- 1Department of Cardiology, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
- 2Department of Geriatrics, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
- 3The Key Laboratory of Geriatrics, Beijing Institute of Geriatrics, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing Hospital/National Center of Gerontology of National Health Commission, Beijing, China
- 4Health Service Department of the Guard Bureau of the Joint Staff Department, Beijing, China
- 5China Research Center on Ageing, Beijing, China
- 6Institute of Psychology, Chinese Academy of Sciences, Beijing, China
Objective: There are few studies on the prevalence and factors associated with frailty and pre-frailty in older adults with asthma worldwide. The aim of this study was to examine the epidemiological status and factors associated with frailty and pre-frailty in older adults with asthma in China.
Research design and methods: Data were obtained from the Sample Survey of Aged Population in Urban and Rural China in 2015, a nationwide cross-sectional survey covering 224,142 older people aged 60 years or older in 31 provinces/autonomous regions/municipalities in mainland China. We performed frailty and pre-frailty assessments using the frailty index, and the diagnosis of asthma in the older adults was self-reported based on the history of the physician's diagnosis.
Results: Nine thousand four hundred sixteen older adults with asthma were included in the study. The age-sex standardized prevalence of frailty and pre-frailty in Chinese older adults with asthma was 35.8% (95% CI 34.8%−36.7%) and 54.5% (95% CI 53.5%−55.5%). Multinomial logistic regression analysis showed that increased age, female, illiteracy, living alone, poor economic status, ADL disability, comorbid chronic diseases, previous hospitalization in the past year, and residence in northern China were associated with frailty and pre-frailty in older adults with asthma.
Conclusion: The prevalence of frailty and pre-frailty in Chinese older adults with asthma is very high, and assessment of frailty should become routine in the management of older adults with asthma. Appropriate public health prevention strategies based on identified risk factors for frailty in older adults with asthma should be developed to reduce the burden of frailty in Chinese older adults with asthma.
Introduction
Asthma is a common non-communicable lung disease, with an aging population, the number of older people suffering from asthma is increasing. Epidemiological data show that the prevalence of asthma in people aged 65 years or over is 4%−15% (1–3). The 2017 global burden of disease study revealed asthma to be the second most prevalent chronic respiratory disease after chronic obstructive respiratory disease and the second leading cause of death from chronic respiratory disease (4). Asthma poses a serious threat to the quality of life and health of older people, and increases the use and burden of healthcare resources on society (5). Frailty is a clinical syndrome characterized by reduced physiological reserve and multisystem dysregulation, which limits the body's ability to respond to internal and external stresses and maintain the stability of the internal environment, increasing the body's susceptibility to stressful events (6–8). The weighted prevalence of frailty in older people in the community is 11% (range 4%−59%) (9). Frail older people are at significantly increased risk of falls, delirium, incapacity, hospitalization and death, and increase the burden on society's healthcare resources (8, 10, 11). There are few large-scale studies in the world on frailty in older adults with asthma. The paucity of research on frailty in older patients with asthma has led to many challenges in the comprehensive management of asthma in older adults. On top of the existing medical care for older adults with asthma, frailty assessment can provide additional valuable information and help clinicians choose better medical care for their patients. This study applied data from the 2015 Sample Survey of Aged Population in Urban and Rural China (SSAPUR) to analyse the prevalence of frailty and pre-frailty and their associated factors in older adults with asthma in China. The aim was to provide information to reduce the decline in cognitive and physical functioning and to prevent frailty and disability in older people with asthma.
Methods
Study design and participants
Data were obtained from the 4th SSAPUR, a cross-sectional study of 224,142 older adults aged 60 years or older in 31 provinces, autonomous regions, and municipalities in mainland China in 2015. The survey used a stratified, multi-stage, proportional probability sampling by size and equal probability sampling design in the final stage. The sampling proportion was ~1 in 1,000 of the national older population in 2015, and the sample obtained was self-weighted to ensure national representativeness. The sample number was assigned based on the proportion of the older population in each province, autonomous regions, and municipalities of the country, after that the number of counties, towns and communities sampled was determined and 462 counties were selected. Based on PPS sampling, four towns were selected from each county and four communities (villages or neighborhood councils) were selected from each town. Finally, 30 older adults were selected from each community using equidistant sampling. Data on the living conditions of older adults were collected through household interviews and questionnaires. More information on the design and sampling methods of the 4th SSAPUR study has been reported in previous studies (12–14). We used the frailty index (FI) for frailty and pre-frailty assessment, and 15,756 (7.0%) older adults were excluded because the number of constructed FI items was <28. Of the 208,386 older adults, 9,416 older adults with asthma, determined on the basis of a self-reported history of diagnosis by a physician, were included in our study (Figure 1). The study protocol was approved by the National Bureau of Statistics (No. [2014] 87) and the Ethics Committee of Beijing Hospital (2021BJYYEC-294-01). Written informed consent was provided by all participants.
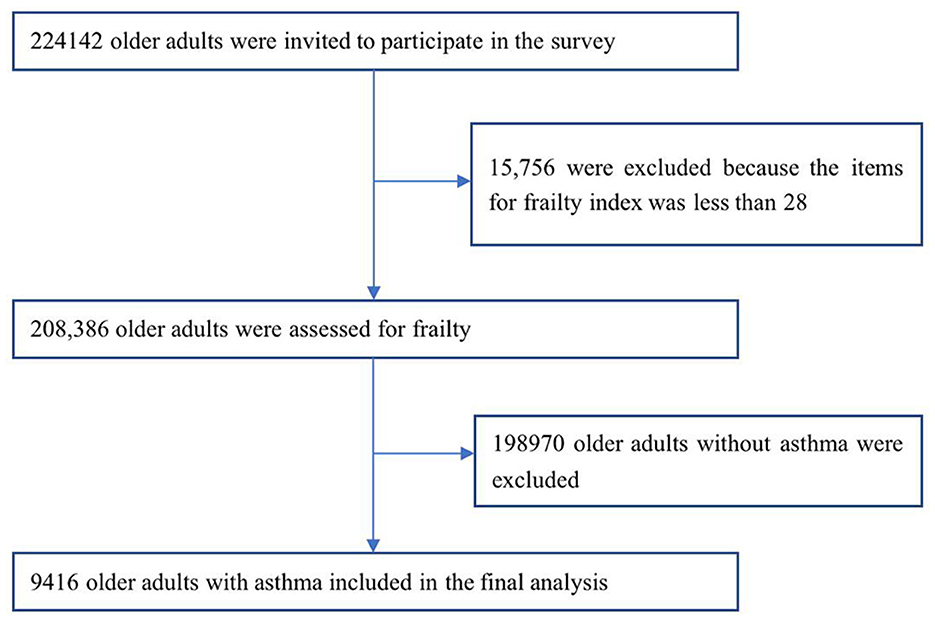
Figure 1. Flowchart of study participants on frailty and pre-frailty prevalence in older adults with asthma in China.
Demographics
Demographic characteristics: age, sex, education, marital status, ethnicity, residence, living status, health checkup within the past year, hospitalization within the past year, financial status, ease of medical reimbursement, activities of daily living (ADL) disability (Inability to do one or more of the following: bathing, dressing, toileting, getting in and out of bed, eating and moving around the room is considered a disability), comorbid chronic diseases, and residence in southern or northern China.
Identification and assignment of health deficit variables for FI
FI refers to the proportion of deficits that are present when a person undergoes a health assessment. We constructed FI following Searle's standard procedure (15). The FI items (n = 33, each subject needs at least 28/33 variables) were selected from the baseline questionnaires of demographic characteristics, physical health, physical functioning, lifestyle, social activity, and mental health status. The variables included eight items of basic activities of daily living (bathing, dressing, toileting, getting in and out of bed, eating, walking around the room, urinary incontinence, and fecal incontinence); 10 items focusing on chronic diseases included glaucoma/cataract, cardiovascular disease, hypertension, diabetes, gastric disease, bone and joint disease, chronic lung disease, asthma, malignancy, and reproductive system disease; two items focused on feelings of loneliness and happiness; three items focused on geriatric syndrome, including visual impairment, hearing impairment, and history of falls; five items focused on assistive devices (hearing aids, dentures, crutches, wheel-chairs, and adult diapers/nursing pads); three items focused on mobility (needing care from others in daily life, self-rated health status, and exercise); two items focused on social activity (regular leisure activities and regular public service activities). The FI was calculated by summing the number of deficits recorded for a patient and dividing this by the total number of possible deficits. The exact construction method has been described in our previous study (12). FI scores ≥0.25 are considered frailty, <0.12 are considered robust, and FI 0.12–0.25 are considered pre-frailty.
Statistical analysis
We used SPSS 24.0 software for statistical analysis. Missing data were interpolated using the Markov chain Monte Carlo (MCMC) multiple fill method (15). The age-standardized prevalence of frailty and pre-frailty among Chinese older adults with asthma was calculated based on the weights established in our study. For continuous variables, we assessed the significance of differences by ANOVA or Student's t-test, and for categorical variables, we passed the χ2 test. Trends in prevalence of covariates were examined by using the Cochran-Armitage test. Multinomial regression analysis was used to identify factors associated with frailty and pre-frailty, including age group, gender, ethnicity, urban/rural, education level, marital status, living alone, economic status, health insurance, ease of medical reimbursement, comorbid chronic diseases, ADL disability, and residence in southern or northern China, with p < 0.05 being statistically significant.
Results
From August 1, 2015 to August 31, 2015, 224,142 older adults aged 60 years or older were invited to participate in the fourth SSAPUR, of which 15,756 participants were excluded because fewer than 28 items were used to construct the FI. Nine thousand four hundred sixteen older adults with self-reported asthma out of 208,386, and the self-reported prevalence of asthma among older adults was 4.5%, with 4.8% prevalence in men and 4.3% prevalence in women. Demographics and frailty risk factors by frailty stage in older adults with asthma are shown in Table 1, demographics and frailty risk factors for older asthmatics by North and South are shown in Supplemental Table S1.
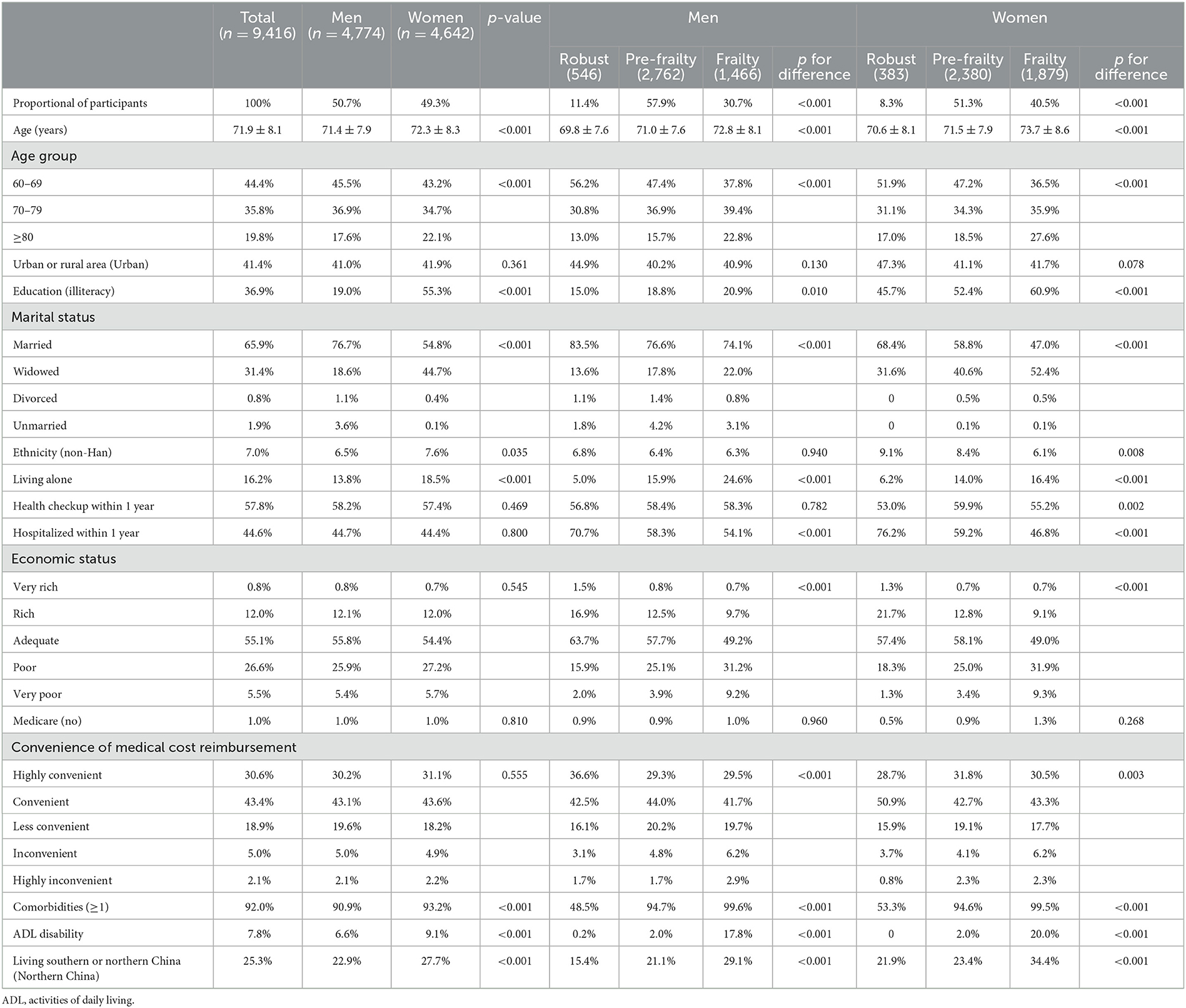
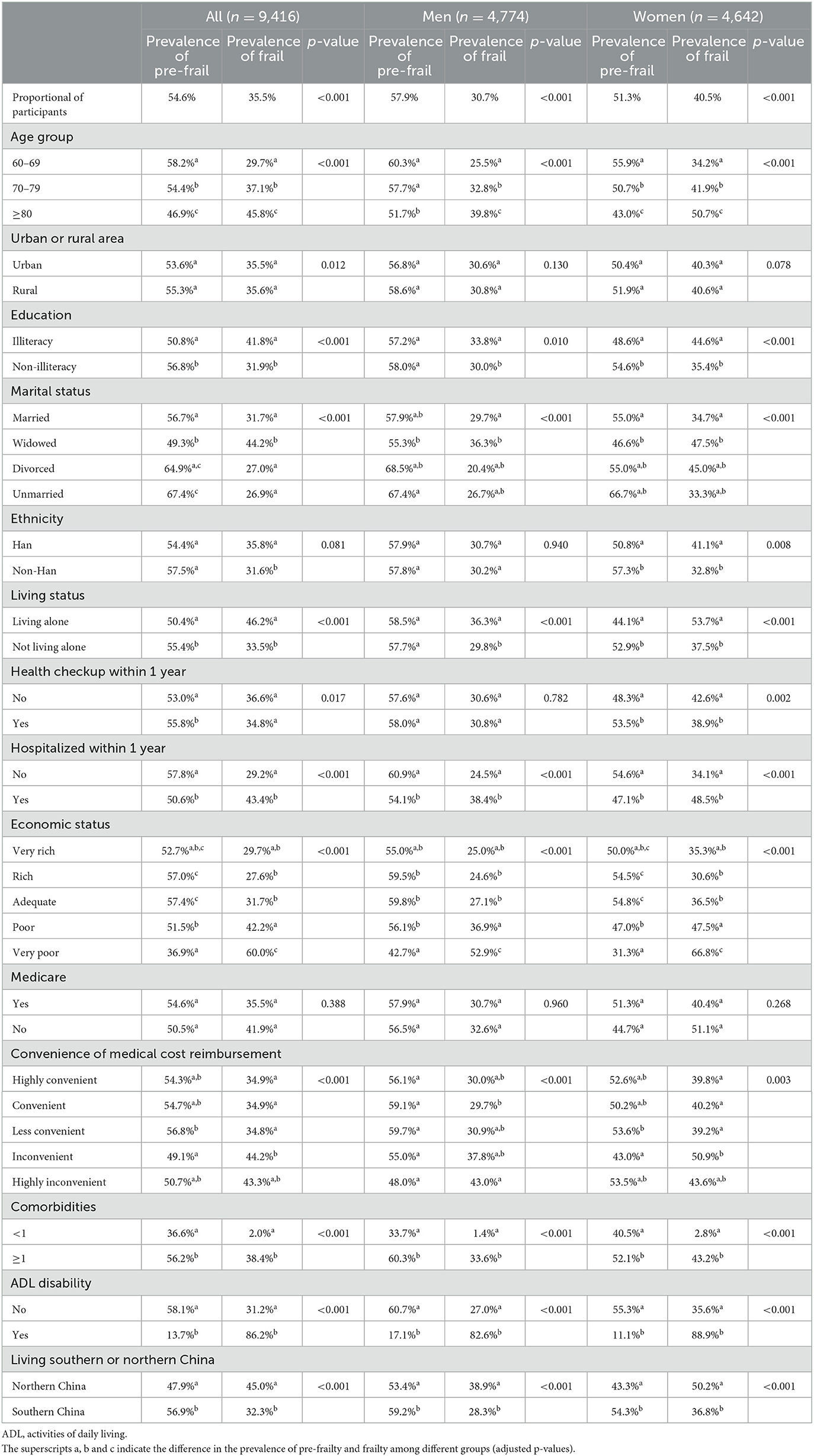
Table 1. Demographics of the Chinese adults aged 60 years or older with asthma in 2015, and related factors for frailty, by frailty stage.
The FI of older adults with asthma was gamma distributed with a statistical value of 0.075, p < 0.0001. The FI of older adults with asthma was 0.21 (0.11; ranging from 0.04–0.70), with 0.23 (0.12) for female asthmatics, which was higher than that of male asthmatics 0.20 (0.11; z = −11.686, p < 0.001).
The prevalence of frailty and pre-frailty in older adults with asthma was 35.5% and 54.6%, respectively, significantly higher than the prevalence of frailty (8.2%) and pre-frailty (46.4%) in older adults without asthma, both p < 0.0001. The prevalence of frailty was higher in female older adults with asthma (40.5%) than in males (30.7%), while the prevalence of pre-frailty was lower in female older adults with asthma (51.3%) than in males (57.9%), both p < 0.001. The age-sex standardized prevalence of frailty and pre-frailty among Chinese older adults with asthma was 35.8% (95% CI 34.8%−36.7%) and 54.5% (95% CI 53.5%−55.5%). The age-sex standardized prevalence of frailty and pre-frailty was 40.9% (95% CI 39.5%−42.3%) and 51.4% (95% CI 49.9%−52.8%) for women, and 30.8% (95% CI 29.5%−32.1%) and 57.5% (95% CI 56.1%−58.9%) for men.
The prevalence of frailty in older adults with asthma increased with age, from 29.7% in the 60–69 years age group to 45.8% in the ≥80 years age group. There was no difference in the prevalence of frailty between rural and urban older adults with asthma. The prevalence of frailty was higher in Han Chinese older adults with asthma than in non-Han Chinese, mainly in Han Chinese women than in non-Han Chinese women. Frailty was mostly seen in older adults with asthma who were illiterate, widowed, living alone, had been hospitalized in the past 1 year, had financial difficulties, had difficulties in reimbursing medical expenses, and had comorbid chronic diseases and disabilities. The prevalence of frailty was higher among older adults with asthma in northern China than in southern China (Table 2). The prevalence of frailty among older adults with asthma in the seven administrative regions of mainland China was highest in northwest China, followed by north China, then northeast China, and then southwest, central, southeast, and south China (Figure 2).
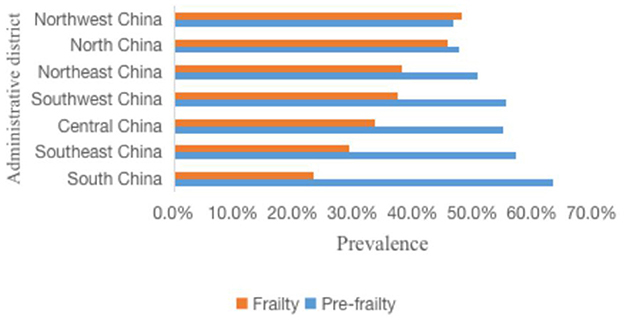
Figure 2. Prevalence of frailty and pre-frailty in older adults with asthma in different administrative regions.
Multinomial regression analysis revealed that female, increased age, illiteracy, living alone, hospitalization in the past 1 year, difficult financial situation, comorbid chronic diseases, ADL disability, and north of residence were risk factors for frailty and pre-frailty in older adults with asthma (Table 3).
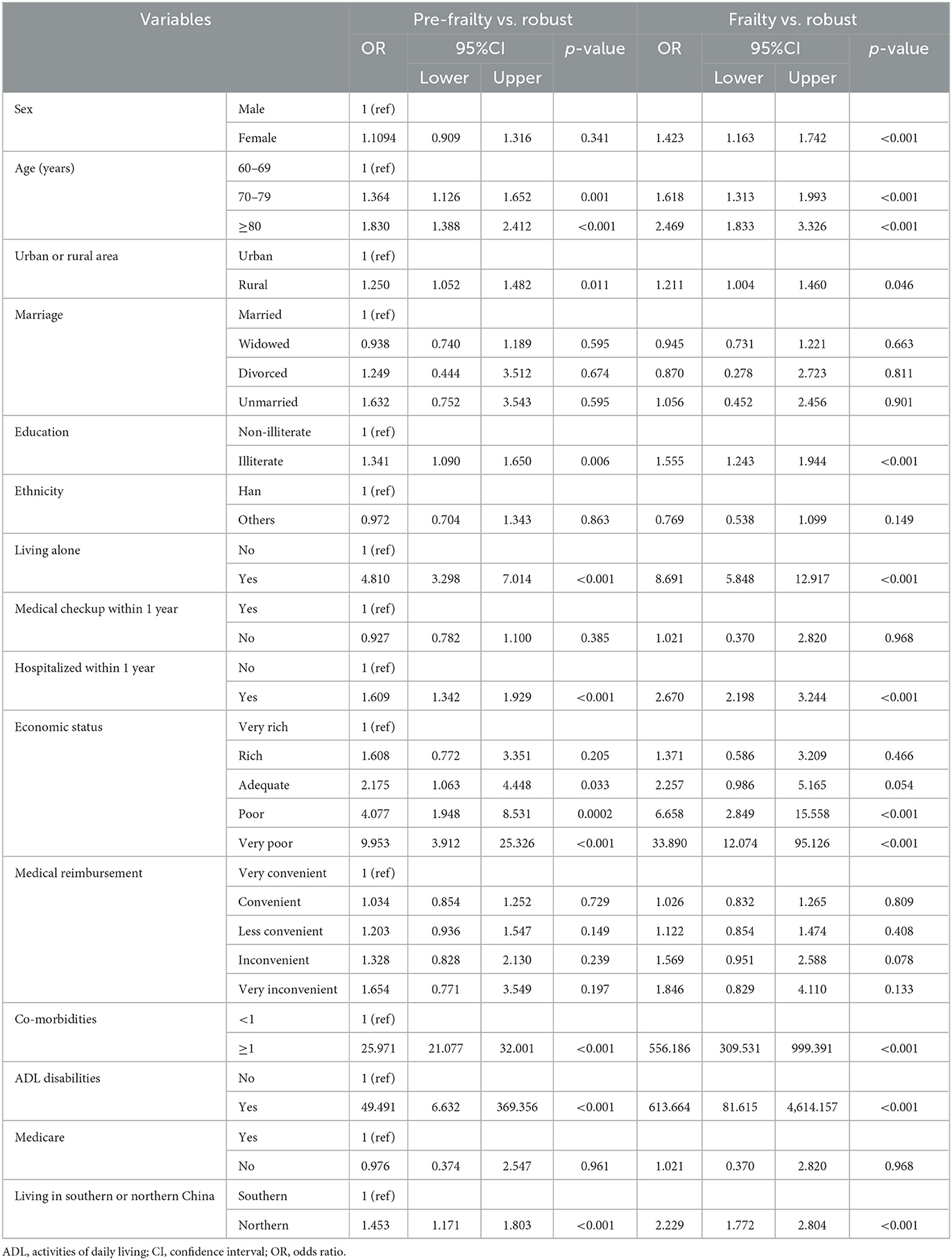
Table 3. Factors associated with frailty and pre-frailty of older adults with asthma by multinomial logistic regression.
Discussion
Asthma has long been recognized as a disease that is prevalent in adolescents. Our study showed a self-reported asthma prevalence of 4.5% in older adults, indicating that the prevalence of asthma in older adults is not low. Data from the 2010–2012 China Epidemiological Survey of Asthma Prevalence and Risk Factors study showed that the prevalence of asthma increased with age, with 2.26% of people aged 61–70 years and 3.10% of people aged ≥71 years (2), and data from the China Adult Lung Health Study from 2012 to 2015 showed that the prevalence of asthma was 6.0% in people aged 60–69 years and 7.4% in people aged ≥70 years (3). The above study showed that asthma prevalence was not low among older adults in China. Foreign epidemiological data showed that the prevalence of asthma in people aged 65 years or over was 4%−15% (1, 16). Asthma surveillance data released by the Centers for Disease Control and Prevention show that the prevalence of asthma among older adults ≥65 years of age in the United States was 8.1% in 2010 (1). The 2017 Global Burden of Disease Study shows that the prevalence of asthma has decreased since 1990, from 3.9% in 1990 to 3.6% in 2017, but it remains the second most prevalent chronic respiratory disease after chronic obstructive respiratory disease, and asthma is also the second leading cause of death from chronic respiratory disease (4).
The rate of severe asthma and mortality in older adults with asthma is higher than in other age groups. The risk of severe and frequent acute exacerbations, resulting in frequent hospitalizations or emergency room visits, significantly increases the direct medical costs of older adults with asthma (5). Prevention and early management of asthma, a common non-communicable disease in older adults, is also one of the key goals for achieving healthy aging, and studies of frailty as an assessment indicator of biological aging have shown a significant increase in negative clinical events in frail older adults (10); therefore, studying the frailty status and risk factors of older asthmatics can help inform public health policymakers to reduce cognitive and physical decline and prevent frailty and disability in older asthmatics.
Our large cross-sectional national study used a stratified, multi-stage, size-proportional probability sampling and a final-stage equal-probability sampling design with a sample covering 31 provinces, municipalities, and autonomous regions in mainland China with different geographic regions and economic development status, and the age distribution, gender, and urban-rural ratios of older adults in the obtained sample were consistent with the demographic characteristics of older adults in the 2015 China Population Survey, ensuring national representativeness. Our study accurately reports the prevalence of frailty and pre-frailty in older Chinese patients with asthma. Our study found a high age-sex standardized prevalence of frailty in older adults with asthma of 35.8% (95% CI 34.8%−36.7%) and an age-sex standardized prevalence of pre-frailty of 54.5% (95% CI 53.5%−55.5%), with a 3.3-fold increase in the prevalence of frailty in older adults with asthma compared to older adults without asthma. The results of our study are generally consistent with those of a small study who found a 37% prevalence of frailty among 203 older outpatients with asthma aged 60 years or older (17), and we report a higher prevalence of frailty among older adults with asthma than a Brazilian cohort study that reported 13% of older patients with current asthma had frailty in 2015 (18). Chronic inflammation in asthmatics is not only present in the respiratory tract but is systemic, characterized by increased levels of peripheral blood eosinophils, immunoglobulin E and type 2 cytokines. Recent studies have found that chronic systemic inflammation is associated with the development of frailty and that chronic systemic inflammation in older adults with asthma may be an important cause of frailty (19–21). Our study showed that the proportion of older asthmatics who never exercised was significantly higher than that of older adults without asthma, and that the reduction in exercise also resulted in older asthmatics being more likely to develop sarcopenia, one of the key factors in the development of frailty syndromes. Until the recent advent of biologic agents, oral corticosteroids (OCS) have been the key controller medication for the treatment of severe intractable asthma. Ryu et al. reported a higher prevalence of frailty in older adults with asthma with longer lifetime OCS exposure (33% of patients with no lifetime OCS use, 59% of low-dose users, and 68% of high-dose users; p < 0.005 for trend). Suggesting that lifetime cumulative OCS exposure was associated with a high prevalence of weakness and muscle weakness (17). Although OCS is effective for asthma, it causes side effects including osteoporosis, fractures, diabetes, obesity, cardiovascular disease, and infections that may promote the onset of frailty. These aforementioned factors may promote the development of frailty in older adults with asthma.
Our study found that being female, increasing age, illiteracy, living alone, hospitalization in the past 1 year, economic hardship, comorbid chronic diseases, ADL disability, and living in northern China were risk factors for frailty and pre-frailty in older asthmatic patients. Studies have shown that aging is an independent risk factor for the onset of frailty, as older adults age, several physiological systems throughout the body undergo degenerative changes, the reserve function of various organs decreases, and the risk of frailty increases (7, 22). Decreased estrogen levels in older women lead to a decrease in muscle strength and a negative impact on neuromuscular function and postural stability, leading to an increased incidence of frailty in older women (23). Educational attainment is highly correlated with income, and difficult economic status makes it difficult to obtain adequate medical care, which increases the risk of frailty (24, 25). Older asthmatics who are living alone are more likely to experience loneliness and depression due to decreased family support, leading to an increased risk of frailty (26). Older adults with asthma have multiple co-morbidities and these chronic diseases contribute to the increased risk of frailty in older adults with asthma (27). Therefore, in the management of older adults with asthma, attention should be paid to identifying risk factors for frailty and providing early targeted interventions to reduce or delay the risk of frailty in older adults with asthma.
Compared with male older adults with asthma, our study found that female older adults with asthma were older, had higher rates in the advanced age group, higher rates of illiteracy, widowhood, living alone, comorbid chronic diseases, disability, and hospitalization in the past 1 year, which are factors associated with higher prevalence of frailty and pre-frailty in female older adults with asthma than in men, and the findings of our study provide information for policy makers to take appropriate measures to reduce and prevent the occurrence of frailty in female asthmatics.
Our study also found that the prevalence of frailty was higher among older adults with asthma living in the north than in the south. We found higher rates of female, widowed, no physical examination in the past 1 year, difficult financial status, inconvenient medical reimbursement, comorbid chronic diseases and ADL disability among older adults with asthma in northern China than in southern China. Differences in the demographic characteristics of older adults with asthma and risk factors for frailty in northern and southern China may explain the higher prevalence of frailty among older adults with asthma in the north than in the south. These findings provide information for policy makers to take appropriate measures to reduce and prevent the occurrence of frailty in asthmatic patients in northern China.
Limitations: firstly, the self-reported diagnostic information of asthma in this study may be subject to recall bias, secondly, there is a lack of information on the course and extent of disease in older adults with asthma, and at least two phenotypes exist in older adults with asthma; long-term asthmatics have more severe airflow limitation and are less fully reversible than asthmatics with late onset asthma. Third, smoking is an important risk factor for chronic airway disease, and this study did not assess the association between smoking and frailty in older adults with asthma. Fourth, this study was a cross-sectional study and could not determine the causal relationship between associated factors and frailty in older adults with asthma.
In conclusion, the prevalence of frailty and pre-frailty in older adults with asthma is very high, and frailty assessment should become a routine in the management of older adults with asthma, and attention should be paid to the early identification of risk factors for frailty in older adults with asthma and targeted interventions to prevent and delay the onset of frailty in older adults with asthma.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the National Bureau of Statistics (No. [2014] 87) and the Ethics Committee of Beijing Hospital (2021BJYYEC-294-01). The patients/participants provided their written informed consent to participate in this study.
Author contributions
X-zZ and NJ wrote the various drafts of the manuscript. X-zZ, L-bM, and JS conducted the statistical analyses. CZ, Y-yL, J-bH, HL, XQ, HW, XH, D-sW, and J-yL participated in data interpretation. D-pL, Q-xZ, JL, and X-zZ conceived and designed this study. X-zZ, NJ, L-bM, CZ, Y-yL, J-bH, JS, HL, XQ, HW, XH, D-sW, J-yL, Q-xZ, JL, and D-pL were revised the drafts of the manuscript for important scientific content. D-pL was the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors gave final approval of the version to be published.
Funding
The present study was funded by the National Key R&D Program of China (grant nos. 2020YFC2003000 and 2020YFC2003001). The study sponsors were not involved in the design of the study, the collection, analysis, and interpretation of data, writing the report, or the decision to submit the report for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1136135/full#supplementary-material
References
1. Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001-2010. Vital Health Stat 3. (2012) 35:1–58.
2. Lin J, Wang W, Chen P, Zhou X, Wan H, Yin K, et al. Prevalence and risk factors of asthma in mainland China: the CARE study. Respir Med. (2018) 137:48–54. doi: 10.1016/j.rmed.2018.02.010
3. Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. (2019) 394:407–18. doi: 10.1016/S0140-6736(19)31147-X
4. Collaborators GBDCRD. Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. (2020) 8:585–96. doi: 10.1016/S2213-2600(20)30105-3
5. Skloot GS, Busse PJ, Braman SS, Kovacs EJ, Dixon AE, Vaz Fragoso CA, et al. An Official American Thoracic Society Workshop Report: evaluation and management of asthma in the elderly. Ann Am Thorac Soc. (2016) 13:2064–77. doi: 10.1513/AnnalsATS.201608-658ST
6. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–56. doi: 10.1093/gerona/56.3.M146
7. Rockwood K, Howlett SE. Age-related deficit accumulation and the diseases of ageing. Mech Ageing Dev. (2019) 180:107–16. doi: 10.1016/j.mad.2019.04.005
8. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
9. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. (2012) 60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x
10. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6
11. Jin HY, Liu X, Xue QL, Chen S, Wu C. The association between frailty and healthcare expenditure among Chinese older adults. J Am Med Dir Assoc. (2020) 21:780–5. doi: 10.1016/j.jamda.2020.03.008
12. Zeng X, Jia N, Meng L, Shi J, Li Y, Hu X, et al. A study on the prevalence and related factors of frailty and pre-frailty in the older population with diabetes in China: a national cross-sectional study. Front Public Health. (2022) 10:996190. doi: 10.3389/fpubh.2022.996190
13. Dang JW, WY, Liu NN. Survey Report on the Living Conditions of China's Urban and Rural Older Persons. Beijing: Social Science Academic Press (2018).
14. Meng L, Xu J, Li J, Hu J, Xu H, Wu D, et al. Self-reported prevalence and potential factors influencing cardio-cerebral vascular disease among the Chinese elderly: a national cross-sectional study. Front Cardiovasc Med. (2022) 9:979015. doi: 10.3389/fcvm.2022.979015
15. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. (2008) 8:24. doi: 10.1186/1471-2318-8-24
16. McHugh MK, Symanski E, Pompeii LA, Delclos GL. Prevalence of asthma among adult females and males in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2001-2004. J Asthma. (2009) 46:759–66. doi: 10.3109/02770900903067895
17. Ryu K, Fukutomi Y, Nakatani E, Iwata M, Nagayama K, Yano K, et al. Frailty and muscle weakness in elderly patients with asthma and their association with cumulative lifetime oral corticosteroid exposure. Allergol Int. (2022). doi: 10.1016/j.alit.2022.10.005
18. Landre B, Nadif R, Goldberg M, Gourmelen J, Zins M, Ankri J, et al. Asthma is associated with frailty among community-dwelling adults: the GAZEL cohort. BMJ Open Respir Res. (2020) 7:e000526. doi: 10.1136/bmjresp-2019-000526
19. Wu IC, Lin CC, Hsiung CA. Emerging roles of frailty and inflammaging in risk assessment of age-related chronic diseases in older adults: the intersection between aging biology and personalized medicine. Biomedicine. (2015) 5:1. doi: 10.7603/s40681-015-0001-1
20. Respiratory Respiratory Allergy Group of Chinese Society of A Asthma Asthma Group of Chinese Thoracic Society CMA. [Chinese guidelines for the diagnosis and treatment of allergic asthma (2019, the first edition)]. Zhonghua Nei Ke Za Zhi. (2019) 58:636–55. doi: 10.3760/cma.j.issn.0578-1426.2019.09.004
21. Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, et al. Asthma in the elderly: current understanding and future research needs–a report of a National Institute on Aging (NIA) workshop. J Allergy Clin Immunol. (2011) 128:S4–24. doi: 10.1016/j.jaci.2011.06.048
22. Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K. Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol. (2017) 27:347–53. doi: 10.1016/j.je.2016.09.008
23. Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. (2017) 89:30–40. doi: 10.1016/j.exger.2016.12.021
24. Li Y, Xue QL, Odden MC, Chen X, Wu C. Linking early life risk factors to frailty in old age: evidence from the China Health and Retirement Longitudinal Study. Age Ageing. (2020) 49:208–17. doi: 10.1093/ageing/afz160
25. Dugravot A, Fayosse A, Dumurgier J, Bouillon K, Rayana TB, Schnitzler A, et al. Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study. Lancet Public Health. (2020) 5:e42–50. doi: 10.1016/S2468-2667(19)30226-9
26. Ge L, Yap CW, Heng BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. (2022) 22:26. doi: 10.1186/s12877-021-02745-2
27. Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. (2018) 3:e323–32. doi: 10.1016/S2468-2667(18)30091-4
Keywords: asthma, China, frailty, older adults, pre-frailty, prevalence
Citation: Zeng X-z, Meng L-b, Jia N, Shi J, Zhang C, Li Y-y, Hu X, Hu J-b, Li J-y, Wu D-s, Li H, Qi X, Wang H, Zhang Q-x, Li J and Liu D-p (2023) Epidemiological status and associated factors of frailty and pre-frailty in older adults with asthma in China: A national cross-sectional study. Front. Public Health 11:1136135. doi: 10.3389/fpubh.2023.1136135
Received: 02 January 2023; Accepted: 10 February 2023;
Published: 03 March 2023.
Edited by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranReviewed by:
Jose Francisco Parodi, Universidad de San Martín de Porres, PeruIda Ghaemmaghamfarahani, Columbia University Irving Medical Center, United States
Copyright © 2023 Zeng, Meng, Jia, Shi, Zhang, Li, Hu, Hu, Li, Wu, Li, Qi, Wang, Zhang, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: De-ping Liu, bGxpdWRlcGluZ0AyNjMubmV0
 Xue-zhai Zeng
Xue-zhai Zeng Ling-bing Meng
Ling-bing Meng Na Jia
Na Jia Jing Shi
Jing Shi Chi Zhang
Chi Zhang Ying-ying Li
Ying-ying Li Xing Hu
Xing Hu Jia-bin Hu4
Jia-bin Hu4 Jian-yi Li
Jian-yi Li Hui Li
Hui Li Xin Qi
Xin Qi Hua Wang
Hua Wang Juan Li
Juan Li De-ping Liu
De-ping Liu