
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 May 2023
Sec. Public Health Education and Promotion
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1091015
This article is part of the Research Topic Health Literacy and Disease Prevention, Volume II View all 23 articles
 Roy Rillera Marzo1,2*
Roy Rillera Marzo1,2* Ritankar Chakraborty3
Ritankar Chakraborty3 Shean Yih Soh4
Shean Yih Soh4 Hui Zhu Thew5
Hui Zhu Thew5 Collins Chong6
Collins Chong6 Ching Sin Siau7
Ching Sin Siau7 Khairuddin Bin Abdul Wahab1
Khairuddin Bin Abdul Wahab1 Indang Ariati Binti Ariffin1
Indang Ariati Binti Ariffin1 Shekhar Chauhan3
Shekhar Chauhan3 Ken Brackstone8
Ken Brackstone8 Bijaya Kumar Padhi9,10
Bijaya Kumar Padhi9,10 Petra Heidler11,12*
Petra Heidler11,12*Introduction: Vaccination programs have been rolled out across the globe to contain and mitigate the spread of the COVID-19 infection. Until recently, such programs were limited to adults and the older population, thereby limiting children from getting vaccinated. Recently, the Malaysian government rolled out vaccination for children aged 5–11 years. However, there are certain factors that might affect vaccination uptake among children. This study explores factors influencing parents’ hesitancy to vaccinate children in Malaysia.
Method: A nationwide online cross-sectional convenience sampling survey from April 21, 2022 to June 3, 2022 was conducted. The study used descriptive statistics to inform about vaccine hesitancy among parents. Cross-tabulation was performed to calculate the frequency and percentage of vaccine hesitancy, quality of life, e-health literacy, and the 5C psychological antecedents of vaccination among parents with children 5-11 years in Malaysia. Graphical methods were used to portray the levels of e-health literacy and levels of 5C psychological antecedents of vaccination. The study used both bi-variate and multivariate analysis to understand the relationship between vaccine hesitancy and the socio-demo-economic factors, quality of life, e-health literacy and 5C psychological antecedents.
Results: Of 382 participants, almost one-third (33%) of participants reported vaccine hesitancy for their children. For 5C’s psychological antecedents of vaccination, around one quarter (26.96%) reported disagreement for confidence in vaccination, almost half (52.36%) reported disagreement for vaccination complacency, three-fifths (60.99%) reported vaccination constraint, one quarter (25.92%) reported calculation antecedent, and almost one-third reported disagreement over collective responsibility antecedent (25.92%). Chi-square test revealed that gender, employment status, and parents’ COVID-19 vaccination status were significantly associated (p<0.05) with vaccine hesitancy among parents. Assessing the influence of transactional e-health literacy, only the communication component contained a significant association (p<0.05). Among the 5C psychological antecedents, confidence, calculation, and collective responsibility were significantly associated (p<0.05) with vaccine hesitancy. Parents with secondary [OR: 8.80; CI: 2.44−31.79, (p<0.05)], post-secondary [OR: 5.21; CI: 2.10-13.41, (p<0.05)], and tertiary education [OR: 6.77; CI: 2.25−20.35, (p<0.05)] had significantly higher likelihood of vaccine hesitancy than those with primary education.
Conclusion: Highly educated parents are more skeptical and are more likely to perceive the vaccine as unsafe and ineffective for their children. It is critical to disseminate the required information about the vaccine safety to the educated group.
The novel coronavirus disease (COVID-19) was first isolated from the Chinese city of Wuhan in December 2019, and has been the source of the most recent global health crisis (1–3). Malaysia detected its first three cases of COVID-19 before the declaration of pandemic status on 25 January 2020 (4–7). Since then, Malaysia has undergone multiple waves of COVID-19 infections. As of 5 October 2022, there were 4.85 million of confirmed COVID-19 cases in Malaysia, while there were 619 million cases globally at the same time (1, 2). Vaccination programs have been since rolled out across the globe to contain and mitigate the spread of the COVID-19 infection. The Malaysian government pledged its commitment toward the COVID-19 Vaccine Global Access (COVAX) partnership, which the World Health Organization (WHO) spearheaded (5). The administration of COVID-19 vaccines in Malaysia was administered via the National COVID-19 Vaccine Immunization Program (Program Imunisasi COVID-19 Kebangsaan – PICK), which began on 24 February 2021 (8)– (9). There were three vaccines first introduced to the country vaccination program, namely AZD1222 (AstraZeneca), BNT162b2 (Pfizer-BioNTech), and CoronaVac (Sinovac) (8, 9). On 23 September 2021, Malaysia began offering COVID-19 vaccines to adolescents in the country, primarily employing the BNT162b2 vaccine (10, 11). It was not until February 2022, however, that the same BNT162b2 vaccine was offered to children aged 5–11, while CoronaVac was too provided to this group in March 2022 (12).
Clinical evidence has shown the efficacies of these vaccines against COVID-19-related mortality, hospitalization, and symptomatic illness (8). Despite this, a small number of people may be unsure about the acceptance of certain vaccines. Vaccine hesitancy was defined by the Strategic Advisory Group of Experts on Immunization (SAGE) as “the delay in acceptance or refusal of vaccination despite the availability of vaccine services” (13, 14), and is regarded a certain hindrance for a country to achieve herd immunity against COVID-19.
A recent systematic review explored vaccine acceptance rates across the globe and found that Malaysia had the highest acceptance rate (94.3%) for COVID-19 (13, 15). Various studies have also explored the attitude of the Malaysian population toward COVID-19 vaccines and the phenomenon of vaccine hesitancy among adults (16, 17). However, these studies primarily focused on vaccine hesitancy rates among adults. A recently published study investigated parents’ willingness to vaccinate their children under 12 years old against COVID-19, and 73.6% of their participants were willing to vaccinate their children (18). Parental levels of vaccine hesitancy, together with parental knowledge and attitudes about the disease and vaccine, has been shown to predict willingness to vaccinate their children (3, 4).
Examining coronavirus-related issues has remained elusive in the Malaysian context as far as vaccine hesitancy for children is concerned, especially from the parents’ perspective. To our knowledge, there is no published study investigating the willingness of parents to vaccinate their adolescent children at the time of writing. However, authors found some studies pertaining to health literacy related to COVID-19 vaccination, although these studies did not examine health literacy from parent’s perspective as we intend to examine in this study (19, 20). Some countries have conducted surveys to investigate COVID-19 vaccine hesitancy among parents with children aged 5–11 years old. In the United States, 40.75% of Malaysian parents were willing to vaccinate their children (21). In research involving multiple Middle Eastern countries, 32% of children were vaccinated against COVID-19 (22). A quarter of mothers participating in a survey in Saudi Arabia expressed hesitancy about their children’s vaccination (23). There were also varying degrees of parental vaccine hesitancy among the Asian regions. Only 11.7–19.4% of parents expressed hesitancy in the Chinese cities of Shandong and Zhejiang (24), whereas 35.3% of Japanese parents were hesitant to vaccinate their children (25). In contrast, more than 70% of the parents in Hong Kong were hesitant to vaccinate their children (26). Some studies have applied health beliefs and planned behavior theoretical models (27–29) to examine the relationship between vaccine hesitancy and parental attitudes and beliefs.
The most consistent predictors of parents’ COVID-19 vaccine resistance for children 5–11 years are a lack of confidence in the safety and effectiveness of the vaccine, followed by lack of trust in government, perceptions that children are not susceptible to the disease, and a lack of community and family support for vaccinating children against COVID-19 (29–42). Positive attitudes toward vaccination experiences or outcomes may also play a role in predicting parental willingness to vaccinate their children (29). Demographic variables have also been associated with parental COVID-19 vaccine acceptance. These include higher parental income and education, and whether the parent has received the COVID-19 vaccination themselves (30, 32, 35). Racial and ethnic differences have also been reported. For example, Asian-American parents were most likely to vaccinate their 5–11-year-old and 12–17-year-old children, whereas non-Hispanic White parents were least likely (43, 44). These differences in parental intentions appear to coincide with the race and ethnicity of older children who have been vaccinated based on their share of the population (45).
The advancement of technology has a major influence on how health information is disseminated and received by the general public. The Transactional Model of eHealth Literacy was first proposed to define a hierarchy of skillsets that may have an impact on an individual’s healthcare engagement experience (46). For example, functional eHealth literacy is defined as basic skills in writing and reading about health on the internet; communicative eHealth literacy involves skills that allowed communication about health with other users on the online environment; and critical eHealth literacy refers to the ability to evaluate the information obtained and understand the risk in the sharing of such information. The ability to apply health knowledge obtained via the internet across different setting forms the highest cognitive level of eHealth literacy and this is termed translational eHealth literacy (46). Health literacy has been proposed as an important element in the fight against COVID-19 and higher health literacy has been associated with higher likelihood of intention to be immunized (47–49).
Further, the 5C model of psychological antecedents, which include confidence, complacency, constraint, calculation, and collective responsibility, is often used to predict vaccination hesitancy in a population (50, 51). Generally, people with greater confidence trust the safety and efficacy of COVID-19 vaccines, and also believe in the competence and reliability of their local healthcare service providers in delivering the vaccination program (32). On the contrary, people lacking confidence may adopt a conspiracy mentality with regards to vaccines, and worry about the harmful effects of vaccine (50). Complacency in the 5C model of psychological antecedents was defined as having low perceived risk of the vaccine-preventable disease and eventually deeming vaccination as unnecessary (50). In view of this, complacent people may express lower intention to receive vaccination. Constraints may be seen as barriers that impede the vaccination process. These barriers may include the accessibility, availability, and affordability of vaccines and the willingness-to-pay of the population (50). Calculation in the 5C model refers to people who would undergo extensive information gathering. Depending on the sources of information search, calculation may influence vaccination attitudes in diverse ways. For example, if anti-vaccination or vaccine - critical information was found, calculation would potentially lead to higher hesitancy (50).
Herd immunity is an important public health concept that can be used to mitigate the spread of an infectious disease. Consequently, some may be willing to receive vaccination in order to protect others within the community. This is termed collective responsibility (50).
Our study aimed to investigate Malaysian parents’ hesitancy, health literacy, and behaviors surrounding COVID-19 vaccinations of their children aged 5–11 years old, and to examine the psychological barriers that may prevent parents in Malaysia from getting their children vaccinated against the COVID-19 virus.
We conducted a nationwide online cross-sectional study in Malaysia from April 21, 2022 to June 3, 2022. The inclusion criteria of the study were as follows: parents with children 5–11 years, and currently a resident in Malaysia. Participants who were unable to read English, those not given consent, and non-citizens of Malaysia were excluded from the study. To calculate the required sample size for a single proportion, we used Pocock’s formula: n = Zα 2 p(1-p)/d2, where n = minimum required sample size, (Zα) = 1.96, d (precision) = 5%, and P = expected prevalence. Based on our extensive literature search, the prevalence of vaccine hesitancy was found to be within the range of 10 to 30%. Using these percentages, an estimated sample size of between 138 and 318 was required. The average provided a required minimum sample size of 227. Considering potential dropouts and incomplete forms (227 + [20%]), 275 was our target sample size. A total of 1,000 questionnaires were distributed with 38.2% response rate.
A pilot study was conducted prior to the actual data collection to test the survey questions, assess the feasibility of the study design, and identify any potential issues. An online survey was used for data collection because of the ongoing COVID-19 pandemic in the country. Participants were recruited using convenience sampling method. Questionnaires were disseminated via various social media platforms such as Instagram, Twitter, Facebook, WhatsApp, and Telegram. Participants completed an online consent form after confirming that they understood the purpose, risks, and benefits of the study. Time for completion of questionnaire was approximately 10–15 min. No incentive was offered for completing the questionnaire. We conducted a follow-up and reminder to ensure a higher response rate. Specifically, we sent a reminder email to all participants who had not completed the survey after 1 week. Face and content validity were considered satisfying by the multidisciplinary panel of five experts including a psychiatrist, clinical psychologist, physician, pharmacist, and public health expert for critical review, content, and face validity. All items were evaluated for necessity, clarity, and relevance. The content validity and face validity were 88 and 92%, respectively.
Malaysian participants indicated their age, gender (male, female), residential area (rural, urban), educational level (no formal education, primary, secondary, tertiary), marital status (single, married, divorced, widowed), employment (unemployed, part-time, full-time), religion (Christian, Buddhism, Muslim, Hinduism, Other, None), ethnicity, and household income.
Next, participants were asked about their perceived quality of life (“How would you rate your quality of life?”), which was rated on a 5-point Likert scale (1 = very poor; 5 = very good; M = 4.57, SD = 1.48). The higher score indicates better quality of life.
This was measured by a single item asking the participants to rate the extent they felt likely to vaccinate their children with the COVID-19 vaccine on a 6-point Likert scale (1 = very likely; 6 very unlikely; M = 4.57, SD = 1.48). Higher scores indicate greater hesitancy. A point greater than or equal to 4 was considered overall likely to vaccinate the child, whereas a point of less than 4 suggested that the parents were overall unlikely to vaccinate their child. So, a score of <4 was coded as 1 and was labelled as “Unlikely,” and a score of 4 and above was coded as 0 and labelled as “Likely” and thus converted into a binary variable.
The 5Cs were assessed using the previously validated 5C scale (32). The scale consisted of 15 items. Each of the Cs — Confidence, Constraints, Calculation, Complacency and Collective responsibility — were captured using three items. Responses were provided on a six-point Likert scale (1 = strongly disagree; 6 = strongly agree). The scale was adapted to focus on COVID-19 vaccinations.
All items were scored in a way such that a higher score indicates a higher degree of the C assessed. Internal consistency, as reflected by Cronbach’s alpha, were acceptable in our sample: Confidence α = 0.87, M = 4.57, SD = 1.48; Complacency α = 0.75, M = 4.57, SD = 1.48; Constraints α = 0.88 M = 4.57, SD = 1.48; Calculation α = 0.76, M = 4.57, SD = 1.48; Collective responsibility α = 0.77, M = 4.57, SD = 1.48.
The 5C psychological antecedents of vaccination consisted of 5 domains. Each of the domains had 3 questions which were measured using a 6-point Likert Scale (1 = strongly disagree; 6 = strongly agree). So, the total possible score of each domain was 18. A cumulative score of greater than 9 was taken as overall agreement to that domain, whereas a score of less than or equal to 9 was taken as overall disagreement to that domain. It was then recoded as 1 “Disagree” and 2 “Agree” and converted to a binary variable. Thus 5 binary variables were created for each domain of the 5C psychological antecedent of vaccination.
Participants’ vaccine literacy was captured by the COVID-19 vaccine literacy scale (45). The scale was comprised of four components, including functional, communication, critical, and translational skills. Each component was measured using four items on a 6-point Likert scale (1 = strongly disagree; 6 = strongly agree; α = 0.86, M = 4.57, SD = 1.48). The total score ranged from 16 to 48. The higher the score, the higher the COVID-19 vaccine literacy.
The anonymous survey data were confidentially stored with password-protected security standards. We utilized an online informed consent process that required participants to read and agree to the terms of participation before beginning the study. The online consent form provided participants with a clear explanation of the study’s purpose, procedures, risks, benefits, confidentiality, and the participant’s rights as a research subject, including information on the use and anonymization of the data and how survey responses guarantee the anonymity of each participant. Participants were also informed that their participation was voluntary, and they could withdraw at any time without consequence. We ensured that participants could only access the survey once to prevent multiple responses. This study was conducted according to the Declaration of Helsinki. Online informed written consent was obtained from all participants before the commencement of the study. Ethics approval was obtained from the Medical Research and Ethics Committee of the Management and Science University.
Vaccine hesitancy was taken as the primary outcome variable for this study. The variable was recoded as a binary variable (Yes = 1/No = 0) for the primary analysis. Socio-economic and demographic categorical predictors included gender, marital status, highest qualification level, household monthly income, ethnicity, religion, employment status, residential area, insurance status of the child, parents’ comorbidity status, comorbidity status of child, parents’ COVID-19 vaccination status, oldest child’s (5–11 years) COVID-19 vaccination status, side effects experienced by respondent after getting the COVID-19 vaccination, side effects experienced by the oldest child (5–11 years) after getting the COVID-19 vaccination, and risk perceptions about COVID-19. Quality of life, transactional e-health literacy, and 5C psychological antecedents to vaccination were also categorized based on scores from the Likert scale and included in the regression analysis.
The study used descriptive statistics to assess vaccine hesitancy among parents with children under 18 years old in Malaysia based on each socio-economic and demographic characteristics. Cross-tabulation was performed to calculate the frequency and percentage of vaccine hesitancy, quality of life, e-health literacy and 5C psychological antecedents of vaccination among parents with children 5–11 years in Malaysia. Graphical methods were used to portray the levels of e-health literacy and levels of 5C psychological antecedents of vaccination among the study subjects.
Next, the study used bi-variate and multivariate analysis to understand the relationship between vaccine hesitancy and the socio-demo-economic factors, quality of life, e-health literacy, and 5C psychological antecedents. Chi-square tests were performed to examine the association between vaccine hesitancy and the different predictor variables. p-values were reported to understand the significance of the association. Multivariate analysis included both unadjusted and adjusted binary logistic regressions with vaccine hesitancy as the binary outcome variable and the predictors as categorical variables.
The adjusted regression was performed taking into account all the predictor variables in a single model. This was used to understand the effect of a predictor variable on the outcome variable after adjusting for the effect of other predictor variables. Odds Ratios (OR) with 95% Confidence Intervals and p-values were reported to understand the significance of the relationship between the outcome variable and the predictor variables. ORs greater than 1 indicated a greater chance of vaccine hesitancy while ORs of less than 1 indicated a lesser risk of vaccine hesitancy.
Table 1 shows percentages of vaccine hesitancy among parents with children 5–11 years old for socio-economic and demographic characteristics. Of the 382 participants, 33% of respondents expressed hesitation in vaccinating their children. In Table 2, among those hesitant to vaccinate their children, the majority were married couples (68.3%). People with lower household income expressed lower hesitation in vaccinating their children, as were people with post-secondary and tertiary education. Among those who were unlikely to vaccinate their children, a majority (62%) were full-time employees and residing in rural areas (78.6%). Further, 73.0% of the hesitant parents had insurance for their children. Among the 126 respondents who expressed hesitancy in vaccinating their children, 108 (85.7%) were without any chronic illness.
Table 3 presents levels of quality of life among parents with children 5–11 years old in Malaysia. Almost 30% of the respondents were satisfied with their lives, and 24% were very satisfied with their lives. 24 and 11% of the parents were very dissatisfied and dissatisfied with their lives, respectively. The remaining 11% were neither satisfied nor dissatisfied.
Tables 4, 5 provides the levels of e-health literacy among parents with children 5–11 years old in Malaysia. Above 90% of the respondents agreed to the functional, communicative, critical, and translational criterions of e-health literacy. The mean scores obtained from the respondents’ answers was 4.13 for the functional criteria, 3.87 for the communication criteria, 3.95 and 4.15 for the critical and translational criterions, respectively, which indicated that most of the respondents agreed to the items asked to them.
Tables 6, 7 shows the levels of 5C psychological antecedents of vaccination among parents with children 5–11 years old in Malaysia. The percentages of agreement and disagreement varied across the 5C areas. 73% agreed in the confidence area, while 52% disagreed in the complacency area. 39% of the respondents agreed in the constraints area, while 71 and 74% agreed in the calculation and collective responsibility areas, respectively. As observed in Table 7, the mean score for the set of questions was above 4 for the confidence, calculation and collective responsibility areas.
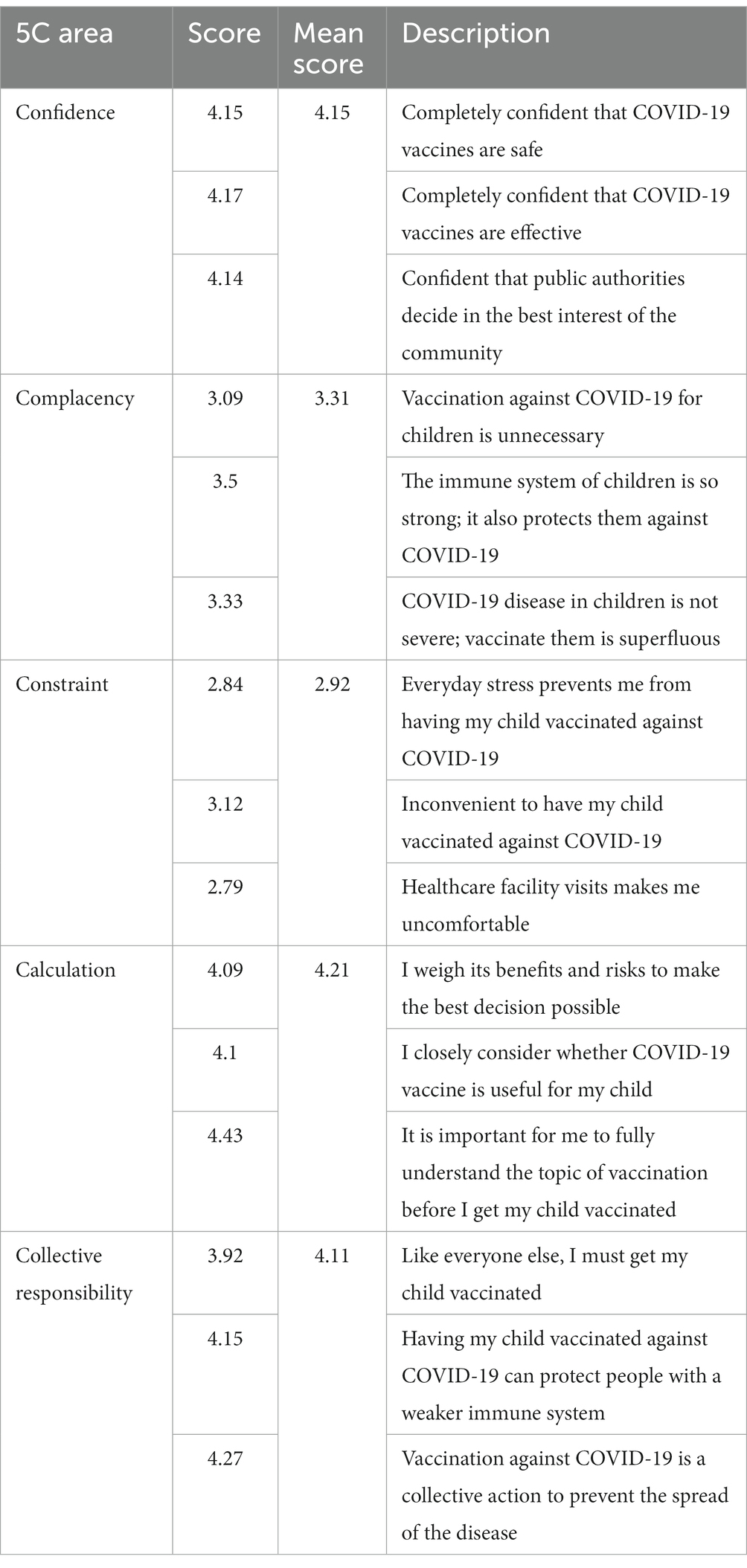
Table 7. Levels of 5C psychological antecedents of vaccination among parents with children 5–11 years old in Malaysia.
Table 8 provides the relationship between socio-economic and demographic variables, quality of life, transactional e-health literacy, 5C psychological antecedents to vaccine hesitancy. The left part of the table gives us the association between vaccine hesitancy and the different independent variables using Pearson’s Chi-Square test. The right part of the table shows the univariate and multivariate logistic regression with vaccine hesitancy as the binary outcome variable. The unadjusted model (univariate regression) shows the effect of each independent variable on the dependent variable separately. The adjusted model (multivariate regression) shows the overall effects of all the independent variables when acting together on the dependent variable. From the p-values obtained from the Chi-Square tests, gender, employment status, and parent’s COVID-19 vaccination status are significantly associated with vaccine hesitancy among parents (p < 0.05). Among transactional e-health literacy, only the communication component had a significant association (p < 0.05). Among the 5C psychological antecedents, confidence, calculation and collective responsibility were significantly associated (p < 0.05) with vaccine hesitancy.
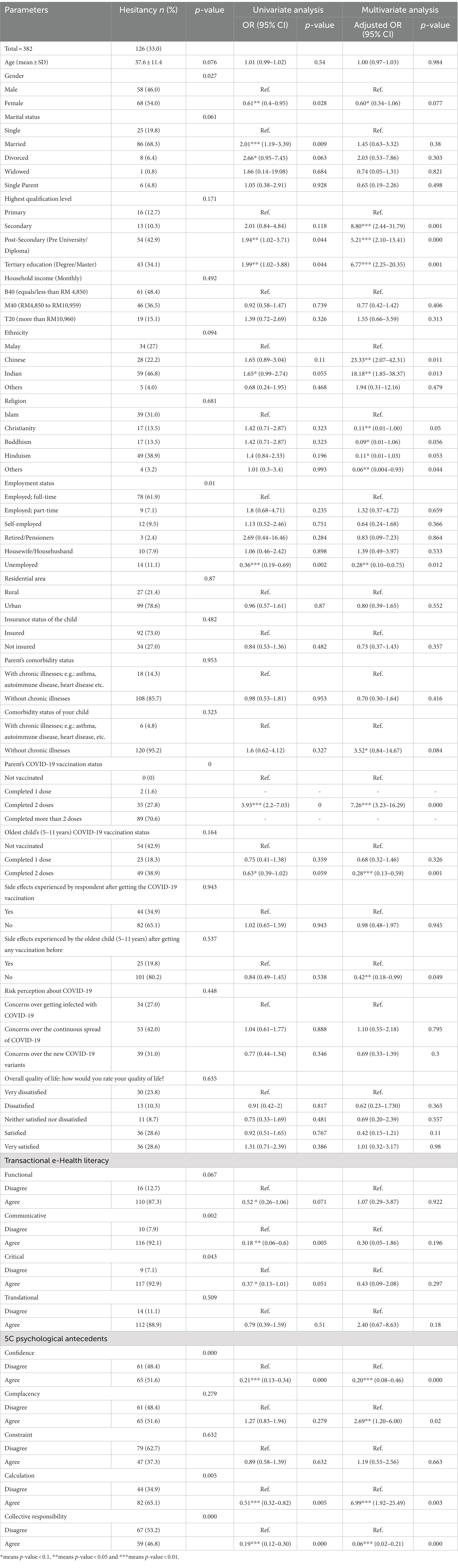
Table 8. Relationship between sociodemographic factors, quality of life, e-health literacy, psychological antecedents to vaccine hesitancy.
Results from the univariate logistic regression suggest that parents who were married were 2 times [OR: 2.01; CI: 1.19–3.39] more likely to hesitate in vaccinating their children than those who were single. Parents with post-secondary and tertiary education also had significant higher risks of hesitancy than those with primary education (p < 0.05). Unemployed parents were 36% less likely to report hesitancy [OR: 0.36, CI: 0.19–0.69, p = 0.002] than those who were full-time employed. Parents who expressed lower confidence, calculation, and collective responsibility were also less likely to report vaccine hesitancy from the unadjusted regression.
After including all the independent variables together in the adjusted model, we found that parents with secondary [OR: 8.80; CI: 2.44–31.79, p = 0.001], post-secondary [OR: 5.21; CI: 2.10–13.41, p = 0.000] and tertiary education [OR: 6.77; CI: 2.25–20.35, p = 0.001] were significantly more likely to express vaccine hesitancy than those with primary education. Parents of Chinese and Indian ethnicity were 23 times and 18 times more likely to report hesitation than Malay people, respectively. Unemployed parents were 28% less likely to express hesitancy [OR: 0.36, CI: 0.19–0.69, p = 0.012] than those who were full-time employed. Parents who expressed low confidence and collective responsibility were significantly less likely to report vaccine hesitancy than those who express high agreement. However, people low in complacency and calculation criteria had significantly higher likelihood of vaccine hesitancy (3 and 7 times, respectively) than those who agreed. Other independent variables did not have any significant association with vaccine hesitancy as per the multivariate analysis.
The core aims of this study were to explore Malaysian parents’ hesitancy, health literacy, and behaviors surrounding COVID-19 vaccinations of their children 5–11 years old, and to examine the psychological barriers that may prevent parents in Malaysia from getting their children vaccinated against the COVID-19 virus. We found that 32.98% of participants expressed hesitancy in allowing their children 5–11 years old to receive COVID-19 vaccines. This finding was similar to the study investigating the willingness of parents to vaccinate their children under 12 years old in Malaysia, where 26.4% of the participants were either unwilling or hesitant (18). Multiple studies investigating attitudes toward vaccinations among the Malaysian adult population reported varied acceptance rates (i.e., between 27.7 and 96%) (52–55). Parents’ experiences and attitudes toward vaccination may play a role in their decision to vaccinate their children. Compared to other countries, parents from Italy and China showed a similar acceptance rate to vaccinate their children. In contrast, parents expressed greater vaccine hesitancy in countries such as Germany, Turkey, and Saudi Arabia (56–60).
Malaysia is a multiracial, multicultural country. Malays and the aborigine people of the country formed the largest ethnic group (61). Higher hesitancy to vaccinate their children was expressed among Chinese and Indian races. This finding was in line with studies investigating the willingness of the country’s adult population in COVID-19 vaccination (53, 62). According to the SAGE working group report, culture and religion were the determinants of vaccine hesitancy via contextual influences (63). This may explain our finding on the differences in vaccine hesitancy among the ethnic groups. Nevertheless, our study found no significant association between most major religions (Islam, Christianity, Buddhism, and Hinduism) and vaccine hesitancy. This finding opposes results of previous studies in Malaysia in which religion was a significant predictor of vaccine hesitancy (62, 64, 65). Islam is the religion with most adherents in the country as 61.3% of Malaysians are Muslims, followed by Buddhism, Christianity, and Hinduism (66). Larger sample sizes are needed to obtain participants with religions proportionate to the country’s population.
Further, higher educational levels was associated with a higher levels of vaccine hesitancy. This result echoed a previous study conducted in Malaysia, in which parents with higher education were more unwilling to vaccinate their children (18). Similar results were obtained in studies conducted in Saudi Arabia and Turkey (59, 67). It is possible that more educated parents may be more skeptical and perceive that the vaccine is unsafe and ineffective for their children. On the contrary, studies reported that higher parental education was associated with higher acceptance vaccinating children in other regions of the world, including China, Thailand, Italy, and the United States (56–59). The SAGE Working Group observed such diverse educational levels’ effects on vaccine hesitancy. The working group reported that higher education may result in higher or lower vaccine hesitancy, despite better education often resulting in better overall health (63).
We found that only communicative eHealth literacy significantly reduced the risk of vaccine hesitancy, whereas the other dimensions of eHealth literacy were not significantly correlated with parental vaccine hesitancy. Studies in Asian countries show significant associations between eHealth literacy and hesitancy toward COVID-19 vaccination (68–70). However, studies on the impact of eHealth literacy on various health related behaviors and attitude are relatively scarce in Malaysia. Therefore, more research is needed in this area to better understand the detrimental effects of misinformation on important health-related issues such as vaccination (71).
We found that higher confidence from the 5C model reduced the risk of vaccine hesitancy among parents. This finding was similar to the studies in Switzerland and Israel, where confidence predicted intentions to vaccinate children against COVID-19 (51, 72). A Malaysian study conducted among the adult population found significant correlation between confidence and vaccine hesitancy (73). The population from our study supported this and showed significant vaccine hesitancy when expressing complacency. However, two studies conducted in Switzerland and Malaysian did not obtain significant correlation between complacency with vaccine hesitancy (72, 73). Parents expressed high calculation – referring to people undergoing extensive information gathering – were 7 times more likely to be vaccine-hesitant as compared to who were low. Various studies have shown that calculation may predict lower vaccine intention (72–75). Depending on the sources of information search, calculation may influence vaccination attitudes in diverse ways. For example, if anti-vaccination or vaccine-critical information was found, calculation may potentially lead to higher hesitancy (50). Healthcare providers may play an important role in providing correct and valuable information regarding vaccines to parents, which may influence their willingness to vaccinate their children. This has been supported in Italy and China (5, 6).
Parents with higher collective responsibility were found to have lower vaccine hesitancy as people would be willing to receive vaccination for the benefits of others. Collective responsibility was found to be a strong predictor of vaccine acceptance in many studies across the globe (72–74, 76). In our study, the only psychological antecedent in the 5C model that was not associated with negative vaccination attitudes was constraint.
Studies from Switzerland and Bangladesh yielded similar results in the aspect of constraint (72, 75). As opposed to our finding, previous research has found that constraint was a significant predictor of vaccine attitudes (73). All in all, the 5C model of psychological antecedents were important predictors of vaccine attitude in our study population.
This study uses eHealth literacy and the 5C model of psychological antecedents to explore Malaysian parents’ hesitancy, health literacy, and behaviors surrounding COVID-19 vaccinations of their children 5–11 years old. It has been found that parents who are in agreement with confidence and collective responsibility are at a lower risk of vaccine hesitancy in their children, as well as complacent parents, who may express a lower intention to receive the vaccination. The results of this study suggest the need for specific interventions in the future to reduce vaccine hesitancy in our practice as a whole.
A limitation of the TeHLI is that it is a self-reported measure. As such, this assessment was not objective as only the respondent’s perceptions toward their own eHealth literacy competencies are measured. Even so, the TeHLI is an instrument built on a robust theoretical foundation and serves as a useful tool for the quick assessment of eHealth literacy levels. Further, the cross sectional design of the study is another important limitation as parental willingness to vaccinate their children is a dynamic process and the picture captured in the current study might have difficulty to reflect the changes over time. Selection bias as a result from convenience sampling method employed in this study may potentially affect the findings. The survey was conducted via online platform and this could also lead to selection bias as eHealth literacy of the people who commonly use the internet and social media may differ from those who are not. This could affect the generalizability of the result from this study. Social desirability bias may be present in the study as all the instruments used were of a self-reporting nature, therefore participants may underreport behaviors or ideas that might be deemed as unfavorable by others.
In conclusion, nearly a third of the participants in the study were hesitant to vaccinate their children. This study also suggests that highly educated parents are more skeptical and more likely to perceive the vaccine as unsafe and ineffective for their children. It is therefore critical to disseminate the required information about the vaccine safety to educated groups. Further, the 5C model of psychological antecedents explained probable reasons behind parental vaccine hesitancy in Malaysia. This is the first study that has examined vaccine hesitancy for children from their parents’ perspective in Malaysia, and the findings could be used by policymakers to understand the ways through which they can improve the vaccination for children. In addition, the study should be replicated, and the results contrasted with countries from Europe (e.g., Italy, Austria and Germany), who faced long lockdowns and conducted studies regarding vaccine hesitancy.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Ethics approval was obtained from the Medical Research and Ethics Committee of the Management and Science University Shah Alam, Selangor, Malaysia. The patients/participants provided their written informed consent to participate in this study.
All authors have made a substantial, direct, and intellectual contribution to the work, and each author has reviewed and approved the final manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ministry of Health Malaysia (2022). COVID now in Malaysia. Available at: https://covidnow.moh.gov.my/?refresh=1679751760482 [Accessed March 25, 2023]
2. Organization WH (2023). WHO coronavirus (COVID-19) dashboard. Available at: https://covid19.who.int/ (Accessed March 25, 2023)
3. Della Polla, G, Pelullo, CP, Napolitano, F, and Angelillo, IF. HPV vaccine hesitancy among parents in Italy: a cross-sectional study. Hum Vaccin Immunother. (2020) 16:2744–51. doi: 10.1080/21645515.2020.1744367
4. Dubé, È, Farrands, A, Lemaitre, T, Boulianne, N, Sauvageau, C, Boucher, FD, et al. Overview of knowledge, attitudes, beliefs, vaccine hesitancy and vaccine acceptance among mothers of infants in Quebec, Canada. Hum Vaccin Immunother. (2019) 15:113–20. doi: 10.1080/21645515.2018.1509647
5. Miraglia del Giudice, G, Napoli, A, Corea, F, Folcarelli, L, and Angelillo, IF. Evaluating COVID-19 vaccine willingness and hesitancy among parents of children aged 5–11 years with chronic conditions in Italy. Vaccine. (2022) 10:396. doi: 10.3390/vaccines10030396
6. Wang, J, Lu, X, Lai, X, Lyu, Y, Zhang, H, Fenghuang, Y, et al. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccine. (2021) 9:191. doi: 10.3390/vaccines9030191
7. Che Mat, NF, Edinur, HA, Abdul Razab, MKA, and Safuan, S. A single mass gathering resulted in massive transmission of COVID-19 infections in Malaysia with further international spread. J Travel Med. (2020) 27:taaa059. doi: 10.1093/jtm/taaa059
8. Suah, JL, Tok, PSK, Ong, SM, Husin, M, Tng, BH, Sivasampu, S, et al. PICK-ing Malaysia’s epidemic apart: effectiveness of a diverse COVID-19 vaccine portfolio. Vaccine. (2021) 9, 1–22. doi: 10.3390/vaccines9121381
9. Dollah, R, Jafar, A, Prayitno Joko, E, Sakke, N, Tahir Mapa, M, Atang, C, et al. Perception of youth in East Malaysia (Sabah) towards the Malaysia national covid-19 immunisation programme (PICK). J Public Health Dev. (2022) 20, 203–217. doi: 10.55131/jphd/2022/200116
10. Jamaluddin, K. . (2021). PEMBERIAN VAKSINASI REMAJA SECARA BERJADUAL BAGI MENGELAKKAN KESESAKAN DI PPV. Ministry of Health Press Statement. Available at: https://covid-19.moh.gov.my/semasa-kkm/2021/09/pick-remaja-vaksinasi-berjadual-elak-ppv-sesak [Accessed August 10, 2022].
11. Husin, M, Tok, PSK, Suah, JL, Thevananthan, T, Tng, BH, Peariasamy, KM, et al. Real-world effectiveness of BNT162b2 vaccine against SARS-CoV-2 infection among adolescents (12 to 17-year-olds) in Malaysia. Int J Infect Dis. (2022) 121:55–7. doi: 10.1016/j.ijid.2022.04.053
12. Ministry of Health Malaysia (2022). PICKids Vaksinasi COVID-19 untuk Kanak-kanak. Available at: https://covid-19.moh.gov.my/vaksin-covid-19/pickids [Accessed August 10, 2022].
13. Sallam, M . COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccine. (2021) 9, 1–14. doi: 10.3390/vaccines9020160
14. MacDonald, NE . Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
15. Shakeel, CS, Mujeeb, AA, Mirza, MS, Chaudhry, B, and Khan, SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccine. (2022) 10, 1–38. doi: 10.3390/vaccines10010110
16. Jafar, A, Dambul, R, Dollah, R, Sakke, N, Mapa, MT, and Joko, EP. COVID-19 vaccine hesitancy in Malaysia: exploring factors and identifying highly vulnerable groups. PLoS One. (2022) 17:e0270868. doi: 10.1371/journal.pone.0270868
17. Chan, NN, Ong, KW, Siau, CS, Lee, KW, Peh, SC, Yacob, S, et al. The lived experiences of a COVID-19 immunization programme: vaccine hesitancy and vaccine refusal. BMC Public Health. (2022) 22:296. doi: 10.1186/s12889-022-12632-z
18. Ng, D-L-C, Gan, GG, Chai, CS, Anuar, NAB, Sindeh, W, Chua, WJ, et al. The willingness of parents to vaccinate their children younger than 12 years against COVID-19: a cross-sectional study in Malaysia. BMC Public Health. (2022) 22:1265. doi: 10.1186/s12889-022-13682-z
19. Dalawi, I, Chen, XW, Isa, MR, Azhar, ZI, and Mohd Nor, F. Assessment of knowledge, attitude, practise and health literacy (KAPH) towards COVID-19 in post-COVID-19 new reality: the need and its challenges in Malaysia. Front Public Health. (2021) 9:704115. doi: 10.3389/fpubh.2021.704115
20. Marzo, RR, Chen, HWJ, Abid, K, Chauhan, S, Kaggwa, MM, Essar, MY, et al. Adapted digital health literacy and health information seeking behavior among lower income groups in Malaysia during the COVID-19 pandemic. Front Public Health. (2022) 10:998272. doi: 10.3389/fpubh.2022.998272
21. Fisher, CB, Gray, A, and Sheck, I. COVID-19 pediatric vaccine hesitancy among racially diverse parents in the United States. Vaccine. (2021) 10, 1–14. doi: 10.3390/vaccines10010031
22. Khatatbeh, M, Albalas, S, Khatatbeh, H, Momani, W, Melhem, O, al Omari, O, et al. Children’s rates of COVID-19 vaccination as reported by parents, vaccine hesitancy, and determinants of COVID-19 vaccine uptake among children: a multi-country study from the eastern Mediterranean region. BMC Public Health. (2022) 22. Available from::1375. doi: 10.1186/s12889-022-13798-2
23. Aldakhil, H, Albedah, N, Alturaiki, N, Alajlan, R, and Abusalih, H. Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J Infect Public Health. (2021) 14:1497–504. doi: 10.1016/j.jiph.2021.08.028
24. Xu, Y, Xu, D, Luo, L, Ma, F, Wang, P, Li, H, et al. A cross-sectional survey on COVID-19 vaccine hesitancy among parents from Shandong vs. Zhejiang. Front Public Health. (2021) 9:779720. doi: 10.3389/fpubh.2021.779720
25. Horiuchi, S, Sakamoto, H, Abe, SK, Shinohara, R, Kushima, M, Otawa, S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. BK Padhi , editor. PLoS One (2021). 16:e0261121. doi: 10.1371/journal.pone.0261121
26. Lau, EYH, Li, J-B, and King Chung Chan, D. Intention to vaccinate young children against COVID-19: a large-scale survey of Hong Kong parents. Hum Vaccin Immunother. (2022) 18, 1–5. doi: 10.1080/21645515.2022.2065838
27. Shmueli, L . Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. (2021) 21:804. doi: 10.1186/s12889-021-10816-7
28. Limbu, YB, Gautam, RK, and Pham, L. The health belief model applied to COVID-19 vaccine hesitancy: a systematic review. Vaccine. (2022) 10:973. doi: 10.3390/vaccines10060973
29. Li, J-B, Lau, EYH, and Chan, DKC. Why do Hong Kong parents have low intention to vaccinate their children against COVID-19? Testing health belief model and theory of planned behavior in a large-scale survey. Vaccine. (2022) 40:2772–80. doi: 10.1016/j.vaccine.2022.03.040
30. Szilagyi, PG, Shah, MD, Delgado, JR, Thomas, K, Vizueta, N, Cui, Y, et al. Parents’ intentions and perceptions about COVID-19 vaccination for their children: results from a National Survey. Pediatrics. (2021) 148:e2021052335. doi: 10.1542/peds.2021-052335
31. Alfieri, NL, Kusma, JD, Heard-Garris, N, Davis, MM, Golbeck, E, Barrera, L, et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. (2021) 21:1662. doi: 10.1186/s12889-021-11725-5
32. Pippert, C.H., Trujillo, K.L., Lazer, D., Baum, M., Simonson, M.D., Ognyanova, K., et al. (2021). The COVID states project #68: heightened parental concerns about COVID-19 vaccinations for children; OSFPREPRINT Available at: https://osf.io/4u6hb (Accessed October 20, 2022).
33. Ruggiero, KM, Wong, J, Sweeney, CF, Avola, A, Auger, A, Macaluso, M, et al. Parents’ intentions to vaccinate their children against COVID-19. J Pediatr Health Care. (2021) 35:509–17. doi: 10.1016/j.pedhc.2021.04.005
34. Shacham, E, Little, G, Scroggins, S, Fredman, A, Wray, R, and Charney, R. Intent to vaccinate children against COVID-19: low levels of Trust in Public Health Agencies Trust across rural communities. SocArXiv Papers. (2021)
35. Teasdale, CA, Borrell, LN, Shen, Y, Kimball, S, Rinke, ML, Fleary, SA, et al. Parental plans to vaccinate children for COVID-19 in new York City. Vaccine. (2021) 39:5082–6. doi: 10.1016/j.vaccine.2021.07.058
36. Teherani, M, Banskota, S, Camacho-Gonzalez, A, Smith, AGC, Anderson, EJ, Kao, CM, et al. Intent to vaccinate SARS-CoV-2 infected children in US households: a survey. Vaccine. (2021) 9:1049. doi: 10.3390/vaccines9091049
37. Temsah, M-H, Alhuzaimi, AN, Aljamaan, F, Bahkali, F, al-Eyadhy, A, Alrabiaah, A, et al. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: a National Survey. Front Public Health. (2021) 9:752323. doi: 10.3389/fpubh.2021.752323
38. Zhang, X, Guo, Y, Zhou, Q, Tan, Z, and Cao, J. The mediating roles of medical mistrust, knowledge, confidence and complacency of vaccines in the pathways from conspiracy beliefs to vaccine hesitancy. Vaccine. (2021) 9:1342. doi: 10.3390/vaccines9111342
39. Brackstone, K, Marzo, RR, Bahari, R, Head, MG, Patalinghug, ME, and Su, TT. COVID-19 vaccine hesitancy and confidence in the Philippines and Malaysia: a cross-sectional study of sociodemographic factors and digital health literacy. PLOS Glob Public Health. (2022) 2:e0000742. doi: 10.1371/journal.pgph.0000742
40. Marzo, RR, Shrestha, R, Sapkota, B, Acharya, S, Shrestha, N, Pokharel, M, et al. Perception towards vaccine effectiveness in controlling COVID-19 spread in rural and urban communities: a global survey. Front Public Health. (2022) 10:958668. doi: 10.3389/fpubh.2022.958668
41. Marzo, RR, Su, TT, Ismail, R, Htay, MN, Essar, MY, Chauhan, S, et al. Digital health literacy for COVID-19 vaccination and intention to be immunized: a cross sectional multi-country study among the general adult population. Front Public Health. (2022) 10:998234. doi: 10.3389/fpubh.2022.998234
42. Marzo, RR, Chen, HW, Abid, K, Chauhan, S, Kaggwa, MM, Essar, MY, et al. Adapted digital health literacy and health information seeking behavior among lower income groups in Malaysia during the COVID-19 pandemic. Front Public Health. (2022) 10:998272. doi: 10.3389/fpubh.2022.998272
43. Fisher, CB, Gray, A, and Sheck, I. COVID-19 pediatric vaccine hesitancy among racially diverse parents in the United States. Vaccine. (2022) 10:31. doi: 10.3390/vaccines10010031
44. Gray, A, and Fisher, CB. Determinants of COVID-19 vaccine uptake in adolescents 12–17 years old: examining pediatric vaccine hesitancy among racially diverse parents in the United States. Front Public Health. (2022) 10:844310. doi: 10.3389/fpubh.2022.844310
45. Kaiser Family Foundation (2022). Latest data on COVID-19 vaccinations by race/ethnicity; USA. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/ (Accessed October 26, 2022).
46. Paige, SR, Stellefson, M, Krieger, JL, Anderson-Lewis, C, Cheong, J, and Stopka, C. Proposing a transactional model of eHealth literacy: concept analysis. J Med Internet Res. (2018) 20:e10175. doi: 10.2196/10175
47. Dodd, RH, Cvejic, E, Bonner, C, Pickles, K, McCaffery, KJ, Ayre, J, et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. (2021) 21:318–9. doi: 10.1016/S1473-3099(20)30559-4
48. Montagni, I, Ouazzani-Touhami, K, Mebarki, A, Texier, N, Schück, S, Tzourio, C, et al. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health. (2021) 43:695–702. doi: 10.1093/pubmed/fdab028
49. Marzo, RR, Su, TT, Ismail, R, Htay, MNN, Essar, MY, Chauhan, S, et al. Digital health literacy for COVID-19 vaccination and intention to be immunized: a cross sectional multi-country study among the general adult population. Front Public Health. (2022) 10:998234. doi: 10.3389/fpubh.2022.998234
50. Betsch, C, Schmid, P, Heinemeier, D, Korn, L, Holtmann, C, and Böhm, R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. (2018) 13:e0208601. doi: 10.1371/journal.pone.0208601
51. Abdou, MS, Kheirallah, KA, Aly, MO, Ramadan, A, Elhadi, YAM, Elbaraz, I, et al. Psychological antecedents towards COVID-19 vaccination using the Arabic 5C validated tool: an online study in 13 Arab countries. medRxiv. (2021):2021.08.31.21262917. doi: 10.1101/2021.08.31.21262917
52. Shakeel, CS, Mujeeb, AA, Mirza, MS, Chaudhry, B, and Khan, SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccine. (2022) 10:110. doi: 10.3390/vaccines10010110
53. Marzo, RR, Ahmad, A, Abid, K, Khatiwada, AP, Ahmed, A, Kyaw, TM, et al. Factors influencing the acceptability of COVID-19 vaccination: a cross-sectional study from Malaysia. Vacunas. (2022) 23:S33–40. doi: 10.1016/j.vacun.2021.07.007
54. Sallam, M, Al-Sanafi, M, and Sallam, M. A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. (2022) 15:21–45. doi: 10.2147/JMDH.S347669
55. Marzo, RR, Sami, W, Alam, MZ, Acharya, S, Jermsittiparsert, K, Songwathana, K, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six southeast Asian countries. Trop Med Health. (2022) 50:4. doi: 10.1186/s41182-021-00393-1
56. Wang, L, Wen, W, Chen, C, Tang, J, Wang, C, Zhou, M, et al. Explore the attitudes of children and adolescent parents towards the vaccination of COVID-19 in China. Ital J Pediatr. (2022) 48:122. doi: 10.1186/s13052-022-01321-7
57. Montalti, M, Rallo, F, Guaraldi, F, Bartoli, L, Po, G, Stillo, M, et al. Would parents get their children vaccinated against SARS- CoV-2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccine. (2021) 9:366. doi: 10.3390/vaccines9040366
58. Yılmaz, M, and Sahin, MK. Parents’ willingness and attitudes concerning the COVID-19 vaccine: a cross-sectional study. Int J Clin Pract. (2021) 75:e14364. doi: 10.1111/ijcp.14364
59. Temsah, M-H, Alhuzaimi, AN, Aljamaan, F, Bahkali, F, al-Eyadhy, A, Alrabiaah, A, et al. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: a National Survey. Front Public Health. (2021) 9:752323. doi: 10.3389/fpubh.2021.752323
60. Brandstetter, S, Böhmer, MM, Pawellek, M, Seelbach-Göbel, B, Melter, M, Kabesch, M, et al. Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: cross-sectional analyses using data from the KUNO- kids health study. Eur J Pediatr. (2021) 180:3405–10. doi: 10.1007/s00431-021-04094-z
61. Department of Statistics Malaysia (2020). Current population estimates, Malaysia, 2020. Available at: https://ophrp.org/journal/view.php?doi=10.24171/j.phrp.2021.0085#b62-j-phrp- [Accessed August 14, 2022].
62. Lau, JFW, Woon, YL, Leong, CT, and Teh, HS. Factors influencing acceptance of the COVID-19 vaccine in Malaysia: a web-based survey. Osong Public Health Res Perspect. (2021) 12:361–73. doi: 10.24171/j.phrp.2021.0085
63. SAGE Working Group (2014). Report of the SAGE working group on vaccine hesitancy. Available at: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf [Accessed August 14, 2022].
64. Ng, JWJ, Vaithilingam, S, Nair, M, Hwang, L-A, and Musa, KI. Key predictors of COVID-19 vaccine hesitancy in Malaysia: an integrated framework. PLoS One. (2022) 17:e0268926. doi: 10.1371/journal.pone.0268926
65. Syed Alwi, SAR, Rafidah, E, Zurraini, A, Juslina, O, Brohi, IB, and Lukas, S. A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health. (2021) 21:1129. doi: 10.1186/s12889-021-11071-6
66. Nordin, MZF. The identity in religious language in Malaysia. Am J humanit soc sci. (2018) 2:74–78.
67. Yigit, M, Ozkaya-Parlakay, A, and Senel, E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. (2021) 40:e134–6. doi: 10.1097/INF.0000000000003042
68. Kim, GY, Shin, T, Son, Y, and Choi, J. Psycho-behavioural factors influencing COVID-19 vaccine hesitancy among Korean adults: the moderating role of age. J Adv Nurs. (2022) 78:2904–15. doi: 10.1111/jan.15273
69. Nath, R, Imtiaz, A, Nath, SD, and Hasan, E. Role of vaccine hesitancy, eHealth literacy, and vaccine literacy in young adults’ COVID-19 vaccine uptake intention in a lower-middle-income country. Vaccine. (2021) 9:1405. doi: 10.3390/vaccines9121405
70. Liu, H, Zhou, Z, Tao, X, Huang, L, Zhu, E, Yu, L, et al. COVID-19 vaccine hesitancy among Chinese residents under the free vaccination policy. Rev Assoc Med Bras. (2021) 67:1317–21. doi: 10.1590/1806-9282.20210633
71. Dib, F, Mayaud, P, Chauvin, P, and Launay, O. Online mis/disinformation and vaccine hesitancy in the era of COVID-19: why we need an eHealth literacy revolution. Hum Vaccin Immunother. (2022) 18:1–3. doi: 10.1080/21645515.2021.1874218
72. Aylin Wagnera, JD, Liberatoreb, F, and Schmelzerb, S. Confident and altruistic – parents’ motives to vaccinate their children against COVID-19: a cross- sectional online survey in a Swiss vaccination Centre. Swiss Med Wkly. (2022) 152:1–10. doi: 10.4414/smw.2022.w30156
73. Azizan, AH, Subramaniam, G, Sivasamugham, LA, Gopinathan, S, Raman, M, and Wong, LS. Vaccine hesitancy toward the COVID-19 vaccine among the Malaysian population. J Exp Biol Agric Sci. (2022) 10:544–53. doi: 10.18006/2022.10(3).544.553
74. Wismans, A, Thurik, R, Baptista, R, Dejardin, M, Janssen, F, and Franken, I. Psychological characteristics and the mediating role of the 5C model in explaining students’ COVID-19 vaccination intention. PLoS One. (2021) 16:e0255382. doi: 10.1371/journal.pone.0255382
75. Hossain, MB, Alam, MZ, Islam, MS, Sultan, S, Faysal, MM, Rima, S, et al. Health belief model, theory of planned behavior, or psychological antecedents: what predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults? Front Public Health. (2021) 9:711066. doi: 10.3389/fpubh.2021.711066
Keywords: vaccine hesitancy, COVID-19, children, Malaysia, health education and awareness
Citation: Marzo RR, Chakraborty R, Soh SY, Thew HZ, Chong C, Siau CS, Abdul Wahab KB, Binti Ariffin IA, Chauhan S, Brackstone K, Padhi BK and Heidler P (2023) Factors influencing parents’ hesitancy to vaccinate their children aged 5–11 years old against COVID-19: results from a cross-sectional study in Malaysia. Front. Public Health 11:1091015. doi: 10.3389/fpubh.2023.1091015
Received: 06 November 2022; Accepted: 11 April 2023;
Published: 16 May 2023.
Edited by:
Deep Shikha, Swami Rama Himalayan University, IndiaReviewed by:
Jian-Bin Li, The Education University of Hong Kong, Hong Kong SAR, ChinaCopyright © 2023 Marzo, Chakraborty, Soh, Thew, Chong, Siau, Abdul Wahab, Binti Ariffin, Chauhan, Brackstone, Padhi and Heidler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roy Rillera Marzo, cnJtdGV4YXNAeWFob28uY29t; Petra Heidler, cGV0cmEuaGVpZGxlckBmaC1rcmVtcy5hYy5hdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.