
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 08 June 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1126126
This article is part of the Research Topic Exercise and Chronic Disease View all 10 articles
Objective: In the present systematic review and meta-analysis, we aimed to evaluate and update the effects of aquatic exercise on physical fitness and quality of life (QoL) in postmenopausal women.
Methods: The databases Cochrane Library, PubMed, Web of Science, and MEDLINE were searched for randomized controlled trials (RCTs) on the topic from inception to July 2022. The GetData software was used to extract data from the published images. RevMan5.4 software was used for statistical analysis. Data are expressed as standardized mean difference (SMD) with 95% confidence intervals (CI). I2 index was employed for heterogeneity. Egger's test was used to assess publication bias. We evaluated the methodological quality of included studies using the Physiotherapy Evidence Database scale.
Results: We included 594 participants in 16 RCTs (19 comparison groups). The results indicated that aquatic exercise can significantly improve lower limb strength (LLS), upper limb strength (ULS), agility, flexibility, and overall QoL. No significant effects were found on aerobic capacity. Subgroup-analysis results indicated that aquatic exercise only significantly improved LLS, ULS, agility, and flexibility in postmenopausal women < 65 years of age. However, aquatic exercise improves the overall QoL both in postmenopausal women < 65 years and ≥ 65 years. Aquatic resistance exercise significantly improves LLS, ULS, agility and flexibility. In addition, aquatic aerobic exercise can effectively increase LLS, and combined aquatic aerobic and resistance exercise can enhance the overall QoL.
Conclusions: Aquatic exercise can effectively improve physical fitness and overall QoL in postmenopausal women, but has limited effects on aerobic capacity; thus, it is highly recommended in postmenopausal women.
With a rapidly aging of global population, the societies of many countries are gradually becoming aged (1, 2). A decline in muscle strength, cardiorespiratory fitness, mobility, and flexibility usually accompany the aging process (3–5). The body functional degeneration is more pronounced in older (6) and postmenopausal women (7). Postmenopausal women experience reduced muscle mass, muscle strength, and neuromuscular function due to ovarian degeneration and decreased secretion of estrogen, which in turn further exacerbates the degeneration of the ability to perform daily activities (8–10) and increases the risk of falling (7, 11). About 30% of people over 65 years fall at least once a year (12–14). Daily physical activity and motivation to participate in exercise are limited due to fear of falls and fractures, leading to a sedentary lifestyle and decreased quality of life (QoL) (15–19).
Exercise is a great means to improve physical fitness and emotional and mental health (20, 21). For persons with poor balance, fear of falling, joint pain, and weak muscle strength, aquatic exercise is a better alternative (22–24). Water buoyancy reduces joint load by 50–90%, especially good for people with decreased lower limb strength (LLS), obesity, and joint pain (22, 25). In older adults, aquatic resistance exercise increases muscle mass and strength and reduces the risk of falls (26, 27). Hydrostatic pressure increases blood circulation in the lower limbs (24). However, no consistent opinions have been reached regarding the efficacy of aquatic exercise on physical fitness and QoL in postmenopausal women. According to several authors, aquatic exercise can significantly improve LLS (1, 28–34), while Dong-Hyun et al. (35) found limited improvement in LLS (35). Ha et al. (1), Lopez et al. (32), and Perkins et al. (33) found that those who carried out aquatic exercise significantly achieved improved aerobic capacity compared to the control group (1, 32, 33), while Hafele, Alberton, Hafele et al. (31) had contrasting results (31). Dong-Hyun et al. (35) confirmed that aquatic aerobic exercise cannot significantly improve flexibility and there was no difference between the experimental group and the control group after aquatic exercise (35). Compared with before exercise in the study of Hafele, Alberton, Hafele et al. (31), 16 weeks of aquatic aerobic exercise and combined of aquatic aerobic and resistance exercise did not improve agility, and there was no difference between groups for agility (31). In a systematic review and meta-analysis, Saquetto et al. (36), confirmed that aquatic exercise can significantly improve LLS, flexibility, agility, and aerobic capacity (36). However, studies are lacking for the arrival at a consensus on the issue. In addition, the different types of exercises (aquatic aerobic, resistance, and multicomponent exercise) were not taken into account in most studies, which may result in different benefits from different exercise types. Furthermore, considering the different menopausal ages (37, 38), studies on the different physical fitness benefits were needed to analyze specifically from participating in aquatic exercise between young and older postmenopausal women. In terms of QoL, Hafele et al. (39) found that 16 weeks of aquatic aerobic exercise and combined aquatic aerobic and resistance exercises can significantly improve the overall QoL in postmenopausal women (39). Silva et al. (34) found that aquatic aerobic exercise significantly improved overall QoL compared with pre-exercise, unlike combined aerobic and resistance exercises (34). Therefore, taking into account the influences of exercise types and ages of participants, the present study systematically evaluated and updated the effects of aquatic exercise on physical fitness and overall QoL in postmenopausal women.
The present study strictly followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (40).
We systematically searched the databases (Cochrane Library, PubMed, Web of Science, and MEDLINE) for randomized controlled trials (RCTs) using the following search terms: (aquatic exercise OR water-based exercise OR water exercise OR head-out water exercise) AND (functional fitness OR physical fitness OR physical capacity OR agility OR flexibility OR cardiorespiratory fitness OR aerobic capacity OR strength endurance OR strength OR quality of life) AND (postmenopausal women OR old women OR older women). All search terms were required to appear in the title or abstract. We also reviewed the reference list of the included literature. The Search was limited to database inception until July 2022. Two researchers (WSZ and SJM) independently completed the databases searching.
(i) RCTs; (ii) with exercise intervention as aquatic exercise or head-out water-based exercise; the control group did not participate in exercise. (iii) with participants being physiological postmenopausal women or women aged > 55 years (41–44); and (iv) with outcomes including physical fitness indicators and the overall QoL.
Two researchers (W-SZ and S-JM) independently conducted the selection of titles and abstracts from each database. The full text was obtained if the researchers deemed one study eligible. Two researchers (W-SZ and S-JM) independently extracted the study characteristics from eligible articles, including authors, publication year, age, sample size, exercise interventions, and primary outcomes. The corresponding authors of these studies were contacted in case of missing data. We deleted articles whose authors could not be reached or could not provide the data. The GetData software was used for extracting data if the results were presented as figures in the included articles (45, 46). Two researchers (W-SZ and S-JM) independently completed the data extraction and review. A third researcher (S-KZ) was invited and a consensus was reached at in case of discrepancies.
The Physiotherapy Evidence Database (PEDro) scale was used to assess the methodological quality of the included articles. The PEDro scale is based on 11 items, including eligibility criteria (not contribute to the total score), random allocation, concealed allocation, similarity baseline, subject blinding, therapist blinding, assessor blinding, >85% retention, intention-to-treat, between-group comparisons, and point and variability measures. Each study was assessed as “yes” (1 point) or “no” (0 points), with a maximum total score of 10. A study is considered to be of very good quality if it has a score of 9 or 10, while a score of 6 to 8 indicates good quality, a score of 4 or 5 indicates moderate quality, and a score of 0 to 3 indicates poor quality (47, 48). Two researchers (S-KZ and HX) independently performed the quality assessment, and a third researcher (W-SZ) was invited and a consensus was reached at if there was any discrepancy.
Data analysis was performed using the Cochrane Collaboration Review Manager (RevMan, version 5.4, Copenhagen, Denmark) software. Standardized mean difference (SMD) was employed if there were different outcome measures (49). I2 index was used to test statistic heterogeneity. An I2 >50% indicated high heterogeneity, and a random-effect model was applied (50). Sensitivity analysis was done by deleting studies one after the other (51). Egger's regression test was used to assess publication bias (52). The statistical significance level was set at p < 0.05.
Using the search strategy, 1,469 studies were retrieved, of which 1,421 studies were deleted because they were duplicates, animal studies, non-RCTs, or included non-postmenopausal women, and so on. Because the participants of 29 studies were on hormonotherapy, nutritional care, or the studies had no control group or failed to extract data, these studies were deleted. Sixteen RCTs (19 comparison groups) were finally included in the present study (Figure 1).
The 16 RCTs were published between 2006 and 2022 and involved 594 participants (320 received aquatic exercise interventions). The participants were aged from 54 to 74.9 years. Exercise duration was from 8 to 24 weeks, exercise frequency was from 2 to 5 times per week, and exercise time was from 30 to 60 min. Aquatic aerobic exercise (1, 28, 31, 32, 34, 35, 39), aquatic resistance exercise (29, 30, 53–55), and multicomponent exercise (aquatic aerobic and resistance exercises) (27, 31, 33, 34, 39, 56, 57) were the main types of exercises involved. The studies of Hafele, Alberton, Hafele, et al. (2022), Hafele, Alberton, Schaun, et al. (2022), and Silva et al. (2018) included both aquatic aerobic and multicomponent exercise (31, 34, 39). The participants compliance ranges from 73.6 to 100%. Each exercise session was supervised by the researchers. The characteristics of the included studies are summarized in Table 1.
The ranges of the quality assessment scores of the included studies was from 3–6. Two studies received scores of 6 (good quality) (31, 39), 13 studies received scores of 4–5 (median quality) (1, 27–30, 32–35, 54–57), and 1 study received scores of 3 (poor quality) (53). The mean score was 4.8 (Table 2).
Using the 30-second chair stand test, LLS was evaluated by 11 RCTs that involved 334 participants. Due to the difference between the studies' assessments, the meta-analysis was performed with SMD. A random-effect model was applied for instances with a high heterogeneity (I2 = 91%, p < 0.00001). Sensitivity analysis results indicated that excluding any single study resulted in no significant effect on the total effect size. Meta-analysis results demonstrated that aquatic exercise can significantly increase LLS (SMD = 1.37, 95% CI: 0.53, 2.21, p = 0.001) (Figure 2).
Subgroup analysis showed that LLS was significantly increased in the age < 65 years (SMD = 3.33, 95% CI: 0.62, 6.03, p = 0.02), aquatic aerobic exercise (SMD = 0.81, 95% CI: 0.03, 1.59, p = 0.04), and Aquatic resistance exercise subgroups (SMD = 4.51, 95% CI: 3.33, 5.68, p < 0.00001). No significant effects were found in the age ≥ 65 years (SMD = 0.55, 95% CI: −0.04, 1.13, p = 0.07) and multicomponent exercise subgroups (SMD = 0.32, 95% CI: −0.23, 0.87, p = 0.26) when compared with the control group (Table 3).
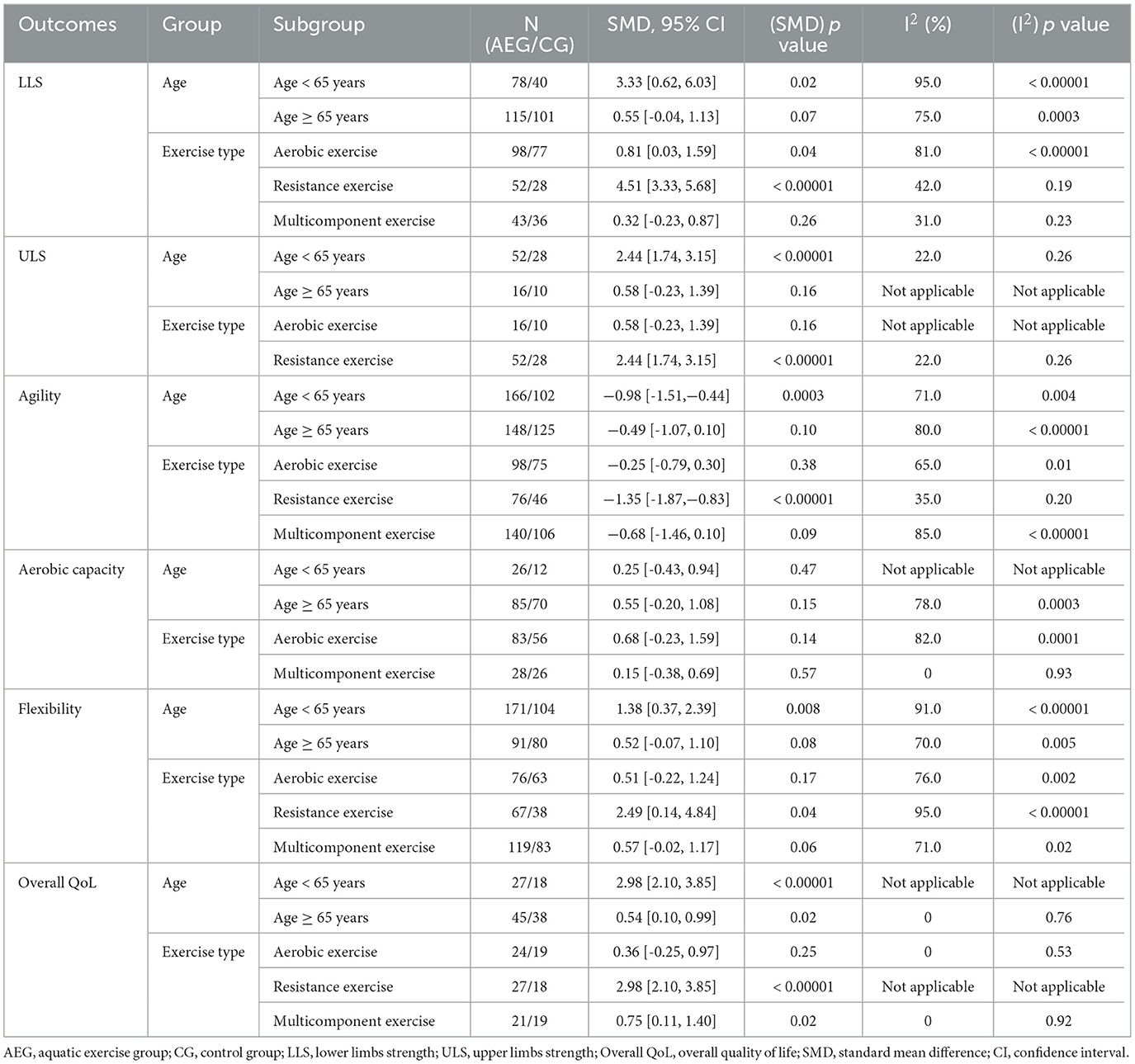
Table 3. Subgroup results of aquatic exercise on physical performance and quality of life according to different age groups and exercise types.
Using the arm curl test, upper limbs strength (ULS) was evaluated by 3 RCTs that involved 106 participants. A meta-analysis was performed with SMD. A random-effect model was applied in instances with a high heterogeneity (I2 = 86%, p = 0.0009). After removing the study of Lopez et al. (32), sensitivity analysis results indicated that the heterogeneity was lower (I2 = 22%, p = 0.26). However, the total effect size did not change significantly. The meta-analysis results demonstrated that aquatic exercise can significantly increase ULS (SMD = 1.86, 95% CI: 0.55, 3.16, p = 0.005) when compared with the control group (Figure 3).
The RCTs of age < 65 years and aquatic resistance exercise subgroups were from the studies of Bocalini et al. (29) and Bocalini et al. (30). Subgroup results showed that ULS had significantly increased in the above two subgroups (SMD = 2.44, 95% CI: 1.74, 3.15, p < 0.00001). The RCTs of age ≥ 65 years were from the study of Lopez et al. (32) and no significant effects were found in the age ≥ 65 years subgroup (SMD = 0.58, 95% CI: −0.23, 1.39, p = 0.16) (Table 3).
Using the timed up and go test, agility was evaluated by 16 RCTs that involved 541 participants. Due to the difference between the studies' assessments, the meta-analysis was performed with SMD. A random-effect model was applied in instances with a high heterogeneity (I2 = 80%, p < 0.00001). Sensitivity analysis results indicated that excluding any single study resulted in no significant effect on the total effect size. The meta-analysis results demonstrated that aquatic exercise can significantly improve agility (SMD = −0.67, 95% CI: −1.09, −0.25, p = 0.002) when compared with the control group (Figure 4).
Subgroup analysis results showed that agility was significantly improved in the age < 65 years (SMD = −0.98, 95% CI: −1.51, −0.44, p = 0.0003) and aquatic resistance exercise subgroups (SMD = −1.35, 95% CI: −1.87, −0.83, p < 0.00001). No significant effects were found in the age ≥ 65 years (SMD = −0.49, 95% CI: −1.07, 0.10, p = 0.10), aquatic aerobic exercise (SMD = −0.25, 95% CI: −0.79, 0.30, p = 0.38), and multicomponent exercise subgroups (SMD = −0.68, 95% CI: −1.46, 0.10, p = 0.09) (Table 3).
Using the 6-minute walking test (6MWT), aerobic capacity was evaluated by 7 RCTs that involved 193 participants. Due to the difference between the studies' assessments, the meta-analysis was performed with SMD. A random-effect model was applied for instances with a high heterogeneity (I2 = 74%, p = 0.0008). Sensitivity analysis results indicated that the heterogeneity was lower (I2 = 3%, p = 0.39) after removing the study of Ha et al. (1). However, the total effect size did not change significantly. The meta-analysis results demonstrated that aquatic exercise does not significantly improve aerobic capacity (SMD = 0.47, 95% CI: −0.14, 1.08, p = 0.13) when compared with the control group (Figure 5).
Subgroup results showed that aerobic capacity was not significantly improved in the age < 65 years (SMD = 0.25, 95% CI: −0.43, 0.94, p = 0.47), age ≥ 65 years (SMD = 0.55, 95% CI: −0.20, 1.29, p = 0.15), aquatic aerobic exercise (SMD = 0.68, 95% CI: −0.23, 1.59, p = 0.14), and multicomponent exercise subgroups (SMD = 0.15, 95% CI: −0.38, 0.69, p = 0.57) (Table 3).
Using the chair sit and reach test, flexibility was evaluated by 12 RCTs that involved 446 participants. Due to the difference between the studies' assessments, the meta-analysis was performed with SMD. A random-effect model was applied for instances with a high heterogeneity (I2 = 86%, p < 0.00001). Sensitivity analysis results indicated that excluding any single study resulted in no significant effect on the total effect size. The meta-analysis results demonstrated that aquatic exercise can significantly improve flexibility (SMD = 0.91, 95% CI: 0.35, 1.47, p = 0.002) when compared with the control group (Figure 6).
Subgroup results showed that flexibility was significantly improved in the age < 65 years (SMD = 1.38, 95% CI: 0.37, 2.39, p = 0.008) and aquatic resistance exercise subgroups (SMD = 2.49, 95% CI: 0.14, 4.84, p = 0.04). No significant effects were found in the age ≥ 65 years (SMD = 0.52, 95% CI:−0.07, 1.10, p = 0.08), aquatic aerobic exercise (SMD = 0.51, 95% CI: −0.22, 1.24, p = 0.17), and multicomponent exercise subgroups (SMD = 0.57, 95% CI: −0.02, 1.17, p = 0.06) (Table 3).
Five RCTs that involved 128 participants evaluated overall QoL using the World Health Organization quality of life assessment. Due to the difference between the studies' assessments, the meta-analysis was performed with SMD. A random-effect model was applied for instances with a high heterogeneity (I2 = 84%, p < 0.0001). Sensitivity analysis results indicated that the heterogeneity was lower (I2 = 0, p = 0.76) after removing the study of Bocalini et al. (30). However, the total effect size did not change significantly. The meta-analysis results demonstrated that when compared with the control group, aquatic exercise can significantly improve overall QoL (SMD = 1.04, 95% CI: 0.06, 2.03, p = 0.04) (Figure 7).
The RCTs of age < 65 years and aquatic resistance exercise subgroups were from the study of Bocalini et al. (30). Subgroup analysis results showed that overall QoL was significantly improved in the age < 65 years, aquatic resistance exercise (SMD = 2.98, 95% CI: 2.10, 3.85, p < 0.00001), age ≥ 65 years (SMD = 0.54, 95% CI: 0.10, 0.99, p =0.02), and multicomponent exercise subgroups (SMD = 0.75, 95% CI: 0.11, 1.40, p =0.02). No significant effects were found in the aquatic aerobic exercise subgroup (SMD = 0.36, 95% CI: −0.25, 0.97, p = 0.25) (Table 3).
Egger test revealed that there was a relatively higher level of publication bias in aerobic capacity (t = −2.67, p = 0.045). There was no obvious publication bias in LLS (t = −1.38, p = 0.201), ULS (t = −0.02, p = 0.984), agility (t = −0.24, p = 0.815), flexibility (t = 0.21, p = 0.838), and overall QoL (t = −1.76, p = 0.177) (Supplementary material).
The present systematic review and meta-analysis demonstrated that aquatic exercise can effectively improve LLS, ULS, agility, flexibility, and overall QoL in postmenopausal women, but has limited effects on aerobic capacity. Aquatic exercise can only significantly improve LLS, ULS, agility, and flexibility in postmenopausal women < 65 years old. There was a significant improvement in overall QoL for both < 65 and ≥ 65 years old. As per our findings, aquatic resistance exercise is the best option for postmenopausal women to improve physical fitness and QoL.
A decline in muscle mass and balance ability in the older adults commonly accompanies the aging process. This leads to limited mobility and loss of independent living ability, which greatly reduces the quality of life of the older adults (58, 59). It is particularly important to maintain LLS in the older adults. Past studies have indicated that LLS is the basic fitness of balance ability and an important factor in fall prevention in the older adults (60). The present study demonstrated that aquatic exercise significantly increases LLS (SMD = 1.37, p = 0.001, n = 334) and ULS (SMD = 1.86, p = 0.005, n = 106). The present findings conform well to those of Saquetto et al. (36), who observed that aquatic exercise significantly increases the muscle strength of knee extension (SMD = 3.34, p = 0.004, n = 216), knee flexion (SMD = 2.51, p = 0.007, n = 82), and arm curl (SMD = 6.78, p = 0.0001, n = 80). In the present review, 11 studies analyzed LLS, and 3 studies analyzed ULS, and the sample size of the included studies was larger. Therefore, our findings further updated the results of the previous study. The results of aquatic exercise efficacy in improving upper and lower extremity muscle strength were confirmed. According to many studies, resistance training can significantly improve muscle strength (61, 62). Resistance exercise in water is a great way for increasing strength, especially for ULS. Most of the studies included showed that the depth of the water reaches the xiphoid, which is beneficial for applying ULS exercise and increasing ULS (63). In addition, walking or jumping in the water is challenged by the drag and resistance of the water, thereby improving lower body muscle strength. The physiological mechanism of aquatic exercise to improve muscle strength mainly due to the improvement of neuromuscular system function (64). The trend of muscle strength decline was reversed (64). Previous studies have suggested that degenerated skeletal muscle recruitment patterns and functions are the main cause of decreased muscle strength (65, 66). Resistance training increases muscle strength by improving neuromuscular recruitment and muscle contraction (66, 67). Moreover, it may also be related to increased muscle mass, which is the main cause of increased muscle strength (68). Previous research confirmed that aquatic exercise significantly increases skeletal muscle mass (69, 70).
It is worth noting that aquatic exercise significantly improves LLS in postmenopausal women < 65 years old (SMD = 3.33, p = 0.02), but no efficacy was found in the ≥ 65 years subgroup. One possible explanation was that higher age-related muscle weakness, poor joint mobility, and poor balance limited body movement in a water environment lead to insufficient exercise intensity (71). Regarding the exercise types, both aquatic aerobic exercise (SMD = 0.81, p = 0.04) and resistance exercise (SMD = 4.51, p < 0.00001) significantly improved LLS. Aquatic resistance exercises induced greater magnitudes of improvement.
Regarding the ULS index, the same two studies were included in the age < 65 years and aquatic resistance exercise subgroups (29, 30). ULS was significantly improved (SMD = 2.44, p < 0.00001), but no efficacy was found in the age ≥ 65 years and aerobic exercise subgroups (SMD = 0.58, p = 0.16). Data for the age ≥ 65 years and aerobic exercise subgroups are from the same study (32). Therefore, the results of these two subgroups should be interpreted and applied with caution, and more studies are needed to be included for a more comprehensive interpretation in the future.
As ages increase, it becomes increasingly challenging for the elder to move quickly and change direction (72, 73). Decreased agility is a key factor in predicting risk for recurrent falls (74). Exercise training is an important way to maintain and improve agility (75). In the present study, agility was significantly improved in the aquatic exercise group compared with the no exercise group (SMD = −0.67, p = 0.002). Our study results were in accordance with the meta-analysis of Saquetto et al. (36), in which 165 participants were included, and agility was significantly increased (SMD = −2.13, p = 0.05). Compared with the study of Saquetto et al. (36), our study has a superiority in including more studies (16 RCTs) and a larger sample size. The effect of improved neuromuscular function on increased muscle strength of the upper and lower limbs may have been responsible for the positive results (76, 77). Agility is the comprehensive embodiment of strength, speed, balance, and coordination, moreover, strength is the foundation of agility (78), and is directly associated with neuromuscular function status (79). In the present study, the overall results showed a significant increase in LLS of 1.37 kg and ULS of 1.86 kg. The results of subgroup showed that agility was improved only in the subgroup with age < 65 years (SMD = −0.98, p = 0.0003). Moreover, only postmenopausal women aged < 65 years showed significant improvement in LLS (SMD = 3.33, p = 0.02) and ULS (SMD = 2.44, p < 0.00001), further emphasizing the importance of strength in improving agility (79, 80). This may also be related to the improvement of joint range of motion. Previous studies have pointed out that agility and flexibility have a significant positive correlation (81), namely the better the flexibility performance, the shorter the agility test time. The present study also indicated that aquatic exercises can significantly improve the flexibility of lower limbs, and thereunto, only the flexibility of the subgroup aged < 65 years was significantly improved (SMD = 1.38, p = 0.008). Therefore, it is believed that the improvement of flexibility may be one of the possible reasons for the improvement of agility. Among the subgroups, agility was found to be improved in the age < 65 years subgroup, emphasizing that changes in agility improved by aquatic exercise were associated with age, precisely a relatively young age can contribute to better effects. Furthermore, subgroup analysis indicated that only aquatic resistance exercises can improve agility, reminding us that the importance and particularity of aquatic resistance exercises should be significantly considered when designing aquatic exercise programs in the future.
6MWT, as an important index that assesses the aerobic capacity, was adopted in the included studies. 6MWT was a submaximal exercise ability test for the middle-aged and the old adults (82, 83). The present study demonstrated that aquatic exercises cannot significantly improve aerobic capacity in postmenopausal women. In addition, subgroup analysis showed that the aerobic capacity was not improved in the aged < 65 years (n = 38), aged ≥ 65 years (n = 155), aerobic exercise (n = 139), and multicomponent exercise subgroups (n = 54). Our findings are consistent with those of the study of Ha et al. (1), who included participants performing aquatic aerobic exercises 3 times a week for a 12-week duration (1). They found that 6MWT was not improved. No significant improvement of 6MWT was found in the study of Perkins et al. (2021) with 60 min of aerobic exercises 5 times a week for a 17-week duration (33). The controversial findings were possibly associated with the low impact when performing aquatic exercises, which was caused by buoyancy and reduced the muscle loads. Although the resistance to water caused the muscle to produce a contractile load, it may not be sufficient to induce a large cardiopulmonary response and therefore did not produce a better adaptive increase in cardiopulmonary function. Furthermore, it may also be related to the lower heart rate level during aquatic exercises. To our knowledge, the reduction in heart rate was mainly due to hydrostatic pressure. Hydrostatic pressure increases venous return and decreases peripheral blood volume. As a result, end-diastolic volume and stroke volume increase, thereby reducing the heart rate (84, 85), accompanied by increased vagal and parasympathetic activity and decreased sympathetic activity caused by atrial and arterial baroreflex mechanisms (86, 87). This results in a lower cardiopulmonary load without an adaptive increase in cardiopulmonary function. We mainly adopted 6MWT to assess the aerobic capacity, and there were also other studies using the VO2max index. The study of Saquetto et al. (36) using VO2max index included 4 articles and the results demonstrated that aquatic exercises could increase VO2max by 4.12 ml/kg, which was inconsistent with the results of our study. Therefore, there was still some controversy about the results of aquatic exercise on improving the aerobic capacity level, and we should be especially cautious when interpreting and applying these results. Our study indicated that there was a relatively higher level of publication bias in aerobic capacity. It may be mainly related to the small number of the included articles. It is well known that participating in exercise for a period of time is helpful to improve aerobic capacity (88), but in the end, it shows negative results in the present study. It is also may be that the research articles with positive results have not been published or published in non-English journals.
Decreased flexibility is associated with the development of musculoskeletal disorders, progressive disability (89), and an increased risk of falls in middle-aged and old adults (90). Exercise is a favorable way to maintain and improve flexibility (91). The present study demonstrated that aquatic exercises can improve lower limb flexibility in postmenopausal women (SMD = 0.91, p = 0.002). Our study results were consistent with the study of Saquetto et al. (36), including only 3 RCTs vs. 12 RCTs in our study, thereby confirming the effectiveness of aquatic exercises on improving lower limb flexibility. Previous studies have shown that exercises are efficacious in improving flexibility. Aquatic exercises, as an intervention method in our study, can make people more relaxed and the action more stretched. Moreover, the buoyancy of water can reduce the fear of falling in middle-aged and old postmenopausal women, and higher water temperature had the effect of hot compress and massage, which further reduced the stiffness of tissues and muscles around joints (92), thus bringing better advantages to the improvement of joint mobility. In addition, our study has confirmed the effectiveness of aquatic exercise on improving muscle strength, especially the increased muscle strength of the lower limbs leading to more stable joints. Under the hydrostatic pressure of water, the blood circulation is better, the blood flow around the joint is more, and the metabolic wastes are recovered and disposed of, thus improving the range of motion of the joint. The subgroup analysis results of the study showed that the flexibility of the aged < 65 years (SMD = 1.38, p = 0.008) and the resistance exercises subgroups (SMD = 2.49, p = 0.04) was significantly increased, while the aged ≥ 65 years, aerobic exercises, and combination exercises subgroups were not significantly improved. It followed then that aquatic exercise can improve the flexibility of postmenopausal women aged < 65 years, and resistance exercise had a better effect on improving flexibility. Due to the importance of flexibility to the ability of voluntary physical activity and fall prevention, older adults should maintain a certain range of joint motion (93).
The decline of physical function associated with aging influenced the ability of daily independent living of older adults. Meanwhile, they had various chronic diseases and emotional burdens, which affect the overall QoL (16, 94, 95). The present study demonstrated that aquatic exercises can significantly improve the overall QoL in postmenopausal women (SMD = 1.04, p = 0.04), moreover, subgroup analysis indicated that aquatic exercises were significantly associated with the effectiveness in the subgroup aged < 65 years and ≥ 65 years. Since only one article was included in the subgroup of age < 65 years (30), caution should be used in the interpretation and application of this finding. Most noteworthy, although no significant improvement was observed in ULS, LLS, agility, and flexibility in the subgroup aged ≥ 65years, aquatic exercise had positive effects on postmenopausal women of this age. It was concluded that aquatic exercise may be a better exercise method to improve the overall QoL of old postmenopausal women. Our findings are consistent with those of the study of Hafele et al. (39), which used aquatic aerobic exercise or a combination of aquatic aerobic and resistance exercise for 60 min three times a week for 16 weeks and showed significant improvements in overall QoL in both exercise intervention groups. However, there was no improvement in the control group (39). Similar to our study, Silva et al. (34) showed a significant 17% improvement in overall QoL in the aquatic aerobic exercise group adopting 12-week aquatic aerobic exercise or a combined aquatic aerobic and resistance exercise intervention with exercise twice a week. Although no beneficial effect of combined aquatic aerobic and resistance exercise was found (34), there was no denying of the relevance of aquatic exercises via improving postmenopausal women population in the area of the body (relating to the pain or discomfort, energy or fatigue, sleep, rest, mobility, daily activities, drug dependence and performance), psychology (including emotion, learning, memory and attention, self-esteem, appearance, spiritual, social, religious, and positive or negative thinking), social identity (personal relationship, social support and sex) and environment (including physical safety, home environment, financial security, information evaluating opportunities, participate in social or cultural activities and leisure time activities). This can be explained by previous studies, which showed that social and psychological problems such as depression, anxiety, or social isolation were significantly associated with chronic diseases (30, 96). In addition, subgroup analysis results showed that the resistance exercise and combination exercise subgroups had a significant improvement in overall QoL, while the aerobic exercise subgroup had no significant effect. The importance of resistance training for postmenopausal women was further emphasized here.
There are some limitations in the present study. First, few high-quality studies were included, and most were of moderate quality, especially in terms of blinding subjects, coaches, and measurements. Second, although more articles were included than the study of Saquetto et al. (36), there may still be the risk of insufficient literatures in the analysis of some indexes, especially in the subgroup analysis, so the results of the present study should be interpreted with caution when practicing.
In the present systematic review and meta-analysis, we evaluated and updated the effects of aquatic exercise on physical fitness and quality of life (QoL) in postmenopausal women. The present findings indicate that, aquatic exercise significantly improved ULS, LLS, agility, flexibility, and overall QoL in postmenopausal women. Aquatic resistance exercise is recommended as the best option for postmenopausal women to improve physical fitness and QoL.
Aquatic exercise significantly improved ULS, LLS, agility, flexibility, and overall QoL in postmenopausal women compared to those with no exercise. The beneficial efficacy of aquatic exercise on ULS, LLS, agility, and flexibility was only seen in postmenopausal women < 65 years old, but that on the overall QoL was seen both in postmenopausal women < 65 years old and ≥ 65 years old. Resistance exercise was better than aerobic/multicomponent exercise in the spectrum of aquatic exercise.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
W-SZ conceptualized the study, searched the databases, extracted the data, performed the statistical analyses, and wrote an original draft. S-JM searched the databases, extracted the data, and reviewed, and edited the original draft. S-KZ evaluated the methodological quality and performed the statistical analyses. HX evaluated the methodological quality. W-LL edited the final draft. All the authors have reviewed and approved the final version of the manuscript.
This research was funded by the Project Funding of Humanities and Social Sciences of the Ministry of Education in China (21YJC890051 to W-SZ).
We are very grateful to all authors. We would like to thank Keteng Edit (www.ketengedit.com) for its linguistic assistance in the present study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1126126/full#supplementary-material
1. Ha MS, Kim JH, Ha SM, Kim YS, Kim DY. Positive influence of aqua exercise and burdock extract intake on fitness factors and vascular regulation substances in elderly. J Clin Biochem Nutr. (2019) 64:73–8. doi: 10.3164/jcbn.18-60
2. He W, Sengupta M, Velkoff VA, DeBarros KA. 65+ in the United States: 2005. New York, NY: Citeseer (2005).
3. Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R. Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol. (2000) 88:1321–6. doi: 10.1152/jappl.2000.88.4.1321
4. Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. (2011) 10:430–9. doi: 10.1016/j.arr.2011.03.003
5. Thelen DG, Wojcik LA, Schultz AB, Ashton-Miller JA, Alexander NB. Age differences in using a rapid step to regain balance during a forward fall. J Gerontol A Biol Sci Med Sci. (1997) 1:M8–13. doi: 10.1093/gerona/52a.1.m8
6. Grounds M, Pinniger GJ. What is the mechanism for in vivo loss of skeletal muscle function in elderly women? Acta Physiol. (2015) 215:9–12. doi: 10.1111/apha.12547
7. Geusens P, Milisen K, Dejaeger E, Boonen S. Falls and fractures in postmenopausal women: a review. J Br Menopause Soc. (2003) 9:101–6. doi: 10.1258/136218003100322314
8. Fragala MS, Kenny AM, Kuchel GA. Muscle quality in aging: a multi-dimensional approach to muscle functioning with applications for treatment. Sports Med. (2015) 45:641–58. doi: 10.1007/s40279-015-0305-z
9. Shore WS, DeLateur BJ. Prevention and treatment of frailty in the postmenopausal woman. Phys Med Rehabil Clin N Am. (2007) 18:609–21. doi: 10.1016/j.pmr.2007.04.004
11. Follis S, Cook A, Bea JW, Going SB, Laddu D, Cauley JA, et al. Association between sarcopenic obesity and falls in a multiethnic cohort of postmenopausal women. J Am Geriatr Soc. (2018) 66:2314–20. doi: 10.1111/jgs.15613
12. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. (2001) 82:1050–6. doi: 10.1053/apmr.2001.24893
13. Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. (2009) 360:2390–3. doi: 10.1056/NEJMp0900963
14. Sieri T, Beretta G. Fall risk assessment in very old males and females living in nursing homes. Disabil Rehabil. (2004) 26:718–23. doi: 10.1080/09638280410001704304
15. An HY, Chen W, Wang CW, Yang HF, Huang WT, Fan SY. The relationships between physical activity and life satisfaction and happiness among young, middle-aged, and older adults. Int J Environ Res Public Health. (2020) 17:4817. doi: 10.3390/ijerph17134817
16. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. (2009) 374:1196–208. doi: 10.1016/S0140-6736(09)61460-4
17. Iglesias C, Manca A, Torgerson D. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. (2009) 20:869–78. doi: 10.1007/s00198-008-0753-5
18. Mehta SP, MacDermid JC, Richardson J, MacIntyre NJ, Grewal R. Reliability and validity of selected measures associated with increased fall risk in females over the age of 45 years with distal radius fracture–A pilot study. J Hand Ther. (2015) 28:2–10. doi: 10.1016/j.jht.2014.09.009
19. Williams LJ, Berk M, Henry MJ, Stuart AL, Brennan SL, Jacka FN, et al. Depression following fracture in women: a study of age-matched cohorts. BMJ Open. (2014) 4:e004226. doi: 10.1136/bmjopen-2013-004226
20. Curfman GD. The health benefits of exercise. A critical reappraisal N Engl J Med. (1993) 328:574–6. doi: 10.1056/NEJM199302253280810
21. Scully D, Kremer J, Meade MM, Graham R, Dudgeon K. Physical exercise and psychological well being: a critical review. Br J Sports Med. (1998) 32:111–20. doi: 10.1136/bjsm.32.2.111
22. Batterham SI, Heywood S, Keating JL. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Disord. (2011) 12:123. doi: 10.1186/1471-2474-12-123
23. Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise in patients with coronary artery disease: effects on body composition, blood lipids, and physical fitness. Am Heart J. (2007) 154:560. doi: 10.1016/j.ahj.2007.06.029
24. Zhou WS, Ren FF, Yang Y, Chien KY. Aquatic exercise for health promotion: a 31-year bibliometric analysis. Percept Mot Skills. (2021) 128:2166–85. doi: 10.1177/00315125211032159
25. Lim JY, Tchai E, Jang SN. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PMR. (2010) 2:723–93. doi: 10.1016/j.pmrj.2010.04.004
26. Kargarfard M, Shariat A, Ingle L, Cleland JA, Kargarfard M. Randomized controlled trial to examine the impact of aquatic exercise training on functional capacity, balance, and perceptions of fatigue in female patients with multiple sclerosis. Arch Phys Med Rehabil. (2018) 99:234–41. doi: 10.1016/j.apmr.2017.06.015
27. Tsourlou T, Benik A, Dipla K, Zafeiridis A, Kellis S. The effects of a twenty-four-week aquatic training program on muscular strength performance in healthy elderly women. J Strength Cond Res. (2006) 20:811–8. doi: 10.1519/R-18455.1
28. Aboarrage Junior AM, Teixeira CVS, Dos Santos RN, Machado AF, Evangelista AL, Rica RL, et al. A High-Intensity Jump-Based Aquatic Exercise Program Improves Bone Mineral Density and Functional Fitness in Postmenopausal Women. Rejuvenation Res. (2018) 21:535–40. doi: 10.1089/rej.2018.2069
29. Bocalini DS, Serra AJ, Murad N, Levy RF. Water- versus land-based exercise effects on physical fitness in older women. Geriatr Gerontol Int. (2008) 8:265–71. doi: 10.1111/j.1447-0594.2008.00485.x
30. Bocalini DS, Serra AJ, Rica RL, Dos Santos L. Repercussions of training and detraining by water-based exercise on functional fitness and quality of life: a short-term follow-up in healthy older women. Clinics. (2010) 65:1305–9. doi: 10.1590/s1807-59322010001200013
31. Hafele MS, Alberton CL, Hafele V, Schaun GZ, Nunes GN, Calonego C, et al. Water-based training programs improve functional capacity, cognitive and hemodynamic outcomes? the active randomized clinical trial. Res Q Exerc Sport. (2022) 4:1–11. doi: 10.1080/02701367.2021.1935433
32. Lopez JAH, Martinez PYO, Meza EIA, Moncada-Jimenez JA, Bertruy OG, Dantas EHM. Programa de entrenamiento de hidrogimnasia sobre las capacidades físicas de adultas mayores / hydrogymnastics training program on physical fitness in elderly women. Revista Internacional De Medicina Y Ciencias De La Actividad Física Y Del Deporte. (2017) 17:283–98. doi: 10.15366/rimcafd2017.66.005
33. Perkins KM, Munguia N, Angulo A, Anaya C, Rios R, Velazquez L. Evaluation of aquafitness exercise on the physical and mental health of older women: a pilot study. J Women Aging. (2021) 33:569–82. doi: 10.1080/08952841.2020.1730681
34. Silva MR, Alberton CL, Portella EG, Nunes GN, Martin DG, Pinto SS. Water-based aerobic and combined training in elderly women: Effects on functional capacity and quality of life. Exp Gerontol. (2018) 106:54–60. doi: 10.1016/j.exger.2018.02.018
35. Dong-Hyun K, Hyun-Hun J, Seul-Hee L, Yun-Hwan K, Il-Kyu P, Sang-Kab P, et al. Effects of aquarobic on health-related physical fitness, cardiovascular factor and frailty-index in pre-frailty elderly women with hypertension. Archives of Budo. (2019) 15:83–91. doi: 10.1039/C3TA13266H
36. Saquetto MB, Dos Santos MR, Alves IGN, Queiroz RS, Machado RM, Neto MG. Effects of water-based exercises on functioning of postmenopausal women: a systematic review with meta-analysis. Exp Gerontol. (2022) 166:111875. doi: 10.1016/j.exger.2022.111875
37. Bailey A. Menopause and physical fitness. Menopause. (2009) 16:856–7. doi: 10.1097/gme.0b013e3181b0d018
38. Cooper GS, Sandler DP. Age at natural menopause and mortality. Ann Epidemiol. (1998) 8:229–35. doi: 10.1016/s1047-2797(97)00207-x
39. Häfele MS, Alberton CL, Schaun GZ, Häfele V, Nunes GN, Andrade LS, et al. Quality of life responses after combined and aerobic water-based training programs in older women: a randomized clinical trial (ACTIVE Study). Aging Clin Exp Res. (2022) 34:1123–31. doi: 10.1007/s40520-021-02040-5
40. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
41. Brett KM, Cooper GS. Associations with menopause and menopausal transition in a nationally representative US sample. Maturitas. (2003) 45:89–97. doi: 10.1016/s0378-5122(03)00139-7
42. Ho SC, Chan SG, Yip YB, Cheng A, Yi Q, Chan C. Menopausal symptoms and symptom clustering in Chinese women. Maturitas. (1999) 33:219–27. doi: 10.1016/s0378-5122(99)00056-0
43. Loh FH, Khin LW, Saw SM, Lee JJ, Gu K. The age of menopause and the menopause transition in a multiracial population: a nation-wide Singapore study. Maturitas. (2005) 52:169–80. doi: 10.1016/j.maturitas.2004.11.004
44. McKinlay SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. (2008) 61:4–16. doi: 10.1016/j.maturitas.2008.09.005
45. Zein H, Tran V, Abdelmotaleb Ghazy A, Mohammed AT, Ahmed A, Iraqi A, et al. How to Extract Data from Graphs using Plot Digitizer or Getdata Graph Digitizer (2015). Available online at: https://www.researchgate.net/publication/279285765_How_to_Extract_Data_from_Graphs_using_Plot_Digitizer_or_Getdata_Graph_Digitizer
46. Wang R, Yao Q, Chen W, Gao F, Li P, Wu J, et al. Stem cell therapy for Crohn's disease: systematic review and meta-analysis of preclinical and clinical studies. Stem Cell Res Ther. (2021) 12:463. doi: 10.1186/s13287-021-02533-0
47. Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther. (2008) 88:156–75. doi: 10.2522/ptj.20070147
48. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. (2003) 83:713–21. doi: 10.1093/ptj/83.8.713
49. Andrade C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. (2020) 81:20f13681. doi: 10.4088/JCP.20f13681
50. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
51. Tobias A. Assessing the influence of a single study in the meta-analysis estimate. Stata Tech Bull. (1999) 8:15–7.
52. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
53. Araújo JP, Neto GR, Loenneke JP, Bemben MG, Laurentino GC, Batista G, et al. The effects of water-based exercise in combination with blood flow restriction on strength and functional capacity in post-menopausal women. Age. (2015) 37:110. doi: 10.1007/s11357-015-9851-4
54. Colado JC, Triplett NT, Tella V, Saucedo P, Abellán J. Effects of aquatic resistance training on health and fitness in postmenopausal women. Eur J Appl Physiol. (2009) 106:113–22. doi: 10.1007/s00421-009-0996-7
55. Sattar M, Esfarjani F, Nezakat-Alhosseini M, Kordavani L. Effect of aquatic resistance training on blood pressure and physical function of postmenopausal women. ARYA Atherosclerosis 178–82. Available online at: https://arya.mui.ac.ir/article_10824.html
56. Bento PCB. Lopes MdFA, Cebolla EC, Wolf R, Rodacki AL. Effects of water-based training on static and dynamic balance of older women. Rejuvenation Res. (2015) 18:326–31. doi: 10.1089/rej.2014.1650
57. Moreira L, Fronza FC, dos Santos RN, Teixeira LR, Kruel LF, Lazaretti-Castro M. High-intensity aquatic exercises (HydrOS) improve physical function and reduce falls among postmenopausal women. Menopause. (2013) 20:1012–9. doi: 10.1097/GME.0b013e3182850138
58. Daley MJ, Spinks WL. Exercise, mobility and aging. Sports Med. (2000) 29:1–12. doi: 10.2165/00007256-200029010-00001
59. Hicks GE, Shardell M, Alley DE, Miller RR, Bandinelli S, Guralnik J, et al. Absolute strength and loss of strength as predictors of mobility decline in older adults: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. (2012) 67:66–73. doi: 10.1093/gerona/glr055
60. Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. (2004) 52:1121–9. doi: 10.1111/j.1532-5415.2004.52310.x
61. Charette S, McEvoy L, Pyka G, Snow-Harter C, Guido D, Wiswell R, et al. Muscle hypertrophy response to resistance training in older women. J Appl Physiol. (1991) 70:1912–6. doi: 10.1152/jappl.1991.70.5.1912
62. Schoenfeld BJ. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. (2010) 24:2857–72. doi: 10.1519/JSC.0b013e3181e840f3
63. Graef FI, Pinto RS, Alberton CL, De Lima WC, Kruel LF. The effects of resistance training performed in water on muscle strength in the elderly. J Strength Cond Res. (2010) 24:3150–6. doi: 10.1519/JSC.0b013e3181e2720d
64. Moritani T. Neuromuscular adaptations during the acquisition of muscle strength, power and motor tasks. J Biomech. (1993) 26:95–107. doi: 10.1016/0021-9290(93)90082-p
65. Chien KY, Kan NW, Liao YH, Lin YL, Lin CL, Chen WC. Neuromuscular activity and muscular oxygenation through different movement cadences during in-water and on-land knee extension exercise. J Strength Cond Res. (2017) 31:750–7. doi: 10.1519/JSC.0000000000001524
66. Cormie P, McGuigan MR, Newton RU. Developing maximal neuromuscular power: Part 1–biological basis of maximal power production. Sports Med. (2011) 41:17–38. doi: 10.2165/11537690-000000000-00000
67. Folland JP, Williams AG. Morphological and neurological contributions to increased strength. Sports Med. (2007) 37:145–68. doi: 10.2165/00007256-200737020-00004
68. Reed RL, Pearlmutter L, Yochum K, Meredith KE, Mooradian AD. The relationship between muscle mass and muscle strength in the elderly. J Am Geriatr Soc. (1991) 39:555–61. doi: 10.1111/j.1532-5415.1991.tb03592.x
69. Irandoust K, Taheri M. The effects of aquatic exercise on body composition and nonspecific low back pain in elderly males. J Phys Ther Sci. (2015) 27:433–5. doi: 10.1589/jpts.27.433
70. Pöyhönen T, Sipilä S, Keskinen KL, Hautala A, Savolainen J, Mälkiä E. Effects of aquatic resistance training on neuromuscular performance in healthy women. Med Sci Sports Exerc. (2002) 34:2103–9. doi: 10.1249/01.MSS.0000039291.46836.86
71. Cadore EL, Izquierdo M. Exercise interventions in polypathological aging patients that coexist with diabetes mellitus: improving functional status and quality of life. Age. (2015) 37:64. doi: 10.1007/s11357-015-9800-2
72. Carmeli E, Reznick AZ, Coleman R, Carmeli V. Muscle strength and mass of lower extremities in relation to functional abilities in elderly adults. Gerontology. (2000) 46:249–57. doi: 10.1159/000022168
73. Simons R, Andel R. The effects of resistance training and walking on functional fitness in advanced old age. J Aging Health. (2006) 18:91–105. doi: 10.1177/0898264305281102
74. Toraman A, Yildirim NÜ. The falling risk and physical fitness in older people. Arch Gerontol Geriatr. (2010) 51:222–6. doi: 10.1016/j.archger.2009.10.012
75. Kallinen M, Markku A. Aging, physical activity and sports injuries. Sports Med. (1995) 20:41–52. doi: 10.2165/00007256-199520010-00004
76. Fatouros I, Kambas A, Katrabasas I, Nikolaidis K, Chatzinikolaou A, Leontsini D, et al. Strength training and detraining effects on muscular strength, anaerobic power, and mobility of inactive older men are intensity dependent. Br J Sports Med. (2005) 39:776–80. doi: 10.1136/bjsm.2005.019117
77. Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C, Kaliton D, et al. The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci. (2004) 59:154–60. doi: 10.1093/gerona/59.2.m154
78. Sonoda T, Tashiro Y, Suzuki Y, Kajiwara Y, Zeidan H, Yokota Y, et al. Relationship between agility and lower limb muscle strength, targeting university badminton players. J Phys Ther Sci. (2018) 30:320–3. doi: 10.1589/jpts.30.320
79. Barber-Westin S, Noyes FR. (2019). Neuromuscular Function, Agility, and Aerobic Testing. Return to Sport after ACL Reconstruction and Other Knee Operations. Cham: Springer.
80. Granacher U, Muehlbaue T, Zahner L, Gollhofer A, Kressig RW. Comparison of traditional and recent approaches in the promotion of balance and strength in older adults. Sports Med. (2011) 41:377–400. doi: 10.2165/11539920-000000000-00000
81. Tatlisu B, Karakurt S, Agirbas O, Ucan I. The relationship beetwen strength, speed, flexibility, agility, and anaerobic power in elite athletes. Int J Appl Exerc Physiol. (2019) 8:66–71. doi: 10.13140/RG.2.2.23990.37445
82. Balke B. (1963). A Simple Field Test for The Assessment of Physical Fitness. Oklahoma City, Okla: Civil Aeromedical Research Institute.
83. Kervio G, Carre F, Ville NS. Reliability and intensity of the six-minute walk test in healthy elderly subjects. Med Sci Sports Exerc. (2003) 35:169–74. doi: 10.1097/00005768-200301000-00025
84. Barbosa TM, Garrido MF, Bragada J. Physiological adaptations to head-out aquatic exercises with different levels of body immersion. J Strength Cond Res. (2007) 21:1255–9. doi: 10.1519/R-20896.1
85. Pendergast DR, Lundgren CE. The underwater environment: cardiopulmonary, thermal, and energetic demands. J Appl Physiol (1985). (2009) 106:276–83. doi: 10.1152/japplphysiol.90984.2008
86. Al Haddad H, Laursen PB, Chollet D, Lemaitre F, Ahmaidi S, Buchheit M. Effect of cold or thermoneutral water immersion on post-exercise heart rate recovery and heart rate variability indices. Auton Neurosci. (2010) 156:111–6. doi: 10.1016/j.autneu.2010.03.017
87. Buchheit M, Peiffer JJ, Abbiss CR, Laursen PB. Effect of cold water immersion on postexercise parasympathetic reactivation. Am J Physiol Heart Circ Physiol. (2009) 296:H421–7. doi: 10.1152/ajpheart.01017.2008
88. Andrade LS, Pinto SS, Silva MR, Schaun GZ, Portella EG, Nunes GN, et al. Water-based continuous and interval training in older women: Cardiorespiratory and neuromuscular outcomes (WATER study). Exp Gerontol. (2020) 134: 110914. doi: 10.1016/j.exger.2020.110914
89. Rikli RE, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60-94. J Aging Phys Act. (1999) 7:162-81. doi: 10.1123/japa.7.2.162
90. American College of Sports Medicine. (2013). ACSM's Guidelines for Exercise Testing and Prescription. New York, NY: Lippincott williams & wilkins.
91. Zhou WS, Lin JH, Chen SC, Chien KY. Effects of dynamic stretching with different loads on hip joint range of motion in the elderly. J Sports Sci Med. (2019) 18:52–7.
92. Kargarfard M, Dehghadani M, Ghias R. The effect of aquatic exercise therapy on muscle strength and joint's range of motion in hemophilia patients. Int J Prev Med. (2013) 4:50–56.
93. Gardner MM, Robertson MC, Campbell AJ. Exercise in preventing falls and fall related injuries in older people: a review of randomised controlled trials. Br J Sports Med. (2000) 34:7–17. doi: 10.1136/bjsm.34.1.7
94. Masoudi FA, Rumsfeld JS, Havranek EP, House JA, Peterson ED, Krumholz HM, et al. Age, functional capacity, and health-related quality of life in patients with heart failure. J Card Fail. (2004) 10:368–73. doi: 10.1016/j.cardfail.2004.01.009
95. Öztürk A, Simşek TT, Yümin ET, Sertel M, Yümin M. The relationship between physical, functional capacity and quality of life (QoL) among elderly people with a chronic disease. Arch Gerontol Geriatr. (2011) 53:278–83. doi: 10.1016/j.archger.2010.12.011
Keywords: hydrotherapy, head-out water exercise, older women, physical performance, muscle strength, agility
Citation: Zhou W-S, Mao S-J, Zhang S-K, Xu H and Li W-L (2023) Effects of aquatic exercises on physical fitness and quality of life in postmenopausal women: an updated systematic review and meta-analysis. Front. Public Health 11:1126126. doi: 10.3389/fpubh.2023.1126126
Received: 17 December 2022; Accepted: 19 May 2023;
Published: 08 June 2023.
Edited by:
Yanan Zhao, Nanjing Normal University, ChinaReviewed by:
Mahdi Hosseinzadeh, Sports Sciences Research Institute of Iran (SSRII), IranCopyright © 2023 Zhou, Mao, Zhang, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Sheng Zhou, emhvdXdlbnNoZW5nQG5qeHpjLmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.