
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 01 February 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1086905
This article is part of the Research Topic Community Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic, Volume IV View all 10 articles
 Sara Nooraeen1
Sara Nooraeen1 Shahrzad Bazargan-Hejazi2
Shahrzad Bazargan-Hejazi2 Morteza Naserbakht3
Morteza Naserbakht3 Camelia Vahidi4
Camelia Vahidi4 Farideh Shojaerad4
Farideh Shojaerad4 Seyedeh Sahar Mousavi4
Seyedeh Sahar Mousavi4 Seyed Kazem Malakouti1*
Seyed Kazem Malakouti1*Background: The implementation of quarantine and social distancing measures to control the COVID-19 pandemic led to restrictions at the community level and most of in-person psychiatric services were discontinued. This situation could affect the psychopathology of the patients and the burden of their caregivers. The aim of this study was to investigate the effects of COVID-19 pandemic on people with severe mental illnesses (SMIs) and their caregivers' burden.
Method: The study sample consisted of 86 patients with severe mental illness and 86 caregivers. The mental status, relapse rate, and rehospitalization rate of the patients and the general health status and burden of caregivers were investigated in three waves, including before and 3 and 6 months after the COVID-19 pandemic.
Results: The relapse rate of the patients was 14%, 33.7%, and 43% (p = 0.000) and the rehospitalization rate was 4.7%, 7%, and 10.5% in waves 0, 1, and 2, respectively (p = 0.000). Most of the psychopathological scales increased in three waves (p = 0.000). The caregivers' burden and health condition worsened during the nine months of the study as well (p = 0.000).
Conclusion: The COVID-19 pandemic led to the exacerbation of symptoms and increased the relapse rate in people with SMIs. It also worsened the caregivers' condition. People with severe mental illnesses (SMIs) and their caregivers are one of the most vulnerable groups on which the COVID-19 pandemic had a marked negative effect.
According to Lancet commission report convened by the world experts in psychiatry in 2018, the universal increase in mental disorders will cost the global economy $16 trillion by 2030 (1). In 2019, the global outbreak of the novel coronavirus (COVID-19) added another layer of concern to the emerging public mental health crisis (2) due to the implementation of lockdown, social distancing, isolation, and quarantine measures to limit its spread (3–5). In the general population, COVID-related restrictions have led to lifestyle disruption, job loss, sleep disturbances, anxiety, depression, and PTSD (6–9). In patients exposed to COVID-19, these restrictions could be exacerbated by fear of isolation, loneliness and boredom, affecting their mental health and even triggering suicidal ideation and suicide (10–12). The pandemic has also prevented people from properly mourning for their beloved ones who were lost to the disease (13). Studies that were conducted during the COVID-19 pandemic found that mental health of the participants significantly decreased during this time compared to the pre- pandemic years (5, 14, 15). The combination of these factors has turned COVID-19 into a crisis in terms of mental health among others. The SARS pandemic and its impact on the needs of patients with pre-existing psychiatric disorders suggest that the health consequences of the pandemic on this vulnerable population could be profound (16, 17). Patients with severe mental illness (SMI) such as schizophrenia or bipolar I disorder often receive a variety of treatments including pharmacological treatment, psychosomatic treatment, and rehabilitation (18). Any disruption in their routine care, as a result of pandemic lockdown policies, is likely to exacerbate their conditions (19, 20).
It has been reported that interruptions in the mental health-related utilization of SMIs are associated with a higher risk of recurrence and relapse of symptoms and readmission to the psychiatric ward in these patients (21–23). Furthermore, the job loss rate has been higher for those with psychiatric diseases at the time of the pandemic compared to the general population (24). This further increases the vulnerability of this group which may receive less attention in the pandemic situation compared to the general population (8, 9, 14, 15, 25–28).
The caregivers of SMI patients play a major role in the management of their patients. Whether caregiving is provided by a family member or a formal caregiver, it is part of the core care system that assists patients in getting prescribed treatments and ensures the continuity of care (29). It is common for caregivers to feel frustrated, stressed, and helpless while trying to strike a balance between the responsibilities of the role and providing the best care without burdening their health (30–32). A review of the literature regarding the caregivers' experiences shows a prevalence of 14–47% for depression and anxiety among the caregivers of the SMI patients (33). In the meantime, a higher prevalence is reported for caregivers of schizophrenia patients (30%) (34, 35). Additionally, the caregivers of the SMI patients have lower levels of perceived social support and quality of life (29). The existing evidence supports the role of community mental health programs in enhancing the quality of life of both caregivers and their SMI patients (36–38). However, the impact of the closure of community-based mental health centers due to the COVID-19 pandemic on the mental health condition of Iranian SMI patients is unclear. The aim of the present study was to estimate the impact of the COVID-19 pandemic on the psychopathology of individuals with SMIs and their caregivers' perceived burden.
A cohort study was conducted between August 2020 and December 2021. The participants were recruited from the Andishe Salamat Ravan (ASR), Tehran, Iran. ASR is a community-based day-care rehabilitation center that provides mental rehabilitation and outreach services for chronic psychiatric patients. The patients were eligible to participate if they were above 18 years, had a diagnosis of SMI including schizophrenia, bipolar disorder, and chronic major depressive disorder, and were receiving regular care from the ASR (before the pandemic). The eligibility criteria for the caregivers were age above 18 years. The participants that provided written informed consent were scheduled for a face-to-face interview at the ASR. They included 86 SMI patients and their caregivers (n = 86). Before the COVID-19 pandemic, as part of the standard of care, these patients were receiving community-based psychiatric services including monthly in-person visits as well as medical and rehabilitation care in the center 3–4 days per week. However, these services were disrupted during the COVID-19 pandemic due to the implementation of quarantine and social distancing protocols and were replaced by telepsychiatry for patients who had access to the Internet and smartphones. Otherwise, the patients were contacted by phone for counseling and were advised to adhere to their individualized treatment plan. All patients received their medications by mail to avoid possible exposure in the drugstore.
Data were collected by three trained interviewers: a physician and two psychologists. The interview time was about 30 min for each patient and his/her caregiver.
Data collection took place in three waves: wave zero refers to 6 months before the COVID-19 pandemic. Waves 1 and 2 refer to 3 and 9 months after World Health Organization declared COVID-19 a pandemic on March 11, 2020 (39). The following measures were used to assess the mental health conditions of the patients with SMIs.
The Positive and Negative Syndrome Scale (PANSS) is used to measure the severity of schizophrenia symptoms. It was published in 1987 by Stanley et al. (29). It is known as a gold standard measure for the evaluation of the severity of schizophrenia symptoms. It includes a positive scale (7 items), a negative scale (7 items), and a general psychopathology scale (16 items), and takes about 45 min to complete. The Cronbach's alpha coefficient of the PANSS is 0.77. This scale was used to determine the severity of schizophrenia symptoms before and after the COVID-19 pandemic. The reliability and validity of the Persian version of this instrument were confirmed by Ghamari et al. (40). Diagnostic and clinical researchers have reported that this questionnaire has an acceptable construct validity (40).
The YMRS is an 11-item interviewer rated scale (41). The items have five defined grades of severity. Four items are double weighted (irritability, speech, thought content, and disruptive/aggressive behavior (42). This questionnaire was validated by Barekatain et al. in Iran (43). The results of differentiation analysis showed a cut-off point of 17.14, a sensitivity of 98.4%, and a specificity of 98.4%. This scale was used to measure mania symptoms in patients with bipolar disorder.
The BDI (44) is a 21-question multiple-choice self-report inventory for measuring the severity of depression. This instrument was validated in Iran in various studies including a study by Ghassemzadeh et al. (45). The BDI was used to evaluate depressive symptoms in patients with bipolar and major depressive disorders.
Disease relapse was assessed in terms of its significance and rehospitalization. A relapse was “mild” if the severity of the illness and the symptoms were serious enough for the therapist to increase medications and frequency of virtual visits to control the exacerbated symptoms.
Rehospitalization indicated that the severity of the exacerbated symptoms made it impossible to control the symptoms at home. To prevent further harm to the patients and their families, hospitalization was inevitable.
The following measures were used to assess the mental health conditions of the caregivers:
The GHQ is a screening tool for identification of minor psychiatric disorders in the general population or within a community or non-psychiatric clinical setting such as a primary care or general outpatient center. The reliability and validity of this questionnaire were evaluated by Taghavi in Iran (46). The coefficients were calculated using three different methods: test-retest, split-half, and Cronbach alpha, which were 0.70, 0.93, and 0.90, respectively. The validity of the questionnaire measured by the Middlesex Hospital Questionnaire (MHQ) was 55 (P < 0001). The subscale-total correlations, as another index of validity, were between 0.72 and 0.87 (46). This questionnaire was used to screen the mental health situation of the caregivers.
The FBIS (47) is a semi-structural interview measurement tool with a reliability coefficient of 0.72. This scale was used to measure the burden of caregiving. This scale was used by Chimeh et al. in Iran (48).
The protocol of the study was approval by the Ethics Committee of Iran University of Medical Sciences (ethics code: IR.IUMS.REC.1399.416). Written consent was obtained from all participants prior to the study.
Analyses were conducted using IBM SPSS 25 statistical software. Descriptive analyses were used to describe the demographic characteristics of the patients and their caregivers. Mauchly's sphericity test was performed to evaluate the sphericity of the tests. Greenhouse–Geisser correction was applied as an alternative to correct the violation of the sphericity. Repeated Measure ANOVA followed by post hoc Bonferroni test was applied to detect any overall difference in the severity of the psychopathological symptoms between the three waves.
Interrater reliability of the interviewers was evaluated using the Pearson correlation coefficient. Statistical significance was determined as p-value < 0.05.
Of 86 patients, 11 withdrew from the study [seven patients with a diagnosis of schizophrenia and four with bipolar mood disorder (BMD)]; therefore, the final sample included 75 patients and 75 caregivers. The Mauchly's sphericity test results were not significant for YMRS (P = 0.188), BDI (0.070) and RELAPS (Sig = 0.348); therefore, the sphericity assumption was met. However, the sphericity assumption was not met for PANSS (P < 0.001), GHQ (P < 0.001), FBIS (P < 0.001) and rehospitalization (P = 0.026). The mean age of the patients was 43.4 ± 9.5 years (range: 26–72 years), and 86.7% were diagnosed with schizophrenia, 86.7% with BMD, and 13.3% with major depressive disorder (MDD). Table 1 shows the demographic characteristics of the patients and their caregivers.
As demonstrated in Table 2, the patients' mean scores for psychopathology measures increased over the three waves except for YMRS. The relapse rate was 14, 33.7, and 43%, and the rehospitalization rates were 4.7, 7, and 10.5% in waves 0, 1, and 2, respectively (Table 2).
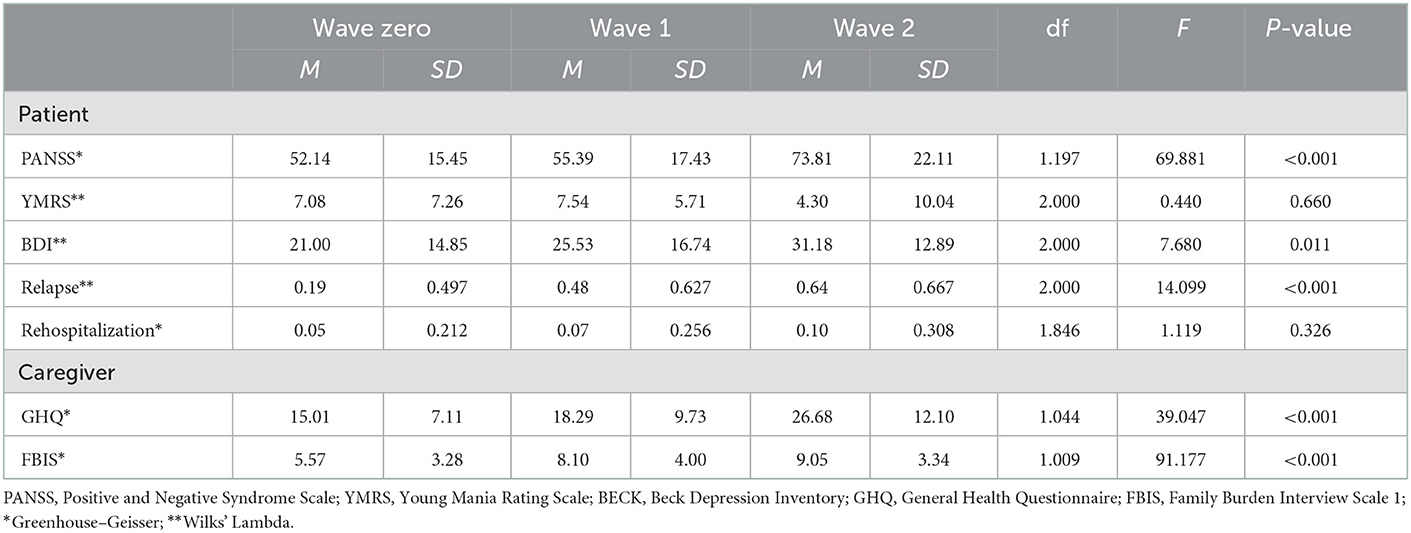
Table 2. Repeated measures analysis of variance (ANOVA) for psychopathology of patients and mental health of caregivers.
The results of post hoc analysis of the severity of psychopathology and relapse rate are presented in Table 3.
The findings showed that the relapse rate rose from 9.3 to 43% during three waves of the study. Additionally, the patients' symptoms deteriorated 9 months after the COVID-19 pandemic. Similar findings are reported from other countries (24, 49–51). The treatment and management of SMIs such as schizophrenia and bipolar disorders are very costly (52–54). Any increase in the incidence of relapse, as reported in the present study, would not be cost-effective (55). Several researchers have suggested the use of telepsychiatry services as an alternative mitigating strategy to minimize disruption in patient care (56–58). The efficacy of telepsychiatry has been proven in neurotic psychiatric disorders (7, 59, 60). A cross-sectional study conducted in the US found that psychiatric visits to patients through telepsychiatry, mostly by telephone, were much higher compared to before the pandemic and face-to-face visits (61). Studies have shown the efficacy of telepsychiatry services for individuals with SMIs (62, 63). However, in low-to-middle income countries (LMICs), such as Iran, barriers such as lack of access to smartphones, digital illiteracy, poor Internet connections, low telepsychiatry awareness, lack of provider training, and ban of e-prescriptions limit the use of telepsychiatry (64). Therefore, the efficacy and effectiveness of telepsychiatry in LMICs that are disproportionally affected by mental health disorders need further research (65–67).
According to the findings, caregivers experienced a higher burden and worsening of mental health situation. In the present study, more than 50% of the caregivers were patients' parents. They were mostly old, had low education levels, and had some physical and mental problems, which made it difficult to take care of the patients.
The caregivers of psychiatric patients are a vulnerable group (68) that is sometimes neglected while the condition of the patients can affect them. Findings indicate that caregivers are more likely to have psychological problems in comparison with the general population (69, 70). It could be due to the burden of long-term caring for individuals with chronic mental conditions such as medication costs, cigarette smoking, patient's unemployment, and some subjective reasons like stigma, shame, avoiding friends, etc. All of the above studies were conducted in non-COVID situations (38). Few studies have examined the status of the patients in such pandemic conditions and concluded that the burden of caregivers increased during the COVID-19 pandemic markedly (71, 72). There are several possible reasons for this finding. First, many patients and their caregivers lost their jobs during the pandemic, and the lack of adequate financial and social support has created many financial problems for them, which may lead to an increase in the burden. Second, patients spent several hours outside the home to receive day center services. Third, the patients and families became bored and domestic violence increased (73–75). Fear of getting infected with COVID-19 and concerns about the person who should care for the patient in case of disease or death were also sources of stress for families. In the present study, the relapse rate was rather high in wave two (about 40%); however, few patients were hospitalized, which could be due to the fear of families who do not wish to hospitalize their patients even in the case of severe relapses. Caregivers accepted the responsibility of caring for the patient at home, which also increased their burden in turn. Providing telepsychiatric and telerehabilitation services to patients and their caregivers could be crucial (76). It is predicted (77) that as the pandemic continues, it will be harder for these families to cope, particularly considering the low vaccination rate.
A small sample size and other methodological problems like the lack of a control group could be considered as the study limitations. Although all of the patients received telephone follow-up (since not all of them had smartphone) and receive their medications, it was not possible to assess the impact of telepsychiatry services due to the lack of a control group.
To the best of our knowledge, this is the first study to understand the degree to which the COVID-19 pandemic exacerbated the symptoms in patients with SMIs and the burden of their caregivers in Iran.
People with SMIs and their caregivers are a vulnerable group during pandemics that may experience the exacerbation of their mental disease. It may also impose more objective and subjective burdens on their families and caregivers (77). They require more attention to keep up with the general population.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Committee of Iran University of Medical Sciences (Ethics code: IR.IUMS.REC.1399.416). The patients/participants provided their written informed consent to participate in this study.
SN: study design, data gathering, interviewing, and writing manuscript. SB-H: data gathering and writing manuscript. MN: data gathering and data analysis. CV: study design and data gathering. FS and SSM: data gathering and interviewing. SKM: study design and data analysis. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The lancet commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
2. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease, (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:729. doi: 10.3390/ijerph17051729
3. Thivolet J, Cambazard F, Genvo MF. Maternally-transmitted severe neonatal aphthosis. Ann Dermatol Venereol. (1982) 109:815–6.
4. Dos Santos CF, Picó-Pérez M, Morgado P. COVID-19 and mental health—what do we know so far? Front Psychiatr. (2020) 11:565698. doi: 10.3389/fpsyt.2020.565698
5. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adol Psychiatr Mental Health. (2020) 14:20. doi: 10.1186/s13034-020-00329-3
6. Kola L. Global mental health and COVID-19. Lancet Psychiatr. (2020) 7:655–7. doi: 10.1016/S2215-0366(20)30235-2
7. Kozloff N, Mulsant BH, Stergiopoulos V, Voineskos AN. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. (2020) 46:752–7. doi: 10.1093/schbul/sbaa051
8. Lima CKT, Medeiros Carvalho PM, Lima IDAAS, Oliveira Nunes JVA, Saraiva JS, Souza RI, et al. The emotional impact of Coronavirus 2019-nCoV, (new Coronavirus disease). Psychiatry Res. (2020) 287:112915. doi: 10.1016/j.psychres.2020.112915
9. Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, et al. Mental Health of Communities During the COVID-19 Pandemic. Los Angeles, CA: SAGE Publications. (2020).
10. Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatr. (2020) 7:468–71. doi: 10.1016/S2215-0366(20)30171-1
11. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatr. (2020) 7:389–90. doi: 10.1016/S2215-0366(20)30141-3
12. Nooraeen S, Javanbakht M, Malakouti SK. Getting closer to our unpleasant previse: possible rise in suicide rate in Iran during COVID-19 pandemic. Iran J Psychiatry Behav Sci. (2021) 15:e112213. doi: 10.5812/ijpbs.112213
13. Eisma MC, Boelen PA, Lenferink LI. Prolonged grief disorder following the Coronavirus (COVID-19) pandemic. Psychiatry Res. (2020) 288:113031. doi: 10.1016/j.psychres.2020.113031
14. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. (2020) 324:93–4. doi: 10.1001/jama.2020.9740
15. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. doi: 10.1016/S2215-0366(20)30308-4
16. Cheng ST, Cheung KCC, Cheung CK. Peer victimization and depression among Hong Kong adolescents. J Clin Psychol. (2008) 64:766–776. doi: 10.1002/jclp.20489
17. Gerstein MB, Lu ZJ, Van Nostrand EL, Cheng C, Arshinoff BI, Liu T, et al. Integrative analysis of the Caenorhabditis elegans genome by the Modencode project. Science. (2010) 330:1775–87. doi: 10.1126/science.1196914
18. Drake RE, Green AI, Mueser KT, Goldman HH. The history of community mental health treatment and rehabilitation for persons with severe mental illness. Commun Mental Health J. (2003) 39:427–40. doi: 10.1023/A:1025860919277
19. Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: a review of research on case management. Schizophrenia Bullet. (1998) 24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314
20. Kopelovich SLM, Buck BE, Brenner C, Moser L, Jarskog LF, Harker S, et al. Community mental health care delivery during the COVID-19 pandemic: practical strategies for improving care for people with serious mental illness. Commun Mental Health J. (2021) 57:405–15. doi: 10.1007/s10597-020-00662-z
21. Dennis RA, Caceda R. Why COVID-19 is especially difficult for those with schizophrenia: reasons and solutions. Primary Care Comp CNS Disorders. (2020) 22:26175. doi: 10.4088/PCC.20com02739
22. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
23. Busch AB, Huskamp HA, Raja P, Rose S, Mehrotra A. Disruptions in care for medicare beneficiaries with severe mental illness during the COVID-19 pandemic. JAMA Network Open. (2022) 5:e2145677. doi: 10.1001/jamanetworkopen.2021.45677
24. Van Rheenen TE, Meyer D, Neill E, Phillipou A, Tan EJ, Toh WL, et al. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: initial results from the COLLATE project. J Aff Disorders. (2020) 275:69–77. doi: 10.1016/j.jad.2020.06.037
25. North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. (2013) 310:507–18. doi: 10.1001/jama.2013.107799
26. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. (2014) 35:169–83. doi: 10.1146/annurev-publhealth-032013-182435
27. Egede LE, Ruggiero KJ, Frueh BC. Ensuring mental health access for vulnerable populations in COVID era. J Psychiatr Res. (2020) 129:147–8. doi: 10.1016/j.jpsychires.2020.07.011
28. Almeda N, García-Alonso C. Mental health planning at a very early stage of the COVID-19 crisis: a systematic review of online international strategies and recommendations. BMC Psychitr. (2021) 21:43. doi: 10.1186/s12888-020-03015-y
29. Stanley S, Balakrishnan S. Informal caregiving in schizophrenia: correlates and predictors of perceived rewards. Social Work Mental Health. (2021) 19:230–47. doi: 10.1080/15332985.2021.1904089
30. Ong HC, Ibrahim N, Wahab S. Psychological distress, perceived stigma, and coping among caregivers of patients with schizophrenia. Psychol Res Behav Managem. (2016) 9:211. doi: 10.2147/PRBM.S112129
31. Alam MS, Ali MJ, Bhuiyan AB, Solaiman M, Rahman MA. The impact of COVID-19 pandemic on the economic growth in Bangladesh: a conceptual review. Am Econ Soc Rev. (2020) 6:1–12. doi: 10.46281/aesr.v6i2.844
32. Fonseca L, Diniz E, Mendonca G, Malinowski F, Mari J, Gadelha A, et al. Schizophrenia and COVID-19: risks and recommendations. Braz J Psychiatr. (2020) 42:236–8. doi: 10.1590/1516-4446-2020-0010
33. Ampalam P, Gunturu S, Padma V. A comparative study of caregiver burden in psychiatric illness and chronic medical illness. Indian J Psychiatr. (2012) 54:239. doi: 10.4103/0019-5545.102423
34. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh DJ. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol. (2005) 40:899–904. doi: 10.1007/s00127-005-0963-5
35. Malakouti SK, Davoudi F, Khalid S, Asl MA, Khan MM, Alirezaei N, et al. The epidemiology of suicide behaviors among the countries of the Eastern Mediterranean Region of WHO: a systematic review. Acta Med Iranica. (2015) 53:257–65.
36. Mansouri N, Chimeh N, Dehghani M, Malakouti SK, Taherkhani H, Abarashi Z, et al. Risk factors associated with psychiatric hospitalization among Iranian schizophrenic patients. Iranian J Psychiatr Behav Sci. (2013) 7:16.
37. Mansouri N, Malakouti SK, Chimeh N, Rezvanifar S, Mohseni M, Mansouri E, et al. Chronic hospitalized and household maintained consumers; characteristics and differences among referees to the Iranian society supporting individuals with Schizophrenia. Iranian J Psychiatr Behav Sci. (2014) 8:5.
38. Ribé JM, Salamero M, Pérez-Testor C, Mercadal J, Aguilera C, Cleris M, et al. Quality of life in family caregivers of schizophrenia patients in Spain: caregiver characteristics, caregiving burden, family functioning, and social and professional support. Int J Psychiatry Clin Practice. (2018) 22:25–33. doi: 10.1080/13651501.2017.1360500
39. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
40. Ghamari GH, Molavi P, Heshmati R. Exploration of the factor structure of positive and negative syndrome scale in schizophrenia spectrum disorders. J Clin Psychol. (2010) 2:6.
41. Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. (1978) 133:429–35. doi: 10.1192/bjp.133.5.429
42. Tohen M, Bowden C, Nierenberg AA, Geddes J. Clinical Trial Design Challenges in Mood Disorders. Cambridge, Academic Press (2015).
43. Barekatain M, Tavakoli M, Molavi H, Maroufi M. Standardization, reliability and validity of the young mania rating scale. Psychology. (2007) 11:150–66.
44. Beck AT, Steer RA. Internal consistencies of the original and revised beck depression inventory. J Clin Psychol. (1984) 40:1365–7. doi: 10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D
45. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a persian-language version of the beck depression inventory–second edition: BDI-II-PERSIAN. Depress Anxiety. (2005) 21:185–92. doi: 10.1002/da.20070
46. Taghavi S. Validity and reliability of the general health questionnaire, (ghq-28) in college students of shiraz university. J Psychol. (2002) 5:381–98.
47. Pai S, Kapur RL. The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry. (1981) 138:332–5. doi: 10.1192/bjp.138.4.332
48. Chimeh N, Malakoti K, Panaghi L, Ahmad Abadi Z, Nojomi M. Care giver burden and mental health in schizophrenia. J Family Res. (2008) 4:277–92.
49. Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID-19 and Severe Mental Illness: Impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. (2020) 291:113265. doi: 10.1016/j.psychres.2020.113265
50. Rajkumar RP. Bipolar disorder, COVID-19, and the risk of relapse. Bipolar Disord. (2020) 22:640. doi: 10.1111/bdi.12947
51. Mutlu E, Anil Yagcioglu AE. Relapse in patients with serious mental disorders during the COVID-19 outbreak: a retrospective chart review from a community mental health center. Eur Arch Psychiatry Clin Neurosci. (2021) 271:381–3. doi: 10.1007/s00406-020-01203-1
52. Brettschneider, C., and Riedel-Heller, S., and König, H. (2014). A systematic review of economic evaluations of treatments for borderline personality disorder. PLoS ONE 9, e107748. doi: 10.1371/journal.pone.0107748
53. Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Aff Disorders. (2018) 226:45–51. doi: 10.1016/j.jad.2017.09.011
54. Kovács G, Almási T, Millier A, Toumi M, Horváth M, Kóczián K, et al. Direct healthcare cost of schizophrenia–European overview. Eur Psychiatr. (2018) 48:79–92. doi: 10.1016/j.eurpsy.2017.10.008
55. Pennington M, McCrone P. The cost of relapse in schizophrenia. Pharmacoeconomics. (2017) 35:921–36. doi: 10.1007/s40273-017-0515-3
56. O'Brien M, McNicholas F. The use of telepsychiatry during COVID-19 and beyond. Irish J Psychol Med. (2020) 37:250–5. doi: 10.1017/ipm.2020.54
57. Schuh Teixeira AL, Spadini AV, Pereira-Sanchez V, Ojeahere MI, Morimoto K, Chang A, et al. The urge to implement and expand telepsychiatry during the COVID- 19 crisis: early career psychiatrists' perspective. Rev Psiquiatr Salud Ment. (2020) 13:174–5. doi: 10.1016/j.rpsm.2020.06.001
58. Zarghami A, Farjam M, Fakhraei B, Hashemzadeh K, Yazdanpanah MH. A report of the telepsychiatric evaluation of SARS-CoV-2 patients. Telemed J E Health. (2020) 26:1461–5. doi: 10.1089/tmj.2020.0125
59. Campbell R, O'Gorman J, Cernovsky ZZ. Reactions of psychiatric patients to telepsychiatry. Ment Illn. (2015) 7:6101. doi: 10.4081/mi.2015.6101
60. Hungerbuehler I, Valiengo L. Home-based psychiatric outpatient care through videoconferencing for depression: a randomized controlled follow-up trial. JMIR Mental. (2016) 3:e36. doi: 10.2196/mental.5675
61. Avalone L, Barron C, King C, Linn-Walton R, Lau J, McQuistion HL, et al. Rapid telepsychiatry implementation during COVID-19: increased attendance at the largest health system in the United States. Psychiatr Serv. (2021) 72:708–11. doi: 10.1176/appi.ps.202000574
62. Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G, et al. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses. (2014) 8:21–7. doi: 10.3371/CSRP.KAFE.021513
63. Baker AL, Turner A, Beck A. Telephone-delivered psychosocial interventions targeting key health priorities in adults with a psychotic disorder: systematic review. Psychol Med. (2018) 48:2637–57. doi: 10.1017/S0033291718001125
64. Ramalho R, Adiukwu F, Gashi Bytyçi D, El Hayek S, Gonzalez-Diaz JM, Larnaout A, et al. Telepsychiatry and healthcare access inequities during the COVID-19 pandemic. Asian J Psychiatr. (2020) 53:102234. doi: 10.1016/j.ajp.2020.102234
65. Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer J, Patel V, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry. (2017) 4:486–500. doi: 10.1016/S2215-0366(17)30096-2
66. De Sousa A, Mohandas E, Javed A. Psychological interventions during COVID-19: challenges for low and middle income countries. Asian J Psychiatr. (2020) 51:102128. doi: 10.1016/j.ajp.2020.102128
67. Diwan MN, Ali Awan H, Aamir A, Filippis DE, Ullah R. Telepsychiatry in low- and middle-income countries during COVID-19: pandemic, barriers, and road model. J Nerv Mental Dis. (2021) 209:144–6. doi: 10.1097/NMD.0000000000001245
68. Moudatsou M, Koukouli S. Caring for patients with psychosis: mental health professionals' views on informal caregivers' needs. J Environ Pub Health. (2021) 18:2964. doi: 10.3390/ijerph18062964
69. Malakouti SK, Nouri Ghasem Abadi R, Naghavi Ravandi M, Ahmadi Abhari SA, Nasr Esphahani M, Afgheh S, et al. The burden of caregivers of chronic mental patients and their needs to care and therapeutic services. Hakim Res J. (2003) 6:1–10.
70. Ebrahim OS, Al-Attar GST, Gabra RH, Osman DMM. Stigma and burden of mental illness and their correlates among family caregivers of mentally ill patients. J Egypt Pub Health Assoc. (2020) 95:31. doi: 10.1186/s42506-020-00059-6
71. Zoladl M, Afroughi S, Nooryan K, Kharamin S, Haghgoo A, Parandvar Y, et al. Applying collaborative care model on intensive caregiver burden and resilient family caregivers of patients with mental disorders: a randomized controlled trial. Iran J Psychiatry. (2020) 15:17–26. doi: 10.18502/ijps.v15i1.2436
72. Yasuma N, Yamaguchi S. Care difficulties and burden during COVID-19 pandemic lockdowns among caregivers of people with schizophrenia: a cross-sectional study. Neuro Rep. (2021) 41:241–7. doi: 10.1002/npr2.12171
73. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. (2020) 29:2047–9. doi: 10.1111/jocn.15296
74. Gulati G, Kelly BD. Domestic violence against women and the COVID-19 pandemic: what is the role of psychiatry? Int J Law Psychiatry. (2020) 71:101594. doi: 10.1016/j.ijlp.2020.101594
75. Mazza M, Marano G, Lai C, Janiri L, Sani G. Danger in danger: interpersonal violence during COVID-19 quarantine. Psychiatry Res. (2020) 289:113046. doi: 10.1016/j.psychres.2020.113046
76. Nirmala BP, Vranda MN, Reddy S. Expressed emotion and caregiver burden in patients with schizophrenia. Indian J Psychol Med. (2011) 33:119–22. doi: 10.4103/0253-7176.92052
Keywords: SMIs, COVID-19, caregiver burden, telepsychiatry, Iran, schizophrenia, bipolar mood disorder
Citation: Nooraeen S, Bazargan-Hejazi S, Naserbakht M, Vahidi C, Shojaerad F, Mousavi SS and Malakouti SK (2023) Impact of COVID-19 pandemic on relapse of individuals with severe mental illness and their caregiver's burden. Front. Public Health 11:1086905. doi: 10.3389/fpubh.2023.1086905
Received: 01 November 2022; Accepted: 05 January 2023;
Published: 01 February 2023.
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
S. M. Yasir Arafat, Enam Medical College, BangladeshCopyright © 2023 Nooraeen, Bazargan-Hejazi, Naserbakht, Vahidi, Shojaerad, Mousavi and Malakouti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seyed Kazem Malakouti,  bWFsYWtvdXRpLmtAaXVtcy5hYy5pcg==
bWFsYWtvdXRpLmtAaXVtcy5hYy5pcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.