
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 14 February 2023
Sec. Occupational Health and Safety
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1082874
 Sajjad Mozaffari1
Sajjad Mozaffari1 Behzad Heibati2,3
Behzad Heibati2,3 Maritta S. Jaakkola2,3
Maritta S. Jaakkola2,3 Taina K. Lajunen2,3
Taina K. Lajunen2,3 Safa Kalteh4
Safa Kalteh4 Hadi Alimoradi5
Hadi Alimoradi5 Mahsa Nazari6
Mahsa Nazari6 Ali Karimi1*†
Ali Karimi1*† Jouni J. K. Jaakkola2,3,7*†
Jouni J. K. Jaakkola2,3,7*†Background: The steel factory work environment contains various chemical exposures that can affect indoor air quality and have impact on respiratory health of the workers.
Aims: The objective of this study was to assess potential effects of occupational exposures in steel factory workers in Iran on the respiratory symptoms, occurrence and the lung function levels.
Method: This was a cross-sectional study of 133 men working in a steel factory forming the exposed group and 133 male office workers forming the reference group from a steel company in Iran. The participants filled in a questionnaire and underwent spirometry. Work history was used both as dichotomous (exposed/reference) and a quantitative measure of exposure, the latter measured as duration of exposure in the specified work (in years) for the exposed group and zero for the reference group.
Results: Multiple linear regression and Poisson regression were used to adjust for confounding. In Poisson regression analyses, an increased prevalence ratio (PR) of all respiratory symptoms was observed in the exposed group. Lung function parameters were significantly reduced in the exposed group (p < 0.001). There was a dose–response relation between duration of occupational exposures and reduction in the predicted value of FEV1/FVC level (0.177, 95% CI −0.198 to −0.156) in all models.
Conclusion: The results of these analyses showed that occupational exposures in steel factory work increase the prevalence of respiratory symptoms and reduce lung function. Safety training and workplace conditions were found to need improvement. In addition, use of proper personal protective equipment is recommended.
In steel industry, exposure to airborne contaminants is considered a risk factor for pulmonary diseases and for occurrence of pathological changes in airways (1, 2). Suspended metals, dust, and toxic gases in steelwork may increase the risk of respiratory symptoms related to diseases such as pneumoconiosis, bronchial asthma, COPD, and cancers (3, 4). Occupational exposure to harmful gases and fumes may cause a variety of respiratory outcomes, and these exposures may also lead to a significant decrease in pulmonary function, such as forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and FEV1/FVC. Workers are often asymptomatic for a long time and may be diagnosed at a so late stage of the disease prevention or treatments are no longer effective (5). Dust particles are ubiquitous pollutants in the work environment of steel industry and are generated from iron ore, coke, and manganese processing steps. Potential association between occupational air pollutants, such as dust and heavy metals, and potential health effects has been a subject of research in several previous studies. For example, Soyseth et al. (6) reported that the prevalence of airflow limitation was higher in Norwegian exposed workers from smelters compared to non-exposed smelter employees. Chen et al. (7) reported that reduced lung function detected in Taiwanese steelworkers is partly due to exposure to inhalable dust particles and it can lead to reduction of both forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1). Johnsen et al. (8) studied the relationship between occupational dust exposure and annual change in lung function among workers in 15 Norwegian smelters. Their results showed that in all smelters there was an annual decline in FEV1 in relation to increasing dust exposure (8). Johnsen et al. investigated potential impairment of lung function among workers from Norwegian smelters. They found that such impairment was significantly related to the job categories of line operator and non-line operator compared to the non-exposed employees (4). Søyseth et al. (9) found a significant association between occupational exposure and the incidence of airflow limitation in non-smoking workers from Norwegian smelters. Søyseth et al. (10) also investigated dust exposure and the incidence of work-related asthma-like symptoms (WASTH) in workers from Norwegian Smelters. They concluded that dust exposure was associated with an increased incidence of WASTH (10). Singh et al. (11) reported from India that the spirometric parameters including FVC, FEV1, FEV1/FVC ratio, FEF25–75, PEFR, PIFR, and FIVC were all significantly lower in an exposed group of steel workers compared to a reference group. Mousavian et al. (12) have reported exceeding air concentrations of Cr in a workplace from Iranian steel industry. In the study of Girma and Kebede (13) from Ethiopia, the FVC values of steel factory workers showed a strong negative correlation with duration of work and age of responders, and a weak negative correlation with the level of particulate matter (PM). Consistently with this, FEV1 values were strongly negatively correlated with exposure duration and the age of workers, while they were weakly negatively correlated with cross-sectional PM levels in the steel factory (13). Summarizing the literature, a significant reduction of ventilatory lung function and an increase in the occurrence of some respiratory symptoms, including prolonged cough, phlegm production, wheezing, bronchitis, shortness of breath, and bronchial asthma, as well as increased number of sick leaves have been found to be associated with long-term exposure to inorganic dust, fumes and toxic gases. However, to date, no study has been conducted on potential effects of occupational exposures of steel factory work on respiratory health among workers from the Middle Eastern countries, such as Iran. To fill in this gap in knowledge, the objectives of this study were to assess potential effects of occupational exposures in steel industry workers in Iran on the occurrence of respiratory symptoms and on the lung function level.
This was a cross-sectional study of steel factory workers (the exposed group) and office workers (the reference group) from Iran. We invited 133 factory workers and 133 office workers from the same factory located in Isfahan. All individuals in both the exposed and unexposed groups (response rates 100%) participated in this study. The exposed group included general workers (n = 92), CO2 welding workers (n = 7), electric welding workers (n = 11), induction arc furnace workers (n = 13), and electric arc furnace workers (n = 10). Office workers were managers and other administrative staff, and the unexposed reference group also included chauffeurs and security staff. The sample size was based on a comparison of the prevalence of respiratory symptoms between the exposed and the reference group (beta = 90%, alpha = 0.05) (14).
The data collection comprised of three parts: air sampling, an interviewer-administered questionnaire and spirometry measurements. First, baseline information from the units with exposure emissions and subjects working there was collected. Information on respiratory symptoms, including current cough, phlegm production, cough with phlegm, wheezing, shortness of breath, and chest tightness were collected by using a standardized respiratory questionnaire translated and modified from the American Thoracic Society's (ATS) respiratory questionnaire (15). Data collection was based on this structured questionnaire and spirometric pulmonary functions tests (PFTs). The questionnaire also included information on (1) individual and working characteristics (age, gender, work experience, marital status, educational level, average working hours per day and per week), (2) history of respiratory diseases, and (3) smoking habits (as cigarettes/day). Participants were advised “If you are in doubt whether the answer is yes or no, answer no” (16). The pulmonary function tests for both groups were performed by the same technician at the workplaces. All participants gave written informed consent after being introduced to the nature of the study, potential risks and how their data may be used. The study was approved by the ethics committee of the Tehran University of Medical Sciences.
The measurements and assessment of inhaled pollutants were performed as follows: The environmental and personal air sampling was carried out in 12 operation units (7 units sampled dust and 5 units fumes) to determine the pollutant concentrations and exposure levels of the workers. Calibrated personal sampling devices (manufactured by Casella, UK) were used to measure the concentrations of particles and of metal fumes at these stations in accordance with the OSHA guidelines. Dust samples were analyzed by gravimetric method, and fume samples were analyzed by atomic absorption spectrometry.
All the participants performed a spirometric lung function test with Fukuda Sangyo ST-150 spirometer (Fukuda, Japan). Forced vital capacity % predicted (FVC%) and forced expiratory volume in the first second % predicted (FEV1%) were already adjusted for sex, age, and height in the prediction equations. These were based on GLI spirometry reference values, i.e., multi-ethnic reference values for spirometry for the 3–95-year age range (17). FVC and FEV1 are the two essential parameters that measure ventilatory lung function. The accuracy and reproducibility of the test results by spirometry are affected by calibration of the device, operator experience, and effort of the patient to carry out the test correctly (18). In this study, the calibration and quality control of spirometry as well as performance of the flow volume measurements were carried out applying the guidelines of the American Thoracic Society and the European Respiratory Society Technical Statement (19). Lung function findings were then categorized into normal, obstruction, restriction, and combined obstruction with restriction.
Prevalence ratio (PR) was applied as the measure of effect of exposure on the risk of respiratory symptoms. We estimated adjusted PR's by Poisson regression analysis with logarithmic link function (SAS procedure GENMOD). We applied LSMEANS statement to obtain the effect estimates and their 95% CIs. The analyses of the respiratory symptoms were first adjusted for age and body mass index (BMI) (model 1), then additionally for smoking (model 2). Multiple linear regression was used to estimate the potential effects of occupational exposures on lung function levels. Work history was used as the quantitative measure of exposure, expressed as the duration of exposure in the specified work (in years) for the exposed group. For the reference group, the value of zero was given for this variable. The analyses of the absolute lung function levels (FEV1, FVC and FEV1/FVC) were first adjusted for age, height, and weight (model 1), and then additionally for smoking (model 2). We conducted sensitivity analyses by excluding smokers. We also used the Haldane-Anscombe correction by adding 0.5 to all cells for wheezing and chest tightness symptoms with zero observations in the unexposed group to be able to estimate the PRs and the 95% confidence intervals (CIs). Data analyses were performed applying SAS V.9.4 statistical package.
The characteristics of the study population divided into the exposed group and the reference group are shown in Table 1. There were no statistically significant differences between the groups in terms of age, height, weight, BMI, or work history. Smoking was more common in the exposed group (p < 0.001).
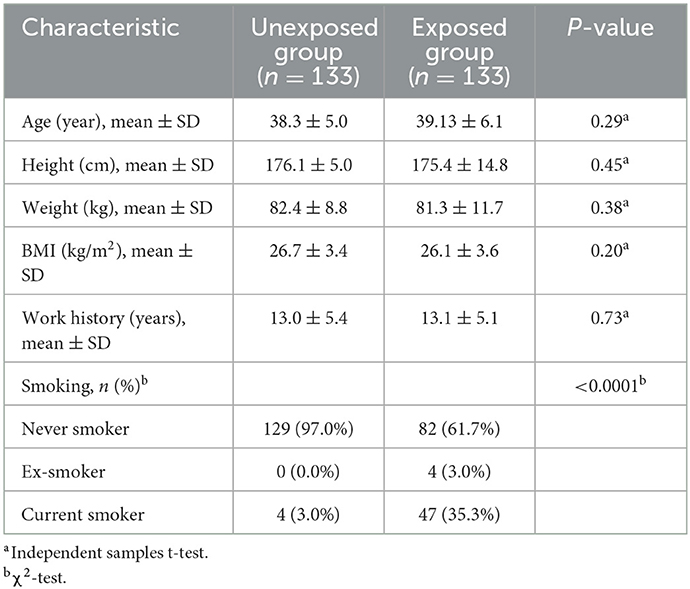
Table 1. Characteristics of the study population including 133 steel factory workers and 133 office workers.
Table 2 shows the results of environmental measurements at the monitoring sites. The mean concentration of dust in six stations and the mean concentration of fumes (Fe and Mn) in two stations (conducting CO2 welding and electric welding) were above the corresponding acceptable exposure limit. The highest mean concentrations of dust were found in workshop 1 (wood dust, 4 mg/m3) and workshop 4 (casting sand, 0.83 mg/m3). The mean concentrations of dust in five workshops (wood and casting sand workshops 1,2,3,4 and 5) and the mean concentrations of fumes in CO2 welding (Fe and Mn) and Electric welding (Fe) exceeded the designated acceptable exposure limits (20). The levels of dust in workshops 2–5 were 7.6, 16.2, 16.6, and 10.6 times higher than the acceptable exposure limits (Table 2). In the CO2 welding unit, the levels of Fe fumes slightly exceeded the maximum allowable limit, while the levels of Mn fumes were 2.7 times greater than the acceptable limit. In addition, the Fe fumes in electric welding unit were slightly greater than the permissible exposure limit.
Figure 1 and Supplementary Table S1 show the prevalence of lung function deficits in the two categories of both groups. The overall prevalence of lung function impairment was 100% (n = 113) in the exposed group, while it was 10.5% (n = 14) in the reference group. In the exposed group, the majority of those with lung function impairment had a combination of obstruction with restriction (54.9%), followed by obstruction alone (45.1%). In addition, obstruction with restriction (75.6%) and obstruction alone (54.4%) were found to be the major impairments among those who were exposed to fumes and dust, respectively.
The prevalence of respiratory symptoms in the exposed and reference groups is presented in Table 3. The exposed group showed consistently a higher prevalence of all respiratory symptoms. In the fully adjusted models, the PR (95% CI) was 20.20 (7.0–58.39) for cough, 24.01 (7.19–80.20) for phlegm, 24.30 (7.48–78.83) for cough with phlegm, and 15.93 (4.84–52.40) for shortness of breath. In addition, the PRs of respiratory symptoms related to fume and dust exposures, when these were evaluated separately, were statistically significantly increased in the exposed group compared to the reference group (Table 3).
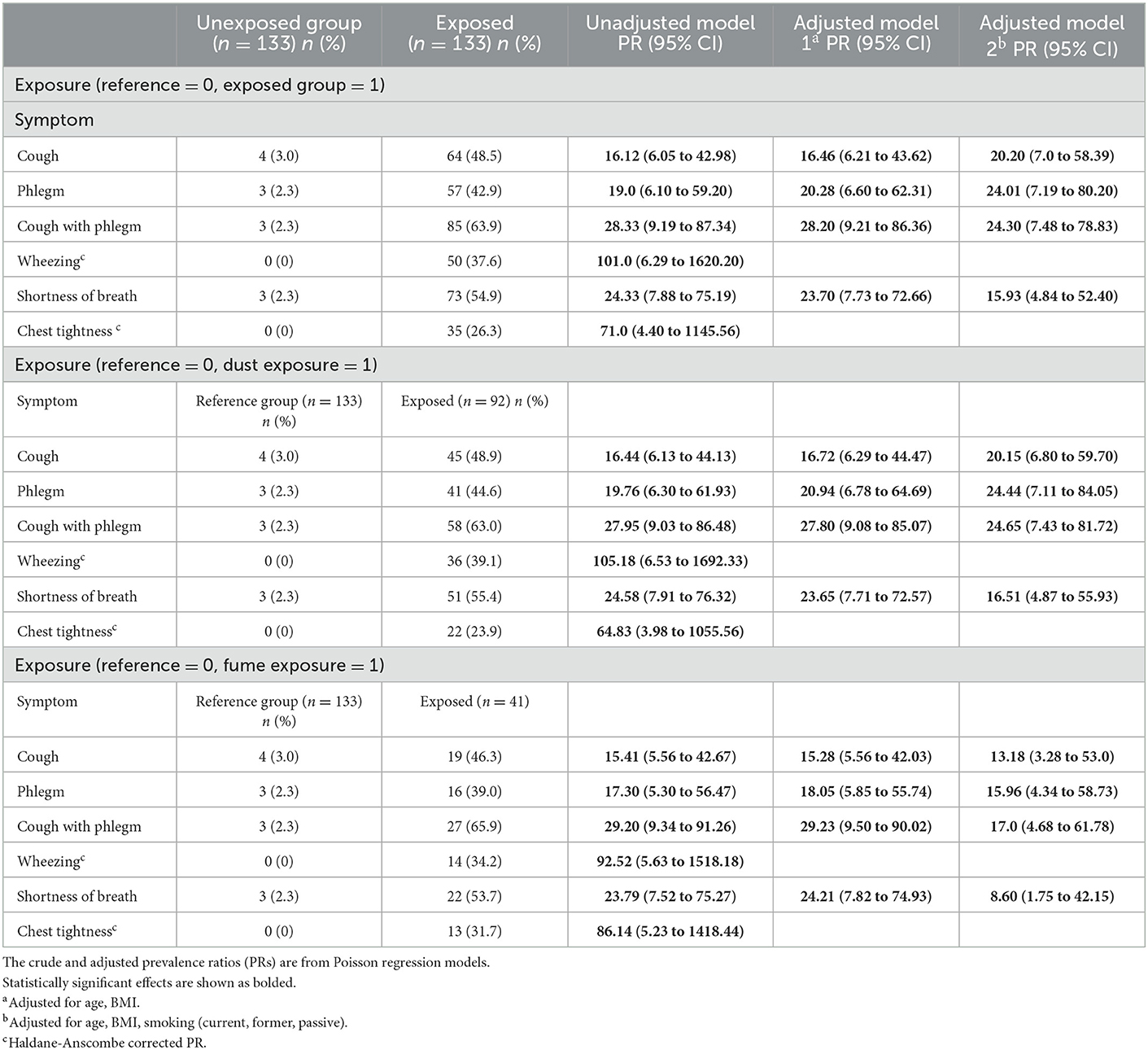
Table 3. Prevalence of respiratory symptoms among steel factory workers compared to the reference group.
Table 4 shows the effects of the steel work exposure on the absolute pulmonary function levels and on %-predicted measures. The absolute FEV1, FVC, and FEV1/FVC levels were reduced among the exposed group compared to the reference group even after adjusting for confounders, including smoking. A dose–response pattern was observed for the associations between work duration and lung function levels. In the unadjusted model, there was a significant reduction in the absolute and the %-predicted FEV1 for each year of increasing work duration. Statistically significant reduction in FEV1/FVC % predicted was detected per year of exposure duration in all models. In addition, the levels of all absolute pulmonary function parameters were lower among workers exposed to both dust and fumes (when these were evaluated separately) and compared to the office workers.
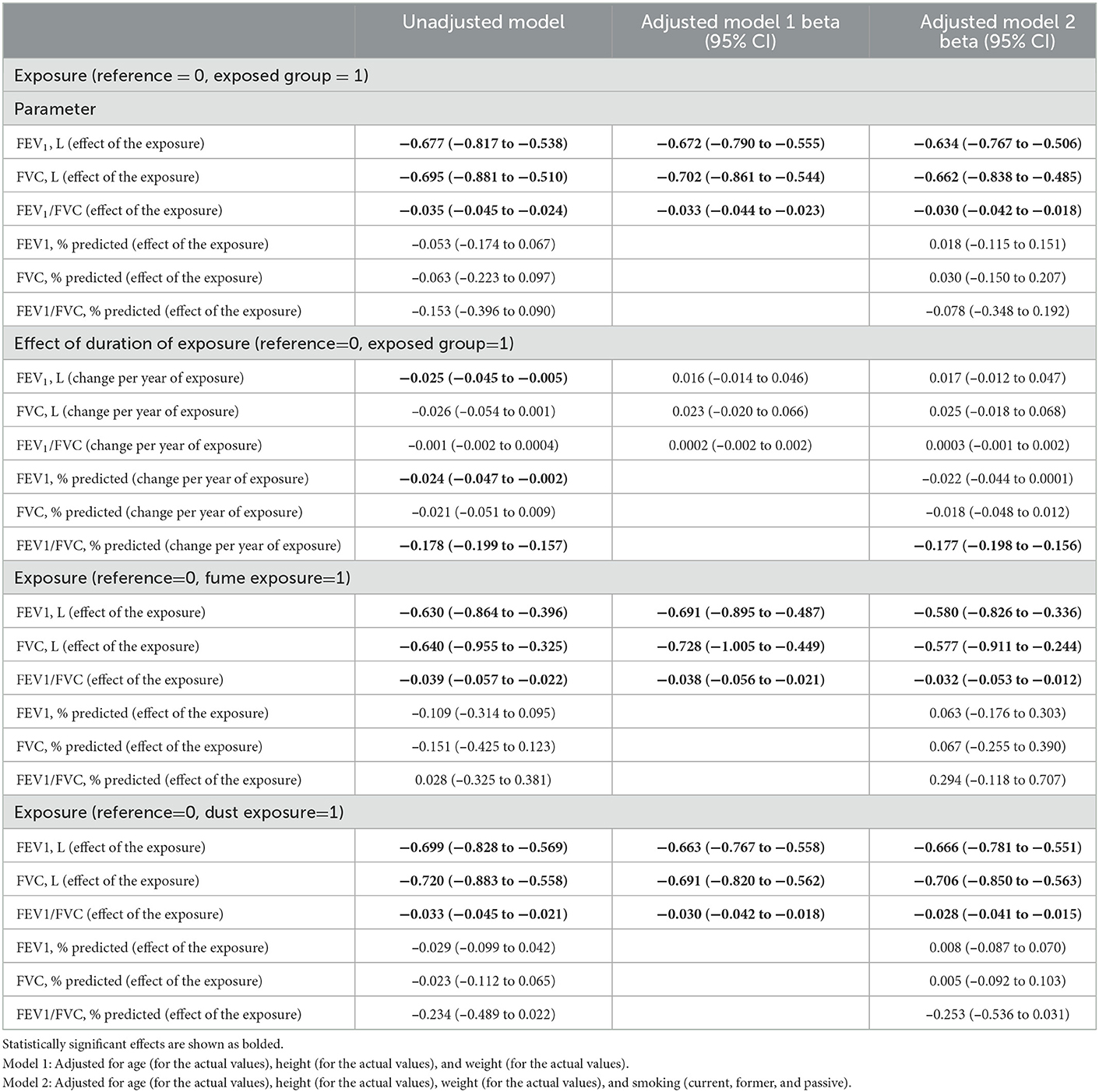
Table 4. Effects on lung function parameters in relation to any exposure, duration of exposure and exposure to fumes and dusts separately.
In this cross-sectional study, the prevalence of respiratory symptoms and level of lung function parameters were compared between steel factory workers and office workers from the same steel industry. We found that exposed study subjects experienced increased prevalence of all respiratory symptoms. Furthermore, the prevalences of obstruction, and obstruction in combination with restriction were higher in the exposed group (Supplementary Table S1). We also observed significant reductions in the absolute pulmonary function levels in the exposed group, and when addressing different types of steel work exposures separately, among those exposed to either fumes or dust when compared to the reference group. Both the absolute and %-predicted values of FEV1 were significantly related to the duration of steel factory exposure in the unadjusted model. Predicted FEV1/FVC% was significantly related to the exposure duration even after adjustment for confounding factors. The results of the sensitivity analyses indicated similar effect estimates (data not shown).
All individuals in both groups (response rates 100%) participated in this study. The characteristics of the study population, apart from smoking habits, were not statistically significantly different between the compared groups. This was a cross-sectional study, so it was not feasible to elaborate on the possibility that workers with respiratory health problems may have been more likely to leave work compared to workers who remained healthy. This type of selection bias would lead to underestimation of the relations of interest, i.e., our estimates could underestimate the real effects. We collected information on several characteristics of the study population and adjusted the analyses of respiratory symptoms and lung function for personal characteristics (BMI, age) and for smoking. Therefore, we believe that confounders are not a likely explanation for our findings.
We found increased occurrence of respiratory symptoms and reduced spirometric lung function parameters among steel factory workers. Our results are in line with some prior studies conducted in steel industry as well as in other industries. Sobaszek et al. (21) reported acute respiratory effects of welding fumes in the workplace by measuring the across-shift changes in a population of 144 stainless steel (SS) and mild steel (MS) welders and 223 controls. A significant decrease in forced vital capacity (FVC) during the shift was observed. Moreover, the across-shift decreases in FEV1, FVC, and peak expiratory flow (PEF) were significantly related to the Manual Metal Arc welding process, compared with Metal Inert Gas techniques (PEF = −2.7% of baseline values (SD, 11.9) vs. 2.0% of baseline values (SD, 7.7) P = 0.04; FVC = −1.5% of baseline values (SD, 4.8) vs. 0.2% of baseline values (SD, 4.5) P = 0.05). A significant influence of the duration of stainless-steel welding exposure on the change of lung function during the work shift was reported. No significant differences between smokers, ex-smokers, and never-smokers were found in terms of the change of ventilatory function during the work shift. The authors concluded that welding-related lung function reductions are seen in stainless-steel welders compared with mild steel welders, as well as in those with a longer lifetime welding history. Giahi et al. (1) examined FVC, FEV1, and FEV1/FVC levels between the exposed and the reference groups in a steel plant from Iran. Their analysis showed that FEV1/FVC values were statistically significantly lower in the exposed group (1). Another study by Koo et al. (22) from South Korea investigated potential effect of silica dust on pulmonary function levels in foundry workers. They found that excess exposure to silica dust among the exposed workers was associated with lower lung function levels, apart from FVC levels, suggesting obstructive pattern (23). Gholami et al. (24) from Iran reported statistically significantly reduced levels of pulmonary function parameters (including FVC, FEV1, FEV1/ FVC, and PEF) in the exposed compared to non-exposed workers at an iron-ore mine in eastern Iran (23). Several other studies have also associated increased dust levels with decreased pulmonary function levels in different types of industries, including brick manufacturing, tile and ceramic industry, and steel industry (7, 13, 24–26).
In our study, all respiratory symptoms were more prevalent in the exposed group compared to the reference group. Sakar et al. (27) found cough and mucus as the most prevalent symptoms among ceramic workers from Turkey. Other studies from Iran have indicated that occupational exposure to excessive levels of dust leads to respiratory symptoms, including cough, mucus production and shortness of breath (1, 23). Similar findings have been reported from other studies conducted in different types of industries, including stoneworkers, miners, and cement factory workers (23, 28). In the present study, we found that the dust levels exceeded the acceptable limit in most of the workstations. We showed that occupational exposure to indoor pollutants in a steel factory laeds to increased respiratory symptoms in the exposed workers compared to office workers. In addition, our study showed a dose-response effect of steel work exposure on reduction of FEV1 (both absolute level and %-predicted). The predicted value of FEV1/FVC% was also reduced significantly in relation to the duration of exposure even after adjustment for confounding. This finding is consistent with the studies conducted in Tanzania and Iran. Mwaiselage et al. (28) studied potential effects of cement dust exposure on ventilatory lung function. They found an increased odds ratio of 9.9 (95% CI: 3.5–27.6) for airflow limitation among workers with cumulative total dust exposure of >300.0 mg/m3 compared to workers with cumulative total dust exposure of <100.0 mg/m3 year. This indicated that workers with long-term exposure to high cement dust levels experienced an excess risk of developing airflow limitation (28). Gholami et al. (24) reported an association (OR: 1.155, CI: 1–1.333) between respirable dust exposure among iron ore mine workers and increased occurrence of shortness of breath (23). Aminian et al. (29) found an association between exposure to workplace fumes and dust and shortness of breath (OR: 4.55, CI: 1.66–12.45) among workers of a steel galvanization factory in Arak, Iran. Consistently with previous studies, our results showed that workers from a steel factory experience an increased risk of respiratory symptoms. Furthermore, our study found signs of reduced FEV1 and FEV1/FVC, which is consistent with obstructive lung disease. In addition, some workers had reduced FVC levels, which suggests restrictive lung function impairment in relation to exposure to dusts in our study. Reduced FEV1 and FEV1/FVC levels were associated with years of exposure in the study by Meo et al. (30), which was in line with our findings.
As the work-related adverse respiratory effects among steel factory workers are likely to be mostly preventable, we recommend that primary preventive actions should be conducted whenever it is possible. As we found in this study, steel factory workplaces still have not taken widely into use basic precautionary measures, such as training on how to protect against exposures present at such factory work or on how to recognize if there is a need for respiratory protection. Such training should also include information on the type of protective equipment that should be used when harmful exposures cannot be avoided in other ways. Another important task is to provide training on how to use protective masks in appropriate way, especially when it is not possible to provide specific local ventilation. For example, N95 respirators recommended by the US National Occupational Safety and Health Administration (OSHA) would provide protection against many particulates but they provide little protection against vapors or gasses (20).
We assume that the environmental conditions and the workers of the studied factory represent well the situation in other factories in Iran and other countries in the same region and thus, the results are generalizable to factory workplaces in Middle Eastern countries and to countries with similar production and standards of living.
This study investigated the relations between occupational exposures in a steel factory and occurrence of respiratory symptoms and lung function deficits in workers of this industry. Our study provides evidence that exposure to dust and fumes in steel industry is related to significantly increased occurrence of respiratory symptoms, and to significant spirometric lung function deficits, including both restriction and obstruction. A dose–response relation was shown between years of employment in steel industry and reduced level of both absolute and %-predicted FEV1. Thus, these results showed that the exposed workers in steel industry are at a high risk of experiencing several respiratory symptoms and lung function impairment. Taking into use appropriate protective respiratory equipment and application of efficient local exhaust system and ventilation is recommended in the future for the steel industry to protect the workers' health.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Tehran University of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Data were collected by SM, SK, HA, and MN. Analysis was performed by TL and BH. The manuscript was drafted by BH, MJ, and SM. Reviewed by MJ and supervised with AK and JJ. SM and BH contributed equally to this paper. All authors were involved in editing of the manuscript for intellectual content.
This study was not funded by the industry itself or by any governmental agency. BH was funded by Biocenter Oulu, Finland. TL was financially supported by the Ella and Georg Ehrnrooth Foundation and by Jenny and Antti Wihuri Foundation. JJ and MJ were supported by the Academy of Finland (grant no. 310372).
The authors would like to thank all subjects participating in this study as well as the occupational health unit of the studied steel factory for giving us the opportunity to carry out this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1082874/full#supplementary-material
1. Giahi O, Darvishi E, Sarabi M, Shahsavari S. The relationship between exposure to respiratory pollutants and pulmonary function tests capacities in steel industry workers. Sci J Kurd Uni Med Sci. (2014) 19:135–45.
2. Ahmad I, Balkhyour MA. Occupational exposure and respiratory health of workers at small scale industries. Saudi J Biol Sci. (2020) 27:985–90. doi: 10.1016/j.sjbs.2020.01.019
3. Vanka KS, Shukla S, Gomez HM, James C, Palanisami T, Williams K, et al. Understanding the pathogenesis of occupational coal and silica dust-associated lung disease. Eur Respir Rev. (2022) 31:210250. doi: 10.1183/16000617.0250-2021
4. Johnsen HL, Kongerud J, Hetland S, Benth JŠ, Søyseth V. Decreased lung function among employees at Norwegian smelters. Am J Respir Crit Care Med. (2008) 51:296–306. doi: 10.1002/ajim.20557
5. Mehrifar Y, Zamanian Z, Pirami H. Respiratory exposure to toxic gases and metal fumes produced by welding processes and pulmonary function tests. Int J Occup Environ Med. (2019) 2019:40–9. doi: 10.15171/ijoem.2019.1540
6. Søyseth V, Johnsen HL, Bugge MD, Hetland SM, Kongerud J. Prevalence of airflow limitation among employees in Norwegian smelters: a longitudinal study. Occup Environ Med. (2011) 68:24–9. doi: 10.1136/oem.2009.049452
7. Chen P-C, Doyle PE, Wang J-D. Respirable dust exposure and respiratory health in male Taiwanese steelworkers. Ind Health. (2006) 44:190–9. doi: 10.2486/indhealth.44.190
8. Johnsen HL, Hetland SM, Benth JS, Kongerud J, Søyseth V. Dust exposure assessed by a job exposure matrix is associated with increased annual decline in FEV1: a 5-year prospective study of employees in Norwegian smelters. Am J Respir Crit Care Med. (2010) 181:1234–40. doi: 10.1164/rccm.200809-1381OC
9. Søyseth V, Johnsen HL, Bugge MD, Hetland SM, Kongerud J. Incidence of airflow limitation among employees in Norwegian smelters. Am J Ind Med. (2011) 54:707–13. doi: 10.1002/ajim.20946
10. Søyseth V, Johnsen HL, Henneberger PK, Kongerud J. The incidence of work-related asthma-like symptoms and dust exposure in Norwegian smelters. Am J Respir Crit Care Med. (2012) 185:1280–5. doi: 10.1164/rccm.201110-1809OC
11. Singh LP, Bhardwaj A, Deepak KK. Occupational exposure to respirable suspended particulate matter and lung functions deterioration of steel workers: an exploratory study in India. Int Sch Res Notices. (2013) 2013:1–9. doi: 10.1155/2013/325410
12. Mousavian NA, Mansouri N, Nezhadkurki F. Estimation of heavy metal exposure in workplace and health risk exposure assessment in steel industries in Iran. Measurement. (2017) 102:286–90. doi: 10.1016/j.measurement.2017.02.015
13. Girma F, Kebede Z. Dust exposure associations with lung function among Ethiopian steel workers. Ann Glob Health. (2019) 85:12. doi: 10.5334/aogh.2422
14. Dupont WD, Plummer WD. Power and sample size calculations for studies involving linear regression. Control Clin Trials. (1998) 19:589–601.
15. Society AT. Recommended respiratory disease questionnaires for use with adults and children in epidemiological research. Am Rev Respir Dis. (1978) 118:7–53.
16. Spruit MA, Singh SJ, Garvey C, Rochester CL, Vogiatzis I, Holland AE, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. (2013) 188:e13–64.
17. Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir Soc. (2012) 40:1324–43. doi: 10.1183/09031936.00080312
18. Christine Jenkins WJ. Better Living with Chronic Obstructive Pulmonary Disease. Milton: Lung Foundation Australia (2006).
19. Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American thoracic Society and European respiratory Society technical statement. Am J Respir Crit Care Med. (2019) 200:e70–88. doi: 10.1164/rccm.201908-1590ST
20. OSHA. Enforcement Guidance for Personal Protective Equipment in General Industry Personal Protective Equipment. Washington, DC: OSHA (2011). Available online at: https://www.osha.gov/news/newsreleases/trade/02152011 (accessed February 15, 2011).
21. Vaz Fragoso CA, Concato J, McAvay G, Van Ness PH, Rochester CL, Yaggi HK, et al. The ratio of FEV1 to FVC as a basis for establishing chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2010) 181:446–51. doi: 10.1164/rccm.200909-1366OC
22. Puente-Maestu L, Stringer WW. Physical activity to improve health: do not forget that the lungs benefit too. Eur Respir Soc. (2018) 51:1702468. doi: 10.1183/13993003.02468-2017
23. Koo JW, Chung CK, Park CY, Lee SH, Lee KS, Roh YM, et al. The effect of silica dust on ventilatory function of foundry workers. J Occup Health. (2000) 42:251–7. doi: 10.1539/joh.42.251
24. Gholami A, Tajik R, Atif K, Zarei AA, Abbaspour S, Teimori-Boghsani G, et al. Respiratory symptoms and diminished lung functions associated with occupational dust exposure among iron ore mine workers in iran. Open Respir Med J. (2020) 14:1. doi: 10.2174/1874306402014010001
25. Dehghan F, Mohammadi S, Sadeghi Z, Atarchi M. Respiratory complaints and spirometric parameters in tile and ceramic factory workers. TANAFFOS. (2009) 8:19–25.
26. Zuskin E, Mustajbegovic J, Schachter EN, Kern J, Doko-Jelinic J, Godnic-Cvar J. Respiratory findings in workers employed in the brick-manufacturing industry. J Occup Environ Med. (1998) 40:814–20.
27. Sakar A, Kaya E, Celik P, Gencer N, Temel O, Yaman N, et al. Evaluation of silicosis in ceramic workers. Tuberk Toraks. (2005) 53:148–55.
28. Mwaiselage J, Bråtveit M, Moen B, Mashalla Y. Cement dust exposure and ventilatory function impairment: an exposure–response study. J Occup Environ Med. (2004) 46:658–67. doi: 10.1097/01.jom.0000131787.02250.79
29. Aminian O, Zeinodin H, Sadeghniiat-Haghighi K, Izadi N. Respiratory symptoms and pulmonary function tests among galvanized workers exposed to zinc oxide. J Res Health Sci. (2015) 15:159–62.
Keywords: air quality, pulmonary function (PF), respiratory symptom, steel industry, epidemiological
Citation: Mozaffari S, Heibati B, Jaakkola MS, Lajunen TK, Kalteh S, Alimoradi H, Nazari M, Karimi A and Jaakkola JJK (2023) Effects of occupational exposures on respiratory health in steel factory workers. Front. Public Health 11:1082874. doi: 10.3389/fpubh.2023.1082874
Received: 28 October 2022; Accepted: 20 January 2023;
Published: 14 February 2023.
Edited by:
Mohammad Reza Khazdair, Birjand University of Medical Sciences, IranReviewed by:
Samrad Mehrabi, Shiraz University of Medical Sciences, IranCopyright © 2023 Mozaffari, Heibati, Jaakkola, Lajunen, Kalteh, Alimoradi, Nazari, Karimi and Jaakkola. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Karimi,  YV9rYXJpbWlAc2luYS50dW1zLmFjLmly; Jouni J. K. Jaakkola,
YV9rYXJpbWlAc2luYS50dW1zLmFjLmly; Jouni J. K. Jaakkola,  am91bmkuamFha2tvbGFAb3VsdS5maQ==
am91bmkuamFha2tvbGFAb3VsdS5maQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.