
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 20 March 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1094776
Background: Healthcare workers were at high risk of psychological problems during the COVID-19 pandemic, but it remains not well-investigated in the post-pandemic era of COVID-19, with regular epidemic prevention and control embedded in burdened healthcare work. This study aimed to investigate the prevalence and potential risk factors of the symptoms of depression and anxiety among healthcare workers at a tertiary hospital in Shenzhen.
Method: Our cross-sectional study was conducted among 21- to 64-year-old healthcare workers in December 2021 at a tertiary hospital in Shenzhen, using a simple random sampling strategy. A wide range of socio-demographic characteristics, individual information, and psychological condition of the subjects were extracted. Healthcare workers' psychological conditions were tested with the Center for Epidemiologic Studies Depression (CESD-10), General Anxiety Disorder (GAD-7), Insomnia Severity Index (ISI), Work-Family Conflict Scale (WFCS), 10-item Connor-Davidson Resilience Scale (CD-RISC-10), and 17-item of Maslach's Burnout Inventory-Human Services Survey (MBI-HSS-17). Data were collected based on these questionnaires. Descriptive statistics were used to assess the difference between healthcare workers with depressive and anxiety symptoms among different groups. Hierarchical logistic regression analyses were conducted to investigate the association between focused variables and mental health outcomes.
Results: A total of 245 healthcare workers were enrolled. The proportion of depressive symptoms, anxiety symptoms and their co-occurrence were 34.7, 59.6, and 33.1%, respectively. Logistic regression showed that for the three outcomes, no history of receiving psychological help and self-rated good or higher health were protective factors, whereas more severe insomnia and job burnout were risk factors. Junior or lower job title and higher psychological resilience were related to a lower prevalence of depressive symptoms, while relatively longer working hours and larger work-family conflict were positively associated with the anxiety symptoms. Psychological resilience was inversely associated with the co-occurrence of depressive and anxiety symptoms.
Conclusions: Our study revealed a high proportion of psychological problems and proved that several similar factors which were significant during the pandemic were also associated with the symptoms of depression and anxiety among healthcare workers in the post-pandemic era of COVID-19. These results provide scientific evidence for psychological interventions for healthcare workers.
First appearing in China's Wuhan province in December 2019 (1), coronavirus disease 2019 (COVID-19) was declared a global pandemic on March 11, 2020 (2). The WHO estimated that as of September 21, 2022, COVID-19 had infected over 609 million individuals worldwide and caused over 6.5 million fatalities (3). This pandemic has caused an unusual situation, with people worldwide suffering from various levels of fear, depression, and anxiety (4). Facing the unprecedented situation, healthcare workers have made great efforts to provide medical treatment and care to control the epidemic quickly during the COVID-19 pandemic and faced excessive workloads and psychological pressure, thereby having a large proportion of psychological problems. Compared to other occupational groups, they were particularly vulnerable to psychological problems (5–7) and more than one-third of healthcare workers experienced anxiety and depression during the COVID-19 pandemic globally (8) and in China (9).
Different from the early pandemic stage without a thorough grasp of the management of COVID-19, China and other countries around the world have already entered the post-pandemic era with routine prevention and control measures embedded in the post-pandemic new normal lifestyles (10, 11). By the time of our study, compared with the early pandemic stage, the epidemic was relatively well-controlled and a relatively strict control measures in this period were routine, which actually lasted for almost 2 years in all areas in China from the end of April 2020 (12). Due to the virus variation of COVID-19, the post-pandemic era might be prolonged for a longer time. It would profoundly impact many aspects (13), further stressing the great need to assess collateral damage in this era, such as mental health problems including depressive and anxiety symptoms (14). A study conducted in Shenzhen also proposed the concept of the post-epidemic era and investigated the prevalence and contributory factors of anxiety and depression among pregnant women during the specific period (10). Moreover, previous major public health emergencies also suggested that psychological issues may continue to exist or even develop in the post-pandemic era (13). Therefore, further investigation of the healthcare workers' psychological status in the post-epidemic era has certain scientific basis and practical significance.
Several studies have been performed during the COVID-19 pandemic to show some potential influencing factors. For example, healthcare workers aged below 40 have been found to have a higher level of depressive and anxiety symptoms than those aged above 40 (6, 15). Women have been found to be more vulnerable to the symptoms of depression (15–17) and anxiety (16, 18) during the COVID-19 pandemic. Nurses had a greater likelihood of developing depression than others, but any job type of healthcare worker developed anxiety at equal odds (6). And studies also revealed that healthcare workers with bachelor's degrees had significantly higher depression and anxiety than those with different education levels (19, 20). The intermediate job title was associated with higher anxiety and depression (5). Moreover, the level of psychological problems among the healthcare workers was reversely correlated with their years of working experience (21) and household income (22). For anxiety symptoms, being married was a risk factor (23). For depressive and anxiety symptoms, rural healthcare workers may have more psychosocial distress than urban ones during the COVID-19 pandemic (17). These results have suggested that the development of depressive and anxiety symptoms among healthcare workers during the COVID-19 pandemic is related to multiple socio-demographic factors, such as age, sex, job type, education level, job title, years of working, employment type, income, marital status, and place of residence. In the post-pandemic era, these socio-demographic factors should still be considered as important variables of the research. In addition to the basic demographic characteristics such as age and sex, the socio-economic decline caused by the mode of normal epidemic management may, to some extent, make education level, job title, income and other factors related to economy and employment become more important factors for the depressive and anxiety symptoms of healthcare workers in the post-pandemic era.
Several studies conducted during the COVID-19 pandemic showed that the alarming level of symptoms of depression and anxiety among healthcare workers could be associated with increased exposure to professional risks, unreasonable work arrangement, and individual physical and mental status (24, 25). In terms of individual-health-related factors, self-rated physical condition, chronic disease status, and psychological-help receiving state are focused factors in this field. The physical condition was closely related to the level of anxiety during the epidemic. The worse the individual's physical quality, the higher their level of depressive and anxiety symptoms (20). In addition, the presence of chronic illnesses was confirmed as a risk factor of getting emotional distress including depression and anxiety in general people (26). Previous studies have proved that psychological help for healthcare workers could reduce the emotional impact of COVID-19 (27). During the post-pandemic era of COVID-19, these effects may keep up among healthcare workers on their symptoms of depressive and anxiety. In the post-pandemic era of COVID-19, the isolation measures of normalized management might reduce the physical activity time of healthcare workers (28), which may make the influence of physical condition and chronic disease status more prominent. After the outbreak of COVID-19, under the condition of continuous optimization of psychological intervention studies among healthcare workers (29, 30), psychological-help receiving rate among healthcare workers might increase during the epidemic, so the influence of the acceptance state of psychological-help receiving state may have a downward trend in the post-epidemic era.
As for work-arrangement-related factors, researchers often focus on traditional job-related factors and specific COVID-19-related factors during the pandemic. Traditional job-related factors often include the frequency of night shifts, working hours and working intensity. The night shift arrangements (31) and working hours of more than 8 h (32) have been proven to be risk factors for depressive and anxiety symptoms among healthcare workers. The higher frequency of night shifts and longer working hours were inversely correlated with the level of these symptoms. Due to the development of COVID-19, epidemic-related factors also greatly influenced healthcare workers' emotional states. Some risk factors, such as additional workload from the sustainability of COVID-19 prevention measures in the post-pandemic period, may strongly burden healthcare workers' wellbeing (25). COVID-19-related departments such as the fever clinic, emergency departments and ICU may take on more epidemic responsibilities at work. Compared to pre-epidemic conditions, the total and regular workload may be changed because of the implementation of epidemic policy in the hospital. Few studies so far have investigated the association between COVID-19-related workload and psychological issues. In the post-pandemic era, traditional job-related factors are still important factors affecting the psychological status of healthcare workers. However, with the continuous extension of normalization management time, the influence of COVID-19-related workload on mental state may also decrease due to the increased role of positive factors such as psychological resilience.
Researchers often focus on depressive and anxiety symptoms as the main focus of psychological problems (9). However, many other psychological factors in the Chinese medical environment can affect the above two symptoms. In addition to depressive and anxiety symptoms, some psychological factors had been widely reported among healthcare workers before and during the pandemic. And previous studies have demonstrated that these psychological factors were risk factor of depressive and anxiety symptoms, which may be more affected by the COVID-19 pandemic. First, many studies showed the importance of sleep quality in mental health (33, 34). Long-standing evidence suggests that insomnia is associated with depression and anxiety (6, 35), and how this factor changes in the post-pandemic era is meaningful to find out. Second, psychological resilience, as a common mediating factor, could help individuals sustain emotional balance in the face of stress-inducing events (36). Previous studies conducted during the COVID-19 pandemic identified a protective role for psychological resilience in healthcare workers against the mental health burden (37). Third, job burnout is a feeling of anger, frustration, suspicion and paranoia at work, which is increasingly recognized among healthcare professionals (38). The feeling of job burnout is known to have a negative impact on mental health (39), which may be mitigated by psychological resilience at the same time (37). Moreover, in the COVID-19 pandemic, the misty boundary between work and personal life potentially resulted in conflicts between work and family or family and work due to changes in the workplace, home environment, and social relationships (40). For healthcare workers, the stress of work-family balance could have a detrimental effect on their performance at work, reduce their feelings of wellbeing, and even cause more serious mental illness (41–43). In the post-pandemic era, due to the constant changes in epidemic policies and work intensity, we predict that the degree of insomnia, job burnout and work-family conflict among healthcare workers would be further strengthened, and the effect of psychological resilience on the improvement of mental status will become more important.
Although previous studies showed the high appearance of mental health problems and confirmed some socio-demographic, individual-health, job-related, COVID-19-related and psychological parameters among healthcare workers during the COVID-19 pandemic, they were only based on the condition in the following months after the pandemic was announced. In the post-pandemic era of COVID-19, few studies investigated depressive and anxiety symptoms in Chinese healthcare workers. However, the current researches into past epidemics suggested that mental health problems could further develop after the pandemic's peak, with increased prevalence among vulnerable group with risk factors (13). Healthcare workers are a special group, with the similar work environment, relatively fixed posts, and the heavy medical work. If they are affected by some unavoidable factors in a short period of time during the COVID-19 pandemic, these factors are likely to continue to exist in the later period of the pandemic, and even deepen. But in the post-pandemic era of COVID-19, healthcare workers may also be disturbed by other factors that had little impact during the pandemic. This suggests that we should continue to focus on the factors that contribute to mental health problems during the pandemic, as well as continue to explore non-significant factors during the pandemic that may have an impact on psychological status in the post-pandemic. Moreover, growing evidence showed that regular screening for mental health symptoms was momentous in minimizing the psychological risk among healthcare workers (44). Therefore, there is a great need to explore its ongoing impact on healthcare workers' mental health in the post-pandemic era of COVID-19 and beyond.
This study aimed to investigate the levels of depressive and anxiety symptoms and their occurrence and explore related factors among healthcare workers during the post-pandemic era at a tertiary hospital in Shenzhen. The finding will be helpful in understanding the level of psychological symptoms among healthcare workers and provide a basis for mental health intervention targeted healthcare workers during the post-pandemic era. We hypothesize that, associated factors of depressive and anxiety symptoms among healthcare workers in the post-pandemic era are similar to those related to psychological status during the COVID-19 pandemic, but some factors may have different effects. In the post-pandemic era: (1) participants with a worse physical health condition, heavier jobs and COVID-19-related additional burden were more likely to have depressive and anxiety symptoms; (2) participants with a higher level of insomnia, more severe work-family conflict, graver job burnout and less psychological resilience were more likely to have depressive and anxiety symptoms.
A cross-sectional study was performed in December 2021 in a general tertiary hospital in Nanshan district, Shenzhen. Shenzhen Shekou Free Trade Zone Hospital is the only tertiary general hospital in Shenzhen Qianhai Shekou Free Trade Zone, with a total of 506 approved beds, covering 65 square kilometers and nearly 800,000 population. As a tertiary general hospital, it provides a full range of medical services and have the ability to provide specialized care for patients with serious or complex medical conditions. According to the Shenzhen Municipal Health Commission, there were about 140 new confirmed cases of COVID-19 in December 2021. This is a period in which the epidemic in majority area across China is under control because of the normalized epidemic prevention and control measures. A standardized electronic questionnaire was distributed. The questionnaire was designed with Wenjuanxing online platform [http://www.wjx.cn/ (China's largest professional online survey platform)], and a QR code was generated at the same time. To calculate the sample size for the study, we used the computational formula: where n is sample size, Z1−α/2 is the z score for α, δ is the tolerance error and p is the prevalence of outcome in population. Assuming that the prevalence of depression was 27.7% (45), the required sample size at α = 0.05 and δ = 0.05 was 308. Considering a at least 20% loss to follow-up and enough sample size of multivariate regression analysis, we set the target sample size as about 400 participants in the study. A simple random sampling strategy was adopted and a total of 400 doctors and nurses were randomly selected from the list of all healthcare workers full-time working in this hospital to be recruited using computer-generated random numbers. For the participants recruitment, a well-designed electronic poster included the QR code and basic information about the project was delivered to the sampled eligible participants. After the online recruitment, 245 doctors and nurses who consented to participate in our study were enrolled in the present study and participate in the online questionnaire.
This study has been approved by the Ethics Committee of Shenzhen Qianhai Shekou Free Zone Hospital. All participants have provided online informed consent to participate in this study at the beginning of the questionnaire. Before the investigation, all participants were informed about the study background, aim, anonymous responses, confidential use of data, and voluntary participation principles.
Each participant's age, sex, job type, education level, job title, years of working, employment type, annual income, marital status, and place of residence were asked in this study.
To investigate individual health conditions, three variables were collected, including the history of receiving psychological help, chronic disease, and self-rated overall physical condition. The situation of the history of receiving psychological help and chronic disease were divided into “yes” and “no.” Individuals' self-rated overall physical condition was categorized into “healthy/good” and “general or below.”
Night duty condition and weekly working hours were utilized to assess job-related factors. The night duty condition was categorized as “yes” and “no.” According to the working hours standard of healthcare workers in China, weekly worktime was divided into “under 42 h,” “42–58 h,” and “over 58 h.”
The COVID-19-related factors comprised four variables, including whether working in the COVID-19-related departments or not (such as fever clinics), the change of total workload compared to pre-epidemic, the change of normal workload (non-COVID-19-related daily work) compared to pre-epidemic, and percentage of COVID-19-related work. The epidemic-related department was divided into “yes” or “no.” Options for total work compared to pre-epidemic and daily work compared to pre-epidemic included “decreased,” “steady,” and “increased.” The proportion of work related to epidemic prevention and control in the total workload was expressed as a percentage.
The validated Chinese version of the 10-item Center for Epidemiologic Studies Depression scale (CESD-10) (46) was used to measure depression. This measure was scored on a four-point Likert scale ranging from 0 (“Never”) to 3 (“Almost every day”) consisting of 10 items. The total score ranges from 0 to 30. The higher score indicated worse depression symptoms and a CESD-10 score ≥10 was indicative of depressive symptoms (47). The scale has been widely used in Chinese adults (48, 49) and has good reliability and validity (50). The Cronbach's alpha for CESD-10 was 0.74 in this study.
The validated Chinese version of the 7-item General Anxiety Disorder scale (GAD-7) was used to measure anxiety. The GAD-7 was developed by Spitzer et al. (51) and translated into Chinese by He et al. (52). It has been previously used in Chinese populations and found to be valid and reliable (53, 54). This measure was scored on a four-point Likert scale ranging from 0 (“none”), 1 (“a few days”), 2 (“more than half the days”), and 3 (“almost every day”) and consisted of seven items. The total score ranges from 0 to 21. The higher score showed worse anxiety symptoms and a GAD-7 score ≥5 was indicative of having anxiety symptoms. The Cronbach's alpha for GAD-7 in this study was 0.93.
The severity of insomnia symptoms was assessed by the Insomnia Severity Index (ISI) (55, 56). Each item is scored from 0 (“none”/“very satisfied”) to 4 (“very severe”/“very dissatisfied”), with a total score from 0 to 28. The psychometric properties of the ISI Chinese version have been validated in Chinese populations (57, 58). Higher scores indicated more severe insomnia. In our study, the Cronbach's alpha coefficient was 0.92.
The 10-item Work-Family Conflict Scale (WFCS) designed by Netemeyer et al. (59) was utilized to evaluate healthcare workers' work-family conflict. The scale included two subscales, corresponding to work-to-family conflict and family-to-work conflict, respectively. Each subscale included five items. Each of the items is scored from 1 (“totally disagree”) to 5 (“totally agree”). The Chinese version of WFCS had good reliability and validity in previous studies (60–62). Higher scores indicated a higher level of work-family conflict. The Cronbach's alpha for WFCS in the current study was 0.88.
The 10-item Connor-Davidson Resilience Scale (CD-RISC-10) (46, 63) was used to measure resilience, capturing the core features of resilience over the preceding month. Items were scored on a five-point Likert scale ranging from 0 (“never”) to 4 (“always”), where higher scores represented better psychological resilience. The total score ranged from 0 to 40. This psychological resilience inventory was demonstrated to have good reliability and validity in the Chinese context (64–66). In this study, the Cronbach's alpha for CD-RISC-10 was 0.94.
In the present study, the Chinese version of Maslach's Burnout Inventory-Human Services Survey (MBI-HSS) (67) with 17 items was used to assess the extent of job burnout of healthcare workers, revised by Zhang (68). This version of MBI-HSS-17 has been proved to have good reliability and validity when revised (68), and has been widely used in previous studies (69, 70). It comprised a total of 17 items that measure job burnout on a seven-point Likert scale, containing three dimensions: emotional exhaustion (EE, seven items), depersonalization (DA, three items), and personal accomplishment (PA, seven items). The participants were asked to rate the extent of their agreement from 0 (“totally disagree”) to 6 (“totally agree”). The dimension of personal accomplishment was reverse-scored. The rating score ranged from 0 to 102, and a higher score indicated a higher degree of job burnout. In this study, MBI-HSS-17 showed good internal consistency with a Cronbach's alpha of 0.79. Meanwhile, Cronbach's alphas for EE, DA, and PA were 0.70, 0.80, and 0.79, respectively.
Descriptive analyses were used for background characteristics. The results were expressed as the percentage value for categorical data and mean ± standard deviation for continuous data. To analyze Chi-square test or Fisher's exact test was used to compare the between-group difference. Hierarchical logistic regression analyses were conducted to investigate the association between main predictor variables and mental health outcomes (depressive symptoms, anxiety symptoms and their co-occurrence).
We adopted three models in the multivariate logistic regression. First, we adjusted for socio-demographic characteristics and mental health outcomes using logistic regression in model 1. Second, we additionally adjusted for individual-health-related factors, job-related factors and COVID-19-related factors in model 2. Third, to examine whether psychological factors were affected with mental health outcomes, we additionally entered all the psychological factors in model 3. The analysis procedure of model 1–3 was carried out for each of the three outcomes. The odds ratios (ORs) and 95% confidence intervals (CI) were presented. Two-sided tests with P < 0.05 were considered statistically significant. All data analyses were conducted using the statistical data analysis package for social sciences SPSS v.260 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp) (71).
A total of 245 participants participated in this study. The mean age of the participants was 37.5 ± 8.2 years, and most participants were aged from 30 to 50 years at the time of data collection (76.7%). More females (72.2%) participated in this survey, and 56.3% of the participants were doctors. The participants had relatively high levels of education levels, with most of the participants (93.9%) having an educational level of undergraduate or above. More than half of the participants (76%) had intermediate or higher job titles. Table 1 shows the prevalence of depressive and anxiety symptoms among healthcare workers and the characteristics of the factors studied.
In this study, 34.7% of healthcare workers experienced depression symptoms. Table 2 shows the results of hierarchical logistic regressions for depressive symptoms. First, model 1 assessed the relationship between socio-demographic characteristics and depressive symptoms. Junior or lower job title (OR = 0.199, 95% CI 0.044–0.899) was found to be associated with lower odds in depressive symptoms. After adjustment for all socio-demographic variables, model 2 showed that no history of receiving psychological help (OR = 0.179, 95% CI 0.040–0.793) and healthier self-rated overall physical condition (OR = 0.289, 95% CI 0.116–0.717) had decreased odds of depressive symptoms. In model 3, a higher score of ISI (OR = 1.311, 95% CI 1.165–1.475) and MBI-HSS-17 (OR = 1.108, 95% CI 1.045–1.175) had a positive association with depressive symptoms, whereas a higher score of CD-RISC-10 (OR = 0.837, 95% CI 0.751–0.934) had a negative association with depressive symptoms.
The prevalence of anxiety symptoms was 59.6% in this study. Table 3 shows the results of hierarchical logistic regressions for anxiety symptoms. In model 2, after adjustment for all socio-demographic variables, healthier self-rated overall physical condition (OR = 0.310, 95% CI 0.112–0.858) had decreased odds of anxiety symptoms, whereas 42–58 weekly working hours (OR = 4.507, 95% CI 1.629–12.473) had increased odds of anxiety symptoms. Model 3 found that a higher score of ISI (OR = 1.156, 95% CI 1.057–1.264), WFCS (OR = 1.103, 95% CI 1.012–1.212), and MBI-HSS-17 (OR = 1.070, 95% CI 1.022–1.121) had a positive association with depressive symptoms.
The co-occurrence of the symptoms of depression and anxiety among healthcare workers was 33.1% in this study. Table 4 shows the results of hierarchical logistic regressions for co-occurrence of depressive and anxiety symptoms. After adjustment for all socio-demographic variables, Model 2 showed that no history of psychological help (OR = 0.162, 95% CI 0.036–0.736) and healthier self-rated overall physical condition (OR = 0.251, 95% CI 0.099–0.636) had decreased odds of the co-occurrence. Model 3 found that a higher score of ISI (OR = 1.285, 95% CI 1.146–1.441) and MBI-HSS-17 (OR = 1.126, 95% CI 1.058–1.199) had a positive association with the co-occurrence, whereas a higher score of CD-RISC-10 (OR = 0.842, 95% CI 0.757–0.937) had a negative association with the co-occurrence.
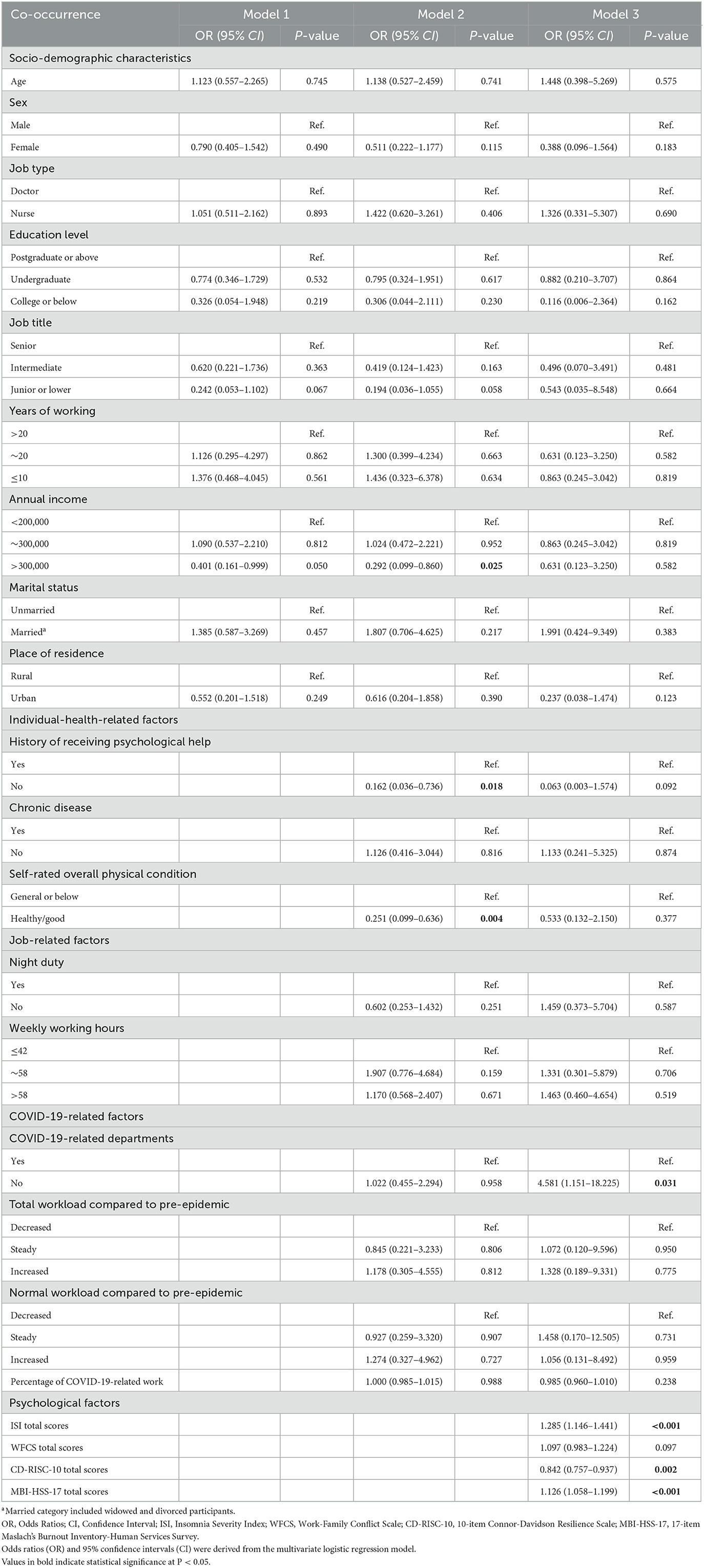
Table 4. Logistic regression analysis of the co-occurrence of the symptoms of depression and anxiety in the participants.
This study examined the prevalence of depressive symptoms, anxiety symptoms, and their co-occurrence among Chinese healthcare workers during the post-pandemic era and to identify key socio-demographic, job-related and psychological correlates of these disorders. We found a prevalence of 34.7% for depressive symptoms, 59.6% for anxiety symptoms, and 33.1% for the co-occurrence of depressive and anxiety symptoms. Our results showed that for depressive symptoms, anxiety symptoms and their co-occurrence, no history of receiving psychological help and self-rated good or higher health were protective factors, whereas more severe insomnia and job burnout were risk factors. Junior or lower job title and a higher score of psychological resilience were related to a lower prevalence of depressive symptoms, while relatively longer working hours and larger work-family conflict were positively associated with the anxiety symptoms. At the same time, a higher score of psychological resilience was inversely associated with co-occurrence of depressive and anxiety symptoms.
Lasting almost for 3 years, healthcare workers have been playing a major role in fighting against COVID-19 and might suffer from a large burden of psychological problems. Understanding their level of depressive/anxiety symptoms and associated factors can help hospital management and government policymakers to take effective measures to enhance the mental health status of healthcare workers, thus improving their professional performance and work efficiency. Our study conducted a cross-sectional survey on mental health status among healthcare workers in the post-pandemic era of COVID-19, about the third year since the first wave. The prevalence rates of depressive and anxiety symptoms for healthcare workers in the post-pandemic era were generally comparable to those observed in previous studies during the COVID-19 pandemic era, but different from the prevalence before the pandemic. In this study, we found that the prevalence of depressive symptoms was 34.7%, which was nearly in line with that reported by Deng et al. in a meta-analysis (72) (31%) and Tong et al. (7) (37%) among healthcare workers in the early stages of the COVID-19 pandemic in China. Compared to Lai et al.'s study (5) (50.4%) among healthcare workers at the peak of the pandemic in China, our study found a lower prevalence in the post-pandemic era, which may be because of the potential decreased fear and uncertainty from a better understanding of the COVID-19 and some appropriate interventions taken to relieve depressive symptoms during the pandemic. The prevalence of depressive symptoms was almost consistent with that reported by Liang et al. (73) (39.5%) in the late stage of the COVID-19 pandemic, which proved that the prevalence of depressive symptoms remains relatively high level in the post-pandemic. For anxiety symptoms, our study found a higher prevalence than the meta-analysis [40% reported by Deng et al. (72)] and previous studies among healthcare workers in China reported by Li et al. (31) (20.6%) and Lai et al. (5) (44.6%) during the COVID-19 pandemic era. Moreover, the prevalence of anxiety symptoms was higher than that reported by Liang et al. (73) (26.0%) in the late stage of the COVID-19 pandemic. The reason for the higher prevalence in our study may result from different pressure from life and work and different prevention and control measures for healthcare workers living in different areas. Our findings first showed that there were as high as 33.1% of healthcare workers suffering from the co-occurrence of depressive and anxiety symptoms, which was higher than that in Cameroon (14.73%) during the COVID-19 pandemic era (74). Moreover, consistent with our results, previous studies have reported an increase in healthcare workers' levels of depressive and anxiety symptoms as the COVID-19 outbreak continued (25). A study on Southeast Asian adults (75) also showed a higher prevalence of psychological problems after 18 months of the declaration of the pandemic compared to the 1st year. In the present study, we are the first study to report the high prevalence of depressive and anxiety symptoms as well as the co-occurrence among healthcare workers at a tertiary hospital in Shenzhen, a city with a large transient population, suggesting a long-lasting psychological impact of the pandemic among healthcare workers in the future. Given the widespread psychological crisis among healthcare workers in the post-pandemic era of COVID-19, it is necessary to provide various support to promote their psychological health in the post-pandemic era.
The findings of our study found few socio-demographic characteristics associated with the prevalence of depressive and anxiety symptoms among healthcare workers in the post-pandemic era. In this study, a junior or lower job title was a protective factor for the development of depressive symptoms in healthcare workers in the post-pandemic era of COVID-19. However, the results regarding job titles were inconsistent with previous studies during the COVID-19 pandemic in China. A meta-analysis during the COVID-19 epidemic has proved that healthcare workers with lower job titles have higher prevalence rates of depressive symptoms than those with higher job titles (76). A cross-sectional study in Anhui Province has also showed that the depression level of healthcare workers with middle and junior job titles were higher than those with senior titles during the pandemic (77). This difference might be due to the different demands for healthcare workers with different job titles at different stages of the epidemic. During the COVID-19 pandemic, due to the continuous outbreaks of the epidemic, a large number of healthcare workers with low job titles were assigned to perform the large-scale nucleic acid testing and epidemic-related prevention and control work. Therefore, the influence of lower job title on the level of depressive symptoms was more obvious. However, in the post-pandemic era, with the maturity of the overall level of epidemic prevention and control, the demand for healthcare workers with lower job titles was not as great as that during the epidemic. The difficulties in medical work have gradually returned to positions with higher job titles requiring higher level of medical technology. Therefore, lower job titles replaced the place of risk factor during the pandemic as a protective factor for depressive symptoms among healthcare workers in the post-epidemic era. Our results suggest that in the post-pandemic era, more attention should be paid to depressive symptoms among healthcare workers with high job titles in the post-pandemic era. However, further research is required to investigate the association between job titles and depressive symptoms, and individualized interventions might be more useful for healthcare workers in different regions of our country.
Although chronic disease condition, night duty condition and COVID-19-related factors, including whether working in a COVID-19-related department or not, the change of the COVID-19-related total/normal workload compared to pre-epidemic, or the percentage of COVID-19-related work were not statistically significant in our logistic regression models, our results showed that the level of anxiety symptoms for people with longer weekly working hours (42–58 h) was significantly higher than shorter weekly working hours ( ≤ 42 h). Increased working hours were one of the important factors contributing to developing anxiety symptoms, and similar findings have been reported in studies during the pandemic (18, 32). Our study showed that the increase in working hours was still an important factor affecting psychological status, with a greater effect on anxiety symptoms among traditional job-related factors in the post-pandemic era. Besides, no history of psychological help was shown to be protective factors for depressive and the co-occurrence in the post-pandemic era, which was inconsistent with previous study (27). The reason may be that the effect of psychological help is diminishing as the epidemic continues to develop. During the epidemic, timely psychological help had a good effect on the relief of healthcare workers who just suffered from stress brought by the epidemic, so the popularity rate of psychological help has been greatly improved. Therefore, in the post-pandemic era, people who have not received psychological help may be those with milder psychological problems. The result inspires us that in order to improve the effect of psychological help on psychological problems in the post-epidemic era, it is necessary to reform the content, form and scope of psychological help. Moreover, good or higher self-rated overall physical condition was inversely associated with depressive symptoms, anxiety symptoms and their co-occurrence in the post-pandemic era, same as the case in previous study during the pandemic (20). Our result suggests that, as during the pandemic, physical condition remains a very important factor in psychological problems in the post-pandemic era. The main reason for the non-significant association of COVID-19-related factors may be that the role of COVID-19 related work effects may have become smaller, or that our survey time was too short to cover various stages of the pandemic to better indicate the impact of work factors. In the future, the impact of COVID-19-related factors on the mental health of healthcare workers in the post-pandemic era needs further research.
Consistent with previous studies (20, 35) during the pandemic, healthcare workers with insomnia were found more likely to have depressive and anxiety symptoms than those with good sleep quality in the post-pandemic era. A study conducted in Bangladesh (35) reported that physicians who were suffering from sleep problems had a higher level of depressive symptoms compared to those who had never suffered from sleep problems. Cheng et al. also demonstrated a moderate association between the level of anxiety and sleep quality among pediatric healthcare workers (20). In fact, several studies have shown a link between insomnia and mental conditions including depression and anxiety during the COVID-19 pandemic in different countries (78–80). The finding suggests that insomnia was a relatively long-lasting factors both during the pandemic and post-pandemic era. Continuous measures should be taken to enhance their sleep quality to improve the mental health status of healthcare workers.
We found that people with a higher level of psychological resilience had a lower level of depressive symptoms and co-occurrence in the post-pandemic era, which agreed with previous studies during the COVID-19 pandemic (39, 80). The finding might be explained by the fact that healthcare workers with different levels of resilience could moderate the effects of perceived stress on depression by adopting different coping styles (81). In the post-pandemic era, our study found that work-family conflict was still be positively associated with anxiety symptoms while job burnout was also found to be positively associated with depressive symptoms, anxiety symptoms and their co-occurrence among healthcare workers, which were also confirmed in other studies during the pandemic (41, 42, 82–84). Lv et al. stated that healthcare workers with high levels of work-family conflict are particularly vulnerable to mental health problems (41). A study in Brazil also reported a positive relationship between burnout and depressive symptoms among workers at a university hospital (19). On the one hand, the workload and working hours of healthcare workers would fluctuate as the pandemic evolved, which was inevitable to bring negative effects to their family life (85) such as increased work-family conflict and thereby increased the level of anxiety symptoms (86). On the other hand, in the post-pandemic era of COVID-19, the uncertainty and variable conditions related to the pandemic can lead to role pressure for their families (87) and in the hospital and aggravate the severity of their work-family conflict (88). Healthcare workers' job burnout will not only reduce work efficiency and cause medical malpractices (89), but also increase the risk for depressive symptoms (90). In the hospital workplace, many healthcare workers might become burnout due to work-family conflict and the doctor-patient relationship in the post-pandemic era, being unable to cope with negative emotions and thus falling into a depressive and anxious state (91). We proved that psychological factors are important for depressive and anxiety symptoms both in the pandemic and the post-pandemic era. However, our study also showed that in the post-pandemic era, work-family conflict mainly positively affected anxiety symptoms, while job burnout positively affected depressive symptoms, anxiety symptoms, and their co-occurrence. Our results suggest that actions can be go on to alleviate work-family conflict and job burnout to decrease mental health problems and enhance positive cognition in healthcare workers in the post-pandemic era (88). Moreover, in designing psychological intervention strategies during the post-epidemic era, more consideration can be given to starting from job burnout, which may have better effects and solve psychological problems more efficiently.
Our study was the first to investigate the mental health problems in the post-pandemic era in China, especially in the special period with under-control pandemic due to very strict routine prevention and control measures. Furthermore, to our knowledge, no study has explored the factors associated with mental health problems among healthcare workers in this special period and we have investigated a variety of factors of depressive and anxiety symptoms and their co-occurrence. Our study indicates that the mental health among healthcare workers in the post-pandemic era needs more attention, and timely screening and early intervention are needed. The results also indicate that there are some common factors during the pandemic and the post-pandemic era. It is reasonable that some factors such as poor sleep quality, work-family conflict, and job burnout in healthcare workers that pose a threat to their mental health during the COVID-19 pandemic may continue to exist in the post-pandemic era. But with the dynamic change in individual psychological status such as worrying about being infected and other factors such as workload under different social background, we considered that the effect of these factors may be different in the development of mental health problems at the two different stages. For example, in our study, we found that higher job titles have negative effect on mental health in post-pandemic era, which was different from the findings during the pandemic (76, 77). The finding might be explained by the higher psychological stress and burnout due to very long duration to cope with different tasks from the regular prevention of COVID-19 pandemic. Therefore, it would be interesting for researchers to explore the difference in the effect of such factors on depressive and anxiety symptoms between the two periods. Our study also had some important implications. In our study, lower job titles and no history of receiving psychological help are protective factors in the post-epidemic era, which suggested that healthcare authorities and policymakers should focus more on healthcare workers with higher job titles and longer working hours. Compared to other types of healthcare workers, regular psychological interventions should be offered to them with priority. Moreover, psychological-related measures should be considered more important in daily preventive and therapeutic actions. It would be better to improve sleep facilities, optimize work arrangements, enrich psychological adjustment courses and so on, in order to improve resilience and ease the level of insomnia, work-family conflict and job burnout. As the influencing factors of both depression and anxiety and their co-occurrence in our study, healthier physical condition, insomnia and job burnout were the three factors that deserve the most attention when developing related prevention strategies in the post-pandemic era. Based on the above discussion, relevant authorities can further improve the mental health among healthcare workers in the post-pandemic era by offering regular physical check-ups and advice, alleviating insomnia, reducing work-family conflict and burnout, and improving psychological resilience. However, considering data on the risk factors of mental health problems among healthcare workers in the post-pandemic era remains lacking, much more studies are warranted to support the findings in our study.
Several limitations of this study should be noted. Firstly, data were collected through an online survey platform, which may lead to potential reporting bias due to social desirability. Secondly, all respondents of this study were healthcare workers at one hospital in Shenzhen, which may affect the representativeness of the samples, and whether the results of this study are applicable to healthcare workers in other regions during the post-pandemic era remains to be further studied. However, in the study period, majority of hospitals face with the similar situation for healthcare workers, where a series of strict prevention measures were taken to control the epidemic of COVID-19. Healthcare workers not only did the daily healthcare works, but also have to be involved in the COVID-19 prevention related works such as large-scale nucleic acid testing. Under the same country-level background of the post-pandemic era with routine prevention and control measures embedded, we think the study findings have a higher possibility to be applied to the similar hospital in other areas event outside Shenzhen. Besides, we sent out questionnaires to 400 recruited subjects, but only received 245 ones in our study, with a relatively low response rate of 61.25%. We cannot make a comparison of the demographic information between the respondents and non-respondents, because we conduct an anonymous investigation and we cannot identify the personal information of the non-respondents. However, similar studies of healthcare workers during the COVID-19 pandemic also had a response rate of around 60% (92, 93). This might depend on the nature of studied populations (94). According to the study of Rindfuss et al. (95), no evidence of bias was found from low response rates when examining the relationships in a multivariate analysis controlling for a variety of background variable, suggesting the reliability of our findings on the two hypotheses. Moreover, a cross-sectional design was conducted among healthcare workers at a tertiary hospital in Shenzhen in this study, so it is difficult to determine the direction or causality among the studied variables based on our data. In measuring mental health status at only one point, our study lacks relevant data about depressive and anxiety status and other variables before and during the pandemic, preventing us from comparing psychological symptoms interested in different periods. Finally, although depressive and anxiety symptoms are regarded as the main psychological problems on healthcare workers in our study, other psychological factors such as insomnia, job burnout and work-family conflict may also be influenced by the above two symptoms. The potential reverse effects among these variables remain to be further explored. If possible, the form of field questionnaire would allow us to obtain more reliable information in the process of collection and analysis in future. In the aspect of sampling method, we should formulate better sampling rules and certain prize mechanism, so as to improve the representativeness of samples and the response rate of questionnaires. A longitudinal study is required to evaluate the prevalence of depressive and anxiety symptoms, the ascertained directions of the associations and other potential psychological factors with the constant changes of COVID-19 during the post-pandemic era, and multi-center studies are needed to justify the findings of this study in the region.
To conclude, mental health problems were common among healthcare workers in Shenzhen during the post-pandemic era of COVID-19, with 34.7, 59.6, and 33.1% of healthcare workers reporting depressive and anxiety symptoms and their co-occurrence, respectively. We identified that job title, physical condition, insomnia, psychological resilience, work-family conflict and job burnout were still significant factors on healthcare workers' mental health, same as the case during the pandemic. Some factors such as job title during the pandemic may also play a role in the post-pandemic era, but with different effects. The findings suggest that healthcare authorities and policymakers should adopt targeted interventions, offer regular physical advice, provide professional psychological counseling, and strengthen communication among colleagues and leaders, thus improving mental health and reducing the appearance of psychological problems such as depression and anxiety symptoms in healthcare workers.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Shenzhen Qianhai Shekou Free Zone Hospital. The patients/participants provided their written informed consent to participate in this study.
ZL wrote the first draft of the paper. YW and XW carried out the conception and design of the research. JM, JW, and SH participated in the acquisition of data. ZL and WW carried out most of the data collection. The work was critically revised by PQ. All authors commented on previous versions of the paper, as well as read, and approved the final version.
We sincerely thank all participants who had contributed, particularly those who helped in collecting data, distributing questionnaires, and participating in our research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization. Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. (2020). Available online at: https://www.whoint/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed February 11, 2020).
2. World Health Organization. Who Director-General's Opening Remarks at the Media Briefing on COVID-19-11 May 2020. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed March 11, 2020).
3. World Health Organization. Weekly Epidemiological Update on COVID-19 - 21 September 2022. (2022). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—21-september-2022 (accessed September 21, 2022).
4. Steffens NK, LaRue CJ, Haslam C, Walter ZC, Cruwys T, Munt KA, et al. Social identification-building interventions to improve health: A systematic review and meta-analysis. Health Psychol Rev. (2021) 15:85–112. doi: 10.1080/17437199.2019.1669481
5. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. J Am Med Assoc Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
6. Juliana N, Mohd Azmi NAS, Effendy N, Mohd Fahmi Teng NI, Azmani S, Baharom N, et al. Exploring the associated factors of depression, anxiety, and stress among healthcare shift workers during the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:159420. doi: 10.3390/ijerph19159420
7. Tong F, Zhang L, Huang L, Yang H, Wen M, Jiang L, et al. The psychological impact of COVID-19 pandemic on healthcare workers. Front Public Health. (2022) 10:963673. doi: 10.3389/fpubh.2022.963673
8. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
9. Dong F, Liu HL, Yang M, Lu CL, Dai N, Zhang Y, et al. Immediate psychosocial impact on healthcare workers during COVID-19 pandemic in China: A systematic review and meta-analysis. Front Psychol. (2021) 12:645460. doi: 10.3389/fpsyg.2021.645460
10. Wu F, Lin W, Liu P, Zhang M, Huang S, Chen C, et al. Prevalence and contributory factors of anxiety and depression among pregnant women in the post-pandemic era of COVID-19 in Shenzhen, China. J Affect Disord. (2021) 291:243–51. doi: 10.1016/j.jad.2021.05.014
11. Konradsen H, Brodsgaard A, Ostergaard B, Garcia-Vivar C, Svavarsdottir EK, Dieperink KB, et al. The COVID-19 post pandemic: Family nursing now more than ever. J Fam Nurs. (2023) 29:3–5. doi: 10.1177/10748407221147965
12. China SCIOotPsRo. Fighting COVID-19: China in Action. (2020). Available online at: http://www.scio.gov.cn/zfbps/ndhf/42312/Document/1682143/1682143.html (accessed June 07, 2020).
13. Ren FF, Guo RJ. Public mental health in post-COVID-19 era. Psychiatr Danub. (2020) 32:251–5. doi: 10.24869/psyd.2020.251
14. Vervoort D, Luc JGY, Percy E, Hirji S, Lee R. Assessing the collateral damage of the novel coronavirus: A call to action for the post-COVID-19 era. Ann Thorac Surg. (2020) 110:757–60. doi: 10.1016/j.athoracsur.2020.04.015
15. Jiang M, Shao X, Rao S, Ling Y, Pi Z, Shao Y, et al. Emotional state of Chinese healthcare workers during COVID-19 pandemic. Front Psychol. (2022) 13:854815. doi: 10.3389/fpsyg.2022.854815
16. Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
17. Islam MS, Sujan MSH, Tasnim R, Sikder MT, Potenza MN, van Os J. Psychological responses during the COVID-19 outbreak among University Students in Bangladesh. PLoS ONE. (2020) 15:e0245083. doi: 10.1371/journal.pone.0245083
18. Hacimusalar Y, Kahve AC, Yasar AB, Aydin MS. Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. J Psychiatr Res. (2020) 129:181–8. doi: 10.1016/j.jpsychires.2020.07.024
19. Lopes MCC, Oliva CCC, Bezerra NMS, Silva MT, Galvao TF. Relationship between depressive symptoms, burnout, job satisfaction and patient safety culture among workers at a University Hospital in the Brazilian Amazon Region: Cross-sectional study with structural equation modeling. São Paulo Med J. (2022) 140:412–21. doi: 10.1590/1516-3180.2021.0614.15092021
20. Cheng FF, Zhan SH, Xie AW, Cai SZ, Hui L, Kong XX, et al. Anxiety in Chinese pediatric medical staff during the outbreak of coronavirus disease 2019: A cross-sectional study. Transl Pediatr. (2020) 9:231–6. doi: 10.21037/tp.2020.04.02
21. Sim SK, Lau BL, Zaila SR, Hazira N, Aniqah NM, Panicker J, et al. Psychological symptoms among healthcare workers handling COVID-19 patients. Med J Malaysia. (2021) 76:138–44.
22. Al Hariri M, Hamade B, Bizri M, Salman O, Tamim H, Al Jalbout N. Psychological impact of COVID-19 on emergency department healthcare workers in a tertiary care center during a national economic crisis. Am J Emerg Med. (2022) 51:342–7. doi: 10.1016/j.ajem.2021.10.055
23. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
24. Diktas H, Oncul A, Tahtasakal CA, Sevgi DY, Kaya O, Cimenci N, et al. What were the changes during the COVID-19 pandemic era concerning occupational risks among health care workers? J Infect Public Health. (2021) 14:1334–9. doi: 10.1016/j.jiph.2021.06.006
25. Miao X, Wang W, Chen Y, Huang X, Wang R. Psychological stress and influencing factors of hospital workers in different periods under the public health background of infectious disease outbreak: A cross-sectional study. Health Sci Rep. (2022) 5:e834. doi: 10.1002/hsr2.834
26. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
27. Dosil Santamaria M, Ozamiz-Etxebarria N, Redondo Rodriguez I, Jaureguizar Alboniga-Mayor J, Picaza Gorrotxategi M. Psychological impact of COVID-19 on a sample of spanish health professionals. Rev Psiquiatr Salud Ment. (2021) 14:106–12. doi: 10.1016/j.rpsmen.2020.05.002
28. Efe Is E, Sahillioglu A, Demirel S, Kuran B, Mustafa Ozdemir H. Effect of COVID-19 pandemic on physical activity habits, musculoskeletal pain, and mood of healthcare workers. Sisli Etfal Hastanesi Tip Bulteni. (2021) 55:462–8. doi: 10.14744/semb.2021.87523
29. Tuna Ö, Ermis C. Mental health support program for healthcare professionals in a pandemic hospital in Turkey and its results on anxiety, depression, insomnia and sexual disorders. Psychiatr Danub. (2022) 34:564–71. doi: 10.24869/psyd.2022.564
30. Xu J, Liu X, Xiao Y, Fang X, Cheng Y, Zhang J. Effect of Eap psychological intervention on improving the mental health of medical workers under the novel coronavirus epidemic in China. Front Public Health. (2021) 9:649157. doi: 10.3389/fpubh.2021.649157
31. Li J, Xu J, Zhou H, You H, Wang X, Li Y, et al. Working conditions and health status of 6,317 front line public health workers across five provinces in China during the COVID-19 epidemic: A cross-sectional study. BMC Public Health. (2021) 21:106. doi: 10.1186/s12889-020-10146-0
32. Yang Y, Lu L, Chen T, Ye S, Kelifa MO, Cao N, et al. Healthcare worker's mental health and their associated predictors during the epidemic peak of COVID-19. Psychol Res Behav Manag. (2021) 14:221–31. doi: 10.2147/PRBM.S290931
33. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
34. Harris LM, Huang X, Linthicum KP, Bryen CP, Ribeiro JD. Sleep disturbances as risk factors for suicidal thoughts and behaviours: A meta-analysis of longitudinal studies. Sci Rep. (2020) 10:13888. doi: 10.1038/s41598-020-70866-6
35. Hasan MT, Anjum A, Biswas M, Hossain S, Alin SI, Koly KN, et al. A survey on depressive symptoms and its correlates amongst physicians in Bangladesh during the COVID-19 pandemic. Front Psychol. (2022) 13:846889. doi: 10.3389/fpsyg.2022.846889
36. Sisto A, Vicinanza F, Campanozzi LL, Ricci G, Tartaglini D, Tambone V. Towards a transversal definition of psychological resilience: A literature review. Medicina. (2019) 55:110745. doi: 10.3390/medicina55110745
37. Hajebi A, Abbasinejad M, Zafar M, Hajebi A, Taremian F. Mental health, burnout, and job stressors among healthcare workers during the COVID-19 pandemic in Iran: A cross-sectional survey. Front Psychiatry. (2022) 13:891430. doi: 10.3389/fpsyt.2022.891430
38. Bridgeman PJ, Bridgeman MB, Barone J. Burnout syndrome among healthcare professionals. Am J Health Syst Pharm. (2018) 75:147–52. doi: 10.2146/ajhp170460
39. Awano N, Oyama N, Akiyama K, Inomata M, Kuse N, Tone M, et al. Anxiety, depression, and resilience of healthcare workers in Japan during the coronavirus disease 2019 outbreak. Intern Med. (2020) 59:2693–9. doi: 10.2169/internalmedicine.5694-20
40. Elahi NS, Abid G, Contreras F, Fernandez IA. Work-family and family-work conflict and stress in times of COVID-19. Front Psychol. (2022) 13:951149. doi: 10.3389/fpsyg.2022.951149
41. Lv M, Tan X, Xing C, Zheng J, Han S. How family-work conflict influences post-traumatic growth among medical workers: A moderated mediation model. Front Psychol. (2021) 12:743970. doi: 10.3389/fpsyg.2021.743970
42. Küçükkaya B, Kahyaoglu Süt H. The relationship between turkish women's self-efficacy for managing work-family conflict and depression, anxiety and stress during the COVID-19 pandemic: A web-based cross-sectional study. Work. (2022) 22:190. doi: 10.3233/WOR-220190
43. Pien LC, Cheng WJ, Chou KR, Lin LC. Effect of work-family conflict, psychological job demand, and job control on the health status of nurses. Int J Environ Res Public Health. (2021) 18:73540. doi: 10.3390/ijerph18073540
44. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. Br Med J. (2020) 368:m1211. doi: 10.1136/bmj.m1211
45. Fu X, Zhang K, Chen X, Chen Z. National Mental Health Development Report of China (2019–2020). Beijing: Social Sciences Academic Press (2021).
46. Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (Cd-Risc): Validation of a 10-item measure of resilience. J Traumat Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
47. Chen H, Mui AC. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int Psychogeriatr. (2014) 26:49–57. doi: 10.1017/S1041610213001701
48. Chen Z, He Q, Shi Q, Xu Y, Yang H, Wei R. Anxiety and depression in dry eye patients during the COVID-19 pandemic: Mental state investigation and influencing factor analysis. Front Public Health. (2022) 10:929909. doi: 10.3389/fpubh.2022.929909
49. He C, Chen H, Guo L, Xu L, Liu Q, Zhang J, et al. Prevalence and factors associated with comorbid depressive symptoms among people with low back pain in China: A cross-sectional study. Front Psychiatry. (2022) 13:922733. doi: 10.3389/fpsyt.2022.922733
50. Mohebbi M, Nguyen V, McNeil JJ, Woods RL, Nelson MR, Shah RC, et al. Psychometric properties of a short form of the center for epidemiologic studies depression (Ces-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. Gen Hosp Psychiatry. (2018) 51:118–25. doi: 10.1016/j.genhosppsych.2017.08.002
51. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The Gad-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
52. He X, Li C, Qian J, Cui H, Wu W. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
53. Wang J, Zhou Y, Qian W, Zhou Y, Han R, Liu Z. Maternal insomnia during the COVID-19 pandemic: Associations with depression and anxiety. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1477–85. doi: 10.1007/s00127-021-02072-2
54. Xi SJ, Shen MX, Wang Y, Zhou W, Xiao SY, Tebes JK, et al. Depressive symptoms, anxiety symptoms, and their co-occurrence among people living with schizophrenia in China: Prevalence and correlates. J Clin Psychol. (2021) 77:2137–46. doi: 10.1002/jclp.23141
55. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
56. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
57. Mao W, Li F, Li B, Li Y, Zhang X, Ou Z, et al. Mental distress, quality of life and physical symptoms in Chinese women with ovarian cancer receiving olaparib treatment during the COVID-19 pandemic. Front Psychiatry. (2022) 13:915225. doi: 10.3389/fpsyt.2022.915225
58. Lu ZA, Shi L, Que JY, Zheng YB, Wang QW, Liu WJ, et al. Long-term psychological profile of general population following COVID-19 outbreak: Symptom trajectories and evolution of psychopathological network. Epidemiol Psychiatr Sci. (2022) 31:e69. doi: 10.1017/S2045796022000518
59. Netemeyer RG, Boles JS, McMurrian R. Development and validation of work–family conflict and family–work conflict scales. J Appl Psychol. (1996) 81:400. doi: 10.1037/0021-9010.81.4.400
60. Wang Y, Liu L, Wang J, Wang L. Work-family conflict and burnout among Chinese doctors: The mediating role of psychological capital. J Occup Health. (2012) 54:232–40. doi: 10.1539/joh.11-0243-OA
61. Hao J, Wu D, Liu L, Li X, Wu H. Association between work-family conflict and depressive symptoms among Chinese female nurses: The mediating and moderating role of psychological capital. Int J Environ Res Public Health. (2015) 12:6682–99. doi: 10.3390/ijerph120606682
62. Chen C. Survey on work-family conflict of nurses. Chin J Nurs. (2010) 45:629–30. doi: 10.3761/j.issn.0254-1769.2010.07.021
63. Cheng C, Dong D, He J, Zhong X, Yao S. Psychometric properties of the 10-item connor–davidson resilience scale (Cd-Risc-10) in Chinese undergraduates and depressive patients. J Affect Disord. (2020) 261:211–20. doi: 10.1016/j.jad.2019.10.018
64. Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: A comparison with the general population. Int J Environ Res Public Health. (2020) 17:186550. doi: 10.3390/ijerph17186550
65. Zhou S, Chen J, Lin H, Ye Y, Xiao Y, Ouyang N, et al. Associations among workplace bullying, resilience, insomnia severity, and subjective wellbeing in Chinese resident doctors. Front Psychiatry. (2022) 13:840945. doi: 10.3389/fpsyt.2022.840945
66. Liu D, Liu S, Zhu L, Li D, Huang D, Deng H, et al. Prevalence and related factors of insomnia among Chinese medical staff in the middle and late stage of COVID-19. Front Psychiatry. (2020) 11:602315. doi: 10.3389/fpsyt.2020.602315
67. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
68. Zhang S. Revision and application of Mbi-human services survey in Chinese police officers. Chin Mental Health J. (2006) 20:85. doi: 10.3321/j.issn:1000-6729.2006.02.004
69. Huang C, Xie X, Cheung SP, Zhou Y, Ying G. Job demands, resources, and burnout in social workers in China: Mediation effect of mindfulness. Int J Environ Res Public Health. (2021) 18:1910526. doi: 10.3390/ijerph181910526
70. Wu Y, Wei Y, Li Y, Pang J, Su Y. Burnout, negative emotions, and wellbeing among social workers in China after community lockdowns during the COVID-19 pandemic: Mediating roles of trait mindfulness. Front Public Health. (2022) 10:952269. doi: 10.3389/fpubh.2022.952269
71. IBM Corp. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp. (2019). Available online at: https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-26 (accessed November 21, 2022).
72. Deng Y, Chen Y, Zhang B. Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: A meta-analysis. Asian J Psychiatr. (2021) 56:102547. doi: 10.1016/j.ajp.2021.102547
73. Liang S, Liu C, Rotaru K, Li K, Wei X, Yuan S, et al. The relations between emotion regulation, depression and anxiety among medical staff during the late stage of COVID-19 pandemic: A network analysis. Psychiatry Res. (2022) 317:114863. doi: 10.1016/j.psychres.2022.114863
74. Mboua CP, Keubo FRN, Fouaka SGN. Anxiety and depression associated with the management of COVID-19 among healthcare workers in Cameroon. L' Evolution Psychiatrique. (2021) 86:131–9. doi: 10.1016/j.evopsy.2020.11.002
75. Tay WWY, Jesuthasan J, Wan KS, Ong T, Mustapha F. Eighteen months into the COVID-19 pandemic: The prevalence of depression, anxiety, and stress symptoms in Southeast Asia and the associated demographic factors. Front Public Health. (2022) 10:863323. doi: 10.3389/fpubh.2022.863323
76. Liu X, Wang G, Zhang J, Wang S. Prevalence of depression and anxiety among health care workers in designated hospitals during the COVID-19 epidemic: A meta-analysis. Chin J Evid Bas Med. (2021) 2021:1035–42. doi: 10.7507/1672-2531.202105079
77. Fang X-H, Wu L, Lu L-S, Kan X-H, Wang H, Xiong Y-J, et al. Mental health problems and social supports in the COVID-19 healthcare workers: A Chinese explanatory study. BMC Psychiatry. (2021) 21:2998. doi: 10.1186/s12888-020-02998-y
78. Youssef N, Mostafa A, Ezzat R, Yosef M, El Kassas M. Mental health status of health-care professionals working in quarantine and non-quarantine Egyptian hospitals during the COVID-19 pandemic. East Mediterr Health J. (2020) 26:1155–64. doi: 10.26719/emhj.20.116
79. Lewis R, Roden LC, Scheuermaier K, Gomez-Olive FX, Rae DE, Iacovides S, et al. The impact of sleep, physical activity and sedentary behaviour on symptoms of depression and anxiety before and during the COVID-19 pandemic in a sample of South African participants. Sci Rep. (2021) 11:24059. doi: 10.1038/s41598-021-02021-8
80. Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 109:110236. doi: 10.1016/j.pnpbp.2020.110236
81. Li P, Liang Z, Yuan Z, Li G, Wang Y, Huang W, et al. Relationship between perceived stress and depression in Chinese front-line medical staff during COVID-19: A conditional process model. J Affect Disord. (2022) 311:40–6. doi: 10.1016/j.jad.2022.05.064
82. López-Núñez MI, Díaz-Morales JF, Aparicio-García ME. Individual differences, personality, social, family and work variables on mental health during COVID-19 outbreak in Spain. Personal Individ Diff. (2021) 172:110562. doi: 10.1016/j.paid.2020.110562
83. Kusnierz C, Rogowska AM, Chilicka K, Pavlova I, Ochnik D. Associations of work-family conflict with family-specific, work-specific, and well-being-related variables in a sample of polish and Ukrainian adults during the second wave of the COVID-19 pandemic: A cross-sectional study. Int J Environ Res Public Health. (2022) 19:1710954. doi: 10.3390/ijerph191710954
84. Wan Mohd Yunus WMA, Badri SKZ, Panatik SA, Mukhtar F. The unprecedented movement control order (lockdown) and factors associated with the negative emotional symptoms, happiness, and work-life balance of malaysian university students during the coronavirus disease (COVID-19) pandemic. Front Psychiatry. (2020) 11:566221. doi: 10.3389/fpsyt.2020.566221
85. Cotrin P, Moura W, Gambardela-Tkacz CM, Pelloso FC, Santos LD, Carvalho MDB, et al. Healthcare workers in Brazil during the COVID-19 pandemic: A cross-sectional online survey. Inquiry. (2020) 57:46958020963711. doi: 10.1177/0046958020963711
86. Cai CZ, Lin YL, Hu ZJ, Wong LP. Psychological and mental health impacts of COVID-19 pandemic on healthcare workers in China: A review. World J Psychiatry. (2021) 11:337–46. doi: 10.5498/wjp.v11.i7.337
87. Wang H, Sun J. The negative effects of empowering leadership: Theoretical mechanisms and boundary conditions. Adv Psycholog Sci. (2022) 27:858–70. doi: 10.3724/SP.J.1042.2019.00858
88. Zhou H, Song X, Fang L, Shi K, Liu R. How empowering leadership influences medical workers' work–family conflict in the post-pandemic era: A moderated mediation model of leadership “Black Box”. Front Psychol. (2022) 13:870753. doi: 10.3389/fpsyg.2022.870753
89. Chen KY, Yang CM, Lien CH, Chiou HY, Lin MR, Chang HR, et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. (2013) 10:1471–8. doi: 10.7150/ijms.6743
90. Salvagioni DAJ, Melanda FN, Mesas AE, Gonzalez AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE. (2017) 12:e0185781. doi: 10.1371/journal.pone.0185781
91. Zheng G, Lyu X, Pan L, Chen A. The role conflict-burnout-depression link among Chinese female health care and social service providers: The moderating effect of marriage and motherhood. BMC Public Health. (2022) 22:230. doi: 10.1186/s12889-022-12641-y
92. Zakeri MA, Hossini Rafsanjanipoor SM, Zakeri M, Dehghan M. The relationship between frontline nurses' psychosocial status, satisfaction with life and resilience during the prevalence of COVID-19 disease. Nurs Open. (2021) 8:1829–39. doi: 10.1002/nop2.832
93. Zhang SX, Chen J, Afshar Jahanshahi A, Alvarez-Risco A, Dai H, Li J, et al. Succumbing to the COVID-19 pandemic-healthcare workers not satisfied and intend to leave their jobs. Int J Ment Health Addict. (2022) 20:956–65. doi: 10.1007/s11469-020-00418-6
94. Stefanowicz-Bielska A, Slomion M, Rapala M. Life satisfaction of nurses during the COVID-19 pandemic in Poland. Int J Environ Res Public Health. (2022) 19:2416789. doi: 10.3390/ijerph192416789
Keywords: healthcare workers, COVID-19, depressive symptoms, anxiety symptoms, prevalence
Citation: Liang Z, Wang Y, Wei X, Wen W, Ma J, Wu J, Huang S and Qin P (2023) Prevalence and associated factors of depressive and anxiety symptoms among healthcare workers in the post-pandemic era of COVID-19 at a tertiary hospital in Shenzhen, China: A cross-sectional study. Front. Public Health 11:1094776. doi: 10.3389/fpubh.2023.1094776
Received: 10 November 2022; Accepted: 28 February 2023;
Published: 20 March 2023.
Edited by:
Julian Chuk-Ling Lai, City University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Elodie Charbonnier, University of Nîmes, FranceCopyright © 2023 Liang, Wang, Wei, Wen, Ma, Wu, Huang and Qin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pei Qin, cWlucGVpMjI1QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.