- 1School of Public Health, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Disciplinary Planning Office, Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Centre for Specialty Strategy Research of China Hospital Development Institute, Shanghai Jiao Tong University, Shanghai, China
- 4Department of Health Policy Research, Shanghai Health Development Research Center, Shanghai, China
- 5School of Foreign Language Education, Jilin University, Jilin, China
- 6Longhua Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 7Department of Biostatistics and Epidemiology, School of Public Health, China Medical University, Shenyang, Liaoning, China
- 8Department of Primary Health, Shanghai Municipal Health Commission, Shanghai, China
Background: In 2017, the Chinese government launched a pilot project in palliative care, in which Shanghai was a pioneer. Nurses play a key role in palliative care services as they are the main providers improving the quality of services for patients and their families. However, little is known about practices and influencing factors in the field of palliative care from a nursing perspective in China. This is an original empirical study that has meticulously analyzed the interrelationship and intensity between practices and other factors among nurses in the initial stage of palliative care in primary healthcare institutions in Shanghai, China.
Methods: A descriptive-correlational study design was used to sample 2,829 eligible palliative care nurses by purposive sampling survey in 225 healthcare institutions in Shanghai, China. Descriptive analyses were performed using IBM SPSS 24.0 software. Structural equation modeling was applied to analyze the data by AMOS 20.0. Data were collected using the well-designed Knowledge, Attitudes, and Practices of Hospice Care (KAPHC) scale.
Results: The final model showed a good model fit. Self-efficacy directly influenced practices (β = 0.506, P < 0.01) and indirectly influenced practices (β = 0.028, P < 0.01) through intention. Subjective norm directly influenced practices (β = 0.082, P < 0.01) and indirectly influenced practices (β = 0.030, P < 0.01) through intention. Intention (β = 0.152, P < 0.01) and knowledge (β = 0.068, P < 0.01) directly influenced practices. Perceived susceptibility (β = −0.027, P < 0.01), perceived benefits (β = −0.017, P < 0.01), and perceived barriers (β = −0.014, P < 0.01) indirectly influenced practices through intention.
Conclusion: This study provided evidence of the associations of knowledge, perceived susceptibility, benefits, barriers, subjective norm, self-efficacy, intention, and practices among nurses concerning palliative care and interventions improving their actual work practices. Our findings revealed that self-efficacy, intention, and subjective norms greatly influenced practices. It is imperative to take interventions that focus precisely on self-efficacy, intention, and subjective norms to improve nurses' practices.
Introduction
Palliative care is the active holistic care of individuals of all ages with serious health-related suffering due to severe illness and especially those near the end of their life (1). With two batches of national pilots launched in 2017 and 2019, China initially established a palliative care service system (2). In clinical palliative care practices, nurses play an active, and often lead role in managing the whole process of patients' disease diagnosis, treatment, and dying and death, as well as meeting their physical, spiritual, cultural, and religious needs during different periods (3). Previous studies have concluded that nurses should equip themselves with diversified psychological and compassionate care comprehensively, instead of previous simple physical symptom management (4, 5). In addition, previous studies have preceded that compared to physicians, nurses had more positive attitudes toward palliative care (6). Furthermore, in the initial stage of palliative care pilot work, there is a shortage of composition and proportion of a specialized team (7). The roles of social workers and psychological counselors in interdisciplinary groups were not fully involved (8, 9); therefore, nurses undertake multi-functional roles and diversified nursing such as communication. The behavioral practices of palliative care nurses directly affect the quality of palliative care services.
However, previous studies were mostly limited to small sample surveys of specialist nurses in one institution in China (10–12). There are scarce in-depth systematic studies focusing on the interrelationship between nurses' practices and large sample surveys on influencing factors. Therefore, based on the above current situation, it is important to comprehensively measure the behavioral profile of palliative care nurses and explore the facilitators of practice in China.
Methods
Study design and participants
This is a cross-sectional study based on purposive sampling. We investigated all health institutions registered with palliative care from November to December 2019, including hospitals, community health centers, and nursing homes covering the whole area of Shanghai. Moreover, 15 registered nurses were recruited from each institution ideally. If the number is < 15, all registered nurses were investigated. The participants' inclusion criteria were as follows: nurses (1) who were nurse practitioners and (2) who voluntarily agreed to participate in the anonymous survey.
Based on a strict logical structure, the questionnaire in Chinese was scientifically designed and electronic, and all key information is required to ensure that all returned questionnaires are valid. The anonymous questionnaire survey was conducted through SO JUMP, a professional online questionnaire survey platform used by a large number of companies and individuals. The QR link and code of the questionnaire were sent to the head nurses, who distributed the questionnaires to the nurses who met the inclusion criteria in their departments. They can fill in the questionnaire using mobile phones or computers. Finally, 2,829 nurses from 225 health institutions were investigated.
Measures
This study employed a descriptive-correlational study by well-designed Knowledge, Attitudes, and Practices of Hospice Care (KAPHC) questionnaire demonstrating good validity and reliability (https://onlinelibrary.wiley.com/doi/10.1002/hpm.3074) (13, 14). The questionnaire contained five sections: demographic and relevant objective work-experience characteristics, knowledge (15 items), attitudes (24 items with four sub-concepts), confidence (11 items), and self-reported practices (11 items). Demographic and relevant objective work-experience characteristics included age (years), gender (male = 0, female = 1), educational level (junior middle school or less = 0, high school or vocational college = 1, and bachelor or above = 2), marital status (unmarried = 0, married = 1, and divorced or widowed = 2), nationality (minorities = 0, Han = 1), religious belief (none = 0, other = 1), professional title (none = 0, junior = 1, intermediate = 2, and senior = 3), the experience of death witness (no = 0, yes = 1), the willingness of providing palliative care (no = 0, yes = 1), and institution type (nurse home = 0, community health centers = 1, and hospital = 2). The Cronbach's α coefficient of knowledge, attitude, confidence, and practices scale was 0.686, 0.868, 0.960, and 0.971, respectively (13). Scores for each subcategory were calculated separately. Regarding the knowledge scale, a score of 1 was given for a correct answer and 0 for an incorrect or unknown answer. The overall score ranges from 0 to 15, with higher scores indicating better palliative care knowledge. Meanwhile, each item in the attitudes section was scored by a 5-point Likert scale (1 = totally disagree to 5 = totally agree) and higher scores indicate better attitudes. Self-efficacy was assessed by a confidence scale (1 = no confidence to 5 = extreme confidence). The overall score ranges from 11 to 55, with higher scores indicating greater self-efficacy. Practices were scored by a 5-point Likert scale (1 = never do to 5 = always do). The overall score ranges from 14 to 70, with higher scores indicating greater work practices.
Model construction
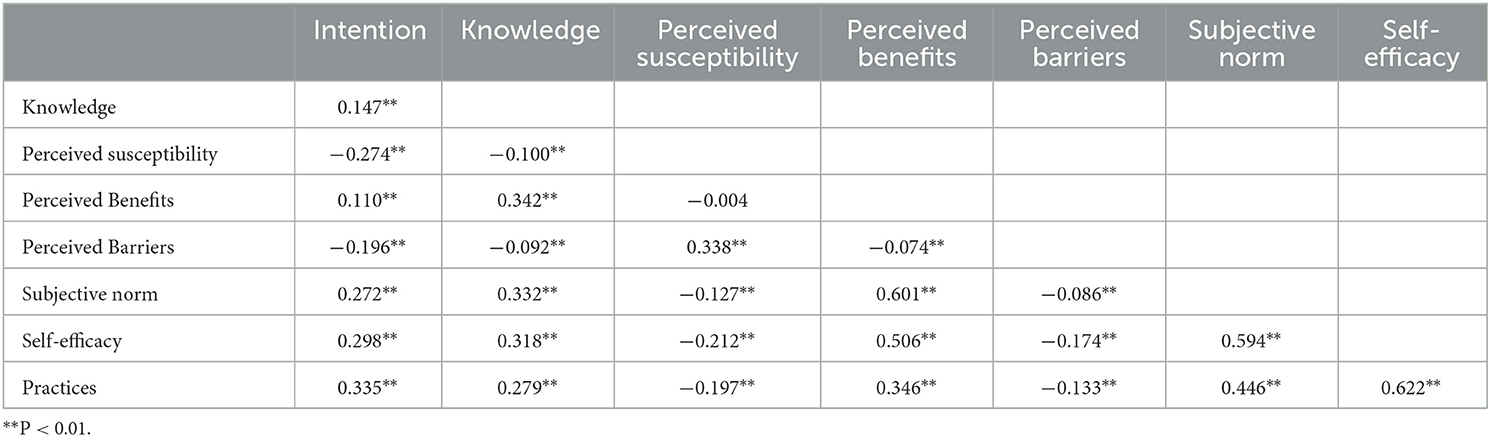
The theoretical framework in this study originates from three classical and widespread health and behavior theories: the Health Belief Model (HBM) (15), the Theory of Reasoned Action (TRA) (16), and the Integrated Behavior Theory (IBT) (17). According to the HBM theory, which is a model of health education that changes people's behavior by intervening in their psychological activities such as perceptions, attitudes and beliefs, perceived susceptibility, perceived benefits, perceived barriers, and self-efficacy influence behavior change. Based on the TRA, whether a person engages in behavior directly depends on their intention to act. In addition, subjective norm affects behavioral intention. IBT theory suggests that behavior is influenced by knowledge. Based on the theoretical components and dimensions mentioned in the above three theories and existing domestic and international research, knowledge, attitudes, self-efficacy, intention, and practices were incorporated into the hypothesis model (Figure 1) for confirmatory analysis. Behavioral intention is a fundamental intermediary factor, determined by self-efficacy and attitudes of individuals. Consequently, nurses' practices in palliative care may be affected by knowledge, attitudes, self-efficacy, and intention in our hypothetical model.
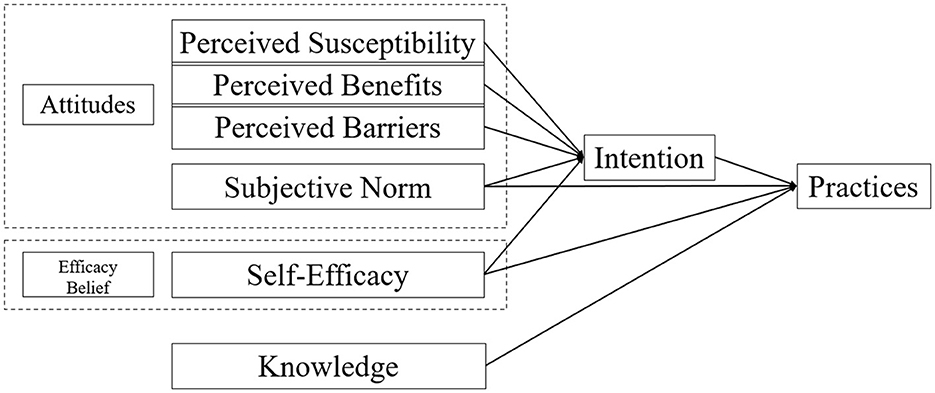
Figure 1. Hypothetical model for practices and their influencing factors among nurses concerning palliative care.
Therefore, in the current study, we verified the associations among knowledge, self-efficacy, subjective norm, perceived susceptibility, benefits, barriers, intention, and practices using the structural equation model. Based on the theoretical framework and literature review, we developed a model to identify the following hypotheses: (1) Intention directly influences practices. (2) Subjective norms and self-efficacy have direct and indirect effects on practices through intention. (3) Knowledge directly influences practices. (4) Perceived susceptibility, benefits, and barriers have indirect effects on practices through intention.
Statistical methods
Descriptive data were generated for all variables. Statistical analyses were performed using commercial software IBM SPSS Statistics 24.0 and AMOS version 20.0 (IBM Corporation, Armonk, NY). The level of significance was set at a p < 0.05. Categorical data were described by frequencies and percentages, and continuous data by means of standard deviations (SD). Pearson's (r) correlation was performed to verify the relationship between all variables. 0 ≤ |r| < 0.3 means low correlation; 0.3 ≤ |r| < 0.8 means medium correlation; 0.8 ≤ |r| ≤ 1.0 means high correlation. A P < 0.05 was considered statistically significant. A structural equation model was used to test the associations between all variables. Path analysis was used to identify both direct and indirect relationships in the model. Standardized regression coefficients (β) and lower and upper bounds for β were reported for direct, indirect, and total effects. The model fit was assessed using the following model-fit indices: relative chi-square (χ2/df) < 3; goodness of fit index (GFI) > 0.900, adjusted goodness of fit index (AGFI) > 0.900, comparative fit index (CFI) > 0.900, normed fit index (NFI) > 0.900, incremental fit index (IFI) > 0.900, Tucker–Lewis index (TLI) > 0.900, and root mean squared error of approximation (RMSEA) < 0.06 (18).
Results
Participants' characteristics
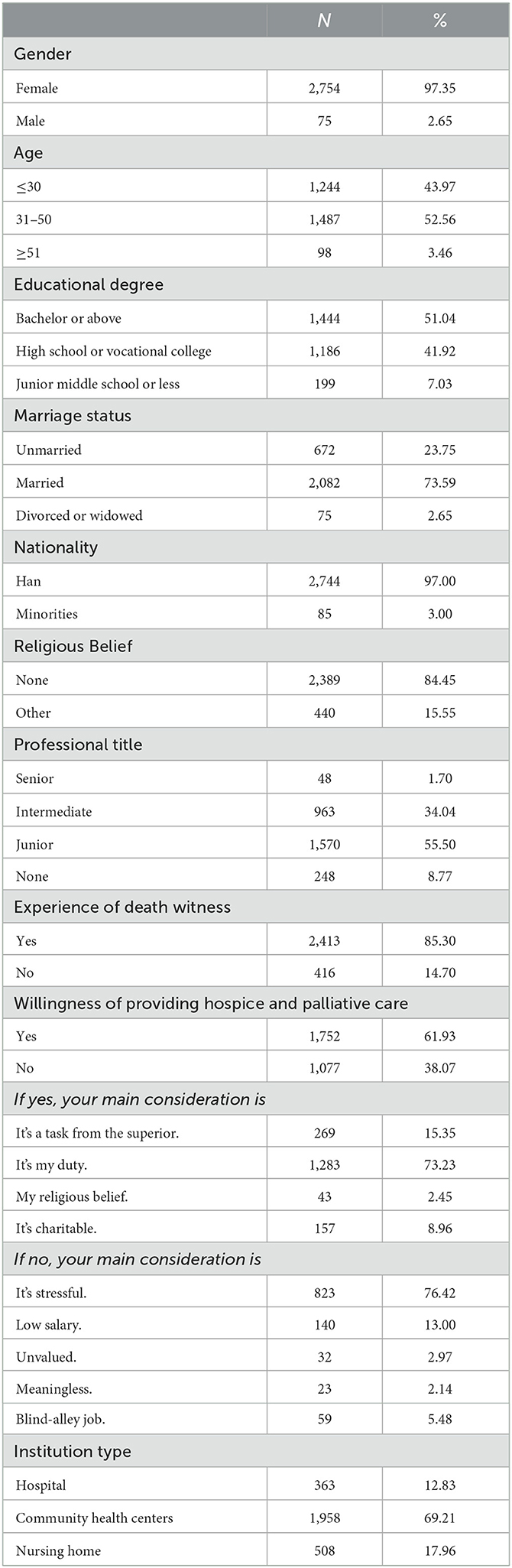
A total of 2,829 nurses from 225 institutions across Shanghai's districts were enrolled. The demographic characteristics of the respondents are listed in Table 1. The nurses' work units included the following: community health centers (69.21%) were the most common units, followed by nursing homes (17.96%) and hospitals (12.83%). The mean age was 36.83 ± 9.35 years.
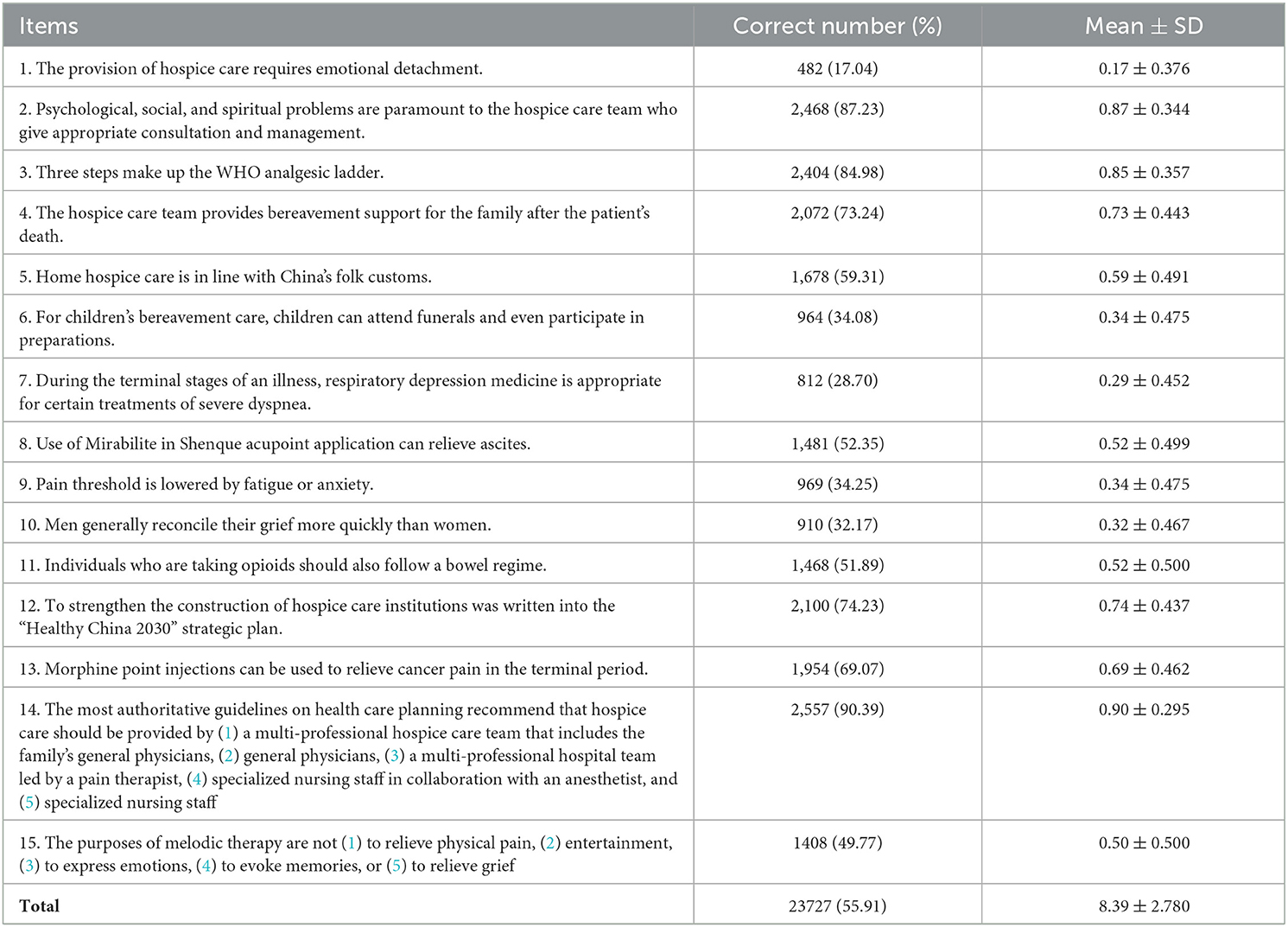
Knowledge
The mean score of the knowledge scale was 8.39 ± 2.780; the response accuracy was 55.91%. Table 2 details the questions and scores.
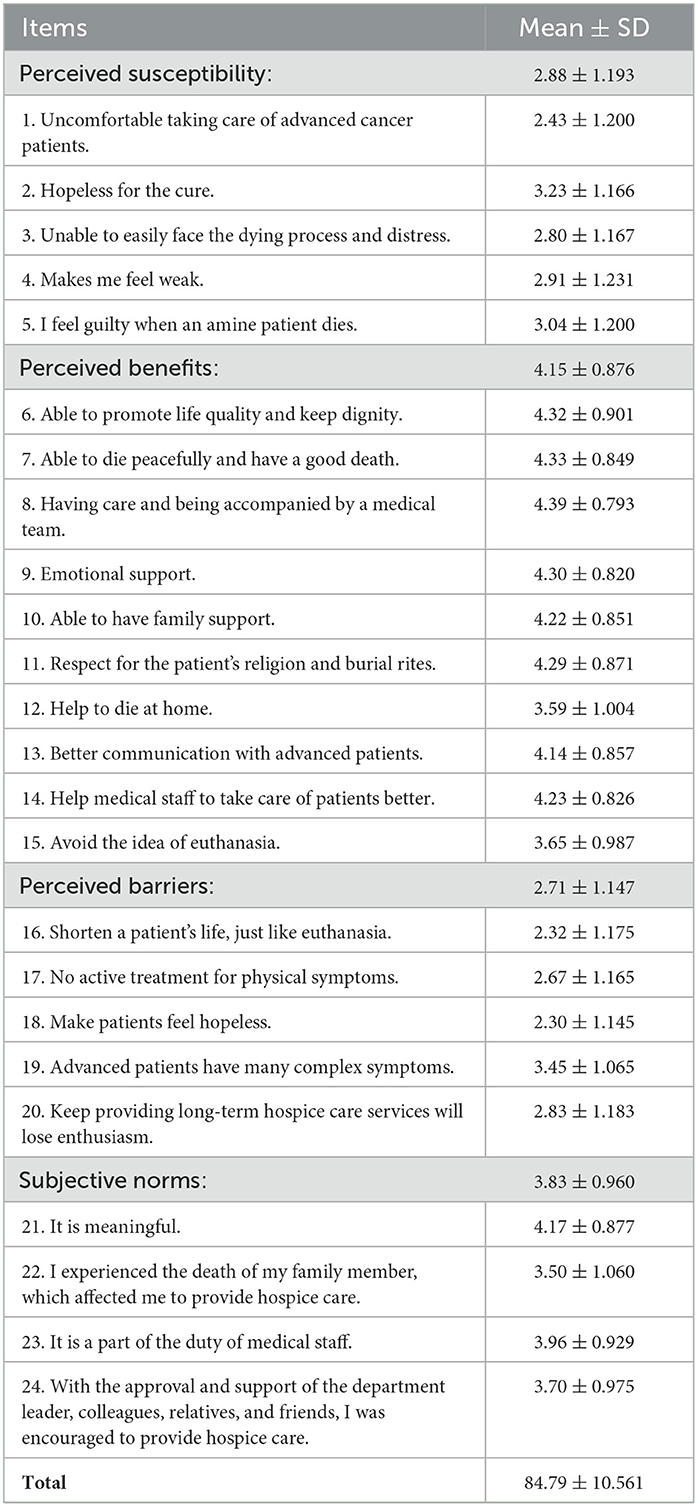
Attitudes
The mean score on the attitudes scale was 84.79 ± 10.561, and the total scoring rate was 70.66%. Table 3 presents the attitudes scale items and their mean scores. The mean scores of perceived susceptibility, perceived benefits, perceived barriers, and subjective norms were 2.88 ± 1.193, 4.15 ± 0.876, 2.71 ± 1.147, and 3.83 ± 0.960, respectively.
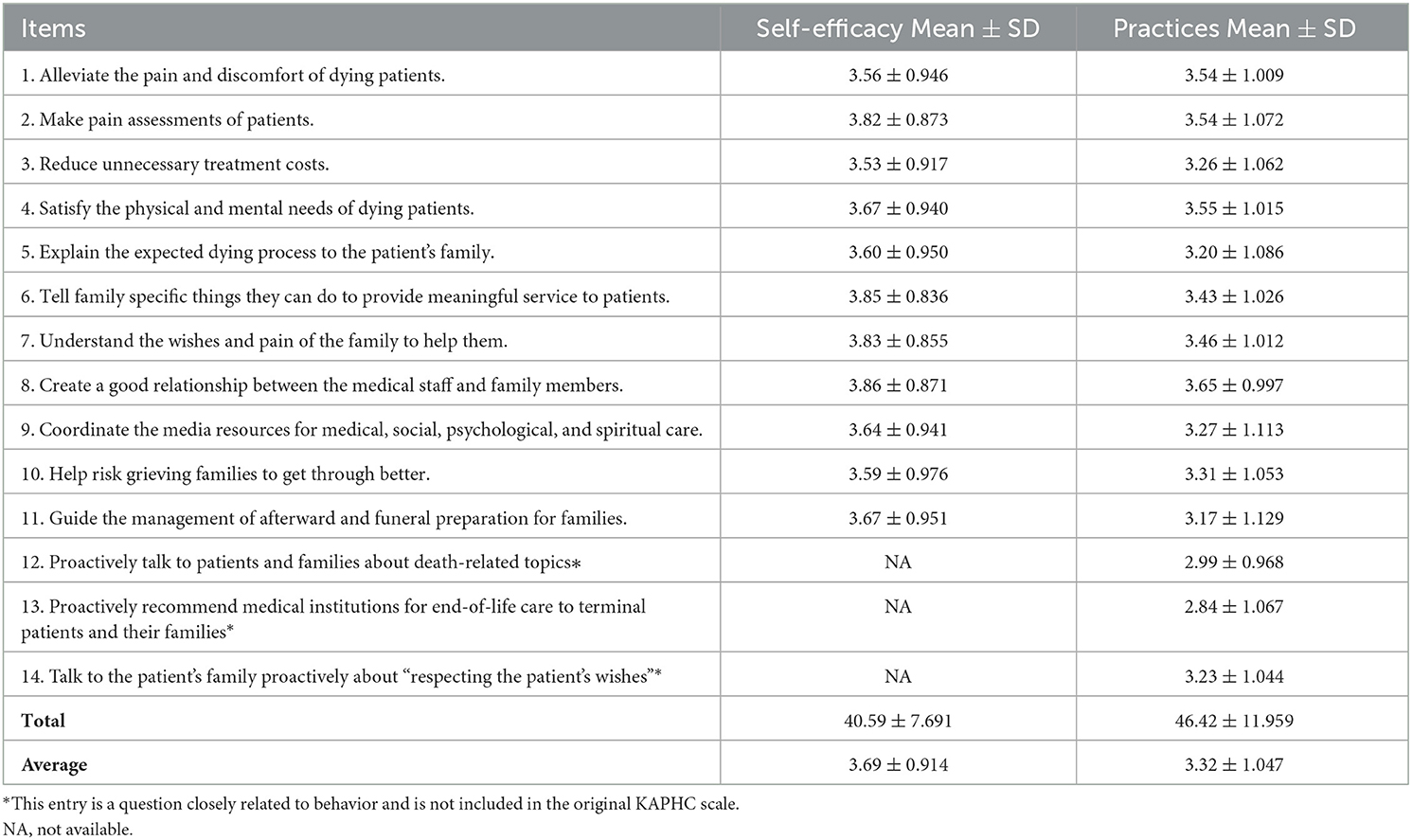
Self-efficacy and practices
The mean score of self-efficacy was 40.59±7.691, which was approximately 73.80% of the total score. The mean score of practices was 46.42±11.959, which was approximately 66.31% of the total score. Table 4 presents the mean scores of each item.
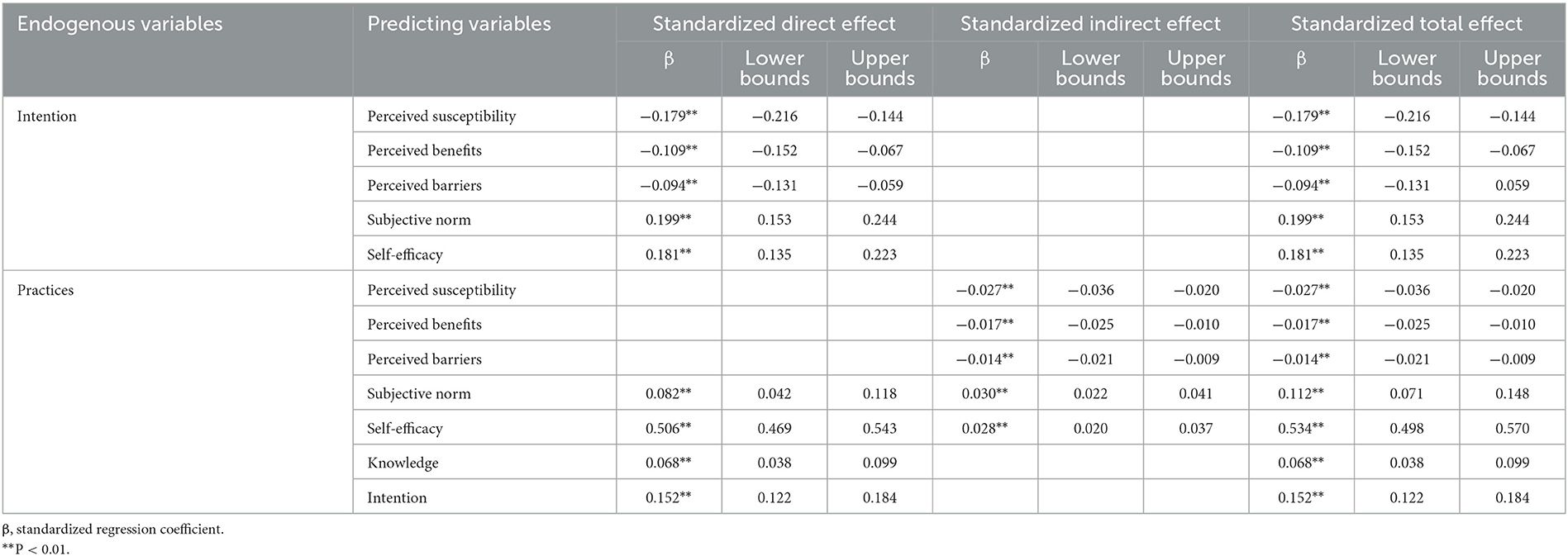
Bivariate analysis
Bivariate correlations are shown in Table 5. Knowledge was positively associated with perceived benefits (r = 0.342, P < 0.01), subjective norm (r = 0.332, P < 0.01), self-efficacy (r = 0.318, P < 0.01), and practices (r = 0.279, P < 0.01). Perceived susceptibility was positively associated with barriers (r = 0.338, P < 0.01). Benefits were positively associated with the subjective norm (r = 0.601, P < 0.01), self-efficacy (r = 0.506, P < 0.01), and practices (r = 0.346, P < 0.01). Subjective norm was moderately positively associated with self-efficacy (r = 0.594, P < 0.01) and practices (r = 0.446, P < 0.01). Self-efficacy was positively associated with practices (r = 0.622, P < 0.01).
Structural equation modeling
The model was modified by removing the non-significant paths using AMOS until the final model showed a good model fit. The revised model is shown in Figure 2. The final model manifested a satisfactory model fit (χ2/df = 2.624; GFI = 0.999, AGFI = 0.992, NFI = 0.998, IFI = 0.999, TLI = 0.992, CFI = 0.999; RMSEA = 0.024, 90%CI = 0.006–0.042). The standardized direct, indirect, and total coefficients are summarized in Table 6. Several important results of this study are as follows: (1) Intention directly influenced practices. The standardized path coefficient of the direct effect is 0.152 (P < 0.01). (2) Subjective norm and self-efficacy had direct and indirect impacts on practices through intention. The standardized path coefficient of the direct, indirect, and total effect of subjective norm on practices was 0.082 (P < 0.01), 0.030 (P < 0.01), and 0.112 (P < 0.01), respectively. The standardized path coefficient of the direct, indirect, and total effect of self-efficacy on practices was 0.506 (P < 0.01), 0.028 (P < 0.01), and 0.534 (P < 0.01), respectively. (3) Knowledge directly influenced practices. The standardized path coefficient of the direct effect is 0.068 (P < 0.01). (4) Perceived susceptibility, perceived benefits, and perceived barriers had indirect effects on practices through intention. The standardized path coefficients of indirect effect are −0.027 (P < 0.01), −0.017 (P < 0.01), and −0.014 (P < 0.01), respectively.

Figure 2. Structural equation model of nurses' practices in palliative care (standardized estimates).
Discussion
Our original study has analyzed the interrelationship and intensity between practices and related factors among palliative care nurses in Shanghai, providing evidence of the associations of knowledge, perceived susceptibility, benefits, barriers, subjective norm, self-efficacy, intention, and practices aiming at palliative care nurses and interventions improving their actual work practices. The structural equation model authenticated the interrelationship and intensity between all dimensions, highlighting that self-efficacy, intention, and subjective norms greatly influenced practices among nurses concerning palliative care. Concretely, self-efficacy and subjective norms had direct and indirect impacts on practices. Intention and knowledge directly influenced practices. Perceived susceptibility, perceived benefits, and perceived barriers had indirect effects on practices through intention. The above hypotheses are verified by the model.
Our study found that the average score rating of nurses' practices (66.3%) was lower than that of all health providers in Shanghai (74.5%) (19) and that of oncology nurses in Shandong Province (82.2%) (20). This result may be in part because the majority of the participants in our study worked in primary healthcare institutions, including community health centers and nursing homes. In the initial stage of palliative care pilot work in Shanghai, there is a shortage of multidisciplinary team composition, and nurses undertake multi-functional roles and diversified nursing in primary healthcare institutions. Strategies to improve nurses' practices should be addressed when developing interventions.
In the model, self-efficacy, which was defined as the degree of confidence of nurses in the provision of palliative care services in this study, had profound the most important direct impacts on practices, indicating that nurses with better confidence have a stronger disposition to practices. A cross-sectional study showed that exploring the traditional Chinese philosophy of life was essential for the improvement of hospice care self-efficacy (21). Another study showed a positive and statistically significant correlation between communication skills and self-efficacy (22). Therefore, it is crucial to strengthen communication skills and enhance confidence through comprehensive and systematic training in respect of Chinese traditional concepts of life and death in order to further promote practical palliative care practice. Meanwhile, this result was in line with the previous study in which a significantly positive association between self-efficacy and practices has been observed (23), indicating that it is also a critical predictor and appropriate index measuring the self-efficacy of nurses to evaluate the level of practices.
Intention, which was defined as a willingness to practice, directly influenced and had a significantly positive association with practices. As shown in the model, the intention was positively affected by subjective norms and self-efficacy and negatively affected by perceived susceptibility to the condition of terminal patients' deterioration and perceived barriers to palliative care service provision. An analysis showed that whether nurses had clinical hospice care experience affected their willingness to practice (23). However, the demographic characteristics of the respondents showed that a part of the participants had no experience with death witnesses and was unwilling to provide palliative care services, which reduced practice frequency. Therefore, nurses should be emboldened to improve their behavioral intention by participating in the real case of end-of-life, improving clinical practices and training on death, and establishing an objective view of life and death.
Subjective norms also had direct and indirect impacts on practices, indicating that social values, expectations of leaders, and encouragement of colleagues had a great impact on the provision of palliative care services. There is a significantly positive correlation between subjective norms and practices, which was in line with another study (24), manifesting that the potential usefulness of subject consciousness and motivation in respect of palliative care services were self-evident. Strategies enhancing norm belief and compliance motivation and interventions, such as implicit messages and intentional teaching, should be considered (25).
The model also revealed the direct effects of knowledge on practices, reflecting the effectiveness of continuing education to improve nurses' competence in providing qualified palliative care services. Empirical research proved that targeted training in palliative care can address the knowledge and skills gaps in time. Moreover, a significantly positive correlation between knowledge and practices was obtained, which resembled another study (10). Despite the frequent phenomenon of knowing without doing, the great majority of researchers hold the view that the effect of knowledge on practices is worth affirming fully and permanently among other factors (26). Previous study showed that the lack of adequate end-of-life and legal literacy training for nurses was a key reason why the overall knowledge of health service providers in Shanghai was generally moderate (21) and a lack of adequate training on end-of-life will and legal knowledge for nurses is a key reason (27). Consequently, it is highly necessary for nurses, the major primary health service providers in diversified nursing, to systematically learn theoretical knowledge in palliative care, strengthen education on life and death, and improve the understanding of the concept and significance of palliative care services.
Perceived susceptibility, benefits, and barriers had negative indirect effects on practices through intention. First, perceived susceptibility had the most dramatic effect among three dimensions, indicating that nurses always felt upset, anxious, weak, hopeless, guilty, suffocated, and grieved and were unable to easily face the dying process of coping with patient death, which was unanimous with another study (28). Second, perceived barriers had indirect effects on practices, showing that nurses who had more perceived difficulties concerning palliative care had lower behavior, which was consistent with a previous study (29). Finally, perceived benefits had an indirect effect on practices. This phenomenon manifests that although nurses can realize the benefit of patients receiving palliative care is that patients are able to die peacefully and had a good death with omnidirectional care, highlife quality, and dignity (30). The patient's religion and burial rites should be respected (31). However, some participants perceived the provision of palliative care services as a serious burden, concerning occupational prospects, low salaries, and coping with a broad range of stressors in actual work practices. Thus, perceived susceptibility and barriers remain dominant factors, which is showing no difference with another study (32). Hence, it is necessary to provide effective strategies to treat themselves with empathy, kindness, and awareness of common humanity in clinical practices, contributing to their wellbeing.
Knowledge and attitudes are the antecedents and prerequisites. Before producing behavior, people transform external and internal needs into motivation and purpose through self-consciousness and understanding, to guide and regulate behavior and practices. After the change in knowledge and attitudes, behavior ultimately changes. A previous study showed that, in regular and continuous behavior, there is a two-way influence in the relationship between motivation, attitudes, beliefs, and behavior (33). In providing palliative care services, nurses' work practices will, in turn, promote changes in their own knowledge, attitudes, subjective norms, self-efficacy, and intention.
Strengths and limitations
The availability and accessibility of palliative care continue to be major global public health problems and are more challenging in China. However, few studies have investigated the interrelationship and intensity between practices and their influencing factors among nurses in palliative care. To our best knowledge, this is an original large-scale empirical study that has meticulously analyzed the interrelationship and intensity between practices and other factors among nurses in the initial stage concerning palliative care in primary healthcare institutions in Shanghai, China. Our findings have some practical implications and valuable information for nurses concerning palliative care. High-quality palliative care services can be achieved only by scaling up interventions to enhance self-efficacy, intention, subjective norm, and knowledge to motivate nurses to provide patient-centered integrated, and comprehensive behavior.
However, several limitations should be noted. First, most recent health behavior theories used in China originated from western culture. Because behavior is the profound embodiment of culture, the suitability of these theories in China is worth considering. Furthermore, most of the participants worked mainly in primary healthcare institutions. There is an urgent need for future basic and applied research studies on the influencing factors on nurses' practices in secondary and tertiary medical institutions. Finally, although the structural equation model is an advanced and reliable quantitative analysis method, it still contains subjective cognition from researchers. Therefore, other several complex mathematical models and analysis methods should be considered in further study to avoid bias.
Conclusion
This study preliminarily established a theoretical foundation by structural equation model among 2,892 nurses in healthcare institutions in Shanghai. The hypothetical model verified the interrelationship and intensity between nurses' practices of palliative care and several significant factors; Intention and knowledge directly influence practices; Subjective norm and self-efficacy have both direct and indirect impacts on practices through intention; Additionally, perceived susceptibility, perceived benefits, and perceived barriers had indirect effects on practices through intention. Ultimately, it is imperative to scale up targeted interventions focusing on self-efficacy, intention, and subjective norms to improve the practices of nurses, especially for nurses working in primary healthcare institutions. High-quality palliative care services can be achieved by motivated nurses with strong practical nursing abilities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LJ secured the funding to conduct this research and was responsible for conceptualizing the manuscript. JH participated in project design and grant article publication. YX and XT collected and analyzed the data. ZS contributed to the design of the scale. YX and SZ drafted the initial manuscript. ML and TC revised and polished the manuscript. JW and YM proofread the logical framework. SL coordinated the investigation. All authors were responsible for critical revisions and approval of the final manuscript.
Funding
This study was supported by grants from the Nature Science Foundation of Shanghai (No. 22ZR1461400), China Medical Board Open Competition Program (CMB-OC grant number 20-386), Shanghai Science and Technology Commission, Soft Science Research Project of Science and Technology Innovation Action Plan (grant number 23692112700), Humanities and Social Science Research Planning Fund of the Ministry of Education (No. 20YJAZH045), and Philosophy and Social Science Planning Project of Shanghai (No. 2019BGL032).
Acknowledgments
We gratefully acknowledge the participation of all healthcare institutions and providers.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, et al. Redefining palliative care-a new consensus-based definition. J Pain Symptom Manage. (2020) 60:754–64. doi: 10.1016/j.jpainsymman.2020.04.027
2. Xu YF, Jing LM, Li XY, Li SJ. Hospice and palliative care services development in Shanghai. Open Access J Complement Altern Med. (2021). doi: 10.32474/OAJCAM.2021.03.000165. [Epub ahead of print].
3. Lukovsky J, McGrath E, Sun C, Frankl D, Beauchesne MA, A. Survey of hospice and palliative care nurses' and holistic nurses' perceptions of spirituality and spiritual care. J Hosp Palliat Nurs. (2021) 23:28–37. doi: 10.1097/NJH.0000000000000711
4. Gómez-Urquiza JL, Albendín-García L, Velando-Soriano A, Ortega-Campos E, Ramírez-Baena L, Membrive-Jiménez MJ, et al. Burnout in palliative care nurses, prevalence and risk factors: a systematic review with meta-analysis. Int J Environ Res Public Health. (2020) 17:7672. doi: 10.3390/ijerph17207672
5. Greene PE. The pivotal role of the nurse in hospice care. CA Cancer J Clin. (1984) 34:204–05. doi: 10.3322/canjclin.34.4.204
6. Teng XH, Jing LM, Shu ZQ, Xu YF, Shu ZQ. Survey on attitude and influencing factors of hospice care among health providers in Shanghai. Chin J Gen Pract. (2021) 20:556–61. doi: 10.3760/cma.j.cn114798-20200815-00909
7. Ling M, Wang XC, Ma YH, Long Y. A review of the current state of hospice care in China. Curr Oncol Rep. (2020) 22:99. doi: 10.1007/s11912-020-00959-y
8. Bitschnau KW, Firth P, Wasner M. Social work in hospice and palliative care in Europe: Findings from an EAPC survey. Palliat Support Care. (2020) 18:662–69. doi: 10.1017/S1478951520000279
9. Middleton AA, Head BA, Remke SS. Role of the hospice and palliative care social worker #390. J Palliat Med. (2020) 23:573–74. doi: 10.1089/jpm.2019.0698
10. Lin HY, Chen CI, Lu CY, Lin SC, Huang CY. Nurses' knowledge, attitude, and competence regarding palliative and end-of-life care: a path analysis. PeerJ. (2021) 9:e11864. doi: 10.7717/peerj.11864
11. Wang HA, Wang DL, Chen YH, Yuan FF, Yang Q, A. qualitative study on nursing experience of hospice care specialist nurse for patients with advanced cancer. Chin Community Doc. (2021) 37:134–35. doi: 10.3969/j.issn.1007-614x.2021.32.064
12. Wu X, Zhang X, Zhang J, Cui X. Analysis of knowledge, attitude and behavior of oncology medical staff in palliative care. Ann Palliat Med. (2020) 9:985–92. doi: 10.21037/apm-20-851
13. Shu ZQ, Wang YT Li TT, Jing LM, Sun XM. Instrument development of health providers' Knowledge, Attitude and Practice of Hospice Care Scale in China. Int J Health Plann Manage. (2021) 36:364–80. doi: 10.1002/hpm.3074
14. Teng XH, Tang MC, Jing LM, Xu YF, Shu ZQ. Healthcare provider knowledge, attitudes, and practices in hospice care and their influencing factors: a cross-sectional study in Shanghai. Int J Health Policy Manag. (2022) 11:3090–100. doi: 10.34172/ijhpm.2022.6525
15. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. (1988) 15:175–83. doi: 10.1177/109019818801500203
16. He J, Wan L, Luo B. Intentions and influencing factors regarding natural childbirth among urban pregnant women in China, based on the theory of reasoned action and structural equation modeling. J Int Med Res. (2019) 47:4482–91. doi: 10.1177/0300060519862089
17. Glanz K, Rimer KB, Viswanath K. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Health behavior: Theory Research and Practice. Glanz K Rimer, BK, Viswanath V. (eds.). Jossey-Bass/Wiley. p. 95–124.
18. Hu, LT, Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
19. Xu YF, Jing LM, Teng XH, Shu ZQ Li SJ. Survey on practice of hospice care and influencing factors among health providers in Shanghai. Chin J Gen Pract. (2021) 20:562–67. doi: 10.3760/cma.j.cn114798-20200815-00910
20. Zhu C, Miao ZL, Wei XA. Investigation on knowledge, belief and practice of hospice care among cancer nurses and its related factors. Int J Nursing. (2021) 40:3677–81. doi: 10.3760/cma.j.cn221370-20191230-01037
21. Teng XH, Shu ZQ, Jing LM, Xu YF. Survey on knowledge and influencing factors of hospice care among health providers in Shanghai. Chin J Gen Pract. (2021) 20:452–57. doi: 10.3760/cma.j.cn114798-20200815-00908
22. Leal-Costa C, Tirado GS, Ramos-Morcillo AJ, et al. Communication skills and professional practice: does it increase self-efficacy in nurses? Front Psychol. (2020) 11:1169. doi: 10.3389/fpsyg.2020.01169
23. Chen L, Li XH, Pan X, Pan QN, Huang HQ, Tao PY, et al. Nurses' knowledge, attitudes, and willingness to practice hospice care: an analysis of influencing factors. PLoS One. (2022) 17:e259647. doi: 10.1371/journal.pone.0259647
24. Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WM, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychol. (2016) 35:1178–88. doi: 10.1037/hea0000387
25. Billings ME, Engelberg R, Curtis JR, Block S, Sullivan AM. Determinants of medical students' perceived preparation to perform end-of-life care, quality of end-of-life care education, and attitudes toward end-of-life care. J PALLIAT MED. (2010) 13:319–26. doi: 10.1089/jpm.2009.0293
27. Xu YF, Wang YT, Teng XH, Jing LM, Shu ZQ Li SJ, et al. Training needs and influencing factors of hospice care for health providers in Shanghai. Chin J Gen Pract. (2021) 20:470–74. doi: 10.3760/cma.j.cn114798-20200815-00911
28. Zheng R, Lee SF, Bloomer MJ. How nurses cope with patient death: A systematic review and qualitative meta-synthesis. J Clin Nurs. (2018) 27:e39–49. doi: 10.1111/jocn.13975
29. Wu XY, Zhou ZH, Zhang YH, Lin XY, Zhang M, Pu FL, et al. Factors associated with behaviors toward end-of-life care among chinese oncology nurses: a cross-sectional study. Asian Nurs Res (Korean Soc Nurs Sci). (2021) 15:310–16. doi: 10.1016/j.anr.2021.10.003
30. Aghdam AM, Aghaei MH, Hassankhani H, Rahmani A. Awareness and attitude of nurses in regard to providing hospice care. Asian Pac J Cancer Prev. (2015) 16:6941–45. doi: 10.7314/apjcp.2015.16.16.6941
31. Holland DE, Vanderboom CE, Dose AM, Moore D, Robinson KV, Wild E, et al. Death and grieving for family caregivers of loved ones with life-limiting illnesses in the era of COVID-19: considerations for case managers. Prof Case Manag. (2021) 26:53–61. doi: 10.1097/NCM.0000000000000485
32. Bar-Sela G, Schultz MJ, Elshamy K, Rassouli M, Ben-Arye E, Doumit M, et al. Training for awareness of one's own spirituality: a key factor in overcoming barriers to the provision of spiritual care to advanced cancer patients by doctors and nurses. Palliat support care. (2019) 17:345–52. doi: 10.1017/S147895151800055X
Keywords: nurse, practices, structural equation model, influencing factors, palliative care
Citation: Xu Y, Zhang S, Wang J, Shu Z, Jing L, He J, Liu M, Chu T, Teng X, Ma Y and Li S (2023) Nurses' practices and their influencing factors in palliative care. Front. Public Health 11:1117923. doi: 10.3389/fpubh.2023.1117923
Received: 07 December 2022; Accepted: 17 April 2023;
Published: 17 May 2023.
Edited by:
Mevhibe Hocaoglu, King's College London, United KingdomReviewed by:
Richard John Siegert, Auckland University of Technology, New ZealandHammoda Abu-Odah, Hong Kong Polytechnic University, Hong Kong SAR, China
Maryam Rassouli, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2023 Xu, Zhang, Wang, Shu, Jing, He, Liu, Chu, Teng, Ma and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Limei Jing, bGltZWlfamluZ0AxNjMuY29t; bG1qaW5nQGxpdmUuY24=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share senior authorship
 Yifan Xu
Yifan Xu Shiwen Zhang1†
Shiwen Zhang1† Limei Jing
Limei Jing Tianshu Chu
Tianshu Chu Xiaohan Teng
Xiaohan Teng Yanan Ma
Yanan Ma