- Kaiser Permanente Evidence-based Practice Center, Kaiser Permanente Center for Health Research, Portland, OR, United States
Objective: To identify policy actions that may improve the interface of public health and health care in the United States.
Methods: A rapid review of publicly-available documents informing the integration of public health and health care, and case examples reporting objective measures of success, with abstraction of policy actions, related considerations, and outcomes.
Results: Across 109 documents, there were a number of recurrent themes related to policy actions and considerations to facilitate integration during peace time and during public health emergencies. The themes could be grouped into the need for adequate and dedicated funding; mandates and shared governance for integration; joint leadership that has the authority/ability to mobilize shared assets; adequately staffed and skilled workforces in both sectors with mutual awareness of shared functions; shared health information systems with modernized data and IT capabilities for both data collection and dissemination of information; engagement with multiple stakeholders in the community to be maximally inclusive; and robust communication strategies and training across partners and with the public.
Conclusion: While the evidence does not support a hierarchy of policies on strengthening the interface of public health and health care, recurrent policy themes can inform where to focus efforts.
1. Introduction
The importance of coordination between public health (PH) and health care (HC) entities became highly apparent during the COVID-19 pandemic. For most PH jurisdictions, the lack of an integrated epidemic response model impaired the ability of both PH and HC entities to respond in a timely and effective manner to mitigate the high rates of COVID-19 transmission and its subsequent morbidity and mortality. Due in large part to the historical evolution and financing of the two in the United States, the PH and HC sectors lack a structured partnership with one another, which has greatly hindered coordination and innovation around the delivery of shared core functions. While there is abundant literature on the need for and barriers to such partnerships, as well as case studies of integrated models of PH and HC, it is less clear what local, state, and federal policy actions are needed to improve the interface between PH and HC. In support of a planned Delphi Process to develop an actionable policy agenda, Kaiser Permanente commissioned this rapid review of publicly available documents on the integration of PH and HC. Integration is an imprecise term and meant, in this report, to encompass the full continuum of coordination from cooperation to collaboration, to partnership, to merger (i.e., single entity).
2. Methods
We searched Medline ALL via Ovid from 2000 through 18 April 2022 to identify English language published evidence, expert or consensus recommendations, concept papers, and case studies of optimal models on the integration of PH and HC. The search was designed to capture papers on PH integration with HC. The concept of PH was captured with the terms “public health” or “population health” or “community health.” The concept of HC included components of a health systems (e.g., primary care, hospitals, health insurance) and health planning (e.g., delivery of care, health policy trends, practice, or local government). We also included terms to capture settings or instances in which integration or coordination would be necessary (e.g., public health emergencies, disaster planning). We supplemented searches with expert input and reference lists of selected documents.
We communicated in real time with our Office of Community Health liaisons at Kaiser Permanente on refining our inclusion criteria as we reviewed titles and abstracts. We included any document that explicitly focused on the integration or interface between PH and HC. HC included health systems (hospital and ambulatory), health plans, long-term care, pharmacies, laboratory services, inclusive of medical, mental/behavioral, and dental services. We included of countries with different PH and HC infrastructures; however we excluded documents focusing only on low- and middle-income countries. We also conducted targeted searches for white papers or policy documents on PH and HC resilience, data sharing and IT interoperability, and international models of the integration of PH and HC. Targeted searches involved searching keywords in Google, government websites, and the websites of other organizations of interest.
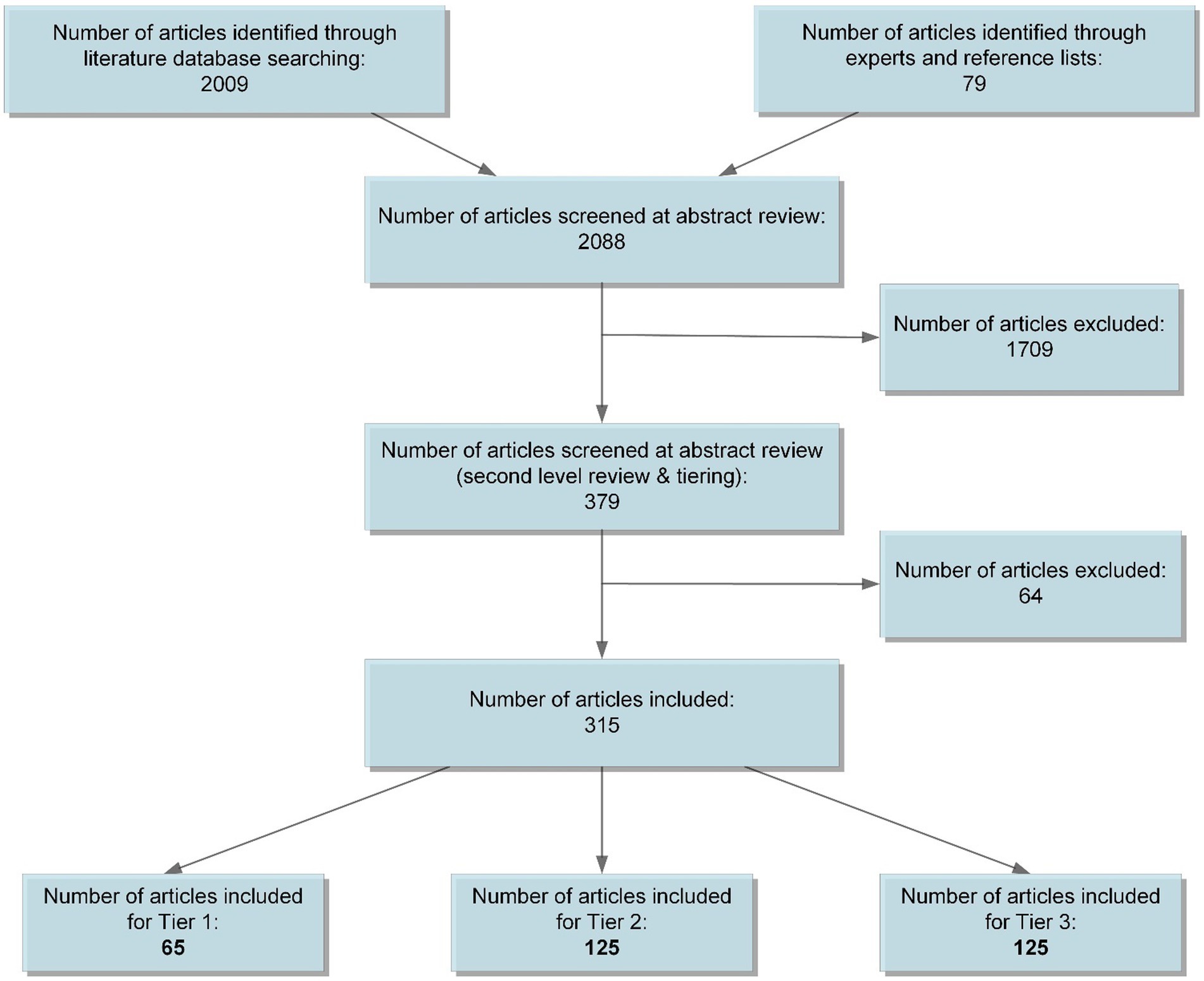
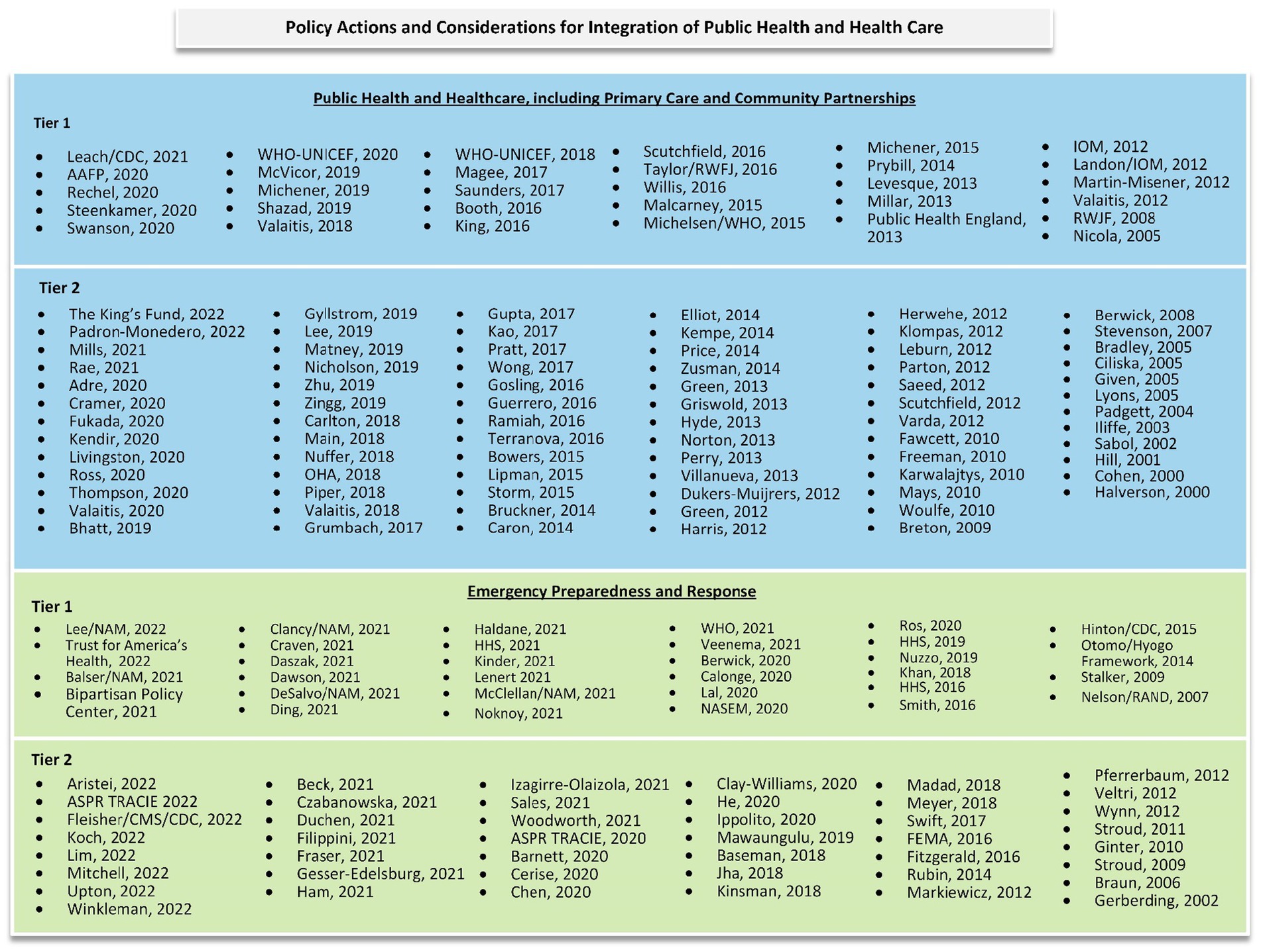
We reviewed titles and abstracts for inclusion. If abstracts were not available, or inclusion could not be determined by title and abstract only, we reviewed the full text for inclusion (Figure 1). After inclusion, we categorized sources into three tiers. Tier 1 consisted of exemplar papers meeting inclusion criteria to be used as our primary source of data (e.g., recent guidance/statements, expert panel or large consensus papers, scoping or systematic reviews, collections of case examples informing broader guidance statements, case studies of multinational efforts). Tier 2 consisted of papers that met inclusion criteria but were single expert or opinion pieces, older publications, and/or individual case studies. Tier 3 consisted of papers that only marginally met our inclusion criteria (i.e., may not have specified collaboration between PH and HC, do not inform policy actions or considerations). Within each tier, we identified two major categories of documents: those generally addressing the integration of PH and HC or primary care and those specific to emergency preparedness and response.
Included articles were not critically appraised for risk of bias. We abstracted main findings focusing on policy actions and considerations from all Tier 1 articles. We then identified shared themes (of actions and considerations) and grouped these themes into general domains. For Tier 1 articles that included an intentional effort to capture a wide representation of case examples (e.g., literature or scoping review), we also recorded when case examples were cited or used to support the policy recommendations. When possible, we added more granularity to policy actions and considerations from these case examples. We then abstracted the main findings from Tier 2 articles and cross-walked these findings with findings from Tier 1 papers to make sure we had achieved saturation of themes. We a priori planned only to abstract Tier 3 articles if saturation of content with Tier 2 articles was not achieved. We did not abstract findings from Tier 3 articles. These themes of potential policy actions and considerations are summarized in two main tables (Supplementary Tables 1, 2). We also abstracted general details from Tier 2 case examples of PH and HC integration, noting if objective measures of success were reported. Published studies reporting objective measures of success are summarized in a separate table (Supplementary Table 3).
A draft of this review underwent external peer review by eight experts in public health, population health, community health, emergency preparedness and response, and laboratory services.
3. Results
3.1. Categorization of included studies and their policy themes
For this review we included 109 Tier 1 and Tier 2 documents addressing the integration of PH and HC (including PC) (1–109) and 76 on integration in the context of emergency preparedness and response (Figure 2) (110–185). Many of the articles that reported on the integration of PH and HC were on multisectoral partnerships or collaborations, of which PH and HC were part. Documents focused on bolstering the infrastructure or resilience of PH, without explicit mention of actions or considerations around the integration of PH and HC, were not included (186–190).
Within in each body of literature, we grouped policy actions and considerations for the integration of PH and HC into eight domains: (1) Funding and finance, (2) Governance and legal, (3) Alignment of the core functions that overlap between PH and HC (i.e., surveillance of population health [systematic and opportunistic], health protection and disease control [communicable and non-communicable], health promotion and action on upstream drivers of health, prevention of disease and injuries, and health advocacy), (4) Quality improvement, (5) Physical infrastructure, medical supplies, technologies, and supply chains, (6) Leadership and workforce development, (7) Data and IT capabilities, and (8) Multisectoral partnerships and public engagement. These domains are not mutually exclusive and in some cases the actions and considerations listed apply to multiple categories.
In most instances, policy actions and considerations were stated without specific mention of who should enact or consider these policies (i.e., which entities, organizations, governing bodies). Likewise, in some instances, the actions and considerations could be enacted or considered at multiple levels (e.g., local, regional, state, or national levels), but this was also, most often, not specified.
Although many documents were supported by explicit efforts to identify case examples, often it was not clear to what extent findings or recommendations were supported by ‘successful’ case examples. In addition, definitions or objective metrics of success were not commonly detailed in these reports. Many case examples demonstrate proof of concept and/or subjective assessment of partners’ satisfaction. When documents were explicit that case examples supported their conclusions or recommendations, statements were general in nature (e.g., most of the successful collaborations included pre-existing partnerships).
3.2. Public health and health care (including primary care)
Most of the documents addressing the integration of PH and HC focused specifically on primary care (PC) or multisectoral partnerships of PH, HC, and community. Articles covered a wide range of conditions and topics including maternal and child health, chronic diseases (e.g., diabetes, cardiovascular disease), communicable diseases (e.g., HIV and sexually transmitted infections, tuberculosis), cancer, behavioral risk factors (e.g., tobacco use), oral health, multimorbidity; models of care and care settings (e.g., federally qualified health centers, palliative care, long-term care, pharmacy); populations (e.g., pediatric, Medicaid); and provider type (e.g., nurses). While some of these documents focus narrowly on the overlap or integration of PH and HC sectors to deliver individual health care, many more address greater alignment of essential public health services that go beyond public health clinics or publicly funded HC.
Common policy actions and considerations articulated in the documents primary clustered around the need for (Supplementary Table 1):
• Adequate financial resources to improve population health (e.g., adequate base funding, long-term funding, funding to maintain data systems), dedicated funding for collaboration (personnel/programs, training);
• Different payment models (i.e., value-based payment and move away from fee-for-service payment) and purchasing and payment systems to foster reorientation in models of care that integrate PH and PC, or offer adequate remuneration of proactive population health activities and services;
• Mandates for PH and HC (including mental health) integration;
• Shared governance structure (or entities) with defined charter and strategic plan to improve population health, developed with all relevant partners (which may go beyond PH and HC);
• Implementation of models of care that promote high-quality, people-centered, PH and PC integrated health services throughout the life course;
• Application of population health approach and focus on upstream drivers of health (e.g., social determinants of health);
• Robust communication channels between different entities in PH and HC (e.g., timely, multilayered, transparent);
• Infrastructure with equitable distribution of telehealth and health data systems across care settings, sectors and geographic locations;
• Learning environment that integrates quality improvement for patient care and program planning, and accountability to stakeholders;
• Shared or aligned multilevel and distributed leadership;
• Skilled workforce with training for a new set of core competencies (e.g., partnering and team-based care, quality improvement, IT skills, and communication skills);
• Modernized multisectoral data system, with oversight and data linkage by personal or regional identifier, as well as linkage between health and socioeconomic information to address equity; and
• Community engagement with a broad range of stakeholders from private and public sectors with adequate bidirectional communication channels, leveraging digital technologies.
Case examples illustrate that integration of PH and PC may be at the level of delivery of care (e.g., community health clinics in the United States) or integrating PH functions into PC such that they function as one entity (e.g., geographically based integrated care systems in the United Kingdom). Case examples with objective metrics of success demonstrate that the integration of PH and HC in the form of maternal child programs, communicable disease prevention and control programs (e.g., HIV), health information exchanges, health promotion and health protection programs, chronic disease prevention and management, as well as efforts focusing on youth health, women’s health, mental health and working with vulnerable populations, can improve access to care and patient health outcomes (Supplementary Table 3).
3.3. Emergency preparedness and response
Most of the emergency preparedness documents were in response to infectious disease PH emergencies (e.g., COVID-19, H1N1) or intended to be broadly inclusive of any PH emergency. A handful of articles focused on other threats, specific topics, or certain populations (e.g., bioterrorism, IT specific, pediatric populations). Common policy actions and considerations articulated in the documents primary clustered around the need for (Supplementary Table 2):
• An increase in flexible and sustained (and stable) funding (personnel/programs, training, infrastructure, data systems);
• Mandates and incentives for PH and HC integration;
• Formal governance structures (or entities) for integration assigning clear roles and responsibilities for each partner;
• Alignment of delivery of shared core functions of PH and HC (e.g., for emergency and non-emergency health services, health risk assessment and surveillance);
• Physical infrastructure that can support surge capacity and weather interruptions, and that leverages telehealth for delivery of core functions;
• Robust measurement strategy to support emergency response, as well as metrics and accountability for performance (to include health equity);
• Dedicated joint leadership between PH and HC with a clear command structure;
• Skilled workforce with adequate (flexible) capacity, training, and support (for mental health and retention);
• Modernized shared data system across sectors (including social sectors) and routinely disaggregated data by key social risk factors (including race/ethnicity); and
• Investment in community partnerships and public engagement with adequate, bidirectional channels of communication that can be a trusted source of timely information as well as used to obtain feedback from public.
Although published case examples of PH and HC integration in the setting of public health emergencies with objective metrics of success are limited, examples demonstrate that coordination of delivery of care using multisectoral coordination or partnership (e.g., PH, hospital, PC, pharmacies, community) can offload hospital demand, improve access to care, and improve vaccination rates during infectious disease outbreaks (Supplementary Table 3).
4. Discussion
This rapid review identified a large volume of published or public documents that can inform policy actions and considerations to support the integration of PH and HC in general or specific to PH emergencies. Although these documents span over 20 years, the general themes are quite consistent over time. Because the path of least resistance will always be to work unilaterally, a deliberate and concerted effort must be made to effectively integrate PH and HC. Dedicated funding, incentives, and governance in a hospitable financial and legal environment, as well as a concerted effort by leadership across the federal, regional/state, and local levels is essential for successful integration. This integration extends to multiple entities within PH and HC that are less often acknowledged (e.g., laboratories, mental health providers, pharmacies, long-term care facilities) but, as demonstrated by the COVID-19 pandemic, are critical elements to PH and HC. Ultimately, integration of PH and HC will allow for a proactive rather than reactive management of individual and population health, both during ‘peace time’ and during public health emergencies. Addressing population health will necessarily require addressing health equity as well as upstream and social drivers of health.
Integration between PH and HC necessarily evolves over time and represents a continuum from mutual awareness to true partnership (or functioning as a single entity, in some other countries). The eventuality of true partnership in part depends on time, such that the most efficient policies may be those that foster initial phases of integration. Likewise, the most efficient policies may be those that leverage existing collaborations (e.g., healthcare coalitions). Demonstrating return on investment is critical, but it is important to understand that realizing ‘success’ in this endeavor will happen on a time scale different than most health-related innovations and will require development of adequate metrics of success.
In our review, we found that successful PH initiatives with collaborations at the local and regional level were frequently made possible by commensurate funding and policies at the federal level. External events with funding (e.g., state federal tobacco settlement funds, federal emergency preparedness grants and funding) were necessary catalysts for collaboration. Case examples revealed multiple factors influencing successful integration between PH and HC, including government involvement, geographic proximity of partners, shared goal (of population health) with clear roles/responsibilities and shared protocols, aligned leadership, accountability, workforce education and training, and sharing and collaborative use of data and analysis. Since a community is the immediate and ultimate ‘caretaker’ of populations served by PH and HC, communities need to be included in these integrative efforts. While PH and HC may be the core partners, engaging a broad range of private and public community partners (e.g., social services, education, business, faith-based organizations, community-based organizations) will be necessary to respond to public health emergencies and achieve population health goals.
4.1. Limitations
This review included only public or published documents since 2000. We acknowledge that the discussion on the integration of PH and HC reaches back further, with much of the seminal work in the 1990s (e.g., Medicine and Public Health, Lasker and Committee on Medicine and Public Health, 1997 191). Although we conducted targeted efforts using experts, selected reference lists, and web searches to supplement database searching, this review is not exhaustive. Additionally, our identification of examples of the integration of PH and HC surfaced successful efforts, rather than analyses of failed PH and HC integration efforts which are also important in developing policy considerations. Nonetheless, we do believe, given the saturation of themes achieved, that this review represents a summary of major policy actions and considerations on the integration of PH and HC.
Due to the rapid nature of this review, there are several important areas related to the integration of PH and HC that are mentioned, but are not comprehensively covered in this report. These areas include: bolstering PH and PH resilience post-pandemic; bolstering under-resourced aspects of HC (i.e., PC, long-term care, safety net care, rural care); bolstering the PH and HC supply chain; implementing population health in HC or PC; hospital or workplace infection prevention and control; addressing social drivers of health and other upstream drivers of health in PH or HC; the current funding and regulatory environment of PH and HC; general data and IT coordination considerations (e.g., technical interoperability); and the role of research and research partnerships (with PH and HC). Additionally, this review includes documents referring to models of care from various countries that integrate or facilitate the integration of PH and PC. While these exemplar models of care are listed, a deep dive on these models of care was not possible. Last, some of the themes for policy actions and considerations relate to health equity (including the equitable distribution of resources), and when explicitly mentioned by source documents this has been documented. However, and especially with current knowledge and context, it can be argued that most if not all the policy actions and considerations should be seen through a health equity lens.
4.2. Conclusion
While the evidence does not support a hierarchy of policy actions and considerations (i.e., it is unclear from case examples of successful integration efforts or models of care what components or external factors contributed to their success), commonalities across examples can help inform where to focus. This review suggests that policy actions and considerations to effectively integrate PH and HC during peace time and during public health emergencies include: the need for adequate and dedicated funding for integration, mandates for integration, shared governance for integration, joint leadership that has the authority/ability to mobilize shared assets, adequately staffed and skilled workforces in both sectors with awareness of shared functions, shared health information systems with modernized data and IT capabilities, engagement with multiple stakeholders in the community to be maximally inclusive, and robust communication strategies and training across partners and with the public.
Author contributions
JL obtained funding, served as the lead on the synthesis of findings, and drafted the manuscript. EW assisted with the synthesis of findings and review of manuscript, as well as conducted the identification of and abstraction from included studies. SB and AM conducted the identification of and abstraction from included studies, as well as created tables and figures. MD conducted all database searches and reviews. All authors contributed to the article and approved the submitted version.
Funding
Funding for this review was provided by Kaiser Permanente’s Office of Community Health.
Acknowledgments
The authors gratefully acknowledge the following individuals for their contributions to this review: David Grossman and Kendall Stagg for their input as our Office of Community Health liaisons at Kaiser Permanente; Onora Lien for her expertise and consultation with regards to healthcare coalitions; Stephen Evans, Paul Wallace, Ned Calonge, Anand Parekh, Elizabeth Frentzel, Jill Taylor, Jennifer Lee, and Michael Fraser for their external peer review of an earlier version of this report; and Jill Pope and Katie Essick for editing this report; and Debra Burch for formatting this report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1098431/full#supplementary-material
References
1. The King's Fund. Integrated care systems (ICSs): Key planning and partnership bodies from July 22. (2022). Available at: https://www.kingsfund.org.uk/audio-video/integrated-care-systems-health-and-care-act#ics-structure (Accessed 27 May 2022). PMID.
2. Padron-Monedero, A, Suárez, RS, Bogaert, P, Abboud, L, van Oyen, H, Tolonen, H, et al. Integrating technical and political views for a sustainable European distributed infrastructure on population health. Arch Public Health. (2022) 80:29. doi: 10.1186/s13690-022-00790-w
3. Rae, M, and Marshall, M. General practice and public health: fostering collaboration for better health for populations. BMJ. (2021) 375:n2916. doi: 10.1136/bmj.n2916
4. Mills, J, Abel, J, Kellehear, A, and Patel, M. Access to palliative care: the primacy of public health partnerships and community participation. Lancet. Public Health. (2021) 6:e791–2. doi: 10.1016/S2468-2667(21)00213-9,
5. Leach, B, Parkinson, S, d'Angelo, C, Gloinson, E, Rodriguez-Rincon, D, Bertscher, A, et al. Assessment of electronic health records for infectious disease surveillance: final mapping exercise report. Stockholm: European Centre for Disease Prevention and Control (ECDC) (2021).
6. Cramer, GR, Young, GJ, Singh, S, McGuire, J, and Kim, D. Evidence that collaborative action between local health departments and nonprofit hospitals helps foster healthy behaviors in communities: a multilevel study. BMC Health Serv Res. (2021) 21:1. doi: 10.1186/s12913-020-05996-8
7. World Health Organization. United Nations Children's fund (UNICEF). Operational framework for primary health care: Transforming vision into action. Geneva: WHO (2020).
8. Valaitis, RK, Wong, ST, MacDonald, M, Martin-Misener, R, O’Mara, L, Meagher-Stewart, D, et al. Addressing quadruple aims through primary care and public health collaboration: ten Canadian case studies. BMC Public Health. (2020) 20:507. doi: 10.1186/s12889-020-08610-y
9. Thompson, H, Swander, L, Cohen, R, Lukazewski, A, Bartholow, T, Pesik, M, et al. Hypertension-focused medication therapy management: a collaborative pilot program uniting pharmacists, public health, and health insurers in Wisconsin. Prev Chronic Dis. (2020) 17:E105. doi: 10.5888/pcd17.200058
10. Swanson, M, Wong, ST, Martin-Misener, R, and Browne, AJ. The role of registered nurses in primary care and public health collaboration: a scoping review. Nurs Open. (2020) 7:1197–207. doi: 10.1002/nop2.496
11. Steenkamer, B, Drewes, H, Putters, K, van Oers, H, and Baan, C. Reorganizing and integrating public health, health care, social care and wider public services: a theory-based framework for collaborative adaptive health networks to achieve the triple aim. J Health Serv Res Policy. (2020) 25:187–201. doi: 10.1177/1355819620907359
12. Ross, LA, Bloodworth, LS, Brown, MA, Malinowski, SS, Crane, R, Sutton, V, et al. The Mississippi Delta health collaborative medication therapy management model: public health and pharmacy working together to improve population health in the Mississippi Delta. Prev Chronic Dis. (2020) 17:E108. doi: 10.5888/pcd17.200063
13. Rechel, B. How to enhance the integration of primary care and public health? Approaches, facilitating factors and policy options [Internet]. European Observatory on Health Systems and Policies. Copenhagen (Denmark) (2020). Available from: https://www.ncbi.nlm.nih.gov/books/NBK553739/
14. Livingston, CJ, Bartelmann, SE, Goff, NM, and Arid, KG. Reducing tobacco use in Oregon through multisector collaboration: aligning Medicaid and public health programs. Prev Chronic Dis. (2020) 17:E155. doi: 10.5888/pcd17.200220
15. Kendir, C, Breton, E, le Bodo, Y, and Bourgueil, Y. Collaboration of primary care and public health at the local level: observational descriptive study of French local health contracts. Prim Health Care Res Dev. (2020) 21:e61. doi: 10.1017/S1463423620000559
16. Fukuda, HD, Randall, LM, Meehan, T, and Cranston, K. Leveraging health department capacities, partnerships, and health insurance for infectious disease response in Massachusetts, 2014-2018. Public Health Rep. (2020) 135:75S–81S. doi: 10.1177/0033354920904084
17. American Academy of Family Physicians. Integration of primary care and public heath (position paper). (2022) Available at: https://www.aafp.org/about/policies/all/integration-primary-care.html (Accessed 14 April 2022).
18. Adre, C, Jump, RLP, and Spires, SS. Recommendations for improving antimicrobial stewardship in long-term care settings through collaboration. Infect Dis Clin N Am. (2020) 34:129–43. doi: 10.1016/j.idc.2019.10.007
19. The 2017 Geneva-IPC Think TankZingg, W, Storr, J, Park, BJ, Jernigan, JA, Harbarth, S, et al. Broadening the infection prevention and control network globally; 2017 Geneva IPC-think tank (part 3). Antimicrob Resist Infect Control. (2019) 8:74. doi: 10.1186/s13756-019-0528-0
20. Zhu, X, Weigel, P, Baloh, J, Nataliansyah, M, Gunn, N, and Mueller, K. Mobilising cross-sector collaborations to improve population health in US rural communities: a qualitative study. BMJ Open. (2019) 9:e030983. doi: 10.1136/bmjopen-2019-030983
21. Shahzad, M, Upshur, R, Donnelly, P, Bharmal, A, Wei, X, Feng, P, et al. A population-based approach to integrated healthcare delivery: a scoping review of clinical care and public health collaboration. BMC Public Health. (2019) 19:708. doi: 10.1186/s12889-019-7002-z
22. Nicholson, K, Makovski, TT, and Stranges, S. The integration of primary care and public health to improve population health: tackling the complex issue of multimorbidity. Int J Public Health. (2019) 64:983–4. doi: 10.1007/s00038-019-01278-1
23. Michener, JL, Castrucci, B, Bradley, DW, Hunter, EL, Thomas, CW, Patterson, C, et al. The practical playbook II: Building multisector partnerships that work. New York, NY: Oxford University Press (2019).
24. McVicar, KL, Ivanitskaya, LV, Bradley, DW, and Montero, JT. Primary care and public health collaboration reports: a qualitative review of integration aims, participants, and success determinants. Popul Health Manag. (2019) 22:422–32. doi: 10.1089/pop.2018.0160
25. Matney, SA, Heale, B, Hasley, S, Decker, E, Frederiksen, B, Davis, N, et al. Lessons learned in creating interoperable fast healthcare interoperability resources profiles for large-scale public health programs. Inform. (2019) 10:087–95. doi: 10.1055/s-0038-1677527
26. Lee, A, Lomazzi, M, Lee, H, and Bedi, R. Integrating oral health with public health systems under the framework of the global charter for the Public's health. Int Dent J. (2019) 69:167–70. doi: 10.1111/idj.12448
27. Hunter, RF, Wickramasinghe, K, Ergüder, T, Bolat, A, Arı, HO, Yıldırım, HH, et al. National action plans to tackle NCDs: role of stakeholder network analysis. BMJ. (2019) 365:l1871. doi: 10.1136/bmj.l1871
28. Gyllstrom, E, Gearin, K, Nease, D Jr, Bekemeier, B, and Pratt, R. Measuring local public health and primary care collaboration: a practice-based research approach. J Public Health Manag Pract. (2019) 25:382–9. doi: 10.1097/PHH.0000000000000809
29. Bhatt, J, Smith, B, Neuhauser, MM, Srinivasan, A, Moore, P, and Hyun, DY. Collaborative solutions to antibiotic stewardship in small community and critical access hospitals. Acad Med. (2019) 94:1419–21. doi: 10.1097/ACM.0000000000002859
30. World Health Organization, United Nations Children's fund (UNICEF). A vision for primary health care in the 21st century: Towards universal health coverage and the sustainable Development goals Geneva: World Health Organization, United Nations Children's fund (UNICEF) (2018).
31. Valaitis, RK, O’Mara, L, Wong, ST, MacDonald, M, Murray, N, Martin-Misener, R, et al. Strengthening primary health care through primary care and public health collaboration: the influence of intrapersonal and interpersonal factors. Prim Health Care Res Dev. (2018) 19:378–91. doi: 10.1017/S1463423617000895
32. The Strengthening Primary Health Care through Primary Care and Public Health Collaboration TeamValaitis, R, Meagher-Stewart, D, Martin-Misener, R, Wong, ST, MacDonald, M, et al. Organizational factors influencing successful primary care and public health collaboration. BMC Health Serv Res. (2018) 18:420. doi: 10.1186/s12913-018-3194-7
33. Piper, CN, Plescia, M, Keener, SR, and DeHaven, M. The Mecklenburg County Interlocal agreement: an 18-year collaboration between medicine and public health. J Public Health Manag Pract. (2018) 24:e1–7. doi: 10.1097/PHH.0000000000000531
34. Oregon Health Authority. CCO 2.0 recommendations of the Oregon health policy board. Portland, OR: Oregon Health Authority (2018).
35. Nuffer, W, Trujillo, T, Harmon, C, and Thompson, M. Engaging with patients in-need through public health partnerships. Innov Pharm. (2018) 9:1–8. doi: 10.24926/iip.v9i2.1055
36. Main, EK, Markow, C, and Gould, J. Addressing maternal mortality and morbidity in California through public-private partnerships. Health Aff. (2018) 37:1484–93. doi: 10.1377/hlthaff.2018.0463
37. Carlton, EL, and Singh, SR. Joint community health needs assessments as a path for coordinating community-wide health improvement efforts between hospitals and local health departments. Am J Public Health. (2018) 108:676–82. doi: 10.2105/AJPH.2018.304339
38. Wong, ST, MacDonald, M, Martin-Misener, R, Meagher-Stewart, D, O’Mara, L, and Valaitis, RK. What systemic factors contribute to collaboration between primary care and public health sectors? An interpretive descriptive study. BMC Health Serv Res. (2017) 17:1–10. doi: 10.1186/s12913-017-2730-1
39. Saunders, C, and Carter, DJ. Is health systems integration being advanced through local Health District planning? Aust Health Rev. (2017) 41:154–61. doi: 10.1071/AH15191
40. Pratt, R, Gyllstrom, B, Gearin, K, Hahn, D, VanRaemdonck, L, Peterson, K, et al. Primary care and public health perspectives on integration at the local level: a multi-state study. J Am Board Fam Med. (2017) 30:601–7. doi: 10.3122/jabfm.2017.05.170034
41. Magee, M, Ali, M, Prabhakaran, D, Ajay, VS, and Narayan, KMV Disease control priorities, third edition (volume 5): Cardiovascular, respiratory, and related disorders. (2017) Washington, DC: World Bank
42. Kao, HY, Ko, HY, Guo, P, Chen, CH, and Chou, SM. Taiwan's experience in hospital preparedness and response for emerging infectious diseases. Health Security. (2017) 15:175–84. doi: 10.1089/hs.2016.0105
43. Gupta, M, Donovan, EF, and Henderson, Z. State-based perinatal quality collaboratives: pursuing improvements in perinatal health outcomes for all mothers and newborns. Semin Perinatol. (2017) 41:195–203. doi: 10.1053/j.semperi.2017.03.009
44. Grumbach, K, Vargas, RA, Fleisher, P, Aragón, TJ, Chung, L, Chawla, C, et al. Achieving health equity through community engagement in translating evidence to policy: the San Francisco health improvement partnership, 2010-2016. Prev Chronic Dis. (2017) 14:E27. doi: 10.5888/pcd14.160469
45. Willis, CD, Greene, JK, Abramowicz, A, and Riley, BL. Strengthening the evidence and action on multi-sectoral partnerships in public health: an action research initiative. Health Promot Chronic Dis Prev Can. (2016) 36:101–11. doi: 10.24095/hpcdp.36.6.01
46. Terranova, E, Tsoi, B, Laraque, F, Washburn, K, and Fuld, J. Strengthening screening for HIV, hepatitis C, and STIs: an innovative partnership between the health department and community health centers in new York City. Public Health Rep. (2016) 131:5–10. doi: 10.1177/00333549161310S102
47. Taylor, E, Bailit, M, Dyer, MB, Bailit Health Purchasing LLC, and Hacker, B. Integrating public health and health care: getting beyond the theory Robert Wood Johnson Foundation (2016) Princeton, NJ: Robert Wood Johnson Foundation.
48. Scutchfield, FD, Prybil, L, Kelly, AV, and Mays, GP. Public health and hospitals: lessons learned from partnerships in a changing health care environment. Am J Public Health. (2016) 106:45–8. doi: 10.2105/AJPH.2015.302938
49. Ramiah, K, Roberson, B, Schrag, J, Susman, K, and Siegel, B. Population health at essential hospitals: findings from moving to action for hospitals and population health. WA, DC: Essential Hospitals Institute (2016).
50. King, RJ, Garrett, N, Kriseman, J, Crum, M, Rafalski, EM, Sweat, D, et al. A community health record: improving health through multisector collaboration, information sharing, and technology. Prev Chronic Dis. (2016) 13:E122. doi: 10.5888/pcd13.160101
51. Guerrero, EG, Andrews, C, Harris, L, Padwa, H, and Kong, Y. Improving coordination of addiction health services organizations with mental health and public health services. J Subst Abus Treat. (2016) 60:45–53. doi: 10.1016/j.jsat.2015.08.002
52. Gosling, R, Davies, SM, and Hussey, JA. How integrating primary care and public health could improve population health outcomes: a view from Liverpool, UK. Public Health Res. (2016) 26:e2611602. doi: 10.17061/phrp2611602
53. Booth, M, Hill, G, Moore, MJ, Dalla, D, Moore, M, and Messenger, A. The new Australian primary health networks: how will they integrate public health and primary care? Public Health Res Pract. (2016) 26:e2611603. doi: 10.17061/phrp2611603
54. Storm, I, van Gestel, A, van de Goor, I, and van Oers, H. How can collaboration be strengthened between public health and primary care? A Dutch multiple case study in seven neighbourhoods. BMC Public Health. (2015) 15:974. doi: 10.1186/s12889-015-2307-z
55. Michener, JL, Koo, D, Castrucci, B, and Sprague, JB. The practical playbook: public health and primary care together. 1st ed (2015).
56. Michelsen, K, Brand, H, Achterberg, P, and Wilkinson, J. Health evidence network Synthesid report: Promoting better integration of health information systems: Best practices and challenges. Copenhagen: World Health Organization (2015).
57. Malcarney, MB, Seiler, N, and Horton, K. Public health laboratories and the affordable care act: what the new health-care system means for public health preparedness. Public Health Rep. (2015) 130:543–6. doi: 10.1177/003335491513000517
58. Lipman, M, and White, J. Collaborative tuberculosis strategy for England. BMJ. (2015) 350:h810. doi: 10.1136/bmj.h810
59. Bowers, K, Carradus, B, Hinkeldey, C, Macek, P, Rettinger, S, Tanner, M, et al. Developing a statewide electronic public health care coordination tracking system. J Pediatr Nurs. (2015) 30:416–20. doi: 10.1016/j.pedn.2014.12.005
60. Zusman, EE, Carr, SJ, Robinson, J, Kasirye, O, Zell, B, Miller, WJ, et al. Moving toward implementation: the potential for accountable care organizations and private-public partnerships to advance active neighborhood design. Prev Med. (2014) 69:S98–S101. doi: 10.1016/j.ypmed.2014.08.009
61. Prybill, L, Scutchfield, FD, Killian, R, Kelly, A, Mays, GP, Carman, A, et al. Improving community health through hospital–public health collaboration: insights and lessons learned from successful partnerships. Lexington, KY: Commonwealth Center for Governance Studies (2014).
62. Price, D, Chan, D, and Greaves, N. Physician surveillance of influenza: collaboration between primary care and public health. Can Fam Physician. (2014) 60:e7–e15.
63. Kempe, A, Albright, K, O'Leary, S, Kolasa, M, Barnard, J, Kile, D, et al. Effectiveness of primary care-public health collaborations in the delivery of influenza vaccine: a cluster-randomized pragmatic trial. Prev Med. (2014) 69:110–6. doi: 10.1016/j.ypmed.2014.08.019
64. Elliott, L, McBride, TD, Allen, P, Jacob, RR, Jones, E, Kerner, J, et al. Health care system collaboration to address chronic diseases: a nationwide snapshot from state public health practitioners. Prev Chronic Dis. (2014) 11:E152. doi: 10.5888/pcd11.140075
65. Caron, RM. Population health management: an approach to improve the integration of the health care and public health systems. Acad Med. (2014) 89:698. doi: 10.1097/ACM.0000000000000227
66. Bruckner, J, and Barr, B. Data-driven population health: collaboration between Macon county public health and community hospitals. N C Med J. (2014) 75:200–1
67. Villanueva, R, Gugel, D, and Dwyer, DM. Collaborating across multiple health care institutions in an urban colorectal cancer screening program. Cancer. (2013) 119:2905–13.23868485. doi: 10.1002/cncr.28153
68. Public Health England. Health and care integration making the case from a public health perspective. London, England: Public Health England (2013).
69. Perry, RE, and Stephenson, C. Improving population health through collaboration and innovation. Popul Health Manag. (2013) 16:S-34–7. doi: 10.1089/pop.2013.0046
70. Norton, WE, Larson, RS, and Dearing, JW. Primary care and public health partnerships for implementing pre-exposure prophylaxis. Am J Prev Med. (2013) 44:S77–9. doi: 10.1016/j.amepre.2012.09.037
71. Millar, J, Bruce, T, Cheng, SM, Masse, R, and McKeown, D. Is public health ready to participate in the transformation of the healthcare system? Healthc Pap. (2013) 13:10–20. doi: 10.12927/hcpap.2014.23689
72. Levesque, JF, Breton, M, Senn, N, Levesque, P, Bergeron, P, Roy, DA, et al. The interaction of public health and primary care: functional roles and organizational models that bridge individual and population perspectives. Public Health Rev. (2013) 35:1–27. doi: 10.1007/BF03391699
73. Hyde, TB, Andrus, JK, Dietz, VJ, Andrus, JK, Hyde, TB, Lee, CE, et al. Critical issues in implementing a national integrated all-vaccine preventable disease surveillance system. Vaccine. (2013) 31:C94–8. doi: 10.1016/j.vaccine.2013.05.034
74. Griswold, KS, Lesko, SE, and Westfall, JM, for the Folsom Group. Communities of solution: partnerships for population health. J Am Board Fam Med. (2013) 26:232–8. doi: 10.3122/jabfm.2013.03.130102
75. Green, ME, Weir, E, Hogg, W, Etches, V, Moore, K, Hunter, D, et al. Improving collaboration between public health and family health teams in Ontario. Healthc Policy. (2013) 8:e93–e104.
76. Varda, DM, and Retrum, JH. An exploratory analysis of network characteristics and quality of interactions among public health Collaboratives. J Public Health Policy. (2012) 1:170–6. doi: 10.4081/jphr.2012.e27
77. Valaitis, R. Strengthening primary health care through primary care and public health collaboration: Final report for the Canadian Health Services Research Foundation (CHSRF). (2012) Washington, DC: Hamilton, ON, Canada: McMaster University.
78. Scutchfield, FD, Michener, JL, and Thacker, SB. Are we there yet? Seizing the moment to integrate medicine and public health. Am J Prev Med. (2012) 42:S97–S102. doi: 10.1016/j.amepre.2012.04.001
79. Saeed, M. Improving the public health/primary care partnership: a perspective from NHS Hounslow. London J Prim Care. (2012) 4:100–3. doi: 10.1080/17571472.2012.11493343
80. Parton, HB, Perlman, SE, Koppaka, R, and Greene, CM. Putting public health into practice: a model for assessing the relationship between local health departments and practicing physicians. Am J Public Health. (2012) 102:S333–5. doi: 10.2105/AJPH.2011.300645
81. Martin-Misener, R, Valaitis, R, Wong, ST, MacDonald, M, Meagher-Stewart, D, Kaczorowski, J, et al. A scoping literature review of collaboration between primary care and public health. Prim Health Care Res Dev. (2012) 13:327–46. doi: 10.1017/S1463423611000491
82. Lebrun, LA, Shi, L, Chowdhury, J, Sripipatana, A, Zhu, J, Sharma, R, et al. Primary care and public health activities in select U.S. health centers. Am J Prev Med. (2012) 42:S191–202. doi: 10.1016/j.amepre.2012.03.011
83. Landon, BE, Grumbach, K, and Wallace, PJ. Integrating public health and primary care systems: potential strategies from an IOM report. JAMA. (2012) 308:461–2. doi: 10.1001/jama.2012.8227
84. Klompas, M, McVetta, J, Lazarus, R, Eggleston, E, Haney, G, Kruskal, BA, et al. Integrating clinical practice and public health surveillance using electronic medical record systems. Am J Prev Med. (2012) 42:S154–62. doi: 10.1016/j.amepre.2012.04.005
85. Institute of Medicine. Primary care and public health: Exploring integration to improve population health. Washington, DC: The National Academies Press (2012).
86. Herwehe, J, Wilbright, W, Abrams, A, Bergson, S, Foxhood, J, Kaiser, M, et al. Implementation of an innovative, integrated electronic medical record (EMR) and public health information exchange for HIV/AIDS. J Am Med Inform Assoc. (2012) 19:448–52. doi: 10.1136/amiajnl-2011-000412
87. Harris, MF, and Harris, E. Partnerships between primary healthcare and population health: preventing chronic disease in Australia. London J Prim Care. (2012) 4:133–7. doi: 10.1080/17571472.2012.11493351
88. Green, LW, Brancati, FL, and Albright, A, The Primary Prevention of Diabetes Working Group. Primary prevention of type 2 diabetes: integrative public health and primary care opportunities, challenges and strategies. Fam Pract. (2012) 29:i13–23. doi: 10.1093/fampra/cmr126
89. Dukers-Muijrers, NH, Somers, C, Hoebe, CJ, Lowe, SH, Niekamp, AMEJWM, Lashof, AO, et al. Improving sexual health for HIV patients by providing a combination of integrated public health and hospital care services; a one-group pre- and post test intervention comparison. BMC Public Health. (2012) 12:1118. doi: 10.1186/1471-2458-12-1118
90. Woulfe, J, Oliver, TR, Zahner, SJ, and Siemering, KQ. Multisector partnerships in population health improvement. Prev Chronic Dis. (2010) 7:A119.
91. Mays, GP, and Scutchfield, FD. Improving public health system performance through multiorganizational partnerships. Prev Chronic Dis. (2010) 7:A116.
92. Karwalajtys, T, and Kaczorowski, J. An integrated approach to preventing cardiovascular disease: community-based approaches, health system initiatives, and public health policy. Risk Manage. (2010) 3:39–48. doi: 10.2147/RMHP.S7528
93. Freeman, E, Presley-Cantrell, L, Edwards, VJ, White-Cooper, S, Thompson, KS, Sturgis, S, et al. Garnering partnerships to bridge gaps among mental health, health care, and public health. Prev Chronic Dis. (2010) 7:A21.
94. Fawcett, S, Schultz, J, Watson-Thompson, J, Fox, M, and Bremby, R. Building multisectoral partnerships for population health and health equity. Prev Chronic Dis. (2010) 7:A118.
95. Breton, M, Levesque, JF, Pineault, R, Lamothe, L, and Denis, J-L. Integrating public health into local healthcare governance in Quebec: challenges in combining population and organization perspectives. Healthc Policy. (2009) 4:e159–78.
96. Robert Wood Johnson Foundation. Turning point: Collaborating for a new century in public health: An RWJF national program. Princeton, NJ: Robert Wood Johnson Foundation (2008).
97. Berwick, DM, Nolan, TW, and Whittington, J. The triple aim: care, health, and cost. Health Aff. (2008) 27:759–69. doi: 10.1377/hlthaff.27.3.759
98. Stevenson Rowan, M, Hogg, W, and Huston, P. Integrating public health and primary care. Healthc Policy. (2007) 3:e160–81.19305749.
99. Nicola, RM. Turning Point's National Excellence Collaboratives: assessing a new model for policy and system capacity development. J Public Health Manag Pract. (2005) 11:101–8. doi: 10.1097/00124784-200503000-00002
100. Lyons, MS, Lindsell, CJ, Ledyard, HK, Frame, PT, and Trott, AT. Health department collaboration with emergency departments as a model for public health programs among at-risk populations. Public Health Rep. (2005) 120:259–65. doi: 10.1177/003335490512000307
101. Given, LS, Black, B, Lowry, G, Huang, P, and Kerner, JF. Collaborating to conquer cancer: a comprehensive approach to cancer control. Cancer Causes Control. (2005) 16:3–14. doi: 10.1007/s10552-005-0499-8
102. Ciliska, D, Ehrlich, A, and DeGuzman, A. Public health and primary care: challenges and strategies for collaboration. Ontario: McMaster University (2005).
103. Bradley, S, and McKelvey, SD. General practitioners with a special interest in public health; at last a way to deliver public health in primary care. J Epidemiol Community Health. (2005) 59:920–3. doi: 10.1136/jech.2005.034405
104. Padgett, SM, Bekemeier, B, and Berkowitz, B. Collaborative partnerships at the state level: promoting systems changes in public health infrastructure. J Public Health Manag Pract. (2004) 10:251–7. doi: 10.1097/00124784-200405000-00009
105. Iliffe, S, and Lenihan, P. Integrating primary care and public health: learning from the community-oriented primary care model. Int J Health Serv. (2003) 33:85–98. doi: 10.2190/40HL-U1B9-F7K7-KK64
106. Sabol, B. Innovations in collaboration for the public's health through the turning point initiative: the W.K. Kellogg Foundation perspective. J Public Health Manag Pract. (2002) 8:6–12. doi: 10.1097/00124784-200201000-00003
107. Hill, A, Levitt, C, Chambers, LW, Cohen, M, and Underwood, J. Primary care and population health promotion: collaboration between family physicians and public health units in Ontario. Can Fam Physician. (2001) 47:22–5.
108. Halverson, PK, Mays, GP, and Kaluzny, AD. Working together? Organizational and market determinants of collaboration between public health and medical care providers. Am J Public Health. (2000) 90:1913–6. doi: 10.2105/ajph.90.12.1913
109. Cohen, NL, and Perl, S. A managed care/public health partnership: opportunities in new York City's Medicaid program. J Urban Health. (2000) 77:663–6. doi: 10.1007/BF02344029
110. Winkelman, TNA, Margolis, KL, Waring, S, Bodurtha, PJ, Khazanchi, R, Gildemeister, S, et al. Minnesota electronic health record consortium COVID-19 project: informing pandemic response through statewide collaboration using observational data. Public Health Rep. (2022) 137:263–71. doi: 10.1177/00333549211061317
111. Trust for America's Health. Ready or not: protecting the Public's health from diseases, Disasters, and Bioterrorism. Washington, DC: Trust for America's Health (2022).
112. Mitchell, AM, Rigler, J, and Baum, K. Regional transfer coordination and hospital load balancing during COVID-19 surges. JAMA Health Forum. (2022) 4:e215048. doi: 10.1001/jamahealthforum.2021.5048
113. Lim, SM, Allard, NL, Devereux, J, Cowie, BC, Tydeman, M, Miller, A, et al. The COVID positive pathway: a collaboration between public health agencies, primary care, and metropolitan hospitals in Melbourne. Med J Aust. (2022) 216:413–9. doi: 10.5694/mja2.51449
114. Lee, P, Abernethy, A, Shaywitz, D, Gundlapalli, AV, Weinstein, J, Doraiswamy, PM, et al. Digital health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. (2022) 2022:10.31478/202201c. doi: 10.31478/202201c
115. Upton, AL, and Denham, MA. Building resilient coalitions: health and medical response through COVID-19 concurrent events. WIT Trans Built Environ. (2022) 207:27–45. doi: 10.2495/dman210031
116. Koch, A, Bohn, J, Corvin, J, and Seaberg, J. Maturing into high-functioning health-care coalitions: a qualitative Nationwide study of emergency preparedness and response leadership. Disaster Med Public Health Prep. (2023) 17:1–9. doi: 10.1017/dmp.2022.13
117. Fleisher, LA, Schreiber, M, Cardo, D, and Srinivasan, A. Health care safety during the pandemic and beyond—building a system that ensures resilience. N Engl J Med. (2022) 386:609–11.35148040. doi: 10.1056/NEJMp2118285
118. Aristei, L, D’Ambrosio, F, Villani, L, Rossi, MF, Daniele, A, Amantea, C, et al. Public health regulations and policies dealing with preparedness and emergency management: the experience of the COVID-19 pandemic in Italy. Int J Environ Res Public Health. (2022) 19:1091. doi: 10.3390/ijerph19031091
119. World Health Organization. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond. Geneva: World Health Organization (2021).
120. Woodworth, KR, Reynolds, MR, Burkel, V, Gates, C, Eckert, V, McDermott, C, et al. A preparedness model for mother-baby linked longitudinal surveillance for emerging threats. Matern Child Health J. (2021) 25:198–206. doi: 10.1007/s10995-020-03106-y
121. Veenema, TG, Waldhorn, R, Toner, E, Adalja, AA, Kobokovich, A, Martin, E, et al. Integrating primary care and public health to save lives and improve practice during public health crises: lessons from COVID-19. Baltimore, MD: Johns Hopkins Center for Health Security (2021).
122. U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for preparedness and response (ASPR) technical resources AC, and information exchange (TRACIE). Healthcare Coalition Engagement in COVID-19 Assessment (2021) Washington, DC: United States Department of Health & Human Services.
123. Sales, C, Kim, Y, Kim, G, Lin, B, and Palaniappan, L. Precision public health matters: an international assessment of communication, preparedness, and coordination for successful COVID-19 responses. Am J Public Health. (2021) 111:392–4. doi: 10.2105/AJPH.2020.306129
124. Noknoy, S, Kassai, R, Sharma, N, Nicodemus, L, Canhota, C, and Goodyear-Smith, F. Integrating public health and primary care: the response of six Asia-Pacific countries to the COVID-19 pandemic. Br J Gen Pract. (2021) 71:326–9.34319893. doi: 10.3399/bjgp21X716417
125. McClellan, M, Rajkumar, R, Couch, M, Holder, D, Pham, M, Long, P, et al. Health care payers COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. (2021) 2021:10.31478/202105a. doi: 10.31478/202105a
126. Lenert, LA, Ding, W, and Jacobs, J. Informatics for public health and health system collaboration: applications for the control of the current COVID-19 pandemic and the next one. J Am Med Inform Assoc. (2021) 28:1807–11. doi: 10.1093/jamia/ocab066
127. Kinder, K, Bazemore, A, Taylor, M, Mannie, C, Strydom, S, George, J, et al. Integrating primary care and public health to enhance response to a pandemic. Prim Health Care Res Dev. (2021) 22:e27. doi: 10.1017/S1463423621000311
128. Izagirre-Olaizola, J, Hernando-Saratxaga, G, and Aguirre-Garcia, MS. Integration of health care in the Basque Country during COVID-19: the importance of an integrated care management approach in times of emergency. Prim Health Care Res Dev. (2021) 22:e39. doi: 10.1017/S146342362100044X
129. Ham, C. A national infrastructure plan for the NHS, social care, and public health is needed to build resilience for the future. BMJ. (2021) 375:n3029. doi: 10.1136/bmj.n3029
130. Haldane, V, de Foo, C, Abdalla, SM, Jung, AS, Tan, M, Wu, S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. (2021) 27:964–80. doi: 10.1038/s41591-021-01381-y
131. Gesser-Edelsburg, A, Cohen, R, and Diamant, A. Experts' views on the gaps in public health emergency preparedness in Israel: a qualitative case study. Disaster Med. (2021) 15:34–41. doi: 10.1017/dmp.2019.115
132. Fraser, MR, Barishansky, RM, and Blumenstock, JS. Twenty years after 9/11: the public health preparedness we need now. Am J Public Health. (2021) 111:1562–4. doi: 10.2105/AJPH.2021.306459
133. Filippini, T, and Vinceti, SR. Italian National Recovery and resilience plan: a healthcare renaissance after the COVID-19 crisis? Acta Biomed Ateneo Parmense. (2021) 92:e2021463. doi: 10.23750/abm.v92iS6.12339
134. Duchen, R, Iskander, C, Chung, H, Paterson, J, Kwong, J, Bronskill, S, et al. The role of a resilient information infrastructure in COVID-19 vaccine uptake in Ontario. Healthc Q. (2021) 24:7–11. doi: 10.12927/hcq.2021.26553
135. Ding, A. Full commitment by our AMA to the betterment and strengthening of public health systems (resolution 401-JUN-21) American Medical Association; (2021) Available from https://www.ama-assn.org/system/files/n21-csaph02.pdf
136. DeSalvo, K, Hughes, B, Bassett, M, Benjamin, G, Fraser, M, Galea, S, et al. Public health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. (2021) 2021. doi: 10.31478/202104c
137. Dawson, WD, Boucher, NA, Stone, R, and van Houtven, CH. COVID-19: the time for collaboration between long-term services and supports, health care systems, and public health is now. Milbank Q. (2021) 99:565–94. doi: 10.1111/1468-0009.12500
138. Daszak, P, Keusch, GT, Phelan, AL, Johnson, CK, and Osterholm, MT. Infectious disease threats: a rebound to resilience. Health Aff. (2021) 40:204–11. doi: 10.1377/hlthaff.2020.01544
139. Czabanowska, K, and Kuhlmann, E. Public health competences through the lens of the COVID-19 pandemic: what matters for health workforce preparedness for global health emergencies. Int J Health Plann Manag. (2021) 36:14–9. doi: 10.1002/hpm.3131
140. Craven, M, Sabow, A, Van der Veken, L, et al. Not the last pandemic: investing now to reimagine public-health systems. New York, NY: McKinsey & Company (2021).
141. Clancy, C, Goodrich, K, Moody-Williams, J, Sheares, KD, O’Kane, ME, Cha, S, et al. Quality, safety, and standards organizations COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. Washington, DC: National Academy of Medicine (2021) doi: 10.31478/202107d
142. Bipartisan Policy Center. Positioning America's public health system for the next pandemic. (2021) Washington, DC: Bipartisan Policy Center.
143. Beck, AF, Hartley, DM, Kahn, RS, Taylor, SC, Bishop, E, Rich, K, et al. Rapid, bottom-up Design of a Regional Learning Health System in response to COVID-19. Mayo Clin Proc. (2021) 96:849–55.33714596. doi: 10.1016/j.mayocp.2021.02.006
144. Balser, J, Ryu, J, Hood, M, Kaplan, G, Perlin, J, and Siegel, B. Care systems COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. (2021) 2021. doi: 10.31478/202104d
145. Tracie, A. Washington medical coordination center collaborates with key health care response partners to mitigate hospital surge and ensure continuity of care during the COVID-19 pandemic. (2022). Available at: https://aspr.hhs.gov/HealthCareReadiness/StoriesfromtheField/Pages/Stories/WA-HospitalSurge-March2020.aspx (Accessed May, 2022).
146. Ros, F, Kush, R, Friedman, C, Gil Zorzo, E, Rivero Corte, P, Rubin, JC, et al. Addressing the Covid-19 pandemic and future public health challenges through global collaboration and a data-driven systems approach. Learn Health Sys. (2021) 5:e10253. doi: 10.1002/lrh2.10253
147. National Academies of Sciences Engineering and Medicine. Evidence-based practice for public health emergency preparedness and response. Washington, DC: The National Academies Press (2020).
148. Lal, A, Ashworth, HC, Dada, S, Hoemeke, L, and Tambo, E. Optimizing pandemic preparedness and response through health information systems: lessons learned from Ebola to COVID-19. Disaster Med Public Health Prep. (2022) 16:333–40. doi: 10.1017/dmp.2020.361
149. Ippolito, G, Lauria, FN, Locatelli, F, Magrini, N, Montaldo, C, Sadun, R, et al. Lessons from the COVID-19 pandemic-unique opportunities for unifying, revamping and reshaping epidemic preparedness of Europe's public health systems. Int J Infect Dis. (2020) 101:361–6. doi: 10.1016/j.ijid.2020.10.094
150. He, R, Zhang, J, Mao, Y, Degomme, O, and Zhang, WH. Preparedness and responses faced during the COVID-19 pandemic in Belgium: an observational study and using the National Open Data. Int J Environ Res Public Health. (2020) 17:7985. doi: 10.3390/ijerph17217985
151. Clay-Williams, R, Rapport, F, and Braithwaite, J. The Australian health system response to COVID-19 from a resilient health care perspective: what have we learned? Public Health Res. (2020) 30:09. doi: 10.17061/phrp3042025
152. Chen, Z, Cao, C, and Yang, G. Coordinated multi-sectoral efforts needed to address the COVID-19 pandemic: lessons from China and the United States. Glob health. Res Policy. (2020) 5:22. doi: 10.1186/s41256-020-00150-7
153. Cerise, FP, Moran, B, Huang, PP, and Bhavan, KP. The imperative for integrating public health and health care delivery systems. NEJM Catalyst. (2021) 2:580. doi: 10.1056/CAT.20.0580
154. Calonge, N, Brown, L, and Downey, A. Evidence-based practice for public health emergency preparedness and response: recommendations from a National Academies of sciences, engineering, and medicine report. JAMA. (2020) 324:629–30. doi: 10.1001/jama.2020.12901
155. Berwick, DM, and Shine, K. Enhancing private sector health system preparedness for 21st-century health threats: foundational principles from a National Academies Initiative. JAMA. (2020) 323:1133–4. doi: 10.1001/jama.2020.1310
156. Barnett, DJ, Knieser, L, Errett, NA, Rosenblum, AJ, Seshamani, M, and Kirsch, TD. Reexamining health-care coalitions in light of COVID-19. Disaster Med Public Health Prep. (2020) 16:859–63. doi: 10.1017/dmp.2020.431
157. ASPR TRACIE. Medical operations coordination cells toolkit. Washington, DC: Hospital Team (2020).
158. Office of the Assistant Secretary for Preparedness and Response, US Department of Health and Human Services. National Health Security Strategy: 2019–2022. (2019) Washington, DC: United States Department of Health & Human Services.
159. Nuzzo, JB, Meyer, D, Snyder, M, Ravi, SJ, Lapascu, A, Souleles, J, et al. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health. (2019) 19:1310. doi: 10.1186/s12889-019-7707-z
160. Mwaungulu, GS Jr, and Dwyer, KS. Responding to public health emergencies at the local level: administrative preparedness challenges, strategies, and resources. J Law Med Ethics. (2019) 47:72–5. doi: 10.1177/1073110519857322
161. Meyer, D, Kirk Sell, T, Schoch-Spana, M, Shearer, MP, Chandler, H, Thomas, E, et al. Lessons from the domestic Ebola response: improving health care system resilience to high consequence infectious diseases. Am J Infect Control. (2018) 46:533–7. doi: 10.1016/j.ajic.2017.11.001
162. Madad, S, Tate, A, Rand, M, Quinn, C, Vora, NM, Allen, M, et al. Zika virus preparedness and response efforts through the collaboration between a health care delivery system and a local public health department. Disaster Med Public Health Prep. (2018) 12:689–91. doi: 10.1017/dmp.2018.5
163. Kinsman, J, Angrén, J, Elgh, F, Furberg, M, Mosquera, PA, Otero-García, L, et al. Preparedness and response against diseases with epidemic potential in the European Union: a qualitative case study of Middle East respiratory syndrome (MERS) and poliomyelitis in five member states. BMC Health Serv Res. (2018) 18:528. doi: 10.1186/s12913-018-3326-0
164. Khan, Y, O’Sullivan, T, Brown, A, Tracey, S, Gibson, J, Généreux, M, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health. (2018) 18:1344. doi: 10.1186/s12889-018-6250-7
165. Jha, A, Lin, L, Short, SM, Argentini, G, Gamhewage, G, and Savoia, E. Integrating emergency risk communication (ERC) into the public health system response: systematic review of literature to aid formulation of the 2017 WHO guideline for ERC policy and practice. PLoS One. (2018) 13:e0205555. doi: 10.1371/journal.pone.0205555
166. Baseman, J, Revere, D, Karasz, H, and Allan, S. Implementing innovations in Public Health Agency preparedness and response programs. Am J Public Health. (2018) 108:S369–71. doi: 10.2105/AJPH.2018.304795
167. Swift, MD, Aliyu, MH, Byrne, DW, Qian, K, McGown, P, Kinman, PO, et al. Emergency preparedness in the workplace: the Flulapalooza model for mass vaccination. Am J Public Health. (2017) 107:S168–76. doi: 10.2105/AJPH.2017.303953
168. Smith, S, Sibal, B, Linnane, J, and Mittal, A. NHS and public health reorganization in England: health protection and emergency planning, preparedness and response perspective. J Public Health. (2016) 39:fdw042–6. doi: 10.1093/pubmed/fdw042
169. Fitzgerald, TJ, Kang, Y, Bridges, CB, Talbert, T, Vagi, SJ, Lamont, B, et al. Integrating pharmacies into public health program planning for pandemic influenza vaccine response. Vaccine. (2016) 34:5643–8. doi: 10.1016/j.vaccine.2016.09.020
170. Department of Health and Human Services, Office of the Assistant Secretary for preparedness and response. 2017–2022 health care preparedness and response capabilities. (2016) Washington, DC: United States Department of Health & Human Services.
171. Agency FEM. Emergency support function #8 – Public health and medical services annex. (2016) Washington, DC: United States Department of Homeland Security. Available at https://www.fema.gov/sites/default/files/2020-04/NRF_FINALApproved_2011028.pdf
172. Hinton, CF, Griese, SE, Anderson, MR, Chernak, E, Peacock, G, Thorpe, PG, et al. CDC grand rounds: addressing preparedness challenges for children in public health emergencies. MMWR Morb Mortal Wkly Rep. (2015) 64:972–4.26356838. doi: 10.15585/mmwr.mm6435a3
173. Rubin, SE, Schulman, RM, Roszak, AR, Herrmann, J, Patel, A, and Koonin, LM. Leveraging partnerships among community pharmacists, pharmacies, and health departments to improve pandemic influenza response. Biosecur Bioterror. (2014) 12:76–84. doi: 10.1089/bsp.2013.0082
174. Otomo, Y, and Burkle, FM. Breakout session 1 summary: frameworks and policies relating to medical preparedness and health management in disasters. Disaster Med. (2014) 8:359–60. doi: 10.1017/dmp.2014.72
175. Wynn, A, and Moore, KM. Integration of primary health care and public health during a public health emergency. Am J Public Health. (2012) 102:e9–e12. doi: 10.2105/AJPH.2012.300957
176. Veltri, K, Yaghdjian, V, Morgan-Joseph, T, Prlesi, L, and Rudnick, E. Hospital emergency preparedness: push-POD operation and pharmacists as immunizers. J Am Pharm Assoc. (2012) 52:81–5. doi: 10.1331/JAPhA.2012.11191
177. Pfefferbaum, B, Schonfeld, D, Flynn, BW, Norwood, AE, Dodgen, D, Kaul, RE, et al. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med Public Health Prep. (2012) 6:67–71. doi: 10.1001/dmp.2012.2
178. Markiewicz, M, Bevc, CA, Hegle, J, Horney, JA, Davies, M, and MacDonald, PDM. Linking public health agencies and hospitals for improved emergency preparedness: North Carolina's public health epidemiologist program. BMC Public Health. (2012) 12:141. doi: 10.1186/1471-2458-12-141
179. Stroud, C, Altevogt, BM, Butler, JC, and Duchin, JS. The Institute of Medicine's forum on medical and public health preparedness for catastrophic events: regional workshop series on the 2009 H1N1 influenza vaccination campaign. Disaster Med Public Health Prep. (2011) 5:81–6. doi: 10.1001/dmp.2011.3
180. Ginter, PM, Rucks, AC, Duncan, WJ, Wingate, MS, Beeman, SK, Reeves, J, et al. Southeastern regional pediatric disaster surge network: a public health partnership. Public Health Rep. (2010) 125:117–26. doi: 10.1177/00333549101250S516
181. Stroud, C, Altevogt, BM, and Goldfrank, LR. Institute of Medicine's forum on medical and public health preparedness for catastrophic events: activities and goals. Disaster Med. (2009) 3:183–5. doi: 10.1097/DMP.0b013e3181be99fc
182. Stalker, SA, Weir, E, Vessel, SL, and Mikail, J. Planning a coordinated local health care system response to a pandemic using an accelerated Delphi technique: phase 1. Can J Public Health. (2009) 100:65–9. doi: 10.1007/BF03405496
183. Nelson, C, Lurie, N, Wasserman, J, and Zakowski, S. Conceptualizing and defining public health emergency preparedness. Am J Public Health. (2007) 97:S9–S11. doi: 10.2105/AJPH.2007.114496
184. Braun, BI, Wineman, NV, Finn, NL, Barbera, JA, Schmaltz, SP, and Loeb, JM. Integrating hospitals into community emergency preparedness planning. Ann Intern Med. (2006) 144:799–811. doi: 10.7326/0003-4819-144-11-200606060-00006
185. Gerberding, JL, Hughes, JM, and Koplan, JP. Bioterrorism preparedness and response: clinicians and public health agencies as essential partners. JAMA. (2002) 287:898–900. doi: 10.1001/jama.287.7.898
186. Harish, V. The Syndemics of emergency: how COVID-19 demands a holistic view of public health promotion and preparedness. Am J Public Health. (2021) 111:353–4. doi: 10.2105/AJPH.2020.306116
187. Bipartisan Policy Center. Public health forward: Modernizing the U.S. public health system. Washington, D.C.: Bipartisan Policy Center (2021).
188. Brownson, RC, Burke, TA, Colditz, GA, and Samet, JM. Reimagining public health in the aftermath of a pandemic. Am J Public Health. (2020) 110:1605–10. doi: 10.2105/AJPH.2020.305861
189. Fraser, M, and Castrucci, B. Beyond the status quo: 5 strategic moves to position state and territorial public health agencies for an uncertain future. J Public Health Manag Pract. (2017) 23:543–51. doi: 10.1097/PHH.0000000000000634
190. DeSalvo, K, Wang, YC, Harris, A, Auerbach, J, Koo, D, and O’Carroll, P. Public health 3.0: a call to action for public health to meet the challenges of the 21st century. Prev Chronic Dis. (2017) 14:E78. doi: 10.5888/pcd14.170017
Keywords: public health, health care, integration, policy, review
Citation: Lin JS, Webber EM, Bean SI, Martin AM and Davies MC (2023) Rapid evidence review: Policy actions for the integration of public health and health care in the United States. Front. Public Health. 11:1098431. doi: 10.3389/fpubh.2023.1098431
Edited by:
Jose M. Martin-Moreno, University of Valencia, SpainReviewed by:
Christopher Mierow Maylahn, New York State Department of Health, United StatesCopyright © 2023 Lin, Webber, Bean, Martin and Davies. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer S. Lin, amVubmlmZXIucy5saW5Aa3BjaHIub3Jn
 Jennifer S. Lin
Jennifer S. Lin Elizabeth M. Webber
Elizabeth M. Webber