- 1Health Systems Strengthening, World Health Organization - Country Office for Liberia, Monrovia, Montserrado, Liberia
- 2World Health Organization, Geneva, Switzerland
- 3Ministry of Health Liberia, Monrovia, Liberia
- 4World Health Organization - Country Office for Liberia, Monrovia, Montserrado, Liberia
- 5National Public Health Institute of Liberia, Monrovia, Montserrado, Liberia
This article is part of the Research Topic ‘Health Systems Recovery in the Context of COVID-19 and Protracted Conflict'
Liberia is one of the three countries worst hit by the 2014–2016 West Africa Ebola Virus disease (EVD) outbreak, during which it recorded over 10,000 cases, including health workers. Estimates suggest that the non-EVD morbidity and mortality resulting from the collapse of the health system exceeded the direct impact of EVD. Lessons from the outbreak were clear, not only for Liberia but also for the regional and global communities: that building health system resilience through an integrated approach is an investment in population health and wellbeing, as well as economic security and national development. It is therefore no surprise that Liberia made recovery and resilience a national priority from the time the outbreak waned in 2015. The recovery agenda provided the platform for stakeholders to work toward the restoration of the pre-outbreak baseline of health system functions while aiming to build a higher level of resilience, informed by lessons from the Ebola crises. Based on the co-authors' experiences of on-the-ground country-support work, this study sought to provide an overview of the Liberia Health Service Resilience project (2018–2023) funded by KOICA, and propose a set of recommendations for national authorities and donors, derived from the authors' perceptions of best practices and key challenges associated with the project. We used both quantitative and qualitative approaches to generate the data represented in this study by reviewing published and unpublished technical and operational documents, and datasets derived through situational and needs assessments and routine monitoring and evaluation activities. This project has contributed to the implementation of the Liberia Investment Plan for Building a Resilient Health System and the successful response to the COVID-19 outbreak in Liberia. Although limited in scope, the Health Service Resilience project has demonstrated that health system resilience could be operationalized by applying a catchment and integrated approach and encouraging multi-sectoral collaboration, partnership, local ownership, and promoting the Primary Health Care approach. Principles applied in this pilot could guide the operationalization of health system resilience efforts in other resource-limited settings similar to Liberia and beyond.
Introduction
Liberia is one of the three countries worst hit by the 2014–2016 West Africa Ebola Virus disease (EVD) outbreak, during which it recorded over 10,000 cases, including health workers. Estimates suggest that the non-EVD morbidity and mortality resulting from the collapse of the health system exceeded the direct impact of EVD (1). The health and socioeconomic impacts of the outbreak were felt by individuals, communities, governments, and organizations long after the outbreak. Lessons from the outbreak were clear, not only for Liberia but also for the regional and global communities: that building health system resilience through an integrated approach (2) is an investment in population health and wellbeing, as well as in economic security and national development. It is, therefore, no surprise that Liberia made recovery and resilience a national priority in 2015 when the outbreak began to wane (3). The recovery agenda provided the platform for stakeholders to work toward the restoration of the pre-outbreak baseline of health system functions while aiming to build a higher level of resilience, informed by lessons from the Ebola crises.
The health system was ill-equipped to effectively respond to EVD with the necessary occupational health, safety, infection prevention, and control (IPC) measures for safe and effective health services. As a result, health workers suffered a 30 times higher risk of infection compared to the general population. As of April 8, 2015, 372 health workers had been infected, of whom 184 died (3). Pre-existing (pre-EVD) system vulnerabilities, partly due to the impact of a 14-year civil war in Liberia, contributed to the aftermath of EVD. Such vulnerabilities included inadequate and poorly motivated health workers, insufficient and unsuitable infrastructure and equipment, a weak supply chain system, and poor overall quality of care. These contributed to around 50% disruption in the delivery of routine health services during EVD due to health facility closures, fears and refusal of health workers to provide routine health services, and community distrust and fears (3). Coverage of life-saving maternal and child health interventions, in particular, declined dramatically, from already low levels (3).
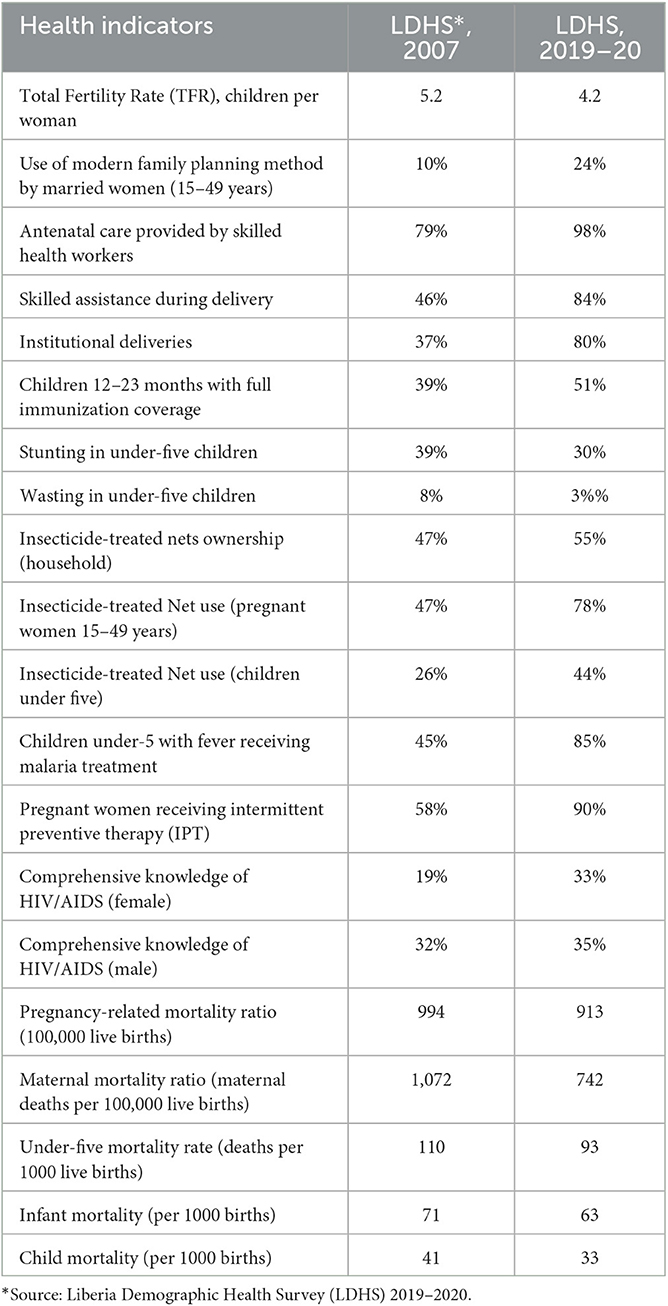
Table 1 presents key health system indicators in the pre- and post-EVD era (4, 5).
Liberia's 2015–2021 Investment Plan for Building a Resilient Health System (3) was developed to support the transition of the health system from EVD response to recovery and the “building back better” of a health system that provided quality routine services while also remaining resilient to future outbreaks. More specifically, the plan aimed to improve the health of Liberians and achieve equitable health outcomes by improving access to safe and quality services, establishing a robust Health Emergency Risk Management System, and building an enabling environment that restored trust in the health system's ability to provide services (3). The plan identified nine key investment areas, namely, building a fit-for-purpose health workforce, re-engineering the health infrastructure, strengthening Emergency Preparedness and Response (EPR) and surveillance, restoring and enhancing service delivery systems, enhancing capacity for essential medicines and supplies, strengthening information and research systems, expanding capacity for leadership and governance, establishing sustainable financing systems, and establishing a professional community workforce (3).
The ultimate goal of the Investment Plan was to enhance health system resilience. The resilience of a health system is the capacity of health actors, institutions, and populations to prepare for and effectively respond to crises; maintain core functions when a crisis hits; and informed by lessons learned during the crisis, reorganize if conditions require (2). An integrated approach (6) to develop and sustain the quality of routine services and emergency preparedness in tandem was emphasized in the Investment Plan. However, operationalizing this integrated approach in the Liberia health system remained a gap (7).
A 5-year (2018–2023) Health Services Resilience (HSR) project, funded by the Korea International Corporation Agency (KOICA) through the Global Disease Eradication Fund (GDEF), was approved for implementation in Liberia in October 2018 with the aim of “Making Health Services Resilient with Quality and Preparedness for Emergency Response in Liberia”. A parallel project, also funded by KOICA, is implemented in Ethiopia. Liberia's project sought to contribute to the implementation of priority activities of the Investment Plan, especially building a fit-for-purpose health workforce that equitably and optimally delivers quality services (Investment Plan Area A and Project Outcome 3). The project leveraged the momentum for focusing on resilience; structures established post-Ebola through the Investment Plan, such as the establishment of the Quality Management Unit within the Ministry of Health (MoH); and aspirations to finalize and roll out a National Quality Strategy.
An in-depth situational assessment (SA) of the state of quality and resilience in Liberia post-EVD (7) foregrounded work on the HSR project. The SA revealed a general weakness in human resource capacity in healthcare quality and resilience and a paucity of associated technical tools (guidelines, plans, strategies, and sets of indicators). It also found a lack of integration of the metrics used for healthcare quality and emergency preparedness in health services. The SA equally highlighted the need for a systematic and integrated approach to improving the capacity of health workers and health system leaders in quality and resilience by ensuring their active participation in activities related to health service quality and preparedness for public health emergencies.
The Health Services Resilience project set out to provide catalytic support (financial and technical) to the Ministry of Health (MoH), the National Public Health Institute of Liberia (NPHIL), and other relevant institutions, coordinated by the World Health Organization (WHO), to address the gaps identified from the SA and enhance the implementation of the Investment Plan. The project also aimed to operationalize the concept of resilience at the policy and operational levels of the health system by applying the key lessons learned from shock experiences, with such lessons essential for the recovery and transformation of a health system post-crisis (6).
Aims and objectives
This study aims to:
• Provide an overview of the Liberia HSR project (2018–2023) funded by KOICA, with a focus on its guiding principles, key features of its set-up, main activities, achievements, best practices, and challenges.
• Explore the contribution of the HSR project to the implementation of the Investment Plan for Building a Resilient Health System in Liberia and broader health system and population health outcomes in Liberia.
• Propose a set of recommendations for national authorities and donors, derived from the authors' perceptions of best practices and key challenges associated with the project, with a focus on “building back better” health systems post-COVID-19 and on strengthening preparedness for future public health events.
Insights from this case study would be useful for learning from Liberia's experience in long-term recovery efforts and the benefits of investing in more integrated, system-strengthening, resilience-focused initiatives. This is particularly timely as many countries are embarking on recovery from the ongoing COVID-19 pandemic and other health system shocks.
Methods
The sources of data represented in this study comprise official reports from the HSR project, published and unpublished technical and operational documents from it, and datasets generated through situational and needs assessments and routine monitoring and evaluation activities. In this section, we describe the methodological steps specific to the current study, namely how we identified documents for review and how findings from them were extracted and synthesized. Sections “Approach to developing and refining the project goals, tools and activities” and “Monitoring and Evaluation” under “Overview of the HSR project” provide detail on data collection methods used to serve the needs of the HSR project development, implementation, and monitoring and evaluation. Relative to the current study, these processes fed in ready data which we only synthesized. As the original goals served by such data were strongly operational, and also somewhat different from the goals of the current study, the pre-existing data we use have significant limitations. These are discussed under the Section Study strengths and limitations at the end of the article.
Identification and prioritization of documents and data sources
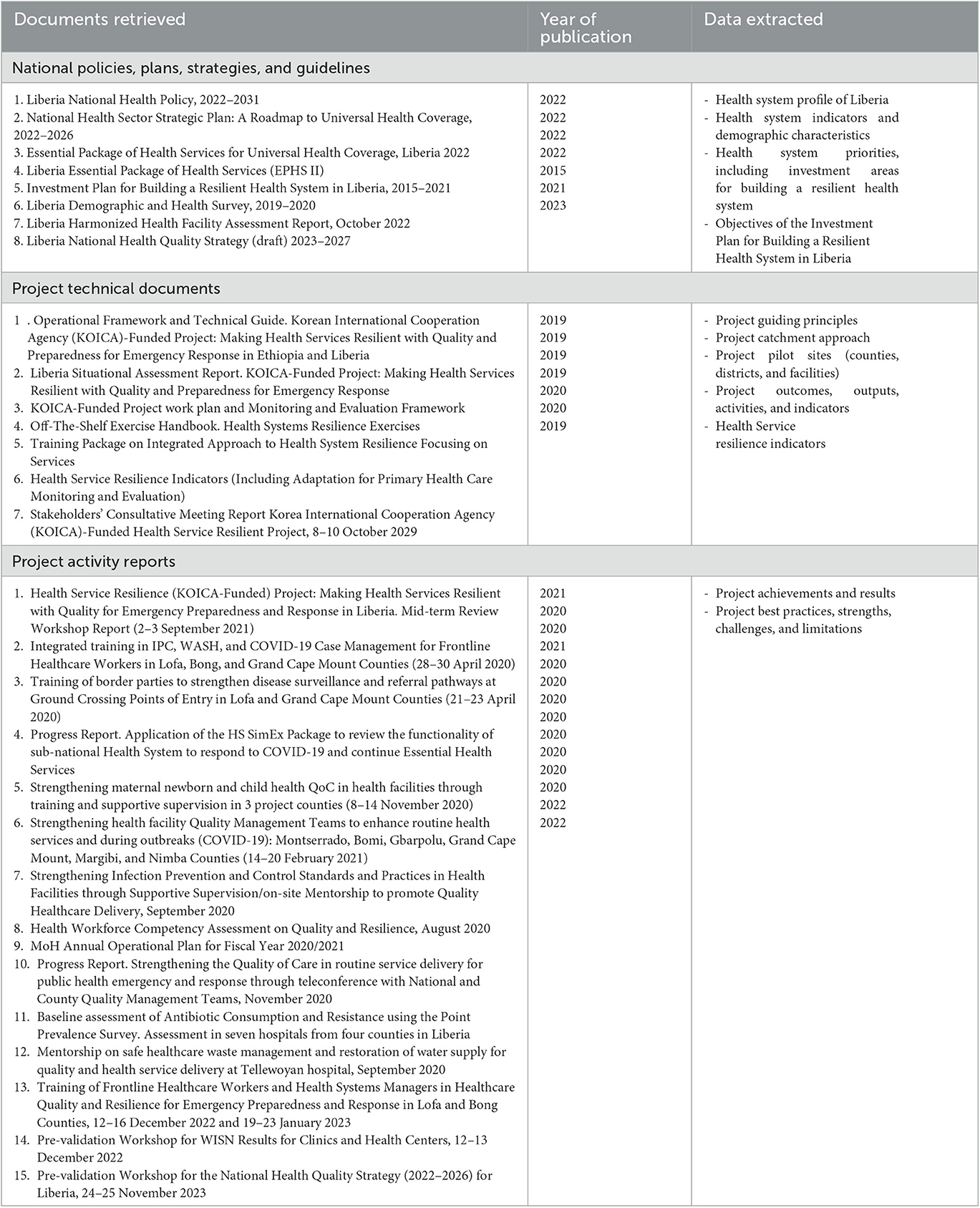
To identify the richest and most reliable documents that can be used to construct an overview of Liberia's HSR project (study goal 1), LA and RS first reviewed all major project folders and developed a draft list of key project-generated documents (Table 2). The list was supplemented by titles of documents concerning the Investment Plan for Building a Resilient Health System and broader health system and population health outcomes (3, 4, 8–13) in Liberia (study goal 2). These were identified through online searches in PubMed, Google Scholar and Google by using search terms such as “public health emergency,” “health care quality,” “service resilience,” “health system resilience,” and “resilience capacities,” and through soliciting advice from MoH colleagues. The combined draft list was then enriched with recommendations made by stakeholders at MoH, NPHIL, WHO, and further relevant institutions and partners [United Nations International Children's Emergency Funds-UNICEF, USAID-supported John Hopkins Program for International Education in Gynecology and Obstetrics-, Jhpiego and Last Mile Health (LMH)]. The process was iterative and resulted in the final list presented in Table 2. All documents from the list were then retrieved, including the most recent drafts of un-finalized policies and plans.
Approach to data extraction and synthesis
LA and RS independently reviewed the selected documents for data that can serve to address the study objectives. Data were extracted in Microsoft Word. Table 1 (third column) shows what types of data were extracted from the different categories of documents. The process of considering the relevance of data and representing and prioritizing it was iterative, with key stages involving all co-authors. Data were synthesized following recommendations made by Lin et al. (14) on using health system data in combination with systematic reviews to support decision-making.
Findings
Overview of the HSR project
Liberia's Health Services Resilience project was designed for implementation over 5 years (October 2018–October 2023) and had a clear work plan comprising five outcomes and 15 outputs as well as a monitoring and evaluation framework (Box 1) (15). These were all agreed upon and jointly implemented by key stakeholders from global, national, sub-national, and service delivery levels. This section offers an overview of the project in terms of its guiding principles; key stakeholders; settings; approaches to the development and implementation of goals, tools, and activities; and monitoring and evaluation framework.
Box 1. Overall goal and summary of expected outcomes of the HSR project.
To build resilience in health systems to enable quality health services in all contexts, along with preparedness.
✓ Build health service resilience with systematic consideration of quality and emergency preparedness for response including health services continuity
✓ Develop bridges between work on health systems (primarily MoH responsibility) and health security (primarily NPHIL responsibility) as well as between the human health sector and allied sectors (such as animal health).
✓ Promote effective health system participation in emergency preparedness and response
The Korean International Cooperation Agency (KOICA) funded the project, through the Global Disease Eradication Fund (GDEF).
Guiding principles
The following key principles underpinned all project activities and tools:
• Government ownership and leadership. All project activities are implemented with the leadership of responsible local and national health authorities. This includes the participation of the Minister of Health and Director General (DG) of NPHIL in project workshops and their guidance on the implementation of project activities.
• Local, national, and international stakeholders' participation and collaboration. The project team applies a collaborative and coordinated approach with national and international stakeholders at all administrative levels to avoid duplication and fragmentation of efforts. A “One work plan, One budget” approach is used to enhance collaboration, transparency, and efficiency in project implementation.
• “One WHO” support. The skills and experience at all three levels of WHO (Country Office, Regional Office for Africa, and Headquarters) have been harnessed in the project development and implementation.
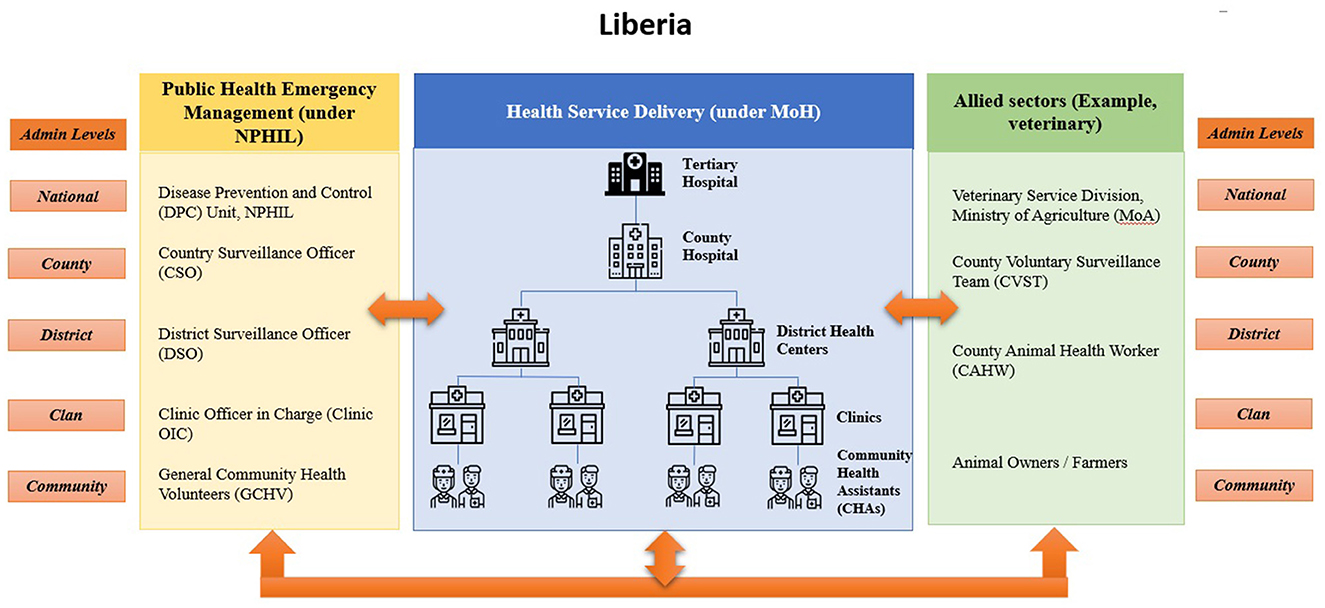
• Catchment approach. Project implementation involves actors responsible for strengthening service delivery and emergency preparedness and response at the four levels of the health system (community/health facility, health district, county, and national levels) and from the animal and environmental health sectors, in addition to the human health one (One-Health umbrella) (16).
• Primary healthcare focus. The project prioritizes high-impact activities at the community and primary health facility level in line with the Essential Package of Health Services (EPHS) (8).
• Integration/system approach. Synergies between health system strengthening and public health emergency efforts are sought, including enabling health services and multi-sectoral participation across all levels (national to sub-national) toward Universal Health Coverage (UHC) and health security as interdependent goals. The project bridged health systems and health security efforts during health sector planning, COVID-19 preparedness and response, After Action Reviews (AAR), and Simulation Exercise (SimEx) by promoting the participation of stakeholders from health services, animal health, and environmental health.
• Multi-sectorial engagement. The project fosters joint working among MoH, NPHIL, and other relevant sectors, such as the Ministry of Agriculture (MoA), Environmental Protection Agency (EPA), Ministry of Internal Affairs (MIA), Port Health Authorities, and academia, especially at the sub-national level.
• Partnership and sustainability. Collaboration with health sector partners is paramount. For example, collaboration with the USAID-funded STAIP (Strategic Technical Assistance for Improved Health System Performance and Health Outcomes) and BRIDGE-U (Bringing Research to Impact for Development, Global Engagement and Utilization) projects resulted in the implementation of county operational planning and completion of the national Guideline for Continuing Professional Development (CPD). In addition, partnership with Jhpiego (the John Hopkins Program for International Education in Gynecology and Obstetrics) and Last Mile Health (LMH) led to the development of the new National Health Quality Strategy.
Key stakeholders
The country-based project team comprises two dedicated project staff from the WHO country office and two project focal persons from MoH (health systems) and NPHIL (health security), jointly implementing the project with support from the WHO Headquarters and Regional Office team. The two dedicated project officers from WHO Liberia Country Office are qualified and experienced public health practitioners and quality improvement specialists. The national focal person from the MoH is an experienced physician and director of the Health Quality Management Unit, while that from NPHIL is the director of training for the institute. Table 3 lists key stakeholders working closely with the WHO project team and national focal points.
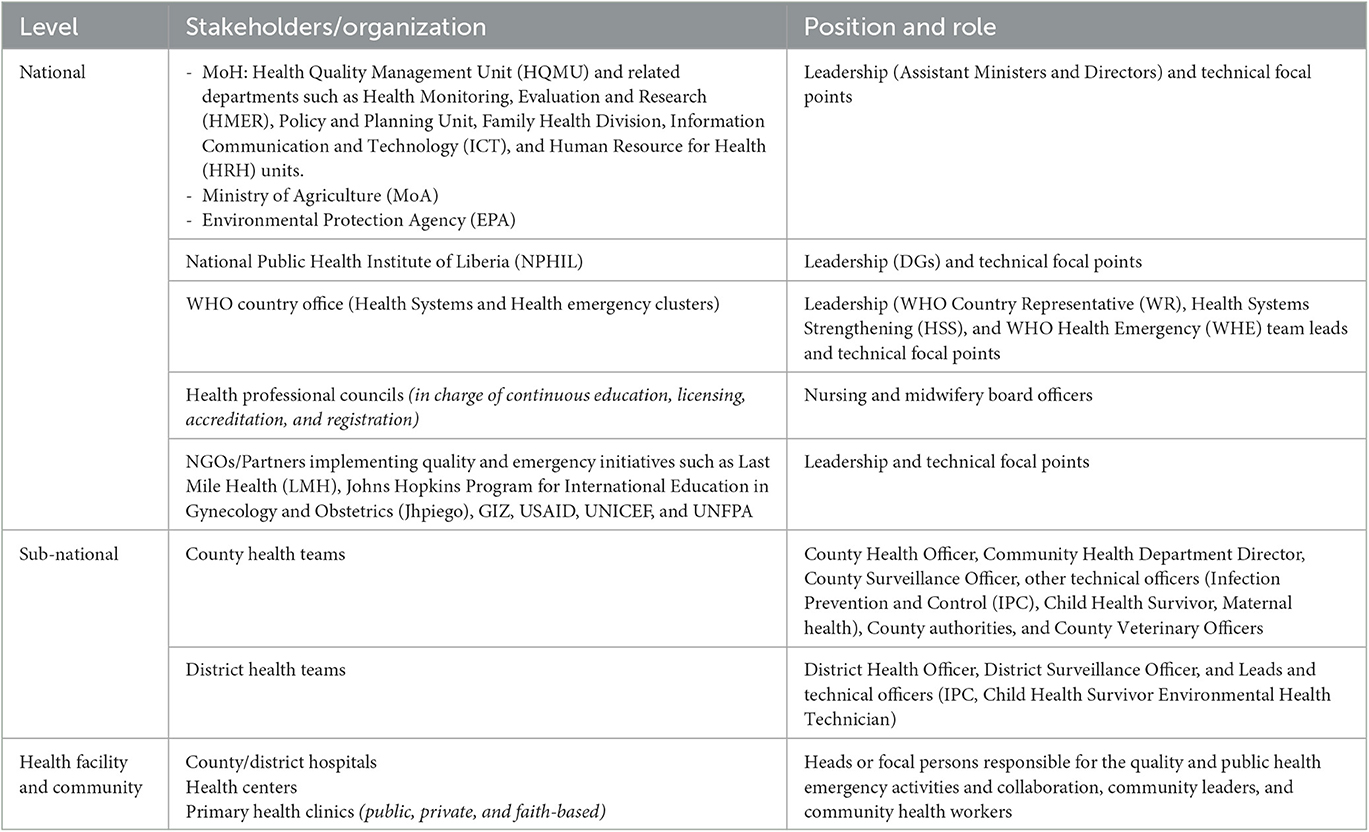
Table 3. Examples of key stakeholders working closely with the WHO project team to implement the project.
Sites and their selection
The selection of project sites was done through the catchment approach, which resulted in the selection of 19 health facilities (10 clinics, four health centers, and five hospitals) in three counties. Figure 1 below illustrates how this approach linked responsible entities in public health emergency management, health service delivery, and animal-environmental health across the 4 levels of the health system [national, county, district, and health facility—public and private—and community) within specified catchment areas. Implementation of the project was carried out in three counties—Bong, Lofa, and Grand Cape Mount, strategically selected in view of their geopolitical location, with significant internal and external borders (see map in Figure 2). Beyond the three pilot counties, the project activities have benefitted other counties prioritized by national authorities, for example, Montserrado, Nimba, and Gbarpolu.
Approach to developing and refining the project goals, tools, and activities
The project applied a mixed methods approach to assess the health system, develop project tools, implement project activities, and evaluate the level of progress. The methods included: (i) Literature review, (ii) Key Informant Interviews, and (iii) Project site assessment (county and facility visits) during the country situational assessment and project mid-term review.
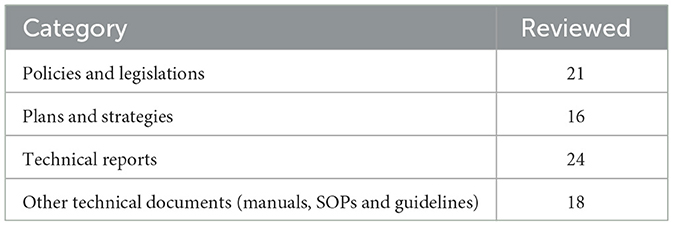
• The literature review was conducted to identify existing tools to support health system resilience, for example, dedicated health system SimEx tools. Medical and health research databases (PubMed and Embase) as well as Google Scholar were searched. Search terms (e.g., health emergency, quality of care, health system resilience, etc.) were combined using Boolean Operators (AND and OR), quotation marks, and spelling variants, as applicable (17). Gray literature was identified mainly through key stakeholders' recommendations. In total, 79 documents (from both the literature search and stakeholders' recommendations) met the inclusion criteria at initial screening; 60 of them were retained for review. From the latter, 11 were peer-reviewed articles (Google Scholar-5, PubMed-4; Embase-2) and the remaining 49 documents were gray literature. Table 4 summarizes the types of documents which were reviewed.
• Key informant interviews were conducted with national (10) and sub-national (5) stakeholders (Table 3), including leadership and technical officers from relevant units within MoH and NPHIL; Environmental Protection Agency (EPA); Ministry of Agriculture (Veterinary division); WHO Country Office; Health professional training institutions; Health professional boards; Health regulatory bodies; Partner organizations; county health teams; district health teams; health facility management teams; community leaders, and healthcare workers (clinicians and community health workers). In addition, a similar group of stakeholders was consulted during an inter-country engagement meeting held in Bishoftu, Ethiopia (April 2019), and an in-country consultative workshop in Gbarnga, Bong County Liberia, in September 2019.
The consultations resulted in the elaboration of the project work plan, selection of project pilot counties and facilities, validation of the SA findings, and approval of the project support package.
• Health facility and county assessments were carried out in 19 health facilities (10 clinics, five hospitals, and four health centers) in 10 health districts and 3 counties (Bong, Lofa, and Grand Cape Mount), as represented in Figure 2. Fifteen (79%) of the health facilities were public. The assessment was done using a structured questionnaire developed by the project team. The respondents included County and District Health Officers, medical directors and officers in charge, heads of units/programs, and community leaders.
Project support package and implementation
Based on the project plan and country SA, the project team developed an operational guide for project implementation (18). The operational guide offered practical guidance on the implementation of 10 interconnected components: training and mentoring of the health workforce; health services quality interventions; measuring health system resilience; risk registering and profiling; emergency management with service continuity planning and policies; advocacy; local resilience fora; simulation exercises (SimEx); after-action reviews (AAR); and knowledge sharing (Figure 3). Each of these areas served as an opportunity to integrate emergency management capacities in routine service delivery (at primary, secondary, and tertiary levels of care) and overall strengthening of all health system building blocks (18, 19).
Monitoring and evaluation
Routine monitoring and evaluation (M&E) of the project uses a framework of five expected outcomes, 15 outputs with specified activities, and the status of implementation.
The M&E mechanism for the project involves all stakeholders at both national and global levels. It includes monthly reports to the national and WHO country office leadership and technical teams; quarterly meetings to provide updates to the KOICA regional team and review progress and challenges encountered; and bi-annual teleconferences with the KOICA-GDEF team, during which WHO provides an update on activities implemented and next steps.
In addition, a project mid-term review (MTR) was conducted in Monrovia in September 2021 involving national and sub-national institutions and stakeholders (see Table 3), with support from the WHO team and participation of KOICA Nigeria country office and other partners (20). The MTR assessed the status of project implementation and identified challenges and opportunities for continuity and scale-up. Data were collected through (1) a field assessment tool exploring the implementation of activities in the 10 technical support areas of the project, including versions for national, county, district, and health facility levels, (2) an online survey administered before the MTR meeting to all participants invited to it (26 out of 36 invited participants completed it), and (3) three focus group discussions (FDGs) (three groups of 12 participants each). The survey and FDGs aimed at gathering a more nuanced and in-depth understanding of the contributions of the HSR project to enhancing collaboration, integration, and health service resilience. Data from the field assessment, online survey, and focus group discussion are reported in the Section Overall evaluation by stakeholders.
Project achievements and contributions to long-term recovery and building back better agenda in Liberia
The HSR project supported the MoH and NPHIL to strengthen Liberia's health system to deliver quality routine health services before, during, and after the COVID-19 pandemic. During the COVID-19 outbreak, project activities were re-aligned and adapted to meet the pandemic-driven priorities of the health system. The HSR project contributed to policymaking, strategic planning, surveillance, measurement of quality and resilience, human resource planning, and capacity building (in-service and pre-service) according to the 5 project outcomes.
Overall evaluation by stakeholders
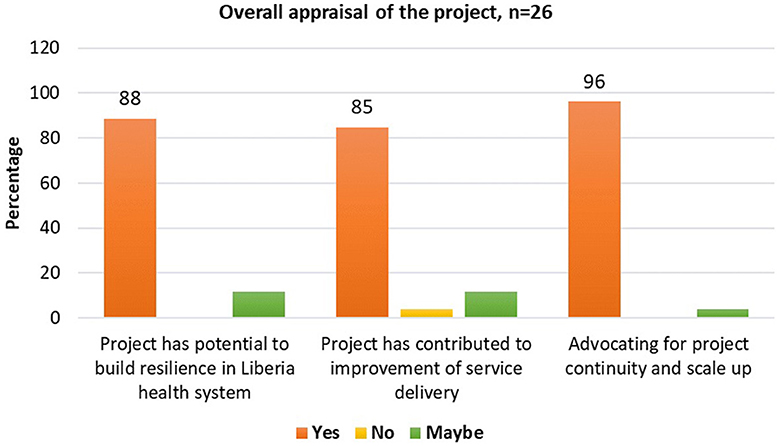
From stakeholders' consultations conducted as part of the project's mid-term review, most key stakeholders (n = 26 respondents) at national and sub-national levels agreed that the project has: (1) contributed to health service improvement (85%), (2) has the potential to strengthen resilience in the health system of Liberia (88%), and therefore (3) advocated for project continuity and scale-up (96%) (see Figure 4). The project approach was appreciated particularly for its uniqueness in promoting the integration of quality health services and emergency preparedness and response (85%), promoting inter-sectoral and multi-disciplinary collaboration (81%), and encouraging ownership and sustainability of Quality improvement interventions (QI) carried out (85%).
The quotes below are the feedback received from the administrator of Kolahun Hospital, Lofa County, and the IPC focal person for Grand Cape Mount County concerning their impression of the Integrated approach used by the KOICA-funded project during health sector operational planning in Lofa and Grand Cape Mount counties.
“This integrated approach of supervising clinicians with administrators, cleaners and security officers in hospitals is very unique and need to be encouraged. It gives us the opportunity to understand challenges in service delivery and how we can jointly find feasible solutions”.
Mr John Kawala, Administrator Kolahun District hospital, Lofa county
“This approach of jointly reviewing the health system and planning together with colleagues of the animal, agriculture and environmental sectors is the first of its kind. The discussions were very rich & comprehensive due to the diversity of the group and the application of the novel Health System SimEx tool developed by the KOICA project”.
Victoria Railey, IPC Focal Point, Grand Cape Mount county
“The project has ensured participation of various stakeholders. Activities are conducted through the MoH and NPHIL making the entities to assume ownership and for long-term sustainability”
Mr Garrison Kerwillain, IPC coordinator, MoH
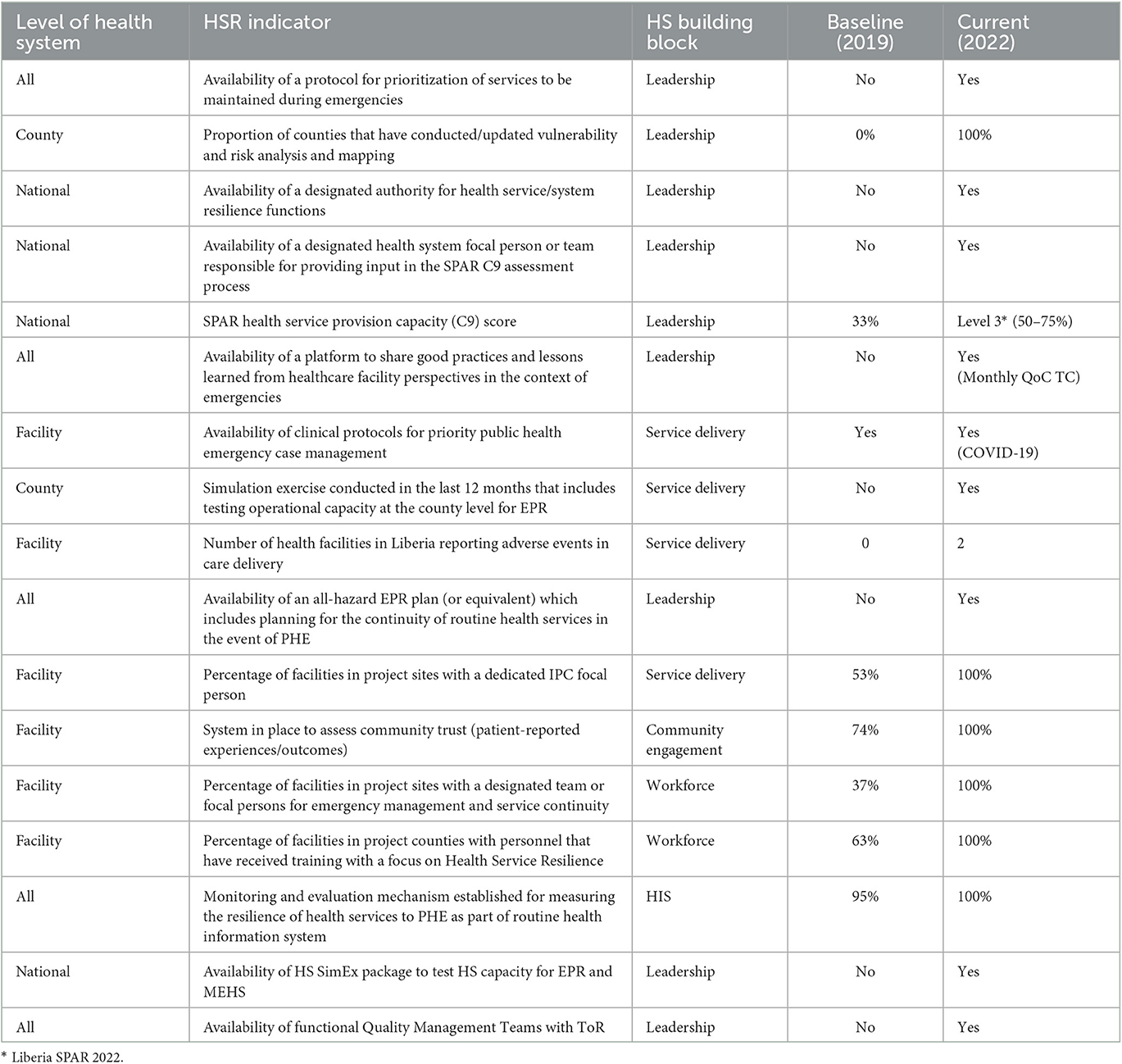
Improvements in key resilience indicators
Table 5 below summarizes progress made in key Health System Resilience indicators (developed by the HSR project) between 2019 (project start year) and December 2022, across the building blocks and levels of the health system. This progress also includes some of the weak areas identified during the Liberia SA on the state of quality and resilience. Overall, the project has contributed to the advancement of key resilience indicators in Liberia.
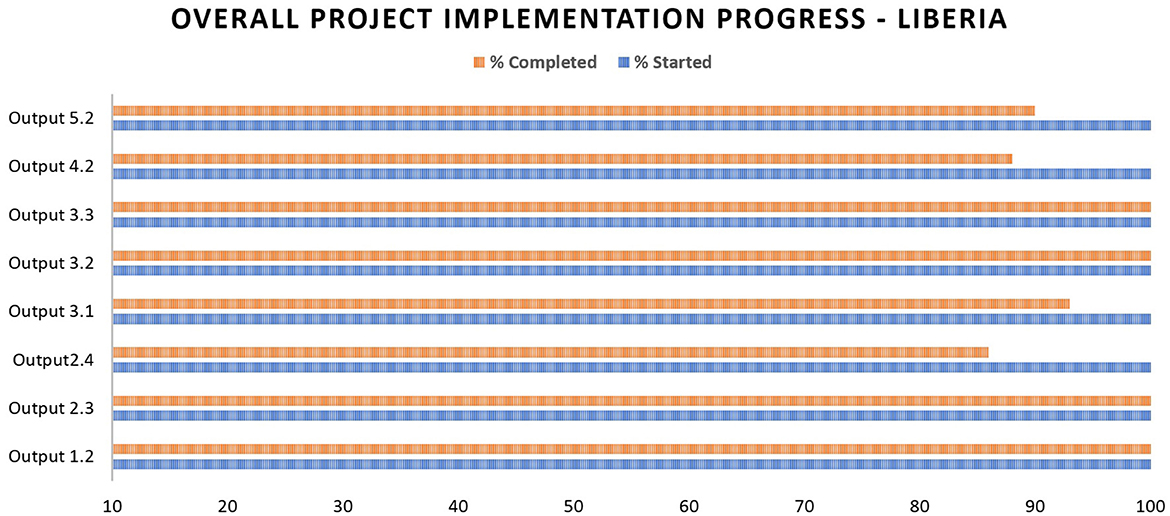
Progress in project implementation
As of December 2022, 95% of the project activities were estimated as completed (see Figure 5). The delay in achieving 100% completion has resulted from: delays in commencing implementation due to administrative and operational bottlenecks; disruptions and re-prioritization of project interventions due to the COVID-19 outbreak; and the longer than predicted time required to develop, adapt, and roll out the project support package at sub-national level. Despite the above delays, the project implementation would be completed within the set timeline of October 2023. Pending interventions are related to the roll out of key project tools such as the HSR training package and the Health System SimEx package.
Achievements relative to Liberia Investment Plan for Resilience
The project has also contributed to the implementation of the Liberia Investment Plan for Resilience, especially in building resilient capacities that enhanced preparedness, response, and recovery from the COVID-19 outbreak. For example, the project supported NPHIL and MoH to conduct a Vulnerability Risk Assessment and Mapping (VRAM) in 2021 (in line with the “awareness” feature of a resilient health system); implement a package of activities with a focus on primary healthcare (“diversity” feature of a resilient health system); enhance surge capacity by supporting integrated training for health workers to ensure rapid detection of outbreaks and minimize disruption of essential services (“self-regulation”); strengthen joint working between health systems and health security (“integration”) and develop tools for testing health system functionality (e.g., Health System SimEx); and planning for health service continuity during public health events (“transformation”).
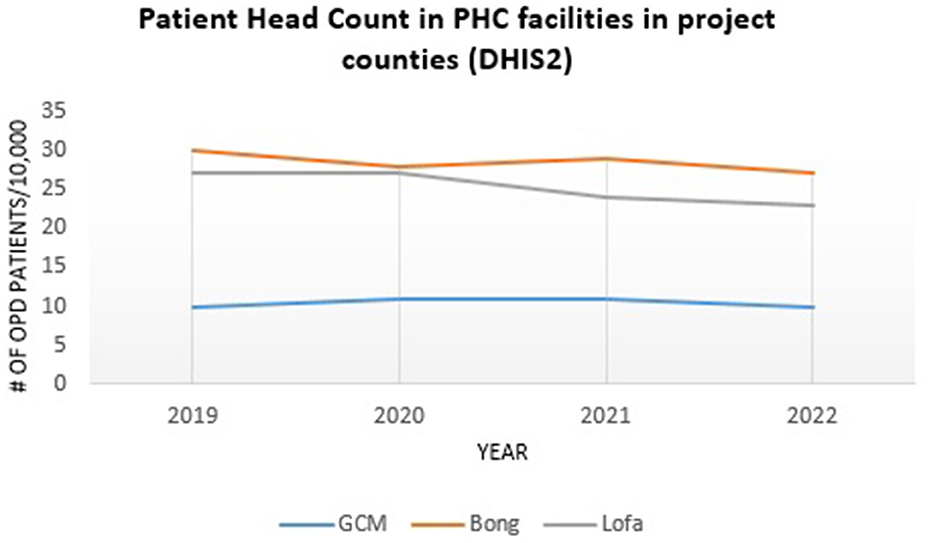
Further research is needed to explore the relative contribution of this project to resilience outcomes as opposed to processes and structures, but there are some indicative data in this respect. For example, outpatient consultations in public and private primary healthcare facilities increased from 3.4 million (2020) to 3.6 million (2021) across the country (16), with a similar trend observed in two of the project counties (Bong and Grand Cape Mount) as depicted in Figure 6.
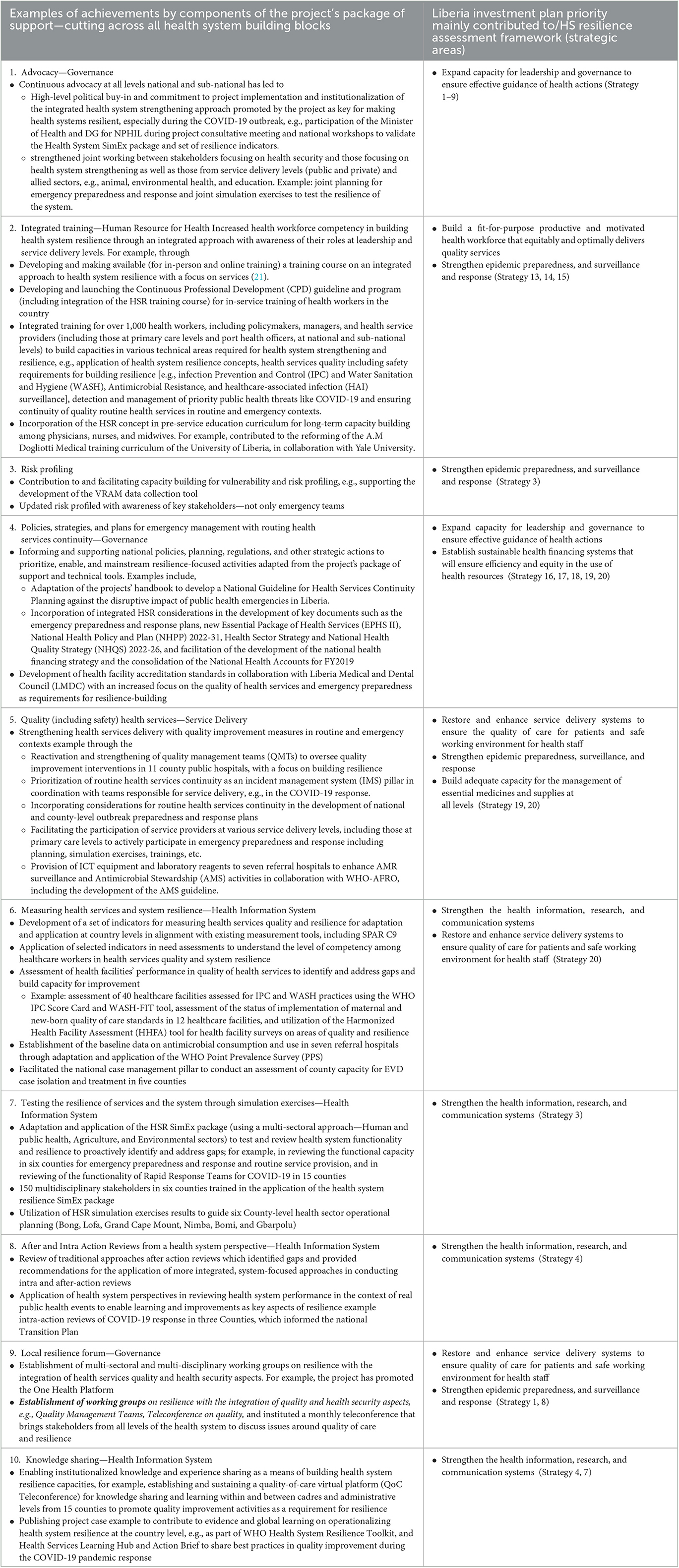
Table 6 summarizes the achievements of the project across the package of support components, the Liberia Investment Plan for Building a Resilient Health System, and the strategic areas for improving health system resilience during COVID-19 (22).
Achievements in mobilizing and supporting the health workforce
The project contributed to the mapping of technical competencies among healthcare workers. It also supported integrated training in COVID-19 prevention and control for over 1,000 health workers (clinicians, health system managers, surveillance officers, administrators, environmental and veterinary officers, and community health workers) in Bong, Lofa, and Grand Cape Mount counties. Key elements of this training addressed Water, Sanitation, and Hygiene (WASH), case management, and the application of maternal and newborn quality of care standards in the context of an infectious disease pandemic. These efforts contributed to zero COVID-19-related death and zero maternal mortality in Grand Cape Mount County between March 2020 and September 2021 (20).
The project has supported long-term improvement in workforce capacity by contributing to the establishment of an integrated learning platform on healthcare quality and a program for Continuing Professional Development (CPD).
Achievements in strengthening public health capacities
Having learned from the EVD outbreak and other emergencies, the project tailored emergency preparedness and response activities to also support and allow the continuity of essential health services during emergencies. For example, following advice from the project team and in coordination with responsible stakeholders, the monitoring and maintenance of essential routine health services were incorporated as a response priority of the COVID-19 Incident Management System. Adopting a catchment approach (such as during stakeholders' workshops) facilitated the cross-pollination of knowledge and skills across the human, animal, and environmental sectors. Involving health facilities at the various levels across the referral system (clinics, health centers, and hospitals), the strengthening of the roles of actors at each level (2), and the creation of interlinkages between and within the different levels and sectors strengthened resilient capacities at service delivery levels to create sustainable impact and foster efficiency.
The HSR project catalyzed Liberia's efforts of building back better from EVD, COVID-19, and beyond, by embedding public health capacities in health system functions based on lessons from past and current public health events. Examples include the prioritization of routine health services continuity and the inclusion of a new response pillar called Maintenance of Essential Health Services (MEHS) during the COVID-19 pandemic (23). This has supported the strengthening of routine health services during COVID-19 as well as the roll out of COVID-19 vaccination, integration of clinical care for COVID-19 patients into routine healthcare, and revision of the essential package of health services (EPHS II, 2022–2026) to include concepts of emergency response and healthcare quality improvement.
In addition, the concept of sustainability has been embodied in the implementation of the project by leveraging and supporting existing partners' efforts to strengthen the health system in Liberia. The project team also facilitated the development of the new National Health Quality Strategy (NHQS 2023–2027) and is supporting the Liberian Medical and Dental Council (LMDC) to draft quality standards for the assessment and accreditation of health facilities in Liberia. These documents will guide the provision of quality healthcare services in the post-COVID-19 era.
Project contributions to the COVID-19 response
The ability to quickly reallocate available funding to support the COVID-19 response was necessary to provide a swift response (24). At the peak of the pandemic, some project activities were revised to re-align with COVID-19 response activities, and project funding was rapidly repurposed to address these needs. Such activities included integrated training in COVID-19 prevention/IPC, detection, isolation, and case management (including home-based care and specific interventions for maternal, newborn, and child health services) in the three project counties. Funding from the project was also used to support surge capacity through the repurposing of project staff to support COVID-19 response in non-project counties.
Technical officers for the project were repurposed to support the COVID-19 response in Montserrado and Grand Kru counties. This support resulted in the development of specific county response plans for COVID and the successful containment of the outbreak. The HSR project personnel contributed to the adaptation, validation, and roll out of the interim guidelines for COVID-19 clinical care and the Handbook for COVID-19 Treatment, which facilitated the management of COVID-19 patients in Treatment Units and county referral hospitals. The project focal point also facilitated the development of the national guideline for home-based isolation and care for COVID-19 patients, which facilitated the treatment and recovery of over 2,000 patients during the response (25).
In addition, through the HSR project, WHO procured and donated laptop computers and printers to eight referral hospitals to improve data collection and reporting on AMR during the COVID-19 outbreak and beyond. The water supply at Tellewoyan Memorial Hospital (Lofa County) was rehabilitated through the procurement and installation of a submersible water pump under the HSR project. This enhanced the quality of care for COVID-19 case management and other patients in routine care for the population of Lofa and the neighboring communities in Guinea and Sierra Leone.
Project challenges and limitations
Early on, there was a 6-month delay in the onset of project implementation due to administrative and operational challenges such as delay in the recruitment of project staff and transfer of project funds to the country office. In addition, project implementation was disrupted by the COVID-19 pandemic response and restrictions, and competing priorities related to ongoing and potential outbreaks, including threats of EVD. However, the lost time was recovered by careful work planning, re-sequencing, and streamlining of activities in line with national and sub-national priorities while maintaining the project's ethos of fostering an integrated approach to health system strengthening for resilience even while adapting activities to support response to various emergencies.
A key limitation of the project was its relatively limited scope. The project was implemented in 19 public and private health facilities in three out of 15 counties in Liberia. However, there were spillovers of project activities in non-pilot counties, such as Montserrado, Nimba, Bomi, and Gbarpolu. Some activities were also implemented at a national level, benefitting stakeholders from MoH, NPHIL, MoA, EPA, National Disaster Management Agency (NDMA), and academia, and are likely to have had an impact on other activities involving the same stakeholders. Importantly, the health system challenges are similar in all 15 counties of Liberia, which will facilitate the transfer of lessons learned from the 3+ pilot counties across the health system.
Discussion and recommendations
To support Liberia in building resilience in its health system, WHO partnered with KOICA to work with the MoH, NPHIL, and other relevant institutions to implement a health system resilience initiative. The project, though catalytic in nature and limited in scope, made a significant contribution toward the realization of the national ambition of building a resilient health system, especially in the three project counties.
Below we highlight what we perceive as the greatest strengths and persistent challenges for the Health Service Resilience project as implemented in Liberia and, based on these, recommend priorities in working toward health systems resilience. Highlights of the achievements of the parallel project in Ethiopia are included in Box 2.
Box 2. Highlights of project implementation in Ethiopia.
This resilience building project model is also being successfully implemented in Ethiopia with positive feedback from stakeholders acknowledging its role in promoting and operationalizing the concept of resilience in the health system as important in the context of recovery from various public health events. This demonstrates the relevance, adaptability, and applicability of the project to different contexts.
Examples of achievements from project support in Ethiopia include establishment of an institutional focus on health system resilience in the Ethiopian Public Health Institute (EPHI) and institutionalizing resilience-focused activities from the project in national public health activities as planning, Public Health Emergency Management (PHEM) guidelines. Emergency response efforts such as the COVID-19 incident management structure incorporated essential health service continuity as a priority, with active participation of health system and services-focused teams for a comprehensive response and timely prevention and mitigation of routine health services disruptions. National universities in Ethiopia have also embedded the concept and application of health systems resilience in their pre-service and advanced degree programs for health professionals, based on the training package from this initiative for long-term impact in health workforce competencies. These are especially timely to further position and expand considerations for integrated health system strengthening and resilience in recovery efforts from COVID-19, conflict-related humanitarian response and other system strengthening initiatives building on the projects best practices and achievements.
Health systems strengthening for resilience needs an integrated approach and multi-partner, multi-sectoral collaboration
Fragmented and siloed approaches have often hampered efforts to make health systems more resilient (26), by prioritizing disease-specific objectives over health system strengthening and clinical care over public health and by not making the most of limited resources. The HSR project, in contrast, mainstreamed the joint working of key stakeholders across various disciplines and sectors at policy, planning, and operational, including service delivery, levels.
The project strengthened the integration of health systems and health security work. It ensured that each project-supported activity contributed to strengthening the capacity of the health system to equally prioritize and serve routine and emergency-related population health needs during and between small- and large-scale emergencies. High-level political buy-in and participation from the top leadership of the MoH and NPHIL was secured. This included the participation of the Minister of Health and Director General of NPHIL during the project stakeholders' consultative meeting in Gbarnga and during the launch of the project toolkit (as shown in Table 6).
The principle of integration also guided the development of national and county health sector and health security plans and policy documents, as well as technical resources developed or supported by the project. Key among these was the integrated Health Sector Operational Plans that included emergency preparedness activities, the integrated health system SimEx package (which was used to test the functionality of the Rapid Response Teams for COVID-19), COVID-19 Preparedness and Response Plans (23) (national and county), and the national guideline for health service continuity planning in emergency context (27) (further detail in Table 6). Health system reporting and programming documents, such as the State Party Self-Assessment Annual Reporting (SPAR) and the antimicrobial resistance (AMR) stewardship programming, were also developed using the integrated approach.
The project achieved significant successes in institutionalizing joint working within and between the health sector and other sectors, such as education, academia, administration, security, internal affairs, agriculture, animal and environmental health, and civil society. Among the most successful examples of such institutionalized joint working and multi-sectoral collaboration were the project activities on public health emergency preparedness; the promotion of the One-Health platform to improve coordination with the animal and environmental sectors; and the national workshop to review and adapt the Health System SimEx package and set of indicators for resilience (Tables 5, 6). The collaboration between the private and public sectors was also strengthened, with the critical role of the private sector becoming evident during the COVID-19 pandemic.
Last, but not least, as far as integration and collaboration are concerned, the project achieved a high level of partner engagement, benefiting from the technical knowledge and skills of partners and driving the agenda for sustainability. As shown in Table 6, the project team has collaborated with Last Mile Health to develop the NHQS2023-27, USAID-STAIP project to conduct integrated training for healthcare workers and conduct health sector operational planning at the county level and the USAID-funded BRIDGE-U project to develop and launch the CPD guideline.
Liberia's successes in improving integration and multi-partner, multi-sectoral collaboration for resilience offer a broad range of steps for other countries to choose from. Within the country, there is a need to further institutionalize integrated health system resilience efforts, including linkages with funding streams and accountability mechanisms (28). The Ministry of Health and NPHIL need to work together to steer available and potential internal and external health investments to promote and operationalize an integrated approach to health system strengthening toward resilience, even when targeting specific health problems such as emergencies, specific diseases, or life-course issues. This would build the capacity of the system to effectively address the various health issues faced by populations served with better efficiency and sustainability.
Health system resilience requires continuous learning and capacity building
The project's package of support (18) remains relevant and timely before, during, and between public health emergencies, thereby allowing continuous learning and improvement even as the health system goes from one public health event to the next. This continuous learning is core to the concept of recovery and long-term resilience building (2) promoted by the project. It contributes to making the health system more adaptive as illustrated by Falope et al. (29). Building on lessons from EVD, COVID-19, and other smaller events, the project established the multi-sector/multi-disciplinary learning platform for regular experience sharing on healthcare quality and resilience between health workers, managers, policymakers, community stakeholders, and partners (Table 6, rows 2 and 10). It also developed and launched the first national guideline for CPD, in collaboration with the University of Liberia and health professional boards (Table 6). Enhancing the competencies of medical directors, CHOs, and other managers and decision-makers through project activities has also enabled a trickle-down effect on frontline health professionals and non-health actors (at both national and sub-national levels) and has enhanced the application of systems thinking for resilience at frontline levels.
Despite the frequent use of the term “health systems resilience”, the understanding of the concept of integrating resilience building in routine health emergency and system functions and service delivery, particularly at sub-national levels and service delivery levels, is generally still growing (30). There is a need to cover more health professionals (especially from the frontline) in training and orientation on the required integrated approach to the concept of resilience, e.g., through more pre-service curricula reviews and CPD programs beyond the current project sites.
Health system resilience requires the promotion of ownership and sustainability
The project has been intentional and systematic in creating a sense of ownership among national stakeholders and in enabling long-term sustainability. As described under Guiding principles, it used a “One-plan One-budget approach” from planning through implementation. Its overall work plan was jointly elaborated by national stakeholders from the MoH, NPHIL, EPA, and MoA during an inception meeting held in Bishoftu Ethiopia, and a stakeholders' consultation meeting in Gbarnga, Bong County in Liberia in 2019. Budgets for the implementation of activities were jointly reviewed and updated with the national counterparts, particularly the two project focal points, and approved by the Minister of Health or Director General of NPHIL before each activity was implemented. In addition, the planning and coordination of some key activities have been handed over to the national teams. For example, the Healthcare Quality Management Unit (HQMU) of the MoH leads the coordination of monthly teleconferences on quality of care (29) (Table 6).
Health system resilience efforts must be further decentralized (28) and owned by key actors within the system, especially at the sub-national levels with a focus on strengthening primary healthcare (22, 28, 31).
Health system resilience requires new investment mechanisms to promote research and innovation
The “panic and neglect” cycle has been a major challenge in building resilience in health systems sustainably, using the recovery phase as a platform for applying learning and improving the quality of health services (6). Most donor funding disappears when the acute phase of an emergency is over. Foundational health issues remain unaddressed and under-prioritized. After the EVD response in Liberia, the country experienced a decline in external support to take forward the lessons from the outbreak. Among the current partners working on aspects of quality and preparedness with national authorities in Liberia, there are very limited resources and support available for promoting and scaling-up an integrated health system strengthening with health security in tandem, in the context of the decline in external support and economic contraction. This is further compounded by the global economic impacts of the COVID-19 pandemic and geo-political crisis.
The occurrence of public health events (PHE) such as the COVID-19 pandemic and the threat of the Ebola outbreak, while disruptive, provide increased momentum to work toward resilience, learning, and strengthening of the health system. The HSR project is an example of a health system initiative implemented from lessons learned from previous PHE, has piloted a series of technical tools to build health system resilience, one of which is the set of resilience indicators (Tables 5, 6). However, there is an increasing need to test this package of tools on a large scale, but also to prioritize the development of robust assessment tools and monitoring and evaluation systems through research.
National and sub-national stakeholders have been calling for the extension and scale-up for the wider impact of Liberia's Health Services Resilience project. The project team and their collaborators are continuing to advocate for the expansion of the project within and beyond the three pilot counties and focused investments beyond the current project scope and the COVID-19 pandemic. One of the major investment priorities identified is addressing the fragmentation in health information systems and enabling integrated and interoperable tracking of quality and resilience indicators at both national and operational levels.
Challenges
Even though the project applies a system approach, there are fundamental health system challenges that have remained outside of its scope, for example, the availability of basic infrastructure for water, sanitation, and hygiene, the procurement of medical supplies, or the retention of health workers. At the same time, the lack of such infrastructure affects both the implementation of the project and the preservation of its legacy. The project's advocacy and technical support for system-wide strengthening can be enhanced by pulling together wider health sector inputs and resources and by broadening partnerships in this area of work. The project team continues to scope out relevant options for collaboration with other partners in supporting the national authorities. Sector-wide and inter-sectoral planning and linking the plans with funding are also essential.
Study strengths and limitations
Strengths
This study presented ongoing, practical work on the operationalization of resilience in a health system of a resource-limited setting, a genre of studies that continues to be seriously under-represented in the academic literature. The operationalization of the concept of resilience in the health system has been limited partly by the limited progress made in developing standardized metrics (32), but also by the multitude of frameworks that have been proposed (30). The pre-existing evidence synthesized here was generated through a mixed methods approach, including a literature review (quantitative and qualitative findings), online survey and focus group discussions (primarily qualitative findings), and health facility assessments (observations, giving rise to both quantitative and qualitative findings). This was complemented by considerations and learnings arising from the study authors' direct involvement in the project. The evidence and learnings presented here are thus rich and multifaceted and have sufficient rigor and credibility, even if also limited in important ways (see below). The lessons shared in this paper can be applied to enhance resilience in similar health systems recovering from COVID-19 and seeking to build back a better health system, which continuously improves how it serves the needs of local populations and its capacity to withstand future pandemics.
Limitations
A substantial part of the data summarized in this study has been collected from key informants, selected for their roles in the health system and by applying the catchment approach. This makes such data amenable to many biases, including sampling, recall, social desirability, and overall reporting bias. This was, to a degree, offset by data triangulation using other methods, including literature reviews and observations in health facilities. Overall, a breadth of evidence was synthesized. However, this was not done by applying a sufficiently structured and transparent research synthesis method. The prioritization of findings and lessons learned was made based on the co-authors' expertise as opposed to using a systematic approach to data extraction and synthesis. Finally, the public health intervention the study describes is still in its implementation phase. Follow-up studies are needed to explore the degree to which the reported achievements and impact are lasting and sustainable.
Conclusion
The Health Service Resilience project as implemented in Liberia has demonstrated that it is possible to operationalize health system resilience in a low-income country and under resource constraints. It has also shown that the priorities of health security and universal health coverage can be advanced in tandem at policy, management, and service delivery levels. This has been achieved by ensuring national ownership and leveraging existing strengths and opportunities such as strong political will at national and sub-national levels and the existence of NPHIL and the Quality Management Unit of the MoH, which are products of the EVD experience.
The project was mainly implemented in three out of 15 countries of Liberia, and the nature of the support has been catalytic as opposed to transformative. However, the HSR project has made a valuable contribution to national efforts for building a resilient health system inspired by the EVD experience. These achievements from the project implementation supported the national preparedness and response efforts for COVID-19 that led to the successful containment of the COVID-19 outbreak in Liberia and are contributing to the gradual restoration of essential health services in the post-COVID-19 era. The project has generated a lot of momentum and enthusiasm among the beneficiary institutions and populations, especially with its integrated, catchment, and multi-sectoral approach.
The principles applied in this pilot and the best practices shared could guide the operationalization of resilience efforts in health systems in other resource-limited settings similar to Liberia.
Author contributions
LA-E drafted manuscript (including method), conducted desk review and stakeholders' consultations, completed editing, referencing, and submission. RS drafted outline for the manuscript, contributed to the desk review (MEF), and reviewed and refined manuscript. SS reviewed and updated manuscript. SW reviewed manuscript to reflect the context. MB contributed to desk review and stakeholders' consultation. BN supported stakeholders' consultation, especially in the identification and engagement of key stakeholders from MoH. RG supported stakeholders' consultation, especially stakeholders from the National Public Health Institute. CO and CP proofread and update the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank Mila Petrova (World Health Organization, Geneva, Switzerland), Kayode S. Adebisi (KOICA Country Office, Nigeria), Son Sungil (KOICA Country Office, Nigeria), Woochan Chang (KOICA Country Office, Nigeria), and Gorbee G. Logan (Ministry of Health, Liberia).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1137865/full#supplementary-material
References
1. Brolin Ribacke KJ, Saulnier DD, Eriksson A, von Schreeb J. Effects of the West Africa Ebola virus disease on health-care utilization–a systematic review. Front Public Health. (2016) 4:222. doi: 10.3389/fpubh.2016.00222
2. Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons from Ebola. Lancet. (2015) 385:1910–2. doi: 10.1016/S0140-6736(15)60755-3
3. Ministry Ministry of Health Government Government of Liberia. Investment Plan for Building a Resilient Health System (2015-2021). Monrovia: Ministry of Health, Government of Liberia (2015).
4. Liberia Liberia Institute of Statistics and Geo-Information Services (LISGIS) Ministry Ministry of Health (MoH) The The DHS Program (ICF). Liberia Demographic Health Survey 2019-20. Monrovia (2021).
5. Healthy New Born Network. Available online at: https://www.healthynewbornnetwork.org/news-item/liberia-newborn-mortality-rate-up-at-1072-per-100k-lives/ (accessed May 03, 2023).
6. Building Health Systems Resilience for Universal Health Coverage and Health Security During the COVID-19 Pandemic and Beyond: WHO Position Paper. Geneva: World Health Organization (WHO/UHL/PHCSP/2021.01) (2021). Available online at: https://www.who.int/publications/i/item/WHO-UHL-PHC-SP-2021.01 (accessed April 22, 2023).
7. World Health Organization/KOICA-Funded Project: Making Health Service Resilient with Quality and Preparedness for Emergency Response: Liberia Situational Assessment Report. Monrovia (2019).
8. Liberia Essential Package of Health Services for Universal Health Coverage (UHC). Monrovia: Ministry of Health (2022).
10. National Health Sector Strategic Plan: A Roadmap to Universal Health Coverage 2022–2026. Monrovia: Ministry of Health (2022).
13. Ministry of Health. Liberia National Health Quality Strategy (Draft) 2023-2027. Monrovia (2023).
14. Lin JS, Murad MH, Leas B, Treadwell JR, Chou R, Ivlev I, et al. A narrative review and proposed framework for using health system data with systematic reviews to support decision-making. J Gen Intern Med. (2020) 35 (6):1830–5. doi: 10.1007/s11606-020-05783-5
15. Liberia Health Service Resilience Project Monitoring and Evaluation Framework. Monrovia: World Health Organization (2018).
17. An Roinn Sainte. How to Conduct a Literature Search? Internal Staff Guide. Hawkin House Dublin (2013).
18. World Health Organization/KOICA-Funded Project: Making Health Service Resilient With Quality and Preparedness for Emergency Response: Operational Framework and Technical Guide. Monrovia (2019).
19. Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: World Health Organization (2007).
20. World Health Organization/KOICA-Funded Project: Making Health Service Resilient With Quality and Preparedness for Emergency Response. Mid-Term Review Workshop Report. Monrovia (2021).
21. WHO Training Course. An Integrated Approach for Building Health System Resilience. Available online at: https://openwho.org/courses/health-service-resilience (accessed April 22, 2023).
22. Sagan A, Webb E, Azzopardi-Muscat N, de la Mata I, McKee M, Figueras J. Health Systems Resilience during COVID-19: Lessons for building back better. Health Policy Series 56. United Kingdom: World Health Organization (2021).
24. Health Systems Resilience Toolkit: A WHO Global Public Health Good to Support Building and Strengthening of Sustainable Health Systems Resilience in Countries With Various Contexts. Geneva: World Health Organization (2022). Available online at: https://www.who.int/publications/i/item/9789240048751 (accessed April 17, 2023).
26. Fostering Resilience Through Integrated Health System Strengthening: Technical Meeting Report. Geneva: World Health Organization (2021) (Fostering resilience through integrated health system strengthening series).
27. Health Service Continuity Planning for Public Health Emergencies: A Handbook for Health Facilities. Interim Version for Field-Testing. Geneva: World Health Organization (2021). Available online at: https://www.who.int/publications/i/item/9789240033337 (accessed April 17, 2023).
28. Balde T, Oyugi B, Byakika-Tusiime J, Ogundiran O, Kayita J, Banza FM, et al. Transitioning the COVID-19 response in the WHO African region: a proposed framework for rethinking and rebuilding health systems. BMJ Glob Health. (2022) 7:e010242. doi: 10.1136/bmjgh-2022-010242
29. Falope O, Nyaku MK, O'Rourke C, Hermany LV, Plavchak B, Mauskopf J, et al. Resilience learning from the COVID-19 pandemic and its relevance for routine immunization programs. Expert Rev Vaccines. (2022) 21:1621–36. doi: 10.1080/14760584.2022.2116007
30. Foroughi Z, Ebrahimi P, Aryankhesal A, Maleki M, Yazdani S. Toward a theory-led meta-framework for implementing health system resilience analysis studies: a systematic review and critical interpretive synthesis. BMC Public Health. (2022) 22:287. doi: 10.1186/s12889-022-12496-3
31. Hort K, Gilbert K, Basnayaka P, Annear PL. Strategies to Strengthen Referral From Primary Care to Secondary Care in Low- and Middle-Income Countries. New Delhi: World Health Organization Regional Office for South-East Asia (2019).
32. Fleming P, O'Donoghue C, Almirall-Sanchez A, Mockler D, Keegan C, Cylus J, et al. Metrics and indicators used to assess health system resilience in response to shocks to health systems in high income countries-A systematic review. Health Policy. (2022) 126:1195–205. doi: 10.1016/j.healthpol.2022.10.001
Keywords: health systems, resilience, integration, catchment approach, emergency preparedness and response, healthcare quality, recovery, COVID-19
Citation: Ako-Egbe L, Seifeldin R, Saikat S, Wesseh SC, Bolongei MB, Ngormbu BJ, George R, Ocan C and Peter Lasuba CL (2023) Liberia health system's journey to long-term recovery and resilience post-Ebola: a case study of an exemplary multi-year collaboration. Front. Public Health 11:1137865. doi: 10.3389/fpubh.2023.1137865
Received: 04 February 2023; Accepted: 22 May 2023;
Published: 19 June 2023.
Edited by:
Aladeen Alloubani, King Hussein Cancer Center, JordanReviewed by:
Janneth Mghamba, Commonwealth Secretariat, United KingdomKaren Sliter, International Atomic Energy Agency, Austria
Copyright © 2023 Ako-Egbe, Seifeldin, Saikat, Wesseh, Bolongei, Ngormbu, George, Ocan and Peter Lasuba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Louis Ako-Egbe, bG91aXNha29lZ2JlMDJAZ21haWwuY29t; Redda Seifeldin, c2VpZmVsZGluckB3aG8uaW50
 Louis Ako-Egbe
Louis Ako-Egbe Redda Seifeldin
Redda Seifeldin Sohel Saikat
Sohel Saikat Sanford C. Wesseh3
Sanford C. Wesseh3 Ballah Jusu Ngormbu
Ballah Jusu Ngormbu Clement Lugala Peter Lasuba
Clement Lugala Peter Lasuba