learning objectives should be the sensitization of medical students to the double-edged role that health (care) systems play for PH including the training of skills for sustainable healthcare (45).
Transformative competencies that would enable learners to effectuate change, were confirmed as a key tenet of high-quality PHE, and also form the basis of high-quality health professional education (46). These can include conventional skills such as communication skills, which can unfold transformative potential if integrated with factual knowledge relevant to PH, for instance regarding the co-benefits of active mobility (meaning health benefits through physical activity as well as less emissions of CO2 and air pollutants), a doctor might effectively integrate into a medical consultation. To adopt the role of change agents, learners also need to develop a set of values and attitudes that is in line with the goals of PH. As changes in values are usually not achieved through classic lecture formats but rather through experiential learning and constructive dialogue (47), PHE needs to encompass formats and nudges to trigger this kind of transformative learning in students (48, 49). Developing confidence as well as a sense of self-efficacy are further important competencies that enable students to be agents of change. Faculty can contribute to this by increasing the students' understanding of transformation and their sense that transformative change is possible; enhancing the students' sense of their own agency and ability to make a difference; helping students see and apply PH concepts during rounds or debriefing of clinical encounters; and give support to articulate a role for themselves in processes of transformative change, also by overcoming a perceived gap between the impacts of individual and collective change (50–53). Recognizing and reflecting on the importance of even small contributions to social change in accordance with e.g., the concept of social tipping dynamics (54) can be beneficial to increase learners' self-efficacy and their self-identification as change agents. However, learners should be supported in setting realistic expectations regarding their impact to prevent them from feeling frustrated, discouraged or paralyzed which could result in impaired mental wellbeing.
Our theme space for reflection and resilience building was—among the three frameworks—only reflected in the AMEE consensus statement (19) as learning to face existing and upcoming uncertainties and to implement “reflective practice” as a teaching method. Our category extends this notion by explicitly mentioning the importance for students to be given space to share their emotions and worries in relation to the climate and environmental crises that they might become fully aware of through participating in PHE. Educators have a special responsibility here to consider students' psychological wellbeing when they are confronted both with the scientific evidence on the climate and ecological crises and their health impacts as well as with the implications these might have for their work as medical doctors, but also for their future life (55). Learning critical reflexivity, for example regarding one's personal standpoint, practice, research, and action, including the negative impact of affluent lifestyles (56) can help students to develop and strengthen personal and professional attitudes, and it can strengthen their emotional resilience (57).
The special role of students is not explicitly emphasized in any of the three frameworks. According to our results, high-quality PHE should be student-centered as they are often the first to advocate for changes in their education based on their already existing civic engagement with the climate and other environmental crises (58). Student-led seminar formats can allow students to deepen their knowledge on a specific topic and strengthen their communication skills, thus swapping the traditional roles of student and teacher. A range of student-driven PHE formats have already been successfully realized and can be used as blueprints for further PHE initiatives (59, 60). Students can also play a central role in implementing PHE in the curricula (61).
Conceptualizing PHE as a longitudinal part of the core curriculum is not specifically mentioned in the central graphs of the three frameworks. More recent literature exists on roadmaps for curricular integration, having the potential to reach those who have not previously dealt with planetary health (62). Examples for curricular integration range from simply changing application examples in standard medical lessons (e.g., explicitly describing the effects of heat waves on elderly people or infants) to full lectures on the health impacts of the climate and ecological crises and dedicated teaching for development of practical skills for transformative action on the individual, organizational, and professional-political level (63, 64).
The central feature of the PHE framework by Guzmán et al. is “interconnection with nature”. Shaw et al. also refer to interconnectedness with nature as an important element of PHE. Surprisingly, this was not explicitly mentioned by our interview participants when they were asked about quality characteristics of PHE. In our opinion, an understanding of human beings as embedded within natural systems and the unconditional dependency of health and wellbeing on intact and thriving natural systems is essential for promoting and achieving PH.
Shaw et al. also highlight the importance of Indigenous knowledge systems which they claim should be recognized and discussed as part of PHE. This aspect did not emerge from our data either. Here a reason might be that compared to other regions of the world (i.e., America, Australia, Asia, and Africa), Germany has no indigenous populations (in the classical sense of living descendants of pre-invasion inhabitants in a given area that is now dominated by other inhabitants) that would lead a lifestyle close to nature. It is important, however, to also convey this perspective to students in Germany as indigenous populations play an important role in guarding a large proportion of the planet's biodiversity (65, 66) and can bear examples of sustainable lifestyles (67). We believe that the potential of Indigenous knowledge systems for addressing the ecological crises as well as sensitization of learners to the shared drivers of these crises and the marginalization of Indigenous communities and others groups - which can be subsumed under the labels of settler-colonialism, Eurocentrism and extractive economic practices - should be part of PHE. Therefore, more work is needed to sensitize educators in Germany to these issues and to practice dialogue between scholars who were scientifically socialized within different ontological and epistemological cultures.
At the time of publication, the data were almost 1.5 years old. Because PHE is a very dynamic area, some progress may have been made in the development of PHE since we collected the data that is not yet reflected in our paper. We used PHE networks for sampling, followed by snowball sampling, therefore we cannot rule out a selection bias. Moreover, most of the interviewers all had a strong interest in promoting PHE, thereby potentially leading to social desirability bias. We interviewed students as experts who are actively promoting PHE within their medical schools, through which the role of students may be slightly overestimated. On the other hand the inclusion of diverse stakeholders, from 15 universities from all over Germany and specifically the inclusion of students with an active role in PHE—whose contribution is essential—allowed us to gain a holistic understanding of current priorities in this dynamic field.
The ten characteristics of PHE we developed from interviews with a diverse group of stakeholders at medical schools throughout Germany can be helpful to all who are currently in the process of implementing and enhancing PHE nationally and internationally. While most of our findings were in line with existing frameworks, we also identified new themes. Focus should be laid on the special role of students, space for reflection and resilience building and transformative competencies. Further studies should focus on other health professions to meet the aspiration of inter- and transdisciplinarity in the design and underlying principles of PHE.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of the University Hospital of Würzburg file number 20210312-01. The patients/participants provided their written informed consent to participate in this study.
E-MS-S conceptualized the study. E-MS-S and JS planned the study and performed the data collection and the thematic qualitative text analysis. E-MS-S, JS, and KW performed the comparison of the themes to existing frameworks. AS supervised the whole project (doctoral thesis of JS). All authors contributed to the manuscript development and approved the final version to be published.
This publication was supported by the Open Access Publication Fund of the University of Wüerzburg.
We thank all interview participants for their participation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1143751/full#supplementary-material
1. Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: lancet and university college London institute for global health commission. Lancet. (2009) 373:1693–733. doi: 10.1016/S0140-6736(09)60935-1
2. Dixson-Declève S, Gaffney O, Gosh J, Randers J, Rockström J, Stoknes PE. Earth for All - A Survival Guide for Humanity. Gabriola Island, BC: New Society Publishers (2022).
3. Romanello M, Napoli CD, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the lancet countdown on health and climate change: health at the mercy of fossil fuels. Lancet. (2022) 400:1619–54. doi: 10.1016/S0140-6736(22)01540-9
4. Mora C, McKenzie T, Gaw IM, Dean JM, von Hammerstein H, Knudson TA, et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat Clim Change. (2022) 12:869–75. doi: 10.1038/s41558-022-01426-1
5. Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet. (2021) 397:129–70. doi: 10.1016/S0140-6736(20)32290-X
6. Nowak D. Global Warming-the German picture. Dtsch Arzteblatt Int. (2019) 116:519–20. doi: 10.3238/arztebl.2019.0519
7. Deutsches Ärzteblatt DÄG. Klimawandel und psychische Gesundheit: Ein relativ neuer Stressfaktor [Climate change and mental health: a relatively new stressor]. Dtsch Arzteblatt. (2020). Available online at: https://www.aerzteblatt.de/archiv/213960/Klimawandel-und-psychische-Gesundheit-Ein-relativ-neuer-Stressfaktor (accessed January 12, 2023).
8. Peter F, Dohm L, Krimmer M. Psychische Konsequenzen der Klimakrise [Psychological consequences of the climate crisis]. Monatsschr Kinderheilkd. (2022) 3:1670. doi: 10.1007/s00112-022-01670-x
9. Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the anthropocene epoch: report of the rockefeller foundation–lancet commission on planetary health. Lancet. (2015) 386:1973–2028. doi: 10.1016/S0140-6736(15)60901-1
10. UNESCO. Framework for the implementation of Education for Sustainable Development. (ESD) beyond 2019 - UNESCO Digital Library. (2019). Available online at: https://unesdoc.unesco.org/ark:/48223/pf0000370215 (accessed January 12, 2023).
11. Gepp S, Jung L, Wabnitz K, Schneider F, Gierke F, Otto H, et al. The Planetary Health Academy—a virtual lecture series for transformative education in Germany. Lancet Planet Health. (2023) 7:e68–76. doi: 10.1016/S2542-5196(22)00253-4
12. Health Care Without Harm. Health Care's Climate Footprint. (2019). Available online at: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed February 23, 2022).
13. Maibach E, Frumkin H, Ahdoot S. Health professionals and the climate crisis: trusted voices, essential roles. World Med Health Policy. (2021) 13:137–45. doi: 10.1002/wmh3.421
14. Kotcher J, Maibach E, Miller J, Campbell E, Alqodmani L, Maiero M, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health. (2021) 5:e316–23. doi: 10.1016/S2542-5196(21)00053-X
15. Ipsos MORI. Ipsos MORI Veracity Index - Trust in Professions - 2021. (2021). Available online at: https://www.ipsos.com/sites/default/files/ct/news/documents/2021-12/trust-in-professions-veracity-index-2021-ipsos-mori_0.pdf (accessed December 12, 2022).
16. Parsa-Parsi RW. The international code of medical ethics of the world medical association. JAMA. (2022) 328:2018–21. doi: 10.1001/jama.2022.19697
17. Bundesärztekammer.. (Muster-)Berufsordnung für die in Deutschland tätigen Ärztinnen und Ärzte [(Model) professional code of conduct for physicians practicing in Germany].. (2021). Available online at: https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/pdf-Ordner/Recht/_Bek_BAEK_MBO-AE_Online_final.pdf (accessed March 3, 2023).
18. Wabnitz, K, Schwienhorst-Stich E., Schmid J. “Planetare Gesundheit - Lehr- und Lernformate für Medizinstudierende [Planetary Health - Teaching and Learning Formats for Medical Students].,” Gesundheit und Nachhaltigkeit. Springer Reference Pflege – Therapie – Gesundheit. Springer (2023).
19. Shaw E, Walpole S, McLean M, Alvarez-Nieto C, Barna S, Bazin K, et al. AMEE consensus statement: planetary health and education for sustainable healthcare. Med Teach. (2021) 43:272–86. doi: 10.1080/0142159X.2020.1860207
20. Stone SB, Myers SS, Golden CD. Cross-cutting principles for planetary health education. Lancet Planet Health. (2018) 2:e192–3. doi: 10.1016/S2542-5196(18)30022-6
21. Guzmán CAF, Aguirre AA, Astle B, Barros E, Bayles B, Chimbari M, et al. A framework to guide planetary health education. Lancet Planet Health. (2021) 5:e253–5. doi: 10.1016/S2542-5196(21)00110-8
22. McLean M, Madden DL, Maxwell J, Nanya Schwerdtle P, Richardson J, Singleton J, et al. “Planetary Health: Educating the current and future health workforce.” In: Nestel D, Reedy G, McKenna L, Gough S, editors. Clinical Education for the Health Professions. Singapore: Springer. (2020).
23. Planetary Health Report Card. 2021-2022 Summary Report Germany. PHRC. (2022). Available online at: https://phreportcard.org/germany/ (accessed January 12, 2023).
24. Medical Students for a Sustainable Future. Curriculum Guide_2022. (2022). Available online at: https://drive.google.com/file/d/1fw3ohKavICVecwi-CpEbm0o9ZaPmJIK6/view (accessed November 15, 2022).
25. Omrani OE, Dafallah A, Paniello Castillo B, Amaro, Bianca Quintella Ribeiro Corrêa, Taneja S, et al. Envisioning planetary health in every medical curriculum: An international medical student organization's perspective. Med Teach. (2020) 42:1107–11. doi: 10.1080/0142159X.2020.1796949
26. Shea B, Knowlton K, Shaman J. Assessment of climate-health curricula at international health professions schools. JAMA Netw Open. (2020) 3:e206609. doi: 10.1001/jamanetworkopen.2020.6609
27. Wabnitz K, Galle S, Hegge L, Masztalerz O, Schwienhorst-Stich E, Eichinger M. Planetare Gesundheit – transformative Lehr- und Lernformate zur Klima- und Nachhaltigkeitskrise für Gesundheitsberufe [Planetary health-transformative education regarding the climate and sustainability crises for health professionals]. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz. (2021) 64:378–83. doi: 10.1007/s00103-021-03289-x
28. Gupta D, Shantharam L, MacDonald BK. Sustainable healthcare in medical education: survey of the student perspectives at a UK medical school. BMC Med Educ. (2022) 22:689. doi: 10.1186/s12909-022-03737-5
29. Klünder V, Schwenke P, Hertig E, Jochem C, Kaspar-Ott I, Schwienhorst-Stich E-M, et al. A cross-sectional study on the knowledge of and interest in Planetary Health in health-related study programmes in Germany. Front Public Health. (2022) 10:7854. doi: 10.3389/fpubh.2022.937854
30. Anmeldung zur Mailingliste der AG Lehre | KLUG [Registration for the mailing list of the working group planetary health education | KLUG]. Available online at: https://www.klimawandel-gesundheit.de/ag-lehre-mailingliste/ (accessed December 20, 2022).
31. Kuckartz U, Rädiker S. Fokussierte Interviewanalyse mit MAXQDA: Schritt für Schritt [Focused interview analysis with MAXQDA: step by step]. Wiesbaden: Springer Fachmedien Wiesbaden (2020). doi: 10.1007/978-3-658-31468-2
32. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
33. Nayna Schwerdtle P, Horton G, Kent F, Walker L, McLean M. Education for sustainable healthcare: a transdisciplinary approach to transversal environmental threats. Med Teach. (2020) 42:1102–6. doi: 10.1080/0142159X.2020.1795101
34. Levin K, Cashore B, Bernstein S, Auld G. Overcoming the tragedy of super wicked problems: constraining our future selves to ameliorate global climate change. Policy Sci. (2012) 45:123–52. doi: 10.1007/s11077-012-9151-0
35. Levin K, Cashore B, Bernstein S, Auld G. Playing it forward: Path dependency, progressive incrementalism, and the “Super Wicked” problem of global climate change. IOP Conf Ser Earth Environ Sci. (2009) 6:502002. doi: 10.1088/1755-1307/6/50/502002
36. Tripto J. Mapping what they know: concept maps as an effective tool for assessing students' systems thinking. Am J Oper Res. (2013) 03:245–58. doi: 10.4236/ajor.2013.31A022
37. Pomeroy–Stevens A, Goldman B, Grattan K. Participatory systems mapping for municipal prioritization and planning. J Urban Health. (2022) 99:738–48. doi: 10.1007/s11524-022-00654-2
38. Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep Wash DC 1974. (2014) 129(Suppl 2):19–31. doi: 10.1177/00333549141291S206
39. Raworth K, A. Doughnut for the Anthropocene: humanity's compass in the 21st century. Lancet Planet Health. (2017) 1:e48–9. doi: 10.1016/S2542-5196(17)30028-1
40. Sell K, Hommes F, Fischer F, Arnold L. Multi-, inter-, and transdisciplinarity within the public health workforce: a scoping review to assess definitions and applications of concepts. Int J Environ Res Public Health. (2022) 19:10902. doi: 10.3390/ijerph191710902
41. Islam SN, Winkel J. Climate Change and Social Inequality. U N - Dep Econ Soc Aff DESA Work Pap No 152. (2017). Available online at: https://www.un.org/esa/desa/papers/2017/wp152_2017.pdf (accessed February 28, 2023).
42. Friel S, Arthur M, Frank N. Power and the planetary health equity crisis. Lancet. (2022) 400:1085–7. doi: 10.1016/S0140-6736(22)01544-6
43. Friel S, Townsend B, Fisher M, Harris P, Freeman T, Baum F. Power and the people's health. Soc Sci Med. (2021) 282:114173. doi: 10.1016/j.socscimed.2021.114173
44. Porter L, Rickards L, Verlie B, Bosomworth K, Moloney S, Lay B, et al. Climate justice in a climate changed world. Plan Theory Pract. (2020) 21:293–321. doi: 10.1080/14649357.2020.1748959
45. Stanford V, Barna S, Gupta D, Mortimer F. Teaching skills for sustainable health care. Lancet Planet Health. (2023) 7:e64–7. doi: 10.1016/S2542-5196(22)00330-8
46. Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. (2010) 376:1923–58. doi: 10.1016/S0140-6736(10)61854-5
47. Frey D. ed. Psychologie der Werte [Psychology of values]. Berlin, Heidelberg: Springer (2016). doi: 10.1007/978-3-662-48014-4
48. Redvers N, Guzmán CAF, Parkes MW. Towards an educational praxis for planetary health: a call for transformative, inclusive, and integrative approaches for learning and relearning in the anthropocene. Lancet Planet Health. (2023) 7:e77–85. doi: 10.1016/S2542-5196(22)00332-1
49. Webb J, Raez-Villanueva S, Carrière PD, Beauchamp A-A, Bell I, Day A, et al. Transformative learning for a sustainable and healthy future through ecosystem approaches to health: insights from 15 years of co-designed ecohealth teaching and learning experiences. Lancet Planet Health. (2023) 7:e86–96. doi: 10.1016/S2542-5196(22)00305-9
50. Leichenko R, Gram-Hanssen I, O'Brien K. Teaching the “how” of transformation. Sustain Sci. (2022) 17:573. doi: 10.1007/s11625-021-00964-5
51. Capetola T, Noy S, Patrick R. Planetary health pedagogy: Preparing health promoters for 21st-century environmental challenges. Health Promot J Aust Off J Aust Assoc Health Promot Prof. (2022) 33(Suppl 1):17–21. doi: 10.1002/hpja.641
52. McLean M, Phelps C, Smith J, Maheshwari N, Veer V, Bushell D, et al. An authentic learner-centered planetary health assignment: 5-year evaluation of student choices to address sustainable development goal 13. (Climate Action). Front Public Health. (2022) 10:1049932. doi: 10.3389/fpubh.2022.1049932
53. Sopdie E, Wolf T, Spicer S, Kennedy S, Errecaborde KM, Colombo B, et al. Ecosystem health education: teaching leadership through team-based assignments. J High Educ Theory Pract. (2021) 21:4385. doi: 10.33423/jhetp.v21i6.4385
54. Otto IM, Donges JF, Cremades R, Bhowmik A, Hewitt RJ, Lucht W, et al. Social tipping dynamics for stabilizing Earth's climate by 2050. Proc Nat Acad Sci. (2020) 117:2354–65. doi: 10.1073/pnas.1900577117
55. Cunsolo A, Ellis NR. Ecological grief as a mental health response to climate change-related loss. Nat Clim Change. (2018) 8:275–81. doi: 10.1038/s41558-018-0092-2
56. Otto IM, Kim KM, Dubrovsky N, Lucht W. Shift the focus from the super-poor to the super-rich. Nat Clim Change. (2019) 9:82–4. doi: 10.1038/s41558-019-0402-3
57. Hickman AC, Johnson RL, Lawler SP. Health-promoting pedagogy: Using reflexivity to support learning and action in planetary health education. Health Promot J Austr. (2022) 1:22–6. doi: 10.1002/hpja.648
58. Affleck A, Roshan A, Stroshein S, Walker C, Luo OD. Accelerating the implementation of planetary health medical curricula to prepare future physicians to work in a climate crisis. Can Med Educ J. (2022) 13:89–91. doi: 10.36834/cmej.73003
59. Navarrete-Welton A, Chen JJ, Byg B, Malani K, Li ML, Martin KD, et al. grassroots approach for greener education: an example of a medical student-driven planetary health curriculum. Front Public Health. (2022) 10:1013880. doi: 10.3389/fpubh.2022.1013880
60. Rabin BM, Laney EB, Philipsborn RP. the unique role of medical students in catalyzing climate change education. J Med Educ Curric Dev. (2020) 7:2382120520957653. doi: 10.1177/2382120520957653
61. Mattijsen JC, Bree EM, van Brakema EA, Huynen MMTE, Visser EH, Blankestijn PJ, et al. Educational activism for planetary health—a case example from The Netherlands. Lancet Planet Health. (2023) 7:e18–20. doi: 10.1016/S2542-5196(22)00314-X
62. Oudbier J, Sperna Weiland NH, Boerboom T, Ravesloot JH, Peerdeman S, Suurmond J. An evidence-based roadmap to integrate planetary health education into the medical curriculum. Med Teach. (2022) 3:1–5. doi: 10.1080/0142159X.2022.2137015
63. Blom IM, Rupp I, Graaf IM de, Kapitein B, Timmermans A, Weiland NHS. Putting planetary health at the core of the medical curriculum in Amsterdam. Lancet Planet Health. (2023) 7:e15–7. doi: 10.1016/S2542-5196(22)00316-3
64. E.-M. Schwienhorst-Stich, K. Wabnitz, and M. Eichinger. “Lehre zu planetarer Gesundheit: Wie Menschen in Gesundheitsberufen zu Akteur:innen des transformativen Wandels werden [Planetary health education: how health professionals become agents of transformative change].” Planetary Health Klima, Umwelt und Gesundheit im Anthropozän edited by C. Traidl-Hoffmann, C. Schulz, M. Herrmann and B. Simon. Medizinisch Wissenschaftliche Verlagsgesellschaft (2021).
65. Artelle KA, Zurba M, Bhattacharyya J, Chan DE, Brown K, Housty J, et al. Supporting resurgent Indigenous-led governance: a nascent mechanism for just and effective conservation. Biol Conserv. (2019) 240:108284. doi: 10.1016/j.biocon.2019.108284
66. IPBES. Global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. In: Zenodo. (2019). doi: 10.5281/zenodo.6417333
Keywords: climate change, climate resilience, planetary health, planetary health education, medical education, transformative education, education for sustainable healthcare, eco health
Citation: Simon J, Parisi S, Wabnitz K, Simmenroth A and Schwienhorst-Stich E-M (2023) Ten characteristics of high-quality planetary health education—Results from a qualitative study with educators, students as educators and study deans at medical schools in Germany. Front. Public Health 11:1143751. doi: 10.3389/fpubh.2023.1143751
Received: 13 January 2023; Accepted: 07 March 2023;
Published: 25 April 2023.
Edited by:
Jouni J. K. Jaakkola, University of Oulu, FinlandReviewed by:
Colin David Butler, Australian National University, AustraliaCopyright © 2023 Simon, Parisi, Wabnitz, Simmenroth and Schwienhorst-Stich. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eva-Maria Schwienhorst-Stich, c2Nod2llbmhvcl9lQHVrdy5kZQ==
†ORCID: Sandra Parisi orcid.org/0000-0003-2029-3659
Eva-Maria Schwienhorst-Stich orcid.org/0000-0002-7715-5022
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.