- 1Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 3Immune Therapy Institute, Renji Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 4School of Global Health, Chinese Center for Tropical Diseases, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 5School of Mathematics and Physics, Xi'an Jiaotong-Liverpool University, Suzhou, China
Limited data are available on the prevalence of prescription opioid use among patients with cardiac conditions who were exposed to increased risks of cardiac events including myocardial failure and cardiac arrest. According to the U.S. National Health Interview Survey, we evaluated the prevalence of opioid use in patients with cardiac conditions who reported prescription opioid use in the past 12 months and 3 months in 2019 and 2020, respectively, and further estimated the prevalence of opioid use for acute pain or chronic pain. We also analyzed the stratified prevalence by demographical characteristics. Our results showed that there was no statistically significant change in the prevalence of opioid use in the past 12 months (26.5% in 2019 vs. 25.7% in 2020) or the past 3 months (66.6% in 2019 vs. 62.5% in 2020) before and during the COVID-19 pandemic. However, there was a significant decline in the prevalence of opioid use for acute pain, from 64.2% (95% confidence interval [CI] 57.6% to 70.3%) in 2019 to 49.6% (95% CI 40.1% to 59.0%) in 2020 (P = 0.012), particularly in the subgroups of men, non-Hispanic white people, adults with education below high school, those with an income-to-poverty ratio ranging from 1.0 to 1.9, and those covered with health insurance. Our findings suggest that monitoring opioid use in the era of living with COVID-19 is important, which will help inform healthcare providers to develop care strategies to reduce health loss for vulnerable individuals.
1. Introduction
An opioid is the most common analgesic treatment for perioperative, acute, and chronic pain (1). It is recognized as the standard of care for patients with acute coronary syndromes to relieve pain (2) and is also used as an analgesic for those with other cardiovascular diseases (CVDs) (3). However, increasing evidence indicated the cardiotoxic effect of opioid administration (4). There may be an increased risk of endocarditis, hypoxia–ischemia, myocardial failure, and even cardiac arrest with opioids (5). Therefore, it is crucial to direct the safe use of opioids to patients with CVD (6).
Recently, the opioid epidemic has become a public health catastrophe and may worsen due to the COVID-19 pandemic. In 2020, ~70,000 fatal opioid overdoses were recorded in the United States, an increase of ~37% in 2019 (7). However, there are limited data on the prevalence of opioid use among those with cardiac conditions. The lack of timely surveillance may pose challenges for healthcare services providing precise management. Hence, we sought to estimate the prevalence of cardiac patients with opioid use and determine recent trends before and during the COVID-19 pandemic to provide population-scale evidence for the monitoring and management of opioid use.
2. Materials and methods
2.1. Data source
In this 2-year population-based study, we retrieved data from the National Health Interview Survey (NHIS), which was conducted by the National Center for Health Statistics (NCHS), Center for Disease Prevention and Control of the United States (8). The NHIS is a nationally representatively cross-sectional household survey aimed to surveil health outcomes in civilian non-institutionalized U.S. residents every year. In 2019, the NHIS added new survey content about prescription opioid use and pain management in the sample adult interview (9). In 2020, that information kept being collected as sponsored by the National Center for Injury Prevention and Control. In addition, the NHIS added coronavirus-related content in 2020 (10). The sampling procedure followed a randomized, multistage, and stratified probability approach to recruiting households to collect health-related information by face-to-face or telephone survey. One sample adult from each household was randomly selected to provide his/her health information by himself/herself or a knowledgeable proxy if the sample adults were physically or mentally unable to answer the questionnaire. Through the random and multistage sampling approach, the NHIS created a sample weight for each survey respondent, which conveyed the number of population units each NHIS respondent represents. The sample weights were adjusted for non-response and further adjusted using post-stratification by age, sex, and race/ethnicity based on population estimates from the recent U.S. census information at the time of each NHIS administration, which was computed and provided by the NHIS. The NHIS data were de-identified, publicly available, and approved by the Research Ethics Review Board of the NCHS and the U.S. Office of Management and Budget. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
2.2. Data collection
We included sample adults aged 20–79 years with cardiac conditions for analysis. The cardiac conditions were ascertained by asking sample adults whether they ever had coronary heart disease, angina, or heart attack told by doctors. The prescription opioid use of participants was ascertained by asking them whether they have taken any opioid pain relievers prescribed by a doctor, dentist, or other health professionals in the past 3 months and the past 12 months. According to the NHIS criteria, prescription opioid drugs included hydrocodone, Vicodin, Norco, Lortab, oxycodone, OxyContin, Percocet, and Percodan, while over-the-counter pain relievers such as aspirin, Tylenol, Advil, or Aleve were not included (9). The purpose of opioid use (relief of acute pain or chronic pain) was also asked among those who reported taking any opioids prescribed by a doctor in the past 3 months. Opioid use for acute pain was defined as prescription opioid administration to treat short-term or acute pain, such as pain due to a broken bone or muscle sprain, pain from dental work, or pain following surgery, while opioid use for chronic pain was to treat long-term or chronic pain, such as low back pain or neck pain, frequent headaches or migraines, or joint pain or arthritis.
This study included sociodemographic and behavioral characteristics as covariates. Sociodemographic variables included age (grouped into 20–64 years and 65–79 years of age), sex (female and male), race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic, and others), educational level (below high school, high school, and beyond high school), income (according to income-to-poverty ratio, IPR, <1.0, 1.0–1.9, 2.0–3.9, and ≥4.0), and health insurance (not covered and covered). The behavioral characteristics included body mass index (BMI stratified into underweight [<18.5 kg/m2], normal [18.5–24.9 kg/m2], overweight [25.0–29.9 kg/m2], and obesity [≥30.0 kg/m2]).
2.3. Statistical analysis
This study calculated and compared the difference in the prevalence of prescription opioid use in 2019 and 2020. All analyses accounted for the complex weighting variable of the surveys. The sample weights were calculated with adjustment by age, sex, race/ethnicity, educational level, IPR, and BMI and gave prevalence estimates with a 95% confidence interval (CI) for patients with cardiac conditions with opioid use in 2019 and 2020, respectively. Since the outbreak of COVID-19 began in late December 2019 and was declared a global pandemic on 11 March 2020 (11), the prevalence of opioid use in 2019 was considered as the prevalence before the COVID-19 pandemic while that in 2020 was during the COVID-19 pandemic. Student's t-test was used to determine the change in the prevalence before and during the COVID-19 pandemic. In addition, to further quantify the impact of the sociodemographic and behavioral variables on the prevalence of opioid use, multivariable logistic regression models were used to calculate the odds ratios (ORs) with the adjustment of age, sex, and race/ethnicity. For all analyses, the level of statistical significance was defined as two-sided P < 0.05. The statistical analyses were performed by the R software 4.0.1.
3. Results
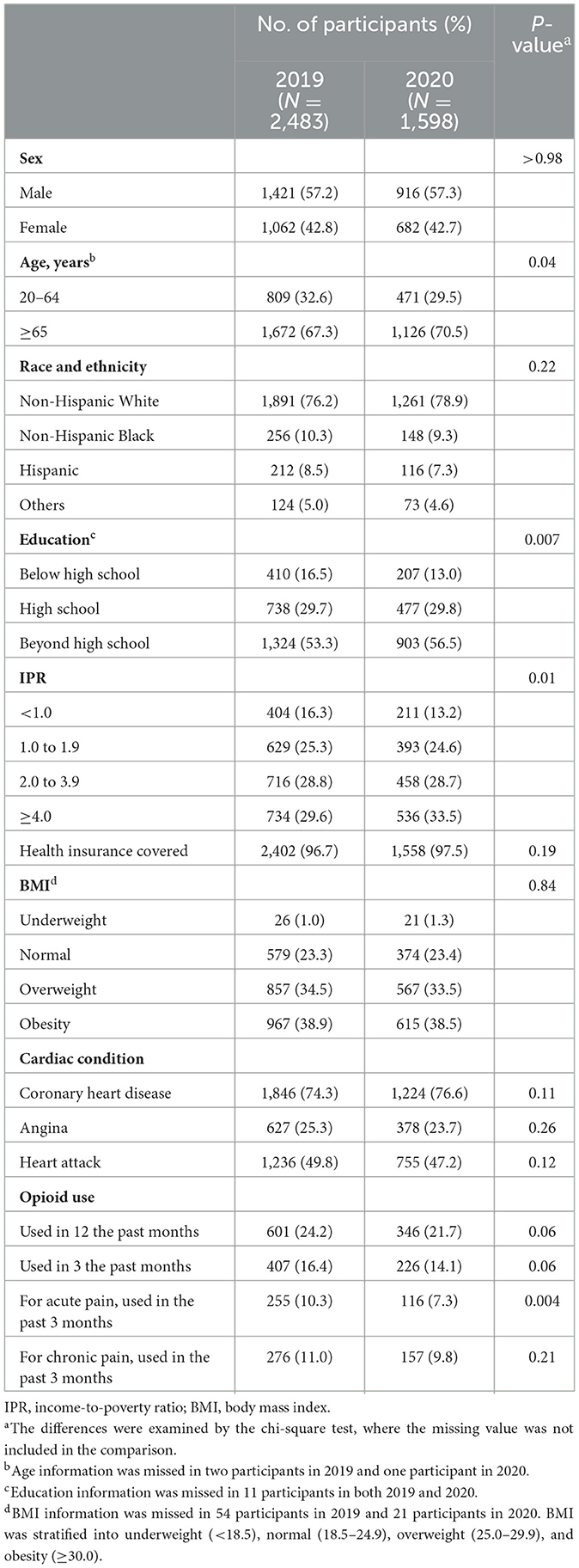
A total of 4,081 sample adults (N = 2,483 in 2019 and N = 1,598 in 2020) who disclosed cardiac conditions from a doctor or other health professionals were included in the analyses. Among them, 2,337 (57.3%) adults were men and 1,744 (42.7%) were women. A total of 3,152 (77.2%) were non-Hispanic white, 404 (9.8%) were non-Hispanic Black, 328 (8.0%) were Hispanic, and 197 (4.8%) were other races/ethnicities. There were 1,280 (31.4%) adults aged between 20 and 64 years old, and 2,798 (68.6%) adults aged between 65 and 79 years old. Overall, there were 601 (24.2%) patients with cardiac conditions reporting their use of prescribed opioid drugs in the past 12 months in 2019 and the number was 346 (21.7%) in 2020. The baseline characteristics of participants in 2019 and 2020 are shown in Table 1.
The prevalence estimates of prescribed opioid use are shown in Table 2. The estimated prevalence of opioid use in the past 12 months was 26.5% (95% CI 24.0 to 29.2%) in 2019 and 25.7% (95% CI 22.5 to 29.2%) in 2020. No significant difference in the prevalence in 2019 and 2020 was observed (P = 0.71). Similarly, the disparities in the prevalence of opioid use within 12 months in 2019 and 2020 by sex, age, race/ethnicity, education, IPR, health insurance, and BMI were statistically non-significant (all P > 0.05).
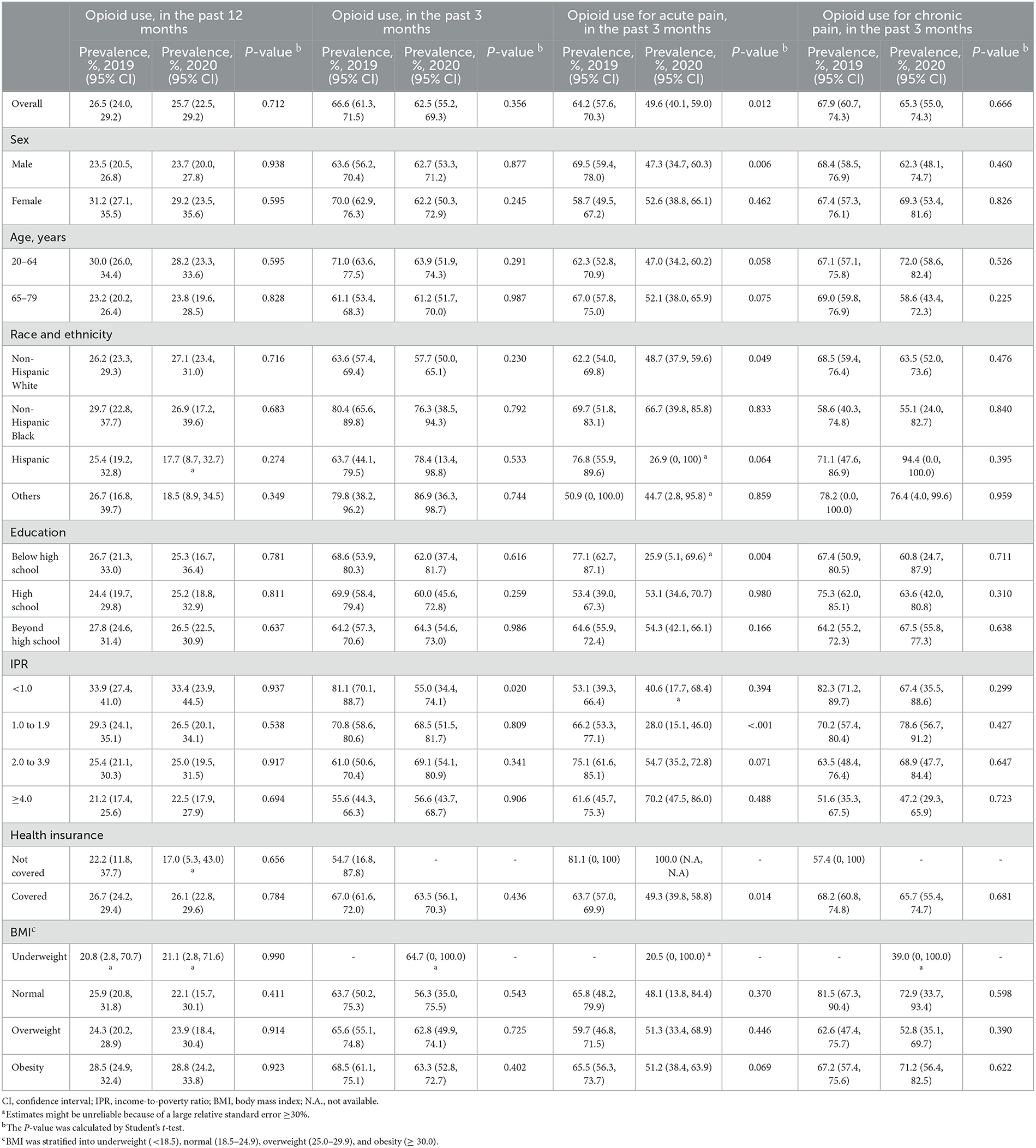
Table 2. Comparison of the prevalence of opioid use in 2019 and 2020 by the purpose of use among U.S. adults with cardiac conditions aged 20–79 years.
For the prevalence of opioid use in the past 3 months, there was a non-significant decline, with an estimated value of 66.6% (95% CI: 61.3 to 71.5%) in 2019 and 62.5% (95% CI: 55.2 to 69.3%) in 2020. Subgroup results showed that the decline mainly occurred among patients with IPR of <1.0 in 2020 (prevalence: 81.1% in 2019 vs. 55.0% in 2020, P = 0.02), and there was no significant difference in prevalence stratified by age, sex, race/ethnicity, education, health insurance, and BMI between 2019 and 2020 (All P > 0.05). In addition, the decline occurred in patients using it for acute pain (Table 2), with an estimate of 64.2% (95% CI: 57.6% to 70.3%) in 2019 and 49.6% (95% CI: 40.1 to 59.0%) in 2020 (P = 0.012). Furthermore, the declined prevalence was shown in male subjects (69.5% in 2019 vs. 47.3% in 2020), non-Hispanic white people (62.2% in 2019 vs. 48.7% in 2020), those with an education level below high school (77.1% in 2019 vs. 25.9% in 2020), those with IPR from 1.0 to 1.9 (66.2% in 2019 vs. 28.0% in 2020), and those with covered health insurance (63.7% in 2019 vs. 49.3% in 2020). In contrast, there was no significant change in opioid use for chronic pain with an estimated prevalence of 67.9% (95% CI: 60.7 to 74.3%) in 2019 and 65.3% (95% CI: 55.0 to 74.3%) in 2020 (P > 0.05).
According to the results from multivariable logistic regression models, we found that family income level might be associated with opioid use in patients with cardiac conditions (Table 3). Opioid use within 12 months was less prevalent among adults with higher family income levels (for IPR≥ 4.0, OR 0.57 [95% CI: 0.38 to 0.85] in 2019; 0.54 [95% CI: 0.32 to 0.94] in 2020). Similarly, in 2019, the prevalence of opioid use within 3 months and opioid use for chronic pain were lower among higher family income levels; however, this effect vanished in 2020. Notably, those with higher family income levels were prone to use opioids for acute pain (for IPR 2.0 to 3.9, OR 2.45 [95% CI: 1.01 to 5.94] in 2019, 3.22 [95% CI: 1.01 to 10.32] in 2020; for IPR ≥4.0, OR 1.35 [95% CI: 0.53 to 3.45] in 2019, 7.77 [95% CI: 2.10 to 28.70]). In addition, the prevalence of opioid use for acute pain was positively associated with high education in 2020 (OR 5.38 [95% CI: 1.48 to 19.6] for adults in high school and OR 5.58 [95% CI: 1.63 to 19.11] for adults beyond high school, respectively), though non-significant or negatively in 2019. We also found that the prevalence was higher among those aged 65–79 years than those aged 20–64 years old in 2019 and not found in 2020 or other subgroups.
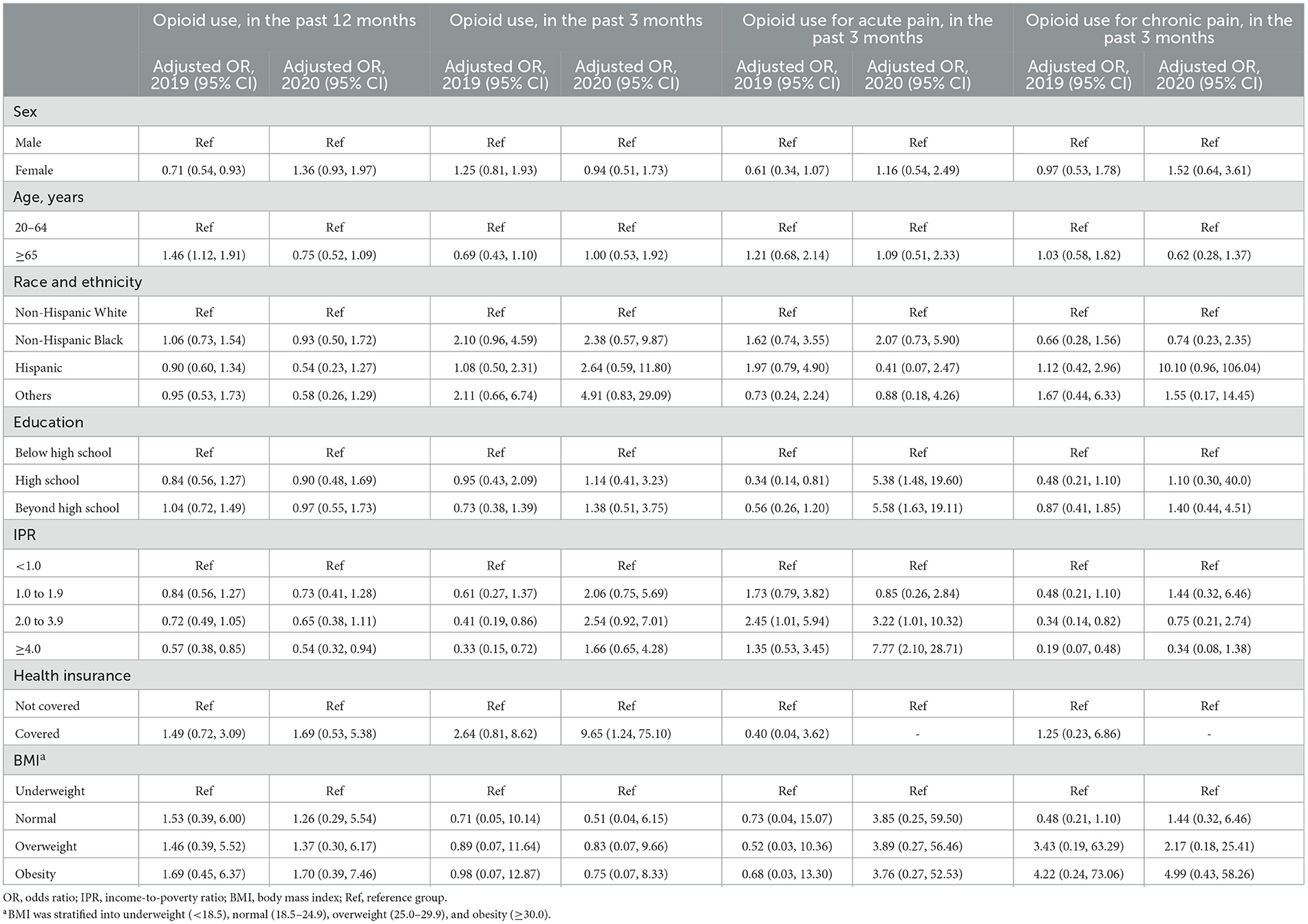
Table 3. Adjusted odds ratios of opioid use by subgroup and purpose of use before in 2019 and 2020 among US adults with cardiac conditions aged 20–79 years.
4. Discussion
In this study, we used nationally representative data from the population-based NHIS to estimate the prevalence of prescription opioid use in patients with cardiac conditions before and during the COVID-19 pandemic. We also analyzed the stratified prevalence by sociodemographic and behavioral characteristics and the purpose of use for acute pain or chronic pain relief. We did not find a significant change in the prevalence of opioid use before and during the COVID-19 pandemic. However, a decreased prevalence of opioid use in the past 3 months was observed for acute pain, particularly in the subgroups of men, non-Hispanic whites, adults with an education level below high school, those with IPRs ranging from 1.0 to 1.9, and those covered with health insurance.
To the best of our knowledge, this is the first nationally representative study to estimate the prevalence of prescription opioid use in patients with cardiac conditions. Previous studies reported that there were 34% of civilian, non-institutionalized adults in the United States reported having used at least one of these specific prescription opioids at least once in the past 12 months, according to the 2015 National Survey on Drug Use and Health (NSDUH) questionnaire items (12). However, our study reported a prevalence of approximately 26% of opioid use with cardiac conditions, lower than estimates in previous years among the general population, although patients with cardiac conditions are thought to potentially have more opioid use. Differences in study design, sampling approaches, data collection procedure, and participant characteristics may partly explain the prevalence differences. The differences between NSDUH and NHIS had been reported previously (13). Moreover, the expanded definition of opioid use might also be the reason. In NHIS, all the opioid use was followed by a doctor, dentist, or other health professionals while not in NSDUH.
Emerging evidence indicated that the COVID-19 pandemic would result in significant increases in opioid use (14, 15). However, no significant changes were observed in our study. This may be due to the following reasons. First, patients with cardiac conditions may be in more careful management, as a result of which the use of opioids may be more regulated. In addition, with restrictions on face-to-face clinical consultations during the COVID-19 pandemic, prescription opioids were more difficult to obtain, which also partly explained the decline in the prevalence of opioid use for acute pain since the COVID-19 pandemic.
The association between income and opioid use was reported previously (16). Consistent with our results, individuals with lower income had a higher level of exposure than those with higher income to opioid prescriptions, though the racial and ethnic disparities were not observed, which might be due to the better management of cardiac events and better health awareness among patients with high income (17, 18). However, the fact that those with higher incomes were prone to use opioids for acute pain has not been reported before, particularly during the COVID-19 pandemic. This might be because patients with high incomes were more able to get opioid prescriptions. It was documented that patients with high incomes were more likely to have access to healthcare during the COVID-19 pandemic (19). In addition, clinicians were more likely to prescribe opioids for pain management to white patients than to racial/ethnic minority patients presenting with the same symptoms (20, 21), which might also exist in high-income vs. low-income patients. Therefore, more studies were warranted to further describe the association between opioid use and income.
Some limitations should be noted in this study. First, the cardiovascular conditions from the NHIS data were confirmed by self-report or proxy report, which may be subjected to recall bias and lead to misclassification of individuals who have heart conditions. Second, NHIS data did not provide additional information about the purpose of opioid use. It is unclear to further understand whether the drugs were used for cardiac events or other purposes. Third, due to the COVID-19 pandemic, the face-to-face survey was hard to achieve and switched to telephone surveys, leading to a decline in survey response rates. Our results should be carefully interpreted in case of the low response disproportionately occurred in particular populations.
5. Conclusion
This study provides national prevalence estimates on opioid use in U.S. patients with cardiac conditions before and during the COVID-19 pandemic. Although the overall prevalence of opioid use among patients with cardiac conditions in 2019 and 2020 leveled off, there was a decline in the prevalence of opioid use in 2020 among the cardiovascular populations who reported using prescription opioids in the past 3 months to relieve acute pain. As the COVID-19 pandemic may continue posing health threats and changing normal life, it is important to keep monitoring opioid use among vulnerable populations. Further investigations are in need to understand the factors associated with the change in opioid use among patients with cardiac conditions in the era of living with COVID-19.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.
Author contributions
LWe conceived and designed the study. LWe, JH, and HS acquired the data. JH, HS, SG, and NQ cleaned and analyzed the data. JH and YL interpreted the results. LWu and JH drafted the manuscript. LWe, JH, YL, HS, YM, SG, NQ, SW, LWu, MH, LX, and LH revised the manuscript. All authors contributed to the content and critical revision of the manuscript and approved the final version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Corder G, Castro DC, Bruchas MR, Scherrer G. Endogenous and exogenous opioids in pain. Annu Rev Neurosci. (2018) 41:453–73. doi: 10.1146/annurev-neuro-080317-061522
2. Furtado RHM, Nicolau JC, Guo J, Im K, White JA, Sabatine MS, et al. Morphine and cardiovascular outcomes among patients with non-ST-Segment elevation acute coronary syndromes undergoing coronary angiography. J Am Coll Cardiol. (2020) 75:289–300. doi: 10.1016/j.jacc.2019.11.035
3. Dawson NL, Roth V, Hodge DO, Vargas ER, Burton MC. Opioid use in patients with congestive heart failure. Pain Med. (2018) 19:485–90. doi: 10.1093/pm/pnx103
4. Chen A, Ashburn MA. Cardiac effects of opioid therapy. Pain Med. (2015) 16(Suppl 1):S27–31. doi: 10.1111/pme.12915
5. Dezfulian C, Orkin AM, Maron BA, Elmer J, Girotra S, Gladwin MT, et al. Opioid-associated out-of-hospital cardiac arrest: distinctive clinical features and implications for health care and public responses: a scientific statement from the American heart association. Circulation. (2021) 143:e836–e70. doi: 10.1161/CIR.0000000000000958
6. Chow SL, Sasson C, Benjamin IJ, Califf RM, Compton WM, Oliva EM, et al. Opioid use and its relationship to cardiovascular disease and brain health: a presidential advisory from the American heart association. Circulation. (2021) 144:e218–e32. doi: 10.1161/CIR.0000000000001007
7. Humphreys K, Shover CL, Andrews CM, Bohnert ASB, Brandeau ML, Caulkins JP, et al. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford-lancet commission. Lancet. (2022) 399:555–604. doi: 10.1016/S0140-6736(21)02252-2
8. National Center for Health Statistics. National Health Interview Survey. (2022). Available online at: https://www.cdc.gov/nchs/nhis/index.htm (accessed June 22, 2023).
9. National Center for Health Statistics. National Health Interview Survey, 2019: Survey Description Hyattsville, Maryland. (2020). Available online at: https://www.cdc.gov/nchs/nhis/2019nhis.htm (accessed June 22, 2023).
10. National Center for Health Statistics. National Health Interview Survey, 2020: Survey Description Hyattsville, Maryland. (2021). Available online at: https://www.cdc.gov/nchs/nhis/2020nhis.htm (accessed June 22, 2023).
11. Adil MT, Rahman R, Whitelaw D, Jain V, Al-Taan O, Rashid F, et al. SARS-CoV-2 and the pandemic of COVID-19. Postgrad Med J. (2021) 97:110–6. doi: 10.1136/postgradmedj-2020-138386
12. Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 national survey on drug use and health. Ann Intern Med. (2017) 167:293–301. doi: 10.7326/M17-0865
13. Pemberton MR, Bose J, Kilmer G, Kroutil LA, Forman-Hoffman VL, Gfroerer JC. Comparison of NSDUH Health and Health Care Utilization Estimates to Other National Data Sources. CBHSQ Data Review. Rockville (MD): Substance Abuse and Mental Health Services Administration (US) (2012). p. 1-69.
14. Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. (2020) 214:108176. doi: 10.1016/j.drugalcdep.2020.108176
15. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. (2021) 594:259–64. doi: 10.1038/s41586-021-03553-9
16. Friedman J, Kim D, Schneberk T, Bourgois P, Shin M, Celious A, et al. Assessment of racial/ethnic and income disparities in the prescription of opioids and other controlled medications in California. JAMA Intern Med. (2019) 179:469–76. doi: 10.1001/jamainternmed.2018.6721
17. Chan PS, McNally B, Vellano K, Tang Y, Spertus JA. Association of neighborhood race and income with survival after out-of-hospital cardiac arrest. J Am Heart Assoc. (2020) 9:e014178. doi: 10.1161/JAHA.119.014178
18. Shin JH, Jung MH, Kwon CH, Lee CJ, Kim DH, Kim HL, et al. Disparities in mortality and cardiovascular events by income and blood pressure levels among patients with hypertension in South Korea. J Am Heart Assoc. (2021) 10:e018446. doi: 10.1161/JAHA.120.018446
19. Cheong JL, Goh ZHK, Marras C, Tanner CM, Kasten M, Noyce AJ. The impact of COVID-19 on access to Parkinson's disease medication. Mov Disord. (2020) 35:2129–33. doi: 10.1002/mds.28293
20. Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. (1993) 269:1537–9. doi: 10.1001/jama.269.12.1537
Keywords: COVID-19 pandemic, opioid use, prevalence, survey study, cardiac patients
Citation: Weng L, Huang J, Lou Y, Shi H, Ma Y, Gu S, Qiang N, Wang S, Wu L, He M, Xu L and Han L (2023) Comparison of the prevalence of opioid use among U.S. adults with cardiac conditions before and during the COVID-19 pandemic. Front. Public Health 11:1127636. doi: 10.3389/fpubh.2023.1127636
Received: 04 January 2023; Accepted: 26 January 2023;
Published: 17 February 2023.
Edited by:
Wendy Margaret Walwyn, University of California, Los Angeles, United StatesReviewed by:
Louis Trevisan, Creighton University, United StatesBrian J. Piper, Geisinger Commonwealth School of Medicine, United States
Copyright © 2023 Weng, Huang, Lou, Shi, Ma, Gu, Qiang, Wang, Wu, He, Xu and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lefei Han,  bGZoYW5Ac2p0dS5lZHUuY24=; Lei Xu,
bGZoYW5Ac2p0dS5lZHUuY24=; Lei Xu,  eGw4NkBzaGNoZXN0Lm9yZw==
eGw4NkBzaGNoZXN0Lm9yZw==
†These authors have contributed equally to this work
 Lvkan Weng1†
Lvkan Weng1† Lefei Han
Lefei Han