- 1Gastric Cancer Center & Gastric Cancer Laboratory, Department of General Surgery, West China Hospital, Sichuan University, Chengdu, China
- 2Department of General Surgery, Second People’s Hospital of Yibin City – West China Yibin Hospital, Sichuan University, Yibin, China
- 3Health Management Center, General Practice Medical Center, West China Hospital, Sichuan University, Chengdu, China
- 4Department of Gastrointestinal Surgery, People’s Hospital of Ya’an City – West China Ya’an Hospital, Sichuan University, Ya’an, China
- 5Yibin Cancer Prevention and Control Center, Second People’s Hospital of Yibin City – West China Yibin Hospital, Sichuan University, Yibin, China
Objectives: The efficacy of updated health policy in improving the generalization of Helicobacter pylori screening and eradication in southwest China was assessed in a longitudinal analysis of multiple cross-sectional studies from an institution.
Methods: In the periods 2009–2010, 2013–2014, and 2019–2021, 8,365, 16,914, and 18,281 urban observations from health check-ups at West China Hospital were analyzed, respectively. The 14C-urea or 13C-urea breath test was consistently used for H. pylori detection. The protocol has been reported elsewhere (PROSPERO Registration number: CRD42019120764).
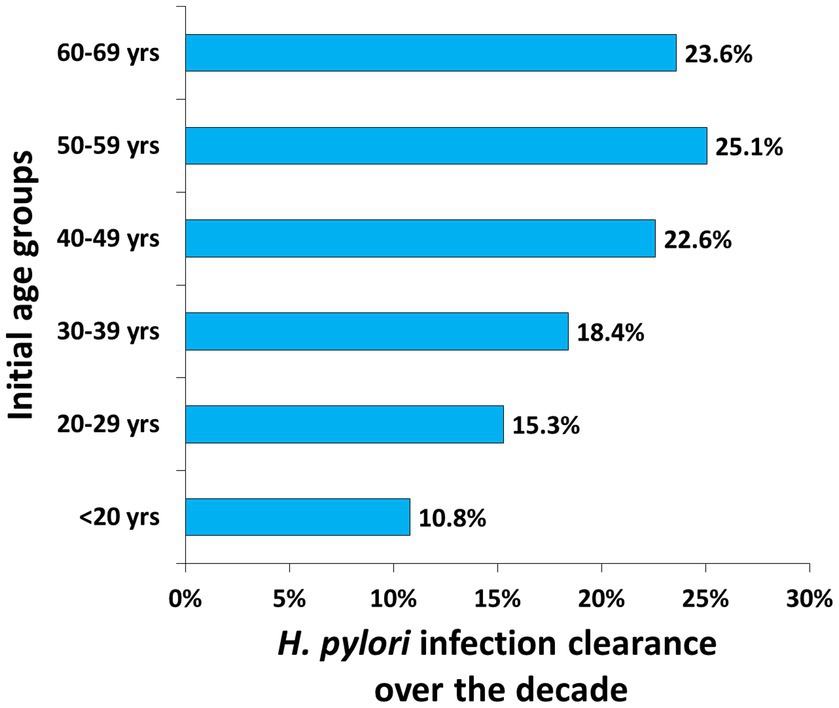
Results: The overall prevalence of H. pylori dramatically decreased from 53.1% to 30.7% over the past decade (OR = 0.39, 95% CI 0.37–0.41), with a similar decline in all sex-specific and age-specific subgroups. The age-specific prevalence consistently increased before 40 years of age and always peaked at 50–59 years. Longitudinal clearance increased along with aging, and prevalence dropped to 22.6%, 25.1%, and 23.6% in the 40–49, 50–59, and 60–69 years initial age groups, respectively.
Conclusion: The generalization of H. pylori screening and eradication could greatly contribute to the control of H. pylori infection among urban health check-up populations and lower gastric cancer incidence.
Introduction
The incidence of and mortality from gastric cancer has been high in China over recent decades (1). H. pylori is the major risk pathogen for gastric cancer in eastern and western populations (2, 3). A nationwide decision-making analysis in China suggested that H. pylori eradication is a cost-saving strategy, with general annual endoscopic screening dominating other protocols (4). Targeted and tailored endoscopic screening among high-risk subpopulations could be more cost-effective from a willingness-to-pay perspective (4). Additionally, it has been highlighted that active H. pylori eradication through the organized screening and surveillance of high-risk subpopulations should be a systematic measure for controlling gastric cancer-specific mortality, especially in high-risk areas. In China, extensive screening of H. pylori has been practiced more commonly in recent years along with updated health policy (5, 6), and infected individuals are consequently actively advised and treated for H. pylori eradication. Therefore, this study aimed to assess the efficacy of the updated health policy in improving and extending H. pylori screening and eradication in China.
Methods
To evaluate the extensive screening and eradication of H. pylori in a macroscopic view, we longitudinally observed the prevalence of H. pylori in health check-ups over the past decade at the Health Management Center of West China Hospital, a central high-volume hospital in southwest China. The targeted populations included self-reported asymptomatic observations from health check-ups. The health check-ups were organized by certain public institutions or enterprises, as well as a few people from urban areas. The 14C-urea or 13C-urea breath test (UBT) was used for H. pylori detection.
Crude data were retrieved from three cross-sectional studies (two published and one unpublished) in the periods 2009–2010, 2013–2014, and 2019–2021, respectively (7, 8). The sex-specific and age-specific prevalence of H. pylori was calculated. Odds ratios (OR) and 95% confidence intervals (CI) were estimated where applicable. Additionally, Ptrend values were tested over the decade. The longitudinal H. pylori infection clearance of each initial age group was estimated, i.e., the prevalence difference between the periods 2019–2021 and 2009–2010.
The protocol has been reported elsewhere (PROSPERO Registration Number: CRD42019120764) (9). The Sichuan Gastric Cancer Early Detection and Screening (SIGES) study was approved by the Biomedical Ethical Committee of West China Hospital, Sichuan University (id: 2015-151-V2; 2018-215-V1).
Results
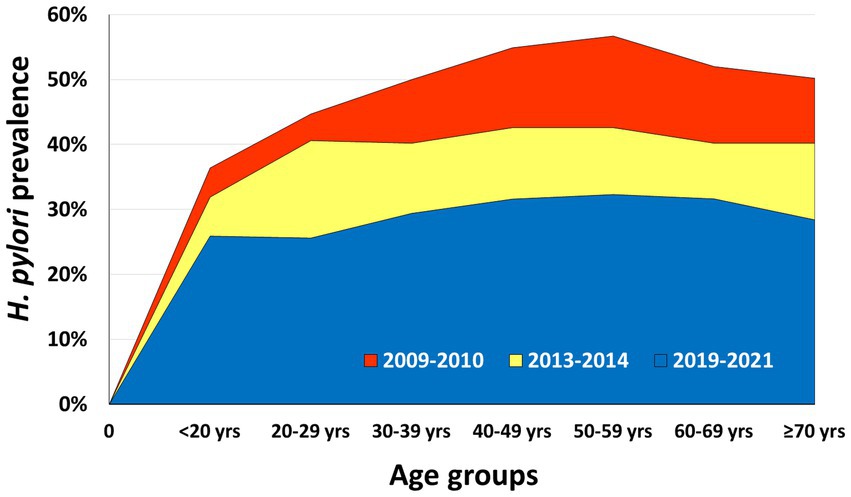
In the periods 2009–2010, 2013–2014, and 2019–2021, 8,365, 16,914, and 18,281 observations from health check-ups were analyzed, respectively. The overall prevalence of H. pylori dramatically decreased from 53.1% to 30.7% over the past decade among urban health check-up populations (OR = 0.39, 95% CI 0.37–0.41; Ptrend < 0.0001) (Table 1; Figure 1).
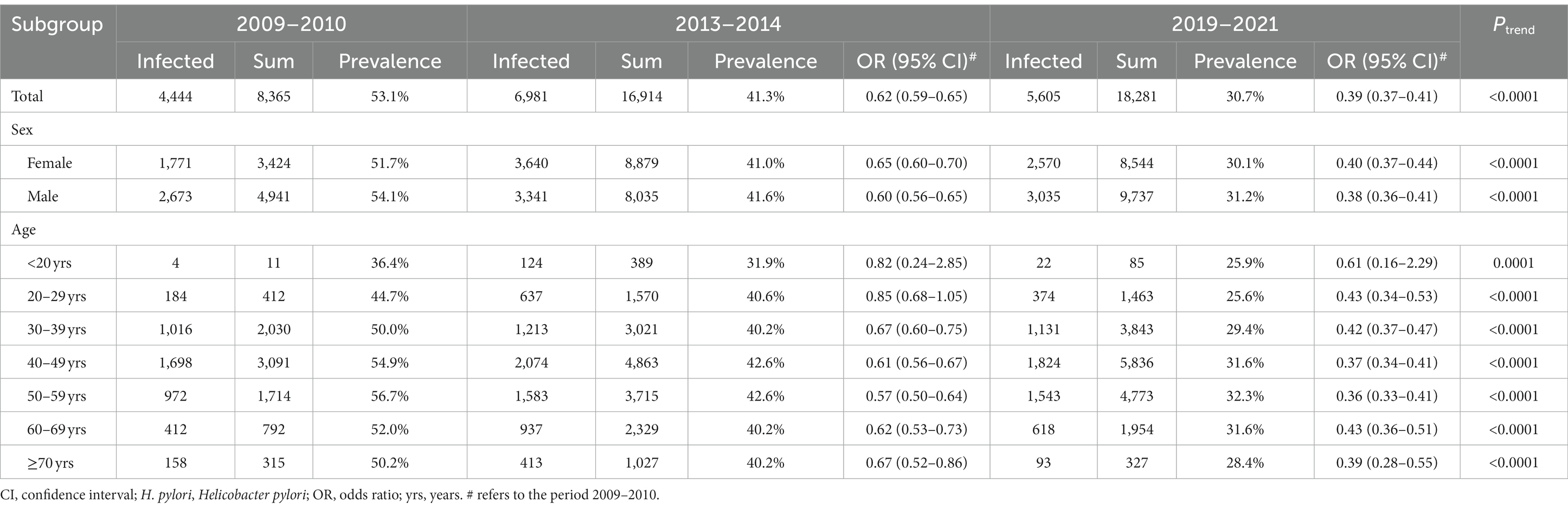
Table 1. The 10-year trend of H. pylori infection prevalence among the urban health check-up population in Chengdu.
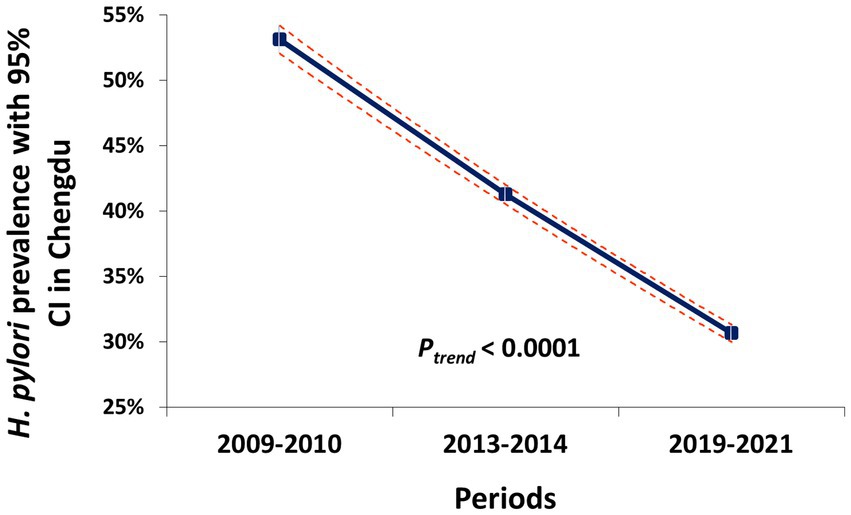
Figure 1. The prevalence trend of H. pylori infection among the urban health check-up population in Chengdu.
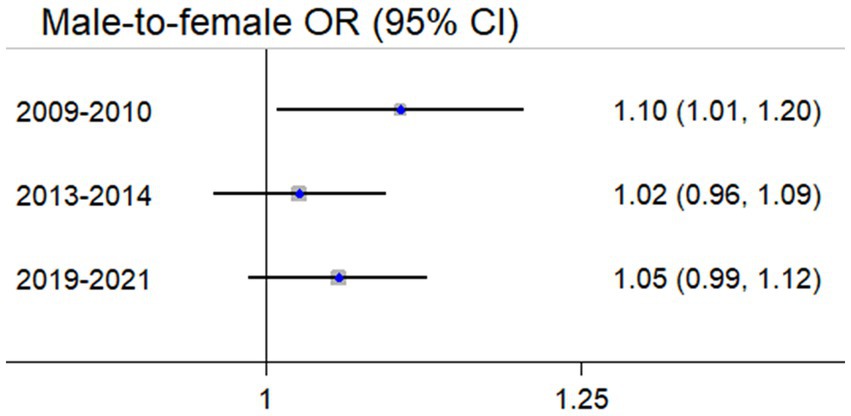
A similar decreasing trend in sex-specific and age-specific subgroups was simultaneously observed (Table 1). H. pylori prevalence in males was previously higher than that of females but the difference became insignificant in the recent period (OR = 1.05, 95% CI 0.99–1.12) (Figure 2). The age-specific H. pylori prevalence consistently increased before 40 years old, and always peaked at 50–59 years (Figure 3).
Accordingly, the longitudinal clearance of H. pylori infection increased with age, and prevalence dropped to 22.6%, 25.1%, and 23.6% in the 40–49 years, 50–59 years, and 60–69 years initial age groups, respectively (Figure 4).
Discussion
These findings confirm that the promotion of extensive H. pylori screening in health check-ups and eradication in general practice among urban health check-up populations can greatly contribute in decreasing the prevalence of H. pylori among any sex-specific or age-specific subpopulation in the long term. The 40–69-year-old age group has a heavier load of H. pylori infection, and therefore may have a stronger willingness to eradicate H. pylori (extrapolated due to greater clearance rate over the decade). Extensive UBT has a moderate predictive strength in gastric cancer screening and might be more cost-effective in the middle-aged subpopulation (40–59 years) (10).
Globally, a worldwide meta-analysis of 2,979,179 individuals from 71 countries or regions showed that the global overall prevalence of H. pylori infection decreased from 58.2% (1980–1990 period) to 43.1% (2011–2022 period), with a particularly sharp decline between 2011 and 2022 (11). Lower prevalence was associated with younger age, high-income countries, countries with a high level of health coverage, etc. (11). However, despite the dramatic decrease in our study, a meta-analysis of the domestic prevalence of H. pylori infection analyzed 670,572 participants from 26 provinces in China during the period 1983–2018, and found the overall prevalence slowly declined by only 0.9% per year (12). Another similar meta-analysis reported a decreased rate from 41.8% (2010–2014 period) to 40.0% (2015–2019 period) (13). A narrative comparison of the changes between worldwide and nationwide prevalence indicated that H. pylori infection control in China might be behind the global average efficacy. Therefore, the burden of H. pylori infection continues to be highly significant in China.
According to the recently released White Paper on H. pylori infection in China, the trend of overall prevalence declined gradually to below 50% between 1983 and 2018 (14). Furthermore, the prevalence was diverse among different subpopulations (between 35.4% and 66.4%), with higher rates in rural and adult subpopulations (14). The major reason for those changes was the rapid economic and societal development in China, as well as the obvious improvement in the public and medical health situation. Consequently, universal education, particular regarding health, increased the understanding and awareness of the importance of H. pylori screening and eradication. Updating the consensus on H. pylori eradication improved the capacity of the standardized and individualized management of H. pylori infection within the healthcare system. Crucial diagnostic tests were widely used and resistant strain detection techniques spread. The primary prevention of gastric cancer by population-based H. pylori eradication was piloted in many areas with a high incidence of gastric cancer.
Particularly, this improvement in H. pylori infection control may be attributed to the health policy of extending H. pylori screening and eradication in the Chinese population (15). The Chinese National Consensuses on the management of H. pylori infection were commonly updated following the serial Maastricht consensuses (16–18). The Third Chinese National Consensuses firstly accepted the eradication indication, including the asymptomatic but infected candidates. After the Kyoto global consensus (19), the Fifth Chinese National Consensuses recommended the eradication for all infected persons (5). Additionally, the Fifth Chinese National Consensuses emphasized health education and public awareness of gastric cancer control involving H. pylori screening and eradication. Therefore, these main changes improved H. pylori infection control in the Chengdu urban area over the past decade, and domestic updates in relevant health policy may be beneficial to gastric cancer prevention and control. In China in particular, it may be predicted that the inflammatory mechanism (i.e., H. pylori-associated atrophic gastritis) associated with gastric cancer would be controlled alone with the declining public prevalence of H. pylori (20).
Therefore, the routine screening of H. pylori was included in the health check-up of the urban population in West China Hospital for more than a decade, and infected persons were commonly recommended standardized intervention and surveillance. The major reason for the rapid decrease in our report could be the high-selected feature of urban observations. Education level, self-awareness of health management, and willingness to participate in H. pylori screening and eradication should be apparently higher among the observations than the average level of the common population. The imbalance between urban and rural areas limits the overall declining rate of H. pylori prevalence.
Wang, et al. used a Markov model to predict the incidence of and mortality from gastric cancer during the period 2021–2035 among Chinese people born between 1951 and 1980 (4). The various protocols of H. pylori eradication and endoscopic screening and surveillance were evaluated regarding their affordability and cost-effectiveness from the perspective of nationwide gastric cancer prevention. We believe primary and secondary prevention must be fairly important with regard to gastric cancer achieving the nationwide goal of an improvement of 5-year overall survival by 15% between 2016 and 2030 in China (10, 21). However, the low proportion of early gastric cancer (generally no more than 20%) is still a difficulty in improving population survival outcome of gastric cancer in China (22).
Some limitations of the present study need to be considered. First, this analysis included extracted data from two published studies, and thus, the relevant original data were unavailable to estimate the proportion of repeated observations within three periods. Second, the health check-up population in West China Hospital was almost entirely composed of staff from public institutions and urban enterprises. Therefore, it does not reflect the overall domestic prevalence situation. Last, the exact rates and details of eradication in separate cross-sections were unavailable, and therefore, no further understanding and evaluation of eradication could be obtained in this study.
In short, this research confirmed that the updated health policy of extending H. pylori screening and increasing eradication could greatly contribute in decreasing the long-term prevalence of H. pylori among urban health check-up populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the study was approved by the Biomedical Ethical Committee of West China Hospital, Sichuan University (id: 2015-151-V2; 2018-215-V1). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
J-CZ and M-YW for the data collection and analysis. X-ZC and YH for the study conception and conduction. X-ZC for the writing. J-KH for the academic inspection. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Foundation of Science and Technology Department of Sichuan Province, China (23ZDYF0839); the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University, China (ZY2017304); and the Medical Research Project of Yibin Health Commission, Yibin, China (2021-34).
Acknowledgments
The authors thank the Sichuan Gastric Cancer Early Detection and Screening (SIGES) project and the substantial work of the Volunteer Team of Gastric Cancer Surgery (VOLTGA), West China Hospital, Sichuan University, China. The study was accepted as a poster presentation by the International Gastric Cancer Congress (IGCC) 2023, Yokohama, Japan, June 14–17, 2023.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chen, XZ, Liu, Y, Wang, R, Zhang, WH, and Hu, JK. Improvement of cancer control in mainland China: epidemiological profiles during the 2004–10 National Cancer Prevention and control program. Lancet. (2016) 388:S40. doi: 10.1016/S0140-6736(16)31967-5
2. Wang, R, and Chen, XZ. High mortality from hepatic, gastric and esophageal cancers in mainland China: 40 years of experience and development. Clin Res Hepatol Gastroenterol. (2014) 38:751–6. doi: 10.1016/j.clinre.2014.04.014
3. Chen, XZ, Schöttker, B, Castro, FA, Chen, H, Zhang, Y, Holleczek, B, et al. Association of helicobacter pylori infection and chronic atrophic gastritis with risk of colonic, pancreatic and gastric cancer: a ten-year follow-up of the ESTHER cohort study. Oncotarget. (2016) 7:17182–93. doi: 10.18632/oncotarget.7946
4. Wang, Z, Han, W, Xue, F, Zhao, Y, Wu, P, Chen, Y, et al. Nationwide gastric cancer prevention in China, 2021–2035: a decision analysis on effect, affordability and cost-effectiveness optimisation. Gut. (2022) 71:2391–400. doi: 10.1136/gutjnl-2021-325948
5. Liu, WZ, Xie, Y, Lu, H, Cheng, H, Zeng, ZR, Zhou, LY, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. (2018) 23:e12475. doi: 10.1111/hel.12475
6. Du, Y, Zhu, H, Liu, J, Li, J, Chang, X, Zhou, L, et al. Consensus on eradication of helicobacter pylori and prevention and control of gastric cancer in China (2019, Shanghai). J Gastroenterol Hepatol. (2020) 35:624–9. doi: 10.1111/jgh.14947
7. Huang, Y, Xu, Y, Zeng, L, Qin, K, Yang, Y, Zou, TF, et al. Investigation on the H pylori infection and risk factors among physical examinees in Chengdu. Modern Prev Med. (2012) 39:3494–7. (In Chinese)
8. Wang, R, Zhang, MG, Chen, XZ, and Wu, H. Risk population of Helicobacter pylori infection among Han and Tibetan ethnicities in western China: a cross-sectional, longitudinal epidemiological study. Lancet. (2016) 388:S17. doi: 10.1016/S0140-6736(16)31944-4
9. Wang, R, Bai, D, Xiang, W, Zhang, YF, Ba, KY, Chen, XZ, et al. Helicobacter pylori prevalence in the southwest of China: a protocol for systematic review. Medicine. (2020) 99:e19369. doi: 10.1097/MD.0000000000019369
10. Xiang, W, Wang, R, Bai, D, Yu, TH, and Chen, XZ, on behalf of the SIGES Research Groups. Helicobacter Pylori related gastric cancer screening and cost-effectiveness analysis: a hospital-based cross-sectional study (SIGES). Nutr Cancer. (2022) 74:2769–78. doi: 10.1080/01635581.2021.2022168
11. National Institute for Communicable Disease Control and Prevention of Chinese Center for Disease Control and Prevention . White Paper on Prevention and Control of Helicobacter pylori Infection in China. Beijing (2023): 1–47. Available at: https://icdc.chinacdc.cn/zxxx/gzdt/202306/P020230603733005731810.pdf (In Chinese)
12. Li, M, Sun, Y, Yang, J, de Martel, C, Charvat, H, Clifford, GM, et al. Time trends and other sources of variation in Helicobacter pylori infection in mainland China: a systematic review and meta-analysis. Helicobacter. (2020) 25:e12729. doi: 10.1111/hel.12729
13. Ren, S, Cai, P, Liu, Y, Wang, T, Zhang, Y, Li, Q, et al. Prevalence of Helicobacter pylori infection in China: a systematic review and meta-analysis. J Gastroenterol Hepatol. (2022) 37:464–70. doi: 10.1111/jgh.15751
14. Li, Y, Choi, H, Leung, K, Jiang, F, Graham, DY, and Leung, WK. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. (2023) 8:553–64. doi: 10.1016/S2468-1253(23)00070-5
15. Zou, JC, Yang, Y, and Chen, XZ, Sichuan Gastric Cancer Early Detection and Screening research group. Active eradication of Helicobacter pylori within organized massive screening might improve survival of gastric cancer patients. Gastroenterology. (2023) 164:162–3. doi: 10.1053/j.gastro.2022.05.009
16. Malfertheiner, P, Megraud, F, O'Morain, C, Bazzoli, F, el-Omar, E, Graham, D, et al. Current concepts in the management of Helicobacter pylori infection: the Maastricht III consensus report. Gut. (2007) 56:772–81. doi: 10.1136/gut.2006.101634
17. Malfertheiner, P, Megraud, F, O'Morain, CA, Atherton, J, Axon, ATR, Bazzoli, F, et al. Management Of helicobacter pylori infection—the Maastricht IV/ Florence consensus report. Gut. (2012) 61:646–64. doi: 10.1136/gutjnl-2012-302084
18. Malfertheiner, P, Megraud, F, O'Morain, CA, Gisbert, JP, Kuipers, EJ, Axon, AT, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut. (2017) 66:6–30. doi: 10.1136/gutjnl-2016-312288
19. Sugano, K, Tack, J, Kuipers, EJ, Graham, DY, el-Omar, EM, Miura, S, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. (2015) 64:1353–67. doi: 10.1136/gutjnl-2015-309252
20. Wang, R, and Chen, XZ. Prevalence of atrophic gastritis in Southwest China and predictive strength of serum gastrin-17: a cross-sectional study (SIGES). Sci Rep. (2020) 10:4523. doi: 10.1038/s41598-020-61472-7
21. Wang, R, Bai, D, Xiang, W, and Chen, XZ, on behalf of SIGES research group. Tibetan ethnicity, birthplace, Helicobacter pylori infection, and gastric cancer risk. Am J Gastroenterol. (2022) 117:1010. doi: 10.14309/ajg.0000000000001757
Keywords: gastric cancer, Helicobacter pylori , epidemiology, screening, health policy
Citation: Zou J-C, Wen M-Y, Huang Y, Chen X-Z and Hu J-K (2023) Helicobacter pylori infection prevalence declined among an urban health check-up population in Chengdu, China: a longitudinal analysis of multiple cross-sectional studies. Front. Public Health. 11:1128765. doi: 10.3389/fpubh.2023.1128765
Edited by:
Dmitry Bordin, A. S. Loginov Moscow Clinical Scientific Centre, RussiaReviewed by:
Marja-Liisa Hänninen, University of Helsinki, FinlandJinhui Li, Stanford University, United States
Copyright © 2023 Zou, Wen, Huang, Chen and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-Zu Chen, Y2hlbnhpbnp1QHNjdS5lZHUuY24=; Yan Huang, aHVhbmd5YW5oeTUxM0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Jin-Chen Zou1,2†
Jin-Chen Zou1,2† Yan Huang
Yan Huang Xin-Zu Chen
Xin-Zu Chen Jian-Kun Hu
Jian-Kun Hu