- Special Program for Primary Health Care, Geneva, Switzerland
This article is part of the Research Topic ‘Health Systems Recovery in the Context of COVID-19 and Protracted Conflict’.
Pursuing the objectives of the Declaration of Alma-Ata for Primary Health Care (PHC), the World Health Organization (WHO) and global health partners are supporting national authorities to improve governance to build resilient and integrated health systems, including recovery from public health stressors, through the long-term deployment of WHO country senior health policy advisers under the Universal Health Coverage Partnership (UHC Partnership). For over a decade, the UHC Partnership has progressively reinforced, via a flexible and bottom-up approach, the WHO’s strategic and technical leadership on Universal Health Coverage, with more than 130 health policy advisers deployed in WHO Country and Regional Offices. This workforce has been described as a crucial asset by WHO Regional and Country Offices in the integration of health systems to enhance their resilience, enabling the WHO offices to strengthen their support of PHC and Universal Health Coverage to Ministries of Health and other national authorities as well as global health partners. Health policy advisers aim to build the technical capacities of national authorities, in order to lead health policy cycles and generate political commitment, evidence, and dialogue for policy-making processes, while creating synergies and harmonization between stakeholders. The policy dialogue at the country level has been instrumental in ensuring a whole-of-society and whole-of-government approach, beyond the health sector, through community engagement and multisectoral actions. Relying on the lessons learned during the 2014–2016 Ebola outbreak in West Africa and in fragile, conflict-affected, and vulnerable settings, health policy advisers played a key role during the COVID-19 pandemic to support countries in health systems response and early recovery. They brought together technical resources to contribute to the COVID-19 response and to ensure the continuity of essential health services, through a PHC approach in health emergencies. This policy and practice review, including from the following country experiences: Colombia, Islamic Republic of Iran, Lao PDR, South Sudan, Timor-Leste, and Ukraine, provides operational and inner perspectives on strategic and technical leadership provided by WHO to assist Member States in strengthening PHC and essential public health functions for resilient health systems. It aims to demonstrate and advise lessons and good practices for other countries in strengthening their health systems.
Introduction
During the last decades, discussions and debates on how to strengthen health systems in order to operationalize the right to health have been running, without finding a common understanding of how to deliver accessible life-saving health services for all. Despite the commitments expressed in the Declaration of Alma-Ata for Primary Health Care (1) in 1978, reiterated in Astana in 2018 (2), and in the 2030 Agenda for Sustainable Development, as well as significant pieces of evidence linking Primary Health Care (PHC) to improved health outcomes (3), the WHO recently acknowledged that the implementation of PHC has been limited and diverse across countries due to a lack of a universally accepted definition (3).
In 2020, the Operational Framework for Primary Health Care (4) describes it as “a whole-of-society approach to health that aims to maximize the level and distribution of health and well-being through three key components: primary care and essential public health functions as the core of integrated health services; multisectoral policy and actions; and empowered people and communities” (4). It also refers to primary care as a “process in the health system that supports first-contact, accessible, continued, comprehensive and coordinated patient-focused care” (4). During the last few years, WHO’s Member States have committed through several WHO resolutions (5) to use PHC as the fundamental programmatic engine to progress toward the Sustainable Development target 3.8 for Universal Health Coverage (UHC). UHC means that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship.
The comprehensiveness of PHC ensures that any healthcare need is addressed through the direct provision of services at the primary care level or through referral to any other level of care, depending on the package of services defined for each level of the health system. This conceptual framework is broader than the health service delivery function alone and includes essential public health functions (health protection, health promotion, disease prevention, surveillance and response, and emergency preparedness); multisectoral policies to address the social, economic, and environmental determinants of health; and empowering processes to include individuals and communities in the health-related policy-making process.
However, at the beginning of the 2000s, while the largest vertical programs for health were established, disease-specific ventures were more prevalent than integration through health systems strengthening. At this stage, some countries did not develop any national health policy, strategy, or plan for health, and in many others, when elaborated, they were perceived as unrealistic documents and rarely operationalized (6).
From 2000 to 2019, the UHC service coverage has globally increased from 45 to 67 (7) and life expectancy by more than 6 years (8). In the same period until 2017, the maternal mortality ratio dropped by 38% worldwide (9) and the under-5 mortality rate dropped by 60% since 1990 (10). However, 30% of the world’s population are still not able to access the essential health services they need, and almost 2 billion people are facing catastrophic or impoverishing health expenditure (11). Yet, 90% of these needs could be addressed by the PHC approach by providing promotive, preventive, curative, and rehabilitative services accordingly (12, 13). The world has, in consequences, made some great progress on global health; however, further work is still strongly required to reduce inequalities and achieve health for all by 2030.
To build a consensus on how to strengthen health systems, the World Health Organization (WHO) has strongly advocated for the integration of all health programs and functions in the Primary Health Care approach. During the last decades, global public health interventions and emergencies have also demonstrated the need to develop public health policies through an inclusive and multidisciplinary approach to ensure public confidence (14, 15). In addition, many normative documents have been published to develop the PHC approach to health system strengthening.
In 2007, the WHO’s publication on the framework for health systems (16) through the building blocks lens marked a significant change in the admission of the need for an integrated approach, based on the recognition of strong interdependencies between each health system block (17). One year later, while the 2008 World Health Report was making a strong case for PHC (18), the leaders of G8 nations for the first time exchanged on health systems strengthening. In 2009, the World Health Assembly passed a critical resolution that emphasized the importance of Member States’ commitment to “Primary Health Care, including Health System Strengthening” (19). Subsequently, the World Health Report (20) in 2010 outlined how Member States could adapt their health financing system to ensure that all people have access to health services and do not suffer financial hardship paying for them.
In this context, following the 2011 WHA resolutions on strengthening national policy dialogue to build more robust health policies, strategies, and plans (21), the WHO also created the Universal Health Coverage Partnership to enhance governance through policy dialogue with the aim to build resilient and integrated health systems to make progress toward UHC through a Primary Health Care approach. A decade on, the WHO has deployed a large network of more than 130 health policy advisers to support the provision of technical assistance for PHC and UHC in 115 countries. They have been progressively incorporated into the core workforce of WHO to create one of the largest and most effective technical operational platforms and networks for international cooperation on PHC and UHC.
Health policy advisers support policy dialogue and use strategic and technical leadership to enable governments to strengthen health systems, support the harmonization and alignment of partners on National Health Policy and Strategies, and facilitate the implementation of political declarations, such as the one adopted for the High-Level Meeting on UHC during the UN General Assembly in 2019 (22). Furthermore, since 2020, the UHC Partnership has incorporated gender, equity, and human rights components to support the integration of these approaches into national health policies, strategies, and plans based on health inequality and equity monitoring and analysis dimensions.
In 2023, the UHC Partnership channels 10 sources of funds from Belgium, Canada, the European Union, France, Germany, Ireland, Japan, Luxembourg, the United Kingdom, and the WHO. This is to ensure the implementation of its activities and build a bridge between commitments at the global level and national health system strengthening priorities in 115 countries. Funded activities support the WHO’s work plan across all three levels of the organization (country, regional, and headquarters) based on WHO’s Thirteenth General Program of Work 2019–2023 (GPW13), and not as a stand-alone project. The UHC Partnership supports Member States with flexible funds and agile programming while adapting quickly to evolving contexts and priorities.
During the COVID-19 pandemic, Member States benefited from specific assistance to build and maintain sustainable country preparedness and response capacities, including the continuity of essential health services, the integration of innovations, as well as service delivery adaptations in response to COVID-19. Based on country experiences from Colombia, the Islamic Republic of Iran, Lao PDR, South Sudan, Timor-Leste, and Ukraine, in the context of health systems recovery following COVID-19, this policy and practice review provides operational and in-depth perspectives on strategic and technical leadership provided by WHO to assist Member States in strengthening PHC for resilient and integrated health systems.
Assessment of policy options and implications—Primary health care for resilient and integrated health systems
The COVID-19 pandemic has confirmed that every country is exposed to public health emergencies through direct impact on mortality and morbidity, disruption to health systems functions and essential services, as well as economic and social consequences at the national and global levels. Progress toward UHC and capacities for health security and health determinants are interdependent elements that influence population health. To sustain progress toward UHC, global health security and improved population health and wellbeing require the whole-of-government and social engagement to build the resilience of health systems through health in all policies, considering the complexity of health and the necessity to apply a wide systemic approach (23).
In times of emergencies, health systems are overstretched to respond efficiently to public health threats, while maintaining essential services and functions for the population in dire need. PHC favors integration, coherence, and alignment of health policy and strategies, as well as community engagement, which are critical to ensure that health systems are maintained and continue to deliver services in all contexts. It is also increasingly recognized that facilitating access to PHC is one of the most efficient and convenient ways to increase awareness of menaces to health in the community, by enabling early notification and mitigating and responding to potential threats (24).
Centered on people, PHC brings health systems closer to communities to consider their needs with respect to cultural norms and practices, enhancing trust between health service providers and the population, and also awareness of diseases and care pathways (25, 26). Many essential public health functions, such as surveillance, detection, and notification of diseases, are enhanced through community engagement. Furthermore, compliance with policies cannot be expected as absolute if populations and actors of health systems are not included in policy-making processes, especially in a world fragmented by inequalities (27). Inclusion, solidarity, transparency, and accountability as key components of health system governance are essential for recovering and sustaining progress toward UHC.
The PHC approach to health systems strengthening encompasses these requirements (28–30). The Declaration of Astana is clear about the objectives of PHC: “enhance capacity and infrastructure for primary care (…) prioritizing essential public health functions (…) to meet all people’s health needs across the life course through comprehensive preventive, promotive, curative, rehabilitative services and palliative care” (31). The WHO has translated these resolutions into its 13th General Program of Work (32), recently extended until 2025, and focuses on promoting health, keeping the world safe, and serving the vulnerable.
In 2020, the WHO published the Operational Framework for Primary Health Care to clarify the renewed vision of PHC and support countries in scaling up PHC implementation. PHC is defined as a whole-of-government and whole-of-society approach to health that combines, in addition to its focus on primary care and essential public health functions, a strong emphasis on a multisectoral policy and actions perspective, as well as people’s and communities’ empowerment, including private organizations for and not for profit (Figure 1). The operational framework proposes operational and strategic levers to translate PHC commitments into actions. Furthermore, in 2022, a primary healthcare measurement framework and indicators has been published to support Member States to assess, track, and monitor PHC performance to accelerate progress toward UHC and the health-related SDGs (33).
Health systems must be integrated and oriented toward PHC as the foundation for UHC and health security. The COVID-19 pandemic has kept the doors open to implementing PHC as one of the best ways to ensure progress toward UHC and health security (23).
Similarly, prioritization of preparedness and response capacities, or vertical disease programs, without considering building basic health systems functions, cannot deliver the essential health services required by the people. Health system integration can be considered as horizontal to cover a continuum of health services through a single delivery platform, and as vertical to ensure the coordination between platforms of health service delivery, such as between primary and referral care to hospitals, or between public and private, for and not for profit health facilities. Primary care facilities are keeping the gate and maintaining the path to specialty care and hospital care.
Methodology to analyze the role and the impact of the UHC partnership
Complexity is a significant element of the difficulty to demonstrate and comprehensively understand the results and effects of the intervention of the UHC Partnership (34, 35). Scholars and public health professionals recognized widely that evaluating complex interventions, especially when randomized controlled trials are not feasible, requires to use “non-experimental, mixed methods and process-based approach, appreciation of the different logics of causality, and use of case study research to understand context” (36).
To analyze the role and impact of the UHC Partnership in countries, a formative evaluation was conducted in 2016. (37) It focused on its actions that focus on lessons learned with regard to its role (convener, broker, and technical assistance), strengths (flexibility, bottom-up approach, seed/catalytic funding, and WHO’s Joint Working Team three-level agile network approach), and weaknesses (roster of technical assistance and difficulties finding appropriate candidates).
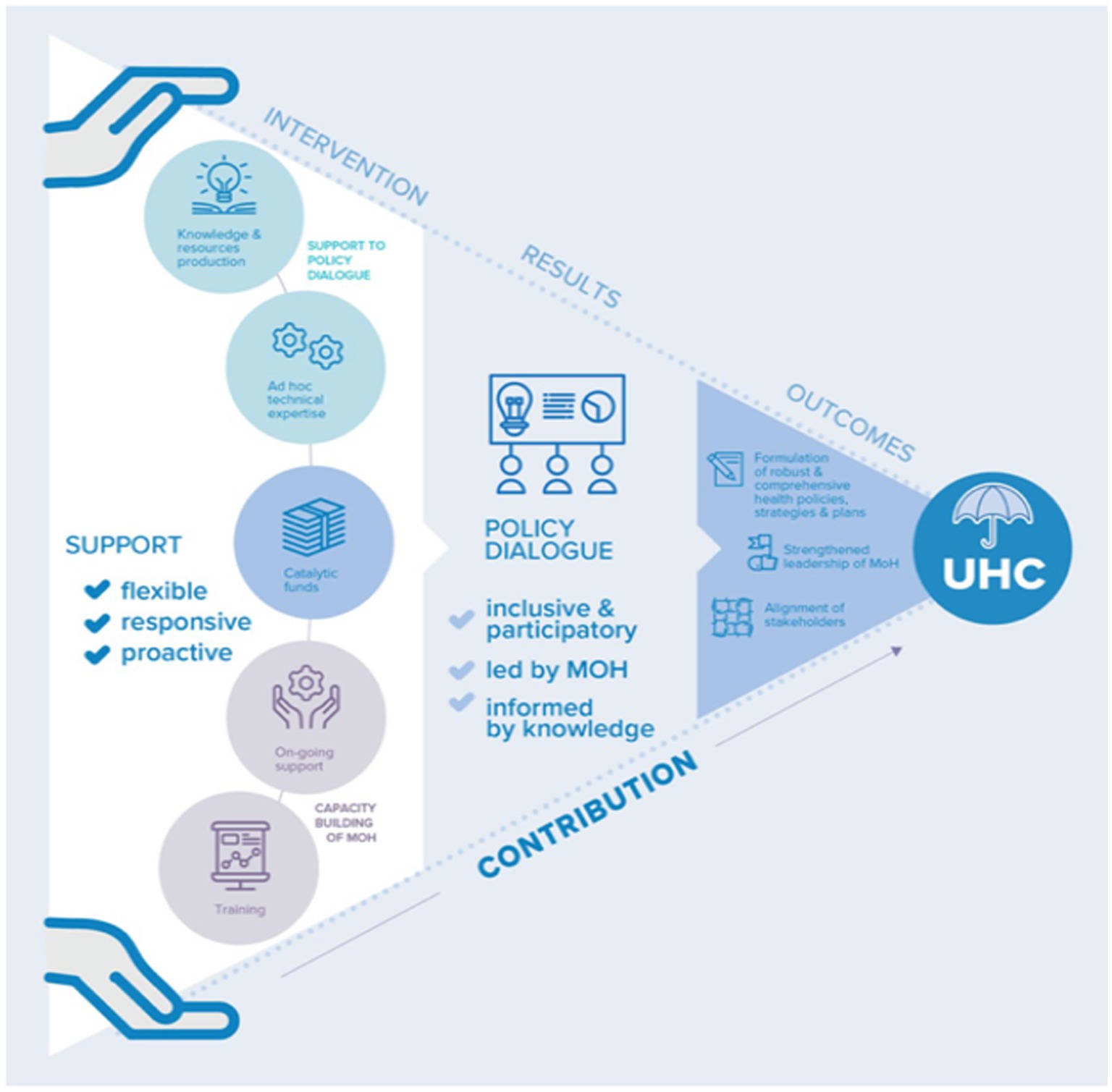
In addition, a research approach was also initiated which led to a protocol for a realist evaluation aiming at analyzing policy dialogue processes in their context to understand what mechanisms have triggered health systems to move toward achieving UHC (38). The results report the theory of the underlying rationale of the WHO through the UHC Partnership (Figure 2) which supports the Ministries of Health (MoH) to lead inclusive, participatory, and evidence-informed policy dialogue (39). The support of the health policy advisers should result in mutual trust to strengthen stakeholders’ collaboration, while the evidence and data provided should bring a shared understanding of needs and policy options. The evaluation also reveals the necessary conditions for successful policy dialogue such as dynamic local stakeholders, promotion of collaboration as a mode of action, involvement and leadership of the Ministry of Health, and synergy of messages and actions of WHO. The African Regional Office also published lessons learned on health policy dialogue led within the continent in the frame of the UHC Partnership (40).
To better understand the effects of the interventions, the implementation of activities and results achieved have been described in a systematic manner (41) since the initiation of the UHC Partnership, through annual reports or diverse strategic and technical analytical deep dives. Furthermore, to improve transparency and mutual accountability, and ensure systematic monitoring of implementation and progress, as well as continuity and stability of the efforts at the national level, the UHC Partnership is established through a high-level governance structure and operational pillars.
The governance structure has two key oversight committees: a Multi-Donor Coordination Committee and a WHO high-level UHC Partnership Steering Committee. The operational pillar is composed of the live-monitoring mechanism; the communication and advocacy strategy; as well as the strategic and operational platform named the three-level Joint Working Team for PHC and UHC. All these mechanisms combined provide various opportunities for WHO and partners to actively engage in a regular dialogue on the provision of support to Member States and results achieved to deliver on their UHC goals.
This policy and practice review is a first attempt to formulate what has been observed over time through these diverse accountability mechanisms, in the frame of a larger contribution analysis (42) that should be implemented in the next phase of the UHC Partnership. Country examples have been selected to reflect the diversity of context where the UHC-P is operating, representing each of the six WHO regions, with a long engagement in four low-income countries (Lao PDR, South Sudan, Timor-Leste, and Ukraine) and a shorter one in two middle-income countries (Colombia and the Islamic Republic of Iran). This diversity of context also includes interventions in fragile and conflict-affected countries (South Sudan and Ukraine).
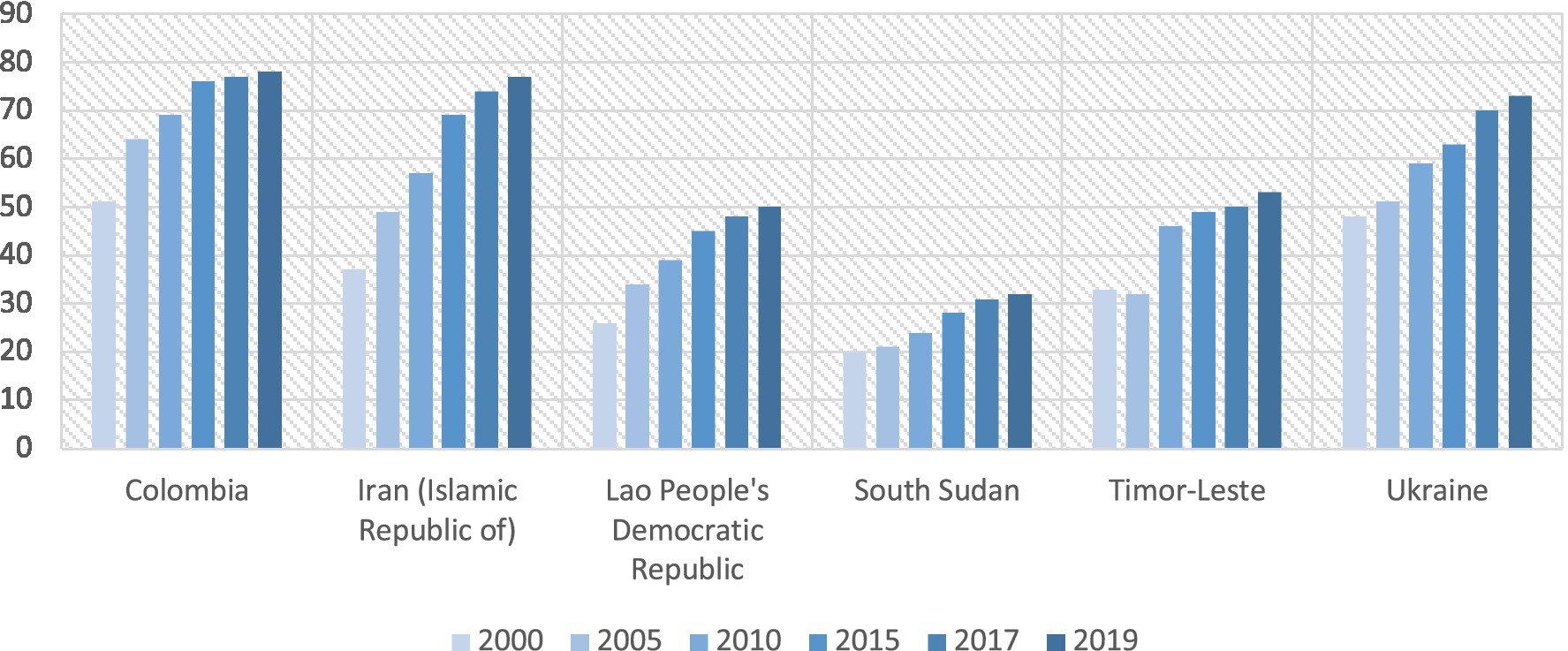
Each case study has been reported in two steps. First, country data for the tracer indicators 3.8.1 and 3.8.2 have been collected to observe the country’s progress toward Universal Health Coverage. These quantitative indicators have been selected because they best reflect the ultimate objective of the UHC Partnership, to increase the coverage of health services and decrease catastrophic health expenditures. Two separate metrics are used to follow this objective, specifically indicator 3.8.1 on the coverage of essential health services and indicator 3.8.2 on catastrophic health spending.
The coverage of essential health services (3.8.1) is defined as the average coverage of essential services based on tracer interventions that include reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases, and service capacity and access, among the general and the most disadvantaged population. The indicator is measured as an index reported on a unitless scale of 0–100, which is computed as the geometric mean of 14 tracer indicators of health service coverage.
The proportion of the population with household expenditures on health >10% of total household expenditure or income (3.8.2) is estimated as the population-weighted average of the country-level share of people with such catastrophic health expenditures (10% threshold) for a reference year. Incidence at the country level for the reference year is estimated using different methods depending upon the availability of information for that country around or at the reference year.
In a second phase, the gray literature produced by the UHC Partnership (annual reports, evaluations, communication and advocacy documents, policy briefs, blog publications, and online presentations) has been reviewed to list qualitative and quantitative information that could support the establishment of a clear theory of change (activities supported, evidence generated, and output and outcome achieved) to explain the contribution of the UHC Partnership to the achievement of the tracer indicators 3.8.1 and 3.8.2.
The general hypothesis, articulated through this article, supposes that the health system guidance supported by the UHC Partnership aims at elaborating public health policies for UHC with a PHC approach, through policy dialogue while supporting the alignment of financial and human resources and coordinating national and international health partners. It is assumed that it can lead to improve health outcomes and outputs as described in the WHO GPW13 and to improve the tracer indicators 3.8.1 and 3.8.2.
Demonstrating the attribution of results from the technical support provided by the WHO to improve the leadership of both WHO and MoH, as well as governance of health systems and essential public health functions is challenging. This is because governance is complex and involves many different actors, spaces, and parameters, in many different contexts, where it is not straightforward to simply articulate how many lives have been saved because of the development of public health policies or the improvement of strategic frameworks for the health sector in a country.
If quantitative studies demonstrated a positive association between better governance and better health outcome through statistical analysis (43, 44), policy studies are not yet able to provide a reasonable and comprehensive theory that can explain with causality relations the different mechanisms leading to better health outcomes through governance. As the WHO and the Alliance for Health Policy and System Research stated in 2013: “despite abundant evidence of the efficacy of affordable, life-saving interventions, there is little understanding of how to deliver those interventions effectively in diverse settings and within the wide range of existing health systems” (45).
This policy and practice paper seeks to contribute to a plausible understanding of how to strengthen the health system by developing, negotiating, implementing, monitoring, and evaluating robust and integrated national health policies oriented toward UHC. It will also determine if the available evidence is sufficient, and if further investigations would be required, to establish strong theories of change in each country to explain the contribution of the UHC Partnership to achieve Universal Health Coverage.
Results
Acting on lessons learned during the 2014–2016 Ebola Outbreaks in West Africa and from fragile, conflict-affected, and vulnerable settings (FCV), health policy advisers have been critical during the COVID-19 pandemic to support health systems’ early recovery, to ensure the continuity of essential health services, and to strengthen PHC for health security, including surveillance and treatment of diseases and preventing routine local outbreaks from becoming larger disruptive emergencies. Due to the flexibility of the planification process, they have been able to adapt their support to the new context of the response to the pandemic and its socioeconomic consequences. Several country experiences have been selected among the 115 countries supported in 2022. They are introduced below to describe how increased PHC can support the resilience of health systems (Table 1).
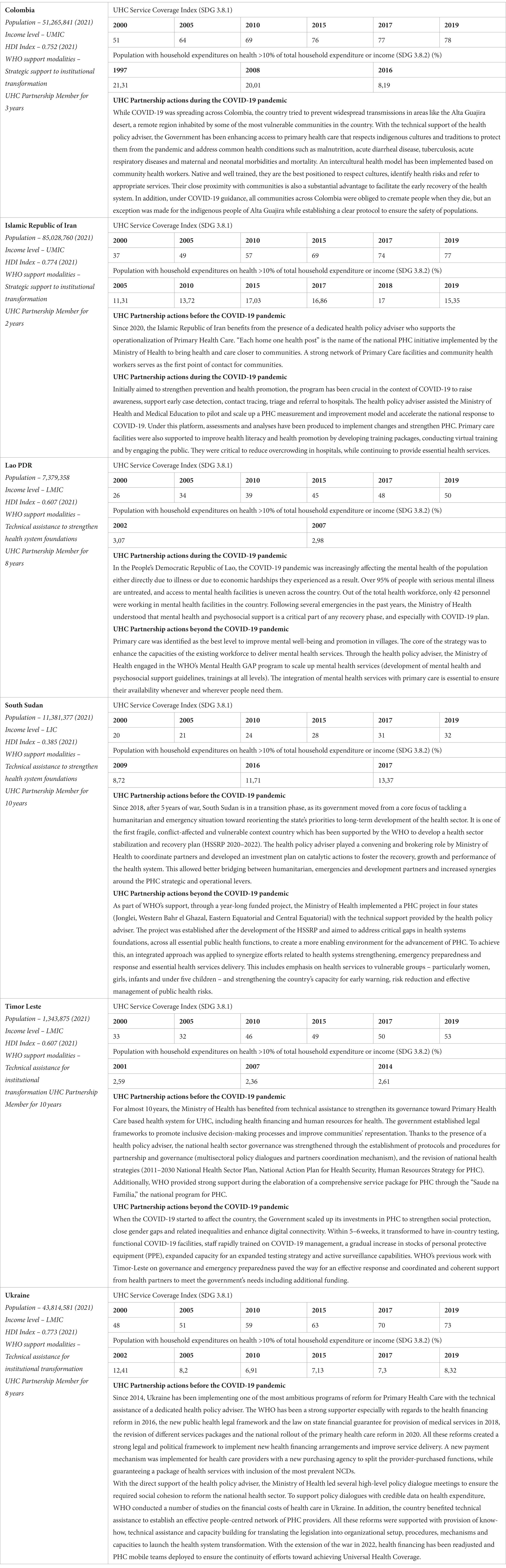
Table 1. Country examples of technical assistance for resilient and integrated health systems (46–48).
Actionable recommendations—Strategic and technical support to move toward UHC and health security
The WHO GPW13 supports a differentiated approach based on capacity and vulnerability to strengthen the integrated health system approach, which defines four different kinds of modalities for WHO support to Member States (49).
1. Policy dialogue to develop health systems in future for the more mature health system.
2. Strategic support to build high-performing systems in advanced health systems.
3. Technical assistance to build national institutions in more fragile health systems.
4. Service delivery to fill critical gaps in emergencies, when national and regional capacities are not able to maintain essential health services.
The UHC Partnership de facto contributed to developing this strategy, operating in countries for the second and third modalities, while always advocating for bottom-up, flexible, catalytic, and long-term support to Member States and implementing a new model of transparency and accountability (consistent and regular annual reporting, communication strategy, live-monitoring meetings, multi-donor, and internal three levels coordination mechanisms).
This strategy quickly brought interesting results in the formulation of public health laws, national strategies, road maps, and national compacts for UHC. Endorsed and acknowledged by the WHO senior management and partners, these results led to constitute a positive environment for the UHC Partnership, which grew from 30 countries to 115 between 2017 and 2020. The UHC Partnership played a key role in highlighting health system strengthening as a fundamental technical priority for WHO and other global health actors. It continues to remain an organizational priority (50), while its strategic approach, principles, and results are recognized by all WHO departments as well as financial and technical partners (51).
The first and most fundamental added value of the UHC Partnership is the long-term deployment of health policy advisers in WHO country offices. Health policy advisers are present in some countries for more than 10 years, and their positions are progressively integrated into the core workforce of the organization. They support the leadership of Ministries of Health in health policy-making processes for essential primary healthcare services and functions, according to WHO health-related guidelines, while convening national and international health stakeholders to build consensus around national health policies and orient human, financial, and technical resources to implement them.
Health policy advisers are senior generalist public health officers recruited to provide leadership and managerial support to country offices, as well as technical and policy advice to Ministries of Health, in the area of public health and health system strengthening, ensuring that the activities in these areas are carried out efficiently and effectively. They constitute the technical country reference for many technical areas and many partners with regard to health system strengthening. They are, for instance, involved in the development of PHC investment plans with the European Investment Bank, as primary providers of evidence and to coordinate technical discussions with National Authorities and partners.
In times of emergency, health policy advisers bring together all technical resources to ensure the continuity of essential health services, strengthen PHC for health security, including surveillance and treatment of diseases, and prevent routine local outbreaks from becoming larger disruptive emergencies. National health security plans can only be integrated into national health strategies to ensure that those specific functions to prepare, prevent, detect, and respond to disease outbreaks and other health emergencies are integrated based on basic health system functions and not separately.
Health policy advisers support the generation of evidence (34), for instance, the institutionalization of national accounts for health financing and workforce or the mapping of available resources and priority actions to increase preparedness capacities. They mobilize policymakers, civil society organizations, and international partners through evidence-based policy dialogues in order to reinforce strategic frameworks and increase resilience and coverage with essential health services, financial protection, and equity. Health policy advisers also encourage and support specific dialogues between Ministries, such as with the Ministry of finance to ensure the coherence and sustainability of the health budget according to national objectives, and to improve public financial management for health.
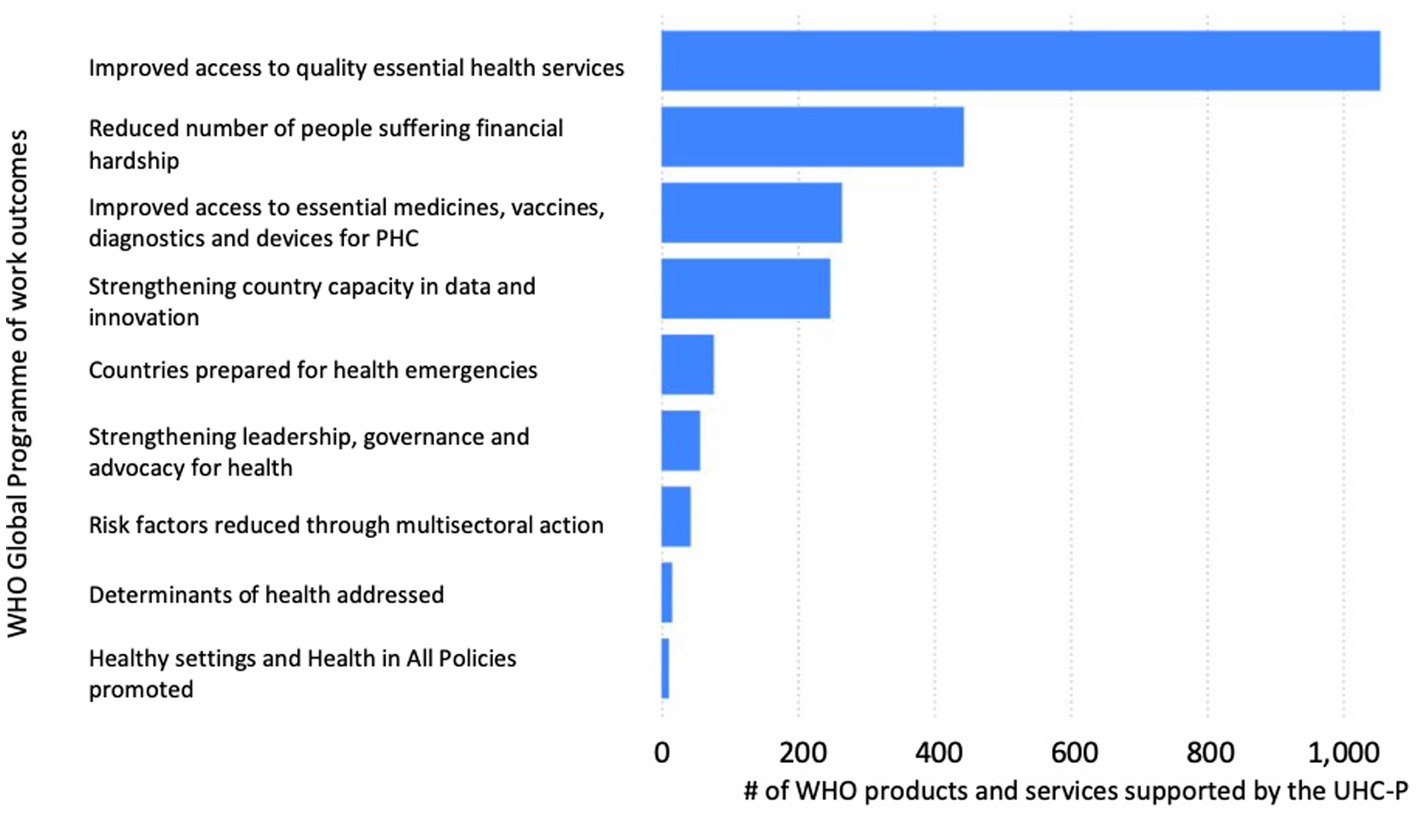
Policy dialogue between the Ministry of Health and other health stakeholders can lead to rationalizing the policy-making process with debates and decisions based on accurate representations of reality (52) and in the respect of international guidelines to strengthen Primary Health Care. This policy-making process can enable the alignment of health system objectives and resources to the needs of the population in order to make and sustain progress toward UHC and health security while enhancing social participation (27). Over the last decade, in many countries, road map, national compact, and legal frameworks for UHC and health security have been developed due to the support provided by the health policy advisers, according to the number of products and services supported by the UHC Partnership (Figure 3).
In 2021, a survey has been conducted among health policy advisers (n = 130) to understand their contribution to the COVID-19 response. Roughly 98% of respondents stated being in almost daily contact with their counterparts at the Ministry of Health. The survey indicated that, on average, respondents had to allocate 50% (range: 3–90%) of their full-time equivalent to support COVID-19-related response activities, albeit the significant amount of work planned under the frame of the UHC Partnership. In addition, due to the UHC Partnership’s flexibility, 90% of respondents were involved in and reinforced the in-country incident management support teams in response to COVID-19. Many of them (56%) even took up a specific position within the incident management support teams, either as an Incident Manager or as a lead or focal point for one of the components of the country’s strategic preparedness and response plan, particularly the pillar 9 on the maintenance of essential health services (53).
Through this network, the WHO has been able to extend its operational arm to bring coherent technical expertise to the Member States from the three levels and experiment with the transformation of the organization. Health policy advisers have enabled WHO country offices to strengthen technical support to Ministries of Health, other National Authorities, as well as Global Health partners by building technical capacities to lead health policy cycles and generate political commitment while creating synergies and harmonization between stakeholders and funding streams. Health policies can then be translated into processes, functions, and services to operationalize UHC, ensure Health Security, and serve population needs. Health policy advisers tend to reinforce all essential public health functions to ensure the minimum requirements to operationalize the right to health, one of the first responsibilities of Member States under the Universal Declaration of Human Rights and the constitution of the WHO.
Health policy advisers are described as crucial assets by WHO Regional and Country Offices in the integration of health systems to enhance their resilience through fostering coherence between essential public health functions and health outputs, always considering the social, economic, and political environment. Similarly, they are designated by the vertical program experts as key players to highlight the importance of integration of programs and provide related support, to move forward the UHC and SDG agenda in countries. The flexibility to adapt their terms of reference to each context and their continuous and long-term presence allow them to monitor policy processes, support technical analysis and participate in policy monitoring and evaluation processes, and use every opportunity to improve health governance. With their support, national authorities, WHO countries, and regional offices are defining actions to be implemented in order to welcome innovations and design theories of change fit for the context.
Discussion
It is now increasingly clear for scholars that political economy is fundamental to understanding the appropriate ways for the implementation of UHC, health security, or essential public health functions as a political exercise (54), but also that “the political routes to UHC are diverse” (55). The WHO also acknowledged that health is primarily a political choice (56) and that a social contract for UHC and health security (27) is needed to ensure its implementation. Experiences from the UHC Partnership tend to confirm these hypotheses, demonstrating how this social contract can be renewed or built through evidence-informed policy dialogue mechanisms including all voices of the health system (57). In Timor-Leste, for instance, the institutionalization of the National Health Sector Coordination Committee leads to open a permanent health forum to oversee and discuss health policies and the implementation of projects and programs guided by one National Health Strategic Plan for all partners and stakeholders.
For a decade, health policy advisers funded by the UHC Partnership played the significant role of convener and broker to support key decision-makers in countries to develop UHC in their social, economic, and health policies for essential public health functions and align stakeholders and resources behind it. The work of the UHC Partnership around governance aims to integrate each essential public health function within its political environment. As demonstrated through multiple accountability mechanisms, supported policy dialogue in many countries has been leading to put UHC and health security on the political agenda and to develop integrated systemic and programmatic policies through the PHC approach (39, 40).
Due to the role of health policy advisers, the WHO is implementing activities that illustrate how the policy-making process for Primary Health Care can be supported in the country. These activities aimed to influence contextual factors (governance, financial and delivery arrangements, institutions, interests, ideas, and external factors) that are shaping health policies (58). The example of Ukraine, for instance, illustrates how the technical assistance contributed to a major reorganization of the health system and especially with regard to the financial and delivery arrangements through the establishment of new payment mechanisms with a National Health Purchasing Agency and a State Guaranteed Benefit Package for Primary Health Care.
John Kingdon’s concept of the window of opportunity (59) could be used to reflect and analyze the approach of the WHO. This classical policy-making model theorizes the setting of public policy agenda, as the intersection of three specific streams related to problem, policy, and politics. This intersection would open a window of opportunity for political decision-making and key reforms. The approach of the WHO to strengthen health systems could be described similarly.
While advocating for a PHC approach to reach UHC and health security, the WHO, through health policy advisers, makes positive propositions of concrete alternative policy and mobilizes policymakers to engage in reforms. Opening windows of opportunity for policy change based on renewed or innovative commitments, the WHO works on fundamental contextual factors for the health policy-making process to ensure that global or country-based strategic frameworks are in place to finally promote health, serve the vulnerable, and keep the world safe. In this perspective, the establishment of the Health Sector Stabilization and Recovery Plan in South Sudan aimed, for instance, to give a common framework to national authorities, humanitarian, and development actors in supporting the health system to move from an emergency situation to long-term development of the health sector.
The flexibility and the long-term presence of health policy advisers are critical to ensure that technical capacities are available when a window of opportunity for the policy-making process is opening, therefore, enhancing the presence and the operational capacities of the WHO. This was especially the case during the COVID-19 pandemic, where health policy advisers were immediately available to provide support to national authorities. Over the 10 years, the WHO has been able to create and sustain one of the largest and most effective platforms for international cooperation on Primary Health Care for UHC and health security. In 115 countries, the WHO has demonstrated what can be achieved through the reinforcement of strategic and technical leadership for health system strengthening and resilience attributable to a PHC-integrated approach, including more recently in the context of a pandemic and health emergencies.
In 2021, the WHO was the subject of the result-oriented monitoring (ROM) review by the European Commission. The role of health policy advisers has been especially distinguished to strengthen WHO support to Member States and deliver high-quality outputs in developing, implementing, and/or strengthening policies and actions of public institutions for health. The need for long-term partnership and financing support for the health reform process is also acknowledged, and the report finally recommends ensuring the sustainability of the intervention through the implementation, monitoring, and evaluation of health policies built during the first phases. The COVID-19 pandemic has nevertheless demonstrated that efforts to strengthen health systems are still mostly fragmented and do not ensure adequate commitment to or resourcing of essential public health functions to enable resilience, safeguard health, and insulate essential health service delivery.
However, as noticed in the 2019 UHC global monitoring report (60), all countries benefiting from dedicated technical assistance, through health policy advisers for health system strengthening from the WHO, have seen an increase in their UHC index during their involvement in the UHC Partnership prior to the COVID-19 pandemic. This progress is the result of the global movement for UHC and can be attributed to the National Authorities with the support of international and national health partners, including the contribution of WHO’s support on policy and strategic aspects for PHC and UHC.
This policy and practice review seeks to trace the first steps of longer research to understand the contribution of the UHC Partnership to the achievement of the Sustainable Development Goal target 3.8 for Universal Health Coverage. Available data, through the diverse accountability mechanisms of the UHC Partnership, have been adequate to demonstrate the contribution of the UHC Partnership to the institutionalization of health policy and strategies for PHC and UHC. The positioning of health policy advisers to provide direct in-country strategic and technical support to Members States, based on their needs, priorities, and strategies, is clearly a key actionable recommendation that needs to be duplicated and intensified to support the achievement of Universal Health Coverage.
However, these data are insufficient to establish a clear linkage between the activities supported by the UHC Partnership and the quantitative indicators 3.8.1 and 3.8.2. To establish stronger causality relations and introduce more reflexivity, a meta-narrative review (61) and deeper country case studies (35) could support a contribution analysis (62) during the next phase of the UHC Partnership. Moreover, the young and promising field of social epistemology demonstrates how political systems are shaping the distribution of population health (63). In an attempt to bridge political sociology and epidemiology (64), this discipline could provide relevant concepts and theories to understand the impact of the UHC Partnership on the social organization of power for health, and especially on health inequities, by supporting policy dialogue and including communities and minorities in policy-making processes.
Conclusion
For more than 10 years, the UHC Partnership has been supporting the establishment of health policies and strategies to elaborate solid health systems foundations for primary care and essential public health functions. As some countries still suffer severe foundational gaps, additional and complementary technical expertise is required to continue the development of health policies and operationalize UHC frameworks and National Actions Plan for Health Security. In addition, aid coordination, domestic resources mobilization, and improved public financial management can orient adequate assets to initiate financial protection services, the supply chain of essential health products, and the development of basic infrastructure for health.
The 2021 UHC global monitoring report (65) revealed that, prior to the pandemic, improvements in service coverage were driven by massive investments to tackle communicable diseases. While much work remains to be done, especially with regard to financial protection (Figure 4), we need to recognize the progress achieved by many countries in improving their UHC service coverage index toward very ambitious targets (Figure 5). On the other hand, the percentage of the total population with households’ expenditures on health continues to be excessive and strong barriers remained, limiting access to healthcare for all, such as poor infrastructure without basic amenities, high level of out-of-pocket payments, shortages of health workers, or the unavailability of good quality pharmaceutical products.
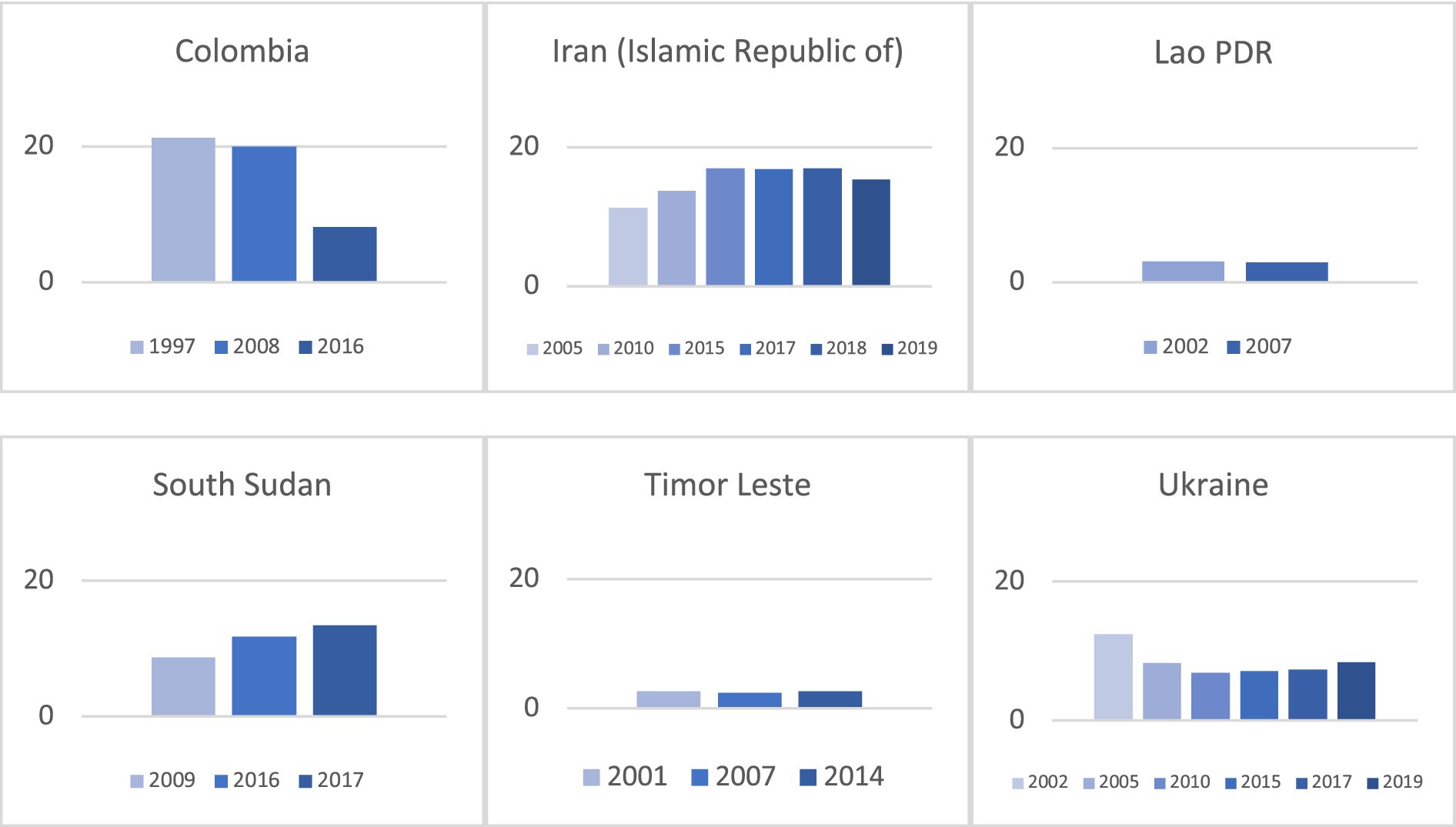
Figure 4. Evolution of the percentage of the total population with household expenditures on health >10% of total household expenditure or income (SDG 3.8.2).
Countries are in need to sustain the acceleration of their journey to UHC and health security. Such effort can benefit from the experiences and lessons learned from countries supported by health policy advisers and can be readily applied when governments implement their recovery plans. Furthermore, the COVID-19 experience has been a trigger for politicians and the public, in general, to further realize and understand the inexplicable linkages among health, socioeconomic development, and whole-of-society constraints.
Public health agencies, and particularly the WHO as a lead health organization, have an important role and responsibilities combined with development banks and multisectoral partners in reinforcing strategic and technical leadership for primary healthcare services and essential public health functions, especially in countries that still suffer from foundational gaps in terms of infrastructures, basic commodities, health financing, or health workforce, for instance. This includes institutionalizing mechanisms for the integration of efforts in health systems strengthening and health security as well as for multisectoral and multi-actor involvement with political commitment and resources for sustainability.
Following the 75th World Health Assembly, the WHO committed to increasing its budget for intensified PHC support to Member States and called for a radical reorientation of health systems toward PHC (66). This will only be possible if all health actors and organizations engage, align, and accelerate the movement to increase strategic and technical leadership, to strengthen health systems, and to make UHC and health security a reality for all.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
This policy and practice review of the Universal Health Coverage Partnership was prepared for the special edition of Frontiers in Public Health. The authors would like to express their gratitude to donors and partners for a very productive and trustful collaboration during the last 10 years. The Universal Health Coverage Partnership is supported and funded by Belgium, Canada, the European Union, France, Germany, Ireland, Japan, Luxembourg, the United Kingdom, and the World Health Organization.
Conflict of interest
The authors are working in the Special Program on PHC of the World Health Organization, which hosts the Universal Health Coverage Partnership. The publishing costs are funded by the World Health Organization. The authors are staff members of the World Health Organization. The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policies, or views of the World Health Organization.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Declaration of Alma-Ata. International conference on primary health care. Alma-Ata, USSR, (1978) 6–12.
2. Declaration of Astana. Global conference on primary health care. Astana, Kazakhstan, (2018) 25–26.
3. WHO. Building the economic case for primary health care, a scoping review, Technical series on primary health care. Geneva: World Health Organization (2018).
4. Operational framework for primary health care: Transforming vision into action. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF) (2020).
5. Declaration of Astana, The accompanying WHA resolution 72/2, the 2019 global monitoring report on UHC, and the United Nations general assembly high-level meeting on UHC.
6. WHO. The world health report 2000, Health systems: improving performance, vol. 2000. Geneva: World Health Organization.
7. WHO. UHC Factsheet. (2022) Available at: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
8. The Global Health Observatory. Life expectancy fact sheet. (2023) Available at: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-life-expectancy-and-healthy-life-expectancy
9. Maternal mortality factsheet. WHO. (2023) Available at https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
10. Child mortality (under 5 years) factsheet. WHO. (2022) Available at: https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-under-5-mortality-in-2020
11. UHC Factsheet, WHO. (2022) Available at: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
12. The Lancet. The Astana declaration: the future of primary health care? Lancet. (2018) 392:1369. doi: 10.1016/S0140-6736(18)32478-4
13. Jamison, DT, Gelband, H, Horton, S, Jha, P, Laxminarayan, R, Mock, CN, et al. eds. Disease control priorities: improving health and reducing poverty. In: Disease control priorities, vol. 9. 3rd ed. Washington, DC: World Bank (2018)
14. Paul, E, Brown, GW, Kalk, A, Van Damme, W, Ridde, V, and Sturmberg, J. “When my information changes, I alter my conclusions.” what can we learn from the failures to adaptively respond to the SARS-CoV-2 pandemic and the under preparedness of health systems to manage COVID-19? Int J Health Policy Manag. (2020) 11:1241–5. doi: 10.34172/ijhpm.2020.240
15. Sagan, A, Webb, E, Rajan, D, Karanikolos, M, and Greer, S. Health system resilience during the pandemic: it's mostly about governance. Eurohealth. (2021) 27
16. WHO. Everybody’s business, strengthening health systems to improve health outcomes. Geneva: World Health Organization (2007) The building blocks are: Governance, financing, medical products and equipment, human resources, information and service delivery.
17. Hafner, T, and Shiffman, J. The emergence of global attention to health systems strengthening. Health Policy Plan. (2013) 28:41–50. doi: 10.1093/heapol/czs023
18. WHO. The world health report 2008, primary health care now more than ever. Geneva: World Health Organization (2008).
20. WHO. The world health report 2010, health systems financing: the path to universal coverage. Geneva: World Health Organization (2010).
22. UNGA 74th. Political declaration of the high-level meeting on universal health coverage, RES/74/2, New York, (2019).
23. WHO. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper. Geneva: World Health Organization (2021).
25. WHO. People-centred and integrated health services: an overview of the evidence. Geneva: World Health Organization (2015).
26. WHO. WHO community engagement framework for quality, people-centred and resilient health services. Geneva: World Health Organization (2017).
27. WHO. Voice, agency, empowerment - handbook on social participation for universal health coverage. Geneva: World Health Organization (2021).
29. WHO, UNICEF. A vision for primary health care in the 21st century: Towards universal health coverage and the sustainable development goals. Geneva: World Health Organization (2018).
30. Kruk, ME, Porignon, D, Rockers, PC, and Van Lerberghe, W. The contribution of primary care to health and health systems in low- and middle-income countries: a critical review of major primary care initiatives. Soc Sci Med. (2010) 70:904–11. doi: 10.1016/j.socscimed.2009.11.025
33. WHO and UNICEF. Primary health care measurement framework and indicators: Monitoring health systems through a primary health care lens. Geneva: World Health Organization (2022).
34. Bosch-Capblanch, X, Lavis, JN, Lewin, S, Atun, R, Røttingen, J-A, Dröschel, D, et al. Guidance for evidence-informed policies about health systems: rationale for and challenges of guidance development. PLoS Med. (2012) 9:e1001185. doi: 10.1371/journal.pmed.1001185
35. Paparini, S, Papoutsi, C, Murdoch, J, Green, J, Petticrew, M, Greenhalgh, T, et al. Evaluating complex interventions in context: systematic, meta-narrative review of case study approaches. BMC Med Res Methodol. (2021) 21:1–22. doi: 10.1186/s12874-021-01418-3
36. Lewin, S, Bosch-Capblanch, X, Oliver, S, Akl, EA, Vist, GE, Lavis, JN, et al. Guidance for evidence-informed policies about health systems: assessing how much confidence to place in the research evidence. PLoS Med. (2012) 9:e1001187. doi: 10.1371/journal.pmed.1001187
37. Formative evaluation of the EU-Luxembourg-WHO. Universal health coverage partnership (UHC Partnership) 2011–2016. Amsterdam: Royal Tropical Institute (2016).
38. Robert, E, Ridde, V, Rajan, D, Sam, O, Dravé, M, and Porignon, D. Realist evaluation of the role of the universal health coverage partnership in strengthening policy dialogue for health planning and financing: a protocol. BMJ Open. (2019) 9:e022345. doi: 10.1136/bmjopen-2018-022345
39. Robert, E, Zongo, S, Rajan, D, and Ridde, V. Contributing to collaborative health governance in Africa: a realist evaluation of the universal health coverage partnership. BMC Health Serv Res. (2022) 22:753. doi: 10.1186/s12913-022-08120-0
40. Nabyonga-Orem, J, Dovlo, D, Kwamie, A, Nadege, A, Guangya, W, and Kirigia, JM. Policy dialogue to improve health outcomes in low income countries: what are the issues and way forward? BMC Health Serv Res. (2016) 16:217. doi: 10.1186/s12913-016-1450-2
41. Skivington, K, Matthews, L, Simpson, SA, Craig, P, Baird, J, Blazeby, JM, et al. Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. Health Technol Assess. (2021) 25:1–132. doi: 10.3310/hta25570
42. Mayne, J. Revisiting contribution analysis. Can J Program Eval. (2019) 34:171–91. doi: 10.3138/cjpe.68004
43. Ciccone, D, Vian, T, Maurer, L, and Bradley, EH. Linking governance mechanisms to health outcomes: a review of the literature in low- and middle-income countries. Soc Sci Med. (2014) 117:86–95. doi: 10.1016/j.socscimed.2014.07.010
44. Acemoglu, D, Naidu, S, Restrepo, P, and Robinson, J. Democracy does cause growth. J Polit Econ. (2019) 127:47–100. doi: 10.1086/700936
45. Peters, DH, Tran, NT, and Adam, T. Implementation research in health: a practical guide. Geneva: World Health Organization and the Alliance for Health Policy and System Research (2013).
46. Population and income level are extracted from the World Bank database. Available at: https://data.worldbank.org/
47. Human Development Index data are extracted from the PNUD database. Available at: https://hdr.undp.org/data-center/human-development-index#/indicies/HDI
48. Health data are extracted from the WHO global health observatory. Available at: https://www.who.int/data/gho/data/indicators
51. European Commission-INTPA. Brussels: Results-oriented monitoring review of the UHC Partnership (2021).
52. Cookson, R. Evidence-based policy making in health care: what it is and what it isn't. J Health Serv Res Policy. (2005) 10:118–21. doi: 10.1258/1355819053559083
53. WHO. COVID-19 strategic preparedness and response plan. Geneva: World Health Organization (2021).
54. Krieger, N. Epidemiology and the People’s health: theory and context. Oxford: Oxford University Press (2011).
55. Rizvi SSDouglas, R, Williams, OD, and Hill, PS. The political economy of universal health coverage: a systematic narrative review. Health Policy Plan. (2020) 35:364–72. doi: 10.1093/heapol/czz171,
56. Kirton, J, and Kickbusch, I. Health: A political choice. Delivering universal health coverage 2030, vol. 2. London: GT Media Group (2019).
57. Schmets, G, Rajan, D, and Kadandale, S. Strategizing National Health in the 21st century: A handbook. Geneva: World Health Organization (2016).
58. Lavis, JN, Røttingen, J-A, Bosch-Capblanch, X, Atun, R, el-Jardali, F, Gilson, L, et al. Guidance for evidence- informed policies about health systems: linking guidance development to policy development. PLoS Med. (2012) 9:e1001186. doi: 10.1371/journal.pmed.1001186
59. Kingdon, J. How do issues get on public policy agendas? In: W Wilson, editor. Sociology and the public agenda. Thousand Oaks, CA: Sage Publications (1993)
60. WHO. Primary health care on the road to universal health coverage: 2019 Global monitoring report. Geneva: World Health Organization. 2019 p.
61. Greenhalgh, T, Robert, G, Macfarlane, F, Bate, P, Kyriakidou, O, and Peacock, R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med. (2005) 61:417–30. doi: 10.1016/j.socscimed.2004.12.001
62. Mayne, J. Revising contribution analysis. Can J Program Eval/La revue Canadienne d’évaluation de programme. (2019) 34.2:171–91.
63. Beckfield, J, and Krieger, N. Epi+ demos+ cracy: linking political systems and priorities to the magnitude of health inequities – evidence, gaps and a research agenda. Epidemiol Rev. (2009) 31:152–77. doi: 10.1093/epirev/mxp002
64. Beckfield, J. Political sociology and the people’s health. Oxford: Oxford University Press (2018). 174 p.
65. WHO. Tracking universal health coverage: 2021 Global monitoring report. Geneva: World Health Organization. 2021 p.
Keywords: Primary Health Care, Universal Health Coverage, health systems strengthening, public health, public health emergency, disaster risk management, global health, World Health Organization
Citation: Cheong Chi Mo J, Shah A, Downey C, Genay-Diliautas S, Saikat S, Mustafa S, Meru N, Dalil S, Schmets G and Porignon D (2023) Developing technical support and strategic dialogue at the country level to achieve Primary Health Care-based health systems beyond the COVID-19 era. Front. Public Health. 11:1102325. doi: 10.3389/fpubh.2023.1102325
Edited by:
Pier Luigi Lopalco, University of Salento, ItalyReviewed by:
Filippo Quattrone, Scuola Sant'Anna di Studi Avanzati, ItalyOrvalho Augusto, University of Washington, United States
Copyright © 2023 Cheong Chi Mo, Shah, Downey, Genay-Diliautas, Saikat, Mustafa, Meru, Dalil, Schmets and Porignon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jeremy Cheong Chi Mo, Y2hlb25nakB3aG8uaW50
 Jeremy Cheong Chi Mo
Jeremy Cheong Chi Mo Archana Shah
Archana Shah Casey Downey
Casey Downey Sophie Genay-Diliautas
Sophie Genay-Diliautas Sohel Saikat
Sohel Saikat Saqif Mustafa
Saqif Mustafa Gerard Schmets
Gerard Schmets Denis Porignon
Denis Porignon