- 1Department of Otorhinolaryngology, Head, and Neck Surgery, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Epidemiology and Health Statistics, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 3Department of Outpatient Nursing, Dazhou Central Hospital, Dazhou, China
- 4Department of Otorhinolaryngology, Head, and Neck Surgery, Santai People's Hospital, Mianyang, China
Background: Population knowledge and attitudes toward obstructive sleep apnea (OSA) syndrome are critical to public health initiatives to overcome the disease. Healthcare education is an appropriate approach to expediting the process to build active medical practice models in the public.
Objective: This study aimed to assess the level of knowledge, attitude, and practice (KAP) regarding OSA and healthcare education demand among the Chinese general population.
Methods: A cross-sectional survey was performed online via Wenjuanxing in China between 8 February and 8 March 2022, using a 34-item questionnaire designed and reviewed by multidisciplinary experts.
Results: This study enrolled 1507 respondents, aged 18 to 68, with a city-to-countryside ratio of approximately 2:1. Four-fifths of respondents reported that they had children (n = 1237), and mothers accounted for 57.7%. If they or their children had symptoms of OSA, nearly nine in 10 respondents would undertake positive medical practices, especially parents. A total of 89.4% of the respondents reported a desire to receive healthcare education through the new multimedia approach, and most were concerned about the etiology of OSA.
Conclusion: The current study indicated that even the higher educated and urban populations in China had insufficient knowledge about positive attitudes toward and practices regarding OSA, indicating an urgent demand for healthcare education. A special emphasis should be placed on appropriating population demand for healthcare education and promoting the benefits of active medical practice models in sleep medicine.
1. Introduction
Obstructive sleep apnea (OSA) is a group of sleep breathing disorders involving both sexes and all ages. It is characterized by recurrent, intermittent upper airway obstruction, or reduced airflow during sleep, leading to repetitive episodes of desaturation, hypercapnia, and arousal (1). Adult patients with OSA typically complain of loud snoring, witnessed apnea, fragmented unrefreshing sleep, and daytime hypersomnolence. OSA is associated with a series of short-term and long-term negative consequences (2). If untreated, it not only can reduce patients' work efficiency and quality of life but also can relate to the occurrence and progression of chronic cardiovascular and metabolic diseases and neurocognitive problems and can increase the risk of all-cause mortality (3–5). The clinical presentation of children is different from that of adults, and pediatric patients with OSA often present with mouth breathing, nocturnal snoring and sweating, enuresis, and restless sleep (6, 7). Secondary to OSA, a myriad of negative consequences severely affect children's and teenagers' facial appearance and quality of life, such as adenoid face, poor school performance, possible depression, growth defects, and neurocognitive dysfunction (7–9).
The main risk factors for OSA are obesity and aging, which have increased in a striking proportion worldwide over the past four decades (10). Consequently, vulnerability to OSA has increased, affecting nearly one billion people or one in seven adults worldwide (11). Therein, the affected general population of China ranks at the top of the global list, with a prevalence of more than 23.6% among adults older than 30 years of age (11). However, as previous surveys have reported, the incidence of OSA has remained underestimated, and the undiagnosed proportion was 75 to 90% in the US (12, 13). In addition, the undiagnosed condition contributed to an enormous global healthcare burden, causing the social level costs to amount to more than $150 billion per year in the US (10, 14, 15), and medical costs up to €10.7 to €32.0 billion per year in Italy were due to OSA (16).
Considering the prevalence and negative effects of OSA on health, medical workers have paid more attention to OSA in various countries (17–19). Effective screening and early recognition performed by healthcare providers are needed to minimize the negative health impacts and maximize cost-effectiveness (11). The absence of awareness of the serious adverse effects of OSA among the general population results in people's unwillingness to be evaluated. However, previous studies have indicated that the current knowledge of and attitudes about OSA are insufficient among medical service providers (20–24). A survey performed in 2017 with a large sample of 1306 participants found that only 13.0% of participants could correctly define OSA (3). Xu et al. (25) conducted a descriptive study of childhood OSA in 2019 focused on parents in the Guangdong Province of China, suggesting that parents had limited awareness of its complications.
However, there is a paucity of data with large-scale samples focused on China regarding the knowledge, attitude, and practice (KAP) regarding OSA and healthcare demand among the general population. The purpose of this study was to evaluate the current KAP level and to investigate the education demand for OSA among the Chinese general population. In addition, we further explored the influencing factors for seeking medical help to determine whether there were correlations between the demographic data and medical practice patterns.
2. Methods
2.1. Participants
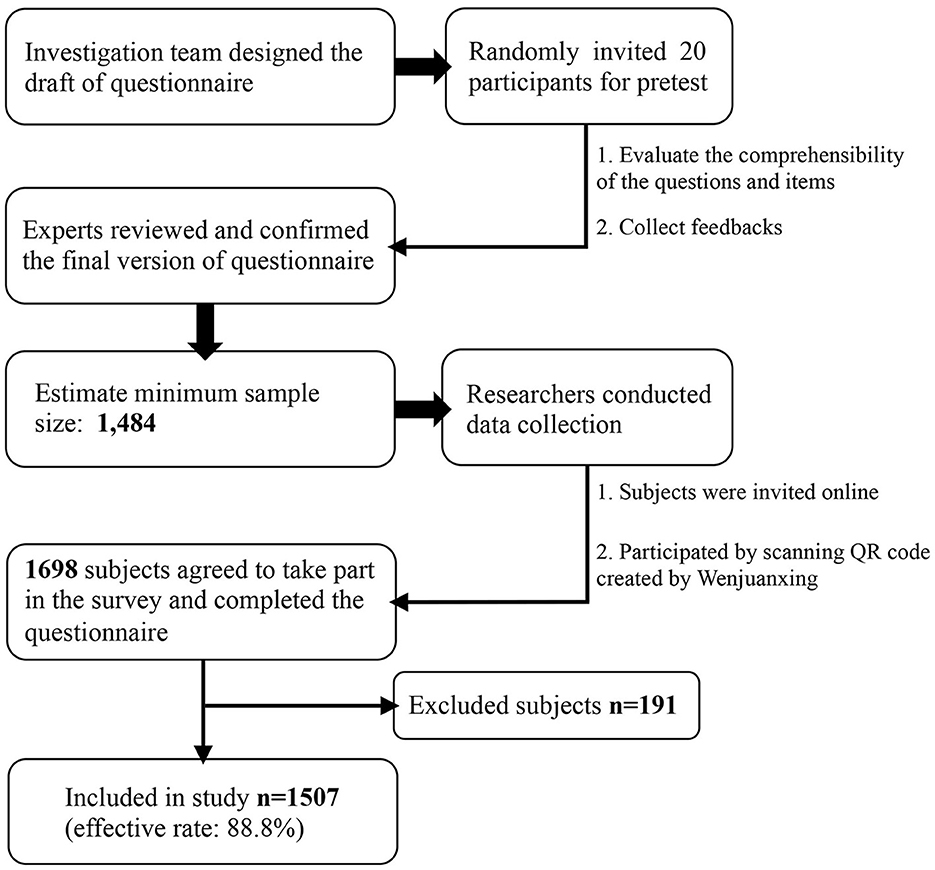
Before distributing the survey, the minimum sample size was calculated using G*Power (version 3.1; Heinrich Heine University) to achieve a power of 0.80. In the G*Power software, a logistic regression test was conducted for a priori power calculation with an odds ratio (OR) of 1.2 and a significance level of.05. The minimum sample needed to achieve a power of 0.80 was 1484 for our study. Considering the missing and non-responsive cases, we expanded it by 10%, yielding a predicted sample size of 1632. In the present study, the population focused on general adult residents who were from China, were at least 18 years old, and were competent to answer the questions online. Those who were illiterate or unwilling to participate were not invited. In the process of data screening, the inclusion criteria were Chinese residents ≥ 18 years old who volunteered to participate and were competent to comprehend the content of the questionnaire. Those who answered contradictory or factual content or had a response time of ≤ 180 s were excluded.
2.2. Ethics approval
Ethical approval regarding human subject research was obtained from the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (approval number: 2022.416). Informed consent was obtained from each participant online by placing a question about their agreement to participate in the study at the beginning of the survey. Participants were assured of the confidentiality and anonymity of this study and their rights to exit at any time. We declare that the data were collected for academic use only.
2.3. Instrument
The primary version of the questionnaire was developed in Chinese by an investigation team based on a deep literature review of comparable studies and international guidelines (3, 25–28), including otolaryngologists, medical sociologists, and a statistician. Researchers randomly invited 20 participants face-to-face from the general population to answer the questionnaire online for pretext and collected their feedback about the comprehensibility of questions and options. Four experts in the field of sleep medicine and survey studies reviewed these responses and each item of the survey and confirmed the final version of a 34-item questionnaire (see Supplementary material). The face validity and content validity of the survey were established. It comprised basic demographic data and four sections about knowledge, attitudes, practices, and demand regarding popular healthcare toward OSA. A series of options were listed with points for each question and zero for ignorance or mistakes. The total scores for symptoms, examinations, complications, and treatments in OSA were 13, 5, 12, and 9, respectively. Cronbach's α was >0.7 for each scale (0.885 for symptoms, 0.738 for examinations, 0.863 for complications, and 0.835 for treatments for OSA).
2.4. Procedures
The cross-sectional survey was conducted in China between 8 February and 8 March 2022, using a 34-item questionnaire designed and reviewed by multidisciplinary experts (Figure 1). The general Chinese adult population was randomly invited online and offline. Participants were informed that the survey was based on voluntary principles and that their data would be anonymous and confidential. First, our investigation team created a questionnaire QR code (quick response code or dimensional barcode) by Wenjuanxing (https://www.wjx.cn), which is an online questionnaire platform widely used in academic studies in China. Then, researchers distributed the QR code using Chinese popular social media to get access to the general populations as many as possible, including WeChat (https://web.wechat.com) and QQ (https://www.qq.com). In addition, five researchers performed face-to-face invitations to scan the QR code in possible surveyed populations in different public scenarios, such as hospitals, universities, and commercial venues. Participants' IP addresses were restricted to ensure only one submission. The chief researcher was responsible for checking the collected data from Wenjuanxing, and up to 11.2% of submitted questionnaires were excluded for invalid response times and logistic errors.
2.5. Statistical analysis
The data are summarized as the means and standard deviations for continuous variables and percentages for categorical variables. Comparisons between groups were performed with the t-test and chi-square test. Univariate (unadjusted) and multivariate logistic regression models (adjusted for confounders) were applied to assess the associations between various demographic factors and the practice of seeking medical help for OSA. All statistical analyses were performed using IBM SPSS statistics software (version 26.0) and two-sided tests at a 5% level of significance (p < 0.05).
3. Results
3.1. Baseline characteristics of respondents
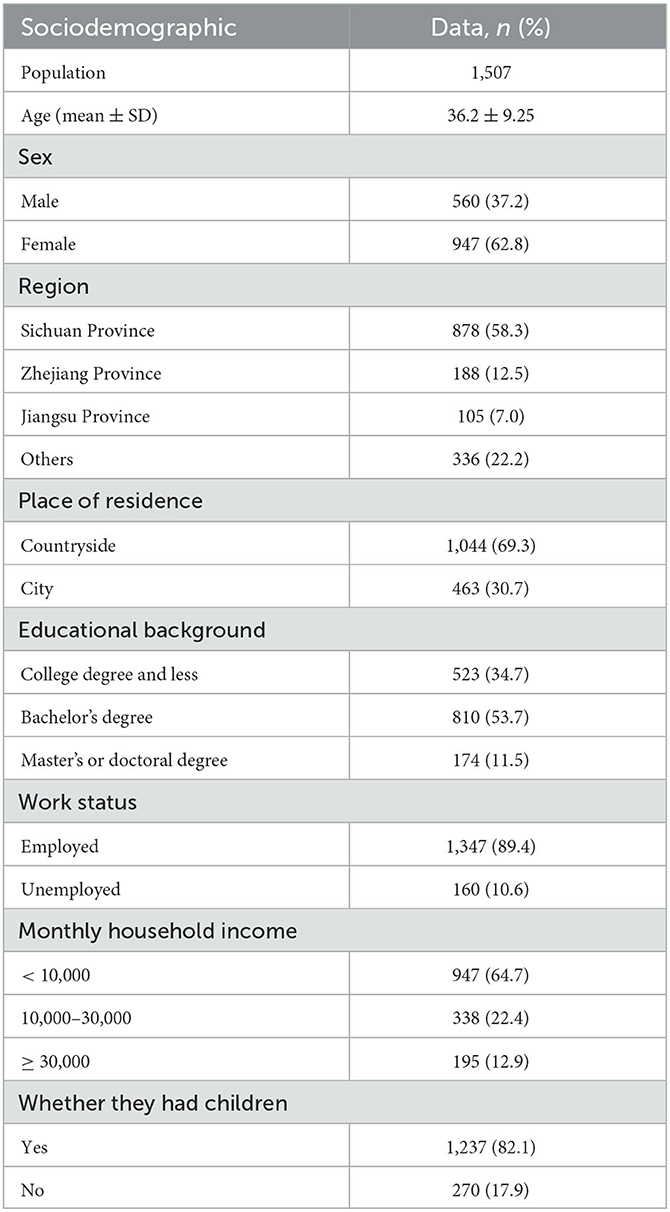
This study enrolled 1507 respondents (560 men and 947 women), their ages ranged from 18 to 68 years, and they came from 28 provinces, autonomous regions, and municipalities (including Sichuan, Zhejiang, Jiangsu, Liaoning, Fujian, Shandong, and Anhui provinces). The respondents' characteristics are shown in Table 1. Among employed respondents (n = 1,347), majors in medicine numbered 40.9%. Four-fifths of respondents reported that they had children (n = 1,237), mothers accounted for 57.7%, and fathers ranked second (36.5%).
3.2. Knowledge of OSA
When asked whether they had heard of OSA, 62.8% of respondents said they had only heard of it or knew little, and 292 respondents reported that they had never heard of it. Nevertheless, the majority regarded OSA as a severe disease (76.0%). In the description of OSA, only 37.2% of respondents answered all four questions correctly (Table 2). In particular, the description of “Untreated OSA would increase the morbidity of traffic accidents” at 68.5% correct was the lowest.
Regarding diagnostic methods in OSA, the respondents were asked to identify the symptoms, examinations, and complications that those suffering from OSA might have, as shown in Figure 2. The average awareness rate of symptoms of OSA was the highest (60.9%), followed by the examination method (55.6%), and the complication rate was only 50.6%. In particular, nocturia more than once per night (44.3%) and bed-wetting in children (44.1%) were the most neglected symptoms of OSA. Approximately 40.5% of respondents could determine that X-rays are commonly used to diagnose OSA. Among its complications, <40% of respondents associated spinal dysplasia, diabetes, and hyperlipidemia with OSA. For the treatment of OSA, the average awareness rate was 55.9%, and continuous positive airway pressure was the most underrated treatment in the general public (46.7%) (Figure 2).
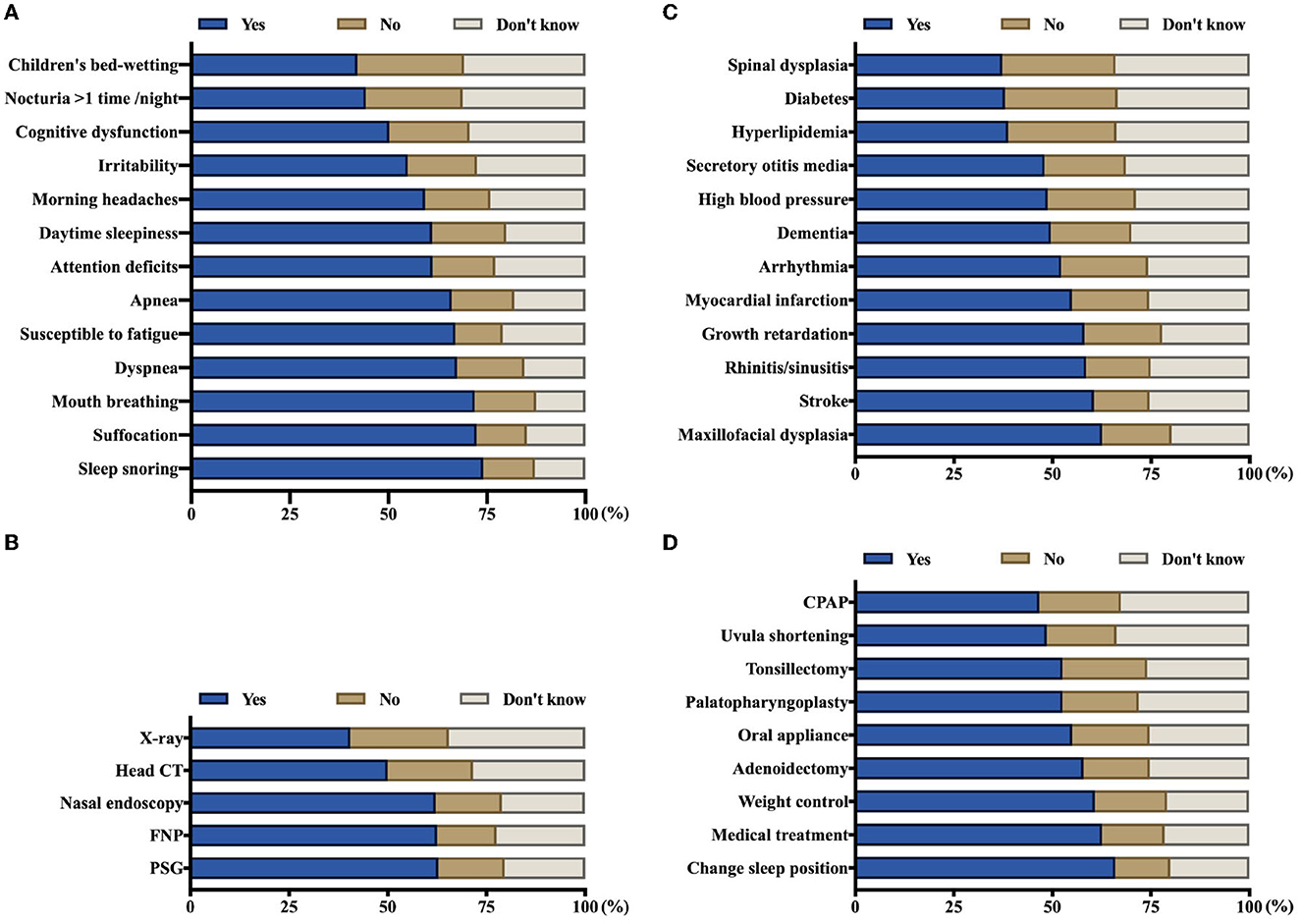
Figure 2. Awareness rate of symptoms, examinations, complications, and treatments among the general population, corresponding to parts (A–D) respectively (N = 1507). FNP, flexible nasopharyngoscopy; PSG, polysomnography; CPAP, continuous positive airway pressure.
3.3. Attitudes and practices in OSA
When asked if they had symptoms of OSA and whether they sought medical help, most of the participants answered positively (87.6%), and they were most likely to visit the otolaryngology and respiratory medicine clinics. For parents, 95.6% of them indicated that they would take their children to see doctors if their child or children had related presentations (n = 1,237). A total of 73.3% of parents also chose to see otolaryngologists, only 39.5% of them chose pediatricians, and several participants referred to sleep medicine, departments of neurology, and traditional Chinese medicine. Regarding the reasons why they did not seek medical advice, more than half of them regarded OSA as a non-fatal disease, as shown in Table 3.
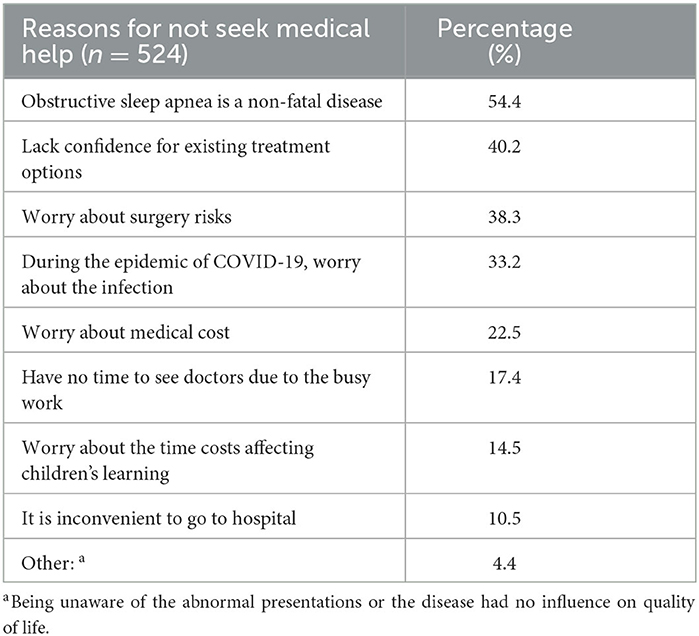
Table 3. Percentage of various reasons why they did not seek medical help when they had symptoms of OSA.
A total of 24.1% of respondents indicated they had a previous diagnosis of OSA, and 42.0% of parents reported that their children had been diagnosed with OSA. Among these children with OSA (n = 519), 42.2% had received conservative therapy, 28.1% had undergone surgical treatment, and 29.5% never had any intervention. Tonsillectomy and adenoidectomy were the most common surgeries they reported (65.8%, n = 146).
3.4. Healthcare education demand of OSA
Nine in 10 (89.4%) of the respondents were willing to receive popular healthcare education about OSA, and the most common referred content that they were eager to receive consisted of the causes, symptoms, complications, and treatment of OSA (74.9%). Some child caregivers reported that they wanted to differentiate OSA from benign snoring. Another wondered whether there were any effective methods to prevent this disease. In terms of the channels to access this healthcare information, the internet/new media and the healthcare delivery produced by medical professionals were the preferred outlets (68.3 and 67.0%, respectively).
3.5. Analysis of the factors influencing the KAP of OSA
In this study, the items of symptoms, examinations, complications, and treatments in OSA were accumulated scores as the baseline data. The comparison between these scores that showed significant differences in sex, age, educational background, household income, occupational background, and residence is shown in Figure 3. In the present study, respondents who were women, ≥ 40 years of age, had a bachelor's degree or more, had <10,000 yuan monthly household incomes, had a related medical occupation, and lived in a city with higher scores in OSA knowledge. The total scores of the four sections showed no significant differences in whether seeking medical advice when one's children had presentations of OSA (p = 0.085). To examine the influencing factors associated with seeking medical advice, the variables of interest were tentatively incorporated into a regression model (Table 4). In the multivariate regression, many demographic and individual factors independently influenced the practices regarding OSA among the general population. The results showed that the respondents with > 30,000 yuan monthly household incomes had a higher odds ratio for active practice regarding OSA (adjusted OR = 4.621, p = 0.001) compared to those in lower income groups (< 10,000 yuan). Additionally, the people who lived in the city had a higher odds ratio for seeking medical advice for OSA than those who lived in the countryside (adjusted OR = 2.789, p < 0.001). Respondents who had a prior diagnosis of OSA and had a positive attitude toward healthcare education were significantly more likely to seek medical advice on their own initiative (p < 0.001). In contrast, sex, age, educational and occupational background, and scores in the four sections of knowledge about OSA did not significantly affect their medical practice (p > 0.05).
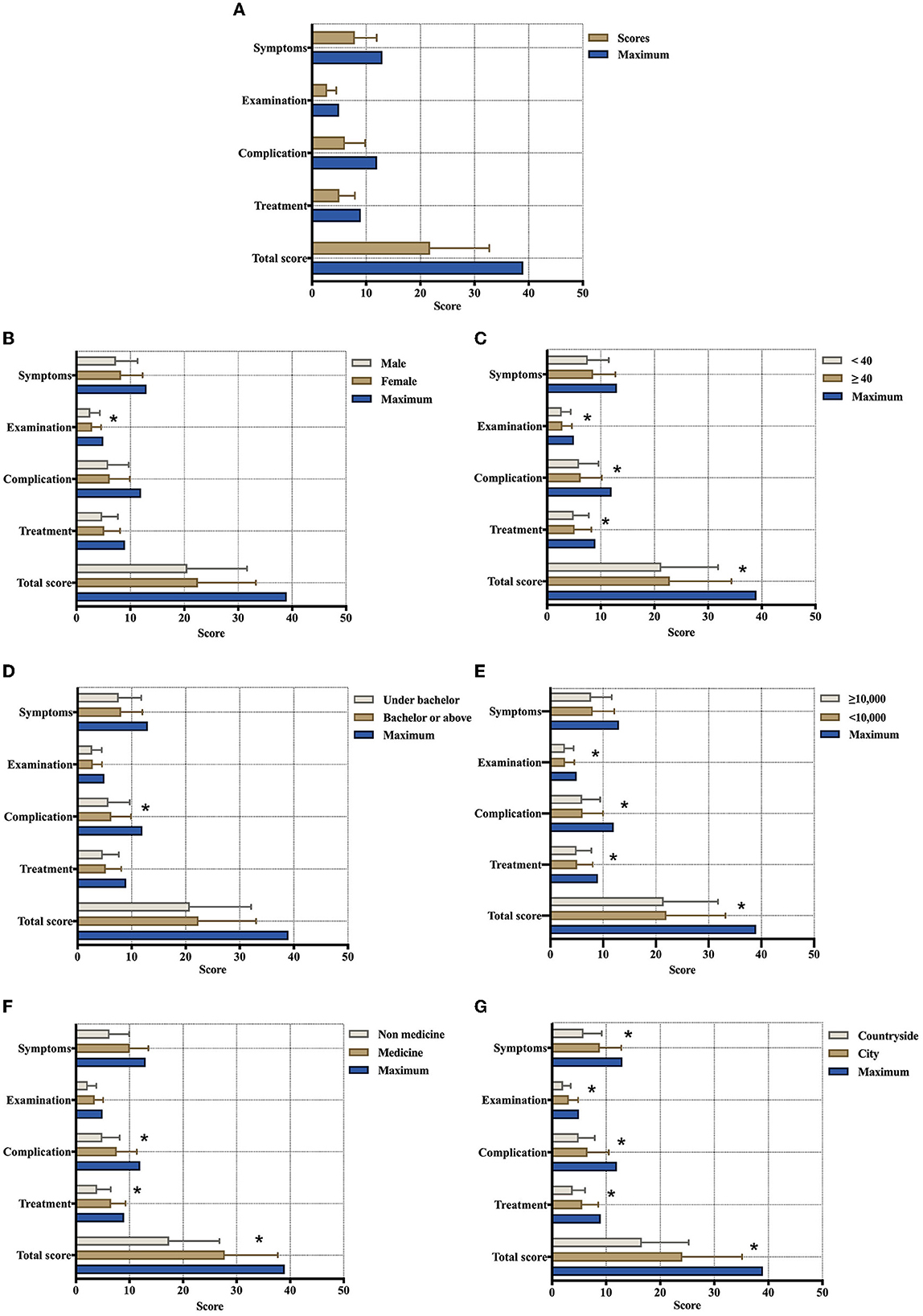
Figure 3. Various subgroups of scores in the symptoms, examinations, complications, and treatments of OSA among the general population. (A) Baseline full scores; (B) sex groups; (C) age groups; (D) educational groups; (E) monthly household income groups; (F) occupational groups (n = 1347); and (G) residential place groups (N = 1,507; *Indicates a significant difference).
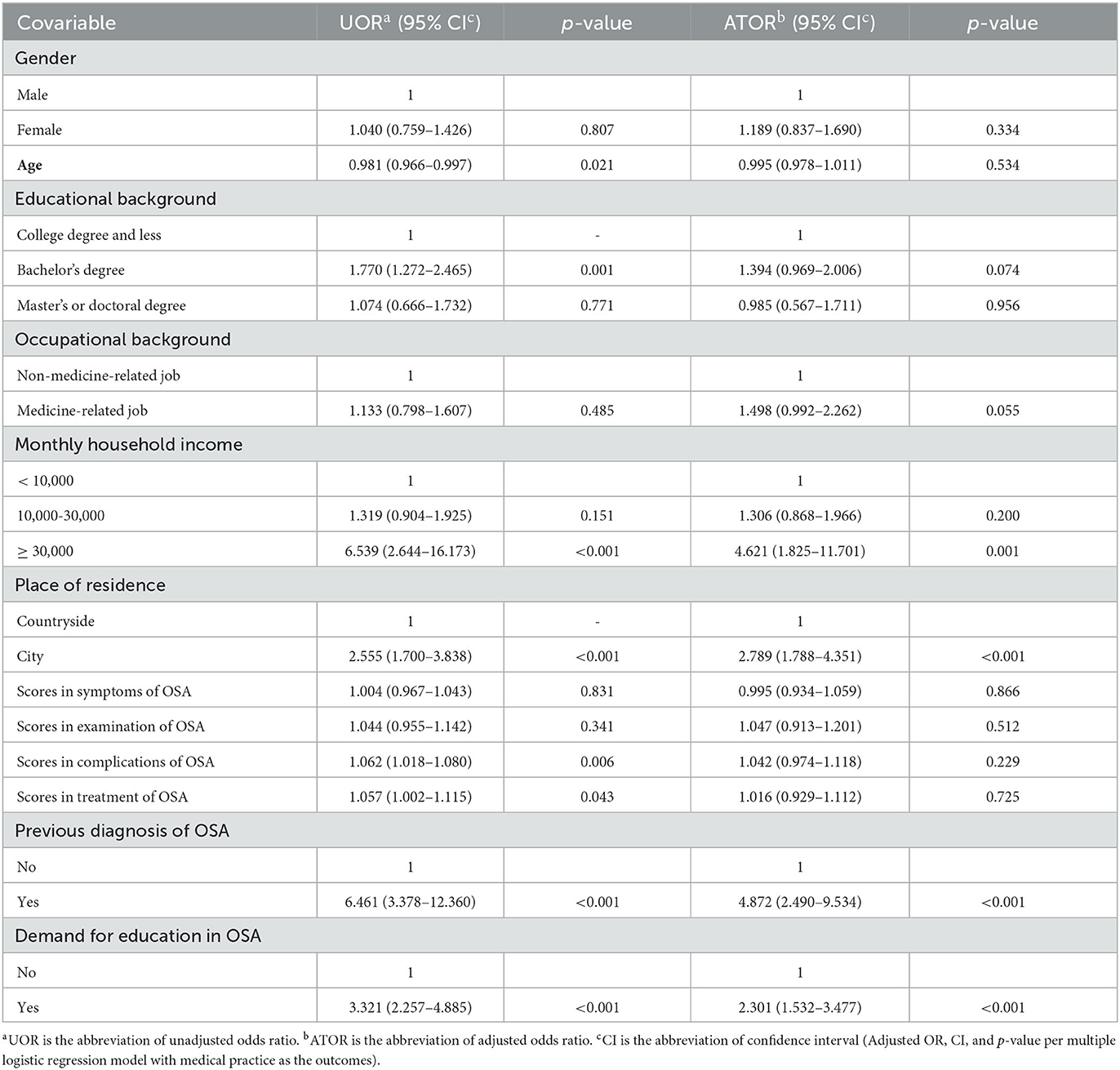
Table 4. Factors associated with seeking medical advice in the general population when people had symptoms (logistic regression N = 1507).
The subsequent analysis focused on the child caregivers group to further determine how demographic, knowledge, and attitude factors affected the practice of taking children to the clinic for OSA. In comparison to unemployed people, respondents who had stable work status (employed) were significantly more likely to undertake an active practice for OSA children (adjusted OR = 2.663, p = 0.03). Among the relationships with children, mothers had a higher odds ratio for taking children to seek medical advice for OSA than fathers (adjusted OR = 2.115, p = 0.017). Parents whose children had ever been diagnosed with OSA were significantly more likely to engage in positive practices for their children's symptoms (adjusted OR = 49.507, p < 0.001). Conversely, age, monthly household income, place of residence, the number of children < 14 years old, and scores in four sections of knowledge about OSA did not significantly affect the practice of treating OSA among child caregivers (p > 0.05) (Table 5).
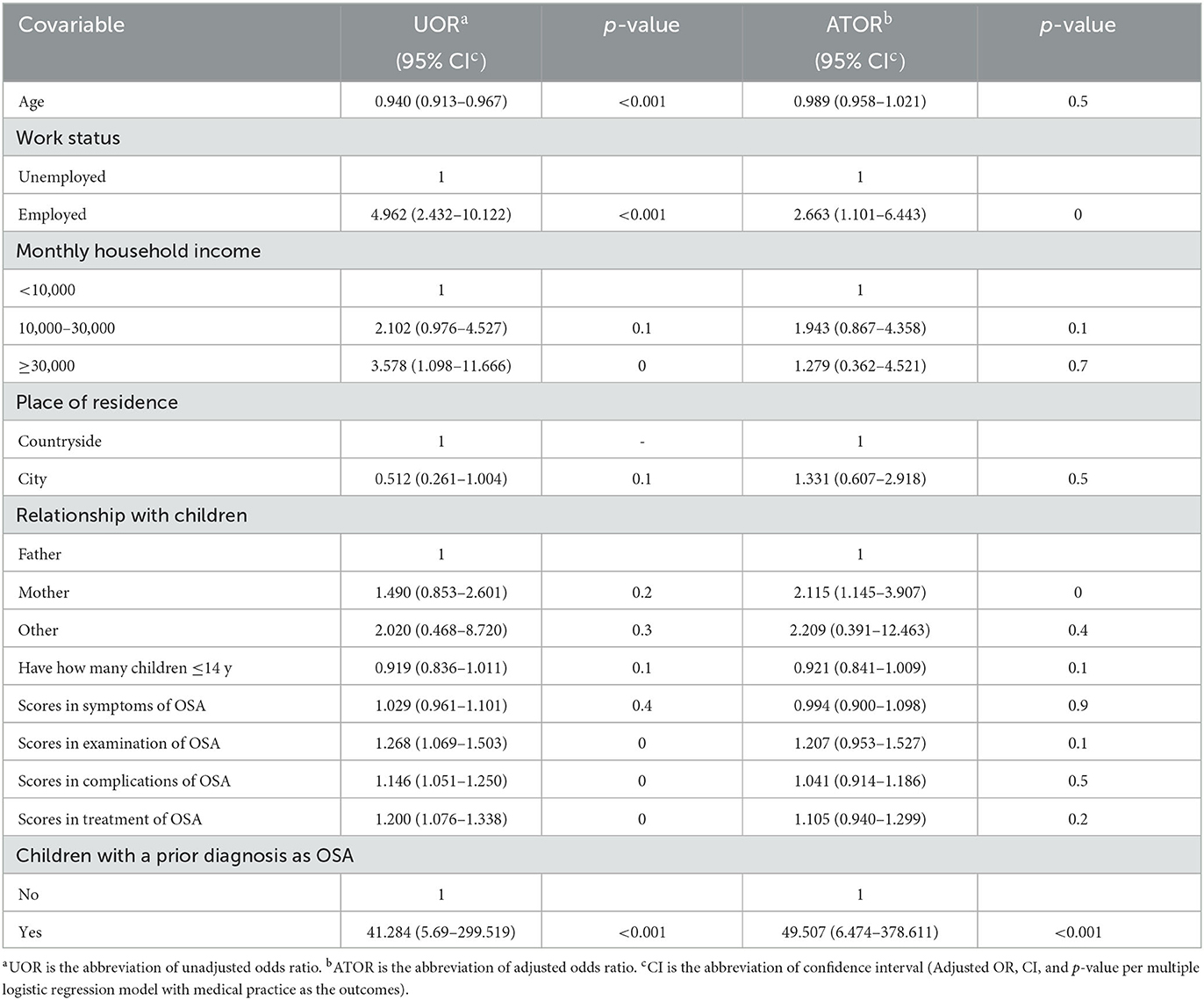
Table 5. Factors associated with seeking medical advice in general populations when people's children had symptoms (logistic regression n = 1,237).
4. Discussion
Obstructive sleep apnea is a common medical condition among the general population with serious medical, psychological, and socioeconomic morbidities, yet most affected patients with OSA remain undetected and lack timely intervention. According to clinical studies, OSA causes significant adverse health and quality of life consequences and has a major impact on the global disease burden (10, 11). Despite the availability of effective diagnostic methods and treatments, screening and case identification of OSA remain difficult challenges (29). Lack of initiative to seek medical help in symptomatic patients was a barrier that impeded the early recognition of and interventions for OSA. Therefore, this lack stimulates the need for improved access to healthcare education among the general population. At the same time, experts in public health and epidemiology are also cooperating with clinicians in popular healthcare science, hoping to identify more subhealthy and preclinical patients through various forms of information provision. Early recognition and intervention for these patients will substantially lower morbidity and mortality rates and reduce overall medical costs (30). In this study, most participants showed insufficient knowledge of OSA, and their average awareness rates in several sections were <60%. Approximately nine-tenths of them had positive attitudes and practices toward OSA, especially parents. If their children had symptoms of OSA, people were more likely to undertake positive medical practices compared with themselves (95.6 vs. 87.6%). For further correlations, household economic factors and related medical history significantly influenced the medical practice pattern. None of the specific sections in scores of knowledge about OSA showed a positive effect on the medical practice pattern. The majority of respondents reported a desire to receive healthcare education through the new multimedia approach, and the majority were concerned about the etiology of OSA.
The survey focused on the general population in China, while the respondents were concentrated in the southwest and coastal areas, and the majority came from urban areas. Encouragingly, more than half of the respondents said that they heard of OSA, and only a few reported being unaware of it. The vast majority considered OSA a serious disease that warranted recognition and early intervention (76.0%). This finding suggested that OSA had a certain public awareness, and its prevalence attracted some people's attention. In the section on knowledge, only seven out of 10 respondents were able to correctly identify the four descriptions of OSA disease. In particular, patients with OSA can present drowsiness, excessive daytime sleepiness, and fatigue proneness during driving, increasing the risk of vehicular accidents (27). Although this association has been fully proven in many large-scale clinical research studies, 31.5% of people did not recognize it. In general, knowledge of OSA was not sufficient since the average awareness rate was <60%.
Among the common symptoms of OSA, “children's bed-wetting” and “nocturia >1 time/night” were the most underestimated. These two presentations are common problems in children (31, 32), affecting approximately 20% of 5-year-old children and 10% of 7-year-old children (6). Parents had a common belief that bed-wetting in children would disappear or be cured with age. However, some clinical trials have indicated that children affected by OSA were at increased risk for nocturnal enuresis (33). In addition, “nocturia > 1 time/night” is not uncommon in middle-aged and older men, who present with an increased number of nocturia episodes due to benign prostatic hyperplasia (34). Attributed to their poor predictive value, these signs have been widely ignored by the general population with potential clinical impacts. Snoring in sleep, the most common symptom recognized by 74.1% of respondents, is the chief complaint of patients with OSA. Nevertheless, this problem was always observed by patients' bedroom partners, and their complaints concerning breathing pauses triggered a referral to a sleep clinic. Regarding examinations, X-ray is the most underestimated diagnostic method for OSA. It is known that tonsil and/or adenoid hyperplasia is a major anatomical contributor to OSA in children (35). For pediatric patients, lateral radiography of the skull base is the most economical, convenient, and non-invasive examination method. Furthermore, the size of the adenoids and the degree of airway obstruction can be quantified by the N/A ratio of the nasopharyngeal airway. Therefore, it has become the first choice for clinicians to evaluate children suspected to have OSA. Compared with other knowledge sections (such as symptoms, examinations, and treatments), respondents showed lower average awareness of the complications of OSA (50.61%). This finding reflected that most people underestimated the potential risks to their health conferred by OSA. Among the complications of OSA, the most well-known were maxillofacial dysplasia (62.6%), such as adenoid face, micrognathia, dentition disorders, and protruding mouth. Owing to their obvious impact on appearance, these signs have received widespread attention among parents. During dental consultations, parents learn from the dentists that the concrete cause of OSA is adenoid/tonsil hypertrophy and receive a referral to an otolaryngologist for etiological treatment. However, spinal dysraphism (37.3%), diabetes (38.0%), and hyperlipidemia (38.8%) were commonly neglected morbidities by respondents. The relationships of OSA with endocrine, metabolic, and developmental diseases are well-documented and unequivocal (4). In addition, continuous positive airway pressure (CPAP) ventilation had the lowest rate of awareness among respondents compared with other treatments. Whereas, it is considered a first-line therapy for patients with symptomatic and moderate to severe OSA with promising clinical effects (27, 36), non-adherence and reduced compliance with CPAP have been widely seen in the literature (37, 38). The probable reasons for this question were chronic nasal congestion, intolerance to nasal masks, and the expensive price of instruments (39). Finally, the results of the present study revealed that women, those >40 years old, those with a bachelor's degree or more, and those from cities are more likely to have higher knowledge scores for OSA than other groups. This finding suggested that men, younger individuals, those with a less educated background and those from the countryside were vulnerable to OSA and required more comprehensive healthcare education.
When they had presentations about OSA, most people chose to seek medical attention for intervention. Only 12.4% (187/1507) of respondents chose not to seek medical help when they became symptomatic. The most common reason for negative medical practice was that OSA was a non-fatal disease (54.4%), indicating that the rest of the people had poor awareness of the potential risks and comorbidities. Other reasons included a lack of confidence in current therapeutic options (40.2%) and fear of surgical risks (38.2%), reflecting a lack of knowledge or clarity about the disease leading to the rejection of medical evaluation. Approximately one in five respondents reported a previous diagnosis of OSA, similar to previous reports (11). Parents displayed a more motivated attitude and practice regarding OSA for their children compared to themselves. Among parents (n = 1,237), 95.6% would take their children to see a doctor if symptoms or signs appeared. However, a difficult problem is that, when parents are inexperienced or unable to distinguish between normal and abnormal conditions, there is a delay in the children's condition. Surprisingly, 42.0% of parents said that their children had ever been diagnosed with OSA. In comparison to the data reported by Burghard et al. (12), that 90% of children did not receive a previous diagnosis of OSA, this population was incredibly well diagnosed. The possibility is that parents concerned about children's conditions were more likely to participate in the survey. In addition, the ratio of previously diagnosed OSA in children was higher than that in adults in this survey. This finding suggests that people are more motivated to seek medical treatment for pediatric OSA, which might be because parents are concerned about cosmetic defects in children. In terms of accepted interventions for childhood OSA (n = 519), only 28.1% of children had undergone surgical treatments. Although many clinical trials have strongly proved that the impaired function of children with OSA would improve after adenotonsillectomy (33, 40), most parents tend to choose a conservative policy. The reason for not considering surgical treatment might be that parents are worried that the removal of immune organs, such as tonsils or adenoids, would affect children's immunity. Another possibility is that they expect the spontaneous regression of OSA during the adolescent period since the adenoid atrophy is from 10 to 12 years old (41).
Almost nine in 10 (89.4%) respondents indicated that they were willing to receive health education. The etiology of OSA was a leading concern (74.9%), and knowledge about surgery, risks, and effects was secondary (68.2%). On the one hand, parents probably want to identify abnormalities in the early stage by learning the etiology and risk factors of OSA, such as obesity and genetic micrognathia. On the other hand, this is a possibility that there are more and more multi-child families in China with the introduction of the two-child policy, and parents are trying to prevent other children from OSA. The second hot spot is knowledge, risks, and effects of surgery, which may be a desperate consideration for solving health problems in time. In the blank of the “others” option, some parents also raised questions regarding how to distinguish between normal and abnormal snoring and whether there is an effective way to prevent OSA. These concrete data provided evidence to devise appropriate popular healthcare content. As Sia et al. (3) reported, traditional media were the most common sources of information about OSA in Singapore among the general population, followed by knowing an affected patient. In contrast, the most popular approach is the new multimedia approach (68.3%), followed by health education manuals (67.0%) in this study. With the rapid development of information technology, medical services have progressed from the traditional face-to-face mode to the current diversified medical mode. Especially after the outbreak of the COVID-19 epidemic, online outpatient clinics have rapidly increased in China (42, 43), making medical services more convenient and accessible (44). At the same time, the popular health science service does not adhere to traditional forms (such as books, brochures, and offline lectures) while creating a new internet media model with more efficient propagation and attracting content (such as short videos, interesting pictures, and WeChat subscription). These analytical outcomes suggest an increasing trend in the general population toward screening health risks by themselves, hoping to recognize abnormal conditions to prevent the occurrence and progression of the disease.
Sia et al. (3) reported that age, race, income, and education level were significant influencing factors for the ability to correctly define OSA. A Pomerania population-based survey conducted by Krüger et al. (45) in 2022 found that socioeconomic factors had no significant effects on OSA. In this survey, two regression models were established to determine the factors affecting medical practice for OSA and childhood OSA. It was illustrated that education background, household income level, place of residence, medical history, and knowledge level of OSA significantly influenced the practice of seeking medical help. For parents, work status, relationships with children, children's previous diagnosis with OSA, and overall OSA awareness were independent influencing factors for whether they would take children to the clinic. Although Krüger et al. (45) indicated that socioeconomic factors were not significantly correlated with the occurrence of OSA, the analysis in this survey confirmed the point that socioeconomic factors could modulate healthcare services. Those people who had a higher education level, household income, and lived in the city were more likely to have a positive attitude and practice toward OSA. Knowledge levels and attitudes showed predictive value for medical practice.
The theory of KAP suggests that correct understanding of diseases, developing positive attitudes, and forming healthy practices are three continuous processes of health education. In this study, the general population had a certain level of knowledge about OSA, but it was not sufficient, and positive practices were not forming completely. This outcome highlights expediting the promotion of popular science propaganda to raise awareness of OSA among the general population. As a consequence, their attitude and practices for seeking medical help could be transformed into an active mode in which the three sections promote each other. Correspondingly, the health impact on individuals and the public health burden on society would be relieved as well.
4.1. Limitations
As with any survey-based research, some possible limitations should be noted in this study. (1) Due to the limited objective conditions, there might be selection bias among participants due to the lack of randomization. Most of the data were collected from most areas of China without even and comprehensive distribution; therefore, the results might not represent the entire population well. (2) Urban residents and women with higher education levels were more likely to respond to the questionnaire, which might be cautiously generalized. (3) Although the researchers invited all general adult population who met the included criteria as much as possible, participation was voluntary. Therefore, people who volunteered to participate in this survey might have been more interested in healthcare knowledge than their counterparts. As mentioned above, the results need to be extrapolated prudently, especially in less educated groups and less economically developed areas. In these groups and areas, e.g., the insufficient KAP level due to OSA might be more severe. Nonetheless, data concerning the KAP and popular healthcare demand regarding OSA from nationwide samples in China supplemented the current sleep medicine studies.
5. Conclusion
The current study indicated that even though the higher educated and urban populations in China had a certain knowledge and positive attitudes about OSA, it was still insufficient. When symptoms or signs appeared, their limited awareness of complications and potentially severe adverse consequences hindered their inner motivation to undertake positive practice for it. The household income level, place of residence, medical history, and attitudes toward healthcare education can significantly affect people's decision to seek medical help. For parents, work status, relationships with children, and children's medical histories can be the influencing factors regarding medical practice. Economically developed factors and disparities between urban and rural areas seem to be the key points influencing the medical practice pattern regarding OSA in populations. However, people's knowledge level about OSA had no specific influence on these patterns. The majority of people expressed active demand for popular healthcare education about OSA. Making full use of the new multimedia approach to expedite the provision of popular science information could be a promising way to improve medical practice in sleep medicine among the general population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee on Biomedical Research of the West China Hospital of Sichuan University (Approval number: 2022.416). The patients/participants provided their written informed consent to participate in this study.
Author contributions
DL and ZP designed the research. TM reviewed the questions. QZ, TX, QR, and TL assisted in the process of collecting data. ZP and TM conducted the data analysis. ZP wrote the manuscript. DL edited and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1128334/full#supplementary-material
Abbreviations
OSA, Obstructive sleep apnea syndrome; KAP, Knowledge, attitude, and practice; QR code, Quick response code; FNP, Flexible nasopharyngoscopy; PSG, Polysomnography; CPAP, Continuous positive airway pressure; UOR, Unadjusted odds ratio; ATOR, Adjusted odds ratio; CI, Confidence interval.
References
1. Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea: a review. JAMA. (2020) 323:1389–400. doi: 10.1001/jama.2020.3514
2. Hu T, Gu Y, Xu Y, Yu J, Wu F, Chen R. Incidence of stroke and mortality in chinese patients with sleep-breathing disorders: a clinical population-based (CPB) study. Med Sci Monit. (2019) 25:10129–35. doi: 10.12659/MSM.918120
3. Sia CH, Hong Y, Tan LWL, van Dam RM, Lee CH, Tan A. Awareness and knowledge of obstructive sleep apnea among the general population. Sleep Med. (2017) 36:10–7. doi: 10.1016/j.sleep.2017.03.030
4. Martins FO, Conde SV. Gender differences in the context of obstructive sleep apnea and metabolic diseases. Front Physiol. (2021) 12:792633. doi: 10.3389/fphys.2021.792633
5. Senaratna CV, English DR, Currier D, Perret JL, Lowe A, Lodge C. Sleep apnoea in Australian men: disease burden, co-morbidities, and correlates from the Australian longitudinal study on male health. BMC Public Health. (2016) 16:1029. doi: 10.1186/s12889-016-3703-8
6. Butler RJ, Heron J. The prevalence of infrequent bedwetting and nocturnal enuresis in childhood. A large British cohort. Scand J Urol Nephrol. (2008) 42:257–64. doi: 10.1080/00365590701748054
7. Joosten KF, Larramona H, Miano S, Van Waardenburg D, Kaditis AG, Vandenbussche N. How do we recognize the child with OSAS? Pediatr Pulmonol. (2017) 52:260–71. doi: 10.1002/ppul.23639
8. Lo Bue A, Salvaggio A, Insalaco G. Obstructive sleep apnea in developmental age. A narrative review. Eur J Pediatr. (2020) 179:357–65. doi: 10.1007/s00431-019-03557-8
9. Thomas S, Patel S, Gummalla P, Tablizo MA, Kier C. You cannot hit snooze on OSA: sequelae of pediatric obstructive sleep apnea. Children. (2022) 9:261. doi: 10.3390/children9020261
10. Lyons MM, Bhatt NY, Pack AI, Magalang UJ. Global burden of sleep-disordered breathing and its implications. Respirology. (2020) 25:690–702. doi: 10.1111/resp.13838
11. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. (2019) 7:687–98. doi: 10.1016/S2213-2600(19)30198-5
12. Burghard M, Brozek-Madry E, Krzeski A. Sleep disordered breathing in children - Diagnostic questionnaires, comparative analysis. Int J Pediatr Otorhinolaryngol. (2019) 120:108–11. doi: 10.1016/j.ijporl.2019.02.008
13. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. (1997) 20:705–6. doi: 10.1093/sleep/20.9.705
14. Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. (2009) 10:753–8. doi: 10.1016/j.sleep.2008.08.007
15. Kapur V, Strohl KP, Redline S, Iber C, O'Connor G. Underdiagnosis of sleep apnea syndrome in US communities Sleep Breath. (2002) 6:49–54. doi: 10.1055/s-2002-32318
16. Borsoi L, Armeni P, Donin G, Costa F, Ferini-Strambi L. The invisible costs of obstructive sleep apnea (OSA): systematic review and cost-of-illness analysis. PLoS ONE. (2022) 17:e0268677. doi: 10.1371/journal.pone.0268677
17. Tamay Z, Akcay A, Kilic G, Suleyman A, Ones U, Guler N. Are physicians aware of obstructive sleep apnea in children? Sleep Med. (2006) 7:580–4. doi: 10.1016/j.sleep.2006.04.004
18. Chan MTV, Wang CY, Seet E, Tam S, Lai HY, Chew EFF. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA. (2019) 321:1788–98. doi: 10.1001/jama.2019.4783
19. Shaw R, McKenzie S, Taylor T, Olafiranye O, Boutin-Foster C, Ogedegbe G, et al. Beliefs and attitudes toward obstructive sleep apnea evaluation and treatment among blacks. J Natl Med Assoc. (2012) 104:510–9. doi: 10.1016/S0027-9684(15)30217-0
20. Al-Khafaji H, Bilgay IB, Tamim H, Hoteit R, Assaf G. Knowledge and attitude of primary care physicians towards obstructive sleep apnea in the Middle East and North Africa region. Sleep Breath. (2021) 25:579–85. doi: 10.1007/s11325-020-02137-7
21. Devaraj NK. Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breath. (2020) 24:1581–90. doi: 10.1007/s11325-020-02040-1
22. Wang CL, Li XZ, Cai XL, Pan XL, Min J. Anesthesiologist's knowledge and attitudes about obstructive sleep apnea: a survey study. Sleep Breath. (2012) 16:41–6. doi: 10.1007/s11325-011-0482-4
23. Selvaraj S, Eusufzai SZ, Asif JA, Bin Jamayet N, Ahmad W, Alam MK. Comparison of knowledge level and attitude towards obstructive sleep apnoea amongst dental and medical undergraduate students of Universiti Sains Malaysia. Work. (2021) 69:173–80. doi: 10.3233/WOR-213466
24. Williams NJ, Nunes JV, Zizi F, Okuyemi K, Airhihenbuwa CO, Ogedegbe G. Factors associated with referrals for obstructive sleep apnea evaluation among community physicians. J Clin Sleep Med. (2015) 11:23–6. doi: 10.5664/jcsm.4356
25. Xu P, Zhang S, Yang J, Chu H, Li D, Zhao H. Survey of parental awareness of obstructive sleep apnea among children in Guangdong province, South China. Auris Nasus Larynx. (2021) 48:690–6. doi: 10.1016/j.anl.2020.10.018
26. Hong PC, Ou Q, Pan MX, Chen BX, Chen ZX, Hong ZG. Investigation on the awareness of snoring hazard and prevalence of obstructive sleep apnea among civil servants. Zhonghua Jie He He Hu Xi Za Zhi. (2020) 43:553–6.
27. Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med. (2019) 380:1442–9. doi: 10.1056/NEJMcp1816152
28. Randerath W, Verbraecken J, de Raaff CA, Hedner J, Herkenrath S, Hohenhorst W. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Eur Respir Rev. (2021) 30:162. doi: 10.1183/16000617.0200-2021
29. Natsky AN, Chai-Coetzer CL, Vakulin A, McEvoy RD, Adams RJ, Kaambwa B. Economic evaluation of diagnostic sleep studies for obstructive sleep apnoea in the adult population: a systematic review. Sleep Med Rev. (2022) 62:101608. doi: 10.1016/j.smrv.2022.101608
30. Chung SA, Jairam S, Hussain MR, Shapiro CM. How, what, and why of sleep apnea. Perspectives for primary care physicians. Can Fam Physician. (2002) 48:1073–80.
31. N. O'Flynn. Nocturnal enuresis in children and young people: NICE clinical guideline. Br J Gen Pract. (2011) 61:360–2. doi: 10.3399/bjgp11X572562
32. Caldwell PH, Deshpande AV, Von Gontard A. Management of nocturnal enuresis. BMJ. (2013) 347:f6259. doi: 10.1136/bmj.f6259
33. Snow A, Vazifedan T, Baldassari CM. Evaluation of nocturnal enuresis after adenotonsillectomy in children with obstructive sleep apnea: a secondary analysis of a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. (2021) 147:887–92. doi: 10.1001/jamaoto.2021.2303
34. Chartier-Kastler E, Leger D, Comet D, Haab F, Ohayon MM. Prostatic hyperplasia is highly associated with nocturia and excessive sleepiness: a cross-sectional study. BMJ Open. (2012) 2:505. doi: 10.1136/bmjopen-2011-000505
35. Wang J, Zhao Y, Yang W, Shen T, Xue P, Yan X. Correlations between obstructive sleep apnea and adenotonsillar hypertrophy in children of different weight status. Sci Rep. (2019) 9:11455. doi: 10.1038/s41598-019-47596-5
36. Usmani ZA, Chai-Coetzer CL, Antic NA, McEvoy RD. Obstructive sleep apnoea in adults. Postgrad Med J. (2013) 89:148–56. doi: 10.1136/postgradmedj-2012-131340
37. Askland K, Wright L, Wozniak DR, Emmanuel T, Caston J, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. (2020) 4:Cd007736. doi: 10.1002/14651858.CD007736.pub3
38. Wang Y, Gao W, Sun M, Chen B. Adherence to CPAP in patients with obstructive sleep apnea in a Chinese population. Respir Care. (2012) 57:238–43. doi: 10.4187/respcare.01136
39. Zarhin D, Oksenberg A. Ambivalent adherence and nonadherence to continuous positive airway pressure devices: a qualitative study. J Clin Sleep Med. (2017) 13:1375–84. doi: 10.5664/jcsm.6828
40. Redline S, Amin R, Beebe D, Chervin RD, Garetz SL, Giordani B. The Childhood Adenotonsillectomy Trial (CHAT): rationale, design, and challenges of a randomized controlled trial evaluating a standard surgical procedure in a pediatric population. Sleep. (2011) 34:1509–17. doi: 10.5665/sleep.1388
41. Spilsbury JC, Storfer-Isser A, Rosen CL, Redline S. Remission and incidence of obstructive sleep apnea from middle childhood to late adolescence. Sleep. (2015) 38:23–9. doi: 10.5665/sleep.4318
42. Liu L, Gu J, Shao F, Liang X, Yue L, Cheng Q, et al. Application and preliminary outcomes of remote diagnosis and treatment during the COVID-19 outbreak: retrospective cohort study. JMIR Mhealth Uhealth. (2020) 8:e19417. doi: 10.2196/19417
43. Gong K, Xu Z, Cai Z, Chen Y, Wang Z. Internet hospitals help prevent and control the epidemic of COVID-19 in China: multicenter user profiling study. J Med Internet Res. (2020) 22:e18908. doi: 10.2196/18908
44. Ge F, Qian H, Lei J, Ni Y, Li Q, Wang S, et al. Experiences and challenges of emerging online health services combating COVID-19 in China: retrospective, cross-sectional study of internet hospitals. JMIR Med Inform. (2022) 10:e37042. doi: 10.2196/37042
Keywords: OSA, general population, sleep health care education, KAP, public health
Citation: Pan Z, Ma T, Zeng Q, Xu T, Ran Q, Li T and Lu D (2023) People's knowledge, attitudes, practice, and healthcare education demand regarding OSA: a cross-sectional study among Chinese general populations. Front. Public Health 11:1128334. doi: 10.3389/fpubh.2023.1128334
Received: 20 December 2022; Accepted: 03 April 2023;
Published: 13 July 2023.
Edited by:
Harshad Thakur, Tata Institute of Social Sciences, IndiaReviewed by:
Li DaiBO, Meishan People's Hospital, ChinaQian Zhao, The First Affiliated Hospital of Xi'an Jiaotong University, China
Copyright © 2023 Pan, Ma, Zeng, Xu, Ran, Li and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Lu, ZGFubHYyMDA4QHdjaHNjdS5jbg==
 Zhongjing Pan1
Zhongjing Pan1 Dan Lu
Dan Lu