- 1Student Research Committee, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran
- 2Department of Epidemiology and Biostatistics, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
- 3Dental Research Center, Dental Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran
Background: Diabetes mellitus is related to variable dental and oral complications like xerostomia and periodontal problems. Therefore, diabetes can affect the oral status and oral health-related quality of life (OHRQoL). A systematic review of evidence can determine the association between diabetes and OHRQoL. so, this study aimed to evaluate the effects of diabetes on OHRQoL.
Methods: After determining the PECO and eligible criteria, a comprehensive search was conducted in PubMed, Scopus, Web of Science, and Embase without any restriction. Further searches were performed in Google Scholar and reference lists of selected articles. Two independent reviewers carried out paper selection, data extraction, and quality assessment. A meta-analysis was conducted using a “random effect model” and the standardized mean difference of OHRQoL with a 95% confidence interval (CI) was reported as estimating pooled effect size.
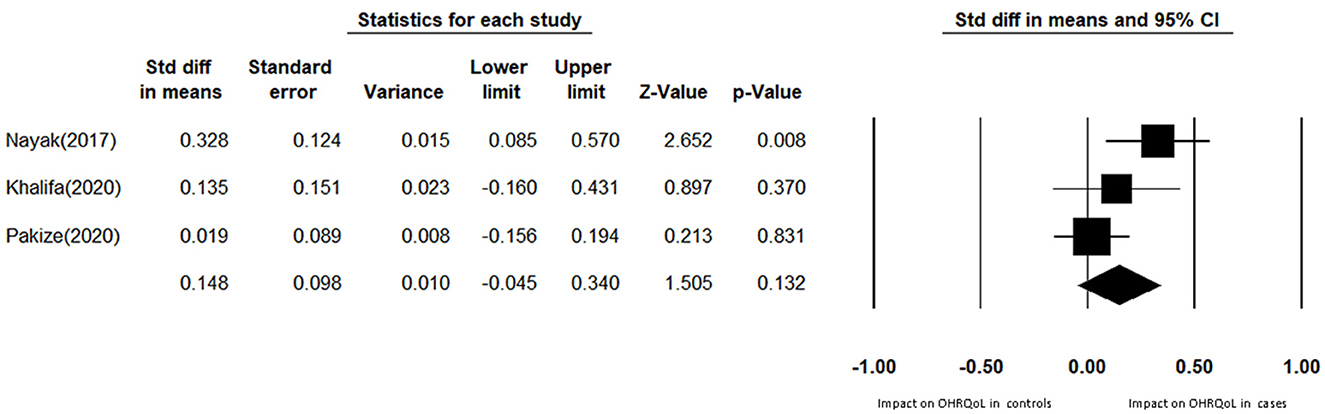
Results: After screening 237 identified records, three case-control and ten cross-sectional studies met eligibility criteria. Two cross-sectional studies were excluded in the quality assessment phase and the rest of the studies have a low or moderate risk of bias. The pooled standardized mean difference between the case and the control groups was 0.148 (95% CI: −0.045 to 0.340).
Conclusion: Diabetes mellitus has no statistical significant association with OHRQoL. Nevertheless, based on the articles' review, it seems that diabetes can lead to functional limitations, physical pain, and psychological discomfort. Also, complications of diabetes adversely affect wellbeing. Hence dentists can play an essential role in the awareness of persons with diabetes about these problems and improve their OHRQoL.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022303038, identifier CRD42022303038.
1. Introduction
Diabetes mellitus is a chronic disease caused by insulin dysfunction and deficiency characterized by hyperglycemia (high blood glucose) (1, 2). Chronic hyperglycemia causes defects and failure in different body parts like the nervous system, eyes, kidneys, and cardiovascular system (3–5).
International Diabetes Federation (IDF) estimated that in 2021, 536.6 million adults had diabetes in 215 countries. It also stated that by 2,045, approximately 783.2 million people worldwide will have diabetes mellitus (6).
Diabetes also relates to variable dental and oral complications, consisting of dental caries (7), gingival problems, periodontal abscess, and periodontitis (8, 9), xerostomia (7), vesiculobullous lesions, oral fungal infections, increased possibility of post-operative infections, and impaired wound healing (10–12).
Several studies consider that oral health complications can adversely affect physical function, social status, psychological comfort, and emotional state (13–15). Therefore, the relationship between oral and dental health and its possible consequences on quality of life is undeniable. Additionally, some original studies considered diabetes as a factor that may affect oral health-related quality of life (OHRQoL) (16–20). On that account, OHRQoL attracts dental practitioners' and researchers' attention toward itself.
OHRQoL is one of the subsets of health-related quality of life that examines the effect of oral health and status on quality of life. OHRQoL reflects people's comfort when eating, sleeping, and engaging in social interaction; their self-esteem; and their satisfaction concerning their oral health (21–23). OHRQoL is mainly assessed by questionnaires such as Oral Health Impact Profile (OHIP) and Geriatric Oral Health Assessment Index (GOHAI). OHIP is The most widely available questionnaire for quantification of OHRQoL, which measures the seven domains of functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap (24).
Thus, our study aimed to perform a systematic review and meta-analysis to evaluate the effects of diabetes on oral health-related quality of life.
2. Methods
2.1. Protocol and registry
This systematic review and meta-analysis were carried out following the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (25), and the protocol was registered to PROSPERO (reg. no. CRD42022303038).
2.2. PECO question
Does diabetes mellitus affect oral health-related quality of life in diabetic adults?
2.3. Eligibility criteria
Observational studies (cross-sectional, case-control, and cohort) that examined diabetes mellitus as the exposure and OHRQoL as the outcome (determined by OHIP or GOHAI questionnaire) and also studied individuals over 18 years of age were included. Studies in which participants had received periodontal treatment in the past 6 months were excluded, along with case reports, reviews, and review protocols. In addition, no restrictions on language or year of publication were considered.
2.4. Literature search and screening
Two independent reviewers (YMH and KA) carried out a systematic literature search using PubMed, ISI Web of Science, EMBASE, and Scopus without any restriction on language or other limitations until April 2022. Further searches were conducted in Google Scholar (gray literature) and reference lists of selected articles until May 2022. We used following search query in PubMed: (“diabetic patient*”[All Fields] OR “diabet*”[All Fields] OR “Diabetes Mellitus”[MeSH Terms] OR “Diabetes Mellitus”[All Fields] OR “diabetes mellitus, type 1”[MeSH Terms] OR “diabetes mellitus type 1”[All Fields] OR “diabetes mellitus, type 2”[MeSH Terms] OR “diabetes mellitus type 2”[All Fields] OR “T1DM”[All Fields] OR “T2DM”[All Fields]) AND (“Oral Health Related Quality of Life”[All Fields] OR “OHRQoL”[All Fields] OR “OHRQL”[All Fields]). The search strategies of other databases are also presented in Supplementary Table 1.
After removing duplicated studies, two independent reviewers (KM and ST) screened the title and abstract of studies according to eligibility criteria. Dubious studies were kept for the next stage. Then, the remaining full-text articles were evaluated according to inclusion and exclusion criteria, and relevant reports were selected. Any disagreements about the selection of articles between two reviewers were resolved by consulting the third reviewer (YMH).
2.5. Quality assessment
The same two reviewers (KM and ST) independently evaluated the quality of studies using NIH quality assessment tools for Observational Cohort and Cross-Sectional Studies and Case-Control Studies (26). For the former, scores of 0–4 were considered poor, 5–9 were considered fair, and scores of 10–14 were considered good quality. For the latter, scores of 0–4 (poor), 5–8 (fair), and 9–12 (good) were considered to assess the quality of the included studies.
2.6. Data extraction
A data extraction spreadsheet was designed, and the following information was independently extracted by two reviewers (KM and ST): first author's name, year of publication, country, study design (Cross-Sectional, Case-Control, and Cohort studies), participant characteristics (sample size, gender, and age), type of questionnaire and statistical summaries related to OHRQoL (effect measures, confidence intervals, and p-values).
2.7. Statistical methods and data synthesis
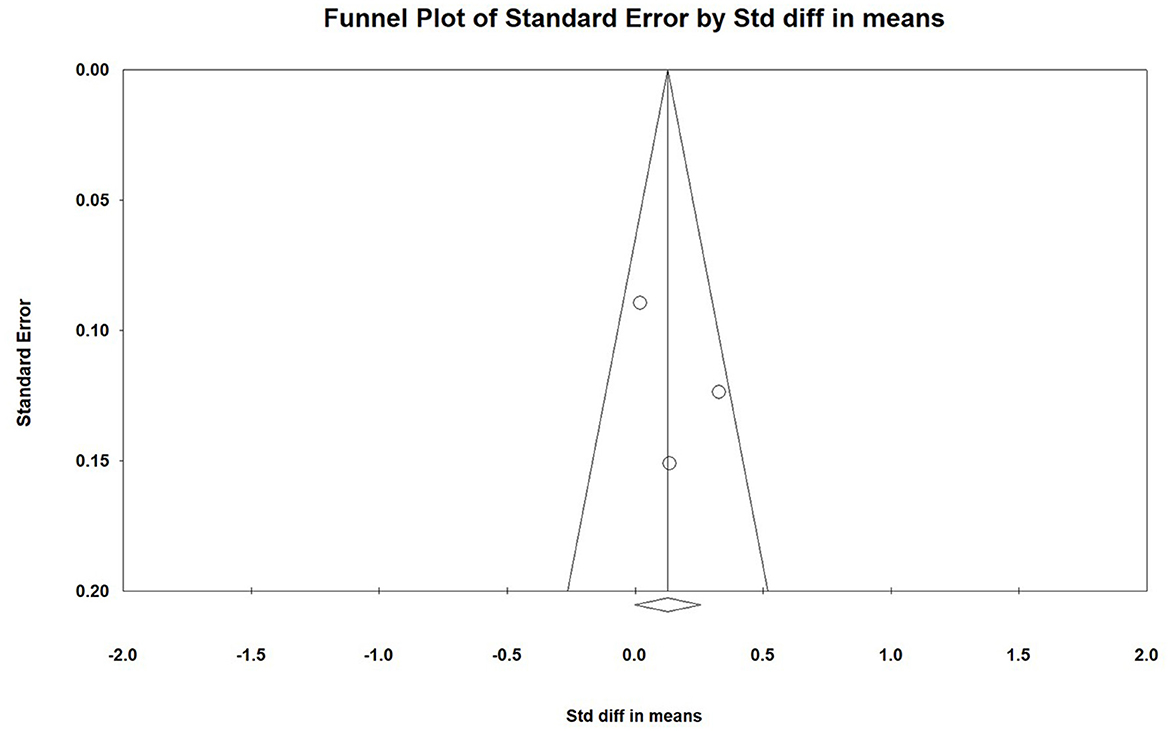
The meta-analysis was conducted using Comprehensive Meta-Analysis software (V3.7). The standardized mean difference (SMD) of OHRQoL with a 95% confidence interval (CI) was reported as estimating pooled effect size. Due to the small number of studies, a “random effect model” was used. Heterogeneity across included studies assessed by the Cochran Q test and I-square index. If the I2 statistic is greater than 50%, heterogeneity may represent Moderate to substantial (27). Publication bias was determined by funnel plot based on Begg's test. In the funnel plot, SMD against standard error was presented. The symmetric funnel plot shows lower biases in results.
Due to the lack of a clear cutoff to determine the effect of OHRQoL on different variables such as diabetes, only the standardized mean difference (SMD) of OHRQoL between the case and control groups was used for meta-analysis.
2.8. Ethics approval
This research was approved by the Research Ethics Committees of Vice-Chancellor in Research Affairs -Medical University of Isfahan (Approval ID: IR.MUI.RESEARCH.REC.1400.421).
3. Results
3.1. Search and study selection
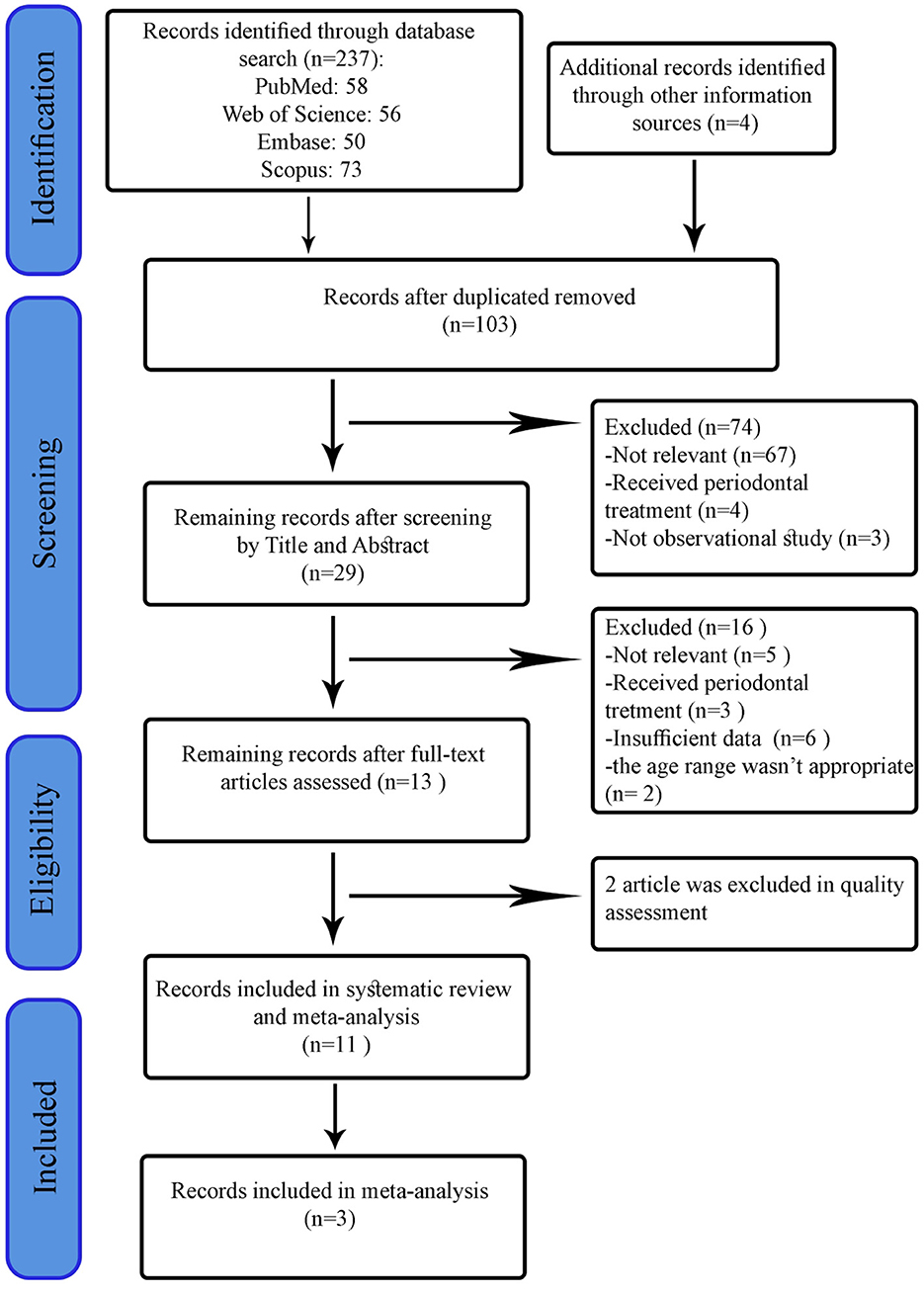
Initially, 237 records were identified from searching in electronic databases and manual search. After removing duplicates, the title and abstract of 103 articles were screened separately by two reviewers. Based on predetermined eligibility criteria, 29 articles were selected for the full-text stage. After scanning the full-text of articles, 16 records were excluded for the following reasons: the outcome wasn't OHRQoL; the age range wasn't appropriate; Insufficient data to investigate the relationship between diabetes and OHRQoL, and periodontal treatments. In addition, two records were excluded during the quality assessment phase (28, 29). Finally, we used eight articles for qualitative review and three articles for quantitative synthesis. The process of study selection flow diagram is shown in Figure 1.
3.2. Study characteristics
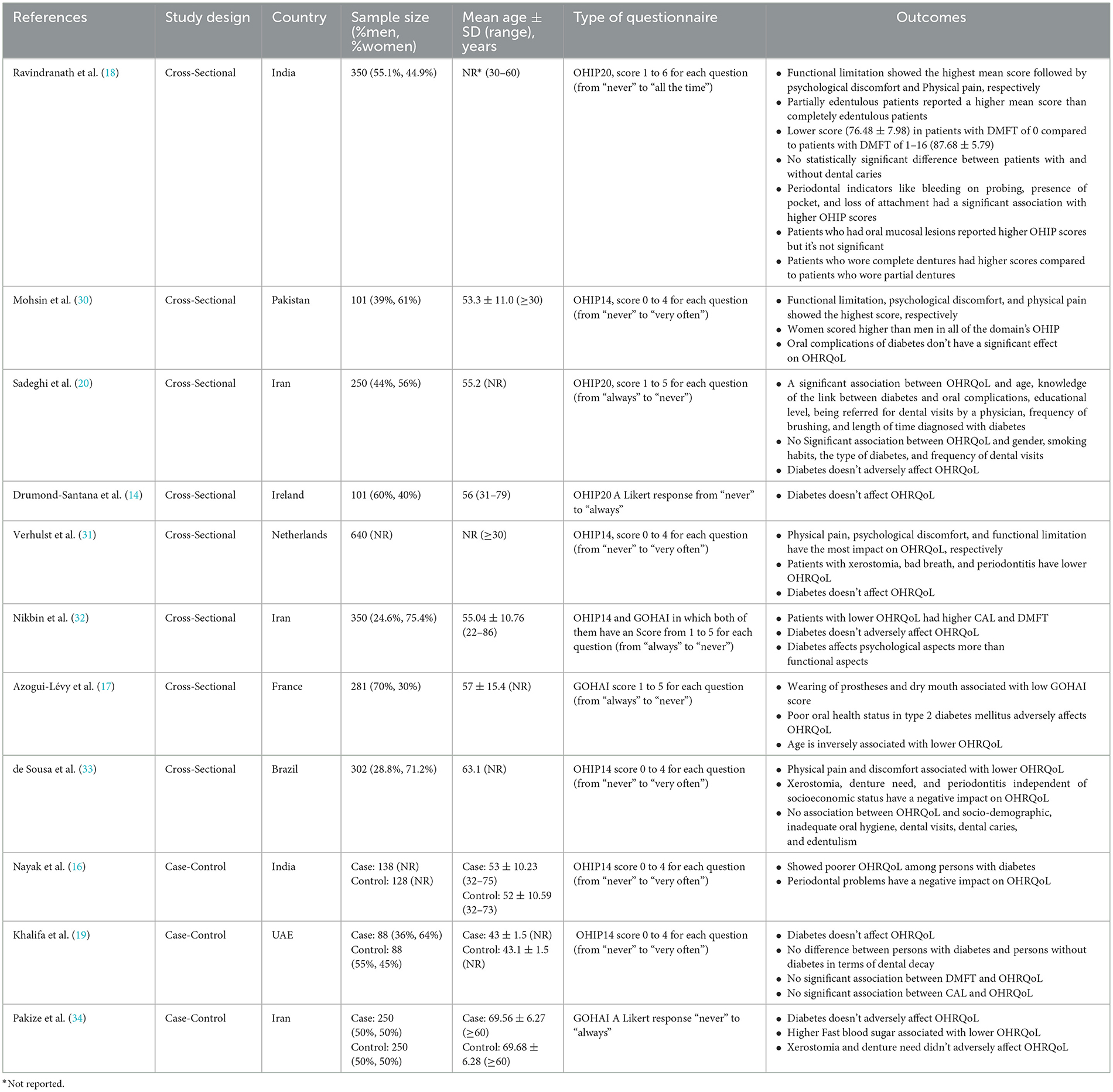
Characteristics of included studies are displayed in Table 1. eight of eleven studies employed a cross-sectional design, and the remaining three were case-control studies. Included studies used OHIP 14 (n = 7), OHIP 20 (n = 3), GOHAI (n = 2), and both the OHIP 14 and GOHAI (n = 1) for measuring the OHRQoL. The sample size varied between included studies, and the age of the diabetic patients ranged from 18 to 86 years old. Three studies included controlled diabetic patients with type 1 and 2 diabetes [62, 66, and 80% of the participants in Azogui-Lévy et al. (17), Sadeghi et al. (20), and Allen et al. (35) studies had type 2 diabetes, respectively], and controlled diabetic patients in other studies had only type 2 diabetes.
3.3. Assessment of methodological quality
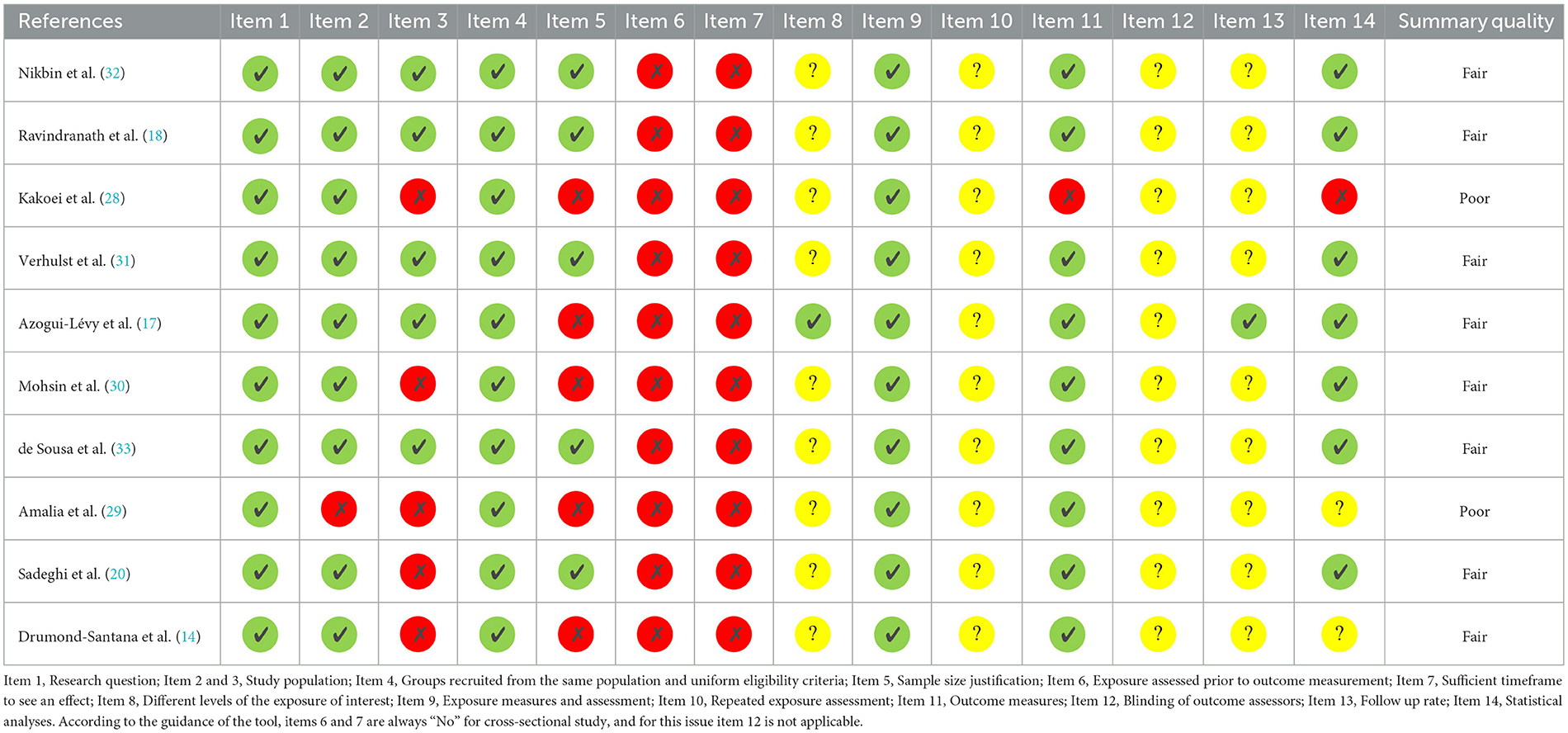
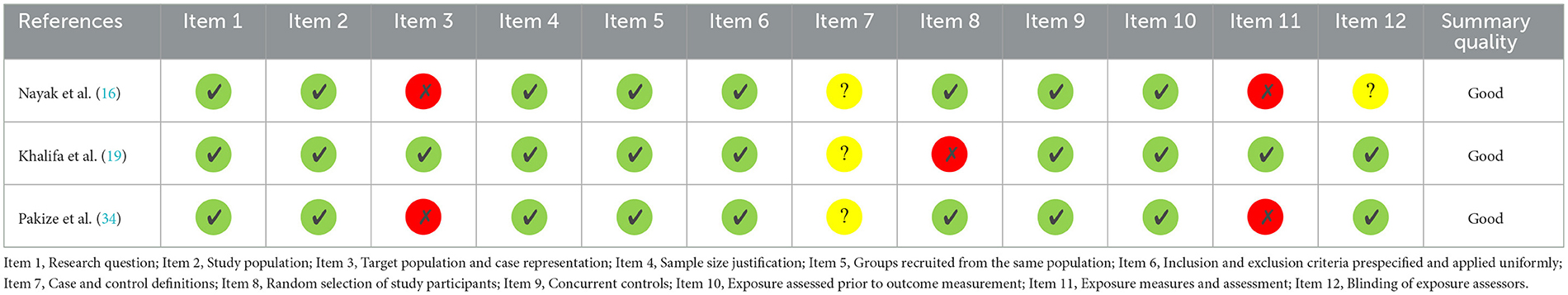
The results of the quality assessment are shown in Tables 2, 3. Based on NIH quality assessment tools, all three case-control studies had a good methodological quality. Except for two studies, the rest of the cross-sectional studies were of fair quality in terms of methodology. The two independent reviewers agreed concerning all items on the scale.
3.4. Impact on OHRQoL and related variables
Table 1 presents detailed information about the effect of diabetes on OHRQoL and its related variables. Included studies have examined various factors affecting OHRQoL in diabetic patients. Two cross-sectional studies investigated the effect of DMFT on OHRQoL in diabetic patients. Most studies have also examined the effects of periodontal indicators caused by diabetes, such as periodontitis and clinical attachment loss (CAL). One study considered the impact of gender on OHRQoL, while another found no association between gender and OHRQoL. In addition, xerostomia was investigated in most included studies as an effective variable on OHRQoL. Five cross-sectional studies that used the OHIP questionnaire examined different domains affecting OHRQoL in which three domains, Physical pain, psychological discomfort, and functional limitation, were more affected than others.
Due to the lack of a clear universal and academic cutoff point to determine the effect of OHRQoL on different variables such as diabetes, the standardized mean difference of OHRQoL between the case and control groups was used for meta-analysis. Therefore, three existing case-control studies were included in the meta-analysis. The pooled SMD score between case and control groups indicates no impact on OHRQoL among diabetic patients (SMD: 0.148; 95% CI: −0.045 to 0.340; P = 0.132; heterogeneity, Cochran Q test = 4.09, P = 0.0129 I2 = 51.16) (Figures 2, 3).
3.5. Publication bias
The funnel plot showed a symmetric distribution of the data in each study (Figure 3). Begg's test detected no significant publication bias too.
4. Discussion
The present study systematically reviewed the evidence on the impact of diabetes mellitus on oral health-related quality of life and Related variables affecting OHRQoL. Our meta-analysis of three case-control studies (16, 19, 34) revealed no statistically significant association between diabetes mellitus and OHRQoL. Also, in 5 cross-sectional studies, no association was observed between diabetes and OHRQoL (20, 30–32, 35), while three cross-sectional studies indicated the effect of diabetes mellitus on OHRQoL (17, 18, 33). This difference between included studies may be due to the consideration of different cutoffs or their different populations. However, according to the results, it seems that diabetes mellitus has no statistically significant association with OHRQoL. One of the possible reasons for the lack of association between OHRQoL and diabetes is that diabetic patients pay more attention to other aspects of personal health. Therefore, they give more importance to promoting their awareness and general health.
Among the included studies, nine studies used the OHIP questionnaire to assess OHRQoL, of which five studies examined each domain of the OHIP questionnaire separately. All five studies reported a high impact of diabetes on three domains of Functional limitation, psychological discomfort, and physical pain than on other domains. The study of Ravindranath et al. (18) and Mohsin et al. (30) considered the Functional limitation to be more effective than the other two domains, while the other three studies considered the domains of psychological discomfort and physical pain to be more effective (31–33). Therefore, we suggest that physicians and dentists pay more attention to these domains. In other words, they should attend to issue such as diet, chewing problems, pain, sore spots, and concerns related to the oral and dental conditions of diabetic patients in their examinations.
The studies included in this research demonstrated that diabetes mellitus reduced OHRQoL in different ways. Ravindranath et al. (18) and Nikbin et al. (32) showed that higher Decayed, Missing, and Filled Teeth index (DMFT) and clinical attachment loss index (CAL) lead to lower OHRQoL in diabetic patients. However, Khalifa et al. (19) suggested that these two affect OHRQoL regardless of participants' diabetic status. Also, Numerous studies have shown that xerostomia, as one of the most common oral complications of diabetes mellitus reduces the oral health-related quality of life of diabetic patients (31, 33, 34). Like xerostomia, several studies have considered the negative impact of periodontal problems in diabetic patients as a factor in reducing their OHRQoL. Bleeding on probing and the pocket presence have been noticed more than other problems (18, 31, 33).
Mohsen et al. (30) suggested that women's oral health-related quality of life scores were more affected by men, while Sadeghi et al. (20) found no association between gender and OHRQoL scores. Also, based on Sadeghi et al. (20) and Allen et al. (35) study, there is no difference between type 1 and type 2 diabetes concerning OHRQoL. In addition, De Sousa et al. (33) showed no association between OHRQoL and socio-demographic features.
Azogui-Lévy et al. showed that age is directly associated with better OHRQoL. The importance of aesthetic demand in younger patients and the greater adaptation of older people to diabetes after years of suffering from it were among the reasons they stated for this association (17).
Like any research, study limitations must be identified to deduce the finding correctly. Participants in most included studies were gathered from diabetic patients who were referred to hospitals or clinics. In other words, most of the studies were hospital-based. Also, the findings were mainly based on the questionnaire results, and patients were not clinically examined. On the other hand, the small number of case-control studies did not allow for performed meta-analyses with a larger population. Hence, we suggest conducting case-control studies in a large-scale, randomized, and community setting. We also recommend that more dependent variables be carefully examined to determine the confounders and the effect of these variables on OHRQoL.
5. Conclusion
Given the finding of this literature, diabetes mellitus has no statistically significant association with oral health-related quality of life. Nevertheless, based on the articles' review, it seems that diabetes can lead to functional limitations as well as physical pain and psychological discomfort. On the other hand, complications of diabetes such as xerostomia and periodontal problems adversely affect wellbeing. Therefore, due to the relationship between some variables related to diabetes and OHRQoL, dentists can play an essential role in the awareness of diabetic patients about these problems and improve their quality of life. In addition, we recommend that visiting a dentist be part of the care protocol for diabetic patients.
Data availability statement
The datasets presented in this article are not readily available because this article is a systematic review and does not have any dataset. Requests to access the datasets should be directed to Zl9uaWxjaGlhbkBkbnQubXVpLmFjLmly.
Author contributions
YM, KA, ST, MT, and FN researched data, designed the study, reviewed, and edited the manuscript. KA and ST screened, evaluated the quality of the studies, and extract a data spreadsheet. YM checked the data as the third reviewer. Statistical analysis was performed by MT, YM, and FN wrote the first draft of the manuscript. FN is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data, and the accuracy of the data analysis. All authors approved the final version of the manuscript.
Funding
This research was supported by Student Research Committee, Isfahan University of Medical Sciences, Isfahan, Iran (Grant No.: 1400365). The supporter of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1112008/full#supplementary-material
Abbreviations
OHRQoL, Oral health-related quality of life; CI, Confidence intervals; IDF, International Diabetes Federation; T2DM, type 2 diabetes mellitus; T1DM, type 1 diabetes mellitus; OHIP, Oral Health Impact Profile; GOHAI, Geriatric Oral Health Assessment Index; SMD, Standardized mean difference; CAL, Clinical attachment loss; DMFT, Decayed, Missing, and Filled Teeth index.
References
1. Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2013) 37:S81–90. doi: 10.2337/dc14-S081
3. Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of diabetes. J Diabetes Res. (2018) 2018:3086167. doi: 10.1155/2018/3086167
4. Afaya RA, Bam V, Azongo TB, Afaya A. Knowledge of chronic complications of diabetes among persons living with type 2 diabetes mellitus in northern Ghana. PLoS ONE. (2020) 15:e0241424. doi: 10.1371/journal.pone.0241424
5. Nordheim E, Geir Jenssen T. Chronic kidney disease in patients with diabetes mellitus. Endocr Connect. (2021) 10:R151–9. doi: 10.1530/EC-21-0097
6. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
7. Rohani B. Oral manifestations in patients with diabetes mellitus. World J Diabetes. (2019) 10:485–9. doi: 10.4239/wjd.v10.i9.485
8. Nascimento GG, Leite FRM, Vestergaard P, Scheutz F, López R. Does diabetes increase the risk of periodontitis? A systematic review and meta-regression analysis of longitudinal prospective studies. Acta Diabetol. (2018) 55:653–67. doi: 10.1007/s00592-018-1120-4
9. Kim E-K, Lee SG, Choi Y-H, Won K-C, Moon JS, Merchant AT, et al. Association between diabetes-related factors and clinical periodontal parameters in type-2 diabetes mellitus. BMC Oral Health. (2013) 13:64. doi: 10.1186/1472-6831-13-64
10. Wan R, Weissman JP, Grundman K, Lang L, Grybowski DJ, Galiano RD. Diabetic wound healing: The impact of diabetes on myofibroblast activity and its potential therapeutic treatments. Wound Repair Regen. (2021) 29:573–81. doi: 10.1111/wrr.12954
11. Patel MH, Kumar J V, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey, 2003-2004. J Am Dent Assoc. (2013) 144:478–85. doi: 10.14219/jada.archive.2013.0149
12. Manfredi M, McCullough MJ, Vescovi P, Al-Kaarawi ZM, Porter SR. Update on diabetes mellitus and related oral diseases. Oral Dis. (2004) 10:187–200. doi: 10.1111/j.1601-0825.2004.01019.x
13. Niklander S, Veas L, Barrera C, Fuentes F, Chiappini G, Marshall M. Risk factors, hyposalivation and impact of xerostomia on oral health-related quality of life. Braz Oral Res. (2017) 31:e14. doi: 10.1590/1807-3107bor-2017.vol31.0014
14. Drumond-Santana T, Costa FO, Zenóbio EG, Soares RV, Santana TD. Impact of periodontal disease on quality of life for dentate diabetics. Cad Saude Publica. (2007) 23:637–44. doi: 10.1590/S0102-311X2007000300022
15. Ferreira MC, Dias-Pereira AC, Branco-de-Almeida LS, Martins CC, Paiva SM. Impact of periodontal disease on quality of life: a systematic review. J Periodontal Res. (2017) 52:651–65. doi: 10.1111/jre.12436
16. Nayak SU, Kamath DG, Pai KK. Periodontal health and its impact on quality of life among type II diabetes mellitus patients. World J Dent. (2017) 8:86–9. doi: 10.5005/jp-journals-10015-1418
17. Azogui-Lévy S, Dray-Spira R, Attal S, Hartemann A, Anagnostou F, Azerad J. Factors associated with oral health-related quality of life in patients with diabetes. Aust Dent J. (2018) 63:163–9. doi: 10.1111/adj.12577
18. Ravindranath N, Raju R. Association of oral health status and oral health-related quality of life among adult patients with type 2 diabetes mellitus: A cross-sectional study. J Indian Assoc Public Heal Dent. (2020) 18:290–5. doi: 10.4103/jiaphd.jiaphd_31_20
19. Khalifa N, Rahman B, Gaintantzopoulou MD, Al-Amad S, Awad MM. Oral health status and oral health-related quality of life among patients with type 2 diabetes mellitus in the United Arab Emirates: a matched case-control study. Health Qual Life Outc. (2020) 18:182. doi: 10.1186/s12955-020-01418-9
20. Sadeghi R, Taleghani F, Farhadi S. Oral health-related quality of life in diabetic patients. J Dent Res Dent Clin Dent Prospects. (2014) 8:230–4. doi: 10.5681/joddd.2014.41
21. John MT. Foundations of oral health-related quality of life. J Oral Rehabil. (2020) 48:355–9. doi: 10.1111/joor.13040
22. Zucoloto ML, Maroco J, Campos JADB. Impact of oral health on health-related quality of life: a cross-sectional study. BMC Oral Health. (2016) 16:55. doi: 10.1186/s12903-016-0211-2
23. Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. (2011) 90:1264–70. doi: 10.1177/0022034511399918
24. Campos LA, Peltomäki T, Marôco J, Campos JADB. Use of oral health impact profile-14 (OHIP-14) in different contexts. What is being measured? Int J Environ Res Public Health. (2021) 18:13412. doi: 10.3390/ijerph182413412
25. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
26. National Heart, Lung and Blood Institute Home Page. (2021). Available online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed July, 2021).
27. Higgins JPT. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
28. Kakoei S, Navabi N, Aghaabbasi S, Hashemipour MA. Oral health-related quality of life in patients with diabetes mellitus type 2 in the year 2012. J Oral Heal Oral Epidemiol. (2016) 5:186–91.
29. Amalia Z, Anggraeni ZK, Adiatman M. Association between oral health status and oral health-related quality of life in diabetes patients. J Int Dent Med Res. (2018) 11:181–6.
30. Mohsin S, Fawwad A, Mustafa N, Shoaib A, Basit A. Impact of type 2 diabetes mellitus on oral health-related quality of life among adults in Karachi, Pakistan - a cross-sectional study. Br J Med Med Res. (2017) 20:1–7. doi: 10.9734/BJMMR/2017/31676
31. Verhulst MJL, Teeuw WJ, Gerdes VEA, Loos BG. Self-reported oral health and quality of life in patients with type 2 diabetes mellitus in primary care: A multi-center cross-sectional study. Diabetes, Metab Syndr Obes Targets Ther. (2019) 12:883–99. doi: 10.2147/DMSO.S207087
32. Nikbin A, Bayani M, Jenabian N, Khafri S, Motallebnejad M. Oral health-related quality of life in diabetic patients: Comparison of the Persian version of Geriatric Oral Health Assessment Index and Oral Health Impact Profile: A descriptive-analytic study. J Diabetes Metab Disord. (2014) 13:1–10. doi: 10.1186/2251-6581-13-32
33. de Sousa RV, Pinho RCM, Vajgel B de CF, Paiva SM de, Cimões R. Evaluation of oral health-related quality of life in individuals with type 2 diabetes mellitus. Brazilian J Oral Sci. (2019) 18:e191431. doi: 10.20396/bjos.v18i0.8655466
34. Pakize F, Mehryari M, Hajimirzamohammad M, Bijani A, Hosseini SR, Motalebnejad M, et al. Evaluation of oral health-related quality of life in elderly people with type ii diabetes mellitus. Iran J Heal Sci. (2020) 8:10–20. doi: 10.18502/jhs.v8i3.4308
Keywords: diabetes mellitus, quality of life, oral health, oral health-related quality of life, systematic review
Citation: Mohseni Homagarani Y, Adlparvar K, Teimuri S, Tarrahi MJ and Nilchian F (2023) The effect of diabetes mellitus on oral health-related quality of life: A systematic review and meta-analysis study. Front. Public Health 11:1112008. doi: 10.3389/fpubh.2023.1112008
Received: 30 November 2022; Accepted: 06 February 2023;
Published: 24 February 2023.
Edited by:
Ryan Moseley, Cardiff University, United KingdomReviewed by:
Norhayati Yusop, Universiti Sains Malaysia, MalaysiaAhmed Makki Abdulrazzaq Al-Qarakhli, Anbar University, Iraq
Copyright © 2023 Mohseni Homagarani, Adlparvar, Teimuri, Tarrahi and Nilchian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Firoozeh Nilchian,  Zl9uaWxjaGlhbkBkbnQubXVpLmFjLmly
Zl9uaWxjaGlhbkBkbnQubXVpLmFjLmly
 Yousef Mohseni Homagarani
Yousef Mohseni Homagarani Kimia Adlparvar1
Kimia Adlparvar1 Mohammad Javad Tarrahi
Mohammad Javad Tarrahi Firoozeh Nilchian
Firoozeh Nilchian