- 1Department of Health and Kinesiology, College of Health, University of Utah, Salt Lake City, UT, United States
- 2ACCORDS Dissemination & Implementation Science Program and Department of Family Medicine, University of Colorado Anschutz Medical Campus, Denver, CO, United States
Introduction
To improve the uptake of evidence-based interventions in the fields of aging and public health there have been calls to apply the methods, models, and measures of dissemination and implementation science (DIS) (1, 2). DIS may be defined as the scientific study of the strategies and mechanisms by which research evidence is adopted, applied, and sustained in community or clinical settings to improve outcomes for a specified population (3, 4). Early work in DIS focused on expanding the reporting of outcomes. This translated into including, but moving beyond efficacy or effectiveness, when testing interventions to improve health outcomes and balancing internal and external validity in the development and testing of new interventions (5). In one early framework, these expanded outcomes were initially summarized by our research team using reach, effectiveness, adoption, implementation, maintenance (RE-AIM) dimensions (5, 6). Within RE-AIM, multi-leveled dissemination outcomes were operationalized at the level of the population intended to benefit (i.e., reach) as well as the staff, settings, and systems (i.e., adoption) intended to deliver an intervention (7). At each level of dissemination, researchers were encouraged to address representativeness, engage the populations and systems that could most benefit, and advance health equity (8, 9). Similarly, implementation outcomes were operationalized within RE-AIM at the staff, setting, and system levels to include the degree to which an intervention was delivered as intended (i.e., implementation), the costs associated with implementation, adaptations made, and the potential for sustainability (i.e., organizational level maintenance).
In addition to expanding outcomes, understanding context is a key aspect of DIS (10, 11). Contextual factors related to DIS outcomes provide constructs that can act as moderators, mediators, or mechanisms of success (4, 12). Indeed, the field has seen a proliferation of theories, models, and frameworks to provide systematic approaches to understand the relationships between contextual factors and outcomes (13–15). For example, the Practical, Robust, Implementation, and Sustainability Model (PRISM) provides constructs multi-level constructs of potential beneficiaries (e.g., economic status; compatibility of intervention with lifestyle) and potential implementers (e.g., expertise; complexity of intervention implementation); implementation and sustainability infrastructure (e.g., structured communication channels); and external environmental factors (e.g., community resources to support or inhibit dissemination and/or implementation) (16, 17). Each of these contextual constructs, when tied to a specific RE-AIM outcome, can be used to map strategies to improve outcomes that can be tailored to address contextual moderators or designed to leverage contextual mediators or mechanisms that lead to success (16, 18).
Over the past 2–3 years there have been several articles articulating how DIS can be applied to aging and health issues (1, 9, 19, 20). Of particular relevance is a paper by Carpenter et al. (19) that discusses how addressing DIS outcomes, moderators, mediators, and mechanisms using the Standards for Reporting Implementation Studies (StaRI) can be applied to advance DIS and aging research. The STaRI guidelines summarize key DIS issues under the various sections of a manuscript for reporting on DIS studies. For example, in the introduction, identification of the DIS theory or framework used is recommended while in the methods section clear operational definitions of the implementation context, outcomes, and economic evaluation are encouraged. The results and discussions sections are recommended to include information on fidelity to protocol, intervention adaptions, and generalizability to other typical clinical or community settings.
Developing a DIS research agenda for aging and public health
Several researchers have developed guidance and recommendations about advancing DIS. To develop successful projects and outcomes, Kilbourne et al. (21) recommended the use of a conceptual model, collaborative methods (e.g., development of a shared agenda, implementation strategies, adaptation recommendations with key system partners), and focusing on building system capacity and a business case for sustained implementation. Other recommendations for advancing DIS include using mixed methods to capture important contextual and systems factors that may not be quantifiable (22, 23) and pragmatic approaches to maintain a focus on generalizability and usability of implementation strategies and outcomes relevant to typical clinical and community settings (24). In addition, to these recommendations, we propose the following areas for DIS in aging and public health.
Focus on the how, what, when and why of dissemination and implementation
Early DIS often focused only on documenting the achievement of implementation (e.g., RE-AIM) outcomes. Active for Life, a multi-site project promoting physical activity in older adults is a good example. The primary focus was on determining if evidence-based physical activity programs could be delivered in typical community settings and demonstrate effectiveness (25, 26). Process evaluation also demonstrated that, possibly due to the collaborative nature of the multi-site trial, there was high implementation fidelity across communities and that communities adapted the interventions to improve fit with delivery settings (27). Studies like Active for Life were critical in addressing external validity and effectiveness, and set the stage for current DIS in aging to focus on understanding not only if dissemination and implementation outcomes can be achieved, but also on understanding how those outcomes can be achieved by monitoring what strategy was used, and when, in the implementation process as well as analyzing why the outcome occurred by examining prespecified mechanism(s) or mediator(s).
Recently, Implementation Research Logic Models have been introduced as an example of how to better support DIS researchers and clinical or community partners to conceptualize and test the how, what, and why of dissemination and implementation outcomes (28). This approach encourages the use of theory to characterize contextual factors that can be used to (a) determine barriers and facilitators related to achieving DIS outcomes, (b) develop context-specific implementation strategies, and (c) identify potential mechanisms and mediators of change that (d) explain if and how changes in DIS outcomes occur as a result of an implementation strategy. We developed Figure 1 as a simplified example of how aging researchers could apply DIS using information from an excellent article on the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) pragmatic trial of an intervention for Falls Care Managers to reduce fall-related injuries in older adults (29).
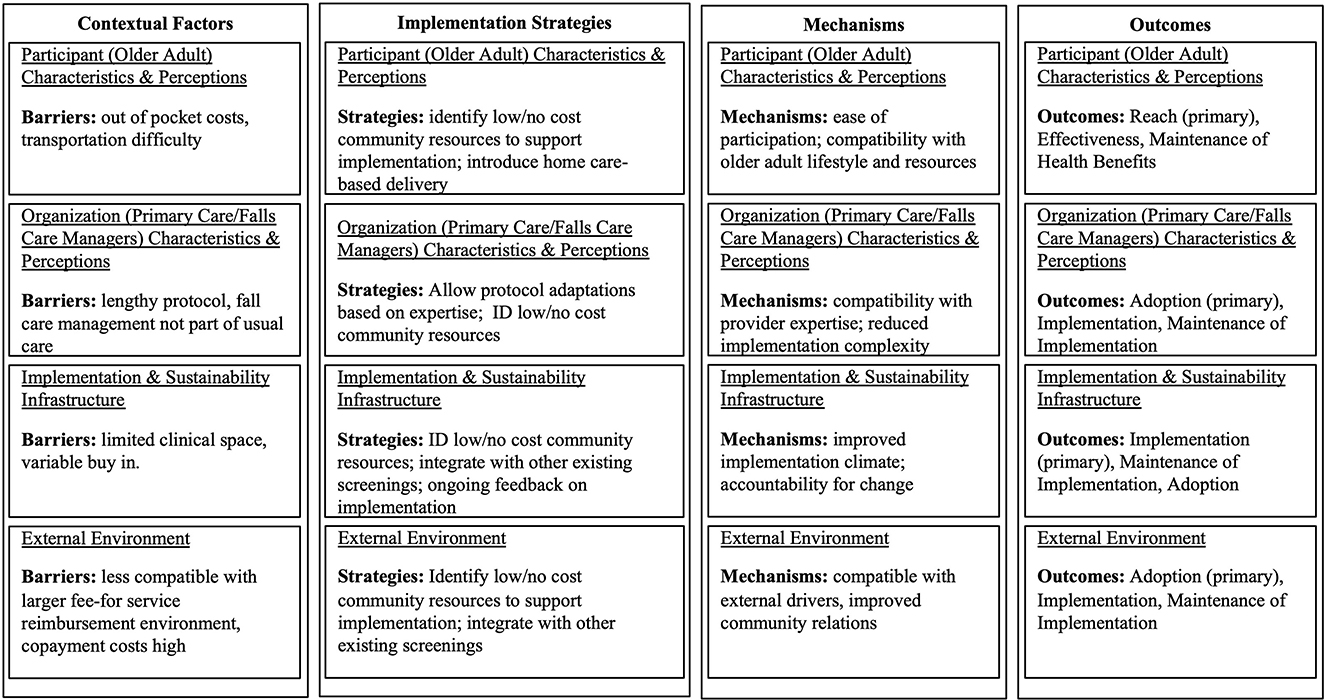
Figure 1. An example application of dissemination and implementation science in aging research: STRIDE, a national study to prevent fall related injuries.
To orient readers to the Figure each row reflects a path model that begins with barriers, strategies to overcome barriers, mechanisms, and outcomes relative to theory-based contextual factors—in this case using PRISM. The STRIDE investigative team reported on qualitative data they used to identify contextual factors that could inhibit intervention implementation and on strategies used across sites to address those factors. For ease of presentation, we only focused on barriers in the figure and linked barriers to reported strategies and then identified potential mechanisms based on PRISM contextual factors. Finally, the Figure identifies the primary DIS outcome that is most likely to change in response to the implementation strategy through the proposed PRISM mechanisms. Of note, implementation research logic models are prone to reductionism and our example uses a reductionist approach for simplicity. However, we also demonstrate that the barrier-strategy-mechanism-outcome link can be very complex with a single strategy, in part, addressing several implementation barriers (e.g., identify low/no cost community resources to support implementation) or conversely several DIS strategies may be needed to address a single barrier. Further, strategies often do not work through a single mechanism and a single mechanism is typically not responsible for a single DIS outcome. As such, we recommend the use of practical tools, such as logic models, to map out proposed relationships, develop hypotheses, and guide trials, but also to avoid oversimplification of the context-strategy-mechanism-outcome relationships.
Acknowledge and address context and adaptations as dynamic factors
Related to the recommendation to avoid oversimplification and reductionism, relevant and active areas of DIS for aging and public health researchers include addressing multi-level contextual factors and adaptation. While public health has historically focused on multiple socio-ecological levels and multiple determinants of health (30), DIS has focused more specifically on key components of context (e.g., implementation infrastructure related to available pragmatic implementation feedback loops) and how the evidence-based programs align with key aspects of context (31). One of the central tenets of DIS is that context is not static, but changes over time, sometimes very rapidly as was seen during the initial (and ongoing) COVID-19 pandemic (11). Understanding, tracking and adapting to contextual changes undergirds DIS and illustrates how it is different than other types of health outcomes research (8, 11, 32).
Adaptations and the balance between evidence-based program implementation fidelity and context specific changes (e.g., tailoring) is critical for implementation success and sustainability (33, 34). DIS posits that fidelity should be to core functions or principles rather to a rigid protocol, and that adaptions to clinical context and conditions may also be necessary (35, 36). One DIS approach that is broadly applicable and often more intuitive than other approaches for community and clinical partners is that of form and function: that there should be fidelity to the key goals or functions of an evidence-based program [e.g., reinforce quality implementation (36)]. But that the specific forms of activities to address these functions should be tailored to specific contextual factors. Public health has always been sensitive to the need to adapt to cultural and local community factors using approaches such as community-based participatory research (37), but DIS extends this focus on adaptations across the lifespan of a program and to address adaptations to the EBP, the strategies used to implement the program, and the context itself (16). DIS authors have also focused on the need for adaptations to address issues of health equity (8) and for programs to be sustainable (11).
Aging and public health research needs to be much more rapid than it has traditionally been to be relevant to decision makers and community groups, to respond to rapidly changing context, and to contribute to learning health systems. One active area of DIS focuses on how to speed the application and relevance of dissemination and implementation research (38, 39). It is acknowledged that research must be not only Rapid, but also Relevant to community and clinical partners, Rigorous, attend to Resources Required, and Replicable [the 5 Rs (40)]. With context continually changing, it is usually the case that adaptions need to be iterative and there is active D&I research applying D&I frameworks in ways that are rapid and iterative (41, 42).
Begin with the end in mind
It may seem obvious but DIS is best conceptualized by initiating action with an eye toward what outcomes are intended. In the early DIS work there was focused on the concept of designing for dissemination (43). It included thinking about the characteristics of interventions that may be most likely to be adopted in typical service settings and to plan for dissemination from the outset of a project. This concept of designing for dissemination has been expanded and we recommend aging and public health researchers interested in DIS take the approach of designing for dissemination, equity, and sustainability (44). This work often includes careful selection of delivery system partners to ensure there is a broad representation in, for example, senior-serving settings, to ensure that those providing services for populations experiencing health disparities and inequities contribute to intervention and implementation strategy design decisions (45). Theory is, again, important in the process of designing for dissemination, equity, and sustainability. For example, considering the ideal or preferred intervention characteristics using PRISM contextual factors focused on participant and organizational perspectives can result in interventions that are attractive to underserved audiences and aligned with the assets available in the organizations that serve that audience (46).
The need for de-implementation
While DIS focused initially on the getting evidence-based interventions into practice, there is also need for the de-implementation of low value interventions that that may be either ineffective or harmful (47). De-implementation and de-intensification represent a growing area of DIS in aging and public health in which new theories and methods may be needed to reduce the use or overuse of ineffective or harmful interventions (19). To help providers decide when and how to “de-adopt” treatments in patients with complex needs. Indeed, the removal of care that may be perceived as potentially beneficial by older patients could be especially challenging for de-implementation (19). User-centered approaches that include patients and providers in the identification of pathways toward de-implementation or de-intensification may be promising approaches, particularly for older adults (48).
Conclusion
Focusing on the what, when, how, and why of dissemination and implementation will advance the speed of translation, as well as the broader public health impact, of evidence-based interventions in aging and public health. We note that this brief article is necessarily cursory and several other DIS recommendation and guidance documents exist for scientists and practitioners that also include many more useful examples. In addition, we used RE-AIM and PRISM as our examples of outcomes and contextual DIS frameworks, though there are a myriad of other frameworks from which to choose. As with our recommendations for matching context-strategy-mechanisms-outcomes, we encourage those in aging and public health research to investigate what is available and pick what seems to be the best fit for your research question and context. There are great resources such as www.dissemination-implementation.org and Brownson et al. (49) that can help facilitate framework selection. Additionally, we invite researchers and practitioners to engage with the National RE-AIM Workgroup and visit (www.re-aim.org) to learn more about public health approaches to improving population health across the life course.
Author contributions
PE and RG collaboratively conceptualized this paper. Both authors contributed to writing sections of the initial draft and subsequent revisions leading to the final submitted manuscript.
Funding
RG's effort on this paper was partially supported by the National Cancer Institute's Implementation Science Center grant P50CA244688. PE's effort on this paper was partially supported by the Osher Center for Integrative Health Award to the University of Utah.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bobitt J, Prusaczyk B. Using implementation science to inform and evaluate health policy. Innov Aging. (2021) 5:50. doi: 10.1093/geroni/igab046.191
2. Estabrooks PA, Brownson RC, Pronk NP. Dissemination and implementation science for public health professionals: an overview and call to action. Prev Chronic Dis. (2018) 15:E162. doi: 10.5888/pcd15.180525
3. Guerin RJ, Glasgow RE, Tyler A, Rabin BA, Huebschmann AG. Methods to improve the translation of evidence-based interventions: a primer on dissemination and implementation science for occupational safety and health researchers and practitioners. Safety Sci. (2022) 152:105763. doi: 10.1016/j.ssci.2022.105763
4. Estabrooks PA. An overview of dissemination and implementation science in physical activity and health promotion. Kinesiol Rev. (2023) 12:4–18. doi: 10.1123/kr.2022-0044
5. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89:1322–7. doi: 10.2105/AJPH.89.9.1322
6. Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:64. doi: 10.3389/fpubh.2019.00064
7. Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Transl Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
8. Shelton RC, Chambers DA, Glasgow RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Front Public Health. (2020) 8:134. doi: 10.3389/fpubh.2020.00134
9. Prusaczyk B, Baumann A. Eliminating disparities and achieving health equity using implementation science. Innov Aging. (2021) 5:50. doi: 10.1093/geroni/igab046.190
10. Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. (2016) 11:33. doi: 10.1186/s13012-016-0398-2
11. Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. (2013) 8:117. doi: 10.1186/1748-5908-8-117
12. Lewis CC, Boyd MR, Walsh-Bailey C, Lyon AR, Beidas R, Mittman B, et al. A systematic review of empirical studies examining mechanisms of implementation in health. Implement Sci. (2020) 15:21. doi: 10.1186/s13012-020-00983-3
13. Esmail R, Hanson HM, Holroyd-Leduc J, Brown S, Strifler L, Straus SE, et al. A scoping review of full-spectrum knowledge translation theories, models, and frameworks. Implement Sci. (2020) 15:11. doi: 10.1186/s13012-020-0964-5
14. Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. (2019) 19:189. doi: 10.1186/s12913-019-4015-3
15. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. (2012) 43:337–50. doi: 10.1016/j.amepre.2012.05.024
16. Rabin BA, Cakici J, Golden CA, Estabrooks PA, Glasgow RE, Gaglio B, et al. citation analysis and scoping systematic review of the operationalization of the Practical, Robust Implementation and Sustainability Model (PRISM). Implement Sci. (2022) 17:62. doi: 10.1186/s13012-022-01234-3
17. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. (2008) 34:228–43. doi: 10.1016/S1553-7250(08)34030-6
18. McCreight MS, Rabin BA, Glasgow RE, Ayele RA, Leonard CA, Gilmartin HM, et al. Using the Practical, Robust Implementation and Sustainability Model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. (2019) 9:1002–11. doi: 10.1093/tbm/ibz085
19. Carpenter CR, Southerland LT, Lucey BP, Prusaczyk B. Around the EQUATOR with clinician-scientists transdisciplinary aging research (Clin-STAR) principles: implementation science challenges and opportunities. J Am Geriatr Soc. (2022) 70:3620–30. doi: 10.1111/jgs.17993
20. Onken L. Implementation science at the national institute on aging: the principles of it. Public Policy Aging Rep. (2022) 32:3. doi: 10.1093/ppar/prab034
21. Kilbourne AM, Glasgow RE, Chambers DA. What can implementation science do for you? Key success stories from the field. J Gen Intern Med. (2020) 35:783–7. doi: 10.1007/s11606-020-06174-6
22. Northridge ME, Metcalf SS. Enhancing implementation science by applying best principles of systems science. Health Res Policy Syst. (2016) 14:74. doi: 10.1186/s12961-016-0146-8
23. Holtrop JS, Rabin BA, Glasgow RE. Qualitative approaches to use of the RE-AIM framework: rationale and methods. BMC Health Serv Res. (2018) 18:177. doi: 10.1186/s12913-018-2938-8
24. Beidas RS, Dorsey S, Lewis CC, Lyon AR, Powell BJ, Purtle J, et al. Promises and pitfalls in implementation science from the perspective of US-based researchers: learning from a pre-mortem. Implement Sci. (2022) 17:55. doi: 10.1186/s13012-022-01226-3
25. Wilcox S, Dowda M, Wegley S, Ory MG. Maintenance of change in the active-for-life initiative. Am J Prev Med. (2009) 37:501–4. doi: 10.1016/j.amepre.2009.07.016
26. Wilcox S, Dowda M, Leviton LC, Bartlett-Prescott J, Bazzarre T, Campbell-Voytal K, et al. Active for life: final results from the translation of two physical activity programs. Am J Prev Med. (2008) 35:340–51. doi: 10.1016/j.amepre.2008.07.001
27. Griffin SF, Wilcox S, Ory MG, Lattimore D, Leviton L, Castro C, et al. Results from the active for life process evaluation: program delivery fidelity and adaptations. Health Educ Res. (2010) 25:325–42. doi: 10.1093/her/cyp017
28. Smith JD Li DH, Rafferty MR. The implementation research logic model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement Sci. (2020) 15:84. doi: 10.1186/s13012-020-01041-8
29. Reckrey JM, Gazarian P, Reuben DB, Latham NK, McMahon SK, Siu AL, et al. Barriers to implementation of STRIDE, a national study to prevent fall-related injuries. J Am Geriatr Soc. (2021) 69:1334–42. doi: 10.1111/jgs.17056
30. Golden SD, McLeroy KR, Green LW, Earp JA, Lieberman LD. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Educ Behav. (2015) 42:8S−14S. doi: 10.1177/1090198115575098
31. Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery J. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR outcomes addendum. Implement Sci. (2022) 17:7. doi: 10.1186/s13012-021-01181-5
32. Stetler CB, Legro MW, Wallace CM, Bowman C, Guihan M, Hagedorn H, et al. The role of formative evaluation in implementation research and the QUERI experience. J Gen Intern Med. (2006) 21 Suppl 2:S1–8. doi: 10.1007/s11606-006-0267-9
33. Wiltsey Stirman S, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. (2019) 14:58. doi: 10.1186/s13012-019-0898-y
34. Holtrop JS, Gurfinkel D, Nederveld A, Phimphasone-Brady P, Hosokawa P, Rubinson C, et al. Methods for capturing and analyzing adaptations: implications for implementation research. Implement Sci. (2022) 17:51. doi: 10.1186/s13012-022-01218-3
35. Estabrooks PA, Harden SM, Almeida FA, Hill JL, Johnson SB, Porter GC, et al. Using integrated research-practice partnerships to move evidence-based principles into practice. Exerc Sport Sci Rev. (2019) 47:176–87. doi: 10.1249/JES.0000000000000194
36. Perez Jolles M, Lengnick-Hall R, Mittman BS. Core functions and forms of complex health interventions: a patient-centered medical home illustration. J Gen Intern Med. (2019) 34:1032–8. doi: 10.1007/s11606-018-4818-7
37. Israel BA, Schulz AJ, Parker EA, Becker AB. Community-Campus Partnerships for Health. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health. (2001) 14:182–97. doi: 10.1080/13576280110051055
38. Proctor E, Ramsey AT, Saldana L, Maddox TM, Chambers DA, Brownson RC, et al. A framework to assess speed of translation of health innovations to practice and policy. Glob Implement Res Appl. (2022) 2:107–19. doi: 10.1007/s43477-022-00045-4
39. Riley WT, Glasgow RE, Etheredge L, Abernethy AP. Rapid, responsive, relevant (R3) research: a call for a rapid learning health research enterprise. Clin Transl Med. (2013) 2:10. doi: 10.1186/2001-1326-2-10
40. Peek CJ, Glasgow RE, Stange KC, Klesges LM, Purcell EP, Kessler RS. The 5 R's: an emerging bold standard for conducting relevant research in a changing world. Ann Fam Med. (2014) 12:447–55. doi: 10.1370/afm.1688
41. Smith J, Rapport F, O'Brien TA, Smith S, Tyrrell VJ, Mould EVA, et al. The rise of rapid implementation: a worked example of solving an existing problem with a new method by combining concept analysis with a systematic integrative review. BMC Health Serv Res. (2020) 20:449. doi: 10.1186/s12913-020-05289-0
42. Glasgow RE, Battaglia C, McCreight M, Ayele R, Maw AM, Fort MP, et al. Use of the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) framework to guide iterative adaptations: applications, lessons learned, and future directions. Front Health Serv. (2022). doi: 10.3389/frhs.2022.959565
43. Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: dissemination research and research dissemination: how can we close the gap? Health Psychol. (2005) 24:443–6. doi: 10.1037/0278-6133.24.5.443
44. Kwan BM, Brownson RC, Glasgow RE, Morrato EH, Luke DA. Designing for dissemination and sustainability to promote equitable impacts on health. Annu Rev Public Health. (2022) 43:331–53. doi: 10.1146/annurev-publhealth-052220-112457
45. Northridge ME, Kum SS, Chakraborty B, Greenblatt AP, Marshall SE, Wang H, et al. Third places for health promotion with older adults: using the consolidated framework for implementation research to enhance program implementation and evaluation. J Urban Health. (2016) 93:851–70. doi: 10.1007/s11524-016-0070-9
46. Estabrooks PA, Fox EH, Doerksen SE, Bradshaw MH, King AC. Participatory research to promote physical activity at congregate-meal sites. J Aging Phys Act. (2005) 13:121–44. doi: 10.1123/japa.13.2.121
47. Kerr EA, Klamerus ML, Markovitz AA, Sussman JB, Bernstein SJ, Caverly TJ, et al. Identifying recommendations for stopping or scaling back unnecessary routine services in primary care. JAMA Intern Med. (2020) 180:1500–8. doi: 10.1001/jamainternmed.2020.4001
48. Caverly TJ, Skurla SE, Klamerus ML, Sparks JB, Kerr EA, Hofer TP, et al. Applying user-centered design to develop practical strategies that address overuse in primary care. J Gen Intern Med. (2022) 37:57–63. doi: 10.1007/s11606-021-07124-6
Keywords: translational sciences, knowledge translation (KT), dissemination & implementation research, reach, effectiveness, adoption, implementation and maintenance (RE-AIM)
Citation: Estabrooks PA and Glasgow RE (2023) Developing a dissemination and implementation research agenda for aging and public health: The what, when, how, and why? Front. Public Health 11:1123349. doi: 10.3389/fpubh.2023.1123349
Received: 13 December 2022; Accepted: 13 January 2023;
Published: 06 February 2023.
Edited by:
Matthew Lee Smith, Texas A&M University, United StatesReviewed by:
David E. Goodrich, United States Department of Veterans Affairs, United StatesCopyright © 2023 Estabrooks and Glasgow. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul A. Estabrooks,  cGF1bC5lc3RhYnJvb2tzQGhlYWx0aC51dGFoLmVkdQ==
cGF1bC5lc3RhYnJvb2tzQGhlYWx0aC51dGFoLmVkdQ==
 Paul A. Estabrooks
Paul A. Estabrooks Russell E. Glasgow
Russell E. Glasgow