- 1Department of Family Medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chia-Yi, Taiwan
- 2Department of Geriatric Medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chia-Yi, Taiwan
- 3School of Medicine, Tzu Chi University, Hualien, Taiwan
- 4Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
- 5Department of Oral Hygiene, College of Dental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 6School of Dentistry, College of Dental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 7Department of Psychiatry, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chia-Yi, Taiwan
- 8Department of Health-Business Administration, Fooyin University, Kaohsiung, Taiwan
- 9Department of Business Management, National Taichung University of Science and Technology, Taichung, Taiwan
- 10Ph.D. Program in Environmental and Occupational Medicine, College of Medicine, and Research Center for Precision Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 11Department of Environmental and Occupational Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
Introduction: Electronic cigarette (e-cigarette) use among adolescents has become increasingly common; therefore, effectively reducing adolescent e-cigarette use is an urgent issue. We aimed to predict and identify potential factors related to adolescent e-cigarette use behaviors.
Methods: This cross-sectional study was conducted using anonymous questionnaires given to Taiwanese high school students in 2020. Approximately 1,289 adolescent students completed questions on e-cigarette use, personal characteristics, family environment, and substances used. We performed multivariate logistic regression analyses to assess the model’s predictive performance in terms of the area under the receiver operating characteristic curve.
Results: We found that 9.3% of adolescent students used e-cigarettes. Tobacco smoking, close friends’ reactions to e-cigarette use, and the use of other substances were independent risk factors for adolescent e-cigarette use. Furthermore, relative to tobacco nonuse, tobacco use and tobacco smoking dependence had odds ratios of 76.49 and 113.81, respectively. The predictive accuracy of adolescent e-cigarette use from personal characteristics, family environment, and substance use status was 73.13, 75.91, and 93.80%, respectively.
Conclusion: The present study highlights the need for early prevention of e-cigarette use among adolescents, particularly those with a history of using tobacco and other substances and those who have close friends with positive attitudes towards e-cigarette use.
Introduction
Electronic cigarettes (e-cigarettes), battery-powered nicotine delivery systems, have been available for purchase since 2005 (1, 2). E-cigarettes were initially developed to help chain smokers quit tobacco smoking (3). Although e-cigarettes’ safety and health effects remain dangerous or lethal particularly by children and adolescents (2, 4), they are thus popular among adolescents and young adults. This is because e-cigarettes are available in numerous flavors, which lead potential users to feel curious about trying them; can be fashionable, stimulating, and a statement of rebellion against conventional values; and may increase positive moods (4–7). Specifically, in the United States, the prevalence of adolescent e-cigarette use increased from 4.2% in 2008 to 16.0% in 2015. In Taiwan, adolescent e-cigarette uses more than doubled from 2.1% in 2014 to 4.5% in 2017 (8, 9). The growing popularity of e-cigarettes among adolescents has raised concerns from policymakers and tobacco control advocates (10).
To date, several risk factors for e-cigarette use have been identified, including personal and sociodemographic characteristics (e.g., age, sex, ethnicity, and school status); substance use (e.g., tobacco); and social factors (close friends to e-cigarette use), particularly with regard to the family (e.g., smoking status of family members, family structure, education level of parents, allowance, and family economic status; Figure 1) (11–26). Most evidence related to adolescent e-cigarette use in Taiwan focused on the prevalence (10, 24, 25, 27–29); however, few studies assessed the risk factors for adolescent e-cigarette use in Taiwan (24–26). We therefore tended to re-identify these risk factors and develop a predictive model. In addition, we examined whether tobacco smoking initiation is associated with the risk of adolescent e-cigarette use (11, 20, 23, 25, 26) and further whether tobacco smoking dependence level influences e-cigarette use among adolescents.
We conducted an anonymous cross-sectional survey of Taiwanese high school students to identify the risk factors for e-cigarette use. Our findings aid tailored interventions against e-cigarette use among adolescents. Furthermore, we investigated whether tobacco smoking dependence level affected e-cigarette use among adolescents.
Methods
Study design and participants
This cross-sectional study distributed anonymous pen-and-paper questionnaires to 12–18-year-old high school students in Chiayi, Taiwan, between January and April 2020. We classified the 58 high schools distributed across Chiayi City and Chiayi County into two subgroups by grade: grades 7–9 (junior high school) and 10–12 (senior high school and vocational high school). We applied multi-level sampling methods for sample selection. First level was administrative areas. There were two administrative areas–Chiayi city and Chiayi country–in Chiayi, Taiwan. And second level was school subgroup. We classified into three subgroup high schools by the grade, which include grades 7–9 (junior high school), grades 10–12 (senior high school), and grades 10–12 (vocational high school). The schools were selected from each subgroup high school by probability proportionate to size sampling, so we selected 16 high schools (including 8 junior high schools, 4 senior high schools, and 4 vocational high schools) among 58 high schools in Chiayi areas.
Procedures and measures
Participants completed the self-administered questionnaire in their classrooms. To ensure that each participant responded willingly and truthfully to the questionnaire, no school staff members were present when the survey was completed. The data were collected by specialists and trained residents from the Dalin Tzu Chi Hospital family medicine department, who provided standardised instructions to the participants.
The questionnaire items covered the following three dimensions: (1) personal characteristics, namely sex, age, and school status (senior high school, junior high school, and vocational school); (2) family environment status, namely family structure, education levels of parents, parents’ ethnicities, allowance, and family economic status; and (3) substance use status, including tobacco use, use of other substances, close friends’ attitudes to tobacco smoking, e-cigarette use, and smoking status of family members. Participants who responded “yes” to “Have you ever used tobacco cigarettes or cigars?” were considered to be tobacco users. If a participant was a cigarette user who had smoked a cigarette in the past month and used ≥100 cigarettes in their lifetime, their level of dependence on tobacco smoking was evaluated using the 6-item Fagerstrom Tolerance Scale (FTS) (30, 31). These participants were then divided into low (FTS score: 0–4) and medium to high (FTS score: 5–10) cigarette dependence groups. In addition, participants who responded “yes” to “Have you ever used electronic cigarettes?” and “Have you used any form of additive products (e.g., alcohol, betel nut, or other illicit drugs such as amphetamine or ketamine)?” were considered to be e-cigarette users and users of other substances, respectively. A participant had a high and low weekly allowance if they received <NT$200 and ≥NT$200 weekly, respectively (in May 2022, US$1 = approximately NT$29).
Statistical analysis
The primary outcome was e-cigarette use. We also collected data on tobacco smoking status. We used the Chi-square and two-sample t-test to determine whether e-cigarette and tobacco smoking differed in their risk factors. The risk factors for e-cigarette use were determined using the adjusted odds ratio (aOR) with 95% confidence interval (CI) in hierarchically multiple logistic regressions. To compare the importance of differ predictors dimension, the area under the curve (AUC) was applied to represent the prediction power among various models. The predictive power of each of the three dimensions that the risk factors fell under was determined using the receiver operating characteristic curve, where a greater AUC indicates greater predictive power. All statistical analyses were performed using SAS software (version 9, SAS Institute, Cary, NC, United States).
Results
Among the 1,289 enrolled participants, 803 (62.4%) were male, and the majority were aged 12–18 years (mean age: 15.6 years). Moreover, 525 (40.7%), 340 (26.4%), and 424 (32.9%) participants were from junior, senior, and vocational high schools, respectively.
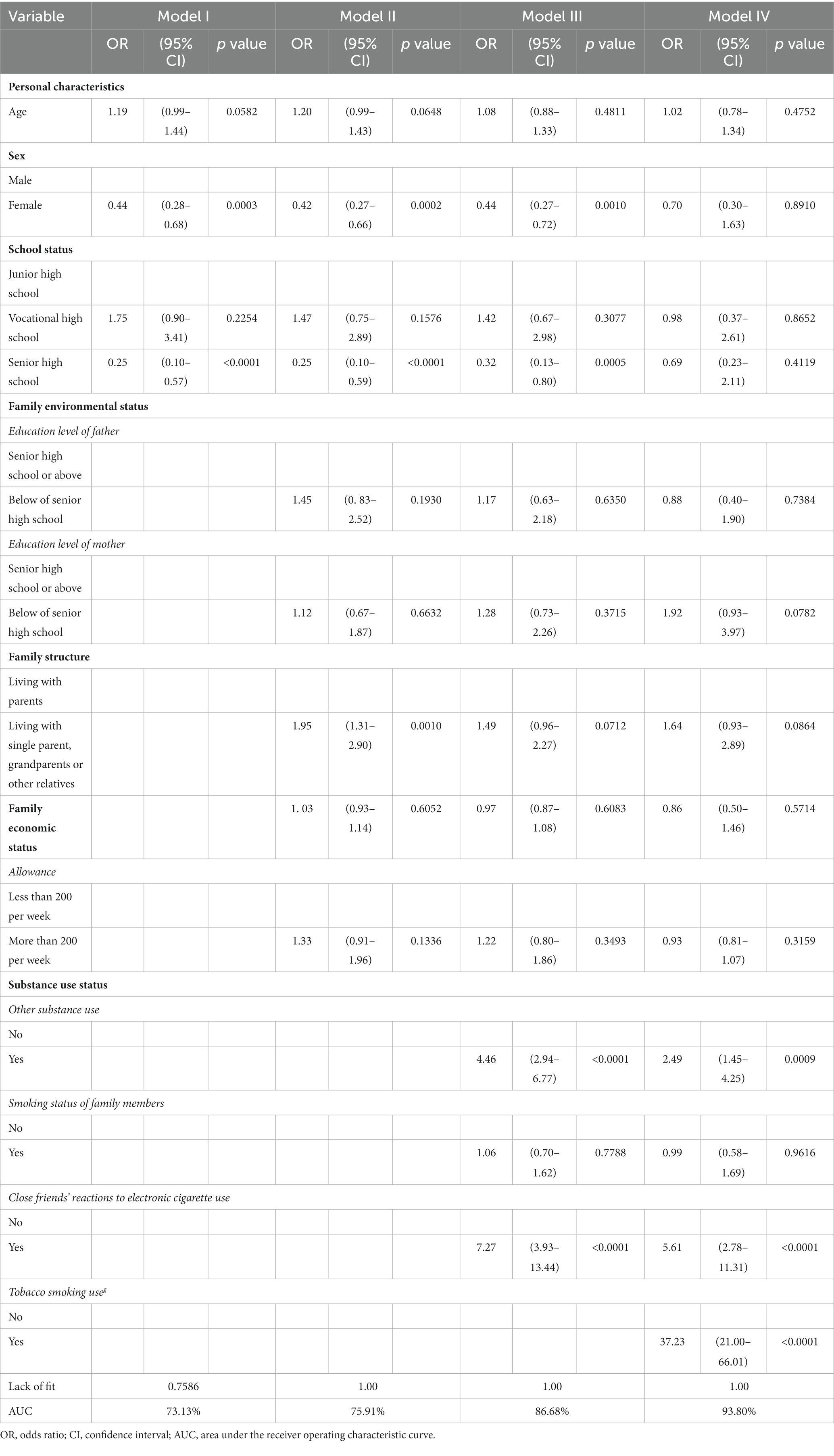
Table 1 presents the distribution of the sociodemographic characteristics of the e-cigarette nonusers and users. We found that 9.3% of all participants had used e-cigarettes at least once. The adolescents were significantly more likely to use e-cigarettes if they were male (p < 0.0001), were significantly older (p = 0.0029), were in a vocational high school (p < 0.0001), had parents with an education level below senior high school (both p < 0.0001), were living with their grandparents or other relatives or were living in a single-parent household (p < 0.0001), had a low allowance (p = 0.0051), had used another substance (p < 0.0001), had smoked tobacco (p < 0.0001), had at least one family member who smoked (p = 0.0032), and had positive close friends to e-cigarette use (p < 0.0001).
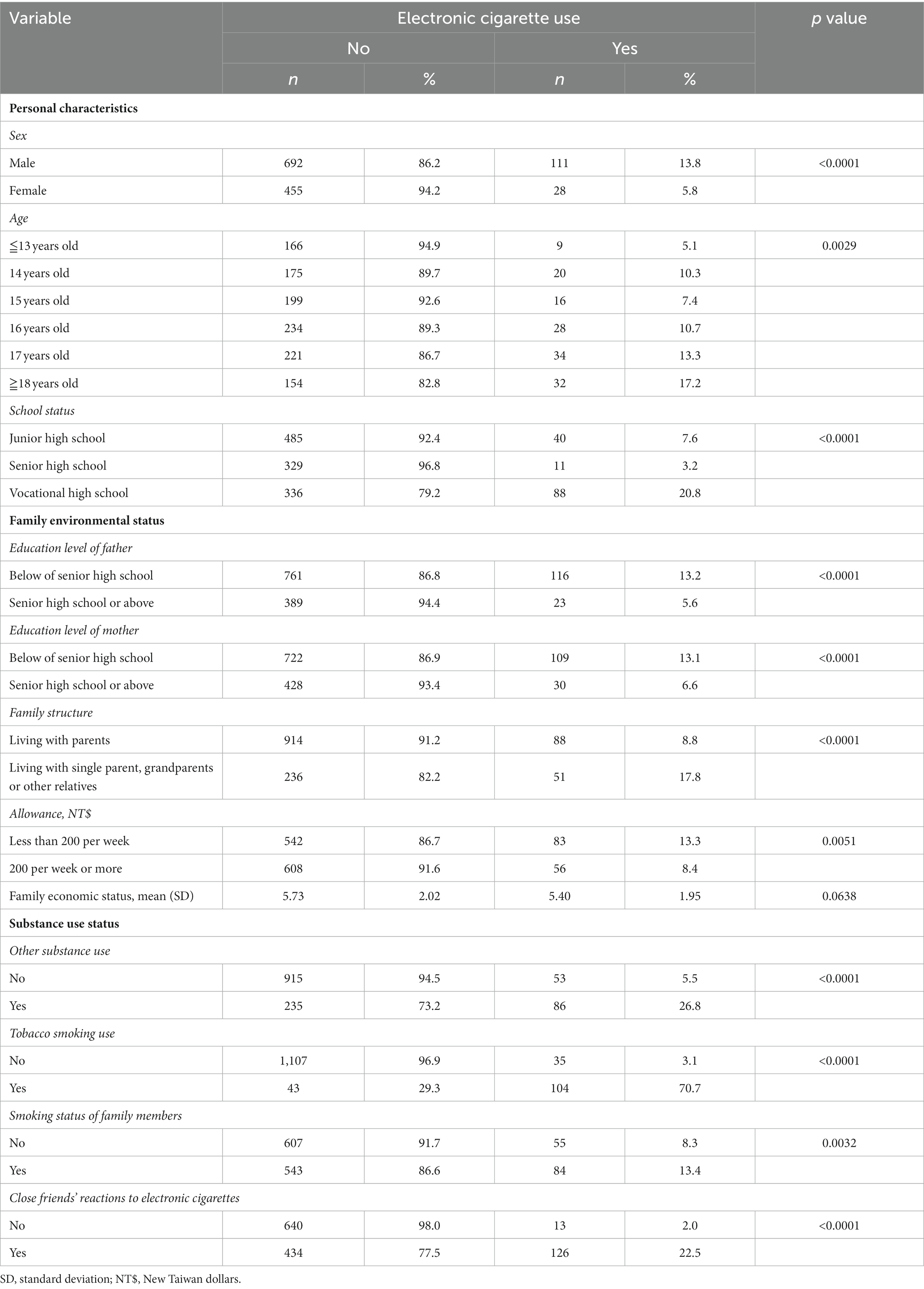
Table 1. Personal characteristics, family environmental and substance use status between the participants with electronic cigarette use and those without in adolescents.
Four regression models were constructed to identify risk factors (Table 2). Model I included risk factors in the dimension of personal characteristics, specifically age, sex, and school status. Female students were less likely to use e-cigarettes than male students (odds ratio [OR] = 0.44; 95% CI 0.28–0.68, p = 0.0003). Compared with junior high school students, senior high school adolescents were significantly less likely to use e-cigarettes (OR = 0.25; 95% CI 0.10–0.57, p < 0.0001) and vocational high school students were nonsignificantly more likely to use e-cigarettes (OR = 1.75; 95% CI 0.90–3.41, p = 0.2254). Model I had high accuracy (AUC = 73.13%).
Model II included risk factors in the dimensions of family environment and personal characteristics. Family structure was significantly related to e-cigarette use (adjusted OR [aOR] = 1.95; 95% CI 1.31–2.90, p = 0.0010). Model II was slightly more accurate than Model I (AUC = 75.91%).
Model III included risk factors in all three dimensions. E-cigarette use was significantly related to close friends to e-cigarette use (aOR = 7.27; 95% CI 3.93–13.44, p < 0.0001) and the use of other substances (aOR = 4.46; 95% CI 2.94–6.77, p < 0.0001). Model III was much more accurate than Models I and II (AUC = 86.68%); this indicated that substance use status is a strong predictor of e-cigarette use among adolescents.
Model IV included only tobacco smoking as a covariate, and e-cigarette use was affected by tobacco smoking (aOR = 37.23; 95% CI 21.00–66.01, p < 0.0001). Model IV was the most accurate model (AUC = 93.80%). Overall, the use of other substances, close friends to e-cigarettes, and tobacco smoking were independent risk factors for e-cigarette use in adolescents.
We also evaluated the risk factors for tobacco use. The distributions of the sociodemographic characteristics of tobacco users and nonusers are displayed in Supplementary Table S1. In total, 11.4% of the participants had smoked tobacco cigarettes and 17.8% had medium to high cigarette dependence. The results for the predictive power of each dimension with regard to tobacco use are presented in Supplementary Table S2.
Models I to III (now with tobacco use as the dependent variable) had AUCs of 78.19, 80.00, and 89.10%, respectively, similar to their respective AUCs when e-cigarette use was the dependent variable. Model I indicated that tobacco users were more likely to be male (aOR = 3.82; 95% CI: 2.33–6.29) and significantly more likely to be in junior high school than in senior high school (aOR = 0.15; 95% CI 0.06–0.40, p < 0.0001). Model III indicated that tobacco users were significantly more likely to have used other substances (aOR = 5.48; 95% CI 3.60–12.84, p < 0.0001) and have close friends who react favourably to tobacco smoking (aOR = 6.90; 95% CI 3.70–12.84, p < 0.0001). Overall, the independent risk factors for tobacco smoking in adolescents were being male, using other substances, and having positive close friends to tobacco smoking.
Tobacco use (OR = 76.49; 95% CI: 0.06–0.40, p < 0.0001; Table 3) and tobacco smoking dependence (OR = 113.81; 95% CI: 26.50–488.82, p < 0.0001) were significantly and positively associated with e-cigarette use.
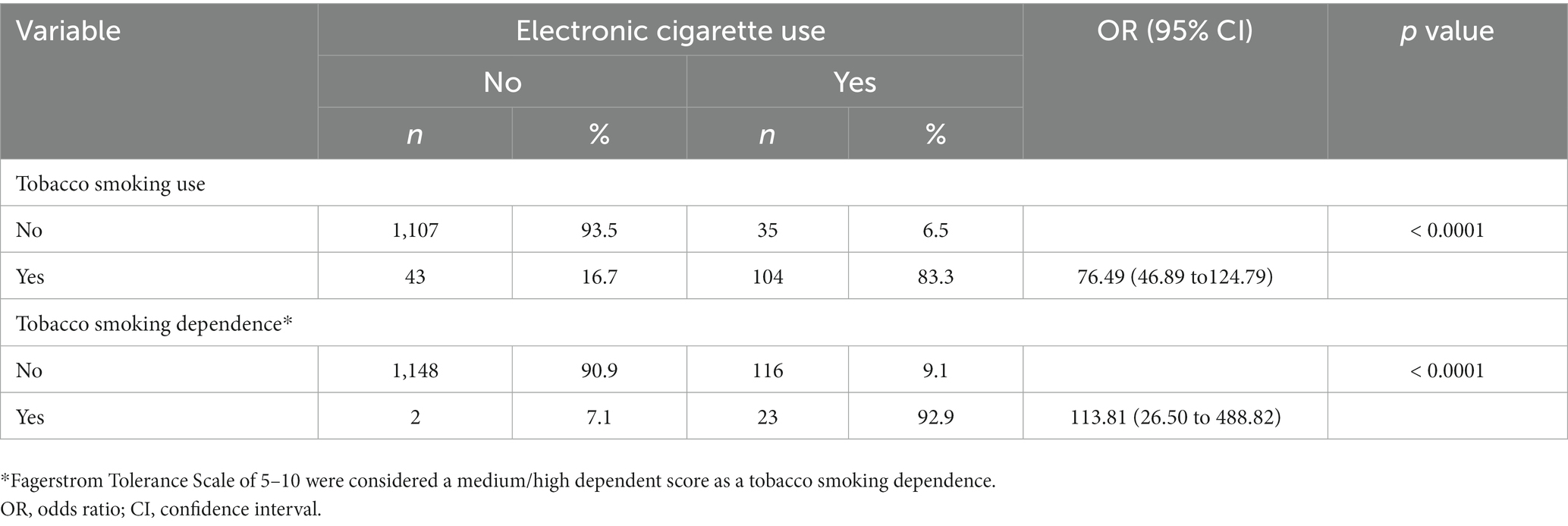
Table 3. Tobacco smoking use and dependence status affect electronic cigarette smoking behaviors in adolescents.
Discussion
To the best of our knowledge, this study is among few studies investigated the related factors that predict e-cigarette use behaviors among ethnic Chinese adolescents (24–26, 32, 33). A total of 9.3% of adolescent students in our study had used e-cigarettes. Tobacco use, the use of other substances, and positive close friends to e-cigarettes were independent risk factors for e-cigarette use in adolescents. The predictive accuracy of personal characteristics, family environment, and substance use status for e-cigarette use were 73.13, 75.91, and 93.80%, respectively. Furthermore, tobacco smoking dependence influenced e-cigarette use among adolescents.
The prevalence of adolescent e-cigarette usage varies with time, area, ethnicity, socioeconomic status, definition, and assessment tool. In our 2020 study, the prevalence of ever having used e-cigarettes among adolescent students in the Chiayi area of Taiwan was 9.3%. The Global Youth Tobacco Survey in Taiwan revealed that the prevalence of e-cigarette use in the previous 30 days among adolescents was 3.54% in 2017 (10). The percentages of adolescent students in Hong Kong who reported “ever having used” and “currently using” e-cigarettes in 2013 were 3.3 and 1.1%, respectively (33). In China, 3.1% of adolescents reported ever having used e-cigarettes in 2015, although only 0.5% of those adolescents reported current e-cigarette use (34). The prevalence of ever using e-cigarettes among adolescents in ethnic Chinese populations is generally lower than that among individuals in Western countries: 4.7% among German adolescent students (19), 12% among Hawaiian students (mean age: 14.6 years) (35), 16.0% among French high school students (36), 17.4% among Finnish students (12–18 years old) (15), and 23.5% among Polish students (15–19 years old) (37). Even in our results, the prevalence of e-cigarette use among ethnic Chinese adolescents remains lower than that that among global adolescents. Nevertheless, given the increase in use, identifying the factors that increase the risk of e-cigarette use is crucial for the early prevention of e-cigarette use among ethnic Chinese adolescents.
In our multivariate logistic regression analyses of risk factors for adolescent e-cigarette use, substance use status had a more influential effect than that of personal characteristics and family environment (Table 2). The independent risk factors for adolescent e-cigarette use were personal tobacco smoking, the use of other substances, and close friends to e-cigarette use. Tobacco smoking has been associated with an increased risk of e-cigarette use among adolescents. Our findings are consistent with other published studies (11, 23). Our study further revealed that personal tobacco smoking (OR = 37.23) was the most influential factor determining adolescent e-cigarette use.
Furthermore, tobacco use and tobacco smoking dependence were risk factors for e-cigarette use, and their ORs were approximately 76 and 114, respectively. The result indicates that tobacco smoking dependence can affect adolescent e-cigarette use. Studies have demonstrated that adolescent e-cigarette use is associated with the use of other substances, such as binge drinking and cannabis use (16, 38). Empirical studies have also demonstrated that using e-cigarettes at any point during adolescence is associated with the use of other substances, such as alcohol, tobacco from shisha, and marijuana (14, 39). These findings are consistent with our findings, suggesting that more attention should be focused on multiple substance use among adolescents. Additionally, research on e-cigarette use has indicated that university students are influenced by their family members to a far lower degree than by their close friends (18). This conclusion agrees with our finding that close friends’ attitudes to e-cigarette use are predictors of e-cigarette usage.
We report three findings regarding the risk factors of e-cigarette use and tobacco use among adolescents (Table 2; Supplementary Table S2). First, our models had high accuracy (AUC > 80%) in predicting e-cigarette and tobacco use among adolescents, with greater accuracy for e-cigarette use (AUC = 93.87% vs. 89.10%). Second, substance use status was a key risk factor for e-cigarette use and tobacco use among adolescents. Third, family environment had a stronger relationship with e-cigarette use than tobacco use, although this relationship was nonsignificant after other risk factors were adjusted for. This result indicates that interventions against e-cigarette use among adolescents should also focus on the adolescent’s family environment.
Our study has several limitations. First, the study was cross-sectional and was conducted in one geographic area. Nonetheless, our findings related to e-cigarette use and tobacco smoking are consistent with those of other studies in Taiwan (8–10, 18) Second, measurement bias might exist because the participants were asked the sensitive question about whether they had ever used e-cigarettes. Furthermore, because of the self-reported nature of the questionnaire, the respondents may have underestimated their e-cigarette use. To minimise this bias, we used anonymous questionnaires and barred school staff members from being present during the survey. Third, we could not determine that the dose–response of tobacco use affects e-cigarette use in adolescents because we did not count the quantity consumption of cigarettes (e.g., how many cigarettes did the participants smoke every day?) in our study. Nonetheless, we determined the qualitative effect of cigarette dependence e-cigarette use by dividing the participants by FTS score. Fourth, and finally, our study did not investigate the reasons for the adoption of e-cigarette use behaviors among adolescents.
Conclusion
The present study analyses the predictive power of personal characteristics, family environment, and substance use status in relation to e-cigarette use among adolescents. Policymakers should pay attention to those who have used tobacco or other substances and to the attitudes of close friend groups towards e-cigarettes when developing smoking prevention and cessation strategies, in addition to regulating e-cigarette advertising and adolescent access to e-cigarettes (23, 40).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study was approved by the Institutional Review Board of Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taiwan (approval number: B10904015). Written informed consent was waived because we used an anonymous survey.
Author contributions
P-IL, P-SH, and J-HT conceptualised and designed the study, conducted the statistical analyses, drafted the initial article, and reviewed and revised the article. M-NL and H-YC supervised the data collection, helped with the initial drafting of the article, and reviewed and revised the article. Y-HY, K-FW, and P-SH assisted with the statistical analyses and interpretation of data. All authors have approved the final article and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Miss Mei-Hsin Ho for her assistance. The primary data of the present study were posted on the 2021 Annual Academic Seminar of Taiwan Association of Family Medicine in Taiwan.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1140615/full#supplementary-material
References
1. Yoong, SL, Stockings, E, Chai, LK, Tzelepis, F, Wiggers, J, Oldmeadow, C, et al. Prevalence of electronic nicotine delivery systems (ENDS) use among youth globally: a systematic review and meta-analysis of country level data. Aust N Z J Public Health. (2018) 42:303–8. doi: 10.1111/1753-6405.12777
2. Hajek, P, Etter, JF, Benowitz, N, Eissenberg, T, and McRobbie, H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. (2014) 109:1801–10. doi: 10.1111/add.12659
3. Patel, D, Davis, KC, Cox, S, Bradfield, B, King, BA, Shafer, P, et al. Reasons for current E-cigarette use among US adults. Prev Med. (2016) 93:14–20. doi: 10.1016/j.ypmed.2016.09.011
4. Jiang, TH, Cheng, LM, and Hawkins, MA. A study of regulatory policies and relevant issues concerning electronic cigarette use in Taiwan. Int J Health Plann Manage. (2017) 33:e119–30. doi: 10.1002/hpm.2440
5. Jessor, R. New Perspectives on Adolescent Risk Behavior In: R Jessor, editor. New perspectives on adolescent risk behavior. New York, NY: Cambridge University Press (1998)
6. Colder, CR, Chassin, L, Villalta, I, and Lee, M. Affect regulation and substance use: a developmental perspective In: J Kassel, editor. Substance Use and Emotion. Washington, DC: American Psychological Association (2010)
7. Pepper, JK, and Brewer, NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review. Tob Control. (2014) 23:375–84. doi: 10.1136/tobaccocontrol-2013-051122
8. Taiwan Health Promotion Administration. Taiwan Tobacco Control Annual Report 2018. Taipei City (Taiwan): Ministry of Health and Welfare (2018).
9. Taiwan Health Promotion Administration. Global Youth Tobacco Survey: Ministry of Health and Welfare; (2018). Available at: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1077&pid=62042018 (Accessed January 28, 2022).
10. Gao, W, Sanna, M, Huang, LL, Chiu, YW, Chen, YH, and Chiou, HY. Juggling two balls-smoking (re) normalization and harm reduction: e-cigarettes-facts and misconceptions in Taiwan. Asia Pac J Public Health. (2018) 30:328–31. doi: 10.1177/1010539518773479
11. Dutra, LM, and Glantz, SA. Electronic cigarettes and conventional cigarette use among us adolescents: a cross-sectional study. JAMA Pediatr. (2014) 168:610–7. doi: 10.1001/jamapediatrics.2013.5488
12. Lee, S, Grana, RA, and Glantz, SA. Electronic cigarette use among Korean adolescents: a cross-sectional study of market penetration, dual use, and relationship to quit attempts and former smoking. J Adolesc Health. (2014) 54:684–90. doi: 10.1016/j.jadohealth.2013.11.003
13. Barrington-Trimis, JL, Berhane, K, Unger, JB, Cruz, TB, Huh, J, Leventhal, AM, et al. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. (2015) 136:308–17. doi: 10.1542/peds.2015-0639
14. White, J, Li, J, Newcombe, R, and Walton, D. Tripling use of electronic cigarettes among New Zealand adolescents between 2012 and 2014. J Adolesc Health. (2015) 56:522–8. doi: 10.1016/j.jadohealth.2015.01.022
15. Kinnunen, JM, Ollila, H, El-Amin, SE, Pere, LA, Lindfors, PL, and Rimpelä, AH. Awareness and determinants of electronic cigarette use among Finnish adolescents in 2013: a population-based study. Tob Control. (2015) 24:e264–70. doi: 10.1136/tobaccocontrol-2013-051512
16. Surís, JC, Berchtold, A, and Akre, C. Reasons to use e-cigarettes and associations with other substances among adolescents in Switzerland. Drug Alcohol Depend. (2015) 153:140–4. doi: 10.1016/j.drugalcdep.2015.05.034
17. Krishnan-Sarin, S, Morean, ME, Camenga, DR, Cavallo, DA, and Kong, G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. (2015) 17:810–8. doi: 10.1093/ntr/ntu243
18. Lotrean, LM. Use of electronic cigarettes among Romanian university students: a cross-sectional study. BMC Public Health. (2015) 15:358. doi: 10.1186/s12889-015-1713-6
19. Hanewinkel, R, and Isensee, B. Risk factors for e-cigarette, conventional cigarette, and dual use in German adolescents: a cohort study. Prev Med. (2015) 74:59–62. doi: 10.1016/j.ypmed.2015.03.006
20. Jeon, C, Jung, KJ, Kimm, H, Lee, S, Barrington-Trimis, JL, McConnell, R, et al. E-cigarettes, conventional cigarettes, and dual use in Korean adolescents and university students: prevalence and risk factors. Drug Alcohol Depend. (2016) 168:99–103. doi: 10.1016/j.drugalcdep.2016.08.636
21. Kinnunen, JM, Ollila, H, Lindfors, PL, and Rimpelä, AH. Changes in electronic cigarette use from 2013 to 2015 and reasons for use among Finnish adolescents. Int J Environ Res Public Health. (2016) 13:1114. doi: 10.3390/ijerph13111114
22. Park, S, Lee, H, and Min, S. Factors associated with electronic cigarette use among current cigarette-smoking adolescents in the Republic of Korea. Addict Behav. (2017) 69:22–6. doi: 10.1016/j.addbeh.2017.01.002
23. Soneji, S, Barrington-Trimis, JL, Wills, TA, Leventhal, AM, Unger, JB, Gibson, LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. (2017) 171:788–97. doi: 10.1001/jamapediatrics.2017.1488
24. Chen, PC, Chang, LC, Hsu, C, and Lee, YC. Dual use of e-cigarettes and traditional cigarettes among adolescents in Taiwan, 2014–2016. Nicotine Tob Res. (2019) 21:48–54. doi: 10.1093/ntr/nty003
25. Chien, YN, Gao, W, Sanna, M, Chen, PL, Chen, YH, Glantz, S, et al. Electronic cigarette use and smoking initiation in Taiwan: evidence from the first prospective study in Asia. Int J Environ Res Public Health. (2019) 16:1145. doi: 10.3390/ijerph16071145
26. Lee, YC, Chang, LC, Hsu, C, and Chen, PC. Comparing the characteristics of cigarette smoking and e-cigarette and IQOS use among adolescents in Taiwan. J Environ Public Health. (2020) 2020:7391587. doi: 10.1155/2020/7391587
27. Chang, HC, Tsai, YW, Shiu, MN, Wang, YT, and Chang, PY. Elucidating challenges that electronic cigarettes pose to tobacco control in Asia: a population-based national survey in Taiwan. BMJ Open. (2017) 7:e014263. doi: 10.1136/bmjopen-2016-014263
28. Chen, YL, Wu, SC, Chen, YT, Hsiao, PC, Yu, YH, Ting, TT, et al. E-cigarette use in a country with prevalent tobacco smoking: a population-based study in Taiwan. J Epidemiol. (2019) 29:155–63. doi: 10.2188/jea.JE20170300
29. Gao, W, Sanna, M, Chuluunbaatar, E, Tsai, MK, Levy, DT, and Wen, CP. Are e-cigarettes reviving the popularity of conventional smoking among Taiwanese male adolescents? A time-trend population-based analysis for 2004-2017. Tob Control. (2021) 30:132–6. doi: 10.1136/tobaccocontrol-2019-055310
30. Heatherton, TF, Kozlowski, LT, Frecker, RC, and Fagerstrom, KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict. (1991) 86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x
31. Health Promotion Administration. 6-item Fagerstrom Tolerance Scale version Chinese. Health Promotion Administration Ministry of Health Welfare: Health 99 Pulse Education Resource, Taiwan; (2010). Available at: http://health99.hpa.gov.tw/onlineQuiz/smoking (Accessed January 28, 2022).
32. Zhu, J, Shi, F, Gang, X, Li, N, Li, J, He, Y, et al. Conventional cigarette and E-cigarette smoking among school personnel in Shanghai, China: prevalence and determinants. Int J Environ Res Public Health. (2019) 16:3197. doi: 10.3390/ijerph16173197
33. Jiang, N, Wang, MP, Ho, SY, Leung, LT, and Lam, TH. Electronic cigarette use among adolescents: across-sectional study in Hong Kong. BMC Public Health. (2016) 16:1–8. doi: 10.1186/s12889-016-2719-4
34. Wang, W, He, Z, Feng, N, and Cai, Y. Electronic cigarette use in China: awareness, prevalence and regulation. Tob Induc Dis. (2019) 17:30. doi: 10.18332/tid/105393
35. Wills, TA, Knight, R, Williams, RJ, Pagano, I, and Sargent, JD. Risk factors for exclusive e-cigarette use and dual e-cigarette and tobacco use in adolescents. Pediatrics. (2015) 135:e43–51. doi: 10.1542/peds.2014-0760
36. Spilka, S, Godeau, E, Le Nézet, O, Ehlinger, V, Janssen, E, Brissot, A, et al. Usages d’alccol, de tabac et de cannabis chez les adolescents du secondaie en 2018. Tendances. (2019) 132:1–4.
37. Goniewicz, ML, and Zielinska-Danch, W. Electronic cigarette use among teenagers and young adults in Poland. Pediatrics. (2012) 130:e879–85. doi: 10.1542/peds.2011-3448
38. Dautzenberg, B, Birkui, P, Noël, M, Dorsett, J, Osman, M, and Dautzenberg, MD. E-cigarette: a new tobacco product for schoolchildren in Paris. Open J Respir Dis. (2013) 3:21–4. doi: 10.4236/ojrd.2013.31004
39. Camenga, DR, Kong, G, Cavallo, DA, Liss, A, Hyland, A, Delmerico, J, et al. Alternato tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smoker. J Adolesc Health. (2014) 55:588–91. doi: 10.1016/j.jadohealth.2014.06.016
Keywords: electronic cigarette, adolescent, prediction, risk factors, tobacco
Citation: Liu P-I, Lin M-N, Ho P-S, Tsai J-H, Yang Y-H, Wu K-F and Chuang H-Y (2023) Prediction and potential risk factors for electronic cigarette use behaviors among adolescents: a pilot study in Chiayi, Taiwan. Front. Public Health. 11:1140615. doi: 10.3389/fpubh.2023.1140615
Edited by:
Jaya Kumar, National University of Malaysia, MalaysiaReviewed by:
Rashidi Mohamed, National University of Malaysia, MalaysiaSharifa Ezat Wan Puteh, National University of Malaysia, Malaysia
Copyright © 2023 Liu, Lin, Ho, Tsai, Yang, Wu and Chuang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jui-Hsiu Tsai, ZmFhbnZhbmdvZ2hAZ21haWwuY29t; Pei-Shan Ho, cHNob0BrbXUuZWR1LnR3
†These authors have contributed equally to this work and share first authorship
 Ping-I Liu1,2†
Ping-I Liu1,2† Pei-Shan Ho
Pei-Shan Ho Jui-Hsiu Tsai
Jui-Hsiu Tsai Ya-Hui Yang
Ya-Hui Yang Hung-Yi Chuang
Hung-Yi Chuang