- The Research Center of National Drug Policy & Ecosystem, China Pharmaceutical University, Nanjing, Jiangsu, China
Background: Primary health care (PHC) serves as the gatekeeper of health system and PHC physicians take on significant obligations to provide health care services in the pursuit of Universal Health Coverage (UHC). PHC physicians' health-related quality of life (HRQoL) can have a strong impact on patients, physicians and the health care system. Lifestyle interventions are found to be effective to improve HRQoL. The purpose of this study was to evaluate the association between lifestyle behaviors and HRQoL among PHC physicians, so that lifestyle intervention can be tailored by policy makers for health promotion.
Methods: A survey covering 31 provinces and administrative regions in China was conducted in 2020 using a stratified sampling strategy. Data on sociodemographic characteristics lifestyle behaviors and HRQoL were collected by a self-administered questionnaire. HRQoL was measured through EuroQol-five dimension-five level (EQ-5D-5L) instrument. A Tobit regression model was performed to evaluate the association between sociodemographic characteristics, lifestyle behaviors and HRQoL.
Results: Among 894 PHC physicians who completed the survey, Anxiety/Depression (AD) was the dimension with the most problems reported (18.1%). Regular daily routine (β = 0.025, 95%CI 0.004 to 0.045) and good sleep quality (β = 0.049, 95% CI = 0.029 to 0.069) were protective factors for HRQoL, while smoking (β = −0.027, 95% CI = −0.079 to −0.003) and frequency of eating breakfast (β = −0.041, 95%CI = −0.079 to −0.003) were negatively associated with HRQoL. Physical activity and alcohol drinking were not significantly associated with HRQoL.
Conclusion: These findings suggest that tailored interventions on daily routine, improving sleep quality, and tobacco control among PHC physicians may be effective strategies to improve their HRQoL.
1. Introduction
Primary health care (PHC) is defined as a whole-of-society approach to effectively organizing and strengthening national health systems to bring services for health and well-being closer to communities, from health promotion to disease prevention, treatment, rehabilitation, palliative care and more (1). PHC serves as the gatekeeper of health system (2) and provides the foundation for the strengthening of the essential public health functions to confront public health crises such as COVID-19. Physicians, the backbone of the primary health care workforce (3), play a vital role in coordinating a person's care needs, from prevention to disease management to curative care (4). With the goal of Universal Health Coverage (UHC) and strengthening PHC system (5), primary health care physicians are expected to take on a heavier burden to provide health care services, particularly in times of crisis such as the COVID-19 pandemic. A number of studies have demonstrated a high prevalence of physical and mental illness, job burnout (6, 7), sleep disturbance (8) and even suicide (9) among physicians, concerning unsatisfactory health-related quality of life (HRQoL).
HRQoL is a multidimensional concept representing both positive and negative aspects of physical and psychological health, social functioning, and overall well-being (10). Poor HRQoL of physicians could have a negative impact on work performance and patient outcomes in addition to their individual health (11, 12). As a result, addressing HRQoL of physicians benefits patients, physicians and the health care system. In China, the total number of PHC physicians was 1.246 million and PHC institutions provided 50.2% of outpatient care (4.3 billion visits) and 14.5% of inpatient care (35.9 million hospital admissions) in 2021 (13). Given the great amount of health care service provided by PHC physicians, it is an urgent public health issue that HRQoL of PHC physicians should be improved in the light of enhancing PHC services and physicians' performance.
It is evidently identified that lifestyle behaviors affect people's health, HRQoL and life expectancy (14–17). Moreover, lifestyle interventions were found to be effective to improve HRQoL (18, 19) as well as the implementation of lifestyle interventions in the workplace has been proven to be cost-effective for both employers and society (20, 21). The occupational category should be considered when designing workplace health promotion programs in the belief that the occupational category produces significant differences in lifestyle behaviors (22–24). In addition, the association between lifestyle behaviors and HRQoL varies between occupations. For instance, smoking was not found to be associated with HRQoL among government employees (25) while current smoker had lower HRQoL in professional drivers (26). The result of a study suggested that breakfast, exercise, smoking and drinking should be given priority to health promotion at work for doctors (23). But it is unknown whether these lifestyle behaviors are risky or not for HRQoL of PHC physicians. Physicians are considered as a group with a higher level of health literacy (27), and their better perceived capacities in finding, understanding and applying health information could directly lead to better physical health and subjective well-being (28). For example, healthcare professionals are more likely to attend medical programs due to their work environment. A research found that smoking and alcohol consumption were not related to quality of life as anticipated among residents participating in the medical checkups (29). Considering the above, the influence of lifestyle behaviors on HRQoL of physicians may not be the same as that in the general population or other occupations. Moreover, despite knowledge of the significance of healthy lifestyle behaviors, healthcare workers do not adopt healthy lifestyle behaviors for various reasons (30–33), such as a false feeling of “protection” due to their medical knowledge, excessive workload, lack of time or motivation, and the tendency to prioritize their patients' health over their own. Knowledge of the relationship between lifestyle behaviors and HRQoL among physicians would help tailor more effective health-promoting interventions.
Prior work has documented the relationship between lifestyle behaviors and HRQoL in different population. However, these studies have primarily focused on patients with different diseases (14, 18, 34–36) and general populations including adolescents, adults and the elderly from different countries or regions (17, 20, 21). In research to date, few studies have examined such relationships in healthcare professional groups (37), especially little is known about that in primary health care physicians. A study investigated the relationship between lifestyle factors (smoking, BMI, cooking oil, meals out per week, total fruit and vegetable intake per day, physical activity level, and hours of TV, laptop, or internet use per day) and quality of life among 72 PHC physicians in Saudi Arabia (38) with limitation of small sample size. However, other important lifestyle behaviors' influence [e.g., alcohol consumption, sleep quality (16, 39–41)] on HRQoL of PHC physicians has not been properly studied yet. Combined consideration of both occupational characteristics of healthcare professionals (23, 30, 42) [e.g. atypical work schedules (43), heavy workload and stress (44)] and lifestyle behaviors which have been identified as potential factors affecting HRQoL in the Chinese population (39, 45–47), lifestyle behaviors including daily routine, breakfast, sleep quality, smoking, drinking and physical activity should be taken into account. The absence of relative research on the relationship between such lifestyle behaviors and HRQoL among PHC physicians, however, is an impediment to health policy consideration for improving their HRQoL.
The aim of this study was to evaluate the association between lifestyle behaviors and HRQoL among Chinese primary health care physicians. Such important information could be informative for local health care policy makers and researchers to consider at which levels effective lifestyle interventions should be implemented to improve the HRQoL of primary health care physicians.
2. Methods
2.1. Setting and study design
This cross-sectional study covering 31 provinces and administrative regions in China in 2020 was designed to investigate the associations between some lifestyle behaviors and HRQoL. PHC physicians were recruited and data were collected by a self-administered questionnaire. The inclusion criteria of respondents were: 18 years or older, able to fill in the questionnaire independently and employed in primary health care sectors as physicians in China. A stratified sampling strategy was adopted, and the detailed steps were as follows: (1) The sample of the study included 31 provinces and administrative regions in China. The cities or districts of each region were categorized into three groups (high, medium, and low) according to GDP per capita in 2018, forming a total of 93 groups. (2) At least two local PHC institutions including community health centers, township health centers, and community health stations were selected respectively for convenience sampling in each group, forming a total of 558 samples of PHC institution. (3) In each PHC institution, at least two physicians selected by convenience sampling were willing to participate in and complete the investigation.
2.2. Instruments
2.2.1. Sociodemographic information
Sociodemographic information was collected including age, sex, height, weight, marital status, number of children, caregiving status, annual household income, educational level, job title, type of residence and chronic diseases. The sociodemographic characteristics mentioned above were included in the study as covariate. Age was divided into three groups: young adults (age 18–44 years), middle-aged adults (age 45–59 years), and older adults (age over 60 years) (48). Body mass index (BMI) was computed from self-reported weight and height and was divided into three groups: BMI < 18.5, 18.5 ≤ BMI ≤ 24.9, BMI ≥ 25 (49). Annual household income was categorized into three levels (RMB): < ¥80,000, ¥80,000 ~ ¥1,50,000 and >¥1,50,000.
2.2.2. Lifestyle behaviors profile
The following health-related lifestyle behaviors were included in the study as independent variables: daily routine, sleep quality, breakfast, smoking, drinking and physical activity. The item “daily routine” was referred to as the established patterns of waking, eating, sleeping, and organizing one's time daily (50), which was evaluated into two statuses: irregular and regular. Sleep quality was answered by “not good” and “good” subjectively. Frequency of eating breakfast weekly means how many times individuals had breakfast in 1 week in the last 6 months, which was divided into two groups: < 4 times and at least 4 times. Both smoking and drinking status were categorized by yes or no. Smoking was defined as at least one cigarette per day in the last 6 months and drinking was defined as at least once a week in the last 6 months. Physical activity was classified as to whether the respondent practice any sports, exercise or other physical activity for at least 30 min during a usual week.
2.2.3. Measurement of HRQoL
HRQoL was measured by the Chinese version of the EuroQol-five dimension-five level (EQ-5D-5L), consisting of a descriptive system and EQ- 5D visual analog scale (EQ-VAS) (51). EQ-5D-5L is one of the major self-reported instruments to evaluate HRQoL due to its simplicity, low respondent burden and high universal acceptance (52). It includes five dimensions: Mobility (MO), Self-Care (SC), Usual Activities (UA), Pain/Discomfort (PD), and Anxiety/Depression (AD). Each dimension has five levels. The responses for the five dimensions can be combined in a 5-digit number describing the respondent's health state (from 11111 meaning no problems at all to 55555 meaning extreme problems in all five dimensions). Then the responses obtained were converted to the EQ-5D utility index based on Chinese value sets (53) to represent HRQoL.
2.2.4. Questionnaire validation
The validity, rationality, comprehensibility, and readability of the questionnaire had been verified by experts and the results of a pilot survey in community health centers in Nanjing, Jiangsu province, China. Based on the feedback from the pilot survey, the research team revised the questionnaire and formulate the final version.
2.3. Data collection
A total of 500 undergraduate students majoring in clinical pharmacy or pharmacy were recruited as investigators. In order to ensure the survey quality, each investigator was strictly trained before the investigation, including understanding the principles and methods of survey design, and standardizing the definition. In the process of collecting data, investigators provided the participants with an electronic device—Interview Master, a survey app in WeChat, and gave them instructions about how to complete the questionnaire on the app. Then the responses were automatically converted into electronic data for analysis software. A total of 5 master students were recruited and trained as auditors. If auditors found obvious errors in the data, the data would be returned to the data collectors and then they would verify it with the respondents.
2.4. Data analysis
Data were analyzed by STATA 17 for Windows and IBM SPSS Statistics 26 for Windows. Means and standard deviations (SD) were used to describe continuous variable data as well as frequencies and percentages are used to describe categorical variable data. Differences in HRQoL based on categories of sociodemographic characteristics and lifestyle behaviors were explored using Mann–Whitney U (two groups) and Kruskal–Wallis one-way analysis of variance (multiple groups) due to the abnormal distribution of the EQ-5D utility index. The EQ-5D utility index was skewed and it was censored at 1 (54), so a Tobit regression model was chosen to explore the potential effects of sociodemographic characteristics and lifestyle behaviors on HRQoL. The level of statistical significance was set at p < 0.05 in all analyses. Variance inflation factor (VIF) was used to test the multicollinearity. Robust test was conducted by changing conversion formula to calculate HRQoL. The formula was as follows: 1 subtract the sum of the five dimensions scores divided by 25. The value represented HRQoL by a single index ranging from 0 (for 55555) to 0.8 (for 11111).
3. Results
3.1. Sociodemographic and lifestyle behaviors
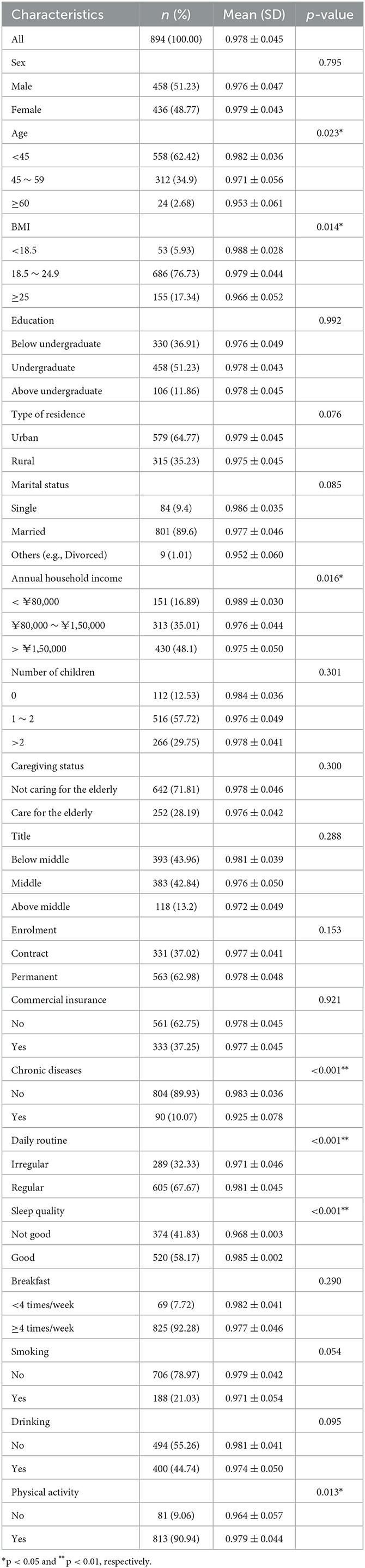
A total of 1,227 participants answered the questionnaire, of which 894 (73%) provided valid information on all included variables (e.g., the measures of weight and height both were valid, current health status was consistent with chronic disease prevalence). Table 1 summarizes the sociodemographic characteristics and lifestyle behaviors of the participants. A total of 894 participants were included and had an average HRQoL of 0.978 (SD = 0.045). The mean age was 41.19 (SD = 9.15), among which the ratio of male to female respondents was around1: 1.05. Annual household income of respondents was ¥1,62,600 (SD = 1,15,500) on average. Majority of them were married (89.60%) and had at least one child (87.47%). Approximately 90.00% of participants reported not having any chronic diseases diagnosed in the hospital at the time of completing the survey. For their lifestyle behaviors, over half of them had regular daily routine (67.67%) and good sleep quality (58.17%). Almost all of them had breakfast at least 4 times a week (92.28%). Most of them did not smoke (78.97%) or consume alcohol (55.26%). The percentage of respondents who never participated in physical activity was 9.06%.
3.2. EQ-5D-5L dimensional profile and HRQoL
Five levels on the EQ-5D dimension included no problem, slight, moderate, severe, and extreme problems. Frequency of item response in each EQ-5D-5L dimension as follows: MO (97.8%, 2.0%, 0.2%, 0.0%, 0.0%), SC (99.6%, 0.4%, 0.0%, 0.0%, 0.0%), UA (98.2%, 1.8%, 0.0%, 0.0%, 0.0%), PD (83.2%, 16.1%, 0.7%, 0.0%, 0.0%) and AD (81.9%, 17.2%, 0.9%, 0.0%, 0.0%). In this survey, the largest number of participants reported problems in the AD dimension (18.1%), followed by the PD dimension (16.8%). Roughly 99% of participants had no problem in the other three dimensions. The least problematic dimension was the SC dimension accounting for only 0.4%.
The results of HRQoL for each factor were also shown in Table 1. Significant differences were found in the subgroups of age, BMI, and annual household income. Younger group (age < 45) had better HRQoL (0.982 ± 0.036) than the older group (0.971 ± 0.056, 0.953 ± 0.061 respectively). Highest BMI group (BMI ≥ 25) had the lowest HRQoL (0.966 ± 0.052), whereas lowest BMI group (BMI < 18.5) had the highest HRQoL (0.988 ± 0.028). HRQoL was progressively lower with an increase in income categories (p = 0.016), and lowest in those with an annual income over ¥1,50,000 (0.975 ± 0.050). Participants suffering from chronic diseases had lower HRQoL (0.925 ± 0.078) than those without chronic disease (0.978 ± 0.045). Regarding lifestyle behaviors, significant differences were found in some factors: daily routine (p < 0.001), sleep quality (p < 0.001) and physical activity (p = 0.013). In the case of daily routine, the average HRQoL of participants who answered “not regular” was 0.971 ± 0.046, while that of participants who answered “regular” was 0.981 ± 0.045. Participants who had good sleep quality and participated in physical activity had better HRQoL. Differences in HRQoL based on other lifestyle behaviors (e.g., breakfast, smoking and drinking) did not reach a statistically significant level.
3.3. Regression analysis
The Tobit regression analysis revealed that several demographic characteristics and lifestyle behaviors were significantly associated with HRQoL in the adjusted model (Pseudo R2 = 0.6038) (Table 2). Female (β = −0.029, p = 0.014, 95% CI = −0.052 to −0.006) and higher annual household income (β = −0.052, p = 0.001, 95% CI −0.083 to −0.021 and β = −0.050, p = 0.002, 95% CI = −0.082 to −0.019) were a risk factor for HRQoL among participants. Suffering from chronic diseases (β = −0.118, p < 0.001, 95% CI = −0.146 to −0.090) and rural residence (β = −0.028, p = 0.011, 95% CI = −0.049 to −0.006) were negatively associated with HRQoL of respondents. In addition, a negative correlation was identified between HRQoL and the frequency of eating breakfast (β = −0.041, p = 0.036, 95% CI = −0.079 to −0.003). A positive association was observed between HRQoL and regular daily routine (β = 0.025, p = 0.018, 95% CI = 0.004 to 0.045) as well as good sleep quality (β = 0.049, p < 0.001, 95% CI = 0.029 to 0.069). Smoking status was significantly associated with the HRQoL. Compared with non-smokers, smokers report significantly lower HRQoL (β = −0.027, p = 0.043, 95% CI = −0.079 to −0.003). Associations between other lifestyle behaviors (drinking and physical activity) and HRQoL did not reach a statistically significant level. Variance inflation factor (VIF) for each independent variable was well below the recommended threshold of 10 (55), suggesting that the models did not have a multicollinearity issue. Changing conversion formula to calculate HRQoL did not materially alter the conclusions of the original tobit model (Appendix Table 1). Associations between sleep quality (β = 0.059, p < 0.001, 95% CI = 0.037 to 0.081), breakfast (β = −0.046, p = 0.029, 95% CI = −0.087 to −0.005) and physical activity (β = 0.035, p = 0.039, 95% CI = 0.002 to 0.068) with HRQoL were significantly observed in the unadjusted model (Pseudo R2 = 0.1879).
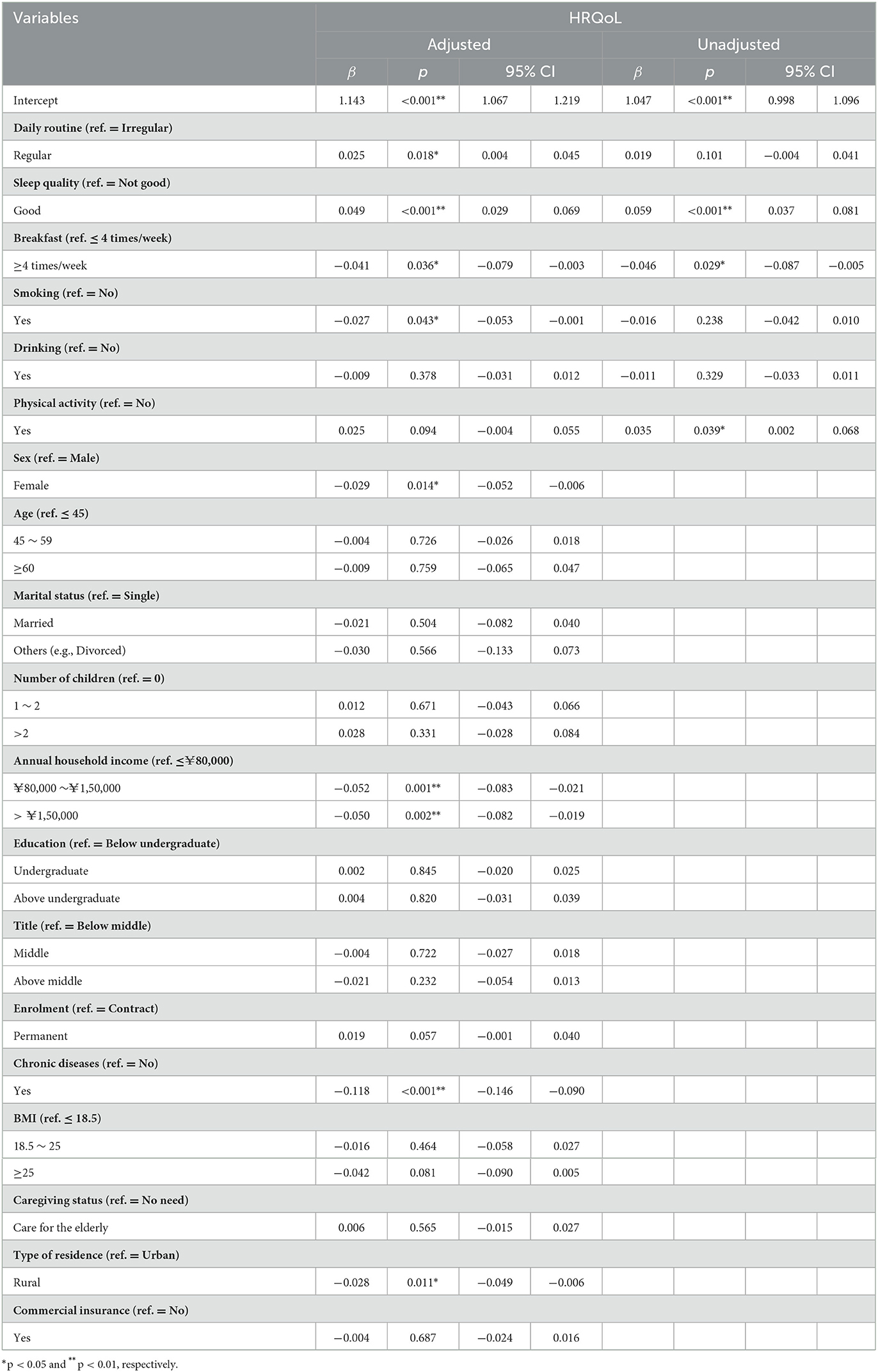
Table 2. Tobit regression analysis between sociodemographic characteristics, lifestyle behaviors and HRQoL.
4. Discussion
The purpose of this study was to explore the relationship between lifestyle behaviors and HRQoL among Chinese primary health care physicians. Our results confirmed the significant association between daily routine, sleep quality, breakfast, smoking and HRQoL, while drinking and physical activity were not found to influence HRQoL of Chinese primary health care physicians.
We found that regular daily routine and good sleep quality were positively associated with HRQoL among Chinese primary health care physicians. Given the 24-h nature of medical care, shift work is common in the healthcare sectors, including evening, night, and early morning shifts, as well as fixed or rotating schedules (56). As a main cause to irregular daily routine, shift work appears to be a risk factor for overweight, obesity, type 2 diabetes, elevated blood pressure, sleep deprivation and the metabolic syndrome, all of which have a poor impact on HRQoL (57, 58). Workers during irregular daily routine will experience the negative influence of sleeping, waking, and eating at an inappropriate circadian phase (59). There is evidence that the circadian rhythms of individuals during an irregular daily routine may deteriorate mood and performance in the healthcare sectors (60, 61). This situation highlights the necessity for examination and intervention programs on negative health outcomes connected with shift work. According to a meta-analysis (8), the pooled prevalence of sleep disturbances among Chinese healthcare professionals was much higher than the general population in China, owing to the changes of lifestyle, increased work pressure, and deteriorating doctor-patient relationships. In addition, physicians are reported more caffeine consumption than the general population (62), which have several negative effects on sleep quality and quantity (63). Poor sleep quality, however, may have a negative impact on immune system and be related to depression and anxiety, which can affect both physical and mental health in HRQoL (64, 65) and result in high levels of burnout causing more medical errors (62, 66, 67). It is suggested that health care policy makers should implement measure to improve sleep quality of primary health care physicians, such as promoting physical activity, strategic naps, work hour reductions and environmental modifications in the workplace (56, 62). Maybe health care organizations can follow an example of some companies which provide rooms with nap pods or beds for the purpose of napping (68).
Our finding that smoking was a risky factor for HRQoL was in accord with earlier researches (45, 46). Physicians may be particularly at risk of smoking, due to heavy workload, work conditions, or nightshifts disrupting the circadian rhythm (69). The overall smoking prevalence among Chinese physicians ranged from 14 to 64% across studies and smoking rates of PHC physicians was 42% (70). On the one hand, smokers are more likely than non-smokers to develop cardio vascular disease, stroke, lung cancer and have higher risks of heart failure (71, 72). On the other hand, physicians who smoke have less knowledge and less favorable attitude toward tobacco control compared to non-smokers (73, 74). Consequently, they would provide less smoking cessation counseling for their patients (75). Furthermore, smoking may cause diminished overall health and increased absenteeism from work (76), which not only have negative impact on the delivery of the healthcare services to their patients but also cause substantial economic burden of sickness absenteeism (77). As a result, it is recommended to develop tailored smoking cessation training programs for primary health care physicians.
Interestingly, we discovered that the frequency of breakfast was inversely connected to HRQoL among primary health care physicians in the current study, whereas a study conducted in Taiwan (78) showed that breakfast skippers had significantly worse HRQoL than breakfast eaters. One possible explanation for this might be that participants are more inclined to skip breakfast for longer sleep durations, since sleep quality (β = 0.049) appears to have greater impact than breakfast (β = −0.042) on HRQoL. Although there are some evidence showed that skipping breakfast is negatively associated with obesity (78), diabetes mellitus (79) and dyslipidemia, the importance of breakfast remains controversial (80, 81). Breakfast skippers seemed to have lower risk for of chronic disease and skipping breakfast as a way for calorie restriction may have potential metabolic benefits including neuroprotective, anti-aging, and anti-inflammatory (81). In addition, there is a study indicating that breakfast skippers showed better HRQOL and lower levels of stress and depression than breakfast eaters who ate a poor or very poor quality of breakfast (40). According to the study, a good quality breakfast comprises of bread/toast/cereal and/or dairy products rather than commercially prepared goods. Moreover, compared with a nutrition-inadequate breakfast and no breakfast, a nutrition-adequate breakfast will significantly improve short-term cognitive function (82), emphasizing the importance of breakfast quality. Physicians may have limited access to healthy breakfast due to work commitments and lack of time in the workplace (83). Hence, the association between breakfast quality and HRQoL should be further studied in future.
Furthermore, an increasing number of studies have been conducted to examine the relationship between physical activity and HRQoL (47, 84, 85). It was evidently demonstrated that physical activity improved HRQoL and well-being when compared with minimal or no-treatment controls for adults aged 18–65 years (86). The typical primary health care physician works long hours and leads a sedentary lifestyle, thus they are encouraged to shift from being sedentary to doing some physical activity which has the greatest potential health gains (87). However, contrary to expectations, physical activity was not significantly associated with HRQoL based on our regression result and this finding was in line with a research among PHC physician in Saudi Arabia (38). Nonetheless, Mann–Whitney U analysis showed that participants who had a habit of physical activity (90.94%) got significantly better HRQoL. The insignificant regression results may be due to the fact that most of the participants had a habit of physical activity, which requires further research on a larger scale. Also, a recent study discovered that shift work seemed to hinder the beneficial effects of physical activity (88). Similarly to physical activity, drinking was not found significantly associated with HRQoL in line with some researches (39, 89) while some studies have demonstrated that drinking is a risk factor for HRQoL (46, 47, 90). By contrast, some studies have reported moderate drinkers tending to have better HRQoL than non-drinkers and heavy drinkers (16, 91, 92). Besides, drinking was found to effectively alleviate stress and be linked to improved mental health in healthcare professionals (93, 94). Such the existence of a causal relationship between alcohol consumption patterns and HRQoL may be resulted from differences in consumption by sex, nationality, and individual characteristics (92). Moreover, a review indicated that alcohol consumption was an independent predictor of chronic conditions (95), which was a significantly negative factor of HRQoL in our study. Our result also could be partly explained by the inclusion of participants who refrain from alcohol consumption permanently or temporarily due to the presence of chronic disease, which consequently would decrease their HRQoL. Therefore, further studies including more specific drinking groups should be conducted in the future to determine the precise correlations between alcohol consumption and HRQoL in primary health care physicians.
Approximately 18.1% of the study participants reported problems in the Anxiety/Depression dimension which was higher than the other four dimensions. Many studies indicated that physicians can be affected by the full spectrum of mental disorders and the most common mental disorders reported among physicians are depression and anxiety (96–98). Workplace risk factors, such as high job demands, a work-family life imbalance and long working hours, are often important in explaining much of the variation in mental ill health among physicians (99). Working as a primary health care physician involves a heavy workload, and consequently they have little leisure time to spend with their family and friends. Furthermore, healthcare workers are always at the frontline of public health responses to major critical incidents and emergencies like COVID-19 (100, 101), causing increases in mental ill health among them. In this regard, it is high time that public health care policy makers should establish ways to mitigate mental health risks and tailor interventions, such as modifications to work processes, shortening of shifts (98) and mental health training, which effectively make an enhancement in some mental health outcomes among primary health care physicians. Another potential solution is eHealth interventions including Cognitive Behavioral Therapy, Stress Management, Mindfulness approaches and Cognitive training through Apps, which appears to be an effective and more feasible way than face-to-face sessions to deliver these types of interventions among PHC physicians (102, 103).
Several study limitations are worth mentioning. First, our results should be generalized with caution to other countries with different cultural backgrounds because this was a cross-sectional study in China. Second, physicians also might have reported underestimation of unfavorable lifestyle behaviors or overestimation of HRQoL in this study because of social acceptability bias. Third, dietary behaviors were not included. It should be fully studied in future. Lastly, we used a simple questionnaire of lifestyle behaviors for greater response by participants, which might result in missing important information. We suggest that future studies use standardized questionnaires to comprehensively measure daily routine, sleep quality, breakfast, smoking, drinking and physical activity. For example, physical activity can be assessed by International Physical Activity Questionnaire (IPAQ) (104).
5. Conclusions
This study evaluated association of lifestyle behaviors including daily routine, sleep quality, frequency of eating breakfast, physical activity, drinking, and smoking with HRQoL in a group of 894 Chinese primary health care physicians. Our study found that lifestyle behaviors including daily routine, sleep quality, frequency of eating breakfast, and smoking affected the HRQoL of Chinese primary health care physicians. However, this association was not observed for other lifestyle behaviors including drinking and physical activity. These findings may guide health policy makers to tailor interventions, such as adequate sleep, strategic naps, and smoking cessation training programs, to improve HRQoL of primary health care physicians effectively.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The research design was reviewed and approved by the Ethics Committee of China Pharmaceutical University, Nanjing city, Jiangsu Province, China (Project Number: CPU2014006). All methods were carried out in accordance with the relevant guidelines and regulations. Based on the principle of informed consent, all data were collected anonymously after obtaining the permission and informed consent signed by respondents.
Author contributions
YH and XX contributed to the conception and design of the study. YL and YH contributed to the data analysis. YL, YH, and XX contributed to the interpretation of data. YL contributed to writing manuscript. All authors had read and approved the final version of the manuscript for submission.
Acknowledgments
We acknowledge the support of Primary Health Care Physicians who volunteered to participate in our research and the help of members involved in data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1131031/full#supplementary-material
References
1. World Health Organization. Available online at: https://www.who.int/health-topics/primary-health-care (accessed November 4, 2022).
2. Liu Q, Wang B, Kong Y, Cheng KK. China's primary health-care reform. Lancet. (2011) 377:2064–6. doi: 10.1016/S0140-6736(11)60167-0
3. Li X, Lu J, Hu S, Cheng K, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
4. Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet. (2020) 395:1802–12. doi: 10.1016/S0140-6736(20)30122-7
5. World Health Organization United Nations Children's Fund (UNICEF). A Vision for Primary Health Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals. Geneva: World Health Organization (2018).
6. Pogosova NV, Isakova SS, Sokolova OY, Ausheva AK, Zhetisheva RA, Arutyunov AA. Occupational burnout, psychological status and quality of life in primary care physicians working in outpatient settings. Kardiologiia. (2021) 61:69–78. doi: 10.18087/cardio.2021.6.n1538
7. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
8. Qiu D, Yu Y, Li R-Q, Li Y-L, Xiao S-Y. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med. (2020) 67:258–66. doi: 10.1016/j.sleep.2019.01.047
9. Steffen MW, Hagen PT, Benkhadra K, Molella RG, Newcomb RD, Murad MH, et al. survey of physicians' perceptions of their health care needs. Occup Med (Lond). (2015) 65:49–53. doi: 10.1093/occmed/kqu145
10. CDC. Health-Related Quality of Life (HRQOL). (2018). Available online at: https://www.cdc.gov/hrqol/concept.htm (accessed December 16, 2022).
11. Tong SC, Tin AS, Tan DM. Lim JF. The health-related quality of life of junior doctors. Ann. Acad. Med. (2012) 41:7. doi: 10.47102/annals-acadmedsg.V41N10p444
12. Iqbal MS. Health-related quality of life among healthcare providers in Pakistan. J Pharm Bioallied Sci. (2021) 13:31–8. doi: 10.4103/jpbs.JPBS_265_20
13. Statistical Bulletin on the Development of Health Care in China in 2021. Available online at: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=51b55216c2154332a660157abf28b09d (accessed December 13, 2022).
14. Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. (2020) 368:l6669. doi: 10.1136/bmj.l6669
15. Baceviciene M, Jankauskiene R, Balciuniene V. The role of body image, disordered eating and lifestyle on the quality of life in Lithuanian university students. Int J Environ Res Public Health. (2020) 17:1593. doi: 10.3390/ijerph17051593
16. Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, et al. The impact of healthy lifestyle factors on life expectancies in the US population. Circulation. (2018) 138:345–55. doi: 10.1161/CIRCULATIONAHA.117.032047
17. Hu Z, Qin L, Kaminga AC, Xu H. Relationship between multiple lifestyle behaviors and health-related quality of life among elderly individuals with prediabetes in rural communities in China. Medicine. (2020) 99:e19560. doi: 10.1097/MD.0000000000019560
18. Menichetti J, Villa S, Magnani T, Avuzzi B, Bosetti D, Marenghi C, et al. Lifestyle interventions to improve the quality of life of men with prostate cancer: A systematic review of randomized controlled trials. Crit Rev Oncol Hematol. (2016) 108:13–22. doi: 10.1016/j.critrevonc.2016.10.007
19. Saha S, Carlsson KS, Gerdtham U-G, Eriksson MK, Hagberg L, Eliasson M, et al. Are lifestyle interventions in primary care cost-effective? – an analysis based on a markov model, differences-in-differences approach and the Swedish Björknäs study. PLoS ONE. (2013) 8:e80672. doi: 10.1371/journal.pone.0080672
20. Orji CC, Ghosh S, Nwaobia OI, Ibrahim KR, Ibiloye EA, Brown CM. Health behaviors and health-related quality of life among US adults aged 18-64 years. Am J Prev Med. (2021) 60:529–36. doi: 10.1016/j.amepre.2020.10.020
21. da Costa BGG, Chaput J-P, Lopes MVV, da Costa RM, Malheiros LEA, Silva KS. Association between lifestyle behaviors and health-related quality of life in a sample of Brazilian adolescents. IJERPH. (2020) 17:7133. doi: 10.3390/ijerph17197133
22. Huang S-L, Li R-H, Tang F-C. Comparing disparities in the health-promoting lifestyles of taiwanese workers in various occupations. Ind Health. (2010) 48:256–64. doi: 10.2486/indhealth.48.256
23. Tsiga E, Panagopoulou E, Niakas D. Health promotion across occupational groups: one size does not fit all. Occup Med. (2015) 65:552–7. doi: 10.1093/occmed/kqv097
24. Väisänen D Kallings LV Andersson G Wallin P Hemmingsson E Ekblom-Bak E. Lifestyle-associated health risk indicators across a wide range of occupational groups: a cross-sectional analysis in 72,855 workers. BMC Public Health. (2020) 20:1656. doi: 10.1186/s12889-020-09755-6
25. Ashri MHM, Saad HA, Adznam SN. Factors associated with health-related quality of life among government employees in Putrajaya, Malaysia. Int J Environ Res Public Health. (2021) 18:2626. doi: 10.3390/ijerph18052626
26. Wong CKH, Fung CSC, Siu S-C, Wong K-W, Lee K-F, Lo YYC, et al. The impact of work nature, lifestyle, and obesity on health-related quality of life in Chinese professional drivers. J Occup Environ Med. (2012) 54:989–94. doi: 10.1097/JOM.0b013e3182535d7d
27. Budhathoki SS, Pokharel PK, Jha N, Moselen E, Dixon R, Bhattachan M, et al. Health literacy of future healthcare professionals: a cross-sectional study among health sciences students in Nepal. Int Health. (2019) 11:15–23. doi: 10.1093/inthealth/ihy090
28. Zhang F, Or PPL, Chung JWY. How different health literacy dimensions influences health and well-being among men and women: the mediating role of health behaviours. Health Expect. (2021) 24:617–27. doi: 10.1111/hex.13208
29. Matsushita T, Matsushima E. Quality of life and lifestyle among city dwellers participating in the medical programs. Psychiatry Clin Neurosci. (2004) 58:642–50. doi: 10.1111/j.1440-1819.2004.01315.x
30. PROFIS M, SIMON-TUVAL T. The influence of healthcare workers' occupation on health promoting lifestyle profile. Ind Health. (2016) 54:439–47. doi: 10.2486/indhealth.2015-0187
31. Yang W, Sim T, Cui K, Zhang J, Yang Y, Ma X. Health-promoting lifestyles among health care workers in a postdisaster area: a cross-sectional study. Disaster Med Public Health Prep. (2019) 13:230–5. doi: 10.1017/dmp.2018.36
32. Ross A, Bevans M, Brooks AT, Gibbons S, Wallen GR. Nurses and health-promoting behaviors: knowledge may not translate into self-care. AORN J. (2017) 105:267–75. doi: 10.1016/j.aorn.2016.12.018
33. Borgan SM, Jassim GA, Marhoon ZA, Ibrahim MH. The lifestyle habits and wellbeing of physicians in Bahrain: a cross-sectional study. BMC Public Health. (2015) 15:655. doi: 10.1186/s12889-015-1969-x
34. Gopalakrishna A, Longo TA, Fantony JJ, Van Noord M, Inman BA. Lifestyle factors and health-related quality of life in bladder cancer survivors: a systematic review. J Cancer Surviv. (2016) 10:874–82. doi: 10.1007/s11764-016-0533-8
35. Wu H, Li H, Li H, Ding Y, Wang C, Zhang G, et al. Evaluation of health-related quality of life in adults with and without dyslipidaemia in rural areas of central China. Qual Life Res. (2020) 29:925–39. doi: 10.1007/s11136-019-02336-0
36. Zhang X, Lu J, Wu C, Cui J, Wu Y, Hu A, et al. Healthy lifestyle behaviours and all-cause and cardiovascular mortality among 09 million Chinese adults. Int J Behav Nutr Phys Act. (2021) 18:162. doi: 10.1186/s12966-021-01234-4
37. Chiou S-T, Chiang J-H, Huang N, Chien L-Y. Health behaviors and participation in health promotion activities among hospital staff: which occupational group performs better? BMC Health Serv Res. (2014) 14:474. doi: 10.1186/1472-6963-14-474
38. Aljohani AM, Al-Zalabani AH. Lifestyle factors and quality of life among primary health care physicians in Madinah, Saudi Arabia. Saudi J Biol Sci. (2021) 28:4732–7. doi: 10.1016/j.sjbs.2021.04.087
39. Song T, Ding Y, Sun Y, He Y-N, Qi D, Wu Y, et al. A population-based study on health-related quality of life among urban community residents in Shenyang, Northeast of China. BMC Public Health. (2015) 15:921. doi: 10.1186/s12889-015-2238-8
40. Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in spanish adolescents. Int J Environ Res Public Health. (2018) 15:E1781. doi: 10.3390/ijerph15081781
41. Lu L, Lok K-I, Zhang Q, Zhang L, Xiang Y, Ungvari GS, et al. Sleep disturbance and its association with quality of life among psychiatric nurses in China. PeerJ. (2021) 9:e10659. doi: 10.7717/peerj.10659
42. Almhdawi KA, Alrabbaie H, Arabiat A, Alhammouri AT, Hamadneh M, Obeidat D, et al. Physicians' health-related quality of life and its associated factors during COVID-19 pandemic in Jordan: a cross-sectional study. Eval Health Prof. (2022) 45:76–85. doi: 10.1177/01632787211068899
43. Power N, Perreault M, Ferrari M, Boudreau P, Boivin DB. Sleep of healthcare workers during the COVID-19 pandemic and the role of atypical work schedules: a scoping review. J Biol Rhythms. (2022) 37:358–84. doi: 10.1177/07487304221103376
44. Bouillon-Minois J-B, Trousselard M, Pereira B, Schmidt J, Clinchamps M, Thivel D, et al. Protocol of the study on emergency health care workers' responses evaluated by karasek questionnaire: the SEEK-study protocol. Int J Environ Res Public Health. (2021) 18:4068. doi: 10.3390/ijerph18084068
45. Jing Z, Li J, Wang Y, Yuan Y, Zhao D, Hao W, et al. Association of smoking status and health-related quality of life: difference among young, middle-aged, and older adults in Shandong, China. Qual Life Res. (2021) 30:521–30. doi: 10.1007/s11136-020-02645-9
46. Xu J, Qiu J, Chen J, Zou L, Feng L, Lu Y, et al. Lifestyle and health-related quality of life: a cross-sectional study among civil servants in China. BMC Public Health. (2012) 12:330. doi: 10.1186/1471-2458-12-330
47. Liao W, Liu X, Kang N, Song Y, Yuchi Y, Hu Z, et al. Associations between healthy lifestyle score and health-related quality of life among Chinese rural adults: variations in age, sex, education level, and income. Qual Life Res. (2022) 32:81–92. doi: 10.1007/s11136-022-03229-5
48. Yu J, Ma G, Wang S. Do age-friendly rural communities affect quality of life? A comparison of perceptions from middle-aged and older adults in China. Int J Environ Res Public Health. (2021) 18:7283. doi: 10.3390/ijerph18147283
49. Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. Treasure Island, FL: StatPearls Publishing (2022).
50. O'Conor R, Benavente JY, Kwasny MJ, Eldeirawi K, Hasnain-Wynia R, Federman AD, et al. Daily routine: associations with health status and urgent health care utilization among older adults. Gerontologist. (2019) 59:947–55. doi: 10.1093/geront/gny117
51. Luo N, Li M, Liu GG, Lloyd A, de Charro F, Herdman M. Developing the Chinese version of the new 5-level EQ-5D descriptive system: the response scaling approach. Qual Life Res. (2013) 22:885–90. doi: 10.1007/s11136-012-0200-0
52. Cunillera O, Tresserras R, Rajmil L, Vilagut G, Brugulat P, Herdman M, et al. Discriminative capacity of the EQ-5D, SF-6D, and SF-12 as measures of health status in population health survey. Qual Life Res. (2010) 19:853–64. doi: 10.1007/s11136-010-9639-z
53. Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L value set for China. Value Health. (2017) 20:662–9. doi: 10.1016/j.jval.2016.11.016
54. Austin PC. Bayesian extensions of the Tobit model for analyzing measures of health status. Med Decis Making. (2002) 22:152–62. doi: 10.1177/0272989X0202200212
55. Jeffrey MW. Introductory Econometrics, a Modern Approach. 5th ed. Nashville, TN: South-Western CENGAGE (2013).
56. Redeker NS, Caruso CC, Hashmi SD, Mullington JM, Grandner M, Morgenthaler TI. Workplace interventions to promote sleep health and an alert, healthy workforce. J Clin Sleep Med. (2020) 15:649–57. doi: 10.5664/jcsm.7734
57. Hemmer A, Mareschal J, Dibner C, Pralong JA, Dorribo V, Perrig S, et al. The effects of shift work on cardio-metabolic diseases and eating patterns. Nutrients. (2021) 13:4178. doi: 10.3390/nu13114178
58. Chen C, ValizadehAslani T, Rosen GL, Anderson LM, Jungquist CR. Healthcare shift workers' temporal habits for eating, sleeping, and light exposure: a multi-instrument pilot study. J Circadian Rhythms. (2020) 18:6. doi: 10.5334/jcr.199
59. Meyer N, Harvey AG, Lockley SW, Dijk D-J. Circadian rhythms and disorders of the timing of sleep. Lancet. (2022) 400:1061–78. doi: 10.1016/S0140-6736(22)00877-7
60. Dall'Ora C, Ball J, Recio-Saucedo A, Griffiths P. Characteristics of shift work and their impact on employee performance and wellbeing: a literature review. Int J Nurs Stud. (2016) 57:12–27. doi: 10.1016/j.ijnurstu.2016.01.007
61. Minors DS, Nicholson AN, Spencer MB, Stone BM, Waterhouse JM. Irregularity of rest and activity: studies on circadian rhythmicity in man. J Physiol. (1986) 381:279–95. doi: 10.1113/jphysiol.1986.sp016327
62. Stewart NH, Arora VM. The impact of sleep and circadian disorders on physician burnout. Chest. (2019) 156:1022–30. doi: 10.1016/j.chest.2019.07.008
63. Watson EJ, Coates AM, Kohler M, Banks S. Caffeine consumption and sleep quality in Australian adults. Nutrients. (2016) 8:479. doi: 10.3390/nu8080479
64. Clement-Carbonell V, Portilla-Tamarit I, Rubio-Aparicio M, Madrid-Valero JJ. Sleep quality, mental and physical health: a differential relationship. Int J Environ Res Public Health. (2021) 18:460. doi: 10.3390/ijerph18020460
65. Chen X, Gelaye B, Williams MA. Sleep characteristics and health-related quality of life among a national sample of American young adults: assessment of possible health disparities. Qual Life Res. (2014) 23:613–25. doi: 10.1007/s11136-013-0475-9
66. Giorgi F, Mattei A, Notarnicola I, Petrucci C, Lancia L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J Adv Nurs. (2018) 74:698–708. doi: 10.1111/jan.13484
67. Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. (2008) 336:488–91. doi: 10.1136/bmj.39469.763218.BE
68. Hunasikatti M. The impact of sleep and circadian disorders on physician burnout: time for “Nap Time.” Chest. (2020) 157:1689. doi: 10.1016/j.chest.2019.11.057
69. Besson A, Tarpin A, Flaudias V, Brousse G, Laporte C, Benson A, et al. Smoking prevalence among physicians: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:13328. doi: 10.3390/ijerph182413328
70. Abdullah AS, Qiming F, Pun V, Stillman FA, Samet JM. A review of tobacco smoking and smoking cessation practices among physicians in China: 1987–2010. Tob Control. (2013) 22:9–14. doi: 10.1136/tobaccocontrol-2011-050135
71. Yang R, Lv J, Yu C, Guo Y, Bian Z, Han Y, et al. Importance of healthy lifestyle factors and ideal cardiovascular health metrics for risk of heart failure in Chinese adults. Int J Epidemiol. (2022) 51:567–78. doi: 10.1093/ije/dyab236
72. Centers for Disease Control Prevention. Health Effects of Cigarette Smoking. (2022). Available online at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm (accessed December 14, 2022).
73. Behbehani NN, Hamadeh RR, Macklai NS. Knowledge of and attitudes towards tobacco control among smoking and non-smoking physicians in 2 Gulf Arab states. Saudi Med J. (2004) 25:585–91. Available online at: https://smj.org.sa/content/25/5/585
74. Hallett R. Intervention against smoking and its relationship to general practitioners' smoking habits. J R Coll Gen Pract. (1983) 33:565–7.
75. Lam TH, Jiang C, Chan Y-F, Chan SSC. Smoking cessation intervention practices in Chinese physicians: do gender and smoking status matter? Health Soc Care Community. (2011) 19:126–37. doi: 10.1111/j.1365-2524.2010.00952.x
76. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking-−50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention (US) (2014).
77. Gianino MM, Politano G, Scarmozzino A, Stillo M, Amprino V, Di Carlo S, et al. Cost of sickness absenteeism during seasonal influenza outbreaks of medium intensity among health care workers. Int J Environ Res Public Health. (2019) 16:E747. doi: 10.3390/ijerph16050747
78. Huang C-J, Hu H-T, Fan Y-C, Liao Y-M, Tsai P-S. Associations of breakfast skipping with obesity and health-related quality of life: evidence from a national survey in Taiwan. Int J Obes. (2010) 34:720–5. doi: 10.1038/ijo.2009.285
79. Nishiyama M, Muto T, Minakawa T, Shibata T. The combined unhealthy behaviors of breakfast skipping and smoking are associated with the prevalence of diabetes mellitus. Tohoku J Exp Med. (2009) 218:259–64. doi: 10.1620/tjem.218.259
80. Betts JA, Chowdhury EA, Gonzalez JT, Richardson JD, Tsintzas K, Thompson D. Is breakfast the most important meal of the day? Proc Nutr Soc. (2016) 75:464–74. doi: 10.1017/S0029665116000318
81. Zilberter T, Zilberter EY. Breakfast: to skip or not to skip? Front Public Health. (2014) 2:59. doi: 10.3389/fpubh.2014.00059
82. Tang Z, Zhang N, Liu A, Luan D, Zhao Y, Song C, et al. The effects of breakfast on short-term cognitive function among Chinese white-collar workers: protocol for a three-phase crossover study. BMC Public Health. (2017) 17:92. doi: 10.1186/s12889-017-4017-1
83. Nicholls R, Perry L, Duffield C, Gallagher R, Pierce H. Barriers and facilitators to healthy eating for nurses in the workplace: an integrative review. J Adv Nurs. (2017) 73:1051–65. doi: 10.1111/jan.13185
84. Cj W, Jl S, Cr L-A, Td S, Kd O, Er L. Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clinic Proc. (2013) 88:1435–42. doi: 10.1016/j.mayocp.2013.09.010
85. Anokye NK, Trueman P, Green C, Pavey TG, Taylor RS. Physical activity and health related quality of life. BMC Public Health. (2012) 12:624. doi: 10.1186/1471-2458-12-624
86. Farris SG, Abrantes AM. Mental health benefits from lifestyle physical activity interventions: a systematic review. Bull Menninger Clin. (2020) 84:337–72. doi: 10.1521/bumc.2020.84.4.337
87. Brockhurst I, Wong J, Garr H, Batt ME. Physical activity in practice: why and how to get GPs moving. Br J Gen Pract. (2019) 69:276–7. doi: 10.3399/bjgp19X703769
88. Härmä M, Tenkanen L, Sjöblom T, Alikoski T, Heinsalmi P. Combined effects of shift work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scand J Work Environ Health. (1998) 24:300–7. doi: 10.5271/sjweh.324
89. Teles MAB, Barbosa MR, Vargas AMD, Gomes VE, e Ferreira EF, Martins AME de BL, et al. Psychosocial work conditions and quality of life among primary health care employees: a cross sectional study. Health Qual Life Outcomes. (2014) 12:72. doi: 10.1186/1477-7525-12-72
90. Wu X, Liu Q, Li Q, Tian Z, Tan H. Health-related quality of life and its determinants among criminal police officers. Int J Environ Res Public Health. (2019) 16:E1398. doi: 10.3390/ijerph16081398
91. Chan AM, von Mühlen D, Kritz-Silverstein D, Barrett-Connor E. Regular alcohol consumption is associated with increasing quality of life and mood in older men and women: the Rancho Bernardo Study. Maturitas. (2009) 62:294–300. doi: 10.1016/j.maturitas.2009.01.005
92. Kim K, Kim J-S. The association between alcohol consumption patterns and health-related quality of life in a nationally representative sample of South Korean Adults. PLoS ONE. (2015) 10:e0119245. doi: 10.1371/journal.pone.0119245
93. Tran TV, Nguyen HC, Pham LV, Nguyen MH, Nguyen HC, Ha TH, et al. Impacts and interactions of COVID-19 response involvement, health-related behaviours, health literacy on anxiety, depression and health-related quality of life among healthcare workers: a cross-sectional study. BMJ Open. (2020) 10:e041394. doi: 10.1136/bmjopen-2020-041394
94. Marshall LL, Allison A, Nykamp D, Lanke S. Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ. (2008) 72:137. doi: 10.5688/aj7206137
95. Wang HH, Wang JJ, Wong SY, Wong MC Li FJ, Wang PX, Zhou ZH, et al. Epidemiology of multimorbidity in China and implications for the healthcare system: cross-sectional survey among 162,464 community household residents in southern China. BMC Med. (2014) 12:188. doi: 10.1186/s12916-014-0188-0
96. He M, Wang Q, Zhu S, Tan A, He Q, Chen T, et al. Health-related quality of life of doctors and nurses in China: findings based on the latest open-access data. Qual Life Res. (2012) 21:1727–30. doi: 10.1007/s11136-011-0088-0
97. Xi X, Lu Q, Wo T, Pei P, Lin G, Hu H, et al. Doctor's presenteeism and its relationship with anxiety and depression: a cross-sectional survey study in China. BMJ Open. (2019) 9:e028844. doi: 10.1136/bmjopen-2018-028844
98. Harvey SB, Epstein RM, Glozier N, Petrie K, Strudwick J, Gayed A, et al. Mental illness and suicide among physicians. Lancet. (2021) 398:920–30. doi: 10.1016/S0140-6736(21)01596-8
99. Harvey SB, Modini M, Joyce S, Milligan-Saville JS, Tan L, Mykletun A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. (2017) 74:301–10. doi: 10.1136/oemed-2016-104015
100. Wang L, Ni X, Li Z, Ma Y, Zhang Y, et al. Mental health status of medical staff exposed to hospital workplace violence: a prospective cohort study. Front Public Health. (2022) 10:930118. doi: 10.3389/fpubh.2022.930118
101. Zou Q, Tang Y, Jiang C, Lin P, Tian J, Sun S. Prevalence of anxiety, depressive and insomnia symptoms among the different groups of people during COVID-19 pandemic: an overview of systematic reviews and meta-analyses. Front Psychol. (2022) 13:1024668. doi: 10.3389/fpsyg.2022.1024668
102. Deady M, Choi I, Calvo RA, Glozier N, Christensen H, Harvey SB. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry. (2017) 17:310. doi: 10.1186/s12888-017-1473-1
103. Stratton E, Lampit A, Choi I, Calvo RA, Harvey SB, Glozier N. Effectiveness of eHealth interventions for reducing mental health conditions in employees: a systematic review and meta-analysis. PLoS ONE. (2017) 12:e0189904. doi: 10.1371/journal.pone.0189904
104. Ren YJ, Su M, Liu QM, Tan YY, Du YK, Li LM, et al. Validation of the Simplified Chinese-character version of the international physical activity questionnaire-long form in urban community-dwelling adults: a cross-sectional study in Hangzhou, China. Biomed Environ Sci. (2017) 30:255–63. doi: 10.3967/bes2017.035
Keywords: health-related quality of life (HRQoL), lifestyle, primary health care, physician, China
Citation: Lin Y, Huang Y and Xi X (2023) Association between lifestyle behaviors and health-related quality of life among primary health care physicians in China: A cross-sectional study. Front. Public Health 11:1131031. doi: 10.3389/fpubh.2023.1131031
Received: 24 December 2022; Accepted: 16 February 2023;
Published: 08 March 2023.
Edited by:
Russell Kabir, Anglia Ruskin University, United KingdomReviewed by:
Xianglong Xu, Shanghai University of Traditional Chinese Medicine, ChinaLimei Jing, Shanghai University of Traditional Chinese Medicine, China
Copyright © 2023 Lin, Huang and Xi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoyu Xi, eGl4eUBjcHUuZWR1LmNu
 Yisha Lin
Yisha Lin Xiaoyu Xi
Xiaoyu Xi