- 1Shazand School of Nursing, Arak University of Medical Sciences, Arak, Iran
- 2Nursing Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
- 3Biostatistical Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
- 4Faculty of Nursing and Health Sciences, Nord University, Bodø, Norway
- 5Faculty of Science and Health, Charles Sturt University, Orange, NSW, Australia
Background and objectives: The population of older people is increasing across the world. Older people need care and support from their families to be able to live independently. This study aimed to design and evaluate the psychometric properties of the family support for older people (FSOP) questionnaire.
Methods: In this instrument development study using a mixed-methods design, the psychometric properties of the FSOP questionnaire in terms of validity and reliability were evaluated.
Results: The FSOP questionnaire consisted of 50 items in six domains. It was shown to have appropriate qualitative and quantitative validities (score > 1.5). The indicators of content validity (CVR > 0.62, ICVI ≥ 0.80, and SCVI > 0.94) and confirmatory factor analysis (indexes of χ2/df = 2.50, CFI = 0.96, GFI = 0.97, AGFI = 0.96, NNFI = 0.96, PNFI = 0.89, TLI = 0.96, and RMSEA = 0.06) were satisfactory. Cronbach's alpha coefficient for reliability was 0.94, indicating an optimal score.
Conclusions: Healthcare providers and family caregivers are suggested to use the FSOP questionnaire for improving the quality of life of older people at home.
1. Introduction
It has been predicted that the number of older adults with low to high dependency levels will increase by almost a third by 2035 (1). Addressing the unmet care and support needs of the aging population and designing services and solutions centered around what older people need or want has become an urgent public health priority (2). However, the present gap in the workforce for the provision of care for patients suffering from long-term diseases requires initiatives emphasizing community-based care and partnership with family caregivers (3). When a society experiences demographic changes in terms of increases in the aging population, more people need to become volunteers and/or take on caregiving roles (4). Therefore, collaborative relationships and interaction between healthcare providers and family members can help smooth transitions of care to older people's own homes, leading to more patient-centered care (5).
Family caregivers are in the best position to support patients at home and coordinate healthcare services for them (6–8). The family has been recognized as the main support system for older people and plays an essential role in their health and wellbeing (9). Special attention to older people by family members is rooted in Asian cultural values, given that the family has always been considered the first line of support for older people (10, 11). The family is also considered responsible for fulfilling older adults' expectations and meeting their physical, mental, and emotional needs (12–15).
Family support can prevent hospitalization or the need to go into a nursing home (16). Older people usually prefer to live in their own home rather than in long-term healthcare settings (17, 18). It has been shown that older people who live in a familial environment and enjoy family support are healthier than those living in a nursing home or living alone (19, 20) and are more satisfied with their own life (21, 22). They often have better perceived health and self-esteem (23), leading to more successful aging (24–26).
The phenomenon of aging is experienced differently depending on country of residence, culture, economic condition, age group, and physical activity level. Accordingly, the phenomenon of support is defined and understood differently in different cultures and contexts (27, 28). In addition, family caregivers often face dilemmas in performing their caring responsibilities due to unclear boundaries and guidelines regarding support for older people in home care (29). The knowledge and skills of family caregivers for the provision of support in home care is improved through experience (30, 31). However, caregivers need education and support to reduce their own stress due to the knowledge gap regarding their roles, responsibilities, and accurately defining the dimensions of family support for older people in home care.
The development of a questionnaire with the consideration of norms and values that are appropriate to the cultural, religious, and social conditions of different societies is required for the development of strategies that can enhance family involvement in home care. It can also suggest a pattern for family caregiver roles in the provision of support in home care and be used for developing competencies to better fulfill their responsibilities. Given the lack of such an instrument in international literature, this study was conducted to design and evaluate the psychometric properties of the family support for older people (FSOP) questionnaire.
2. Materials and methods
2.1. Design
An instrument development study was conducted using a mixed-methods design consisting of qualitative and quantitative research approaches. The review of international literature and directional qualitative content analysis led to the definition of the research phenomenon (32). From this, perceived family support for older people in home care and the questionnaire's items were identified (13). Briefly, qualitative research was carried out to explore the perceived family support for older people from the perspectives of older people and their family members in the Iranian family context. The collected data was analyzed using the primary matrix developed based on existing international literature. Six main themes were used, upon which the items of the FSOP questionnaire were developed. The psychometric properties of the FSOP questionnaire in terms of validity and reliability have been reported in this article.
2.2. Psychometric properties of the FSOP questionnaire
The research was conducted from November 2020 until August 2021. The dimensions of the FSOP questionnaire and the related design matrix were as follows: instrumental (IN), financial (FI), affective (AF), therapeutic (TH), technological (TE), and social (SO). These dimensions defined the phenomenon of support for older people by family caregivers, helped with setting goals to measure perceived family support by older people, depicted the data analysis map, and developed a blueprint for producing items and scoring rules (33).
2.2.1. Participants and sampling
The spread of the COVID-19 pandemic throughout the country led to the long-term closure of healthcare institutions, as well as rehabilitation and daycare centers for older people. Also, home quarantine was implemented, especially for the vulnerable groups of older people. Therefore, the imposed restrictions limited direct contact with older people for data collection.
For the recruitment of older participants, the family members of older people who participated in the qualitative research (13) from 30 cities across Iran were contacted via email using a convenience sampling method. Moreover, they were requested to nominate other families from their acquaintances using the snowball sampling method.
Recruitment was performed based on these inclusion criteria: older people aged ≥65 years; willingness to take part in this research; having no cognitive impairment; living at home; receiving support from family members.
An electronic version of the FSOP questionnaire was developed by the researchers. Distributing the electronic version of the questionnaire had the benefit of reaching older people with a greater geographical variation. Choosing the appropriate layout and font, displaying each question on a separate page, simplifying the questionnaire's items, and allocating enough time to provide answers were all considered in order to facilitate data collection from the participants.
The family members were asked to hand the FSOP questionnaire to older participants and request them to fill it out. The researcher could be contacted via email or telephone to answer probable questions and remove ambiguities during the data collection.
The sample size was estimated based on the number of items in the questionnaire. Between 2 and 10 participants for each item was recognized as sufficient (34). To avoid bias due to missing and/or incomplete data collection and to be assured of the adequacy of the sample size for confirmatory factor analysis (CFA), the highest accessible sample was recruited, which was 4.5 participants for each item. Therefore, the sample size was 235 older people.
2.2.2. Face validity
To examine the qualitative face validity of the FSOP questionnaire, the principal investigator (SSH) conducted individual interviews with 10 older people to identify their perspectives on the understandability and simplicity of the questionnaire's items (33). These participants were approached by their family members via email and invited to take part in individual face-to-face interviews at times and places convenient to them. The interviews were mostly held in the older people's own homes or city parks. The participants' feedback and suggestions were included in the final version. For quantitative face validity, a five-point Likert scale was used to assess the questionnaire's items, from “strongly important” (score 5) to “not at all important” (score 1). The impact scores for each item were calculated and values over 1.5 were considered appropriate (33, 35).
2.2.3. Content validity
Using the qualitative content validity method, ten experts in the fields of gerontology, family nursing, and questionnaire development were invited to review and give comments on the writing and presentation style of the FSOP questionnaire (36). The revised questionnaire was sent back to the expert panel for final approval. For quantitative content validity, the same expert panel was requested to assess the questionnaire upon which the content validity ratio (CVR), the item content validity index (ICVI), and Scale content validity index (SCVI) were calculated. According to the Lawche table, a CVR score above 0.62 indicates satisfactory content validity for the questionnaire (37). The ICVI determines relevance, simplicity, and clarity of items using a four-point Likert scale, and an ICVI score ≥ 0.80 is considered appropriate. A score greater than 0.90 for SCVI is considered appropriate (33, 35). The four-point Likert scale used to assess the ICVI was as follows: the sentence is complicated; the sentence needs rectification; the sentence is simple, but it needs rectification; the sentence is simple and clear.
2.2.4. Item analysis
The preliminary evaluation of a questionnaire in its target population before its widespread use for data collection is item analysis. Item analysis is usually performed before evaluating the validity of a questionnaire's structure with a small sample of participants. Therefore, 30 older people were selected using the convenience sampling method and requested to complete the FSOP questionnaire (38). Each item in the questionnaire was evaluated for mean, standard deviation, correlation with other items, and the internal consistency of the whole questionnaire. The loop method was used for item analysis by which the reliability coefficient of the entire questionnaire was evaluated. If reliability increased with the omission of each item, the item had an effective role in coordination with other items, so it was entered into other stages of psychometric evaluation (33). The basis for deleting the item was whether the correlation of the item with the total item score was negative or <0.3.
2.2.5. Construct validity
The structural validity of a questionnaire is assessed using factor analysis. It examines the relationship between items and identifies those items that are most related to each other and can form a single domain. In this research, CFA was performed, given that the aim of construct validity was to explore the relationships between the questionnaire's items based on predetermined factors or domains. Therefore, the questionnaire's items were assigned to factors based on theoretical expectations. The model fit statistics were used to assess the compatibility of collected data using the specified factor model (37), and confirm the goodness of the model fit (39).
Since the questionnaire used a Likert scale and the data distribution was far from normal, the robust version of the weighted least squares method was used, as the weighted least squares with robust standard errors and a mean- and variance-adjusted test statistic and other related methods were suitable for sequential scale data. The minimum acceptable factor loading was considered 0.3 (40). For evaluating the fit of the CFA, goodness of fit indicators were used along with the ideal score. Indices used in this study and their acceptable values to confirm the goodness fit of the model were as follows: x2/df ratio < 2, residual mean square error approximate (RMSEA) < 0.06; goodness of fit (GFI) > 0.90; and comparative goodness of fit index (GFI) > 0.90 (41, 42).
2.2.6. Reliability
Internal consistency and stability were used for assessing reliability. Internal consistency was assessed using the calculation of Cronbach's alpha coefficient and composite reliability (CR). For stability, the intraclass correlation coefficient (ICC) was calculated via the test–retest reliability method. The closer the ICC was to one, the higher reliability level of the FSOP questionnaire. Test-retest reliability was evaluated through filling out the questionnaire twice within a 2-week interval by 30 older people (38). The values of Cronbach's alpha, ICC, and CR ≥0.70 were considered acceptable (41, 42).
2.2.7. Responsiveness
The questionnaire should be sensitive to changes and be responsive. For this purpose, a hypothesis testing was performed to examine the total score of the FSOP questionnaire in relation to the participants' age using the independent t-test.
2.2.8. Absolute stability
Absolute stability was assessed through the calculation of the minimum significant changes (MIC) of the questionnaire. For calculating MIC, the standard deviation of the base line score was multiplied by the mean effect size of 0.50 which was 17.18. The minimum detectable change (MDC) was also calculated using 1/96*SEM. Also, the percentage of MDC was calculated using . The MIC should be larger than the MDC.
2.2.9. Ceiling and floor effect
One of the criteria for interpretability is the desired ceiling and floor effects (35). The total score of the FSOP questionnaire was set between numbers from one to 100. Accordingly, the percentage of participants who scored either zero or 100 was determined. Also, the ceiling and floor effects were calculated separately for each domain. This index should be <20% (34), though there is no agreement among researchers, and some believe that it should be more than 15% (43).
2.2.10. Feasibility
In order to evaluate the ease of the questionnaire, the average time to complete the questionnaire and the percentage of people who did not answer each item were calculated. The development of a lengthy questionnaire was avoided during item analysis and in the narrative stage.
2.3. Data analysis
Descriptive statistics were used for the description of the sociodemographic characteristics of older people. Inferential statistics were used to assess the psychometric properties of the FSOP questionnaire. All statistical tests were performed with a significance level of 0.05. The statistical software used for data analysis was SPSS 25 (IBM, Armonk, NY) and the Rosseel et al. package 2012 under R software (44, 45).
2.4. Ethical considerations
Ethics approval was granted by the ethics committee of Tarbiat Modares University (decree code: IR.MODARES.REC.1398.140). The participants and their family members were informed of the research aim being to assess the psychometric properties of the FSOP rather than to collect data about the current condition of family support for older people. The older people signed the informed consent form and sent it back to the main researcher via email. The designed questionnaire was distributed among participants who remained anonymous. Measures to ensure the confidentiality of the collected data were the restriction of access to the collected data, the anonymous sharing of data with research team members during data analysis, and saving the data on a password-protected computer.
3. Results
3.1. Demographic characteristics of the participants
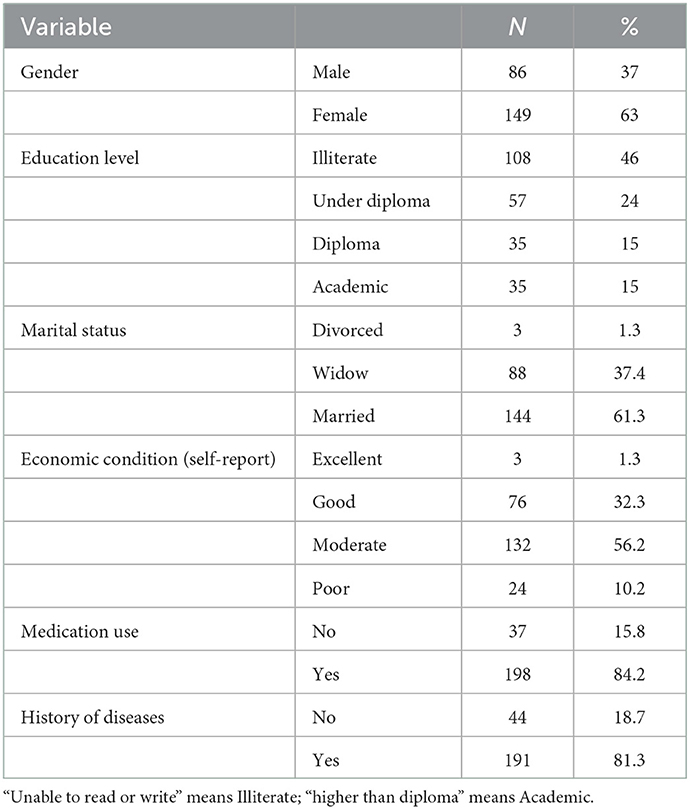
In the present study, 149 women (63.7%) and 86 men (36.3%) participated. Of these, 143 participants (61.3%) lived with their families and 92 (38.7%) lived alone at home but received support from families. Table 1 presents the demographic characteristics of the participants.
3.2. Psychometric properties of the FSOP questionnaire
3.2.1. Face validity
The item pool consisted of 62 items. During the qualitative face validity, six items were revised due to the perspective of the participants in terms of clarity. Also, the impact score of the items was reported as >1.5.
3.2.2. Content validity
The CVR was reported as 0.94. Also, ICVI and SCVI were reported ≥ 0.80 and > 0.94, respectively. The CVI score of item 7 was 0.4. The item, stating “Without my children and other family members' help, it is not possible for me to clean the house,” had a CVR = 0.2 and overlapped with other items. Therefore, it was deleted. Items 10, 14, 15, and 52 had borderline CVR scores in comparison to the numerical value of the Lawche table. However, considering that they had acceptable CVI scores, they were kept in the questionnaire. Item 51 (“My children and other family members teach me how to use a bank card”), item 47 (“My children and other family members accompany me when using my bank card”), item 52 (“My children and other family members patiently repeat to me how to work with electrical devices and technological tools such as mobile phones, bank cards, computers, and the internet”), and item 53 (“My children and other family members explain to me the use of internet”) were all merged into item 58 (“My children and other family members help me patiently to use tools such as a mobile, computer, and the internet”).
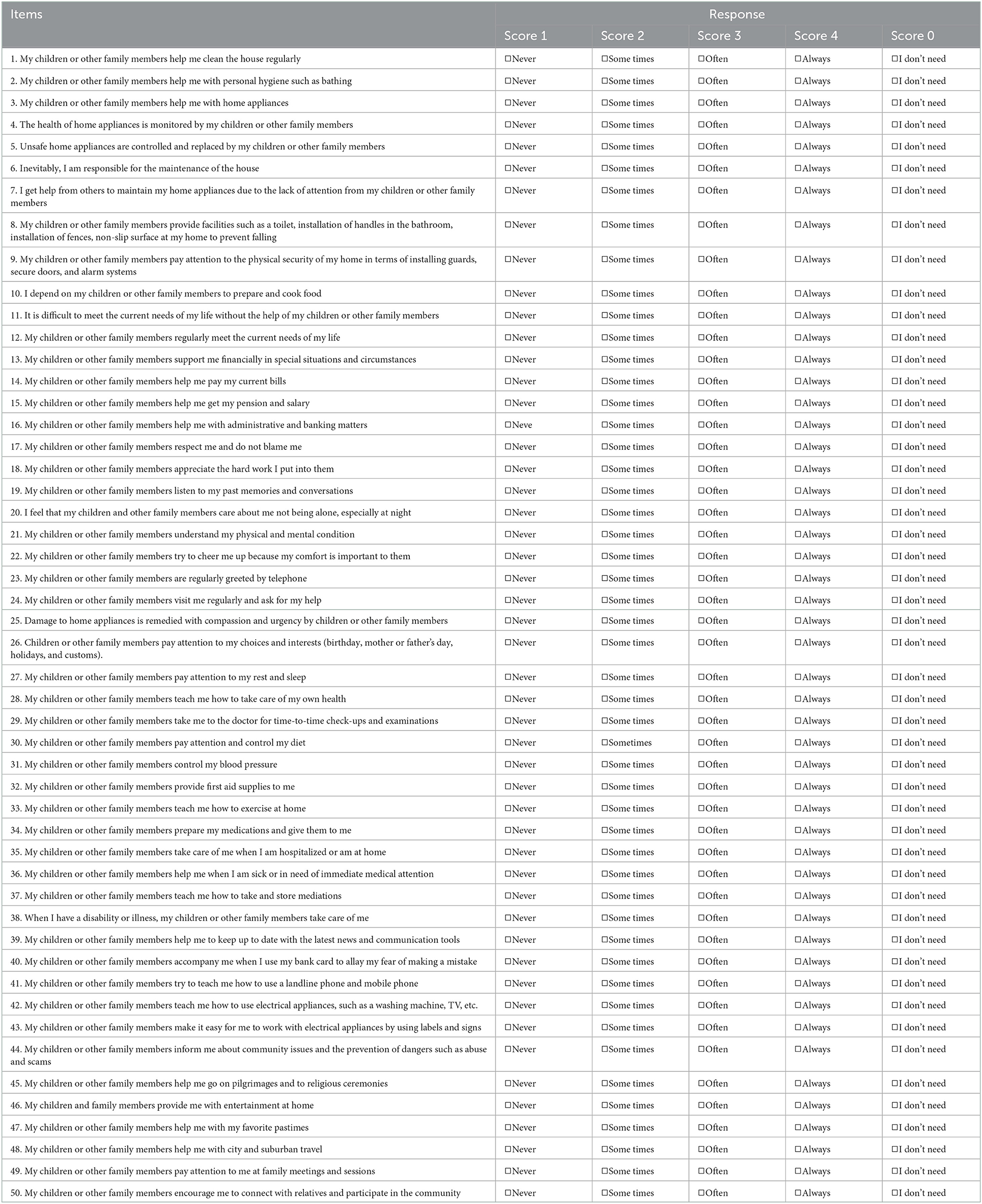
The clarity and adequacy of the items were approved by the expert panel. Required corrections were made during qualitative and quantitative content validities. A 58-item questionnaire with a Likert scale of “always,” “often,” “sometimes,” “never,” and “rarely” was developed.
The questionnaire was first distributed to older people via a pilot study and the response process to the items was evaluated by the research team. This led to some modifications in the response scale. Some older people reported that they did not need support at some time periods. Therefore, the option of “I do not need support” was added to the Likert scale corresponding to the score of zero. The options of “rarely” and “sometimes” were found to be indistinguishable, so to remove this ambiguity the “rarely” option was deleted. Finally, the FSOP questionnaire as a 58-item questionnaire with the Likert scale of “always,” “often,” “sometimes,” “never,” and “I do not need” was developed.
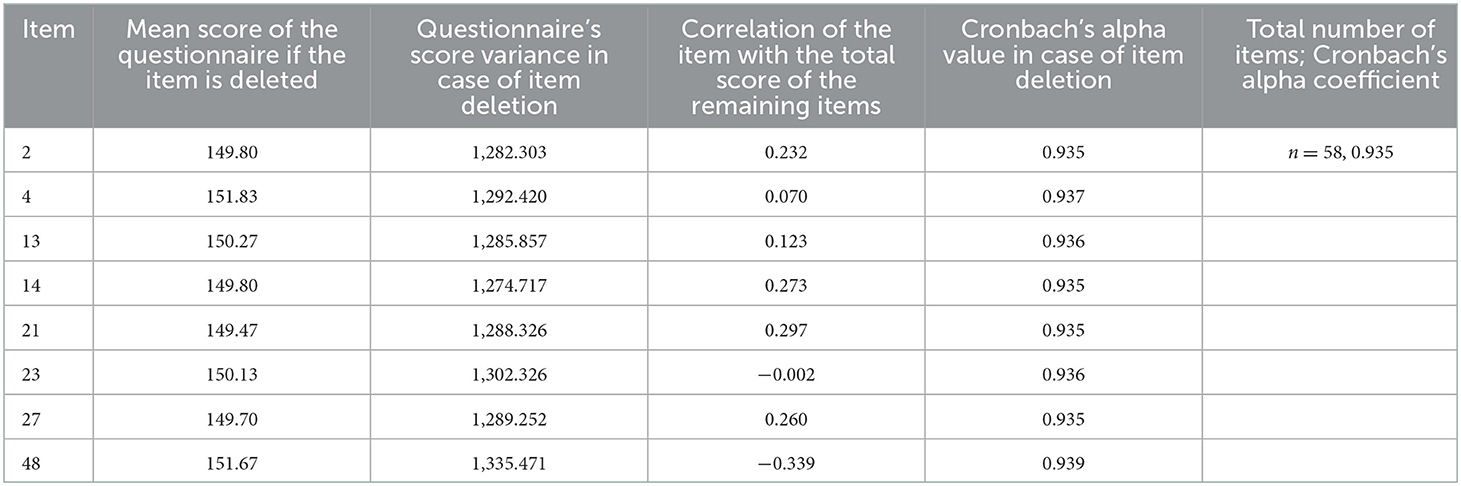
3.2.3. Item analysis
The research team evaluated the items based on the results of item analysis and made decisions regarding the need to maintain necessary items and improve the structure of the whole questionnaire. Accordingly, eight items were deleted. The coefficient after the deletion of items was 0.935 (Table 2). Therefore, the 50-item questionnaire was entered into CFA (Table 3).
3.2.4. Construct validity
The appropriateness of CFA was confirmed using goodness-of-fit indicators (Figure 1). These indicators, along with the ideal score, showed in general that all items had significant roles in the validity of the FSOP questionnaire. In particular, the important indicators of goodness of fit (CFI, TLI, RMSEA, ) for all models were within their acceptable ranges (Figures 2–7). The items were assigned to the following six domains: instrumental (IN), consisting of 12 items; financial (FI), 4 items; affective (AF), 10 items; therapeutic (TH), 12 items; technological (TE), 6 items; social (SO), 6 items.

Figure 1. All indexes of , CFI = 0.96, GFI = 0.97, AGFI = 0.96, NNFI = 0.96, PNFI = 0.89, TLI = 0.96 and RMSEA = 0.06 were measured and accepted in all domains. There were at least three observable variables for each latent variable and each observed variable measured only one latent variable of the agent.
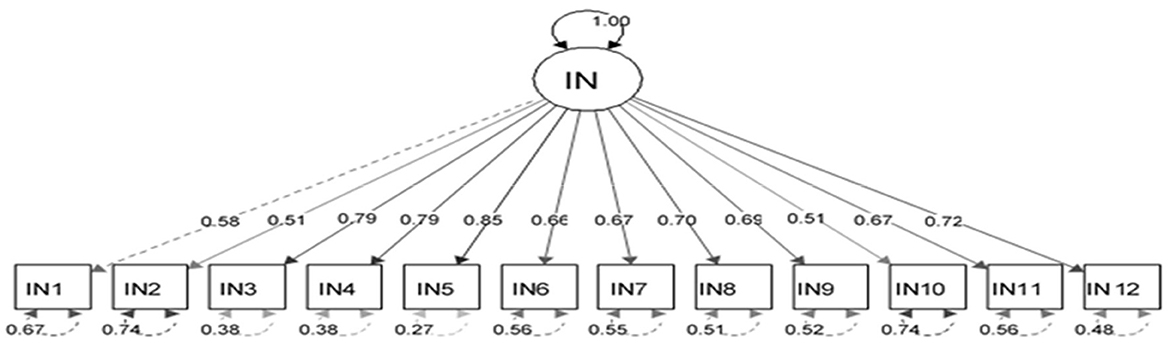
Figure 2. Confirmatory factor analysis model of the instrumental dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.
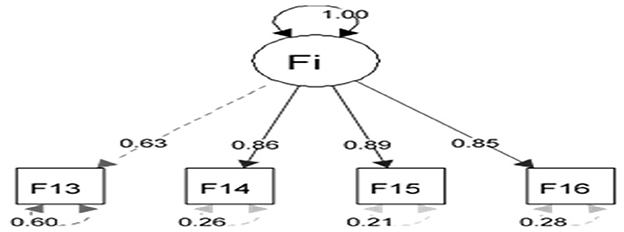
Figure 3. Confirmatory factor analysis model of the financial dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.
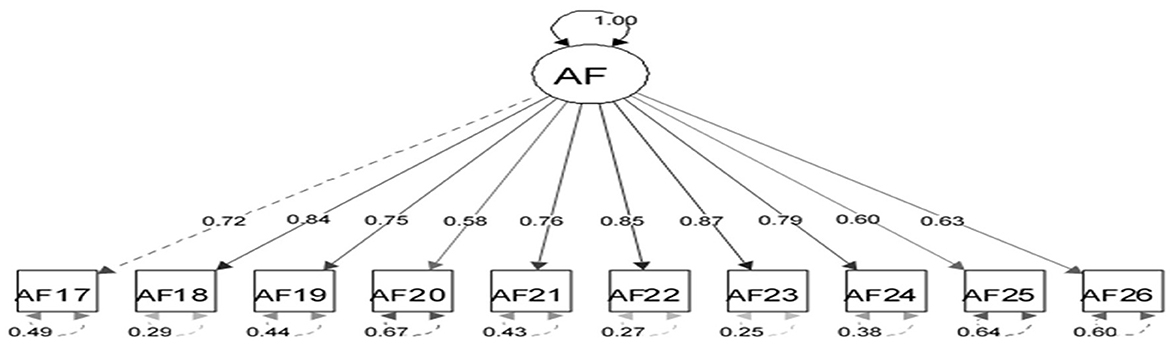
Figure 4. Confirmatory factor analysis model of the affective dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.
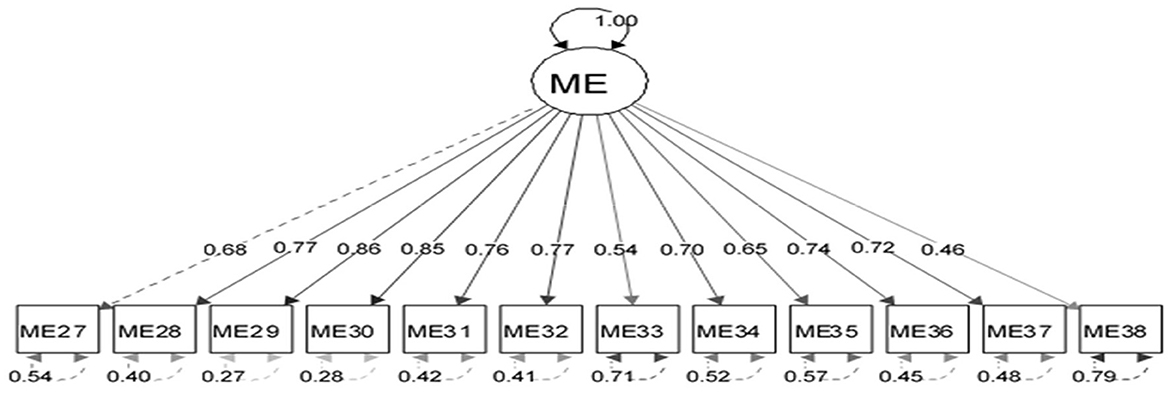
Figure 5. Confirmatory factor analysis model of the therapeutic dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.

Figure 6. Confirmatory factor analysis model of the questionnaire on the technology dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.
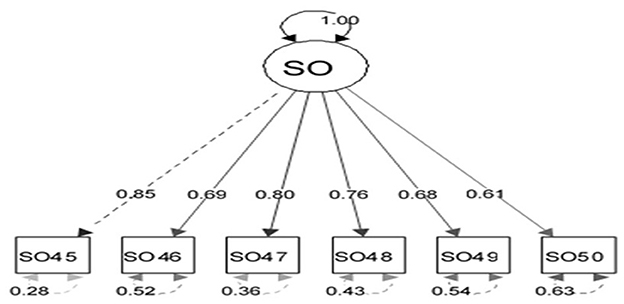
Figure 7. Confirmatory factor analysis model of the social dimension of the family support for older people questionnaire. All items in the questionnaire showed a factor load >0.3, indicating appropriate metrics for the tool factor.
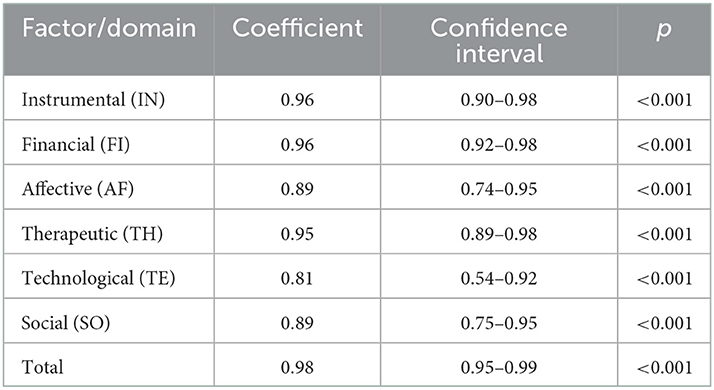
3.2.5. Reliability
Cronbach's alpha coefficient for the whole questionnaire was 0.94. The coefficients for the domains were as follows: IN = 0.87, FI = 0.82, AF = 0.86, TH = 0.87, TH = 0.76, and SO = 0.79. With regard to stability, ICC scores, with a 95% confidence interval for the whole questionnaire and for each domain, were reported in Table 4.
3.2.6. Responsiveness
The results of the independent t-test (Table 5) showed a statistically significant difference between the participants' age and the mean score of the whole questionnaire (p = 0.032). Therefore, the results indicated the appropriate sensitivity of the FSOP questionnaire.
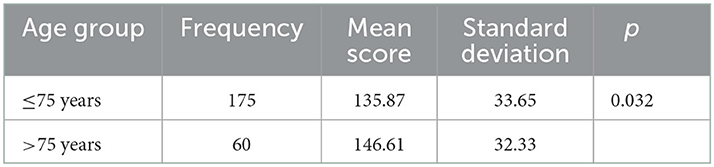
Table 5. Examination of the total score of the FSOP questionnaire in relation to the participants' age.
3.2.7. Absolute stability
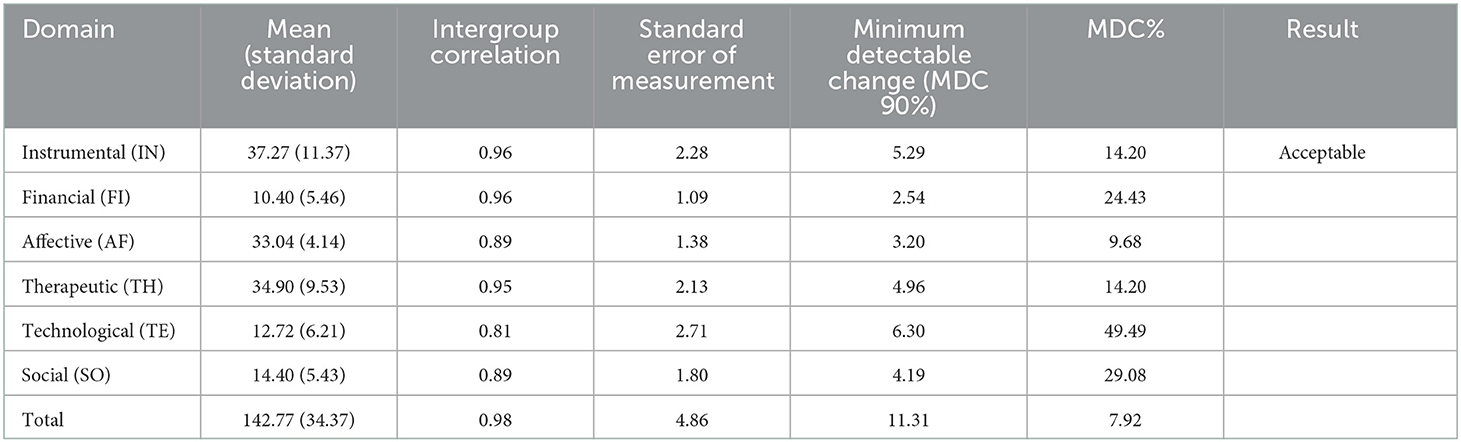
The percentages of MDC in all domains except TH was close to or <30%, which were acceptable. Also, the MDC percentage of the whole questionnaire was 7.92 (Table 6).
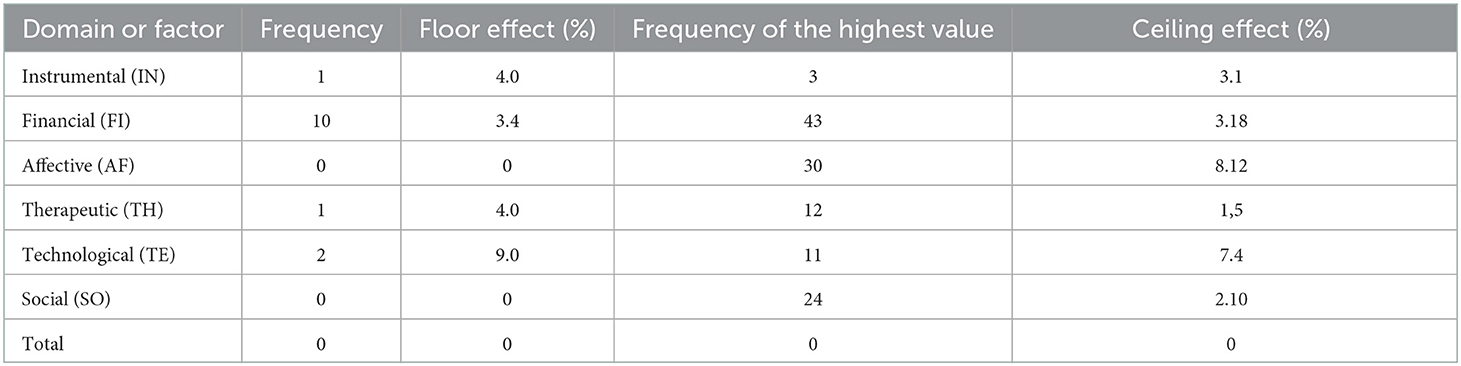
3.2.8. Ceiling and floor effect
The values for all domains reported were under 20%, indicating no ceiling and floor effects (Table 7). It showed the appropriate interpretability of the FSOP questionnaire, and the ability of the questionnaire to express true variability.
3.2.9. Feasibility
The approximate duration of completing the questionnaire was between 15 and 20 mins. Also, the option “I don't need support” provided more choice to the participants and reduced the number of unanswered items.
3.2.10. Scoring
The FSOP questionnaire had a five-point Likert scale. For the scoring of positive items, a score of 1 was given to the option “never,” 2 to “sometimes,” 3 to “often,” and 4 to “always.” For negative items, scoring was in reverse so that a score of 1 was given to the option “always,” 2 to “often,” 3 to “sometimes,” and 4 to “never.” Items 6, 7, and 11 had reverse scoring. In both positive and inverse cases, a score of 0 was given to the option “I do not need support.”
The score for each domain was determined through calculating the scores of related items of the domain. The total score of the FSOP questionnaire was determined through the summation of the scores for each domain according to a formula. The total score of the questionnaire varied from 50 to 200 and the level of family support was interpreted according to the qualitative quarters.
The following formula is based on the total raw score of each person divided by the minimum score that the same person achieved. For example, if for ten items the participant selected the option of “I do not need support,” he/she answered 40 questions with a minimum of 40 and a maximum of 160. If the total score of the tool was 100, this should be divided by 40 (the participant's minimum score), which achieves a score of 2.5, indicating a poor qualitative range of family support for the participant. If the participant selected “I do not need support” for eight items, their score ranged from 42 to 168. If he/she achieved a score of 110, divided by 42, the calculated score was 2.61, indicating the desired or good family support. According to qualitative quarters, a score of 1–1.75 denotes adverse family support, 1.76–2.5 is poor family support, 2.26–3.25 is favorable or good family support, and 3.26–4 is excellent family support. To facilitate the use of this questionnaire, the calculation of questionnaire scores can be easily performed using Excel.
4. Discussion
The research process led to the development and evaluation of the FSOP questionnaire consisting of 50 items divided into the following six domains: instrumental (IN), financial (FI), affective (AF), therapeutic (TH), technological (TE), and social (SO). First, 72 items were extracted from the data matrix. The scrutiny of the items by the research team led to the deletion of 13 items, and the 59 remaining items underwent evaluation for their psychometric properties, during which a further 3 items were added and 4 items were deleted. Therefore, 58 items underwent CFA, leading to the deletion of 8 items and 50 items remaining in the final questionnaire.
The process of evaluating the psychometric properties of this questionnaire complied with the Cosmin checklist as a consensus-based standard on the properties of instruments for the measurement of health statuses (35). The main characteristics and differences between the FSOP questionnaire and other similar instruments are discussed as follows.
In comparison to the FSOP questionnaire, the questionnaire by Wang et al. (46) on family support is focused on daily life, emotional support, and decision making using a Likert scale from never to always. Although friends and families were the main sources of support, instrumental support was exclusive to families in the Wang et al. questionnaire. In addition, the three important areas of family support only had three general questions.
The psychometric properties of the FSOP questionnaire were evaluated using valid scientific methods. Nevertheless, its adaptation to other cultures requires further investigations. In our study, frequent greetings were a type of emotional support. Xu et al. (47) assessed family support in terms of structural, instrumental, financial, and emotional support. Accordingly, structural family support was considered as whether participants lived with any of their children. Instrumental support was assessed by the question “Can your children accompany you to see a doctor?” the question for assessing child support was “Have you received financial support from your child in the last 12 months?,” and the emotional domain was weighed using the question “In general, do you think your children are respectful?” (47). No psychometric assessment was performed to ensure of the validity and reliability of these support domains. Xu et al. (47) also acknowledged that the evaluation of any kind of support with only one question was a limitation of their research.
Zimmer and Kwong's (48) instrument highlighted instrumental and financial support from children and other sources. Instrumental support was assessed through receiving assistance from a list of potential resources such as family members in four instrumental tasks, including food preparation, washing clothes, doing household chores, and shopping. Financial support was mentioned as any financial aid that added to older people's income. Respondents were asked if their children had sponsored them in the past year (48). In the comparison of this questionnaire with the FSOP questionnaire, commonalities in two domains and their content can be observed. However, the whole structure of the instrumental domain cannot be sufficiently evaluated through asking only one question. Also, construct validity of the FSOP questionnaire was investigated through CFA. The fit evaluation of the extracted model showed an acceptable fit with the dimensions of family support. In addition to evaluating the overall fit of the model, the model was fitted separately for each domain and an acceptable fit between the domains and the items was observed.
Komjakraphan et al. (28) developed a scale based on the results of exploratory factor analysis with three domains of: attention to daily life, financial and material assistance, and emotional and reassuring resources. These domains accounted for 57.03% of the total variance of family support for older people (28). Instrumental and financial constructs were two independent and important constructs that were merged after factor analysis, and the structure of accompaniment and companionship created the third domain (28).
Uddin and Bhuiyan (27) and Tselebis et al. (36) developed family support scales for older people, but they did not conduct factor analysis as the most important aspect of evaluating psychometric properties. The factor analysis process of the FSOP questionnaire showed that some items had more factor burden and were therefore more important in assessing the validity of the related domains. For instance, older people's concerns regarding continuing their independent life were highlighted. In general, older people prefer to stay at home as much as possible (22). The reduction of sensory, motor, and cognitive functions among older people often impairs their ability to perform activities of daily living and disturbs their peace of mind at home. Therefore, the safety and accessibility of household items should be assessed periodically (49). This could confirm the statement that a questionnaire should be developed based on the mental experiences of individuals that are rooted in their cultural constructions (50).
In the factor analysis of the technology domain of the FSOP questionnaire, the item regarding educating older people to use electrical appliances gained the most factor load. Older people face many obstacles using technology for performing daily life activities (51). They have to use various electronic appliances, indicating the impact of technology on their quality of life and their need for educational support from families (52). It has been shown that 98.8% of older people watch television in their spare time (53–55).
During factor analysis of the social structure of the FSOP questionnaire, the support of family members to assist going on pilgrimage trips and attending religious ceremonies was factor-loaded. Older people consider preparation for traveling as the duty of their children and prefer being accompanied by their children on such journeys (13, 50). In Muslim societies, a common spare time activity for older people is to go to the mosque to partake in religious rituals (55, 56). It can bring peace of mind and increase social interactions. Rahimi et al. (57) stated that older people were not supported by their families in leisure and recreational activities. The family support tool questionnaire developed in the Thai cultural context was shown to have an acceptable reliability and stability level. According to the Cronbach's alpha coefficients for reliability assessment, moderate to favorable correlations between subclasses were reported. Therefore, it was assumed that concepts measured by subscales were not completely distinct (28), which was converse to the FSOP questionnaire.
According to the Cosmin checklist, responsiveness and interpretability should be considered during the evaluation of a questionnaires' psychometric properties. Criteria for interpretability include the number of unanswered items, least significant change, distribution of total scores, and assessment of the ceiling and floor effects (35). Responsiveness, standard error, interpretability, ceiling and floor effects, and ease of the FSOP questionnaire were within acceptable ranges. Other similar questionnaires in international literature have not reported on these psychometric criteria (27, 28, 36).
Reliability assessment is an important part of the questionnaire's psychometrics evaluation. Most tool developers often assess internal correlation and stability of the questionnaire. Standard error calculation of the questionnaire has been neglected as an important component of reliability assessment in most questionnaires (58, 59).
4.1. Strengths and limitations
A strength of the FSOP questionnaire is the use of a mixed-methods design consisting of qualitative and quantitative methods for its development. Furthermore, there were no missing data, given that the principal researcher checked the participants' answers before entering data into the data analysis process. In addition, the psychometric properties of the FSOP questionnaire were evaluated based on various scientific criteria mentioned in the Cosmin checklist (35). The items of the FSOP are easy for older people to read and understand. In comparison to other questionnaires, the wide range of dimensions included in the FSOP questionnaire, such as instrumental, financial, affective, therapeutic, technological, and social, make it suitable for use in other cultures and contexts. However, further research should be conducted for the adaptation of this instrument to the culture of use. A limitation of this study was the probable inability of older people in understanding the instrument's content and items given the lack of presence of the main researcher during the data collection. However, the participants knew that they could reach the researcher via email or telephone and seek answers to their questions. Also, the feedback and suggestions by the older participants and the expert panel were included in the final version of the FSOP questionnaire to ensure the simplicity and understandability of its items.
5. Conclusion
The FSOP questionnaire covers various aspects of family support for older people in instrumental, affective, financial, therapeutic, social, and technology domains. It has successfully passed all stages of evaluation of psychometric properties and also goodness of fit for all six domains of family support. The FSOP questionnaire can be completed by both self-report and interview. This questionnaire has short and understandable items that suit older people's memory and cognitive conditions. The dimensions and items of the FSOP questionnaire can be used as a guide for developing educational programs to meet the educational needs of family caregivers with regard to support for older people in home care. It is suggested that healthcare providers and family caregivers use it for improving the quality of life of older people in their own homes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Tarbiat Modares University, Tehran, Iran. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SS, FA, AK, and MV: study design, conceptualization, data collection, data analysis, interpretation, and manuscript writing. FA, AK, and MV: study supervision. All authors contributed to the article and approved the submitted version.
Funding
The authors disclose the receipt of support from Tarbiat Modares University, Tehran, Iran to conduct this research (Decree code: IR.MODARES.REC.1398.140).
Acknowledgments
This study was one part of the PhD dissertation by SS. The authors would like to thank all participants who helped with the evaluation of the psychometric properties of the FSOP questionnaire.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kingston A, Comas-Herrera A, Jagger C. Forecasting the care needs of the older population in England over the next 20 years: estimates from the Population Ageing and Care Simulation (PACSim) modelling study. Lancet Public Health. (2018) 3:e447–55. doi: 10.1016/S2468-2667(18)30118-X
2. Vlachantoni A. Unmet need for social care among older people. Ageing Society. (2019) 39:657–84. doi: 10.1017/S0144686X17001118
3. Shalev D, Docherty M, Spaeth-Rublee B, Khauli N, Cheung S, Levenson J, et al. Bridging the behavioral health gap in serious illness care: challenges and strategies for workforce development. Am J Geriatr Psychiatry. (2020) 28:448–62. doi: 10.1016/j.jagp.2019.09.003
4. Jika BM, Khan HTA, Lawal M. Exploring experiences of family caregivers for older adults with chronic illness: a scoping review. Geriatr Nurs. (2021) 42:1525–32. doi: 10.1016/j.gerinurse.2021.10.010
5. Gregory A, Mackintosh S, Kumar S, Grech C. Experiences of health care for older people who need support to live at home: a systematic review of the qualitative literature. Geriatr Nurs. (2017) 38:315–24. doi: 10.1016/j.gerinurse.2016.12.001
6. Godfrey M, Townsend J. Older people in transition from illness to health: trajectories of recovery. Qual Health Res. (2008) 18:939–51. doi: 10.1177/1049732308318038
7. Bunn F, Burn A-M, Robinson L, Poole M, Rait G, Brayne C, et al. Healthcare organisation and delivery for people with dementia and comorbidity: a qualitative study exploring the views of patients, carers and professionals. BMJ Open. (2017) 7:e013067. doi: 10.1136/bmjopen-2016-013067
8. Baxter K, Glendinning C. Making choices about support services: disabled adults' and older people's use of information. Health Soc Care Commun. (2011) 19:272–9. doi: 10.1111/j.1365-2524.2010.00979.x
9. Sigalingging G, Sitopu SD. Measuring family support in the elderly's independence in performing activities of daily living (a case study in Medan Tuntungan District, Medan City, Indonesia). J Nurs Health Sci. (2017) 6:1–5. doi: 10.9790/1959-0603060105
10. Feng Q, Straughan PT. What does successful aging mean? Lay perception of successful aging among elderly Singaporeans. J Gerontol Ser B Psychol Sci Social Sci. (2017) 72:204–13. doi: 10.1093/geronb/gbw151
11. Shamsikhani S, Ahmadi F, Kazemnejad A, Vaismoradi M. Meaning of respect for older people in family relationships. Geriatrics. (2022) 7:57. doi: 10.3390/geriatrics7030057
12. Cheng S-T, Lee CK, Chan AC, Leung EM, Lee J-J. Social network types and subjective well-being in Chinese older adults. J Gerontol Ser B Psychol Sci Social Sci. (2009) 64:713–22. doi: 10.1093/geronb/gbp075
13. Shamsikhani S, Ahmadi F, Kazemnejad A, Vaismoradi M. Typology of family support in home care for iranian older people: a qualitative study. Int J Environ Res Public Health. (2021) 18:6361. doi: 10.3390/ijerph18126361
14. Deng J, Hu J, Wu W, Dong B, Wu H. Subjective well-being, social support, and age-related functioning among the very old in China. Int J Geriatr Psychiatry. (2010) 25:697–703. doi: 10.1002/gps.2410
15. Rejeh N, Heravi-Karimooi M, Vaismoradi M. Iranian nursing students' perspectives regarding caring for elderly patients. Nurs Health Sci. (2011) 13:118–25. doi: 10.1111/j.1442-2018.2011.00588.x
16. Elers P, Hunter I, Whiddett D, Lockhart C, Guesgen H, Singh A. User requirements for technology to assist aging in place: qualitative study of older people and their informal support networks. JMIR Mhealth Uhealth. (2018) 6:e10741. doi: 10.2196/10741
17. Boldy D, Grenade L, Lewin G, Karol E, Burton E. Older people's decisions regarding ‘ageing in place': a Western Australian case study. Australas J Ageing. (2011) 30:136–42. doi: 10.1111/j.1741-6612.2010.00469.x
18. Zamanzadeh V, Pakpour V, Salimi S, Rahmani A, Mohammadi E, Shikhnejad L. Dissatisfaction: Iranian older people's experiences from living in aged care home. Iran J Nurs. (2018) 31:56–66. doi: 10.29252/ijn.31.112.56
19. Nazari S, Farhadi A, Sadegh Moghadam L, Namazi shabestari A. Perceived affective support From the Iranian older adult's viewpoint: a directed content analysis. J Gerontol. (2017) 2:51–64. doi: 10.29252/joge.2.1.51
20. Hosseini zare SM, Movahed E, Pourreza A, Rahimi Foroshani A. The effect of social support on the health of the elderly in Tehran. Hospital. (2015) 13:115–21.
21. Beyaztas FY, Kurt G, Bolayir E. Life satisfaction level of elderly people: a field study in Sivas, Turkey. JPMA. (2012) 62:221.
22. Karimi T, Nouhi E, Iranmanesh S. Comparing Life satisfaction of elderly between nursing home residents and seniors living in their own homes in Isfahan. J Geriatr Nurs. (2014) 1:43–54.
23. Shin S, Sok S. A comparison of the factors influencing life satisfaction between Korean older people living with family and living alone. Int Nurs Rev. (2012) 59:252–8. doi: 10.1111/j.1466-7657.2011.00946.x
24. Hsu H-C. Exploring elderly people's perspectives on successful ageing in Taiwan. Ageing Soc. (2007) 27:87–102. doi: 10.1017/S0144686X06005137
25. Kim SH, Park S, Park KS. Correlates of successful aging in South Korean older adults: a meta-analytic review. Asia Pac J Public Health. (2017) 29:544–59. doi: 10.1177/1010539517717021
26. Han SY, Ko Y. A structural equation model of successful aging in Korean older women: using selection-optimization-compensation (SOC) strategies. J Women Aging. (2021) 33:84–99. doi: 10.1080/08952841.2019.1681883
27. Uddin MA, Bhuiyan AJ. Development of the family support scale (FSS) for elderly people. MOJ Gerontol Geriatrics. (2019) 4:17–20. doi: 10.15406/mojgg.2019.04.00170
28. Komjakraphan P, Isalamalai S-a, Boonyasopun U, Schneider JK. Development of the Thai family support scale for elderly parents (TFSS-EP). Pac Rim Int J Nurs Res. (2009) 13:118–32.
29. Sunde OS, Vatne S, Ytrehus S. Professionals' understanding of their responsibilities in the collaboration with family caregivers of older persons with mental health problems in Norway. Health Soc Care Commun. (2022) 30:1325–33. doi: 10.1111/hsc.13456
30. Lawson S, Mullan J, Wong G, Zaman H, Booth A, Watson A, et al. Family carers' experiences of managing older relative's medications: insights from the MEMORABLE study. Patient Educ Couns. (2022) 105:2573–80. doi: 10.1016/j.pec.2021.12.017
31. Gehr TJ, Freiberger E, Sieber CC, Engel SA. A typology of caregiving spouses of geriatric patients without dementia: caring, worried, desperate. BMC Geriatr. (2021) 21:483. doi: 10.1186/s12877-021-02425-1
32. Jones EG, Kay M. Instrumentation in cross-cultural research. Nurs Res. (1992) 41:186–8. doi: 10.1097/00006199-199205000-00012
33. Waltz CF, Strickland OL, Lenz ER. Measurement in Nursing and Health Research. Fifth ed. Berlin: Springer Publishing Company (2017).
34. Munro BH. Statistical Methods for Health Care Research. Fifth ed. Philadelphia: Lippincott Williams & Wilkins (2005).
35. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. (2010) 19:539–49. doi: 10.1007/s11136-010-9606-8
36. Tselebis A, Anagnostopoulou T, Bratis D, Moulou A, Maria A, Sikaras C, et al. The 13 item Family Support Scale: reliability and validity of the Greek translation in a sample of Greek health care professionals. Asia Pac Fam Med. (2011) 10:3. doi: 10.1186/1447-056x-10-3
37. Lawshe CH. A quantitative approach to content validity. Pers Psychol. (1975) 28:563–75. doi: 10.1111/j.1744-6570.1975.tb01393.x
38. Bujang MA, Omar ED, Baharum NA. A review on sample size determination for cronbach's alpha test: a simple guide for researchers. Malays J Med Sci. (2018) 25:85–99. doi: 10.21315/mjms2018.25.6.9
39. Altikriti S, Anderson CN. Factor analysis and structural equation modeling. In:Barnes JC, Forde DR, editors. The Encyclopedia of Research Methods in Criminology and Criminal Justice. London (2021). p. 833–8. doi: 10.1002/9781119111931.ch159
40. Knapp TR, Brown JK. Ten measurement commandments that often should be broken. Res Nurs Health. (1995) 18:465–9. doi: 10.1002/nur.4770180511
41. Polit DF, Yang F. Measurement and the Measurement of Change: A Primer for the Health Professions. First ed. Philadelphia, PA: Wolters Kluwer (2016).
42. Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis: Pearson New International Edition. Seventh ed. Philadelphia, PA: Pearson Education (2013).
43. Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
44. Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
45. The R Core Team. A Language and Environment for Statistical Computing: R Foundation for Statistical Computing. (2021). Available online at: https://mran.microsoft.com/snapshot/2020-12-31/doc/manuals/r-release/fullrefman.pdf?msclkid=295cc152b19c11ecb8e2860c9c82ca04 (accessed April 01, 2022).
46. Wang L, Yang L, Di X, Dai X. Family support, multidimensional health, and living satisfaction among the elderly: a case from Shaanxi Province, China. Int J Environ Res Public Health. (2020) 17:8434. doi: 10.3390/ijerph17228434
47. Xu L, Li Y, Min J, Chi I. Worry about not having a caregiver and depressive symptoms among widowed older adults in China: the role of family support. Aging Ment Health. (2017) 21:879–88. doi: 10.1080/13607863.2016.1181708
48. Zimmer Z, Kwong J. Family size and support of older adults in urban and rural China: current effects and future implications. Demography. (2003) 40:23–44. doi: 10.1353/dem.2003.0010
49. Fielo SB, Warren SA. Home adaptation: Helping older people age in place. Geriatric Nursing. (2001) 22:239–46. doi: 10.1067/mgn.2001.119473
50. Nazari S, Farokhnezhad Afshar P, Sadeghmoghadam L, Namazi Shabestari A, Farhadi A. Developing the perceived social support scale for older adults: a mixed-method study. AIMS Public Health. (2020) 7:66–80. doi: 10.3934/publichealth.2020007
51. Yazdani-Darki M, Rahemi Z, Adib-Hajbaghery M, Izadi F. Older adults' barriers to use technology in daily life: a qualitative study. Nurs Midwif Stud. (2020) 9:229–36. doi: 10.4103/nms.nms_91_19
52. Roupa Z, Nikas M, Gerasimou E, Zafeiri V, Giasyrani L, Kazitori E, et al. The use of technology by the elderly. Health Sci J. (2010) 4:118.
53. Gautam R, Saito T, Kai I. Leisure and religious activity participation and mental health: gender analysis of older adults in Nepal. BMC Public Health. (2007) 7:299. doi: 10.1186/1471-2458-7-299
54. Strain LA, Grabusic CC, Searle MS, Dunn NJ. Continuing and ceasing leisure activities in later life: a longitudinal study. Gerontologist. (2002) 42:217–23. doi: 10.1093/geront/42.2.217
55. Hosseini Zare SM, Tajvar M, Abdi K, Esfahani P, Geravand B, Pourreza A. Leisure time activities and mental health among tehran older people in 2018. Iran J Ageing. (2020) 15:369–79.
56. Madah SB. The status of social and leisure time activities in the elderly residing in Iran and Sweden. Salmand Iran J Ageing. (2008) 3:597–606.
57. Rahimi A, Anoosheh M, Ahmadi F, Foroughan M. Tehranian elderly people's experiences about leisure time activities and recreations. Salmand Iran J Ageing. (2010) 5:61–77.
58. Ebadi A, Taghizadeh Z, Montazeri A, Shahvari Z, Tavousi M, Bagherzadeh R. Translation, development and psychometric properties of health related measures-Part 2: construct validity, reliability and responsiveness. Payesh. (2017) 16:1–11.
Keywords: family support, home care, factor analysis, older people, psychometric properties
Citation: Shamsikhani S, Ahmadi F, Kazemnejad A and Vaismoradi M (2023) Design and psychometric properties of the family support for older people questionnaire. Front. Public Health 11:1068839. doi: 10.3389/fpubh.2023.1068839
Received: 13 October 2022; Accepted: 04 January 2023;
Published: 02 February 2023.
Edited by:
Tino Prell, University Hospital in Halle, GermanyReviewed by:
Ezequiel Pinto, University of Algarve, PortugalKatalin Papp, University of Debrecen, Hungary
Copyright © 2023 Shamsikhani, Ahmadi, Kazemnejad and Vaismoradi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fazlollah Ahmadi,  YWhtYWRpZiYjeDAwMDQwO21vZGFyZXMuYWMuaXI=
YWhtYWRpZiYjeDAwMDQwO21vZGFyZXMuYWMuaXI=
 Soheila Shamsikhani
Soheila Shamsikhani Fazlollah Ahmadi
Fazlollah Ahmadi Anoshirvan Kazemnejad
Anoshirvan Kazemnejad Mojtaba Vaismoradi
Mojtaba Vaismoradi