- 1School of Social Development, East China University of Political Science and Law, Shanghai, China
- 2Rory Meyer College of Nursing, New York University, New York, NY, United States
- 3School of Customs and Public Administration, Shanghai Customs College, Shanghai, China
- 4School of Sociology and Political Science, Shanghai University, Shanghai, China
Background: Internal migrants are exposed to higher risks of depressive symptoms due to migration-related stress. It has been recognized that perceived neighborhood social cohesion has direct and indirect associations with depressive symptoms. However, the pathway from perceived social cohesion to internal migrants' depressive symptoms was less discussed.
Objectives: To assess mental health disparities among internal migrants. To investigate the association between social cohesion and depressive symptoms among urban-to-urban and rural-to-urban migrants and to examine the mediating role of social adaptation.
Methods: Data from the “2017 Urbanization and New Migrant Survey” was used, including 2,584 internal migrants age 18–65 from 10 cities in China. Social cohesion was measured by a six-item modified Community-level Cohesion Scale. Depressive symptoms was measured using the Center for Epidemiological Studies Depression Scale, and social adaptation was assessed by a single-item question of migrants' adaptation to local life. Multivariate linear regression models were used to examine the association between social cohesion and depressive symptoms. Baron and Kenny's mediation tests were conducted to examine the mediating role of social adaptation on the association. All analyses were adjusted using sampling weights to account for this survey's sampling design.
Results: Rural-to-urban migrants were found to have more clinically significant depressive symptoms, lower perceived social cohesion, and fair or low social adaptation than urban-to-urban migrants (all p < 0.001). Being rural-to-urban migrants as compared with urban-to-urban migrants [Odds Ratio (OR) = 1.46, 95% Confidence Interval (CI) = 1.456, 1.461, p < 0.001], had lower perceived social cohesion (OR = 1.46, 95% CI = 1.458, 1.463, p < 0.001), and poorer social adaptation (OR = 1.94, 95% CI = 1.932, 1.941, p < 0.001), are associated with higher odds of having clinically significant depressive symptoms. Social adaptation partially mediated the association between social cohesion and depressive symptoms by explaining 15.39% of its effect for urban-to-urban migrants and 18.97% for rural-to-urban migrants.
Conclusions: Findings from this study reveal mental health inequalities among internal migrants and demonstrate the importance of social adaption on the association between social cohesion and depressive symptoms. Social strategies and public policies are needed to build a more cohesive community that serves both local residents and internal migrants, especially rural-to-urban migrants.
Introduction
Depressive symptoms are common mental health problems among migrants in many countries. This issue could be exacerbated due to an increase in the migrant population around the world (1). Internal migrants are individuals who migrate between regions within one country (2). Due to China's economic development since 1978, internal migrants have increased dramatically. Internal migrants reached 244 million in 2017, accounting for more than 17.5% of the total population (3). For migrants, depressive symptoms are especially associated with their intention to settle in the host place (4). However, the mental health status of internal migrants did not receive much attention (5, 6).
Increasing evidence suggests that migrants experience higher levels of depressive symptoms than native-born residents (7–10) because of migration-related changes, such as separation from family, reducing size in social support, and weakened social ties (11). In China, migration has been regarded as a stressful process (10, 12). For migrants, due to the housing registration system (i.e., Hukou) that limits their access to employment, education, housing, and health insurance (13, 14), they are more likely to be exposed to social stress and social exclusion (6, 11, 12, 15) that may lead to a higher level of depressive symptoms. There are two major internal migration patterns in China: one is from rural-to-urban migration and the other from urban-to-urban migration (16). However, most previously studies that examined mental health status were only focused on rural-to-urban migrants (5, 11, 17, 18).
In addition, it has long been recognized that individual and family level social factors, such as family socioeconomic status, social capital, and social support, have direct relationships with depressive symptoms (19–24), while little attention has been paid on the role of social cohesion, as a community-level social factor that is associated with depressive symptoms among internal migrants. Social cohesion indicates the inclusion and integration of a community (25, 26). As an important environmental factor, social cohesion is related to individuals' psychological wellbeing (27, 28). In a migrant community, social cohesion has an impact on internal migrants' positive interactions including obtaining social support and help, or negative interactions such as suffering from social stress and/or exclusion from native-born residents. However, little attention has been paid to the association of social cohesion, as a community-level social factor, with depressive symptoms among internal migrants in China.
The rapid increase of the migration population, intertwined with dramatic social transition, suggests that Chinese society has reached a critical stage in mental health care challenges. Nevertheless, little is known about how social environmental context, beyond intra-personal factors, affects depressive symptoms among internal migrants in China. To address these knowledge gaps, this study aims to investigate the association between social cohesion and depressive symptoms among urban-to-urban and rural-to-urban migrants and to examine the mediating role of social adaptation, using the data drawn from the “2017 Urbanization and New Migrant Survey,” a large-scale sample with 2,584 internal migrants from 10 cities in China. Gaining a better understanding of the pathways would provide a better knowledge on community-level social factors that are associated with depressive symptoms and help develop social strategies and public policies in addressing mental health issues among migrant population.
Literature review
Social inequalities: Disparities in depressive symptoms within migrants
When studying the migrant-related health disparities, scholars often use a native-born population in the host society as the reference group. Most of the studies demonstrated that migrants had poorer mental health, e.g., depressive symptoms, than native-born residents (6, 11, 29, 30). Depressive symptoms may lead to a series of complications that affect individual's quality of life and cause other critical health issues such as suicide, frailty, functional disability, and mortality (31–33). For migrants (including both international and internal migrants), depressive symptoms are also associated with their intention to settle down in the host place (4).
However, most studies on health outcomes in China only focused on the rural-to-urban migrants (6, 11, 17, 18). These studies suggest that there are significant mental health disparities within migrants. Furthermore, more information about migration status, e.g., the housing registration status of migrants, and reasons for migration, should be considered when examining the mental health disparities among migrants. In China, the most important characteristic that distinguishes the patterns of migration from those in other countries is the housing registration system (Hukou system) (13, 34). Since Hukou is linked with entitlement and benefits for individuals, whether migrants come from urban or rural is an indicator for their education background, financial status, and social support (13, 34–36), which may result in different mental health outcomes, such as depressive symptoms. To assess disparities in depressive symptoms among migrants, we proposed the following hypothesis:
Hypothesis 1: Rural-to-urban migrants are more likely to have a higher level of depressive symptoms than urban-to-urban migrants.
Social cohesion in reducing depressive symptoms
There is no doubt that environmental context plays a crucial role in shaping psychological wellbeing (27, 37, 38). When investigating risk and protective factors for depressive symptoms of migrants, it is likely that community-level factors are at play.
It is well-recognized that individual and neighborhood-level factors, such as neighborhood socioeconomic status, social capital, and social support, have strong associations with residents' depressive symptoms (19–22, 37–43). A related concept of particular importance to the migrant community is social cohesion (27, 44). Social cohesion refers to communal bonds characterized by altruism, reciprocity, and shared norms and values (27). It generates mutual trust and support, collective efficacy, and a sense of belonging, which are all conducive to improved mental health (27, 45). Previous studies show that social cohesion was defined as a neighborhood-level factor, and lower neighborhood social cohesion was linked to a variably of health outcomes, such as depression and mortality (46–52).
Neighborhood social cohesion is the network of relationships, shared values, and norms of residents in a neighborhood and it shares some similarities to an individual's social network (53). Social cohesion, however, exists in a larger field. It accounts for value systems, degree of social interaction, and considers the cohesion of a broader community rather than cohesion within a neighborhood or a small group of individuals. However, little attention has been paid to the association of social cohesion, as a community-level social factor, with depressive symptoms among internal migrants in China. In a migrant community, social cohesion refers to the quality of social interactions which is closely related to individuals' mental health status (11, 20, 22, 41, 54). In a more cohesive community, migrants may feel a stronger sense of inclusion. Social cohesion has an impact on internal migrants' positive interactions including obtaining social support and help, or negative interactions such as suffering from social stress and/or exclusion from native-born residents. In a community where native-born residents and migrants trust each other, they will have more social connections and interactions. For migrants, the trust they have built will make it easier for them to establish new social ties and social networks that are important to adapt to a new life and maintain a good psychological status (20, 21, 42). In addition, a higher level of social cohesion would lead to less social stress or social exclusion, which may result in fewer depressive symptoms (6, 11, 12). Furthermore, in a well-integrated community, native-born residents and migrants are more likely to provide mutual social support, which is a protective factor against depressive symptoms (22, 41). Even if some migrants suffer from depressive symptoms, they are more likely to be able to receive timely assistance in a more cohesive community. To investigate the associations between social cohesion and depressive symptoms of both urban-to-urban and rural-to-urban migrants, here is the second hypothesis:
Hypothesis 2: A lower level of perceived social cohesion is associated with more depressive symptoms among both urban-to-urban and rural-to-urban migrants.
Social adaptation: Pathways from social cohesion to depressive symptoms
Although recent studies have shown the correlation between social cohesion and health outcomes (49, 50, 52, 55, 56), limited studies have been conducted to examine the mediating role of social adaptation on the association between social cohesion and migrants' mental health. Increasing attention has been paid to improve social adaptation as an effort to improve individual's mental health (57, 58). Social adaptation concerns the interactions between an individual and the environment. It refers to the performance in the activities of daily intercultural living (59) and involves the intercultural competence with emphasis on behavioral domains. As an important indicator of migrants' integration into the host community, social adaptation would mediate the pathways from social cohesion to depressive symptoms. Individual's allostatic load would be lower in a highly cohesive community where internal migrants have more positive interactions with local residents and a higher sense of being trusted and belonging, Individuals are more likely to “doing well” in the activities of daily intercultural living in the host city (59). Additionally, “doing well” in social adaptation may help buffer the effects of social stress and social exclusion they may face in the migration process (6, 11, 12); thus, avoiding the occurrence of psychological disorders. Therefore, no such studies have been conducted to examine whether social adaptation is a factor that could mediate between social cohesion and depressive symptoms. Thus, we propose the following hypothesis:
Hypothesis 3: Social adaptation mediates the association between social cohesion and depressive symptoms for both urban-to-urban and rural-to-urban migrants.
Methods
Data source and study sample
Data were drawn from the “2017 Urbanization and New Migrant Survey,” a cross-sectional survey focusing on policy issues such as population migration, social mobility, and social integration in Chinese adults. A multi-stage stratified sampling strategy was used, and data were collected from 10 cities in China, including economically developed cities (GDP per capita of is more than 100,000 RMB), such as Zhengzhou, Tianjin, Xiamen, Guangzhou, and Changsha, and less developed ones (GDP per capita of is <100,000 RMB), including Harbin, Changchun, Yanji, Shenyang, and Anshan. Data were collected during in-home interviews by well-trained interviewers. Inclusion criteria for participation were: (1) full-time residence in this city >6 months in the past year; (2) aged 18–65 years; and (3) capable of communicating answers to interview questions and giving consent.
A sample of 2,752 adult internal migrants (i.e., the movement of people between usual residences within national states) were drawn from the survey data. After excluding 168 adults with missing values, the final analytical sample consisted of 2,584 internal migrants. Among them, 1,152 reported living in another urban area before moving to their current locations, defined as urban-to-urban migrants, and 1,432 reported living in a rural area before moving to their current locations, defined as rural-to-urban migrants.
Measures
Dependent variables: Depressive symptoms
Depressive symptoms were measured using the original 20-item version of the Center for Epidemiological Studies Depression Scale (CES-D), a widely used screening measure for depressive symptoms (60). The CES-D assesses how often a person has experienced symptoms of depression, such as restless sleep, poor appetite, and feeling lonely over the past week. Each scale item is scored from 0 to 3, with a higher score representing greater depressive symptom severity. The potential range of the scale is 0–60. A cut-off score of 16 or higher is generally used to determine clinically significant depressive symptoms (61). The Cronbach's alpha for the total scale was 0.873, indicating favorable internal-consistency.
Independent variables: Social cohesion
The concept of perceived social cohesion in this study focuses on native-born residents' intergroup relationships with internal migrants. It refers to whether internal migrants could perceive a high or low sense of being welcomed and trusted by local residents or belonging to the community (62). With reference to the neighborhood-level cohesion scale (63–65), we generated a summary variable based on six questions, including “How much do you think native-born people are willing to (1) work with you; (2) talk with you; (3) be your neighbors; (4) make friends with you; (5) be your relatives; (6) manage the community together with you?” Each item was scored 1–5, 1 = very unwilling to, 2 = unwilling to, 3 = fair, 4 = willing to, and 5 = very willing to, with lower values representing lower perceived social cohesion. The potential range of the scale is 0–30. The six items showed good internal consistency in this study (Cronbach's α = 0.929). Considering that the median score on the social cohesion scale was 24, we then dichotomized the variable, with scores below 24 indicating a low perception of social cohesion.
Mediating variables: Social adaptation
Social adaptation was assessed based on the single-item question: “How much do you think you have adapted to local life?” The five-point response to this question—very poor, poor, fair, good, and very good—was then dichotomized into participants who reported fair or poor social adaptation vs. all else. Approximately 13% of the sample was categorized into the fair or poor category. We chose the fair or poor cut-off point because this is a qualitatively different group of migrants than those who are “doing well” and reporting good, or very good social adaptation (59).
Control variables
We included a set of confounding variables associated with depressive symptoms (7–10). Specifically, we controlled for: (i) socio-demographic characteristics, including gender (1 = female, 0 = male), age (in years), marital status (1 = married or with a partner, 0 = single or without a partner), education (years of schooling), and income (log-transformed); (ii) health behaviors, including smoking (1 = current smoker, 0 = non-smoker), alcohol consumption (1 = less than once a month, 2 = one to three times a month, 3 = one or two times a week, 4 = three to four times a week, and 5 = almost every day), and physical activity (1 = never, 2 = once a month, 3 = two or three times a month, 4 = two or three times a week, and 5 = almost every day); (iii) health status measured by self-reported physician-diagnosed chronic diseases (yes or no), including type 2 diabetes, hypertension, and heart disease. Additionally, we controlled for migration characteristics, including reasons for migration, migration time (in years), and city of residence. Reasons for migration were dichotomized into voluntary migration, which includes training or career opportunities (i.e., labor migration, occupation mobility, training and learning, and business investment), and involuntary migration for marriage or family reunion. Time since migration (in years) indicated how long migrants lived in the hosting city. The city of residence was dichotomized into more developed or less developed, depending on whether the GDP per capita of the hosting city is more than 100,000 RMB (equivalent to 14,286 US dollars).
Analytic strategy
We used Stata 15.0 for all statistical analysis (66). We used descriptive statistics to characterize the analytical sample separately for urban-to-urban and rural-to-urban migrants. To assess the disparities between groups, we conducted ANOVA tests for continuous variables and Chi-squared tests for categorical variables.
The bivariate logit models were used to examine whether there were significant differences in depressive symptoms between different groups. The multivariate linear regression models were used to examine the associations between social cohesion and depressive symptoms for both groups. Testing for mediation presumes a causal chain of events. The analyses cannot actually prove this causality, but they can show whether the data are in alignment with the proposed chain of events. In our analyses, we followed the procedure for establishing mediation proposed by Baron and Kenny (67). Adjusting for all covariates, we examined the mediating role of social adaptation on the association between social cohesion and depressive symptoms (67). Sobel and Goodman's methods were adapted to test the indirect effects of the mediating variables (68, 69).
Weighting
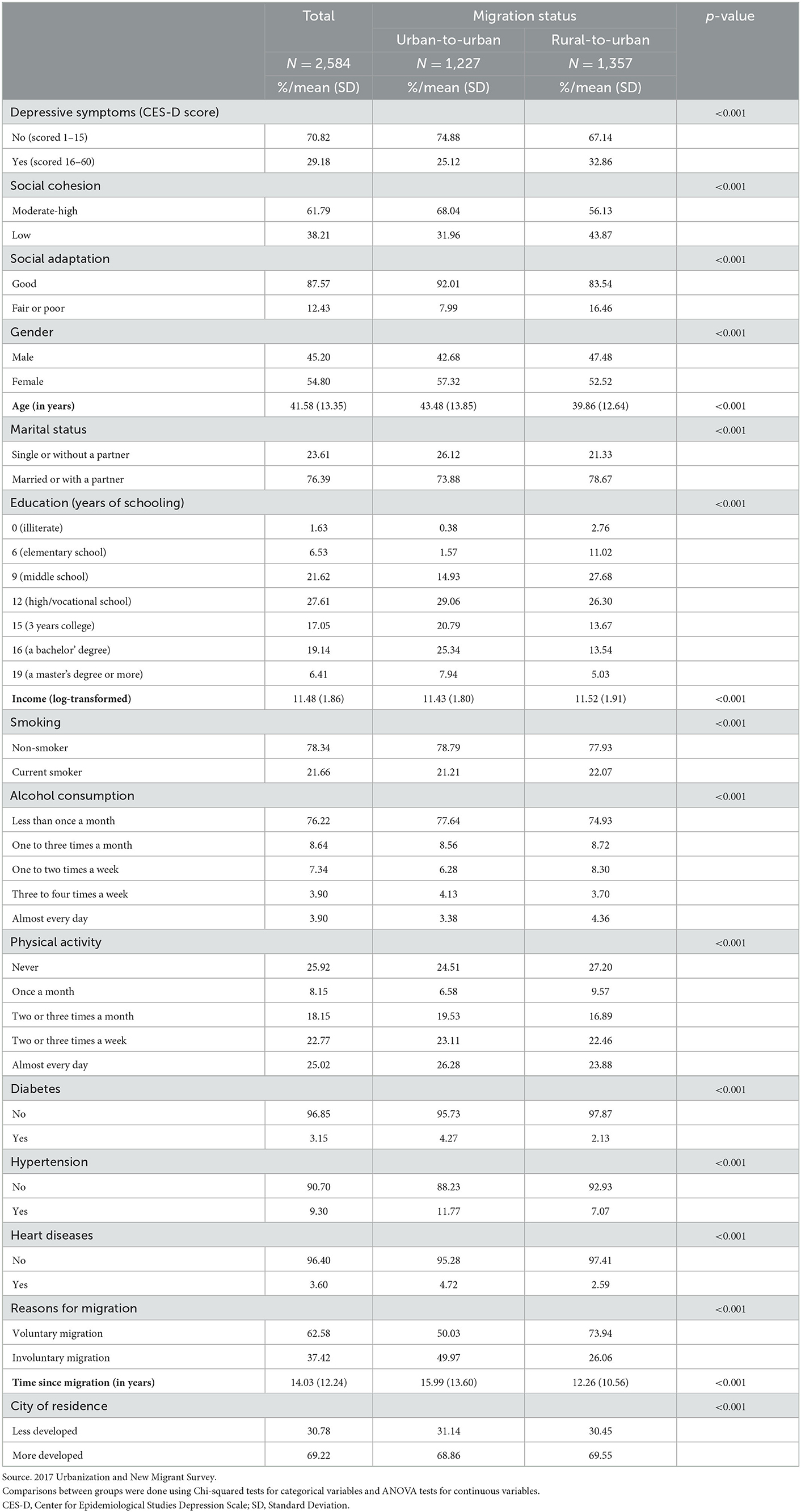
A multi-stage stratified sampling strategy was used, and the sampling process involved four stages: city, neighborhood, household, and individual. Ten cities were selected from seven provinces in China. At the city level, 20 neighborhoods were randomly selected from each city. At the neighborhood level, 25 households were selected from a housing registration database obtained from each neighborhood community. One individual was selected from each selected household. In this survey, the quota for migrants and non-migrants was designed to be close to 1:1. The “2017 Urbanization and New Migrant Survey” has individual-level sampling weights that take the complex sampling design into consideration. We defined the city as SU (n = 10), and the neighborhood as strata (n = 20). All analyses presented in Tables 1–4 were adjusted for sample weights (70).
Results
Descriptive statistics
Descriptive characteristics of the final weighted analytical sample are presented by migration status in Table 1. Rural-to-urban migrants were found to have more clinically significant depressive symptoms than urban-to-urban migrants (32.86 vs. 25.12%, p < 0.001). Approximately 43.87% of rural-to-urban migrants reported low social cohesion compared to 31.96% of urban-to-urban migrants. Approximately 16.46% of rural-to-urban migrants reported fair or low social adaptation compared to 7.99% of urban-to-urban migrants. Moreover, rural-to-urban migrants were less educated than urban-to-urban migrants. They tended to stay in the hosting city for a shorter duration (12.26 vs. 15.99 years, p < 0.001).
Prevalence of depressive symptoms by migration status, social cohesion, and social adaptation
Weighted prevalence of depressive symptoms by migration status, social cohesion, social adaptation and covariates are presented in Table 2. Results showed that being rural-to-urban migrants as compared with urban-to-urban migrants [Odds Ratio (OR) = 1.46, 95% Confidence Interval (CI) = 1.456, 1.461, p < 0.001], had lower perceived social cohesion (OR = 1.46, 95% CI = 1.458, 1.463, p < 0.001), and poorer social adaptation (OR = 1.94, 95% CI = 1.932, 1.941, p < 0.001), are associated with higher odds of having clinically significant depressive symptoms. Moreover, being married or with a partner (OR = 0.68, 95% CI = 0.679,0.682, p < 0.001) are associated with lower odds of having clinically significant depressive symptoms. Self-reported physician-diagnosed type 2 diabetes (OR = 1.71, 95% CI = 1.707,1.723, p < 0.001) and heart diseases (OR = 1.18, 95% CI = 1.172,1.183, p < 0.001) are associated with higher odds of having clinically significant depressive symptoms.
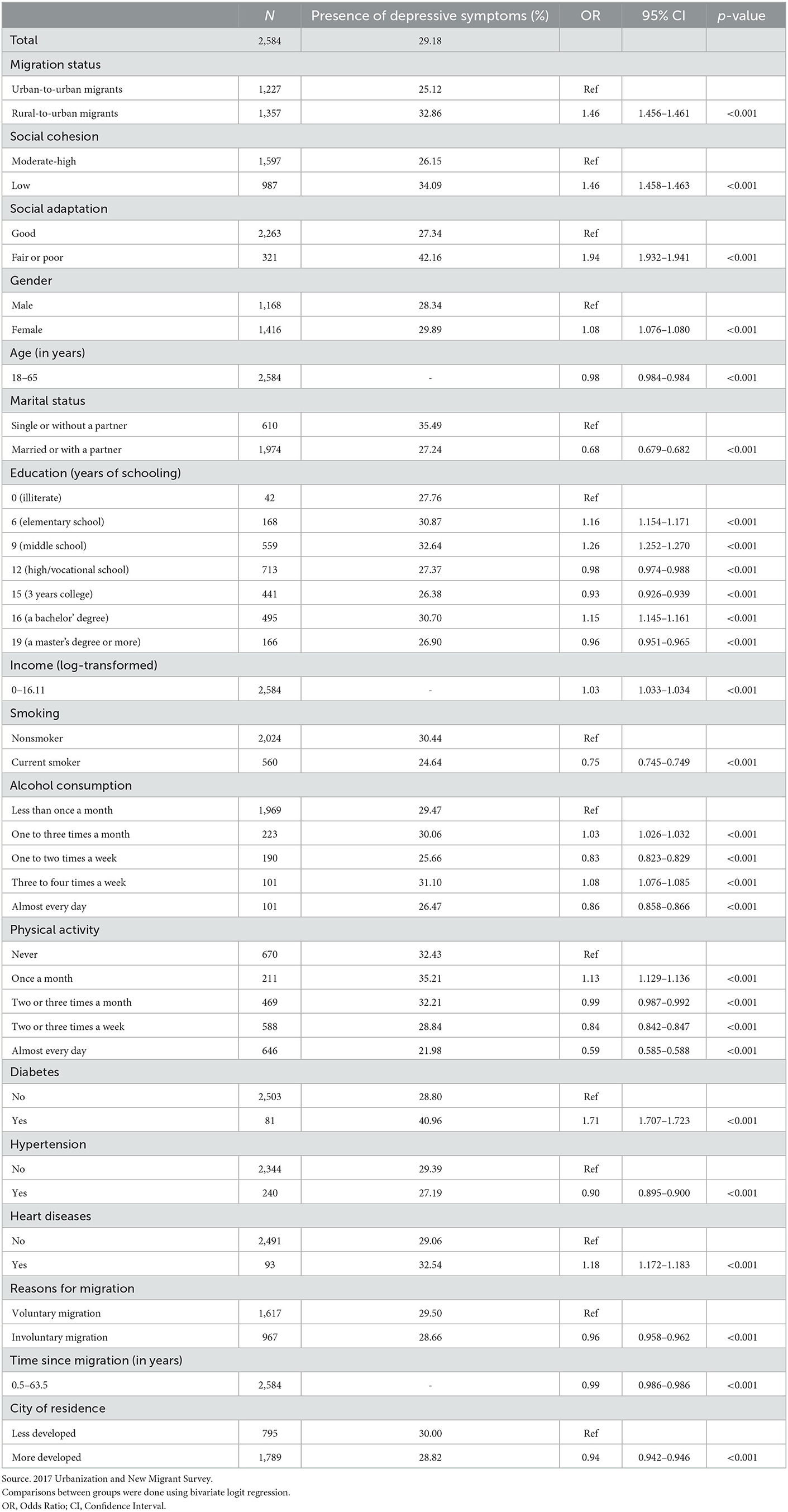
Table 2. Presence of depressive symptoms by migration status, social cohesion, social adaptation, and covariates (weighted).
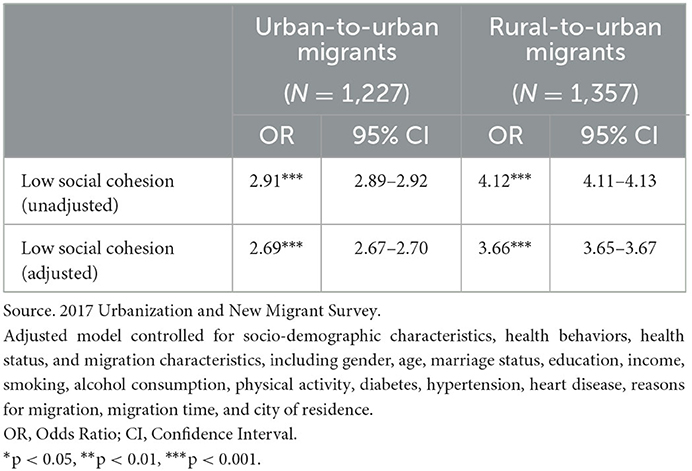
Associations between social cohesion and social adaptation
As shown in Table 3, fair or poor social adaptation was associated with a higher odd of migrants with a low perceived social cohesion for both urban-to-urban migrants (OR = 2.91, 95% CI = 2.89, 2.92, p < 0.001) and rural-to-urban migrants (OR = 4.12, 95% CI = 4.11, 4.13, p < 0.001). After adjustment for all covariates, the odds ratio reduced to 2.69 (95% CI = 2.67, 2.70, p < 0.001) for urban-to-urban migrants and 3.66 (95% CI = 3.65, 3.67, p < 0.001) for rural-to-urban migrants.
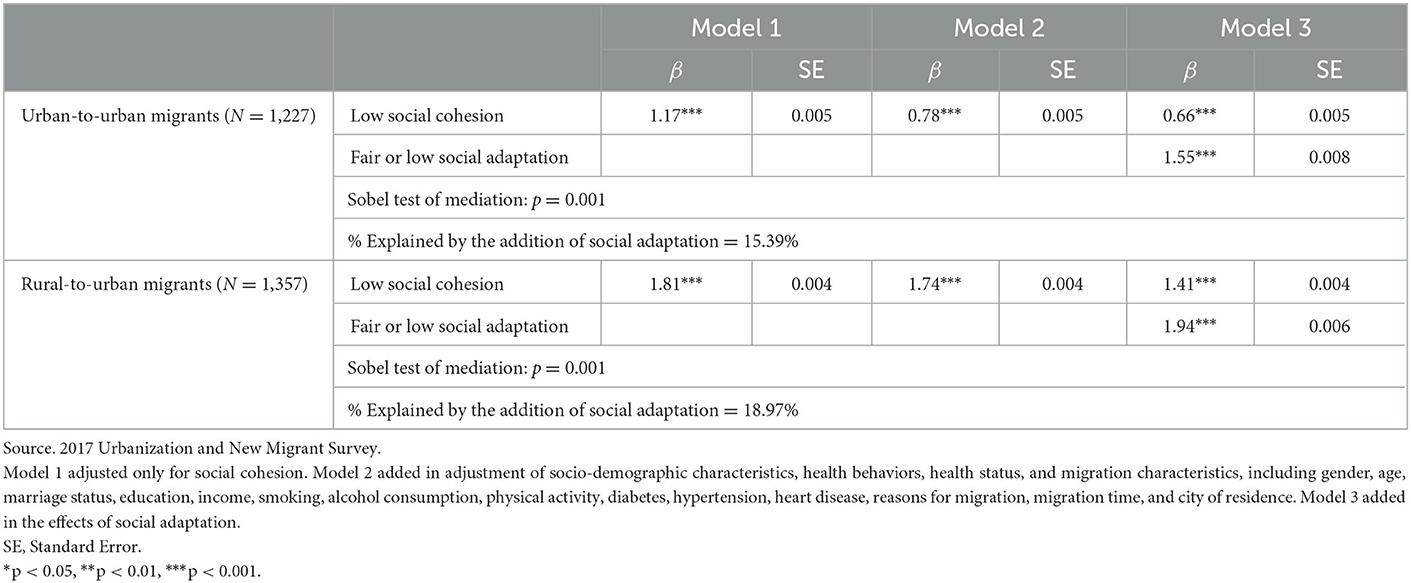
Associations between social cohesion and depressive symptoms
Table 4 shows the associations between social cohesion and depressive symptoms. As shown in Model 1, migrants with a low perceived social cohesion had a higher CES-D score for urban-to-urban migrants [β = 1.17, Standard Error (SE) = 0.005, p < 0.001] and rural-to-urban migrants (β = 1.81, SE = 0.004, p < 0.001) compared to those with moderate-high social cohesion. As shown in Model 2, the addition of covariates reduced the β-coefficient for low social cohesion to 0.78 (SE = 0.005, p < 0.001) for urban-to-urban migrants and 1.74 (SE = 0.004, p < 0.001) for rural-to-urban migrants. Moreover, the addition of social adaptation to Model 3 further reduced the β-coefficient for low social cohesion to 0.66 (SE = 0.005, p < 0.001) for urban-to-urban migrants and 1.41 (SE = 0.004, p < 0.001) for rural-to-urban migrants, and the associations remained significant.
Formal mediation analysis was conducted to examine the mediating role of social adaptation on the associations between social cohesion and depressive symptoms in both groups. The Sobel mediation tests were significant for both groups at the p = 0.001 level. Social adaptation partially mediated the association between social cohesion and depressive symptoms by explaining 15.39% of its effect for urban-to-urban migrants and 18.97% of its effect for rural-to-urban migrants.
Discussion
Using data from the “2017 Urbanization and New Migrant Survey,” we investigated the association between social cohesion and depressive symptoms among urban-to-urban and rural-to-urban migrants aged 18–65 in China and examined the mediating role of social adaptation. All three hypothesis were supported. The study findings demonstrated the significant mental health inequalities across urban-to-urban and rural-to-urban migrants. Also, we provided new knowledge to the field by identifying the protective role of social cohesion, as an important community-level factor, on depressive symptoms of migrants. Furthermore, this study identified the mediating role of social adaptation on the association between social cohesion and depressive symptoms. Our study has provided a scientific foundation for developing policy and research agenda to improve the mental health of migrants in China.
Mental health care challenges: Disparities in depressive symptoms within migrants
Our findings that rural-to-urban migrants had a higher prevalence of depressive symptoms than urban-to-urban migrants confirmed the mental health inequalities within migrants. Whether they migrated from urban or rural may have implications for their housing registration status (Hukou), educational background, financial status, social capital, and sense of wellbeing. All these factors are related not only to the challenges they may face in the migration process but also to their abilities to overcome the challenges that could affect their probability of suffering from depressive symptoms.
The limited resources and opportunities due to their Hukou could partially explain rural-to-urban migrants' higher prevalence of depressive symptoms. Rural Hukou limits their access to both economic and social resources in the host city. In this situation, the social stress and social exclusion they experienced may have significant mental health implications (6, 10–12). Our results showed that a higher proportion of rural-to-urban migrants had less perceived social cohesion and fair or poor social adaptation than urban-to-urban migrants. Although China has gradually relaxed its policies on its Hukou system, it remains challenging for rural-to-urban migrants, especially those with low education, to settle permanently in the receiving city or are entitled to the same social benefits as urban residents (14, 35, 36). These inequalities could limit their opportunities for upward mobility and ultimately affect their mental health outcomes.
Our results also suggest that, among rural-to-urban migrants, involuntary migrated participants had higher depressive symptoms than those who voluntarily migrated. Several reasons may shed a slight on the findings. For example, these involuntary migrants may have limited social connections because family members are likely to be the only social network they can interact with. In addition, involuntary migrants have limited access to formal financial support, social capital, and health insurance, all are considered protective factors for maintaining good mental health (19).
Social strategies: Building a higher cohesive community
Findings on the association between social cohesion and depressive symptoms are in line with previous studies which demonstrated that a higher level of neighborhood social cohesion is associated with better mental health outcomes (49, 50, 52, 55, 56).
Findings from linear regression models indicate that the level of depressive symptoms of rural-to-urban migrants is more dependent on social cohesion. It seems that social environmental context is even more important for rural-to-urban migrants' psychological wellbeing than for urban-to-urban migrants. In a host city, rural-to-urban migrants face much greater mental health risks than urban-to-urban migrants (6, 11, 17, 18); including (i) lack of urban Hukou that comes with a variety of economic and social resources (i.e., social security, unemployment insurance, and health insurance). (ii) Lack of sufficient level of education that could help them achieve a stable occupation and a higher socioeconomic position. (iii) Lack of sufficient social capital that is an important protective factor of psychological wellbeing. Although social capital appears to exist among rural-to-urban migrants, they have less-developed organizational social networks. Most of them rely on family members and friends from hometowns as primary personal networks (71). Thus, we speculate that they are more in need of support and help from a well-integrated community than urban-to-urban migrants. Tailored social strategies are needed to target rural-to-urban migrants for addressing mental health disparities among migrant population.
Additionally, our study identified the mediating role of social adaptation on the association between social cohesion and depressive symptoms for both groups. Reflecting the interactions between local residents and migrants, community-level social cohesion impacts whether migrants could “doing well” in the activities of daily living (59) and achieve good psychological wellbeing in the host city.
Our study findings demonstrate that social cohesion matters in mental health outcomes among migrants in China. Improving social cohesion could be an effective social strategy to promote the mental health of the migrant population. Social cohesion is undoubtedly influenced by governance, socio-economic and public policies (26). Thus, public programs and intervention strategies are needed to construct a more integrated community that serves both local residents and internal migrants.
Some limitations of this study need to be acknowledged. First, this study used cross-sectional survey data; we are only able to examine the associations of the variables of interest. First, this study used cross-sectional survey data; we are only able to examine the associations of the variables of interest. From a life-course perspective, the impact of migration and migration-related changes accumulate throughout the life-course; therefore, longitudinal studies are needed for future research. Second, this study was conducted in 10 cities, which is not representative of all migrant-receiving cities in China. Third, to better identify the pathways of social cohesion on depressive symptoms, we need to explore more mediating factors, such as social stress and social exclusion, in future studies. We thus call for future studies to develop and evaluate socio-behavioral interventions in addressing the mental health problems of the increasing number of internal migrants in China.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors. Requests to access these datasets should be directed to bWlsbGllX3F1QDE2My5jb20=.
Ethics statement
The 2017 Urbanization and New Migrant Survey involving human participants were reviewed and approved by Ethics Committee of Shanghai University (ECSHU 2020-097). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
BW contributed to conceptualization, design, and manuscript preparation. XQu contributed to data analysis and manuscript preparation. XQi, JY, and HZ contributed to manuscript preparation. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Social Science Foundation of China under program number of (17ZDA111) and (17ASH004). The content is solely the responsibility of the authors.
Acknowledgments
The 2017 Urbanization and New Migrant Survey was designed and conducted by the Shanghai Social Science Survey Center, Shanghai University. The authors would like to thank them for making the data used in this study available.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. International Organization for Migration. World Migration Report 2018. (2018). Available online at: https://publications.iom.int/books/world-migration-report-2018 (accessed October 13, 2022).
2. Zhou J, Zhou J, Zhang H, Zhang J. Social integration as mediator and age as moderator in social capital affecting mental health of internal migrant workers: A multi-group structural equation modeling approach. Front Public Health. (2022) 10:865061. doi: 10.3389/fpubh.2022.865061
3. National Health Commission of People's Republic of China. Reports on China's Migrant Population Development. Beijing: China Population Publishing House (2018).
4. Xie S, Wang J, Chen J, Ritakallio VM. The effect of health on urban-settlement intention of rural-urban migrants in China. Health Place. (2017) 47:1–11. doi: 10.1016/j.healthplace.2017.06.008
5. Smyth R, Nielsen I, Zhai Q. Subjective well-being of China's off-farm migrants. Monash Univ Dep Econ Dev Res Unit Work Pap Ser. (2009) 11:9. doi: 10.1007/s10902-009-9142-9
6. Li J, Rose N. Urban social exclusion and mental health of China's rural-urban migrants – A review and call for research. Health Place. (2017) 48:20–30. doi: 10.1016/j.healthplace.2017.08.009
7. Silveira E, Allebeck P. Migration, ageing and mental health: An ethnographic study on perceptions of life satisfaction, anxiety and depression in older Somali men in east London. Int J Soc Welf. (2001) 10:309–20. doi: 10.1111/1468-2397.00188
8. Bhugra D. Migration, distress and cultural identity. Br Med Bull. (2004) 69:129–41. doi: 10.1093/bmb/ldh007
9. Ornelas IJ, Perreira KM. The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Soc Sci Med. (2011) 73:1169–77. doi: 10.1016/j.socscimed.2011.07.002
10. Lu Y, Hu P, Treiman DJ. Migration and depressive symptoms in migrant-sending areas: Findings from the survey of internal migration and health in China. Int J Public Health. (2012) 57:691–8. doi: 10.1007/s00038-011-0314-0
11. Cheung NWT. Social stress, locality of social ties and mental well-being: The case of rural migrant adolescents in urban China. Health Place. (2014) 27:142–54. doi: 10.1016/j.healthplace.2014.01.013
12. Mou J, Cheng J, Griffiths SM, Wong SYS, Hillier S, Zhang D. Internal migration and depressive symptoms among migrant factory workers in Shenzhen, China. J Community Psychol. (2011) 39:212–30. doi: 10.1002/jcop.20428
13. Froissart C, Wang FL. Organizing through division and exclusion. China's Hukou system. Perspect Chin. (2006) 94:62–4. doi: 10.4000/chinaperspectives.638
14. Liang Z, Li Z, Ma Z. Changing patterns of the floating population in China, 2000–2010. Popul Dev Rev. (2014) 40:695–716. doi: 10.1111/j.1728-4457.2014.00007.x
15. Wang H, Hou Y, Zhang L, Yang M, Deng R, Yao J. Chinese elderly migrants' loneliness, anxiety and depressive symptoms: The mediation effect of perceived stress and resilience. Front Public Health. (2022) 10:998532. doi: 10.3389/fpubh.2022.998532
16. Zheng Z, Yang G. Internal migration in China: Changes and trends. In: CZ Guilmoto, GW Jones, editors, Contemporary Demographic Transformations in China, India and Indonesia. Demographic Transformation and Socio-Economic Development. Cham: Springer International Publishing (2016). p. 223–37. doi: 10.1007/978-3-319-24783-0_14
17. Keung Wong DF, Li CY, Song HX. Rural migrant workers in urban China: Living a marginalised life. Int J Soc Welf. (2007) 16:32–40. doi: 10.1111/j.1468-2397.2007.00475.x
18. Wen M, Zheng ZZ, Niu JL. Psychological distress of rural-to-urban migrants in two Chinese cities: Shenzhen and Shanghai: Asian Population Studies. Asian Popul Stud. (2017) 13:5–24. doi: 10.1080/17441730.2016.1233655
19. Wu Q, Harwood RL, Feng X. Family socioeconomic status and maternal depressive symptoms: Mediation through household food insecurity across five years. Soc Sci Med. (2018) 215:1–6. doi: 10.1016/j.socscimed.2018.08.043
20. Ehsan AM, De Silva MJ. Social capital and common mental disorder: A systematic review. J Epidemiol Community Health. (2015) 69:1021–8. doi: 10.1136/jech-2015-205868
21. Cohen-Cline H, Beresford SA, Barrington W, Matsueda R, Wakefield J, Duncan GE. Associations between social capital and depression: A study of adult twins. Health Place. (2018) 50:162–7. doi: 10.1016/j.healthplace.2018.02.002
22. Stice E, Ragan J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? J Abnorm Psychol. (2004) 113:155–9. doi: 10.1037/0021-843X.113.1.155
23. Guo M, Stensland M. A systematic review of correlates of depression among older Chinese and Korean immigrants: What we know and do not know. Aging Ment Health. (2018) 22:1535–47. doi: 10.1080/13607863.2017.1383971
24. Misra S, Wyatt LC, Wong JA, Huang CY, Ali SH, Trinh-Shevrin C, et al. Determinants of depression risk among three Asian American Subgroups in New York City. Ethn Dis. (2020) 30:553–62. doi: 10.18865/ed.30.4.553
25. Lister R. Strategies for social inclusion: Promoting social cohesion or social justice? In:P Askonas, A Stewart, , editors, Social Inclusion: Possibilities and Tensions. Basingstoke, London: Macmillan (2000). p. 37–54.
26. Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. (2000) 51:843–57. doi: 10.1016/S0277-9536(00)00065-4
27. Kawachi I, Berkman L. Social cohesion, social capital, and health. In: L Berkman, I Kawachi, editors, Social Epidemiol. 2 edn. New York, NY: Oxford University Press (2014). p. 290–319. doi: 10.1093/med/9780195377903.003.0008
28. Baranyi G, Sieber S, Cullati S, Pearce JR, Dibben CJL, Courvoisier DS. The longitudinal associations of perceived neighborhood disorder and lack of social cohesion with depression among adults aged 50 years or older: An individual-participant-data meta-analysis from 16 high-income countries. Am J Epidemiol. (2020) 189:343–53. doi: 10.1093/aje/kwz209
29. Gkiouleka A, Avrami L, Kostaki A, Huijts T, Eikemo TA, Stathopoulou T. Depressive symptoms among migrants and non-migrants in Europe: Documenting and explaining inequalities in times of socio-economic instability. Eur J Public Health. (2018) 28(Suppl.5):54–60. doi: 10.1093/eurpub/cky202
30. Navodani T, Gartland D, Brown SJ, Riggs E, Yelland J. Common maternal health problems among Australian-born and migrant women: A prospective cohort study. PLoS ONE. (2019) 14:e0211685. doi: 10.1371/journal.pone.0211685
31. Waern M, Rubenowitz E, Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. (2003) 49:328–34. doi: 10.1159/000071715
32. Wada T, Ishine M, Sakagami T, et al. Depression in Japanese community-dwelling elderly—Prevalence and association with ADL and QOL. Arch Gerontol Geriatr. (2004) 39:15–23. doi: 10.1016/j.archger.2003.12.003
33. Kondo N, Kazama M, Suzuki K, Yamagata Z. Impact of mental health on daily living activities of Japanese elderly. Prev Med. (2008) 46:457–62. doi: 10.1016/j.ypmed.2007.12.007
34. Chan KW, Zhang L. The Hukou system and rural-urban migration in China: Processes and changes. China Q. (1999) 160:818–55. doi: 10.1017/S0305741000001351
35. Nielsen IL, Russell S. Migration and Social Protection in China (September 16, 2008). Series on Contemporary China, Vol. 14. Available online at: https://ssrn.com/abstract=1470507 (accessed October 13, 2022).
36. Zhang Z, Treiman DJ. Social origins, Hukou conversion, and the wellbeing of urban residents in contemporary China. Soc Sci Res. (2013) 42:71–89. doi: 10.1016/j.ssresearch.2012.08.004
37. Coyne JC, Downey G. Social factors and psychopathology: Stress, social support, and coping processes. Annu Rev Psychol. (1991) 42:401–25. doi: 10.1146/annurev.ps.42.020191.002153
38. Mulvaney-Day NE, Alegría M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Soc Sci Med. (2007) 64:477–95. doi: 10.1016/j.socscimed.2006.08.030
39. Richardson R, Westley T, Gariépy G, Austin N, Nandi A. Neighborhood socioeconomic conditions and depression: A systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1641–56. doi: 10.1007/s00127-015-1092-4
40. Liu J, Guo M, Xu L, Mao W, Chi I. Family relationships, social connections, and depressive symptoms among Chinese older adults in international migrant families. J Ethn Cult Divers Soc Work. (2017) 26:167–84. doi: 10.1080/15313204.2016.1206496
41. Chou KL. Pre-migration planning and depression among new migrants to Hong Kong: The moderating role of social support. J Affect Disord. (2009) 114:85–93. doi: 10.1016/j.jad.2008.06.005
42. Zhu Y, Gao J, Nie X, Dai J, Fu H. Associations of individual social capital with subjective well-being and mental health among migrants: A survey from five cities in China. Int Health. (2019) 11(Suppl.1):S64–71. doi: 10.1093/inthealth/ihz041
43. Yamaguchi M, Inoue Y, Shinozaki T, Saito M, Takagi D, Kondo K, et al. Community social capital and depressive symptoms among older people in Japan: A multilevel longitudinal study. J Epidemiol. (2019) 29:363–9. doi: 10.2188/jea.JE20180078
44. Bollen KA, Hoyle RH. Perceived cohesion: A conceptual and empirical examination. Soc Forces. (1990) 69:479–504. doi: 10.2307/2579670
45. Cramm JM, van Dijk HM, Nieboer AP. The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. Gerontologist. (2013) 53:142–52. doi: 10.1093/geront/gns052
46. Kawachi I, Kennedy BP. Health and social cohesion: Why care about income inequality? Br Med J. (1997) 314:1037–40. doi: 10.1136/bmj.314.7086.1037
47. Echeverría S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The Multi-Ethnic Study of Atherosclerosis. Health Place. (2008) 14:853–65. doi: 10.1016/j.healthplace.2008.01.004
48. Ahern J, Galea S. Collective efficacy and major depression in urban neighborhoods. Am J Epidemiol. (2011) 173:1453–62. doi: 10.1093/aje/kwr030
49. Ruiz M, Malyutina S, Pajak A, Kozela M, Kubinova R, Bobak M. Congruent relations between perceived neighbourhood social cohesion and depressive symptoms among older European adults: An East-West analysis. Soc Sci Med. (2019) 237:112454. doi: 10.1016/j.socscimed.2019.112454
50. Miao J, Wu X, Sun X. Neighborhood, social cohesion, and the Elderly's depression in Shanghai. Soc Sci Med. (2019) 229:134–43. doi: 10.1016/j.socscimed.2018.08.022
51. Robinette JW, Charles ST, Gruenewald TL. Neighborhood cohesion, neighborhood disorder, and cardiometabolic risk. Soc Sci Med. (2018) 198:70–6. doi: 10.1016/j.socscimed.2017.12.025
52. Holmes LM, Marcelli EA. Neighborhood social cohesion and serious psychological distress among Brazilian immigrants in Boston. Community Ment Health J. (2020) 56:149–56. doi: 10.1007/s10597-019-00468-8
53. Rosenblatt AM, Crews DC, Powe NR, Zondermann AB, Evans MK, Tuot DS. Association between neighborhood social cohesion, awareness of chronic diseases, and participation in healthy behaviors in a community cohort. BMC Public Health. (2021) 21:1611. doi: 10.1186/s12889-021-11633-8
54. Jin L, Wen M, Fan JX, Wang G. Trans-local ties, local ties and psychological well-being among rural-to-urban migrants in Shanghai. Soc Sci Med. (2012) 75:288–96. doi: 10.1016/j.socscimed.2012.03.014
55. Zhang L, Jiang J, Wang P. Social cohesion associated with health mediated by emotional experience and life satisfaction: Evidence from the internal migrants in China. Appl Res Qual Life. (2021) 16:1285–303. doi: 10.1007/s11482-020-09818-1
56. Ruiz M, Scholes S, Bobak M. Perceived neighbourhood social cohesion and depressive symptom trajectories in older adults: A 12-year prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:1081–90. doi: 10.1007/s00127-018-1548-4
57. Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. (2016) 69:313–32. doi: 10.1016/j.neubiorev.2016.07.002
58. Sheehan DV, Nakagome K, Asami Y, Pappadopulos EA, Boucher M. Restoring function in major depressive disorder: A systematic review. J Affect Disord. (2017) 215:299–313. doi: 10.1016/j.jad.2017.02.029
59. Ward C, Kennedy A. The measurement of sociocultural adaptation. Int J Intercult Relat. (1999) 23:659–77. doi: 10.1016/S0147-1767(99)00014-0
60. Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
61. Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample: Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. (1982) 39:1195–200. doi: 10.1001/archpsyc.1982.04290100059010
62. Chan J, To HP, Chan E. Reconsidering social cohesion: Developing a definition and analytical framework for empirical research. Soc Indic Res. (2006) 75:273–302. doi: 10.1007/s11205-005-2118-1
63. Cagney KA, Glass TA, Skarupski KA, Barnes LL, Schwartz BS, Mendes de Leon CF. Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. J Gerontol B Psychol Sci Soc Sci. (2009) 64:415–24. doi: 10.1093/geronb/gbn041
64. Erdem Ö, Van Lenthe FJ, Prins RG, Voorham TAJJ, Burdorf A. Socioeconomic inequalities in psychological distress among urban adults: The moderating role of neighborhood social cohesion. PLoS ONE. (2016) 11:e0157119. doi: 10.1371/journal.pone.0157119
65. Latham K, Clarke PJ. Neighborhood disorder, perceived social cohesion, and social participation among older Americans: Findings from the National Health & Aging Trends Study. J Aging Health. (2018) 30:3–26. doi: 10.1177/0898264316665933
67. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
68. Goodman LA. On the exact variance of products. J Am Stat Assoc. (1960) 55:708–13. doi: 10.1080/01621459.1960.10483369
69. Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. (1982) 13:290–312. doi: 10.2307/270723
70. Heeringa SG, West BT, Berglund PA. Applied Survey Data Analysis. Boca Raton: Chapman and Hall/CRC, Taylor and Francis Group (2010).
Keywords: social cohesion, social adaptation, depression, migration, mental health disparities
Citation: Qu X, Qi X, Wu B, Yu J and Zhang H (2023) Perceived social cohesion and depressive symptoms among internal migrants in China: The mediating role of social adaptation. Front. Public Health 11:1096318. doi: 10.3389/fpubh.2023.1096318
Received: 12 November 2022; Accepted: 23 January 2023;
Published: 07 February 2023.
Edited by:
Roger C. Ho, National University of Singapore, SingaporeCopyright © 2023 Qu, Qi, Wu, Yu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaomin Qu,  bWlsbGllX3F1QDE2My5jb20=; Bei Wu,
bWlsbGllX3F1QDE2My5jb20=; Bei Wu,  YmVpLnd1QG55dS5lZHU=
YmVpLnd1QG55dS5lZHU=
 Xiaomin Qu
Xiaomin Qu Xiang Qi
Xiang Qi Bei Wu
Bei Wu Jiaojiao Yu
Jiaojiao Yu Haidong Zhang
Haidong Zhang