
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 28 March 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1132798
 Noha Fadl1*†
Noha Fadl1*† Salah T. Al Awaidy2,3
Salah T. Al Awaidy2,3 Abdelhamid Elshabrawy4†
Abdelhamid Elshabrawy4† Mona Sayed Aly Hassan Makhlouf5†
Mona Sayed Aly Hassan Makhlouf5† Sarah Assem Ibrahim4†
Sarah Assem Ibrahim4† Suzan Abdel-Rahman4†
Suzan Abdel-Rahman4† Nazir Ahmad Tookhy6†
Nazir Ahmad Tookhy6† Abdullah Alsalmani7†
Abdullah Alsalmani7† Mays Al-Saeedi8†
Mays Al-Saeedi8† Ibrahim Al-Sawalha9†
Ibrahim Al-Sawalha9† Mohammad Amin Aly El-Din10†
Mohammad Amin Aly El-Din10† Janet Saad11†
Janet Saad11† Zainab Ayoob12†
Zainab Ayoob12† Mohamed Khalil Rourou13†
Mohamed Khalil Rourou13† Manahil Ali14†
Manahil Ali14† Salha M. Tawati15†
Salha M. Tawati15† Yahia Marwan Ahmed Gadain16
Yahia Marwan Ahmed Gadain16 Sara Yunis Al-saidi17†
Sara Yunis Al-saidi17† Ghadeer Ali Hassan18
Ghadeer Ali Hassan18 Mariam Alsanafi19†
Mariam Alsanafi19† Leen Sandouk20†
Leen Sandouk20† Naglaa Youssef21†
Naglaa Youssef21† Shaykhah Alothman22
Shaykhah Alothman22 Saja Yazbek23†
Saja Yazbek23† Khlood Saleh Al-Ansi24†
Khlood Saleh Al-Ansi24† Slimane Mehdad25†
Slimane Mehdad25† Mohammed Fathelrahman Adam26†
Mohammed Fathelrahman Adam26† Assem Gebreal27†
Assem Gebreal27† Ramy Mohamed Ghazy28†
Ramy Mohamed Ghazy28†Background: Seasonal influenza vaccine can reduce the risk of influenza-associated hospitalizations and deaths among children. Given that parents are the primary decision makers, this study examined the parental attitude toward childhood influenza vaccine and identified determinants of vaccine hesitancy (VH) in the Eastern Mediterranean region (EMR).
Methods: A cross-sectional study was conducted using an anonymous online survey in 14 EMR countries. Parents of children aged 6 months to 18 years were included. The Parent Attitude about Childhood Vaccines (PACV) was used to assess VH. Chi square test and independent t-test were used to test for association of qualitative and quantitative variables, respectively. A structural equations model (SEM) was used to identify direct and indirect determinants of parental VH.
Results: Almost half of the parents were hesitant about vaccinating their children against influenza (50.8%). Parental VH was significantly higher among older mothers (37.06 ± 8.8 years, p = 0.006), rural residents (53.6%, p < 0.001), high-income countries residents (50.6%, p < 0.001), and mothers with higher educational levels (52.1%, p < 0.001). Parents of school-aged children (5–9 years) (55.6%, p < 0.001), children free from any comorbidities (52.5%, p < 0.001), children who did not receive routine vaccination at all (51.5%, p = 0.03), children who were not vaccinated against COVID-19 (54.3%, p < 0.001), in addition to parents who were not vaccinated against influenza (57.1%, p < 0.001) were significantly associated with increased likelihood of VH. Parents who were depending on healthcare provider as a source of information regarding vaccines were less likely to report VH (47.9%, p < 0.001), meanwhile those who used social media as their source of health information showed a significantly higher VH (57.2%, p < 0.001). The SEM suggested that mother’s age, residence, country income level, child gender, total number of children and source of information regarding vaccines had a direct effect on VH. Meanwhile, parents vaccinated against influenza, children completely or partially vaccinated with routine vaccines and children vaccinated against Coronavirus disease 2019 (COVID-19) had an indirect effect on VH.
Conclusion: A high proportion of included parents were hesitant to vaccinate their children against seasonal influenza. This attitude is due to many modifiable and non-modifiable factors that can be targeted to improve vaccination coverage.
Seasonal influenza is an acute respiratory illness caused by influenza viruses. Seasonal influenza viruses come in four different types: A, B, C, and D. The influenza A and B viruses result in yearly epidemics. Pandemics have only been reported to be caused by influenza type A viruses. The influenza C virus is less often seen, it typically causes minor illnesses. Influenza D viruses are known to mainly infect cattle; they are not known to infect humans (1). According to the World Health Organization (WHO), the influenza epidemics result in between 290,000 and 650,000 reported global mortality, 3–5 million severe cases with secondary complications annually, which are most prevalent among the elderly, patients with comorbidities, infants and toddlers (2). The Eastern Mediterranean Region (EMR) is a home to 22 countries and is a major area for the spread of influenza, with winter (December to March) being the period when the virus is at its most active state. However, some countries like Qatar and Oman have a two-peak pattern every year that resembles the tropics (3).
Seasonal influenza vaccination is the most effective intervention to reduce the incidence of influenza and mitigate disease severity. The Centers for Disease Control and Prevention (CDC) recommends annual influenza vaccination for all children older than 6 months and who do not have contraindications (4). Unfortunately, the share of seasonal influenza vaccination in the EMR is approximately 2.2% of the globally distributed doses (5).
Although seasonal influenza infection is linked to severe morbidity and mortality, especially in young children, seasonal influenza vaccination is one of the vaccines that is associated with many debates among parents (6). Due to declining vaccination rates and the rise of anti-vaccination campaigns, the world is currently dealing with a number of outbreaks of infectious diseases that represent a threat to children’s health and can be prevented by vaccination (7). The anti-vaccine attitude has been extended to low- and middle-income countries (LMICs) of the EMR, specially against coronavirus disease 2019 (COVID-19) among adults (8–10), and parents (11, 12).
Vaccine hesitancy (VH) is defined by the WHO as a delay in acceptance or refusal of vaccines in spite of the availability of vaccination services (13). The Vaccine Hesitancy Matrix was created by the WHO (14), which broadly divides the causative factors of hesitancy into “contextual influences,” “individual and group influences,” and “vaccine- or vaccination-specific issues” and offers a comprehensive framework for understanding VH. By employing open-ended questions for these causal factors, the Strategic Advisory Group of Experts (SAGE) established indicators for VH according to the national schedule (15).
In the EMR, parental VH toward routine immunization and COVID-19 has been investigated, but limited studies specifically addressed the influenza VH (12, 16–18). In the United Arabs of Emirates (UAE), only 12% of the caregivers were hesitant to give their children routine vaccines (17). Meanwhile, in Egypt and Saudi Arabia, 70.6 and 61.9% of the parents hesitated to vaccinate their children against COVID-19, respectively (12, 16). Interestingly, high VH toward influenza was observed among Jordanian health care workers (18). Such a study could assist in the development of evidence-based interventions to improve influenza vaccine equity and optimize vaccine uptake among children. Thus, the aim of the present study was to investigate parental attitude toward childhood seasonal influenza vaccine and identify determinants of VH using the validated Parent Attitude about Childhood vaccines (PACV).
A cross-sectional study was conducted using an online survey (Qualtrics platform and Google form). Parents/guardians of children aged 6 months to 18 years were recruited using a convenient snowball sampling method from 14 EMR countries; Afghanistan, Bahrain, Egypt, Iraq, Jordan, Kuwait, Libya, Palestine, Pakistan, Qatar, Saudi Arabia, Syria, Tunisia, and UAE. The youngest child was included when parents had more than one child in the target age group. Parents of children under 6 months were excluded because the influenza vaccine is not recommended for this group. The online survey was distributed in bilingual format (Arabic and English) via social media channels to reach out most of the participants. The survey was administered from September 8th to October 16th, 2022.
Since the main language used in Pakistan is Urdu and the main languages used in Afghanistan are Pashto and Persian and there are no validated versions of the PACV in these languages, data collectors distributed the survey through online platforms in addition to face-to-face interviews to collect the required sample size. Based on an assumption of a prevalence rate of 50% for parental VH toward their children influenza vaccination, using 5% accepted degree of precision, α of 0.05 and power of 80%, the minimal required sample size was 384 participants from each country. The total sample size for the included countries was 5,376 and it was increased to 6,000 to compensate for missing data. The distribution of study sample size across the EMR is shown in Figure 1. We excluded 36 responses as they had incomplete data. The sample size was calculated using EPI-Info software version 7.2.5.
Data collection sheet was constructed based on literature review (13, 19, 20). Sociodemographic data was collected including country, residence area, mother’s age, mother’s education, mother’s occupation, total number of children (Supplementary File S1). Countries were classified according to the World Bank into 4 categories; high-income (Bahrain, Kuwait, Qatar, Saudi Arabia and UAE), upper middle income (Iraq, Jordan and Libya), lower middle income (Egypt, Palestine, Pakistan and Tunisia), and low income countries (Afghanistan and Syria) (21). Parental influenza vaccine uptake and source of information on vaccines were added. Data about children such as age, gender, birth order, and presence of chronic comorbidity were collected. Age of children were categorized into infants: from 6 months to the first year of life, preschool age: 2–4 years, school age: 5–9 years, and adolescents: 10–18 years. Childhood routine vaccination uptake and COVID-19 vaccine uptake were determined based on parental recall.
The English and Arabic validated versions of the PACV were used to identify parents who were hesitant toward childhood influenza vaccine (22, 23). The PACV has 15 elements with three domains: behavior toward the vaccine, beliefs about the safety and efficacy of the vaccine, and general attitudes and trust. The PACV response formats (dichotomous, 5-point Likert scale and 10-point Likert scale) were collapsed into three response categories: ‘Hesitant’ responses receive a score of 2, ‘not sure or do not know’ a score of 1, and ‘not hesitant’ 0. The total PACV score was calculated by summing each item and transformed into a 0–100 scale. The total PACV score generated, with a score < 50 indicating non hesitancy and ≥ 50 indicating hesitancy (23). The overall Cronbach’s alpha value of the PACV was 0.726.
A pilot test of the questionnaire was carried out to test its applicability. Corrective measures were taken including linguistic corrections to make sure that the language was clear. Additionally, a question asking about income was removed as the majority of pilot-test participants reported that it was a sensitive question. Pilot-test participants were excluded from the final study sample.
The frequency distribution and descriptive statistics (mean ± standard deviation) were used to describe the characteristics of the study participants. Bivariate analysis using the Chi-square test was performed to analyze the study participants according to hesitant or non-hesitant to vaccination. The Exact Fisher test or Monte Carlo test was used when Chi-square test assumptions were violated. Independent t-test was used to compare the means of quantitative variables between two unrelated groups. Two-tailed p value <0.05 was considered statistically significant. Statistical testing was performed using the Statistical Package for Social Sciences (SPSS), version 22.0 (IBM Corp., Armonk, NY, United States). A structural equations model (SEM) using the Analysis of Moment Structures (AMOS) software (version 23), was built to assess the direct, indirect, and total effects of exogenous and endogenous variables on the PACV. The goodness of fit was investigated using the root mean square residual (RMSR), the goodness of fit index (GFI) >0.9, comparative fit index (CFI) >0.9, and the normed fit index >0.9.
This study was approved by the Alexandria Faculty of Medicine Ethics’ Committee (IRB number 00012098/0305688). After explanation the study purpose, all participants agreed to the online informed consent before filling out the questionnaire. The online survey was conducted anonymously to ensure the confidentiality of data.
The mean age of the mothers was 36.7 ± 9.1 years, more than three-quarters of them were high school graduates or higher (4,725, 79.2%), and nearly one-fifth were low-income country residents (1,021, 17.1%). Children of the participants were nearly equally distributed by sex [male (3,085, 51.7%) vs. female (2,879, 48.3%)], with age group classified into four categories: infants (1,317, 22.1%), preschool children (1,647, 27.6%), school children (1,420, 23.8%), and adolescents (1,580, 26.5%). Other characteristics of the study participants are demonstrated in Table 1.
Nearly half of the parents were hesitant about vaccinating their children against seasonal influenza (3,018, 50.6%). Parental VH was significantly higher among older mothers (37.06 ± 8.8 years, p = 0.006), rural residents (426, 53.6%, p < 0.001), high-income countries residents (1,058, 50.6%, p < 0.001), and mothers with higher educational levels (2,462, 52.1%, p < 0.001), children free from any comorbidities (2,610, 52.5%, p < 0.001), children not getting routine vaccination at all (200, 51.5%, p = 0.03), children not vaccinated against COVID-19 (2,497, 54.3%, p < 0.001), in addition to parents who were not vaccinated against seasonal influenza (2,162, 57.1%, p < 0.001) were significantly associated with likelihood of VH. Parents depending on healthcare provider as a source of information regarding vaccines were less likely to report VH (2056, 47.9%, p < 0.001), meanwhile those who used social media as their source showed a significantly higher VH (1,194, 57.2%, p < 0.001; Table 1).
Figure 2 shows the total, direct, and indirect effect of exogenous and endogenous variables on the parental attitude toward childhood seasonal influenza vaccines using the SEM. Supplementary Table S1 shows the variables included in the SEM. The framework suggests that exogenous variables: mother’s age, residence (urban, rural), country income level (high-income countries, upper middle-income countries, lower middle-income countries), gender of the child, total number of children, and source of information regarding vaccines (social media and internet) had a direct effect on PACV. High-income country residency had a positive total effect on parental attitude toward vaccination, this means that parents living in high-income countries were more likely to be hesitant regarding vaccinating their children compared to those from low-income countries by positive total effect value of 4.03. The total, direct and indirect effects of other exogenous variables are demonstrated in Table 2.
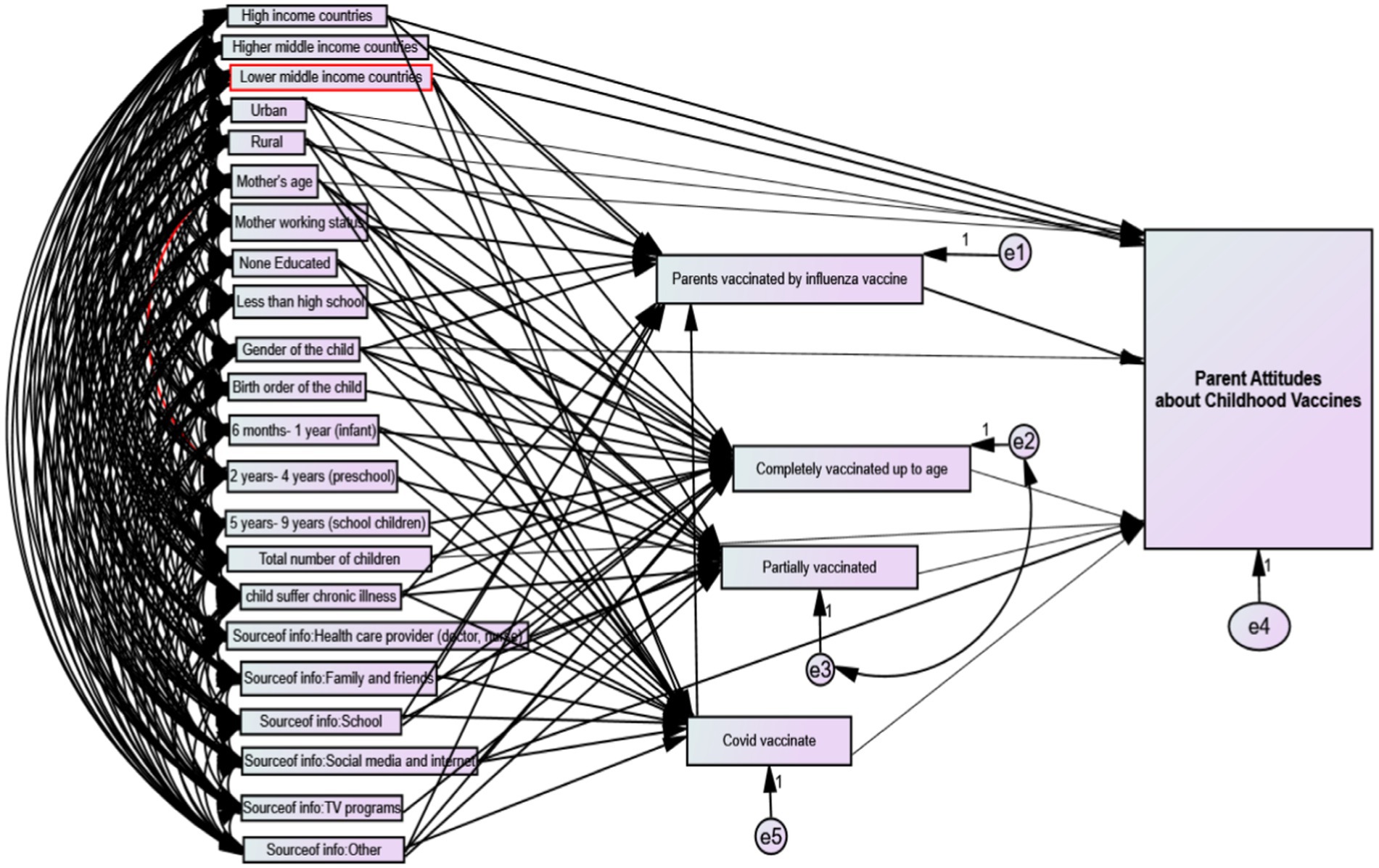
Figure 2. Visualization of the structural equations model for parental attitude toward childhood influenza vaccines.
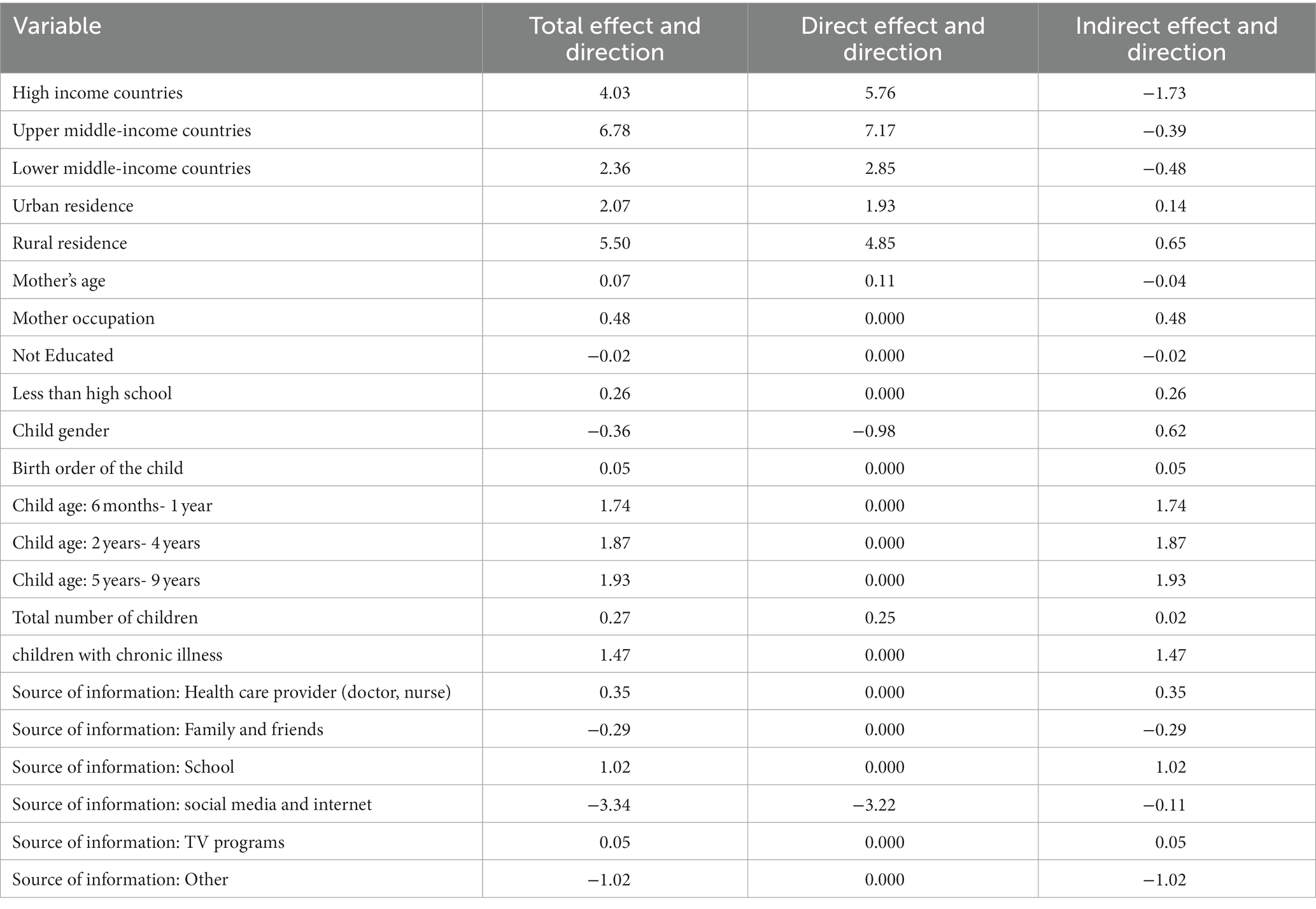
Table 2. Value and direction of the total, direct, and indirect effect of exogenous variables on parental attitude toward childhood influenza vaccines.
Table 3 shows the total, direct and indirect effects of the endogenous variables on parental attitude toward childhood seasonal influenza vaccines. Parents vaccinated against seasonal influenza had a positive total and direct effect on PACV with value of 6.74, while children completely and partially vaccinated have a negative total and direct effect on PACV with value of −4.57 and −3.76, respectively. There is no indirect effect of parents vaccinated against seasonal influenza, children completely or partially vaccinated on PACV; meanwhile children vaccinated against COVID-19 had an indirect effect on PACV with value of 1.67.
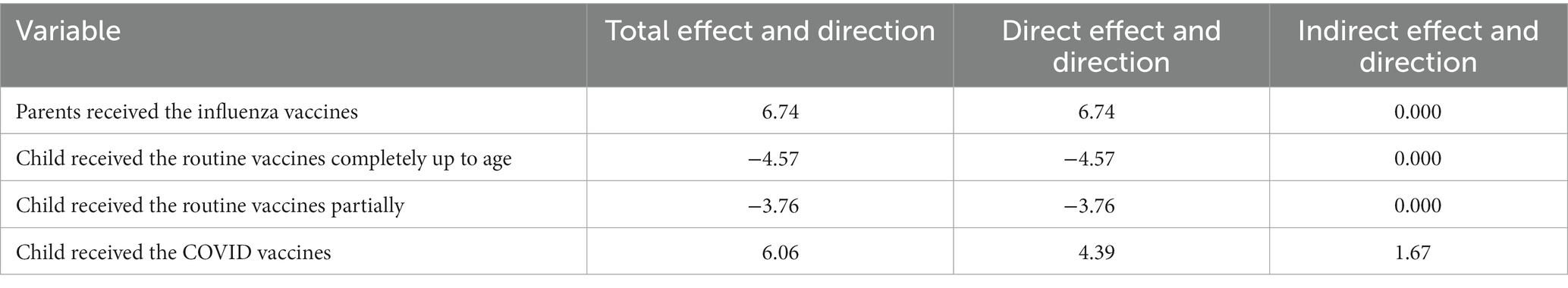
Table 3. Value and direction of the total, direct, and indirect effect of endogenous (intermediate) variables on parental attitude toward childhood influenza vaccines.
The model had an acceptable goodness of fit (GFI = 0.998, CFI = 0.997). The minimum discrepancy index = 4.328, the root means square residual = 0.081, the goodness of fit index = 0.998, the adjusted goodness of fit index was 0.980 which is acceptable, the comparative fit index was 0.997. The normed fit index was 0.996. The parsimony ratio index was 12.8%. Finally, the root mean square error of approximation was 0.024 (Supplementary Table S2).
In the current study, we provide the first estimates of parental attitude toward seasonal influenza vaccination from a large sample of parents in the EMR in addition to using the SEM to identify the direct and indirect determinants of VH. Almost half of the parents were hesitant to vaccinate their children with the seasonal influenza vaccine. This may be because the seasonal influenza vaccine is still a category B vaccine (non-EPI) compared to the free vaccine in the Expanded Program on Immunization (EPI) for children in most countries of the EMR. Only five EMR countries reported incorporating the influenza vaccine into their national immunization program namely; Iran, Libya, Qatar, Syria and Tunisia (5). Worldwide, the prevalence of VH among parents and caregivers toward childhood influenza vaccination ranged from 13% in Italy (33/255) (24), 25.8% in United States (530/2,176) (25), up to 56.03% in China (3,736/6,668) (19). These discrepancies among studies are likely the result of the difference in economic factors, cultural norms, level of knowledge about seasonal influenza vaccine, access to medical care, parents’ perception in addition to difference in study design and sample size.
Although seasonal influenza vaccine distribution is low in LMICs (26), the current study showed that VH was significantly higher among higher income parents. Previous studies reported that higher household incomes were negatively associated with the intention to vaccinate children against seasonal influenza (19, 27). In United States, it was also found that children living in high-affluent neighborhoods had 1.08% lower routine vaccination coverage than children in low-affluent areas (28). Furthermore, individuals in high-income countries showed more hesitancy toward COVID-19 vaccine due to concerns about vaccine safety (29). Meanwhile Harapan et al. (30) showed greater VH against COVID-19 vaccine in LMICs when compared to high income countries. On the contrary, a systematic review stated that the influence of income on seasonal influenza immunization has been inconsistent (31). The current study also showed a higher rate of VH among rural residents. Similarly, Vasudevan et al. (32) reported that rural mothers had more vaccine-related concerns compared to urban mothers. However, Lai et al. (19) reported that urban residents were more hesitant to vaccinate children. The current findings would be explained as high wealth may indicate more knowledge about medical exemptions and anti-vaccination campaigns (28), and more confidence in the quality of care provided to those of high economic status (27). Moreover, rural residence may reflect limited utilization of health care services (33), lower access to health information (34), and lower prevalence of health-related behaviors (35).
Surprisingly, the current study identified a higher educational level of mothers as a potential barrier to childhood seasonal influenza vaccination. The association between mother’s education and VH is still inconsistent; with some studies aligned with the current findings (19, 36, 37), while others found no relation (38, 39). Goldman et al. (40) suggested that parents with higher education might be less likely to change their mind about vaccination or could be more exposed to misinformation on social media. Role of education in VH is complex and may interplay with other factors influencing vaccination adherence. Furthermore, older age mothers were found to report a statistically significant impact on their VH behavior which was similar to the findings of Hamada et al. (41)
In the present study, parents of school-aged children were more likely to have VH. Similarly, a study found that parents of children aged 7–12 years (OR: 1.923), 12–14 years (OR: 2.372) had higher seasonal influenza VH compared to the under-3 years age group (36). Gates et al. (42) found that seasonal influenza vaccination coverage among children aged 5–12 years was 33.2%, which was lower than the rate reported among under-five children (52.6%). The result may be due to the fact that some parents assume that the risk of seasonal influenza infection and health threat is low and that their children’s immunity may improve with age. The current study also reported that parents of chronically ill children were less likely to show VH. Children with comorbidities are at higher risk for severe influenza and poorer progression (43), which explains why such parents would be more cautious of getting their children sick with influenza. On the contrary, Napolitano et al. (44) reported that existence of chronic medical conditions negatively affects immunization coverage rates among children, including seasonal influenza vaccination. While Almalki et al. (18) did not find an association between VH and chronic illness in children (16).
The current study showed that parents who were vaccinated against seasonal influenza showed lower level of VH. Awad et al. (45), and Alolayan et al. (38) also reported similar findings. Likewise, a previous systematic review has identified past vaccination experience and behavior as strong predictors of seasonal influenza vaccine acceptance (20). This may be because parents obtained the protective effect from the vaccine. Furthermore, the current study showed that parents of children who did not receive their EPI vaccines were more likely to have higher VH. Zakhour et al. (6) stated that parents who accepted seasonal influenza vaccination were more likely to believe in vaccine efficacy, have higher trust and show less VH and were more compliant with other vaccinations. Similarly. Goldman et al. (40) found that parents vaccinating their children up to date showed higher willingness to vaccinate them against seasonal influenza in the next year. Correspondingly, the current study found that parents whose children received the COVID-19 vaccine had a lower likelihood of VH, which is consistent with previous studies (36, 40, 46). This could reflect higher parental health literacy.
The current study showed that when a healthcare provider was the source of information about vaccines, parents were less likely to have VH. In line with present finding, Fan et al. (36) found that recommendations from medical staff to vaccinate children against seasonal influenza had reduced parental VH. Trusting in healthcare providers’ advice about seasonal influenza vaccine was also associated with decreased parental VH or refusal (19). Healthcare providers are the most trusted influencer of vaccination decisions (47). The current study also found that the use of social media as source of health information about vaccines increased the likelihood of VH. Likewise, using social media was negatively associated with seasonal influenza vaccine uptake among both pediatric (36) and adult population (48). However, Ahmed et al. (49) found that adult users of Twitter and Facebook as sources of health information were more likely to be vaccinated against influenza than those who did not use social media. Social media and internet are double-edged sword. Positive information could improve knowledge and trust, but misinformation advocating against vaccines have the opposite effect.
The current study showed that VH was not influenced by child gender, which was supported by findings of Lai et al. (19) On the contrary, a study reported that VH was significantly more common among parents who had girls (44). Additionally, the current study did not find an association between the number of children in the household and VH, which was similar to previous studies (17, 25, 44). However, another study reported that influenza VH was higher among caregivers with the only child in the family (19). Birth order of the index child did not have a significant impact on VH in the current study. Alsuwaidi et al. reported similar results (17).
To our knowledge, this is the first study to assess parental attitude toward seasonal influenza vaccination in the EMR. We used two languages (English and Arabic) to increase the response rate and the representation of the studied population. Another point of strength was that the analyzed data was from a large representative sample of parents in the EMR and were collected by a valid and reliable methodology. The large sample size provided the study with good statistical power. The data set also contained several contributing factors for the risk of VH including parental and child sociodemographic characteristic, child health status, and vaccination status. Furthermore, the CDC recommends offering influenza vaccine during September or October (4), that corresponds with timing of the present study and could affect parent’s decision to accept the seasonal influenza.
However, the findings of the current study should be interpreted in light of the following limitations. The online survey was susceptible to recall and social desirability bias, since it is based on self-reporting. Parental recall of their children’s vaccination status may also lead to recall bias, underreporting, and/or selective reporting. The sample selection was based on a non-probability technique using an online survey that may violate the generalization of the present findings. Another limitation was that the PACV was not validate in Urdu, Pashto and Persian languages. Further research is also needed to include more factors that could contribute to the likelihood of VH, such as the availability and accessibility of health care services and vaccination for children and other sociodemographic characteristics (e.g., fathers’ education and marital status). Finally, the inherent limitation of cross-sectional survey like recall bias and inability to assess causality could not be avoided.
The prevalence of parental VH toward childhood seasonal influenza vaccine in the EMR was considerably high, particularly among older mothers, residents of rural areas and high-income countries, mothers with higher educational levels, parents of school-aged children, children free from any comorbidities, children who did not receive routine vaccination at all, children not vaccinated against COVID-19, in addition to parents who were not vaccinated against influenza. The present findings have highlighted a significant public health concern regarding seasonal influenza vaccination. Understanding parental attitudes toward vaccinating their children is crucial in developing and implementing interventions to increase vaccination coverage. Moreover, plans and strategies should be directed toward incorporating seasonal influenza vaccination into the existing EPI schedules to reduce the disease burden among children in the EMR.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Alexandria Faculty of Medicine Ethics’ Committee IRB number (00012098/0305688). The patients/participants provided their written informed consent to participate in this study.
RG and NF: conceptualization and methodology. NT, AA, MA-S, IA-S, ME-D, JS, ZA, MR, ManA, ST, YG, SA-s, GH, MarA, LS, NY, SA, SY, KA-A, SM, and MFA: data collection and data cleaning. RG, AE, SA-R, and SI: data analysis. RG, NF, AE, SA-R, and SI: data curation. RG, NF, and MM: writing–original draft preparation. RG, NF, AG, and STA: writing–review and editing. RG: visualization. All authors have read and agreed to the published version of the manuscript.
This study was supported by Princess Nourah Bint Abdulrahman University Researchers Supporting Project number (PNURSP2023R177), Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia. The research team also expresses their deep thanks to the study participants for providing their time and sharing in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1132798/full#supplementary-material
VH, Vaccine hesitancy; PACV, Parent attitude about childhood vaccines; COVID-19, Coronavirus disease 2019; EMR, East Meditteranian Region; LMICs, Low-middle income countries; UAE, United Arab Emirates; USA, United States of America; EPI, Extended program of immunization; CDC, Centers for Diseases Control and Prevention; WHO, World Health Organization; SAGE, The Strategic Advisory Group of Experts; SEM, Structural equations model; GFI, Goodness of fit index; CFI, Comparative fit index; RMSEA, Root Mean Square Error of Approximation; AMOS, The Analysis of Moment Structures software; RMSR, The root mean square residual; OR, Odds ratio.
1. Moghadami, M. A narrative review of influenza: a seasonal and pandemic disease. Iranian J Med Sci. (2017) 42:2–13.
2. World Health Organization. (2023). Influenza (seasonal). Available at: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal).
3. Khan, W, El Rifay, AS, Malik, M, and Kayali, G. Influenza research in the Eastern Mediterranean region: a review. Oman Med J. (2017) 32:359–64. doi: 10.5001/omj.2017.70
4. Grohskopf, LA, Sokolow, LZ, Broder, KR, Walter, EB, Bresee, JS, Fry, AM, et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2017–18 Influenza Season. Amsterdam: Elsevier. (2017). 2970–2982.
5. Abubakar, A, Melhem, N, Malik, M, Dbaibo, G, Khan, WM, and Zaraket, H. Seasonal influenza vaccination policies in the Eastern Mediterranean region: current status and the way forward. Vaccine. (2019) 37:1601–7. doi: 10.1016/j.vaccine.2019.02.001
6. Zakhour, R, Tamim, H, Faytrouni, F, Khoury, J, Makki, M, and Charafeddine, L. Knowledge, attitude and practice of influenza vaccination among Lebanese parents: a cross-sectional survey from a developing country. PLoS One. (2021) 16:e0258258. doi: 10.1371/journal.pone.0258258
7. O'Leary, ST, Allison, MA, Fisher, A, Crane, L, Beaty, B, Hurley, L, et al. Characteristics of physicians who dismiss families for refusing vaccines. Pediatrics. (2015) 136:1103–11. doi: 10.1542/peds.2015-2086
8. Elbarazi, I, Yacoub, M, Reyad, O, Shawky, M, Elhadi, Y, Kheirallah, K, et al. Exploring Enablers and Barriers to COVID-19 Vaccine Acceptance Among Arabs: A Qualitative Study 2022.
9. Ghazy, R, Shawky, M, Sallam, M, Elbarazi, I, Awaidy, S, Ismail, I, et al. Acceptance of COVID-19 vaccine booster doses using the health belief model: a cross-sectional study in low-middle- and high-income countries of the East Mediterranean region. Int. J Environ. Res. Pub. Health. (2022) 19:12136. doi: 10.3390/ijerph191912136
10. Shawky, M, Kheirallah, K, Aly, M, Ramadan, A, Elhadi, Y, Elbarazi, I, et al. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: an online survey in 13 Arab countries. PLoS One. (2021):16. doi: 10.1371/journal.pone.0260321
11. Elkhadry, SW, Salem, TAEH, Elshabrawy, A, Goda, SS, Bahwashy, HAA, Youssef, N, et al. COVID-19 vaccine hesitancy among parents of children with chronic liver diseases. Vaccine. (2022) 10:2094. doi: 10.3390/vaccines10122094
12. Ghazy, RM, Sallam, M, Fadl, N, Bouraad, E, Youssef, N, and Ghoneim, OSA. Attitude of parents of children with cerebral palsy towards COVID-19 vaccination. Int J Environ Res Public Health. (2023) 20:1909. doi: 10.3390/ijerph20031909
13. MacDonald, NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
14. World Health Organization. (2022). Report of the SAGE working group on vaccine hesitancy. Available at: https://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf?ua=1 (Accessed December, 2022).
15. World Health Organization. (2022). WHO/UNICEF joint reporting process. Available at: https://www.who.int/immunization/monitoring_surveillance/routine/reporting/en/ (Accessed November, 2022).
16. Almalki, OS, Alfayez, OM, Al Yami, MS, Asiri, YA, and Almohammed, OA. Parents' hesitancy to vaccinate their 5–11-year-old children against COVID-19 in Saudi Arabia: predictors from the health belief model. Front Public Health. (2022):728. doi: 10.3389/fpubh.2022.842862
17. Alsuwaidi, AR, Elbarazi, I, Al-Hamad, S, Aldhaheri, R, Sheek-Hussein, M, and Narchi, H. Vaccine hesitancy and its determinants among Arab parents: a cross-sectional survey in the United Arab Emirates. Hum Vaccin Immunother. (2020) 16:3163–9. doi: 10.1080/21645515.2020.1753439
18. Sallam, M, Ghazy, RM, Al-Salahat, K, Al-Mahzoum, K, AlHadidi, NM, Eid, H, et al. The role of psychological factors and vaccine conspiracy beliefs in influenza vaccine hesitancy and uptake among Jordanian healthcare workers during the COVID-19 pandemic. Vaccine. (2022) 10:1355. doi: 10.3390/vaccines10081355
19. Lai, X, Li, M, Hou, Z, Guo, J, Zhang, H, Wang, J, et al. Factors associated with caregivers’ hesitancy to vaccinate children against influenza: a cross-sectional survey in China. Vaccine. (2022) 40:3975–83. doi: 10.1016/j.vaccine.2022.05.023
20. Schmid, P, Rauber, D, Betsch, C, Lidolt, G, and Denker, M-L. Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. (2017) 12:e0170550. doi: 10.1371/journal.pone.0170550
21. The world Bank. Countries and economies. Available at: https://data.worldbank.org/country (Accessed December 22, 2022).
22. ElSayed, DA, Bou Raad, E, Bekhit, SA, Sallam, M, Ibrahim, NM, Soliman, S, et al. Validation and cultural adaptation of the parent attitudes about childhood vaccines (PACV) questionnaire in Arabic language widely spoken in a region with a high prevalence of COVID-19 vaccine hesitancy. Trop Med Infect Dis. (2022) 7:234. doi: 10.3390/tropicalmed7090234
23. Opel, DJ, Taylor, JA, Mangione-Smith, R, Solomon, C, Zhao, C, Catz, S, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. (2011) 29:6598–605. doi: 10.1016/j.vaccine.2011.06.115
24. Williams, JT, Rice, JD, Lou, Y, Soderborg, TK, Bayliss, EA, Federico, SG, et al. Parental vaccine hesitancy and risk of pediatric influenza under-vaccination in a safety-net health care system. Acad Pediatr. (2021) 21:1126–33. doi: 10.1016/j.acap.2021.05.017
25. Kempe, A, Saville, AW, Albertin, C, Zimet, G, Breck, A, Helmkamp, L, et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics. (2020) 146:3852. doi: 10.1542/peds.2019-3852
26. Ortiz, JR, and Neuzil, KM. Influenza immunization in low-and middle-income countries: preparing for next-generation influenza vaccines. J Infect Dis. (2019) 219:S97–S106. doi: 10.1093/infdis/jiz024
27. Chen, C-H, Chiu, P-J, Chih, Y-C, and Yeh, G-L. Determinants of influenza vaccination among young Taiwanese children. Vaccine. (2015) 33:1993–8. doi: 10.1016/j.vaccine.2015.01.032
28. Hegde, S, Wagner, A, Clarke, P, Potter, R, Swanson, R, and Boulton, M. Neighbourhood influence on the fourth dose of diphtheria-tetanus-pertussis vaccination. Public Health. (2019) 167:41–9. doi: 10.1016/j.puhe.2018.11.009
29. Solís Arce, JS, Warren, SS, Meriggi, NF, Scacco, A, McMurry, N, Voors, M, et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat Med. (2021) 27:1385–94. doi: 10.1038/s41591-021-01454-y
30. Harapan, H, Anwar, S, Yufika, A, Sharun, K, Gachabayov, M, Fahriani, M, et al. Vaccine hesitancy among communities in ten countries in Asia, Africa, and South America during the COVID-19 pandemic. Pathogens Global Health. (2022) 116:236–43. doi: 10.1080/20477724.2021.2011580
31. Brien, S, Kwong, JC, and Buckeridge, DL. The determinants of 2009 pandemic a/H1N1 influenza vaccination: a systematic review. Vaccine. (2012) 30:1255–64. doi: 10.1016/j.vaccine.2011.12.089
32. Vasudevan, L, Baumgartner, JN, Moses, S, Ngadaya, E, Mfinanga, SG, and Ostermann, J. Parental concerns and uptake of childhood vaccines in rural Tanzania–a mixed methods study. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-09598-1
33. Casey, MM, Call, KT, and Klingner, JM. Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med. (2001) 21:182–8. doi: 10.1016/S0749-3797(01)00349-X
34. Chen, X, Orom, H, Hay, JL, Waters, EA, Schofield, E, Li, Y, et al. Differences in rural and urban health information access and use. J Rural Health. (2019) 35:405–17. doi: 10.1111/jrh.12335
35. Matthews, KA, Croft, JB, Liu, Y, Lu, H, Kanny, D, Wheaton, AG, et al. Health-related behaviors by urban-rural county classification-United States, 2013. MMWR Surveill Summ. (2017) 66:1–8. doi: 10.15585/mmwr.ss6605a1
36. Fan, J, Ye, C, Wang, Y, Qi, H, Li, D, Mao, J, et al. Parental seasonal influenza vaccine hesitancy and associated factors in Shanghai, China, during the COVID-19 pandemic: a cross-sectional study. Vaccine. (2022) 10:2109. doi: 10.3390/vaccines10122109
37. Strelitz, B, Gritton, J, Klein, EJ, Bradford, MC, Follmer, K, Zerr, DM, et al. Parental vaccine hesitancy and acceptance of seasonal influenza vaccine in the pediatric emergency department. Vaccine. (2015) 33:1802–7. doi: 10.1016/j.vaccine.2015.02.034
38. Alolayan, A, Almotairi, B, Alshammari, S, Alhearri, M, and Alsuhaibani, M. Seasonal influenza vaccination among Saudi children: parental barriers and willingness to vaccinate their children. Int J Environ Res Public Health. (2019) 16:4226. doi: 10.3390/ijerph16214226
39. Henrikson, NB, Anderson, ML, Opel, DJ, Dunn, J, Marcuse, EK, and Grossman, DC. Longitudinal trends in vaccine hesitancy in a cohort of mothers surveyed in Washington state, 2013-2015. Public Health Rep. (2017) 132:451–4. doi: 10.1177/0033354917711175
40. Goldman, RD, McGregor, S, Marneni, SR, Katsuta, T, Griffiths, MA, Hall, JE, et al. Willingness to vaccinate children against influenza after the coronavirus disease 2019 pandemic. J Pediatr. (2021) 228:87–93.e2. doi: 10.1016/j.jpeds.2020.08.005
41. Hamadah, RE, Hussain, AN, Alsoghayer, NA, Alkhenizan, ZA, Alajlan, HA, and Alkhenizan, AH. Attitude of parents towards seasonal influenza vaccination for children in Saudi Arabia. J Fam Med Primary Care. (2021) 10:904–9. doi: 10.4103/jfmpc.jfmpc_1602_20
42. Gates, DM, Cohen, SA, Orr, K, and Caffrey, AR. Pediatric influenza vaccination rates lower than previous estimates in the United States. Vaccine. (2022) 40:6337–43. doi: 10.1016/j.vaccine.2022.09.053
43. Norman, DA, Barnes, R, Pavlos, R, Bhuiyan, M, Alene, KA, Danchin, M, et al. Improving influenza vaccination in children with comorbidities: a systematic review. Pediatrics. (2021) 147:1433. doi: 10.1542/peds.2020-1433
44. Napolitano, F, Miraglia del Giudice, G, Angelillo, S, Fattore, I, Licata, F, Pelullo, CP, et al. Hesitancy towards childhood vaccinations among parents of children with underlying chronic medical conditions in Italy. Vaccine. (2022) 10:1254. doi: 10.3390/vaccines10081254
45. Awad, S, Abdo, N, Yusef, D, Jawarneh, A, Babaa, A, Al-Bawayeh, H, et al. Knowledge, attitudes and practices related to influenza illness and vaccination in children: role of awareness campaigns in changing parents’ attitudes toward influenza vaccination in Jordan. Vaccine. (2019) 37:3303–9. doi: 10.1016/j.vaccine.2019.04.083
46. Helmkamp, LJ, Szilagyi, PG, Zimet, G, Saville, AW, Gurfinkel, D, Albertin, C, et al. A validated modification of the vaccine hesitancy scale for childhood, influenza and HPV vaccines. Vaccine. (2021) 39:1831–9. doi: 10.1016/j.vaccine.2021.02.039
47. Paterson, P, Meurice, F, Stanberry, LR, Glismann, S, Rosenthal, SL, and Larson, HJ. Vaccine hesitancy and healthcare providers. Vaccine. (2016) 34:6700–6. doi: 10.1016/j.vaccine.2016.10.042
48. Benis, A, Khodos, A, Ran, S, Levner, E, and Ashkenazi, S. Social media engagement and influenza vaccination during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2021) 23:e25977. doi: 10.2196/25977
Keywords: influenza, vaccination, parental hesitancy, parental attitude, childhood, Eastern Mediterranean
Citation: Fadl N, Al Awaidy ST, Elshabrawy A, Makhlouf MSAH, Ibrahim SA, Abdel-Rahman S, Tookhy NA, Alsalmani A, Al-Saeedi M, Al-Sawalha I, El-Din MAA, Saad J, Ayoob Z, Rourou MK, Ali M, Tawati SM, Gadain YMA, Al-saidi SY, Hassan GA, Alsanafi M, Sandouk L, Youssef N, Alothman S, Yazbek S, Al-Ansi KS, Mehdad S, Adam MF, Gebreal A and Ghazy RM (2023) Determinants of parental seasonal influenza vaccine hesitancy in the Eastern Mediterranean region: A cross-sectional study. Front. Public Health 11:1132798. doi: 10.3389/fpubh.2023.1132798
Received: 27 December 2022; Accepted: 07 March 2023;
Published: 28 March 2023.
Edited by:
Satinder Aneja, Sharda University, IndiaReviewed by:
Eman Salem, University of Menoufia, EgyptCopyright © 2023 Fadl, Al Awaidy, Elshabrawy, Makhlouf, Ibrahim, Abdel-Rahman, Tookhy, Alsalmani, Al-Saeedi, Al-Sawalha, El-Din, Saad, Ayoob, Rourou, Ali, Tawati, Gadain, Al-saidi, Hassan, Alsanafi, Sandouk, Youssef, Alothman, Yazbek, Al-Ansi, Mehdad, Adam, Gebreal and Ghazy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Noha Fadl, nohaosama@alexu.edu.eg
†ORCID: Noha Fadl https://orcid.org/0000-0001-9807-2720
Abdelhamid Elshabrawy https://orcid.org/0000-0003-4748-0008
Mona Sayed Aly Hassan Makhlouf https://orcid.org/0000-0002-4561-9689
Sarah Assem Ibrahim https://orcid.org/0000-0002-9157-2252
Suzan Abdel-Rahman https://orcid.org/0000-0002-5779-0926
Nazir Ahmad Tookhy https://orcid.org/0000-0001-7906-0652
Abdullah Alsalmani https://orcid.org/0000-0001-5022-7834
Mays Al-Saeedi https://orcid.org/0000-0001-2345-6789
Ibrahim Al-Sawalha https://orcid.org/0000-0003-4295-5553
Mohammad Amin Aly El-Din https://orcid.org/0000-0003-1298-7482
Janet Saad https://orcid.org/0000-0003-1848-5803
Zainab Ayoob https://orcid.org/0000-0002-7320-8238
Mohamed Khalil Rourou https://orcid.org/0000-0001-6902-5423
Manahil Ali https://orcid.org/0000-0002-6936-7746
Salha M. Tawati https://orcid.org/0000-0003-2280-7465
Sara Yunis Al-saidi https://orcid.org/0000-0002-8175-4917
Mariam Alsanafi https://orcid.org/0000-0002-1366-3693
Leen Sandouk https://orcid.org/0000-0001-6347-2732
Naglaa Youssef https://orcid.org/0000-0002-0368-1759
Saja Yazbek https://orcid.org/0000-0002-1612-8709
Khlood Saleh Al-Ansi https://orcid.org/0000-0001-6056-5204
Slimane Mehdad https://orcid.org/0000-0002-3800-6817
Mohammed Fathelrahman Adam https://orcid.org/0000-0001-6930-9004
Assem Gebreal https://orcid.org/0000-0002-2155-8500
Ramy Mohamed Ghazy https://orcid.org/0000-0001-7611-706X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.