- 1School of Nursing, Johns Hopkins University, Baltimore, MD, United States
- 2Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
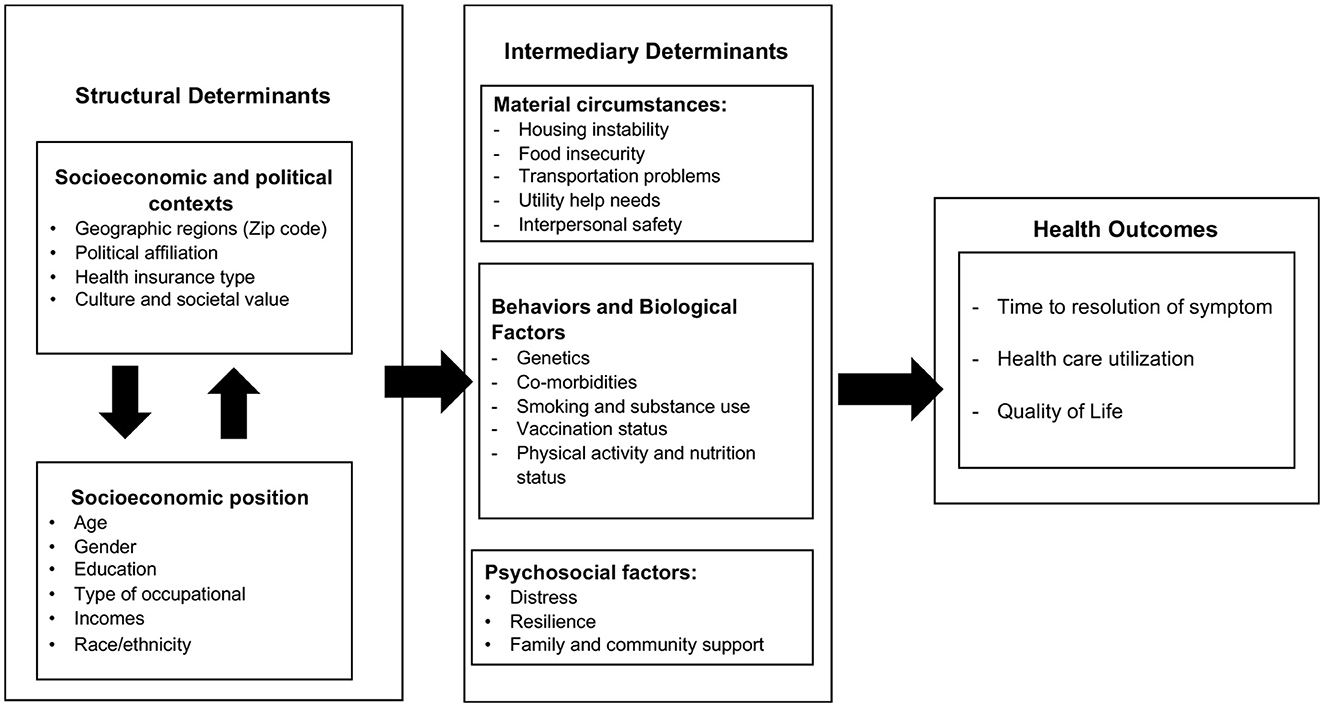
The COVID-19 pandemic has been a challenge for the public health system and has highlighted health disparities. COVID-19 vaccines have effectively protected against infection and severe disease, but some patients continue to suffer from symptoms after their condition is resolved. These post-acute sequelae, or long COVID, continues to disproportionately affect some patients based on their social determinants of health (SDOH). This paper uses the World Health Organization's (WHO) SDOH conceptual framework to explore how SDOH influences long COVID outcomes.
Introduction
The COVID-19 pandemic has created numerous challenges for the public health system and has highlighted health disparities. Since the first known case of COVID-19 coronavirus-induced atypical pneumonia was reported on November 16, 2019, in China (1), there have been over 626 million confirmed cases with over 6.6 million deaths worldwide as of October 20, 2022 (2). Black, Hispanic, and Asian people have been disproportionately affected by COVID-19 infection, hospitalization, and death (3). In April 2021, the US Food and Drug Administration approved multiple vaccines for COVID-19 prevention for the general population. Despite highly transmissible variants, COVID-19 vaccines are, in general, highly efficient in protecting against infection and severe disease (4–6), and the number of COVID-19 survivors has exponentially increased since the rollout of COVID vaccines.
Nevertheless, emerging evidence indicates that patients may continue to suffer from persistent post-infectious symptoms (e.g., fatigue, brain fog, chest or throat pain, or dyspnea) for more than 2 months (median 72 days) and might also have at least one unscheduled outpatient visit up to 6 months post-diagnosis (7, 8). The prevalence of these persistent symptoms is 50% among non-hospitalized patients and up to 87% among hospitalized patients (9–11). To this end, the Centers for Disease Control and Prevention (CDC) have described the COVID-19-related symptoms that last longer than 4 weeks as “Post-Acute Sequelae of COVID-19” or long COVID (12).
Common symptoms associated with long COVID include persistent fatigue, pain, difficulty sleeping, and brain fog (13–15). A systematic review of 47 studies published from January 1, 2020 to March 11, 2021 explored the frequency and variety of persistent symptoms following COVID-19 infection and revealed that the prevalent long COVID symptoms are fatigue (40%), shortness of breath or dyspnea (36%), sleep disorders or insomnia (29.4%), cognitive deficit (17.6%), and atypical chest pain (13.1%) (16); however, the follow-up period, measurement of symptoms, and patient care settings varied across the studies, with the majority of studies focused on individuals previously hospitalized with COVID-19.
Caring for persistent COVID-19 symptoms and complications after the acute period increases healthcare utilization and financial burden for the patients and the healthcare system (17). Vulnerable populations with underlying conditions and individuals with low socioeconomic status may not seek the necessary advanced care because of the increased cost of care and lack of health insurance. Additionally, those struggling with long COVID symptoms are more likely to miss work, leading to decreased job security and less access to health care through reduced availability of occupational health services (18), highlighting the importance of assessing and addressing the social needs of individuals with long COVID.
In 2022, the American Academy of Physical Medicine and Rehabilitation (AAPM&R) published several multidisciplinary, collaborative consensus guidance statements for the assessment and treatment of long COVID-related conditions (19–22). All guidance statements highlighted the importance of health equity to recommend the consideration of social determinants of health (SDOH) in assessing and managing COVID-related symptoms. CDC's interim guidance for evaluating and caring for post-COVID conditions also included recommendations to assess SDOH for patients with long COVID-19 (23). To increase our understanding of SDOH's role in long COVID, this paper explores current evidence on health outcomes in long COVID (e.g., time to symptoms resolution, health care utilization, and quality of life, etc.) in the context of the SDOH framework.
Long COVID in social determinants of health context
The impact of unfavorable SDOH on acute COVID-19 outcomes is well documented (24–27). Multiple attempts have been made to identify vulnerable populations by examining the predictors of risk of infection and the severity of COVID-19. The following factors were identified as potential contributors to the disparity in exposure to the infection, morbidity, and mortality of COVID-19: race/ethnic differences, older age, living with multiple chronic conditions, genetic differences in Human Leukocyte Antigen (HLA) alleles, low socioeconomic status, and limited access to care (28–31).
The role of SDOH in the persistent symptoms of long COVID is less clear. Limited evidence has revealed contributing factors of long COVID. Some studies suggest certain conditions such as sex, age, and comorbidities may increase the risk for developing long COVID (32–36). In an attempt to understand the impact of SDOH on persistent symptoms, we used the World Health Organization (WHO)'s SDOH as a conceptual framework for this paper.
According to WHO, equity in health and wellbeing is impacted by two major elements: structural determinants and intermediary determinants (37). Adapting from the WHO's SDOH conceptual framework, long COVID-related health outcomes such as time to COVID-related symptoms resolution, healthcare utilization, and quality of life are impacted by structural and intermediary determinants (Figure 1).
Structural determinants include (1) socioeconomic and political context, and (2) socioeconomic positions. The socioeconomic and political contexts are a broad set of structural, cultural, and functional aspects of a social system including governance, public and economic policies, culture, and societal values that affect health and affect an individual's health by interplay with the social structure (37). During the pandemic, evidence supported the role of geographic regions in COVID-19-related health outcomes. Cities and towns with high racially-based economic segregation, household crowding, and poverty had higher COVID-19-related mortality rates than predominantly white and wealthy suburban cities (38, 39). The beliefs, institutional trust, and political party affiliation have played key roles in most public health measures (e.g., social distancing, mandatory masks, and vaccination) to prevent the spread of COVID-19 (40–42). The results from US national survey data and a cohort study reported that individuals who self-identified as Republicans had the highest percent of “not wearing a mask,” infrequent physical distancing, and frequent visits to public indoor venues, restaurants/bars/clubs or attending or host parties with more than 10 people than Democrats and Independents (42, 43). Access to healthcare in low socioeconomic ethnic communities was the most significant predictor of high mortality rates related to COVID-19 (44).
The interplay between the socioeconomic and political contexts and social structure leads to social stratification or socioeconomic positions (37). In many societies, incomes, education and occupation, and race/ethnicity are proxies for the socioeconomic position (45). Factors such as sex and age play a role in long COVID as reported by studies that persistent COVID-19 symptoms are commonly reported by individuals identifying as female with an age range from 40 to 66 years (33, 34). For Black or African Americans, lower education rates and sociodemographic disadvantages (e.g., compact housing and lack of health care) are strong contributors to high COVID-19 cases and mortality rates (46, 47). Moreover, some occupations and industries are at higher risk for COVID-19 infection than others because of exposure to infections and proximity to others (48, 49). Therefore, the heightened risk of COVID-19 infection among these populations contributes to an increased risk for subsequent long COVID.
Intermediary determinants include three main categories: (1) material circumstances (e.g., housing instability, food insecurity, transportation problems, utility help needs, interpersonal safety); (2) health behaviors (e.g., smoking and substance use, vaccination status, physical activity, and nutrition) and biological factors (e.g., genetic and comorbidities); and (3) psychosocial circumstances (e.g., distress, resilience, and family/community support). Research has shown that the COVID-19 pandemic has had significant impacts on people of lower socioeconomic status and unfavorable material circumstances (50). During the pandemic, essential and low-income workers have had to continue to work in frontline roles, impacting their ability to comply with physical distancing and increasing their risk for exposure to COVID-19 (50). Additionally, food insecurity makes families unable to stockpile food supplies, thereby resulting in more frequent trips to supermarkets and increased risk of infection (50). Moreover, those experiencing housing instability are forced to rely on temporary living arrangements, often close to others, impacting their ability to physically distance and increasing their risk for COVID-19 infection (51). Finally, those with limited access to transportation must rely on public transit, which not only increases risk for exposure to COVID-19 but also limits access to health care due to transportation unreliability (52). Therefore, material circumstances influence one's risk for COVID-19 infection, in turn contributing to increased long COVID rates.
Evidence suggests that certain behaviors contribute to more severe acute COVID-19 infection and long COVID symptoms (53, 54). Smoking, for example, is known to be associated with poorer outcomes of acute COVID-19 (53). Using a new tool—“Post-COVID-19 Functional Status (PCFS) scale”—Hussein et al.'s (54) found statistically significant differences in functional restrictions related to smoking status, indicating more severe impairments among active smokers compared to former and non-smokers following COVID-19 infection. On the contrary, COVID-19 vaccination may protect against long COVID symptoms. In fact, decreasing or disappearing symptoms (e.g., fatigue, shortness of breath, insomnia, muscle pain, and gastrointestinal problems)—that is, symptom resolution—have been reported following at least one dose of a COVID-19 vaccine (55). Such symptom resolution is believed to be due to vaccine-induced T cells, stimulation of innate immune response, and the diversion of leukocytes, which cause long COVID (56). Pre-existing comorbid conditions (e.g., chronic inflammation, hypertension, cardiovascular disease, and diabetes) were the factors most associated with not returning to “usual health” after COVID (35, 36). Finally, possession of some genetic variations in Angiotensin-converting enzyme, apolipoprotein E, and Brain-Derived Neurotrophic Factors have also been identified as potential predictors for COVID-19 susceptibility and fatality (57–66).
Psychological factors also play a role in persistent symptoms. Not only is long COVID frequently associated with anxiety and depression, but these patients are also at risk for developing somatic symptom disorder due to excessive health-related thoughts as well as post-traumatic stress disorder (67). COVID-19 has increased the prevalence of mental health disorders and there is an expectation that this trend will also be reflected in individuals with long COVID symptoms (68, 69). These psychological outcomes are due in part to social isolation, concerns for family, and limited access to health services, which negatively impact mental health (70, 71). These factors, especially social isolation, and healthcare access may be worsened by material circumstances such as transportation restrictions and Wi-Fi inaccessibility. Additionally, the pandemic contributed to a rise in anti-Asian discrimination and pre-existing structural racism, such as wealth gaps and occupational segregation which disproportionately affect Black and Latinx people (72, 73). Although the prevalence of mental disorders and substance use does not differ among racial and ethnic minority groups, these groups are less likely to receive treatment (74). Furthermore, mental health may be worsened by hospitalization, as patients are exposed to additional risk factors, such as the side effects of treatments. Individuals who are exposed to increased stress in addition to having preexisting mental health vulnerabilities are at an increased risk for developing or worsening poor mental health outcomes.
Resilience has previously been explored as a buffer to negative health outcomes (75), and during the COVID-19 pandemic, it has reaffirmed that enhancing individual resilience can have a positive outcome for mental health conditions including depression (76–78). Although research has failed to find any statistical significance regarding resilience following acute COVID-19 infection, resilience may be a protective factor for the psychiatric outcomes of COVID-19 infection and long COVID (79). Moreover, resilience can be strengthened through the reduction of loneliness, which is a key contributor to distress and poor health (80). As we continue to gather evidence of the direct impact of long COVID-19 symptoms on mental health, primary care providers should be proactive in screening, referrals to local support services, and the provision of resources to target the increased negative impact related to individuals' SDOH (81–83).
Health outcomes: Individuals with long COVID may require specialized care, such as rehabilitation services, mental health counseling, pulmonary support, ongoing medication management, and monitoring of long-term health complications (84). Structural and intermediary determinants may play major roles in how individual seek help, use healthcare resources, and quality of life within the context of long COVID. For example, individuals with low socioeconomic status and low education who suffer from prolonged symptoms may not be aware of the long COVID symptoms or may have limited access to healthcare and social support, and face difficulty returning to work (85, 86). Some ethnic minority individuals with long COVID reported feeling stigmatized or dismissed by healthcare providers which contributed to delays in seeking care, inability to obtain disability benefits, and increased financial hardship (87). Dealing with prolonged health issues that impact living conditions, social support, employment status, and financial security may negatively influence an individual's quality of life.
Discussion
The aim of this paper is to provide an initial assessment of available evidence that is consistent with the concepts in WHO's SDOH framework. We found evidence supporting the structural and intermediary determinants of long COVID outcomes. While the use of an established framework is a strength of this paper, the authors acknowledge that the overall interpretation and conclusion of this paper are potentially impacted by the following limitations. First, no inclusion and exclusion criteria were used for article selection, which could have led to selection bias. Second, the focus of this paper is on evidence in the United States. While other countries may face the challenges of addressing SDOH among individuals with long COVID, the response to these issues can vary significantly between countries. The recognition and response to SDOH can be influenced by a range of factors, including political will, cultural attitudes, historical context, and economic development. These limitations warrant extensive review of evidence and comparison of the perspectives on SDOH among countries.
Conclusion
As we continue to see the new COVID-19 cases and mortality rate decline in 2022, the duration and recovery trajectories of COVID-related symptoms have yet to be clarified. Some patients with COVID will be disproportionally impacted by the long-term symptom burden. Ongoing support should remain a priority for these individuals, with ongoing reassessment and counseling as individuals discover and recover from long COVID-19 symptoms. Moreover, the recognition of emerging scientific evidence on long COVID-related symptoms and the impact of SDOH on long COVID could direct our efforts in promoting equity in the healthcare system. More research is needed to identify the time to symptoms resolution and contributing factors of long COVID-related outcomes, develop systematic and reliable measures for social determinants of health, and cultivate programs or interventions that can provide appropriate care and monitoring processes for patients with COVID who may be at risk of developing long COVID.
Author contributions
NL wrote the editorial. TR, CL, BD, and H-RH participated in reviewing and editing the text. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge with much appreciation to our research assistants and students (Megan Kelly, Jessica Nelson, and Thanakrit Jeamjitvibool) for their help in searching and identifying related literature for this paper. We would like to express our sincere gratitude to Martin Blair for comments and editing assistance for this manuscript. This endeavor would not have been possible without the support from the Johns Hopkins School of Nursing Center for Community Programs, Innovation, and Scholarship (COMPASS Center).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
2. Johns Hopkins University Medicine. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). (2022). Available online at: https://coronavirus.jhu.edu/map.html (Accessed October 20, 202).
3. Lopez L, Hart LH, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. (2021) 325:719–20. doi: 10.1001/jama.2020.26443
4. Chagla, Z. The BNT162b2 (Biontech/Pfizer) vaccine had 95% efficacy against COVID-19 ≥7 days after the 2nd dose. Annal Int Med. (2021) 174:JC15. doi: 10.7326/ACPJ202102160-015
5. Chagla, Z. In adults, the oxford/astrazeneca vaccine had 70% efficacy against COVID-19 >14 D after the 2nd dose. Annal Int Med. (2021) 174:JC29. doi: 10.7326/ACPJ202103160-029
6. Chagla Z. In high-risk adults, the moderna vaccine had 94% efficacy against COVID-19 ≥14 D after the 2nd dose. Ann Intern Med. (2021) 174:JC28. doi: 10.7326/ACPJ202103160-028
7. Hernandez-Romieu AC, Leung S, Mbanya A, Jackson BR, Cope JR, Bushman D, et al. Health care utilization and clinical characteristics of nonhospitalized adults in an integrated health care system 28–180 days after COVID-19 diagnosis — Georgia, May 2020–March 2021. MMWR Morb Mort Weekly Rep. (2021) 70:644–50. doi: 10.15585/mmwr.mm7017e3
8. Mallia P, Meghji J, Wong B, Kumar K, Pilkington V, Chhabra S, et al. Symptomatic, biochemical and radiographic recovery in patients with COVID-19. BMJ Open Resp Res. (2021) 8:e000908. doi: 10.1136/bmjresp-2021-000908
9. Armange L, Bénézit F, Picard L, Pronier C, Guillot S, Lentz P, et al. Prevalence and characteristics of persistent symptoms after non-severe COVID-19: a prospective cohort study. Eur J Clin Microbiol Inf Dis. (2021) 40:2421–5. doi: 10.1007/s10096-021-04261-y
10. Carfi A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. (2020) 324:603–5. doi: 10.1001/jama.2020.12603
11. González-Hermosillo JA, Martínez-López JP, Carrillo-Lampón SA, Ruiz-Ojeda D, Herrera-Ramírez S, Amezcua-Guerra LM, et al. Post-Acute COVID-19 symptoms, a potential link with myalgic encephalomyelitis/chronic fatigue syndrome: a 6-month survey in a Mexican cohort. Brain Sci. (2021) 11:760. doi: 10.3390/brainsci11060760
12. Centers for Disease Control Prevention. Post-COVID Conditions: Information for Healthcare Providers. (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-COVID-conditions.html (Accessed August 5, 2022).
13. Malcolm RS. Chronic fatigue syndrome and long COVID: individualisation, not compartmentalisation. BMJ. (2021) 374:n1863. doi: 10.1136/bmj.n1863
14. Newman M. Chronic fatigue syndrome and long COVID: moving beyond the controversy. BMJ. (2021) 373:n1559. doi: 10.1136/bmj.n1559
15. Wong TL, Weitzer DJ. Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)—a systemic review and comparison of clinical presentation and symptomatology. Medicina. (2021) 57:418. doi: 10.3390/medicina57050418
16. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Network Open. (2021) 4:e2111417. doi: 10.1001/jamanetworkopen.2021.11417
17. Berger Z, Altiery De Jesus V, Assoumou SA, Greenhalgh T. Long COVID and health inequities: the role of primary care. Milbank Q. (2021) 99:519–41. doi: 10.1111/1468-0009.12505
18. Berger AA, Urits I, Hasoon J, Gill J, Aner M, Yazdi CA, et al. improved pain control with combination spinal cord stimulator therapy utilizing sub-perception and traditional paresthesia based waveforms: a pilot study. Anesthesiol Pain Med. (2021) 11:e113089. doi: 10.5812/aapm.113089
19. Blitshteyn S, Whiteson J, Abramoff B, Azola A, Bartels MN, Bhavaraju-Sanka R, et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 Infection (PASC). PMR. (2022) 14:1270–91. doi: 10.1002/pmrj.12894
20. Fine JS, Ambrose AF, Didehbani N, Fleming TK, Glashan L, Longo M, et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of cognitive symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PMR. (2022) 14:96–111. doi: 10.1002/pmrj.12745
21. Maley JH, Alba GA, Barry JT, Bartels MN, Fleming TK, Oleson CV, et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of breathing discomfort and respiratory sequelae in patients with post-acute sequelae of SARS-CoV-2 Infection (PASC). PMR. (2022) 14:77–95. doi: 10.1002/pmrj.12744
22. Whiteson JH, Azola A, Barry JT, Bartels MN, Blitshteyn S, Fleming TK, et al. Multi-Disciplinary collaborative consensus guidance statement on the assessment and treatment of cardiovascular complications in patients with post-acute sequelae of SARS-CoV-2 Infection (PASC). PMR. (2022) 14:855–78. doi: 10.1002/pmrj.12859
23. Centers for Disease Control Prevention. Evaluating and Caring for Patients With Post-COVID Conditions: Interim Guidance. (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-COVID-index.html (Accessed August 22, 2022).
24. Rodriguez J, Quintana Y. Understanding the social determinants of health and genetic factors contributing to the differences observed in COVID-19 incidence and mortality between underrepresented and other communities. J Natl Med Assoc. (2022) 114:430–9. doi: 10.1016/j.jnma.2022.04.002
25. Romain CV, Trinidad S, Kotagal M. The effect of social determinants of health on telemedicine access during the COVID-19 pandemic. Pediatr Ann. (2022) 51:e311–5. doi: 10.3928/19382359-20220606-04
26. Venkataramany B, Sutton J. The importance of social determinants of health for cancer patients in the era of COVID-19. Curēus. (2022) 14:e27993. doi: 10.7759/cureus.27993
27. Wiley Z, Kulshreshtha A, Li D, Kubes J, Kandiah S, Leung S, et al. Clinical characteristics and social determinants of health associated with 30-day hospital readmissions of patients With COVID-19. J Inv Med. (2022) 70:1406–15. doi: 10.1136/jim-2022-002344
28. Adesse D, Gladulich L, Alvarez-Rosa L, Siqueira M, Marcos AC, Heider M, et al. Role of aging in blood-brain barrier dysfunction and susceptibility to SARS-CoV-2 infection: impacts on neurological symptoms of COVID-19. Fluids Barriers CNS. (2022) 19:1–63. doi: 10.1186/s12987-022-00357-5
29. Basir HRG, Majzoobi MM, Ebrahimi S, Noroozbeygi M, Hashemi SH, Keramat F, et al. Susceptibility and severity of COVID-19 are both associated with lower overall viral-peptide binding repertoire of HLA class I molecules, especially in younger people. Front Immunol. (2022) 13:891816. doi: 10.3389/fimmu.2022.891816
30. Huang C, Shi M, Wu H, Luk AOY, Chan JCN, Ma RCW, et al. Human serum metabolites as potential mediators from type 2 diabetes and obesity to COVID-19 severity and susceptibility: evidence from mendelian randomization study. Metabolites. (2022) 12:598. doi: 10.3390/metabo12070598
31. Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. (2021) 174:362–73. doi: 10.7326/M20-6306
32. Brodin P. Immune Determinants of COVID-19 disease presentation and severity. Nat Med. (2021) 27:28–33. doi: 10.1038/s41591-020-01202-8
33. Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Inf. (2021) 27:258–63. doi: 10.1016/j.cmi.2020.09.052
34. Petersen MS, Kristiansen MF, Hanusson KD, Danielsen ME, Steig Á. Long COVID In the Faroe Islands – a longitudinal study among non-hospitalized patients. Clin Infect Dis. (2021) 73:e4058–63. doi: 10.1093/cid/ciaa1792
35. Callender LA, Curran M, Bates SM, Mairesse M, Weigandt J, Betts CJ, et al. The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front Immunol. (2020) 11:1991. doi: 10.3389/fimmu.2020.01991
36. Kayaaslan B, Eser F, Kalem AK, Kaya G, Kaplan B, Kacar D, et al. Post-COVID syndrome: a single-center questionnaire study on 1007 participants recovered from COVID-19. J Med Virol. (2021) 93:6566–74. doi: 10.1002/jmv.27198
37. World Health Organization. A Conceptual Framework for Action on the Social Determinants of Health: World Health Organization. (2021). Available online at: https://apps.who.int/iris/handle/10665/44489 (accessed October 24, 2022).
38. Bauer C, Zhang K, Lee M, Fisher-Hoch S, Guajardo E, McCormick J, et al. Census tract patterns and contextual social determinants of health associated with COVID-19 in a hispanic population from South Texas: a spatiotemporal perspective. JMIR Public Health Sur. (2021) 7:e29205. doi: 10.2196/29205
39. Dalsania AK, Fastiggi MJ, Kahlam A, Shah R, Patel K, Shiau S, et al. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J Racial Ethnic Health Disp. (2022) 9:288–95. doi: 10.1007/s40615-020-00952-y
40. Gratz KL, Richmond JR, Woods SE, Dixon-Gordon KL, Scamaldo KM, Rose JP, et al. Adherence to social distancing guidelines throughout the COVID-19 pandemic: the roles of pseudoscientific beliefs, trust, political party affiliation, and risk perceptions. Ann Behav Med. (2021) 55:399–412. doi: 10.1093/abm/kaab024
41. Rabin C, Dutra S. Predicting engagement in behaviors to reduce the spread of COVID-19: the roles of the health belief model and political party affiliation. Psychol Health Med. (2022) 27:379–88. doi: 10.1080/13548506.2021.1921229
42. Schoeni RF, Wiemers EE, Seltzer JA, Langa KM. Political affiliation and risk taking behaviors among adults with elevated chance of severe complications from COVID−19. Prev Med. (2021) 153:106726. doi: 10.1016/j.ypmed.2021.106726
43. Leventhal AM, Dai H, Barrington-Trimis JL, McConnell R, Unger JB, Sussman S, et al. Association of political party affiliation with physical distancing among young adults during the COVID-19 pandemic. JAMA Intern Med. (2021) 181:399–403. doi: 10.1001/jamainternmed.2020.6898
44. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
45. Ribeiro AI, Fraga S, Severo M, Kelly-Irving M, Delpierre C, Stringhini S, et al. Association of neighbourhood disadvantage and individual socioeconomic position with all-cause mortality: a longitudinal multicohort analysis. Lancet Public Health. (2022) 7:e447–57. doi: 10.1016/S2468-2667(22)00036-6
46. Hawkins RB, Charles EJ, Mehaffey JH. Socio-economic Status and COVID-19–Related Cases and Fatalities. Public Health. (2020) 189:129–34. doi: 10.1016/j.puhe.2020.09.016
47. Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Network Open. (2021) 4:e2036462. doi: 10.1001/jamanetworkopen.2020.36462
48. Baker MG, Peckham TK, Seixas NS. Estimating the burden of united states workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS ONE. (2020) 15:e0232452. doi: 10.1371/journal.pone.0232452
49. Webb J. Social aspects of chronic transfusions: addressing social determinants of health, health literacy, and quality of life. Hematology. (2020) 2020:175–83. doi: 10.1182/hematology.2020000104
50. Green H, Fernandez R, MacPhail C. the social determinants of health and health outcomes among adults during the COVID-19 pandemic: a systematic review. Public Health Nurs. (2021) 38:942–52. doi: 10.1111/phn.12959
51. Schulz AJ, Mehdipanah R, Chatters LM, Reyes AG. Moving health education and behavior upstream: lessons from COVID-19 for addressing structural drivers of health inequities. Health Educ Behav. (2020) 47:519–24. doi: 10.1177/1090198120929985
52. Chen KL, Brozen M, Rollman JE, Ward T, Norris KC, Gregory KD, et al. How is the COVID-19 pandemic shaping transportation access to health care? Transportation research. Interdis Persp. (2021) 10:100338. doi: 10.1016/j.trip.2021.100338
53. Augustin M, Schommers P, Stecher M, Dewald F, Gieselmann L, Gruell H, et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Regional Health. (2021) 6:100122. doi: 10.1016/j.lanepe.2021.100122
54. Hussein MH, Elshazli RM, Attia AS, Nguyen TP, Aboueisha M, Munshi R, et al. Asthma and COVID-19; different entities, same outcome: a meta-analysis of 107,983 patients. J Asthma. (2021) 59:851–8. doi: 10.1080/02770903.2021.1881970
55. Massey D, Huang C, Lu Y, Cohen A, Oren Y, Moed T, et al. Engagement with COVID-19 public health measures in the United States: a cross-sectional social media analysis from June to November 2020. J Med Internet Res. (2021) 23:e26655. doi: 10.2196/26655
56. Iwasaki A. How Vaccines Might Improve Long COVID. (2021). Available online at: https://elemental.medium.com/how-vaccines-might-improve-long-COVID-c1f41c4d7378 (accessed October 24, 2022).
57. Baker HA, Safavynia SA, Evered LA. The ‘third wave': impending cognitive and functional decline in COVID-19 survivors. Br J Anaesthesia. (2021) 126:44–7. doi: 10.1016/j.bja.2020.09.045
58. Bektas A, Schurman SH, Franceschi C, Ferrucci LA. Public health perspective of aging: do hyper-inflammatory syndromes such as COVID-19, SARS, ARDS, cytokine storm syndrome, and post-ICU syndrome accelerate short- and long-term inflamming? Immun Ageing. (2020) 17:1–23. doi: 10.1186/s12979-020-00196-8
59. Bonnell LN, Crocker AM, Kemp K, Littenberg B. The relationship between social determinants of health and functional capacity in adult primary care patients with multiple chronic conditions. J Am Board Family Med. (2021) 34:688–97. doi: 10.3122/jabfm.2021.04.210010
60. Datta SD, Talwar A, Lee JTA. Proposed framework and timeline of the spectrum of disease due to SARS-CoV-2 infection: illness beyond acute infection and public health implications. JAMA. (2020) 324:2251–2. doi: 10.1001/jama.2020.22717
61. Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. (2020) 44:258–79. doi: 10.2337/dci20-0053
62. Kuo C, Pilling LC, Atkins JL, Fortinsky RH, Kuchel GA, Melzer DAPOE, et al. Genotypes increase risk of delirium during COVID-19-related hospitalizations: evidence from a large UK cohort. J Gerontol Series A. (2022) 77:879–80. doi: 10.1093/gerona/glab184
63. Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol. (2021) 12:698169. doi: 10.3389/fmicb.2021.698169
64. Quiñones J, Hammad Z. Social determinants of health and chronic kidney disease. Curēus. (2020) 12:e10266. doi: 10.7759/cureus.10266
65. Rodrigues JCG, Pinto P, Leitão LPC, Vinagre LWMS, Monte N, Fernandes MR, et al. Influence of APOE locus on poor prognosis of COVID-19. Heliyon. (2021) 7:e07379. doi: 10.1016/j.heliyon.2021.e07379
66. Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. (2014) 47:29–48. doi: 10.1007/s12020-014-0195-0
67. Horn M, Fovet T, Vaiva G, D'Hondt F, Amad A. Somatic symptom disorders and long COVID: a critical but overlooked topic. Gen Hosp Psychiatry. (2021) 72:149–50. doi: 10.1016/j.genhosppsych.2021.06.007
68. Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:813–24. doi: 10.1016/S2215-0366(20)30307-2
69. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
70. Abdalla SM, Ettman CK, Cohen GH, Galea S. Mental health consequences of COVID-19: a nationally representative cross-sectional study of pandemic-related stressors and anxiety disorders in the USA. BMJ Open. (2021) 11:e044125. doi: 10.1136/bmjopen-2020-044125
71. Adikari A, Nawaratne R, De Silva D, Ranasinghe S, Alahakoon O, Alahakoon D, et al. Emotions of COVID-19: content analysis of self-reported information using artificial intelligence. J Med Internet Res. (2021) 23:e27341. doi: 10.2196/27341
72. Garcia MA, Homan PA, García C, Brown TH. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older black and latinx adults. J Gerontol Series B. (2021) 76:e75–80. doi: 10.1093/geronb/gbaa114
73. Da Teixeira Silva JA. Stigmatization, discrimination, racism, injustice, and inequalities in the COVID-19 era. Int J Health Policy Manage. (2020) 9:484–5. doi: 10.34172/ijhpm.2020.87
74. McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, Njai R, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic — United States, April and May 2020. MMWR. (2021) 70:162–6. doi: 10.15585/mmwr.mm7005a3
75. Melnyk BM, Kelly SA, Stephens J, Dhakal K, McGovern C, Tucker S, et al. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: a systematic review. Am J Health Promot. (2020) 34:929–41. doi: 10.1177/0890117120920451
76. Chan ACY, Piehler TF, Ho GWK. Resilience and mental health during the COVID-19 pandemic: findings from Minnesota and Hong Kong. J Affect Disord. (2021) 295:771–80. doi: 10.1016/j.jad.2021.08.144
77. Tamarit A, De la Barrera U, Schoeps K, Castro-Calvo J, Montoya-Castilla I. Analyzing the role of resilience and life satisfaction as mediators of the impact of COVID-19 worries on mental health. J Commun Psychol. (2022) 51:234–50. doi: 10.1002/jcop.22900
78. Verdolini N, Amoretti S, Montejo L, García-Rizo C, Hogg B, Mezquida G, et al. Resilience and mental health during the COVID-19 pandemic. J Affect Disord. (2021) 283:156–64. doi: 10.1016/j.jad.2021.01.055
79. Gramaglia C, Gambaro E, Bellan M, Balbo PE, Baricich A, Sainaghi PP, et al. Mid-term psychiatric outcomes of patients recovered from COVID-19 from an italian cohort of hospitalized patients. Front Psychiatry. (2021) 12:667385. doi: 10.3389/fpsyt.2021.667385
80. Mikocka-Walus A, Stokes M, Evans S, Olive L, Westrupp E. Finding the power within and without: how can we strengthen resilience against symptoms of stress, anxiety, and depression in australian parents during the COVID-19 pandemic? J Psychosom Res. (2021) 145:110433. doi: 10.1016/j.jpsychores.2021.110433
81. Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. Can Med Assoc J. (2016) 188:E474–83. doi: 10.1503/cmaj.160177
82. Mughal F, Hossain MZ, Brady A, Samuel J, Chew-Graham CA. Mental health support through primary care during and after COVID-19. BMJ. (2021) 373:n1064. doi: 10.1136/bmj.n1064
83. Popay J, Kowarzik U, Mallinson S, Mackian S, Barker J. Social problems, primary care and pathways to help and support: addressing health inequalities at the individual level. J Epidemiol Commun Health. (2007) 61:972–7. doi: 10.1136/jech.2007.061945
84. Koumpias AM, Schwartzman D, Fleming O. Long-haul COVID: healthcare utilization and medical expenditures 6 months post-diagnosis. BMC Health Serv Res. (2022) 22:1–14. doi: 10.1186/s12913-022-08387-3
85. Heller O, Chun Y, Shapira S, Troen A, Shlomo Y, Acri M, et al. Prevalance of long COVID among low-income and marginalized groups: evidence from Israel. Int J Public Health. (2022) 28:1–11. doi: 10.3389/ijph.2022.1605086
86. Schiavi M, Fugazzaro S, Bertolini A, Denti M, Mainini C, Accogli MA, et al. “Like before, but not exactly”: the QUALY-react qualitative inquiry into the lived experience of long COVID. BMC Public Health. (2022) 22:599. doi: 10.1186/s12889-022-13035-w
Keywords: long COVID, post-acute sequelae SARS-CoV-2 infection, social determinants of health, health disparities, health equality
Citation: Lukkahatai N, Rodney T, Ling C, Daniel B and Han H-R (2023) Long COVID in the context of social determinants of health. Front. Public Health 11:1098443. doi: 10.3389/fpubh.2023.1098443
Received: 14 November 2022; Accepted: 03 March 2023;
Published: 28 March 2023.
Edited by:
Cyrille Delpierre, INSERM U1027 Epidémiologie et analyses en santé publique: Risques, Maladies Chroniques et Handicap, FranceReviewed by:
Vandentorren Stéphanie, Santé Publique France, FranceCopyright © 2023 Lukkahatai, Rodney, Ling, Daniel and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nada Lukkahatai, bmFkYS5sdWtrYWhhdGFpQGpodS5lZHU=
 Nada Lukkahatai
Nada Lukkahatai Tamar Rodney
Tamar Rodney Catherine Ling
Catherine Ling Brittany Daniel
Brittany Daniel Hae-Ra Han
Hae-Ra Han