- 1School of Nursing, Wannan Medical College, Higher Education Park, Wuhu City, Anhui Province, China
- 2School of Marxism, Jinzhou Medical University, Jinzhou City, Liaoning Province, China
- 3Department of Internal Medicine Nursing, School of Nursing, Wannan Medical College, Higher Education Park, Wuhu City, Anhui Province, China
Objective: Depression in diabetes patients is caused by their own disease or the surrounding social environment. How to cope with changes in mentality and adjust psychological stress responses, especially under China’s dynamic zero COVID-19 policy, is worth further discussion. The researchers constructed a moderated mediation model to test the effect of psychological resilience during dynamic zero COVID-19 on depression in diabetes patients and the mediating role of stigma and the moderating effect of medication burden.
Method: From June to September, 2022, data were collected in Jinghu District, Wuhu City, Anhui Province, by multi-stage stratified sampling. Firstly, we selected a tertiary hospital randomly in Jinghu District. Secondly, departments are randomly chosen from the hospital. Finally, we set up survey points in each department and randomly select diabetes patients. In addition, we used the Connor-Davidson Elasticity Scale (CD-RISC) to measure psychological resilience of patients, and used the Stigma Scale for Chronic Illness (SSCI) to measure stigma, medication burden was measured by the Diabetes Treatment Burden Scale (DTBQ), and depression was assessed by the Patient Health Questionnaire-9 (PHQ-9). We used SPSS (version 23.0) and PROCESS (version 4.1) for data analysis.
Results: (1) Psychological resilience was negatively correlated with stigma, medication burden, and depression. Stigma was positively associated with medication burden and depression. Medication burden and depression are positively correlated, (2) The mediation analysis showed that psychological resilience had a direct predictive effect on depression, and stigma partially mediated the relationship, and (3) Medication burden moderates the direct pathway by which psychological resilience predicts depression; Medication burden moderates the first half of “psychological resilience → stigma → depression.”
Conclusion: Under the mediating effect of stigma, psychological resilience can improve depression. Medication burden has a moderating effect on the relationship between psychological resilience and depression, and it also has a moderating effect on the relationship between psychological resilience and stigma. These results facilitate the understanding of the relationship mechanisms between psychological resilience and depression.
1. Introduction
A health crisis has swept the globe for more than 2 years since the World Health Organization (WHO) officially declared a coronavirus disease (COVID-19) pandemic in 2019 (1). In response to the current situation, the Chinese government has implemented a nationwide “Dynamic Zero COVID-19” policy (2, 3). The policy under the COVID-19 pandemic is also a public health emergency that has had an extremely significant impact on people with diabetes in China (4), as the government has implemented strict control measures requiring people to lock down and stay at home and keep their distance to prevent the spread of the virus (5, 6). Prolonged isolation and uncertainty can easily worsen the psychological condition of people with diabetes (7). Dynamic clearance policies and isolation can easily have a range of consequences for people with diabetes: sudden community closure, chronic and acute stress, fear of infection and concerns about accessing medical care and self-management of blood glucose (8, 9). All these adverse factors may trigger depression (10, 11). People with diabetes are a more susceptible group compared to the normal population (12).
Globally, depression is the second leading cause of disability, characterized by loss of happiness, depressed mood and suicidal behaviors (13). Depression is a common mental illness among people with diabetes and can debilitate and impair the mental health of patients (14). There is a bidirectional association between diabetes and depression, with depression being associated with a 60% increased risk of T2DM as reported in a meta-analysis (15). A prospective study (16) showed a 1.6-fold increase in the prevalence of mild or greater depressive symptoms among older adults with type 2 diabetes and overweight/obesity in the United States from before COVID-19 to the COVID-19 pandemic. Also, in previous studies (17, 18), co-occurrence of psychiatric disorders (e.g., depression) was more prevalent in patients with diabetes than in the general population, with prevalence rates ranging from 15–24% and a prevalence of 12.61 cases of depression per 1,000 patients in the first year after initiation of oral antidiabetic therapy. These results suggest the importance of developing strategies to mitigate the negative impact on the mental health of people with diabetes during COVID-19.
Many factors can affect depression, including psychological resilience. Psychological resilience (PR) plays an important role in adapting to the changes brought about by a pandemic and seeking to restore psychological well-being in people with diabetes (19). PR refers to an individual’s ability or dynamic process to adapt and thrive after a serious threat. Past research (20–22) has reported that PR can buffer t the psychological trauma caused by sudden public health events, depression, negative emotions, and chronic illness. It can also help people with diabetes to increase treatment adherence in the face of challenges and difficulties (23). When people are faced with adversity, traumatic events and post-events, their level of PR plays an important role in maintaining or restoring their psychological well-being. Academic research (24, 25) on the relationship between PR and depression has shown a significant correlation between the two. Martin and Marsh reported (26) that PR was a significant predictor of depression in people with diabetes.
The long-term medication burden of diabetes increases the burden of self-experience for patients, who are left in a state of chronic stress and loss of control, triggering stress reactions including depression, anxiety, stigma and other diabetes-related psychological problems (27). Originally defined as “a characteristic of a person whose reputation has been greatly damaged,” stigma often extends to the psychological stigma that patients experience as a result of certain illnesses (28). As a negative emotion, stigma can have a negative impact on treatment adherence and self-management in people with diabetes (29). Stigma also has a negative impact on person’s mental health, often in the form of depression, anxiety, irritability, etc. (30). A study (31) had shown that PR affected the level of stigma of patients and played an important role in reducing the level of stigma, and the higher level of patient’s PR, the lower level of stigma. Meanwhile, PR can also improve the negative emotional state of patients (32). In the USA (33), resilience is negatively associated with depression and general distress in people with diabetes. For people with diabetes in Germany (34), resilience can be considered a non-specific protective factor against depression, anxiety, and impaired quality of life. The association between resilience and depression has been shown to be strong (35). Lower resilience is also considered a predictor of distress and depression during diabetes (36).
Medication burden (MB) is one of the key components of treatment burden. Xin et al. (37) defined medication burden simply as the burden incurred by patients in obtaining, planning, and organizing medication, taking medication, monitoring treatment, and managing adverse drug reactions. MB can seriously affect patient medication adherence, adverse event rates, readmission rates, prolonged hospital stays and reduced physical function (38, 39), as well as increasing the risk of falls, frailty, and patient mortality (40). At the same time, older patients with diabetes or chronic co-morbidities are more likely to develop various psychological problems during long-term multiple medication use (41), such as negative emotions such as anxiety, distress, worry and depression (42).
Therefore, we hypothesized the following: (1) PR is negatively associated with depression in diabetes patients, (2) Stigma mediates the relationship between PR and depression, and (3) MB plays a moderating role in the relationship between PR, stigma, and depression in diabetes patients (Figure 1).
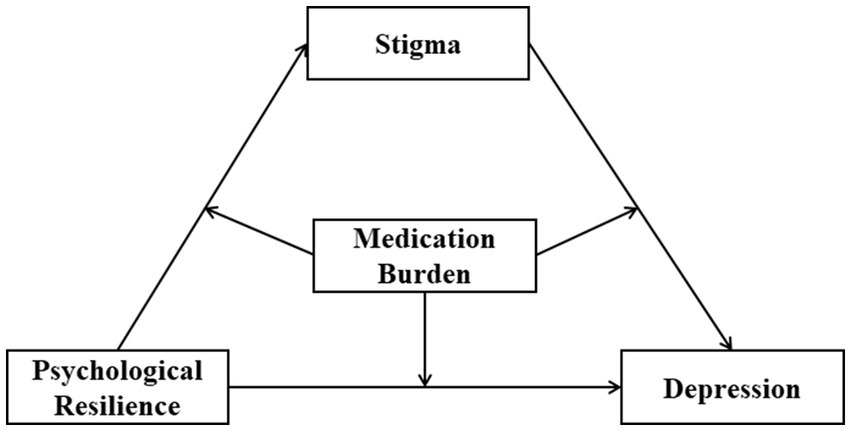
Figure 1. Hypothetical model of the relationships between psychological resilience, stigma, and medication burdenand depression.
2. Materials and methods
2.1. Participants and data collection
Participants were recruited from a tertiary hospital in the Wuhu City (China) by multi-stage sampling. The inclusion criteria were as follows: (i) All patients should meet the diagnostic criteria for DM established by the American Diabetes Association, (ii) Patients are conscious and have full mobility and cognitive ability, and (iii) Patients are willing to cooperate and complete the questionnaire. Exclusion criteria are as follows: (i) presence of severe mental impairment or intellectual problems, (ii) severe diabetic complications or inability to care for themselves, (iii) other serious illnesses such as severe cardiovascular disease, severe infectious diseases, cancer, visual and hearing impairment due to complications of DM, and (iv) pregnancy or other specific diabetes. To reduce errors, relevant personnel was trained before the investigation to clarify communication skills and scoring standards. After obtaining the informed consent of the diabetic, the questionnaire was issued, and the patients answered by themselves. For illiterate patients, the investigators asked face-to-face and then filled out the questionnaire. All methods are implemented following the declaration of Helsinki.
2.2. Sampling and sample size
From June to September 2022, this study used a multi-stage sampling method and random number table method to collect data from tertiary hospitals in Jinghu District, Wuhu City, Anhui Province. Firstly, the First Affiliated Hospital of Wannan Medical College was randomly selected from all tertiary hospitals in Wuhu, Anhui Province. Secondly, four departments were strategically selected from this hospital: endocrinology, geriatrics, traditional Chinese medicine, and dermatology. Thirdly, survey points were set up in each department, and diabetes patients were strategically selected for questionnaire surveys. Based on the criteria proposed by Kendall (5 ~ 10 times the number of items and expanded by at least 10% to ensure an adequate sample size), we need at least 228 samples. Eventually, a total of 334 questionnaires were distributed and 329 valid questionnaires were returned, with a valid return rate of 95.85%.
2.3. Measurements
2.3.1. Psychological resilience
The Conner-Davidson Resilience Questionnaire (CD-RISC) was developed by psychologists Professors Conner and Davidson in 2003 (43). The CD-RISC contains 25 items on a five-point Likert scale ranging from 0 (“not at all true”) to 4 (“almost always true”). The lower the score, the lower the psychological resilience. The score of the items is added up to the total score of the scale, which is 0 ~ 100 points. The higher the score, the higher the level of psychological resilience. The score ≤ 60 is poor, 61 ~ 69 is average, 70 ~ 79 is good, and ≥ 80 is excellent. The scale consists of 5 dimensions. The first dimension (0 ~ 32 scores) reflects high standards, resilience, and ability. The second dimension (0 ~ 28 scores) reflects dealing with emotions and believing in one’s intuition. The third dimension (0 ~ 20 scores) reflects having a constructive attitude towards change and safe relationships. The fourth dimension (0 ~ 12 scores) is perceived control and the fifth dimension (0 ~ 8 scores) is mental strength. The Cronbach’s alpha value (44) for this study scale was 0.861.
2.3.2. Stigma
The Stigma Scale for Chronic Illness (SSCI) was an instrument developed by Rao to measure stigma in people with chronic illnesses (45). It consists of 24 items and two dimensions: intrinsic stigma (0 ~ 52 scores) and extrinsic stigma (0 ~ 44 scores). The first 13 items refer to internal stigma and ask about the respondent’s own feelings of stigma. The next 11 items ask about the stigma that the respondent feels as a result of external actions. A five-point Likert scale ranging from 0 (never) to 4 (always) was used. The total score is 0 ~ 96, with higher scores indicating greater stigma. The Cronbach’s alpha value (46) for this study scale was 0.829.
2.3.3. Medication burden
The Diabetic Treatment Burden Questionnaire (DTBQ) was compiled by Professors Ishii H and Shin K in 2018 (47), and it is used to assess the burden associated with medication in diabetes patients. The DTBQ includes three factors: administrative burden, (0 ~ 60 score) flexibility burden (0 ~ 18 score), and blood glucose control burden (0 ~ 30 score). A seven-point Likert scale ranging from 0 (strongly disagree) to 6 (strongly agree) was used, the total score is 0 ~ 108. Among them, items of 1 ~ 10 are positive scoring, higher scores indicate a more significant treatment burden; items of 11 ~ 18 are inversely scored, with higher scores indicating a lower treatment burden. The Cronbach’s alpha value (48) for this study scale was 0.780.
2.3.4. Depression
The Patient Health Questionaire-9 (PHQ-9) was derived from the depression part in the Patient Health Questionnaire (PHQ) compiled by Spitzer in 1999 (49). PHQ-9 was recommended by the diagnostic and Statistical Manual of mental disorders, Fifth Edition (DSM-5). The response options for the project range from “not at all” (0 points) to “almost every day” (3 points), the total score is 0 ~ 27. Score 0 ~ 4 with no depression, 5 ~ 9 with mild depression, 10 ~ 14 with moderate depression, 15 ~ 19 with moderate to severe depression, and 20 ~ 27 with severe depression. The scale can not only screen for depression but also show the severity of depression. Because of its convenient use, good reliability, and effectiveness, it has been widely used in medical tumor screening in grass-roots hospitals. The Cronbach’s alpha value (50) for this study scale was 0.842.
2.4. Statistical analyses
SPSS23.0 was used to conduct all statistical analyses. Harman single factor test was used for exploratory factor analysis of all the questionnaire items. The results showed that there were 25 factors with eigenvalues greater than 1. The first factor explained only 18.913% of the variance, which was less than 40% critical standard, suggesting that there was no common methodological bias.
We used SPSS 23.0 to accomplish all the statistical analyses. Firstly, we calculated general and controlled variables for descriptive statistics and bivariate correlations. Secondly, we used Hayes’ PROCESS (2013) macro (model 4) to evaluate the mediating effect of stigma. Finally, we analyzed the moderator–mediator model with Hayes’s PROCESS macro (model 8) (2013). All the continuous variables were standardized, and the interaction terms were calculated from these standardized scores. The bootstrap method produces 95% bias-corrected CIs for these effects from 5,000 re-sample of the data. CIs that do not contain zero indicate a significant effect.
2.5. Ethical considerations
Approval for this study was given by the medical ethics committee of Wannan Medical College (approval number 2021-3). All the participants were informed that they would bear no penalty for refusal to participate in the study and would be allowed to withdraw at any time without affecting their treatments. Informed consents were obtained before questionnaires were administered to participants.
3. Results
3.1. Descriptive statistics
Table 1 shows the demographic characteristics of the study objects and a univariate analysis of depression with different features. Of the 329 diabetes patients, 198 (60.2%) were men, and 131 (39.8%) were women. The age range of diabetes patients was 45 ~ 95 years and the mean age being 62.02 ± 11.77 years. There were significant differences in individual monthly income and SMBG. Most patients with diabetes (72.9%) had a middle school education or less. Only 8.5% of diabetes patients were able to SMBG regularly, and more than a third (37.4%) reported a monthly income of less than 1,000 CNY. 7.9% of the older diabetic patients did not have depression. 27.1% of the patients had mild depression; 28.9% of patients were moderately depressed; 27.7% of the patients had moderate to severe depression; 8.4% of older diabetic patients were severely depressed.
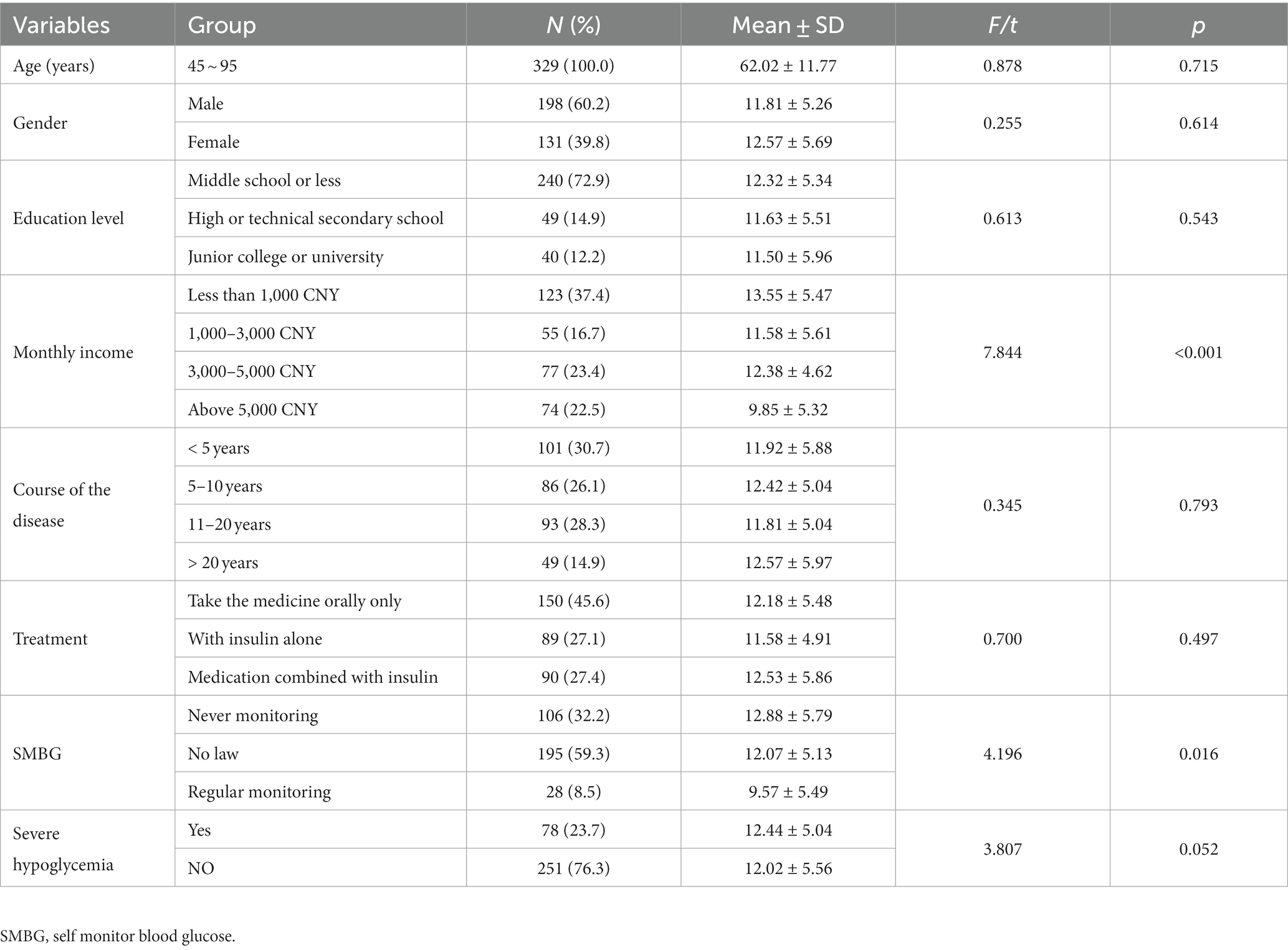
Table 1. Univariate analysis of depression of diabetic patients with different characteristics (n = 329).
3.2. Bivariate correlation analyses
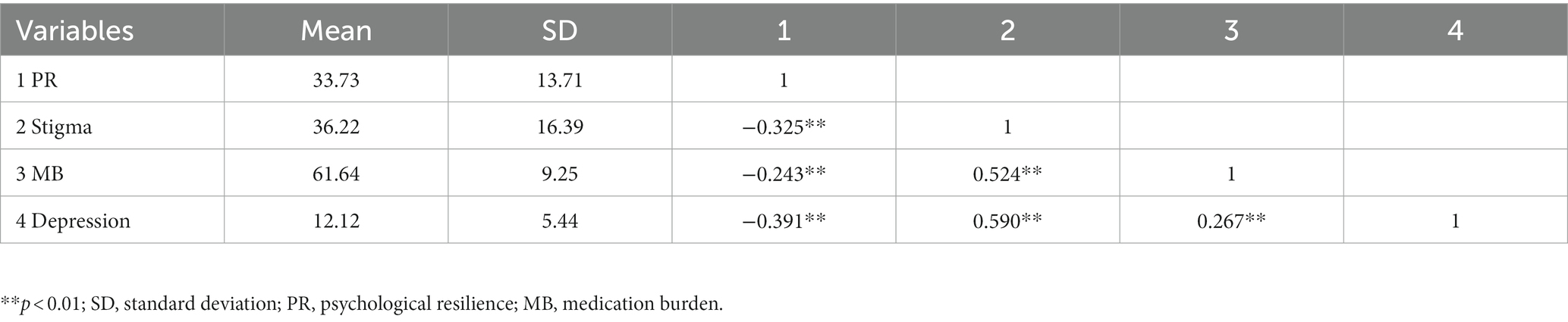
The mean, standard deviation, and correlation between variables are shown in Table 2. The score for depression was 12.12 ± 5.44. The results indicate that PR has a significant and negatively correlated with stigma (r = −0.325, p < 0.01) and MB (r = −0.243, p < 0.01), as well as depression (r = −0.391, p < 0.01).The stigma was positively correlated with MB (r = 0.524, p < 0.01) and depression (r = 0.590, p < 0.01). MB was positively correlated with depression (r = 0.267, p < 0.01).
3.3. The mediation analyses
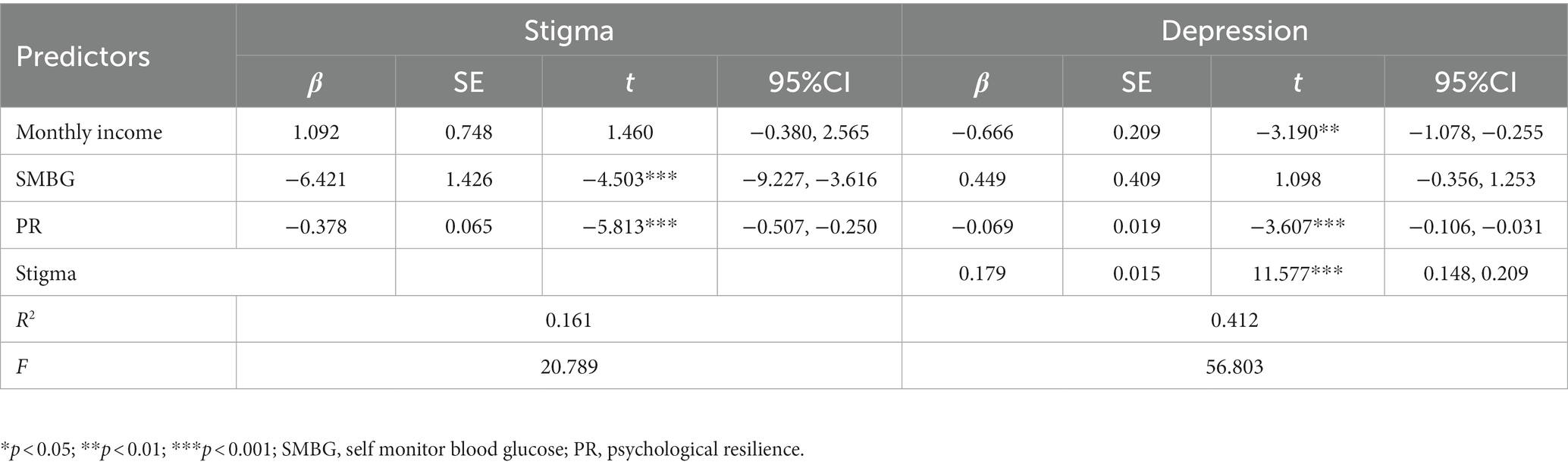
To investigate H1, we examined the mediating effect of stigma on the relationship between PR and depression using the PROCESS 3.3 macro (model 4) proposed by Hayes, after controlling for the variables of monthly income and SMBG demographics (Table 3). The results showed that PR was associated negatively with depression (β = −0.069, p < 0.001), and PR explained a total of 41.2% of depression (F = 56.803, p < 0.001, ΔR2 = 0.412). PR was associated negatively with stigma (β = −0.378, p < 0.001). Stigma was associated positively with depression (β = 0.179, p < 0.001). We examined the indirect effect (β = −0.068, SE =0.015, 95%CI = [−0.098, −0.039]) and direct effects (β = −0.069, SE =0.019, 95%CI = [−0.106, −0.312]) of PR on depression by testing 95% CIs based on 5,000 bootstrapped samples, indicating stigma partially mediated the relationship between PR and depression (Table 4). The indirectly and directly effects accounted for 49.40 and 50.60% of the total effect, respectively.
3.4. The moderation analyses
To examine H2 and H3, we adopted PROCESS macro (Model 8) proposed by Hayes to examine the moderated mediation. Specially, we estimated parameters for two models. In Model 1, we estimated the moderating effect of MB on the relationship between PR and depression. In Model 2, we estimated the moderating effect of MB on the relationship between depression and stigma.
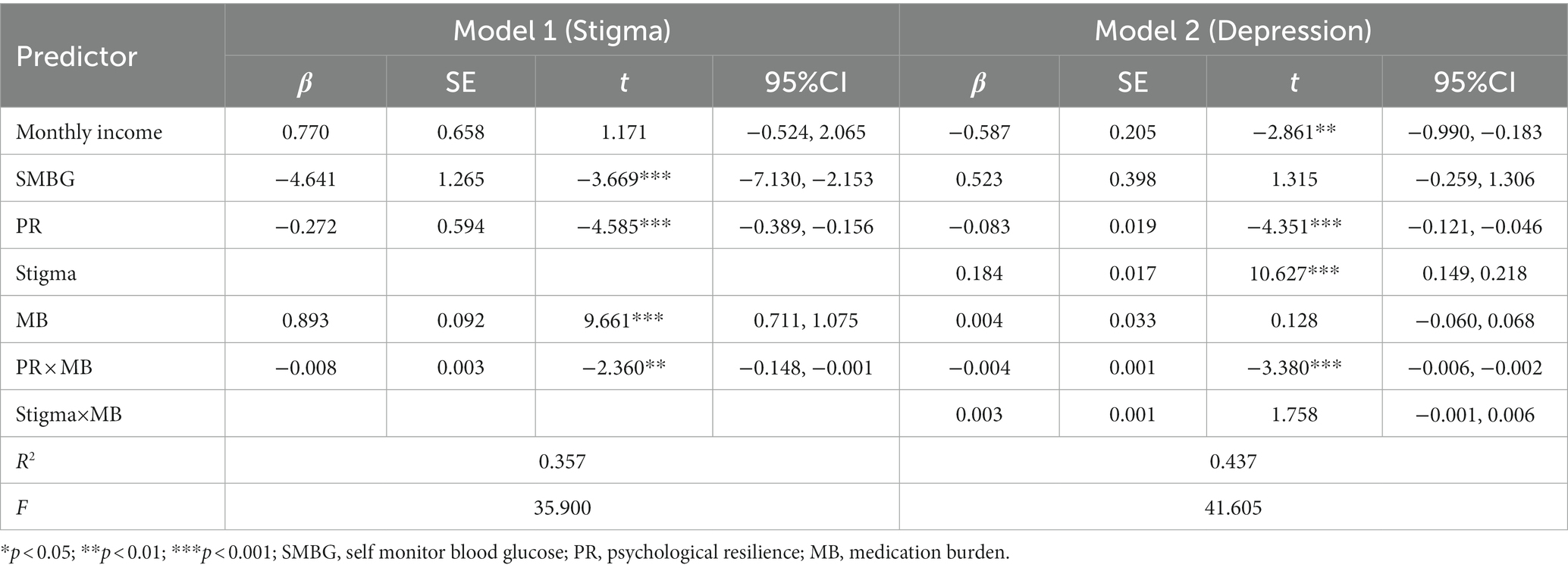
As shown in Table 5, Model 1 revealed a major impact of PR on stigma (β = −0.272, SE = 0.594, 95%CI = [−0.389, −0.156]), which was moderated by MB (β = −0.008, SE = 0.003, 95%CI = [−0.148, −0.001]). Model 2 revealed a major impact of PR on depression (β = −0.083, SE = 0.019, 95%CI = [−0.121, −0.046]), which was moderated by MB (β = −0.004, SE = 0.001, 95%CI = [−0.006, −0.002]). And it revealed a major impact of stigma on depression (β = 0.184, SE = 0.017, 95%CI = [−0.149, −0.218]), which was not moderated by MB (β = 0.003, SE = 0.001, 95%CI = [−0.006, 0.001]). Hence, hypothesis 2 and 3 were partially supported. The final moderated mediation model was shown in Figure 2.
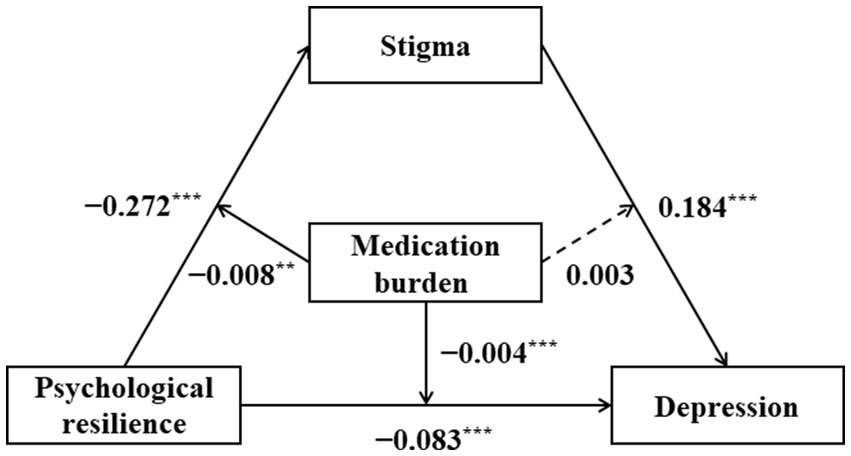
Figure 2. Confirmed model of the relationships between psychological resilience, stigma, and medication burdenand depression.
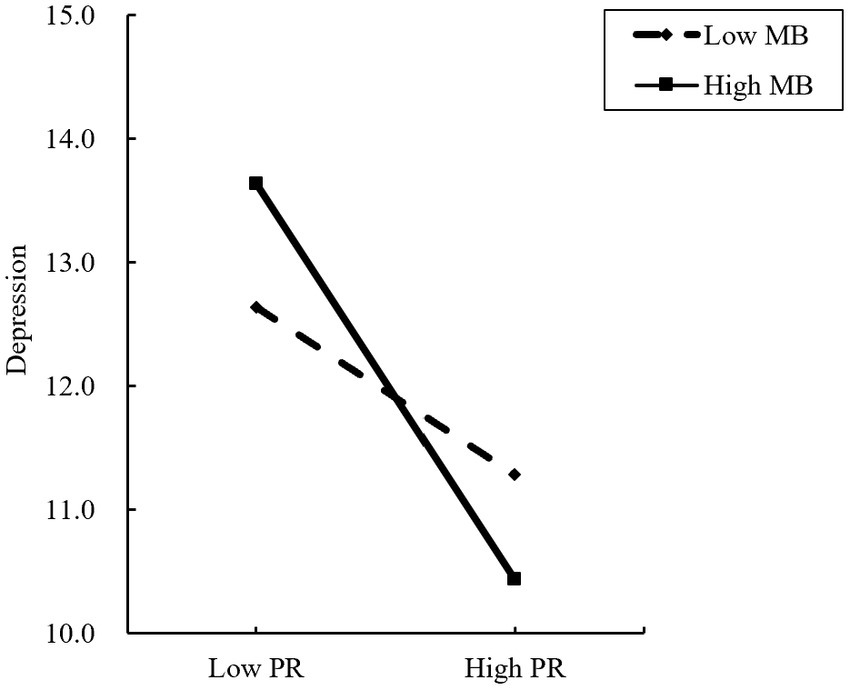
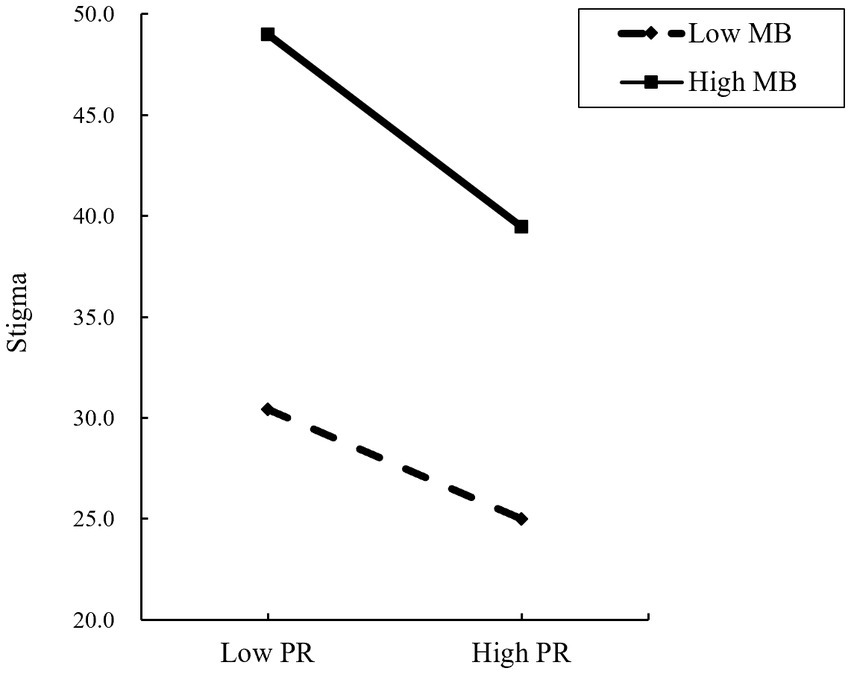
Figure 3 provides an intuitive view of how the effect of PR on depression is moderated by the MB. A simple slope test shows that for diabetic patients with a low-level MB (Z = −1), depression has a significant downward trend with the increase of PR (β = −0.049, p < 0.001), PR increased by one standard deviation, and the total score of depression decreased by 0.049 standard deviations, that is, the higher the level of PR, the lower the degree of depression; For diabetes patients with high-level MB (Z = 1), With the increase of stigma, the degree of depression also showed a significant downward trend (β = −0.117, p < 0.001), and the downward trend was higher than that of diabetes patients with low MB.
Figure 4 shows how the MB moderates the relationship between PR and stigma. A simple slope test showed that for diabetes patients with low-level MB (Z = −1), stigma decreased significantly with the increase of PR (β = −0.363, p < 0.001). One standard deviation increase in psychological resilience was associated with a 0.363 standard deviation decrease in stigma. The higher the PR, the lower the degree of stigma; For diabetes patients with high-level MB (Z = 1), with the increase in PR, the decline of stigma was also significant (β = −0.639, p < 0.001). One standard deviation increase in psychological resilience was associated with a 0.639 standard deviation reduction in stigma, slightly higher than in diabetes patients with a lower MB.
4. Discussion
In this study, the results showed that PR was negatively associated with depression in older patients with diabetes, and this relationship was mediated by stigma. Furthermore, the moderating effect suggests that MB moderated these relationships during the COVID-19 policy. And, consistent with our hypothesis about the moderating effect, we found that MB moderated the association between PR and depression, and moderated the effect of PR on stigma. At the same time, the study results showed that only 7.9% of older diabetic patients did not have depression, up to 56% of patients had mild to moderate depression, and 36.1% had moderate to severe depression. This phenomenon indicates that the incidence of depression in older diabetic patients in China is high during COVID-19. Overall, our findings broaden our understanding of PR and depression and contributed to research linking depression to PR.
Older people with diabetes were at high risk for increased depression associated with dangerous public health emergencies. Our results were consistent with previous studies (51, 52), and noted that older adults with diabetes showed a high incidence of depression during the COVID-19 pandemic (53), people going through this period were susceptible to mental health problems (54). Depression could be one of the worst experiences experienced by older people with diabetes, and evidence from different countries suggested that older people with diabetes had the highest increase in rates of psychological distress during the pandemic (55).
Our results showed that PR was negatively correlated with stigma and depression, which was consistent with previous findings (56). Thus, PR and stigma influenced the risk of depression in older people with diabetes due to the COVID-19 pandemic. Patients with higher resilience experience lower levels of stigma and depression because they could cope more successfully with the stressors of the COVID-19 pandemic (57). Research’s (58, 59) had found that PR could help individuals remain optimistic in the face of negative events and improve responses to negative events. Thus, even during the COVID-19 pandemic, compensatory factors such as PR can help offset possible negative effects on mental health (60). Thus, resilience could prevent and improve depression in older people with diabetes during the COVID-19 pandemic.
Modeling predictors of depression had identified PR as a protective factor in young people and stigma as a precipitator of depression. This finding highlighted the importance of monitoring stigma in older diabetics. In our study, stigma was found to mediate between PR and depression, suggesting that older diabetics who experience the shame of their illness and the blame of others reduce perceived PR and thus increase depression in the context of COVID-19. These findings were consistent with previous research on depression (61, 62). Our research suggested that stigma was a harmful negative emotion that reinforces people’s negative feelings about negative events. Therefore, stigma allowed individuals to take a negative rather than a positive view of an event, which could cause them to alter their emotional responses and harm their mental health (63).
Many studies (64, 65) supported MB as a potential regulator. Our findings suggested that MB may play a moderating role in the relationship between loneliness and depression during the COVID-19 pandemic. When people were in a high MB state, people with high PR were less likely to develop depression than people with low PR. MB thus played a significant moderating role by attenuating the perceived relationship between PR and depression. In addition, the impact of MB on PR and stigma varies from individual to individual. When PR level was high, stigma of older diabetic patients with high or low MB showed a decreasing trend. However, the downward trend in older patients with high MB was less than that in patients with low MB. Thus, the results further suggested that elasticity moderated the mediating role of stigma assessment between PR and depression.
In this study, we constructed and tested a hypothetical model based on the results of previous research and theory to determine whether PR might be a protective factor for depression. We also examined the mediating role of stigma and investigated whether MB moderated the mediation model in the context of the COVID-19 pandemic. Clearly, the model shows that older diabetics can maintain their mental health during the COVID-19 pandemic if they have good high levels of mental resilience and pay attention to managing stigma and MB. Resilience is associated with the ability of individuals to manage stress (66). At the same time, psychological problems resulting from continued exposure to traumatic events such as death anxiety and negative emotions remain unavoidable (67). Therefore, PR was one of the most effective strategies that older diabetes could use to solve the negative emotional reactions caused by psychological adversity (68).
The current study suggested that stigma and MB mediate the relationship between PR and depression, a finding that may have useful clinical implications. Our study suggested that the relationship between PR and depression can be partially affected by more frequent stigma in older diabetics. In addition, we found that MB not only moderated the relationship between PR and depression, but also the effect of PR on stigma. Therefore, risk factors such as stigma and MB increased the risk of depression among older Chinese patients with diabetes during the COVID-19 pandemic. These findings suggested that governments and educational institutions should work together to address the deterioration of mental health in older people with diabetes and provide timely and effective services to promote adaptive and positive mental health in this age group. Together, our findings shed light on the relationship between PR and depression and broaden our understanding of how to use protective factors, such as resilience, to formulate public health interventions during the COVID-19 pandemic, especially in the older adult population with diabetes.
4.1. Limitations
There are several limitations to this study. Firstly, due to the study’s cross-sectional design, we could not make any causal inferences about the observed associations. Future research should use longitudinal studies to better define the pathways in our theoretical model. Secondly, although self-reporting has been widely used in the literature, this data collection method has inherent disadvantages, such as being highly subjective, inevitably leading to some bias in the data. Future research should include multiple data collection methods to cross-check and obtain more objective and accurate data. Finally, future research should explore the mechanisms of influence of different psychological factors to obtain more accurate findings. Further investigations should not only use a more representative sample and validate the findings, but also focus more on the different mechanisms by which resilience and depression affect others, and clearly measure the impact that the COVID-19 pandemic may have on variables (e.g., depression as a direct result of the pandemic). As a result, future research may involve more psychological structures, such as social anxiety, social support, and self-esteem, to better understand how individuals cope with the adverse consequences of COVID-19 and possibly respond more adaptive in future pandemics.
5. Conclusion
This is the first time we have established a moderating mediation model between PR and depression. Our findings showed that stigma played a mediating role in the association between PR and depression. MB plays a role in regulating the relationship between PR and depression. Specifically, with the increase of PR, depression decreased, and the decreasing trend of depression in patients with high MB was greater than that in patients with low MB; In addition, MB also played a moderating role between patient stigma and depression. As patients’ PR increased, stigma decreased, with a slightly greater tendency to decrease in patients with high MB than in those with low MB. Therefore, we should be fully aware of patients’ PR levels and intervene in a timely manner to improve their psychological status. At the same time, MB as an influencing factor needs to be considered with a view to better protecting patients’ psychological well-being. Medical professionals should give regular public lectures on stigma and depression prevention and control measures to achieve early screening, diagnosis, and intervention. Patients should also be regularly questioned about their medication in order to understand the presence of MB and intervene in a timely manner.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by medical ethics committee of Wannan Medical College. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LZ conceived and designed the research. YM wrote the paper. YM and LZ analyzed the data. YM, LZ, XY, YL, JG, XZ, YW, and CL revised the paper. YM, XY, JG, YL, XZ, YW, WC, MC, CL, and LZ reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The research was supported by the Support Program for Outstanding Young Talents from the Universities and Colleges of Anhui Province for LZ (gxyqZD2021118); The study was supported by the Research on the Creation of International Rules for China’s Participation in Global Health Governance and Path Selection” (21yjcgjw006); The study was supported by the National Innovation and Entrepreneurship Training Program for College Students (202210368016); The study was supported by the Research Practice of Elderly Nursing (2021shsjkc030).
Acknowledgments
The authors thank all participants for their contributions and study members for their cooperation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CD-RISC, Conner-Davidson Resilience Scale; SSCI, Stigma Scale for Chronic Illness; DTBQ, Diabetes Treatment Burden Scale; COVID-19, Corona Virus Disease 2019; CIs, confidence intervals; DM, Diabetes Mellitus; PHQ-9, Patient Health Questionaire-9; SMBG, Self Monitor Blood Glucose; PR, Psychological Resilience; MB, Medication Burden; ANOVA, One-way Analysis of Variance.
References
1. Umakanthan, S, Sahu, P, Ranade, AV, Bukelo, MM, Rao, JS, Abrahao-Machado, LF, et al. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med J. (2020) 96:753–8. doi: 10.1136/postgradmedj-2020-138234
2. Bai, W, Sha, S, Cheung, T, Su, Z, Jackson, T, and Xiang, YT. Optimizing the dynamic zero-COVID policy in China. Int J Biol Sci. (2022) 18:5314–6. doi: 10.7150/ijbs.75699
3. Halpin, DMG, Criner, GJ, Papi, A, Singh, D, Anzueto, A, Martinez, FJ, et al. Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2021) 203:24–36. doi: 10.1164/rccm.202009-3533SO
4. Lima-Martínez, MM, Carrera Boada, C, Madera-Silva, MD, Marín, W, and Contreras, M. COVID-19 and diabetes: a bidirectional relationship. Clin Investig Arterioscler. (2021) 33:151–7. doi: 10.1016/j.arteri.2020.10.001
5. Zhou, Y, Chi, J, Lv, W, and Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (Covid-19). Diabetes Metab Res Rev. (2021) 37:e3377. doi: 10.1002/dmrr.3377
6. Palumbo, C, Nicolaci, N, La Manna, AA, Branek, N, and Pissano, MN. Association between central diabetes insipidus and type 2 diabetes mellitus. Medicina. (2018) 78:127–30.
7. World Health Organization. Use of glycated Haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. Geneva: World Health Organization (2011).
8. Juan, J, and Yang, H. Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China. Int J Environ Res Public Health. (2020) 17:9517. doi: 10.3390/ijerph17249517
9. Forrester, JV, Kuffova, L, and Delibegovic, M. The role of inflammation in diabetic retinopathy. Front Immunol. (2020) 11:583687. doi: 10.3389/fimmu.2020.583687
10. Kudiyirickal, MG, and Pappachan, JM. Diabetes mellitus and oral health. Endocrine. (2015) 49:27–34. doi: 10.1007/s12020-014-0496-3
11. Sartorius, N. Depression and diabetes. Dialogues Clin Neurosci. (2018) 20:47–52. doi: 10.31887/DCNS.2018.20.1/nsartorius
12. Park, M, and Reynolds, CF 3rd. Depression among older adults with diabetes mellitus. Clin Geriatr Med. (2015) 31:117–37, ix. doi: 10.1016/j.cger.2014.08.022
13. Kalomo, EN, Jun, JS, Lee, K, and Kaddu, MNHIV. Stigma, resilience and depressive symptoms among older adults living with HIV in rural Namibia. Afr J AIDS Res. (2020) 19:198–205. doi: 10.2989/16085906.2020.1797841
14. Cho, OH, Cho, YH, and Chung, MY. Depression, and awareness of information on safety behavior in Korean hemodialysis patients during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:10348. doi: 10.3390/ijerph181910348
15. Habib, S, Sangaraju, SL, Yepez, D, Grandes, XA, and Talanki Manjunatha, R. The nexus between diabetes and depression: a narrative review. Cureus. (2022) 14:e25611. doi: 10.7759/cureus.25611
16. Prigge, R, Wild, SH, and Jackson, CA. Depression, diabetes, comorbid depression and diabetes and risk of all-cause and cause-specific mortality: a prospective cohort study. Diabetologia. (2022) 65:1450–60. doi: 10.1007/s00125-022-05723-4
17. Williams, JK, Collings, R, Kent, B, and Paton, J. Prevalence and incidence of mental health issues amongst adults with diabetes at risk of foot complications in the European Union: a systematic review protocol. JBI Evid Synth. (2022) 20:2094–101. doi: 10.11124/JBIES-21-00372
18. Masaryková, L, Tesař, T, Lehocká, U, and Bernáthová, K. Evaluation of adherence to treatment in patients suffering from diabetes mellitus. Ceska Slov Farm. (2020) 69:67–74.
19. Winkley, K, Upsher, R, Stahl, D, Pollard, D, Kasera, A, Brennan, A, et al. Psychological interventions to improve self-management of type 1 and type 2 diabetes: a systematic review. Health Technol Assess. (2020) 24:1–232. doi: 10.3310/hta24280
20. Meng, R, Yu, C, Liu, N, He, M, Lv, J, Guo, Y, et al. Association of depression with all-cause and cardiovascular disease mortality among adults in China. JAMA Netw Open. (2020) 3:e1921043. doi: 10.1001/jamanetworkopen.2019.21043
21. Bauer, H, Emeny, RT, Baumert, J, and Ladwig, KH. Resilience moderates the association between chronic pain and depressive symptoms in the elderly. Eur J Pain. (2016) 20:1253–65. doi: 10.1002/ejp.850
22. Sisto, A, Vicinanza, F, Campanozzi, LL, Ricci, G, Tartaglini, D, and Tambone, V. Towards a transversal definition of psychological resilience: a literature review. Medicina. (2019) 55:745. doi: 10.3390/medicina55110745
23. Verdolini, N, Amoretti, S, Montejo, L, García-Rizo, C, Hogg, B, Mezquida, G, et al. Resilience and mental health during the COVID-19 pandemic. J Affect Disord. (2021) 283:156–64. doi: 10.1016/j.jad.2021.01.055
24. Mace, RA, Doorley, J, Bakhshaie, J, Cohen, JE, and Vranceanu, AM. Psychological resiliency explains the relationship between emotional distress and quality of life in neurofibromatosis. J Neuro-Oncol. (2021) 155:125–32. doi: 10.1007/s11060-021-03852-1
25. Sardella, A, Lenzo, V, Bonanno, GA, Basile, G, and Quattropani, MC. Expressive flexibility and dispositional optimism contribute to the Elderly's resilience and health-related quality of life during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:1698. doi: 10.3390/ijerph18041698
26. Song, S, Yang, X, Yang, H, Zhou, P, Ma, H, Teng, C, et al. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Front Psychol. (2020) 11:618509. doi: 10.3389/fpsyg.2020.618509
27. Liu, KL, Chuang, CK, Pang, ST, Wu, CT, Yu, KJ, Tsai, SC, et al. Emotional state and cancer-related self-efficacy as affecting resilience and quality of life in kidney cancer patients: a cross-sectional study. Support Care Cancer. (2022) 30:2263–71. doi: 10.1007/s00520-021-06644-5
28. Nyblade, L, Stockton, MA, Giger, K, Bond, V, Ekstrand, ML, Lean, RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. (2019) 17:25. doi: 10.1186/s12916-019-1256-2
29. Cremers, AL, de Laat, MM, Kapata, N, Gerrets, R, Klipstein-Grobusch, K, and Grobusch, MP. Assessing the consequences of stigma for tuberculosis patients in urban Zambia. PLoS One. (2015) 10:e0119861. doi: 10.1371/journal.pone.0119861
30. Woo, S, Zhou, W, and Larson, JL. Stigma experiences in people with chronic obstructive pulmonary disease: an integrative review. Int J Chron Obstruct Pulmon Dis. (2021) 16:1647–59. doi: 10.2147/COPD.S306874
31. Zhang, YB, Yang, Z, Zhang, HJ, Xu, CQ, and Liu, T. The role of resilience in diabetes stigma among young and middle-aged patients with type 2 diabetes. Nurs Open. (2023) 10:1776–84. doi: 10.1002/nop2.1436
32. Jeamjitvibool, T, Duangchan, C, Mousa, A, and Mahikul, W. The association between resilience and psychological distress during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 19:14854. doi: 10.3390/ijerph192214854
33. Naushad, N, Dunn, LB, Muñoz, RF, and Leykin, Y. Depression increases subjective stigma of chronic pain. J Affect Disord. (2018) 229:456–62. doi: 10.1016/j.jad.2017.12.085
34. Zeng, C, Li, X, Yang, X, Du, H, and Lin, D. Experiences of stigma and suicidal behaviors among rural-to-urban migrants: the mechanistic roles of depression and substance use. Psychol Health Med. (2020) 25:446–56. doi: 10.1080/13548506.2019.1687921
35. Eton, DT, Ramalho de Oliveira, D, Egginton, JS, Ridgeway, JL, Odell, L, May, CR, et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas. (2012) 3:39–49. doi: 10.2147/PROM.S34681
36. Ab Rahman, N, Lim, MT, Thevendran, S, Ahmad Hamdi, N, and Sivasampu, S. Medication regimen complexity and medication burden among patients with type 2 diabetes mellitus: a retrospective analysis. Front Pharmacol. (2022) 13:808190. doi: 10.3389/fphar.2022.808190
37. Xin, Y, Davies, A, Briggs, A, McCombie, L, Messow, CM, Grieve, E, et al. Type 2 diabetes remission: 2 year within-trial and lifetime-horizon cost-effectiveness of the diabetes remission clinical trial (DiRECT)/counterweight-plus weight management programme. Diabetologia. (2020) 63:2112–22. doi: 10.1007/s00125-020-05224-2
38. Liu, SY, Huang, J, Dong, QL, Li, B, Zhao, X, Xu, R, et al. Diabetes distress, happiness, and its associated factors among type 2 diabetes mellitus patients with different therapies. Medicine. (2020) 99:e18831. doi: 10.1097/MD.0000000000018831
39. Hamilton, JE, Blanco, E, Selek, S, Wirfel, KL, Bernstam, EV, Velligan, D, et al. Patient and provider perspectives on medication non-adherence among patients with depression and/or diabetes in diverse community settings – a qualitative analysis. Patient Prefer Adherence. (2022) 16:1581–94. doi: 10.2147/PPA.S328785
40. Xu, N, Xie, S, Chen, Y, Li, J, and Sun, L. Factors influencing medication non-adherence among Chinese older adults with diabetes mellitus. Int J Environ Res Public Health. (2020) 17:6012. doi: 10.3390/ijerph17176012
41. Alidrisi, HA, Bohan, A, and Mansour, AA. Barriers of doctors and patients in starting insulin for type 2 diabetes mellitus. Cureus. (2021) 13:e18263. doi: 10.7759/cureus.18263
42. Soylar, P, Kadioglu, BU, and Kilic, K. Investigation of the barriers about insulin therapy in patients with type 2 diabetes. Niger J Clin Pract. (2020) 23:98–102. doi: 10.4103/njcp.njcp_138_19
43. Velickovic, K, Rahm Hallberg, I, Axelsson, U, Borrebaeck, CAK, Rydén, L, Johnsson, P, et al. Psychometric properties of the Connor-Davidson resilience scale (CD-RISC) in a non-clinical population in Sweden. Health Qual Life Outcomes. (2020) 18:132. doi: 10.1186/s12955-020-01383-3
44. Martinez, S, Jones, JD, Brandt, L, Hien, D, Campbell, ANC, Batchelder, S, et al. Factor structure and psychometric properties of the Connor-Davidson resilience scale (CD-RISC) in individuals with opioid use disorder. Drug Alcohol Depend. (2021) 221:108632. doi: 10.1016/j.drugalcdep.2021.108632
45. Lu, Q, Deng, C, Fu, L, Wu, R, Chang, L, Qi, H, et al. Reliability and validity of a Chinese version of the stigma scale for chronic illness (SSCI) in patients with stroke. Top Stroke Rehabil. (2019) 26:312–7. doi: 10.1080/10749357.2019.1592306
46. Ballesteros, J, Martínez-Ginés, ML, García-Domínguez, JM, Forero, L, Prefasi, D, Maurino, J, et al. Assessing stigma in multiple sclerosis: psychometric properties of the eight-item stigma scale for chronic illness (SSCI-8). Int J MS Care. (2019) 21:195–9. doi: 10.7224/1537-2073.2018-053
47. Ishii, H, Shin, K, Tosaki, T, Haga, T, Nakajima, Y, Shiraiwa, T, et al. Reproducibility and validity of a questionnaire measuring treatment burden on patients with type 2 diabetes: diabetic treatment burden questionnaire (DTBQ). Diabetes Ther. (2018) 9:1001–19. doi: 10.1007/s13300-018-0414-4
48. Wee, PJL, Kwan, YH, Loh, DHF, Phang, JK, Puar, TH, Østbye, T, et al. Measurement properties of patient-reported outcome measures for diabetes: systematic review. J Med Internet Res. (2021) 23:e25002. doi: 10.2196/25002
49. Arnold, SRC, Uljarević, M, Hwang, YI, Richdale, AL, Trollor, JN, and Lawson, LP. Brief report: psychometric properties of the patient health questionaire-9 (PHQ-9) in autistic adults. J Autism Dev Disord. (2020) 50:2217–25. doi: 10.1007/s10803-019-03947-9
50. Glazer, K, Rootes-Murdy, K, Van Wert, M, Mondimore, F, and Zandi, P. The utility of PHQ-9 and CGI-S in measurement-based care for predicting suicidal ideation and behaviors. J Affect Disord. (2020) 266:766–71. doi: 10.1016/j.jad.2018.05.054
51. Li, X, Yu, H, and Yang, N. The mediating role of resilience in the effects of physical exercise on college students' negative emotions during the COVID-19 epidemic. Sci Rep. (2021) 11:24510. doi: 10.1038/s41598-021-04336-y
52. To QGVandelanotte, C, Cope, K, Khalesi, S, Williams, SL, Alley, SJ, et al. The association of resilience with depression, anxiety, stress and physical activity during the COVID-19 pandemic. BMC Public Health. (2022) 22:491. doi: 10.1186/s12889-022-12911-9
53. Şahin, H, and Türk, F. The impact of cognitive-behavioral group psycho-education program on psychological resilience, irrational beliefs, and well-being. J Ration Emot Cogn Behav Ther. (2021) 39:672–94. doi: 10.1007/s10942-021-00392-5
54. Hong, Y, Yuhan, L, Youhui, G, Zhanying, W, Shili, Z, Xiaoting, H, et al. Death anxiety among advanced cancer patients: a cross-sectional survey. Support Care Cancer. (2022) 30:3531–9. doi: 10.1007/s00520-022-06795-z
55. Peker, A, and Cengiz, S. Covid-19 fear, happiness and stress in adults: the mediating role of psychological resilience and coping with stress. Int J Psychiatry Clin Pract. (2022) 26:123–31. doi: 10.1080/13651501.2021.1937656
56. Brown, RL. Perceived stigma among people with chronic health conditions: the influence of age, stressor exposure, and psychosocial resources. Res Aging. (2015) 37:335–60. doi: 10.1177/0164027514533133
57. Mora-Rios, J, Ortega-Ortega, M, and Natera, G. Subjective experience and resources for coping with stigma in people with a diagnosis of schizophrenia: an intersectional approach. Qual Health Res. (2016) 26:697–711. doi: 10.1177/1049732315570118
58. Mukhtar, S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int J Soc Psychiatry. (2020) 66:512–6. doi: 10.1177/0020764020925835
59. Chin, ED, and Armstrong, D. Anticipated stigma and healthcare utilization in COPD and neurological disorders. Appl Nurs Res. (2019) 45:63–8. doi: 10.1016/j.apnr.2018.12.002
60. Oliver, MD, Datta, S, and Baldwin, DR. A sympathetic nervous system evaluation of obesity stigma. PLoS One. (2017) 12:e0185703. doi: 10.1371/journal.pone.0185703
61. Violant-Holz, V, Gallego-Jiménez, MG, González-González, CS, Muñoz-Violant, S, Rodríguez, MJ, Sansano-Nadal, O, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2020) 17:9419. doi: 10.3390/ijerph17249419
62. Singhai, K, Swami, MK, Nebhinani, N, Rastogi, A, and Jude, E. Psychological adaptive difficulties and their management during COVID-19 pandemic in people with diabetes mellitus. Diabetes Metab Syndr. (2020) 14:1603–5. doi: 10.1016/j.dsx.2020.08.025
63. Yan, AF, Sun, X, Zheng, J, Mi, B, Zuo, H, Ruan, G, et al. Perceived risk, behavior changes and health-related outcomes during COVID-19 pandemic: Findingsamong adults with and without diabetesin China. Diabetes Res Clin Pract. (2020) 167:108350. doi: 10.1016/j.diabres.2020.108350
64. Alexandre, K, Campbell, J, Bugnon, M, Henry, C, Schaub, C, Serex, M, et al. Factors influencing diabetes self-management in adults: an umbrella review of systematic reviews. JBI Evid Synth. (2021) 19:1003–118. doi: 10.11124/JBIES-20-00020
65. Al-Sofiani, ME, Albunyan, S, Alguwaihes, AM, Kalyani, RR, Golden, SH, and Alfadda, A. Determinants of mental health outcomes among people with and without diabetes during the COVID-19 outbreak in the Arab gulf region. Diabetes. (2021) 13:339–52. doi: 10.1111/1753-0407.13149
66. Joensen, LE, Madsen, KP, Holm, L, Nielsen, KA, Rod, MH, Petersen, AA, et al. Diabetes and COVID-19: psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark—what characterizes people with high levels of COVID-19-related worries? Diabet Med. (2020) 37:1146–54. doi: 10.1111/dme.14319
67. Ghosh, A, Arora, B, Gupta, R, Anoop, S, and Misra, A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in North India. Diabetes Metab Syndr. (2020) 14:917–20. doi: 10.1016/j.dsx.2020.05.044
Keywords: resilience, stigma, medication burden, depression, diabetes patients
Citation: Mei Y, Yang X, Gui J, Li Y, Zhang X, Wang Y, Chen W, Chen M, Liu C and Zhang L (2023) The relationship between psychological resilience and depression among the diabetes patients under the background of “dynamic zero COVID-19”: the mediating role of stigma and the moderating role of medication burden. Front. Public Health. 11:1124570. doi: 10.3389/fpubh.2023.1124570
Edited by:
Mohammad Ishraq Zafar, Zhejiang University School of Medicine, ChinaReviewed by:
Jing Deng, Central South University, ChinaMohammad Ali Zakeri, Rafsanjan University of Medical Sciences, Iran
Copyright © 2023 Mei, Yang, Gui, Li, Zhang, Wang, Chen, Chen, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Zhang, eWFvcmFuMjAwOEAxNjMuY29t
 Yujin Mei
Yujin Mei Xue Yang1
Xue Yang1 Lin Zhang
Lin Zhang