
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 17 February 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1082637
This article is part of the Research Topic World AIDS Day 2022: Putting ourselves to the test: achieving equity to end HIV View all 30 articles
Background: In China, the HIV/AIDS epidemic among men who have sex with men (MSM) has been expanding in recent years. Substance abuse in MSM was not well studied as the independent risk factor for HIV and syphilis infection and other sexually transmitted diseases. The present review aimed to determine the correlation between HIV/Syphilis infections and substance abuse and other sexual risk behaviors among MSM.
Methods: We conducted a comprehensive search of PubMed, Web of Science, Embase, Scopus, Chinese National Knowledge Infrastructure, Chinese Wanfang Data, and VIP Chinese Journal Database for relevant articles of quantitative studies published between 2010 and May 31, 2022. Meta-analysis was performed using R software. Pooled estimated of the association-odds ratio, with 95% confidence intervals were calculated using random-effects models stratified by study design. Q statistics and I2 were used to measure the heterogeneity.
Results: Our meta-analysis included 61,719 Chinese MSM from 52 eligible studies. The pooled HIV prevalence rate among substance-abusing MSM was 10.0% (95% CI = 0.08–0.13). Substance abusers were more likely to have a higher prevalence of HIV (OR = 1.59) and syphilis (OR = 1.48) infections than non-substance abusers. Substance abusers were also more likely to seek sexual partners through the internet or social media applications (OR = 1.63), engage in unprotected anal intercourse (UAI) (OR = 1.69), group sex (OR = 2.78), and engage in commercial intercourse (OR = 2.04) compared to non-users. Regarding testing behaviors, substance abusers had a higher proportion of HIV or STI testing in their lifetime (OR = 1.70) compared with non-substance abusers (p < 0.05). They were also more likely to have had more sexual partners (≥2; OR = 2.31) and more likely to have consumed alcohol (OR = 1.49) in the past 6 months.
Conclusions: Our study shows the correlation between substance abuse and HIV/Syphilis infection. Eliminating disparities in HIV/Syphilis infection among substance abusing men who have sex with men (MSM) can be achieved if the Chinese government and public health sectors could provide targeted knowledge popularization and diagnosis interventions among high-risk populations.
In China, the HIV/AIDS epidemic is increasing among men who have sex with men (MSM). By the end of 2020, the estimated number of people living with HIV was 2.1 million worldwide, with homosexual transmission accounting for 45.0% of reported HIV/AIDS cases (1). The HIV epidemic has exacted a severe toll on MSM, with HIV infections from 9.1% in 2009 to 23.3% in 2020 (2). In addition, the prevalence of HIV and syphilis co-infection has increased from 8% (Mexico, 2010–2018) to 25% (Turkey, 2013) (3, 4). Previous studies have found that syphilis infections could potentially facilitate HIV transmission and increase the likelihood of acquiring HIV (5). The increasing HIV/AIDS epidemic among MSM is undoubtedly a major public health problem. Therefore, clarifying the risk factors associated with HIV acquisition among Chinese MSM is urgently needed to HIV prevention and intervention strategies.
Similarly, the global rates of substance abuse among men who have sex with men have increased dramatically. Evidence from European countries and China suggests that methamphetamine and ecstasy are the most popular drugs used by MSM in the past years (4–6). A recent study among 3,588 number of participants that explored drug use problems found that the use of nitrite inhalers have overtaken methamphetamine as the most popular substance abused among MSM (7). Chinese MSM has increasingly purchased poppers, and the proportion of poppers used among MSM was 24% in 2020 (8, 9). The recreational use of drugs like rush poppers are more likely to be associated with sex and may thus be linked to the transmission of HIV and other sexually transmitted infections (STI).
On the one hand, drugs like meth/amphetamine, are often used to increase sexual desire and facilitate sexual experimentation (10). Rush popper may reduce pain by dilating capillaries and relaxing anal sphincters, increasing sexual confidence. However, substance abuse has both physiological and psychological effects on users. It may facilitate risky sexual practices, such as unprotected anal intercourse (UAI), thereby potentially increasing the risk of HIV and STI transmission (11–16), substance abuse and UAI are co-occurring risk behaviors that may contribute to the HIV infection rates among MSM.
Over the past years, research studies have explored the association between substance abuse and other risk behaviors that might contribute to HIV infection in the MSM population (6, 15–20). However, the results of these studies have been inconsistent on the significance of this association, previous meta-analyses on substance abuse among MSM or HIV infection failed to provide evidence of underlying differences in HIV-related risk behaviors and associated factors between substance abusers and non-users (21, 22). Still, more evidence is needed. This quantitative review aimed to explore the risk factors associated with higher HIV/Syphilis infection rates among MSM substance abusers compared to the general MSM population. We focused on the sexual risk behaviors between substance abusers and non-users. Furthermore, understanding these issues could further facilitate effective intervention and prevention strategies among Chinese MSM.
This meta-analysis adhered to the PRISMA guidelines. We conducted a comprehensive search of PubMed, Web of Science, Embase, Scopus, Chinese National Knowledge Infrastructure, Chinese Wanfang Data, and VIP Chinese Journal Database for relevant studies with quantitative outcomes associated with HIV/Syphilis infection among men who have sex with men (MSM). And these articles published in English or Chinese between 2010 and May 31, 2022. Meta-analyses were performed to compare HIV and syphilis risks between substance abusers and non-users across studies.
An appropriate combination of keywords and the MeSH subject headings for the search, including (1) “men who have sex with men” OR “MSM” OR “gay man” OR “male homosexual” AND (2) (“HIV infection”) OR “HIV”AND (3) “Club drug use” OR “Recreational drug use” OR “Illicit drug use” OR “Substance abuse.” AND (4) “China.” We also reviewed the bibliographies of included citations to identify references for consideration.
The inclusion criteria were as follows: (1) cross-sectional or longitudinal study design; (2) MSM as a target population; (3) the main outcome focus was HIV prevalence rate or HIV incidence; (4) reported the proportion of substance abuse among MSM in China; (5) were published in English or Chinese and conducted in China; (6) Sample sizes >50; (7) was a master or doctoral thesis which satisfied the above requirements.
Studies were excluded for the following reasons: (1) the study population was not MSM; (2) it exclusively focused on MSM living with HIV or substance abusers; (3) the studies without relevant quantitative data; (4) the study was a systematic review. The most comprehensive studies were included in the meta-analysis.
We imported the literature into Zotero to build a library, eliminated duplicates, and two authors (GH and ZT) screened the titles and abstracts for eligibility. According to the inclusion and exclusion criteria, two authors (CQ and ZT) conducted the full text screening. Discrepancies were discussed until agreement was reached, with an arbitrator (Gengfeng Fu) for unresolved disagreement.
Two authors (GH and ZT) used a standardized form for data extraction, including the following information: source (the primary author, publication year), study periods, sample size, study setting (city, state), recruitment strategy, survey methods, and recall window; types and proportion of substances abused; population characteristics (e.g., sexual risk behaviors including unprotected anal intercourse, the number of male sexual partners, engaging in commercial sex or group sex); the proportion of reporting HIV-positive and syphilis-positive. All abstracted data were used to calculate prevalence rate ratios and relative risk.
We used the Quality Assessment Checklist (QATSO score) (23) for quality assessment. This checklist is a validated quality assessment tool for HIV prevalence/risk behaviors among MSM (the checklist is provided in Supplementary material). The scoring system was based on five items: (1) Whether the sampling method is representative of the population of the study; (2) the measurement of the HIV objective (if the article is focusing only on risk behavior among MSM); (3) Whether response rate is reported in studies; (4) Whether confounding bias is controlled (such as stratification/matching/restriction/adjustment) when analyzing the associations; (5) Whether privacy or the sensitive nature of HIV is considered when conducting the survey. According to these quality items, the scores are 1, 0, and NA, representing “yes,” “no,” and “not applicable,” respectively. All scores were categorized into poor (0%−32%), satisfactory (33%−66%), and good (67%−100%) groups. Quality assessment scores are provided in Supplementary material.
Meta-analysis was performed using R software and was stratified by study design. We used a random -effects model to aggregate every outcome and estimated the pooled association between substance abuse and HIV infection and their 95% CI. Q statistics defined the heterogeneity between studies. Based on the I2 classification suggested by Higgins and Thompson, we used the cut-off of 25, 50, and 75% to define as low, medium, and high levels of heterogeneity, respectively. If significant homogeneity was detected (I2 > 50%), random effect models were employed to calculate the pooled effect rates and OR, otherwise, fixed effects models were employed.
Another subgroup analysis was performed to explore the sources of heterogeneity in these studies, such as sampling size, study periods, and study setting. Egger's regression test and the funnel plot evaluated the possible publication bias and the effect of small sample sizes. Finally, the sensitivity analysis was performed to explore the possible impact of abnormal or outlier data. We used R software (version 4.2.0) to conduct all statistical analyses.
We identified 3,111 unique articles, 3,049 of which did not meet the inclusion criteria, and 62 articles progressed to full-text screening. Eventually, 52 eligible articles (including 61,719 MSM) were selected in this meta-analysis (7–9, 18–20, 24–69). The flow of the review process is shown in Figure 1.
All included papers contained 47 cross-sectional studies and 5 cohort studies. A total of 61,719 MSM was included across the included studies, with a maximum sample size of 6,710, a minimum sample size of 139, and 50 studies with more than 200 participants. The study location involved 24 cities and 11 provinces, and the sampling methods included peer referrals, snowball method, internet recruitment, voluntary counseling test, and venue-based mobilization. Five studies used voluntary counseling test (VCT) method to recruit MSM population, and seven studies used snowball sampling method to recruit participants. Other forty studies used more than one sampling methods to recruit participants. The survey methods were based on self-administrated questionnaires and a face-to-face interview. The characteristics of the studies selected for this review are summarized in Table 1.
Among these selected articles, the pooled proportion of MSM who had ever used substance was 23% (95% CI: 0.17–0.30) (I2 = 99.3%; 95% CI: 0.93–0.94, P < 0.01), and in the past 6 months, a 25% (95% CI: 0.19–0.34) pooled proportion of Chinese MSM reported substance abuse. To examine the possible differences in the proportion of substance abusers, subgroup analyses were conducted by study period, study setting (city), sample size, and recall window (Figure 2).
Subgroup analysis indicated that the proportion of substance abuse varied at different study time intervals (19% from 2010 to 2017; 27% from 2018 to 2022). Whether the studies were conducted in a single city or in more than two cities, the differences in substance abuse rates were not significant (23% vs. 22%). The proportion of substance abuse was higher when the sample size was small: 28% for studies with 1,000 participants or fewer, 20% for 1,000–2,000 participants, and 12% for over 2,000 participants. Moreover, we also analyzed 26 studies conducted in 11 cities with strong comprehensive strength and the substance abuse rate in these cities (Beijing, Tianjin, Nanjing, Guangzhou, Shenzhen, Hangzhou, Xian, Wuhan, Changsha, Qingdao, and Chongqing) was 20% (95% CI: 0.14–0.28) (7, 20, 26, 31, 32, 35, 40, 42, 45–49, 51, 52, 55, 56, 58, 64, 65). Finally, the proportion of substance abuse was different when studies with a recall window of 12 months (17%), 6 months (25%), and 3 months (20%) (Table 2).
Of the 47 cross-sectional studies in the meta-analysis, 12 did not report HIV prevalence rates, and the other 35 used HIV ELISA testing to confirm HIV infection status. So we used data from the 35 studies to compare HIV prevalence rates among substances abusers and non-users (8, 18, 20, 24–27, 29, 31–44, 46–48, 51, 52, 55–57, 64, 66, 68, 69).
Twenty-eight studies contributed findings to aggregate the HIV prevalence of substance abusers and non-users among MSM (10.0% vs. 7.0%), the pooled prevalence rate of HIV among substance abusers was 10.0% (95% CI: 0.08–0.13) (I2 = 88%; 95% CI: 0.88–0.91, P < 0.01). MSM who reported ever using substances were 1.59 times more likely to be HIV positive than non-users [Pooled OR = 1.59 (95% CI: 1.33–1.89); I2 = 59%; P < 0.01] (Table 3).
Subgroup analysis by location showed that the difference in pooled HIV prevalence was not significant (9.0% vs. 7.0%) between single-city and multi-cities; in the study period subgroup, the pooled prevalence rate of HIV among MSM from 2011 to 2018 was estimated to be 11% (95% CI: 0.08–0.13) and 7% (95% CI: 0.05–0. 09) after 2018; Subgroup analysis by sample size showed that the HIV prevalence for studies with sample size < 1,000, sample size of 1,000–2,000, and sample size >2,000 was: 8% (95% CI: 0.06–0.10), 9% (95% CI: 0.06–0.13), and 10.0% (95% CI: 0.08–0. 12), respectively. We also extracted information on syphilis infection status from 16 studies and found that the current prevalence of syphilis was higher among substance abusers than non-users (8.0% vs. 5.7%, pooled OR = 1.48 (95% CI: 1. 20–1.83); I2 = 67%, P < 0.01) (Figure 3).
Forty-four studies compared sexual behaviors between substance abusers and non-users. Twenty studies reported that substance abusing MSM were more likely to find male partners through the internet, including WeChat and Blued (pooled percentages: 77.75% (4,904/6,307) vs. 66.03% (11,211/16,978); pooled OR = 1.63 (95% CI: 1.26–2.12); I2 = 91%; P < 0.01) (8, 18, 20, 24, 26, 28, 29, 34, 38, 47–49, 51, 53–56, 66, 67).
Sixteen studies found statistically significant for unprotected anal intercourse as substance abusers tended to have UAI in the last 6 months [pooled percentages: 46.28% (2,457/5,309) vs. 33.75% (4,497/13,323); pooled OR = 1.69 (95% CI: 1.39–2.09); I2 = 84%; P < 0.01] (8, 18, 20, 26, 28, 30, 34, 38, 47–49, 51, 53, 55, 66, 67). Further, MSM who reported ever using substance were 2.31 times more likely to have multiple sexual partners than non-users [pooled OR = 2.31 (95% CI: 1.87–2.84); I2 = 85%; P < 0.01] (18, 20, 25, 28–31, 47–49, 66, 67). Eleven studies included information on group sex between substance users and non-users. By comparison, MSM who reported ever using substance were 2.78 times more likely to engage in group sex in the past 6 months than non-users [pooled OR = 2.78 (95% CI: 1.47–5.24); I2 = 96%; P < 0.01] (8, 18, 20, 26, 28, 29, 42, 48, 55, 65, 67).
Seventeen studies found that substance abusers were more likely to have engaged in commercial sexual behavior in the past 6 months than non-users [pooled OR = 2.04 (95% CI: 1.28–3.23); I2 = 91%; P < 0.01] (5, 6, 8, 12, 15, 18, 26, 35, 37, 41–43, 47, 51, 65, 66). Also, substance abusers were more likely to report HIV testing in the past 6 months or a history of repeat HIV testing than non-users (pooled OR = 1.70, 95% CI: 1.41–2.06, I2 = 74%; P < 0.01) (8, 24, 27, 28, 30, 34, 39, 48, 51, 56, 66, 67). Five studies focused on alcohol consumption among MSM participants, and substance abusers were more likely to drink alcohol in the past 6 months [pooled OR = 1.49 (95% CI: 1.07–2.10; I2 = 70%; P < 0.01)] than non-users (6, 28, 31, 42, 51). Six studies have provided information about MSM who had sex with the women in the past 6 months [pooled OR = 0.96 (95% CI: 0.71–1.29); I2 = 75%; P < 0.01] (19, 34, 45, 48, 51, 65) (Table 4).
None of the individual study's results affected the pooled estimate odds ratio. ORs remained similar in the sensitivity analysis, which suggested that the results were stable and reliable. Egger's test suggested no significant evidence of publication bias in comparing the prevalence of HIV (P = 0.51) between substance abusers and non-users (Figure 4).
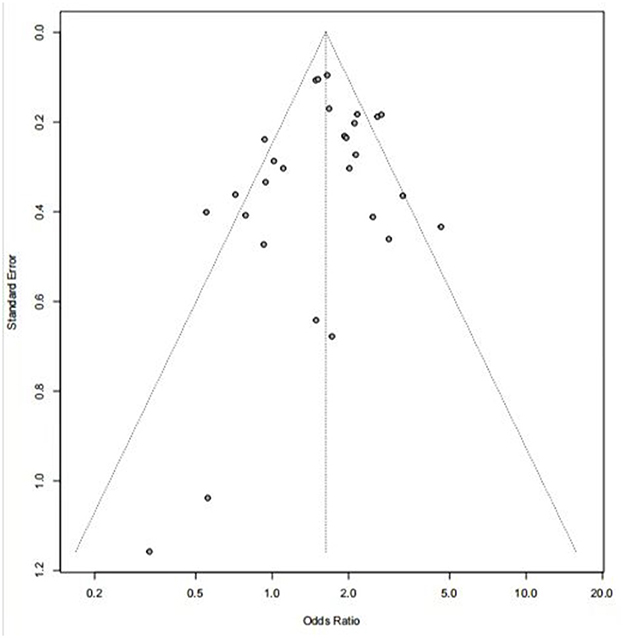
Figure 4. Funnel plot for assessing the publication bias of HIV prevalence between substance abusers and non-users.
We conducted a quantitative review in China to assess the HIV/syphilis epidemic and the correlation between these epidemics and substance abuse and other sexual risk behaviors among MSM in China. This meta-analysis provides insight into HIV transmission among substance abusers. It also provides an important suggestion for China's public health sector to develop more effective prevention and intervention strategies for the MSM population. We integrated and analyzed data from 52 studies and further validated that the prevalence of HIV or syphilis among substance abusers of Chinese MSM is significantly higher than the general MSM population, similar to previous results (17, 22). We aggregated the characteristics, related sexual risk behaviors, and current HIV and syphilis status among Chinese MSM. We also identified the factors associated with HIV/syphilis infection between substance abusing MSM and non-users.
Our review showed a 23% (95% CI: 0.17–0.29) pooled proportion of Chinese MSM reported substance abuse, and in the past 6 months, a 25% (95% CI: 0.19–0.34) pooled proportion of Chinese MSM reported substance abuse. This finding is lower than the proportions reported among Chinese MSM in a global meta-analysis conducted in 2021 (P = 0.306, 95% CI: 0.238–0.373) (17). Furthermore, the pooled HIV prevalence was 10% among substance abusers, much higher than the HIV positivity rate in the general MSM population (P = 0.0507, 95% CI: 5.4%−6.1%) (2). The high HIV prevalence among substance-abusing Chinese MSM is a signal that, without effective intervention strategies, it may contribute to the HIV transmission risks among MSM will would lead to severe public health consequences. Our study results also showed that the substance abuse rate among Chinese MSM gradually increased over time. The proportion of substance-abusing MSM was about 19% (95% CI: 0.13–0.28) before 2018 and reached 27.0% (95%CI: 0.19–0.38) after 2018. One possible explanation for this phenomenon is that the rapid growth of the internet and the popularity of social media applications (such as Blued) have made MSM more susceptible to use substances. In recent years, a number of gay applications like Blued have been developed specifically for MSM social and sexual networking, increased used may facilitate seeking multiple sex partners (70, 71). Some applications targeting MSM have also emerged as important a venue through which MSM seek and maintain relationship with sex partners and substance abuse partners (72). The diversification of e-commerce platforms has provided convenient ways for MSM to obtain substances. It is worth noting that the rush popper and capsule zero were the most popular recreational drug among MSM. Although rush popper is banned or restricted in some countries like Canada and European Union (37), it is still not regulated as an illegal drug, and it can be easily obtained at a low cost online in China. In 2019, Chinese researchers investigated 2,616 MSM in six provinces through an online questionnaire (19). They found that 842 (32.2%) MSM had used at least one psychoactive substance, and 377 (14.4%) MSM reported using more than two psychoactive substances. For the MSM population, the rush poppers is still an important factor contributing to sexual behaviors, such as increasing sexual desire and reducing sexual inhibition (18). MSM were more likely to seek casual sex partners and engage in UAI after using the drug. Moreover, rush poppers are believed to prolong erection which prolongs anal intercourse, thus increasing the likelihood of anal bleeding and the risk of HIV infection (29, 65). It is strongly suggested that the public health sectors should pay attention to the issue of substance abuse, especially the rush poppers, and adopt targeted screening and detection for these subgroups of MSM.
Regarding the sexual risk behaviors among MSM, our study suggests that Chinese substance abusers were more likely to seek sex partners through the internet or gay applications than non-users in the last 6 months. These social media applications greatly facilitate the identification of sexual partners and do not have any restrictions on the time or location (70, 71). In addition, these applications also provide a platform for individuals to organize private parties where the combination of drug use and gay applications may contribute to an increase in the risk of HIV transmission among MSM (24).
Consistent with previous studies, our study suggests that substance abuse is associated with unprotected anal intercourse, commercial sex, and group sex (73–75). Similar results were reported by a United States study which found that substance-abusing MSM were twice more likely to have had commercial sex in the last 6 months than non-users (9). This result was lower than the 5.07 odds found in the study by Robert et al. abroad (76). The high level of sexual activity among substance abusers might make it more difficult to maintain a stable and regular sexual partner relationship. Drug abuse was positively associated with multiple sex partners during a sexual encounter (77, 78), and unprotected sex encounter is more likely to occur during participation in group sex. Moreover, it has been demonstrated that the perianal skin is more susceptible to damage during unprotected anal intercourse and therefore provides optimal conditions for the transmission of HIV.
Alcohol consumption among MSM may also be a cause for concern although only five included papers provided information to compare substance abusers with non-users (6, 45, 51, 62, 73). Substance users were more likely to drink alcohol, and the combination of alcohol and drug use may reduce the sense of restraint and increase the sexual risk behaviors (15, 49, 51).
In our study, pooled HIV testing prevalence was higher among substance abusers than non-users. Substance abusers seem more likely to engage in high-risk sex behaviors (such as group sex, commercial sex, and unprotected anal intercourse) than non-users. Thus, they are more likely to use preventative methods, including frequent HIV and STI testing. The HIV and syphilis prevalence rates were higher among substance abusers than non-users, which suggested that MSM with a history of substance abuse were particularly more likely to develop HIV/syphilis infection. Compromised immunity due to syphilis infection may increase the risk of HIV acquisition and facilitate HIV transmission. Hence, screening and referral efforts for sexually transmissible infections are needed.
This meta-analysis is not without several limitations. First, as the cross-sectional surveys pooled together, it is difficult to infer the temporal sequence between substance abuse and HIV/Syphilis infection. Second, as respondents' drug abuse has not been confirmed by standardized laboratory testing, reporting bias and recall bias could affect the veracity of the results and thus underestimate the HIV prevalence of MSM. Third, some studies included in this meta-analysis used convenient samples or a cross-sectional design. The resulting selection bias may have affected the veracity of our results. Moreover, for a lack of surveys from rural areas, we could not further explore the impact of substance abuse on the infection of HIV/Syphilis among all Chinese MSM.
This study highlights the correlation between substance abuse and HIV/Syphilis infection. Substance abuse among the MSM population can increase the rate of high-risk sexual behaviors and facilitate HIV/Syphilis infection. The mechanism still needs to be explored and strengthened. Targeted knowledge promotion and expanding diagnostics interventions among high at-risk populations should be adopted for HIV/Syphilis prevention. Meanwhile, care providers should pay attention to substance abusers and related high-risk behaviors and encourage safe sex practices. Moreover, intervention programmers should utilize internet-based social organizations to provide peer education and implement social discrimination and HIV-related stigma reduction interventions to help slow the spread of HIV/Syphilis.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
HL, XG, and GF contributed to the manuscript's conception, design, and review. GC and TZ carried out the data collection and drafted the first manuscript. TZ and CS performed the statistical analysis. All authors contributed to the manuscript revision and approved the submitted version.
We want to express our gratitude to all those who helped us while writing this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1082637/full#supplementary-material
MSM, Men who have sex with men; HIV, Human Immunodeficiency Virus; AIDS, Acquired immunodeficiency syndrome; STD, History of sexually transmitted diseases; STI, Sexually transmitted infection; UAI, Unprotected anal intercourse; CAI, Condomless anal intercourse.
1. Chinese Medical Association Infectious Diseases Branch AIDS Hepatitis C Group. Chinese guidelines for diagnosis and treatment of human immunodeficiency virus infection /acquired immunodeficiency syndrome (2021 edition). Med J Peking Union Med Coll Hosp. (2022) 13:203–26. doi: 10.12290/xhyxzz.2022-0097
2. He N. Research progress in the epidemiology of HIV/AIDS in China. CCDCW. (2021) 3:1022–30. doi: 10.46234/ccdcw2021.249
3. Sarigül F, Sayan M, Inan D, Deveci A, Ceran N, Çelen M, et al. Current status of HIV/AIDS-syphilis co-infections: a retrospective multicentre study. Cent Eur J Public Health. (2019) 27:223–8. doi: 10.21101/cejph.a5467
4. Mata-Marín JA, Sandoval-Sánchez JJ, Huerta-García G, Arroyo-Anduiza CI, Alcalá-Martínez E, Mata-Marín LA, et al. Prevalence of antibodies against Treponema pallidum among HIV-positive patients in a tertiary care hospital in Mexico. Int J STD AIDS. (2015) 26:81–5. doi: 10.1177/0956462414530888
5. Zhou L, Yan H, Xu J, Hu H, Chen L, Yang T, et al. HIV incidence and its associated factors among MSM in Nanjing. Chin J Dis Control Prev. (2016) 20:333–336+356. doi: 10.16462/j.cnki.zhjbkz.2016.04.003
6. Ramchand R, Fisher MP, Griffin BA, Becker K, Iguchi MY. Drug use among gay and bisexual men at weekend dance parties: the role of intentions and perceptions of peers' behaviors. AIDS Behav. (2013) 17:1540–9. doi: 10.1007/s10461-012-0382-z
7. Liu G, Cai WD, Chin L, Zhao J, Yang ZR, Tan JG, et al. Study on influential factors and epidemiological characteristics of drug abuse among men who have sex with men. Chin J Dis Control Prev. (2010) 14:1063–5.
8. Duan Q. Study on new-type drugs HIV syphilis infection among men who have sex with men in Shandong province (Master's thesis). Jinan University, Jinan, China (2019). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201902&filename=1019066898.nh&v= (accessed May 29, 2022).
9. Yang X, Ma Y, Zhu X, Ma X. Analysis on status influence factors of synthetic drug abuse among MSM of Luoyang. Chin J AIDS STD. (2017) 23:849–51. doi: 10.13419/j.cnki.aids.2017.09.20
10. Thu Vu NT, Maher L, Zablotska I. Amphetamine-type stimulants and HIV infection among men who have sex with men: implications on HIV research and prevention from a systematic review and meta-analysis. J Int AIDS Soc. (2015) 18:19273. doi: 10.7448/IAS.18.1.19273
11. Xu JJ, Qian H, Chu Z, Zhang J, Hu Q, Jiang Y, et al. Recreational drug use among Chinese men who have sex with men: a risky combination with unprotected sex for acquiring HIV infection. Biomed Res Int. (2014) 2014:1–9. doi: 10.1155/2014/725361
12. Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. JAIDS. (2007) 45:85–92. doi: 10.1097/QAI.0b013e3180417c99
13. Darrow WW. Risky sexual behaviors associated with recreational drug use among men who have sex with men in an international resort area: challenges and opportunities. J Urban Health Bull N Y Acad Med. (2005) 82:601–9. doi: 10.1093/jurban/jti122
14. Lampinen A, Robert S. Hogg unprotected anal intercourse associated with recreational drug use among young men who have sex with men depends on partner type and intercourse role. Sex Transm Dis. (2004) 31:492–8. doi: 10.1097/01.olq.0000135991.21755.18
15. Clatts MC, Goldsamt LA Yi H. Club drug use among young men who have sex with men in NYC: a preliminary epidemiological profile. Subst Use Misuse. (2005) 40:1317–30. doi: 10.1081/JA-200066898
16. Prestage G, Hammoud M, Jin F, Degenhardt L, Bourne A, Maher L. Mental health, drug use and sexual risk behavior among gay and bisexual men. Int J Drug Policy. (2018) 55:169–79. doi: 10.1016/j.drugpo.2018.01.020
17. Liu X, Huo Z, Huang B, Ge F, Chen Y, Luo Z. Meta-analysis of substance abuse among men who have sex with men, China. Modern Prev Med. (2021) 48:3960–6.
18. Mao X, Leuba SI, Hu Q, Yan H, Wang Z, Lu L, et al. Use of multiple recreational drugs is associated with new HIV infections among men who have sex with men in China: a multicenter cross-sectional survey. BMC Public Health. (2021) 21:354. doi: 10.1186/s12889-021-10223-y
19. Li L, Zhou C, Li X, Wang X, Wu Z. Psychoactive substances use in men who have sex with men in China: an internet based survey. Chin J Epidemiol. (2021) 42:690–4. doi: 10.3760/cma.j.cn112338-20200615-00842
20. Wang X, Li Y, Tang Z, Reilly KH, Nong Q, Wu Z. Nitrite inhalant use and HIV infection among Chinese men who have sex with men in 2 large cities in China. J Addict Med. (2017) 11:468–74. doi: 10.1097/ADM.0000000000000347
21. Zhang W, Xu J-J, Zou H, Zhang J, Wang N, Shang H, et al. incidence and associated risk factors in men who have sex with men in Mainland China: an updated systematic review and meta-analysis. Sex Health. (2016) 13:373. doi: 10.1071/SH16001
22. Nong Q, Liang C, Lu L, Guo Z, Lei C, Guo L, et al. Meta-analysis of influencing factors of HIV infection and newly diagnosed HIV infection among men who have sex with men in China. Chin J AIDS STD. (2015) 21:1038–42. doi: 10.13419/j.cnki.aids.2015.12.11
23. Wong WC, Cheung CS, Hart GJ. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol. (2008) 5:23. doi: 10.1186/1742-7622-5-23
24. Zhao P, Tang S, Wang C, Zhang Y, Best J, Tangthanasup TM, et al. Recreational drug use among Chinese MSM and transgender individuals: results from a national online cross-sectional study. PLoS ONE. (2017) 12:e0170024. doi: 10.1371/journal.pone.0170024
25. Chen X, Li X, Zheng J, Zhao J, He J, Zhang G, et al. Club drugs and HIV/STD infection: an exploratory analysis among men who have sex with men in Changsha, China. PLoS ONE. (2015) 10:e0126320. doi: 10.1371/journal.pone.0126320
26. Lu S. A survey of relationship between drug abusing unprotected anal intercourse among men who have sex with men (Master's Thesis). Chinese Center for Disease Control Prevention (2018). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201901&filename=1018309001.nh&v= (accessed April 13, 2022).
27. Cai Y, Song Y, Liu H, Hong F. Factors associated with drug abuse among men who have sex with men in Shenzhen. Chin J AIDS STD. (2016) 22:361–4. doi: 10.13419/j.cnki.aids.2016.05.16
28. Chen M, Cheng W, Xu H, Cai Y, Fan H, Zhong F, et al. Predictors of rush popper use among 825 men who have sex with men in education in Guangdong Province. Chin J Prev Med. (2016) 50:949–53. doi: 10.3760/cma.j.issn.0253-9624.2016.11.006
29. Dai Y, Musumari PM, Chen H, Huang Y, Techasrivichien TS, Pilar S, et al. Recreational drug use, polydrug use and sexual behaviors among men who have sex with men in Southwestern China: a cross-sectional study. Behav Med. (2019) 45:314–22. doi: 10.1080/08964289.2018.1538099
30. Duan C, Wei L, Cai Y, Chen L, Yang Z, Tan W, et al. Recreational drug use and risk of HIV infection among men who have sex with men: a cross-sectional study in Shenzhen, China. Drug Alcohol Depend. (2017) 181:30–6. doi: 10.1016/j.drugalcdep.2017.09.004
31. Han N. Status influencing factors of club drug use among men who have sex with men in Tianjin (Master's thesis). Tianjin Medical University, Tianjin, China (2018). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201901&filename=1018886052.nh&v= (accessed April 13, 2022).
32. He W, Ye X, Tang S, Zhuang J, Liang R. The prevalence of HIV and syphilis and related factors among men who have sex with men in Guangzhou. Chin Prev Med. (2015) 16:684–8. doi: 10.16506/j.1009-6639.2015.09.009
33. Hu Y. Synthetic drug abusers' behavior characteristics associated HIV infection risk: Reflection from one coastal city in China (Doctoral thesis). Chinese Center for Disease Control Prevention (2014). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CDFD&dbname=CDFDLAST2015&filename=1015525955.nh&v= (accessed May 31, 2022).
34. Huang P, Duan Q, Liao M, Wang G, Zhu X, Yang X, et al. Analysis of rush poppers use and related factors in men who have sex with men in Jinan and Qingdao, 2016. Chin J Prev Med. (2020) 54:861–6. doi: 10.3760/cma.j.cn112150-20190815-00659
35. Jia H, Zhang M, Chang W. Status and influencing factors of club drug use among men who have sex with men in Xi'an. Modern Prev Med. (2017) 44:332–5.
36. Jiang H. Research on the HIV infection status risk factors of communication of men who have sex with men using the club drugs in Chongqing (Master's thesis). Chongqing Medical University, Chongqing, China (2017). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201801&filename=1017844523.nh&v= (accessed May 16, 2022).
37. Li D, Yang X, Zhang Z, Qi X, Ruan Y, Jia Y, et al. Nitrite inhalants use and HIV infection among men who have sex with men in China. Biomed Res Int. (2014) 2014:1–9. doi: 10.1155/2014/365261
38. Li J, Li X, Ren Q, Liao M. Trends and related factors of new-type drug abuse among men who have sex with men in Jinan from 2017 to 2020. Modern Prev Med. (2022) 49:1086–90.
39. Li M. Study on the related factors of HIV infection drug use in men who have sex with men in Harbin (Master's thesis). Yantai University, Yantai, China (2018). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201901&filename=1018849574.nh&v= (accessed May 11, 2022).
40. Liu L, Zhang M, Zhu Z, Wu S. Analysis on HIV prevalence and related risk factors among men who have sex with men in Nanjing. Jiangsu J Prev Med. (2015) 26:33–5. doi: 10.13668/j.issn.1006-9070.2015.02.013
41. Shan D, Wu D, Liu L, Liu H, Yin W, Yu M, et al. Survey on high-risk behaviors and HIV infection among men having sex with men who use drugs in Tianjin in 2016. Chin J Prev Med. (2017) 51:718–22. doi: 10.3760/cma.j.issn.0253-9624.2017.08.011
42. Shi H, Li S, Wang T, Cao Y, Li J, Yan H. Drug abuse and its influencing factors among young men who have sex with men in Wuhan, China. Chin J Public Health. (2016) 32:329–32. doi: 10.11847/zgggws2016-32-03-20
43. Wang L, Huang P, Liao M, Zhu X, Zhang N, Huang T, et al. Status and influencing factors of HIV self-testing among men who have sex with men who use synthetic drugs in Shandong Province. Chinese Preventive Medicine (2022) 2022:1–7.
44. Wang Y. The situation of sexual features HIV influence factors among college students men who have sex with men (Master's thesis). Kunming Medical University, Kunming, China (2016). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201701&filename=1016295932.nh&v= (accessed May 29, 2022).
45. Wang Z, Li D, Joseph TF, Lau, Yang X, Shen H, Cao W. Prevalence and associated factors of inhaled nitrites use among men who have sex with men in Beijing, China. Drug Alcohol Depend. (2015) 149:93–9. doi: 10.1016/j.drugalcdep.2015.01.021
46. Xi S. Study on AIDS prevention knowledge, behavioral characteristic, HIV infection its influencing factors among men who have sex with men in Hangzhou City (Master's thesis). Zhejiang University, Hangzhou, China (2011). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2012&filename=1011187299.nh&v= (accessed June 6, 2022).
47. Xu Y, Zhu Z, Li X, Yan HJ, Zhang M. Rush poppers use and risks of HIV and syphilis infections among MSM in Nanjing : mediation through unprotect anal intercourse. Chin J AIDS STD. (2017) 23:726–729+751. doi: 10.13419/j.cnki.aids.2017.08.14
48. Xu Y, Zhu Z, Wu S, Liu L, Guo L, Lin L. Status and associated factors of recreational drug use among man who have sex with man in Nanjing. Chin J Dis Control Prev. (2019) 23:1476–81. doi: 10.16462/j.cnki.zhjbkz.2019.12.009
49. Yan Y, Tan Z, Li J, Chen X, Cheng W, Yang Y, Jiang H. Prevalence and associated factors of rush poppers use among men who have sex with men in Guangzhou. Modern Prev Med. (2020) 47:2597–601.
50. Yang G, Zhang A, Yu Y, Liu H, Long F, Yan J. Drug use and its associated factors among money boys in Hunan Province, China. Public Health. (2016) 140:213–20. doi: 10.1016/j.puhe.2016.06.005
51. Yu Z, Huang H, Zhang H, Liu Y, Cui Z, Li C, et al. Recreational new drug use and influencing factors among young men who have sex with men in Tianjin. Chin J School Health. (2021) 42:1504–7. doi: 10.16835/j.cnki.1000-9817.2021.10.014
52. Zhang C, Qian H, Yin L, Liu Y, Shiela M, Ruan Y, et al. Vermund sexual behaviors linked to drug and alcohol use among men who have sex with men in China. Subst Use Misuse. (2016) 51:1821–30. doi: 10.1080/10826084.2016.1197264
53. Zhang D. HIV-related behaviors related factors of male students who have sex with men in three cities (Master's thesis). Anhui medical University, Anhui, China (2019). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201902&filename=1019175167.nh&v= (accessed May 29, 2022).
54. Zhang Z, Zhang L, Zhou F, Li Z, Yang J. Knowledge, attitude, and status of nitrite inhalant use among men who have sex with men in Tianjin, China. BMC Public Health. (2017) 17:690. doi: 10.1186/s12889-017-4696-7
55. Zhou F, Li Z, He S, Gao Y, Yang J. Comparison of awareness of nitrite inhalant and characteristics of demographic and sexual behavioral factors among men who have sex with men in Tianjin, China. Capital J Public Health. (2020) 14:174–7. doi: 10.16760/j.cnki.sdggws.2020.04.002
56. Zhu Z, Zhang M, Xu Y, Xu W, Liu L, Wu S, et al. Cross-sectional surveys on the use of recreational drug nitrous-acid-ester rush-popper in men who have sex with men, Nanjing. Chinese J Epidemiol. (2017) 38:189–93. doi: 10.3760/cma.j.issn.0254-6450.2017.02.011
57. Zhou X, Xia H, Zhu P, Zhou J, Ma P. Analysis of club drug abuse and HIV infection among men who have sex with men in Nantong City. Chin J Dermatovenereol. (2020) 34:1283–8. doi: 10.13735/j.cjdv.1001-7089.202001068
58. Li H. A study on unprotected anal intercourse associated factors among men who have sex with men in Tianjin (Master's thesis). Tianjin Medical University, Tianjin, China (2019). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD202001&filename=1019696497.nh&v= (accessed June 8, 2022).
59. Ni Z. A prospective cohort about incidence of HIV among men who have sex men (Master's thesis). Ningbo University, Ningbo, China (2020).
60. Shan D, Ning Z, Ning Z, Zheng H, Huang D, Yu M, et al. A cohort study on the incidence of HIV infection in drug users among men who have sex with men in Shanghai and Tianjin. Chinese J Epidemiol. (2021) 42:2149–55. doi: 10.3760/cma.j.cn112338-20210715-00551
61. Chu Z, Shang H. Prospective cohort study on the relationship between club drugs and HIV infection among men who have sex with men (MSM) in Shenyang (Master's thesis). China Medical University, Shenyang, China (2013).
62. Peng E, Xu J. The HIV incidence and risk facts among student men who have sex with men : a cohort study (Master's thesis). China medical University, Shenyang, China (2019).
63. Guo X, Cui W, Zhu F, Liu S, Li Y, Chen T, et al. Association between the characteristics of sexual partners and substance use before sexual behavior in young male students who have sex with men. Chin J School Health. (2020) 41:1791–4. doi: 10.16835/j.cnki.1000-9817.2020.12.007
64. Li D, Sun Z, Zhang Y, Wang L, Zhang L, Zhang H, et al. Prevalence and related factors among men who have sex with men in Beijing. Chin Prev Med. (2016) 17:321–6. doi: 10.16506/j.1009-6639.2016.05.001
65. Li Y, He X, Zhang L, Chen Y. Drug abuse among HIV negative men who have sex with men in Chongqing. Chin J Infect Control. (2020) 19:126–30. doi: 10.12138/j.issn.1671-9638.20205838
66. Wang Z, Lu Y, Meng MX, Jia T, Luo Z, Chen W, et al. Study on synthetic drug use and associated factors among men who have sex with men at high risk of HIV infection. Chin J Epidemiol. (2020) 2020:231–5. doi: 10.3760/cma.j.issn.0254-6450.2020.02.017
67. Chen J, Huang Y, Chen H, Xia J. Nitrite inhalants use, sexual behaviors and HIV/syphilis infection among men who have sex with men in Chongqing, China. Infect Dis Poverty. (2020) 9:127. doi: 10.1186/s40249-020-00748-6
68. He L, Pan X, Wang N, Yang J, Jiang J, Luo Y, et al. New types of drug use and risks of drug use among men who have sex with men: a cross-sectional study in Hangzhou, China. BMC Infect Dis. (2018) 18:182. doi: 10.1186/s12879-018-3091-z
69. Lan G, Chen Y, Tang S, Shen Z, Tang Z, Ruan Y, et al. syphilis and behavioral risk factors among men who have sex with men in a drug-using area of southwestern China: Results of 3 cross-sectional surveys from 2013 to 2015. Medicine. (2018) 97:e0404. doi: 10.1097/MD.0000000000010404
70. Holloway IW. Substance use homophily among geosocial networking application using gay, bisexual, and other men who have sex with men. Arch Sex Behav. (2015) 44:1799–811. doi: 10.1007/s10508-015-0581-6
71. Bien CH, Best JM, Muessig KE, Wei C, Han L, Tucker JD. Gay apps for seeking sex partners in China: implications for MSM sexual health. AIDS Behav. (2015) 19:941–6. doi: 10.1007/s10461-014-0994-6
72. Landovitz RJ, Tseng C-H, Weissman M, Haymer M, Mendenhall B, Rogers K, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health. (2013) 90:729–39. doi: 10.1007/s11524-012-9766-7
73. Zhang Y, Bao R, Leuba SI, Li J, Wang H, Zhang J, et al. Association of nitrite inhalants use and unprotected anal intercourse and HIV/syphilis infection among MSM in China: a systematic review and meta-analysis. BMC Public Health. (2020) 20:1378. doi: 10.1186/s12889-020-09405-x
74. Daskalopoulou M, Rodger A, Phillips AN, Sherr L, Speakman A, Collins S, et al. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: results from the cross-sectional ASTRA study. Lancet HIV. (2014) 1:e22–31. doi: 10.1016/S2352-3018(14)70001-3
75. Garofalo R, Mustanski BS, McKirnan DJ, Herrick A, Donenberg GR. Methamphetamine and young men who have sex with men: understanding patterns and correlates of use and the association with HIV-related sexual risk. Arch Pediatr Adolesc Med. (2007) 161:591–6. doi: 10.1001/archpedi.161.6.591
76. Israelstam S, Lambert S, Oki G. Poppers, a new recreational drug craze. Can Psychiatr Assoc J. (1978) 23:493–5. doi: 10.1177/070674377802300711
77. Marcus U, Nostlinger C, Rosinska M, Sherriff N, Gios L, Dias SF, et al. Behavioural and demographic correlates of undiagnosed HIV infection in a MSM sample recruited in 13 European cities. BMC Infectious Diseases. (2018) 18:1–15. doi: 10.1186/s12879-018-3249-8
Keywords: HIV, syphilis, substance abuse, men who have sex with men (MSM), correlation
Citation: Zhao T, Chen G, Sun C, Gong X, Li H and Fu G (2023) The epidemic of HIV and syphilis and the correlation with substance abuse among men who have sex with men in China: A systematic review and meta-analysis. Front. Public Health 11:1082637. doi: 10.3389/fpubh.2023.1082637
Received: 28 October 2022; Accepted: 30 January 2023;
Published: 17 February 2023.
Edited by:
Man-Qing Liu, Wuhan Centre for Disease Prevention and Control, ChinaReviewed by:
Rezvan Hosseinzadeh, Babol University of Medical Sciences, IranCopyright © 2023 Zhao, Chen, Sun, Gong, Li and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiyong Li,  bGh5ODAwMTI1QDEyNi5jb20=; Gengfeng Fu,
bGh5ODAwMTI1QDEyNi5jb20=; Gengfeng Fu,  ZnVnZkBqc2NkYy5jbg==
ZnVnZkBqc2NkYy5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.