- 1Department of Health Education and Health Promotion, National Taiwan Normal University, Taipei, Taiwan
- 2Continuing Education Master's Program of Addiction Prevention and Treatment, National Taiwan Normal University, Taipei, Taiwan
- 3Department of Nursing, Mackay Medical College, New Taipei City, Taiwan
Background: Improper or insufficient treatment of mental health illness harms individuals, families, and society. When psychiatric treatment shifts from a hospital-based to a community-based health care system, risk management is essential to the provision of effective care.
Objective: We examine whether an upgrade in home visit frequency of psychiatric patients as identified by public health nurses can predict the subsequent need for emergency escort services for medical treatment.
Design: A 2-year retrospective medical record review.
Setting(s): A district of New Taipei City in Taiwan.
Participants: A total of 425 patients with a diagnosed mental health illness cared for through home visits by public health nurses from January 2018 to December 2019.
Methods: We accessed the Ministry of Health and Welfare's psychiatric care management information system to identify a set of medical records, and analyzed these records using chi-square and regression analyses.
Results: The analyses indicated that the groups experiencing the greatest need for emergency escort services were: male, 35–49 years old, with a senior high school level of education, without a disability identification card, with a schizophrenia diagnosis, and had been reported by the nurse as having progressed to a serious level. Nurses' increased frequency of home visits (an indicator that the patient's overall condition was worsening) and nurses' reports of increased severity of problems were significant predictors of the need for emergency escort services.
Conclusions: The nurses' adjustment of visit frequency based on the results of the visit assessment predicts the need for emergency escort services for mental patients. The findings support not only the professional roles and functions of public health nurses, but also the importance of strengthening psychiatric health community support services.
Background
Mental and addictive disorders affect more than a billion people (1). Individuals, families, and society may be subject to daily burdens and serious loss when people with mental illness do not receive proper treatment. In Taiwan, people with mental disorders have a higher mortality rate than the general population (2). The number of outpatients and inpatients (including emergency room visits) is rising every year, as are healthcare costs (3–8). The damage caused by mental illness to the social life and productivity of the patient is huge. Mental pain can be worse than physical pain; it is difficult to tolerate.
People with mental illness often experience social barriers due to stigma, culture, and negative perceptions (9). They experience higher rates of poverty and unemployment (10). Long-term isolation may cause the patient's social functions to deteriorate. They may lack of sense of reality, or have increased feelings of inferiority and dependence, which make it more difficult to recover (11). After the de-institutionalization movement in United States in the 1970's, society paid more attention to psychiatric rehabilitation and recovery (12, 13). In Taiwan, by 2007, the Mental Health Act Amendment encourage patient to return and stay in the community and the primary goal is supporting the patients to live normally in the community (14).
Outpatient care is the most common treatment for many mental health problems. However, patients with mental illness who live in the community may relapse at any time with the sudden onset of severe psychotic symptoms, impaired mental function, fluctuating symptoms, or the inability to make accurate judgments, all of which bring an increased risk of self-harm as well as of suicide (15–17). If a patient is in danger of harming him or herself or others, a consultation with a mental health professional may be needed to determine whether the patient needs the more intensive care that comes with inpatient treatment. The longer a severe mental illness goes untreated, the more damage the illness can cause (18, 19).
Public health nurses play a major role in community mental health visiting services for patients with mental disorders in Taiwan. Public health nurses need to be good communicators and critical thinkers, and they have to be able to manage multiple priorities, especially in preventive and therapeutic psychiatry (20–24). A quality therapeutic relationship between the healthcare provider and a patient with mental illness is critical to successful treatment. It is also a reliable predictor of clinical outcomes (25). Patients' understanding of their own status through public health nurses can increase their awareness of their condition, which can effectively allow them to recognize and accept the progress of their disease, and help them to seek medical care when needed to reduce damage and stabilize their condition (26, 27). Furthermore, nurse-delivered interventions, such as case management, telephone and in-person supportive contact, problem-solving, and basic psychoeducational counseling can improve patients' depression, anxiety, physical and social functions, medication compliance, and life satisfaction (28, 29).
The literature shows that compulsory treatment reduces the number of days of hospitalization and frequency of psychiatric readmission, and it increases usage of community services and treatment adherence (30). Involuntary treatment and care that involves the use of coercive measures is a common psychiatry practice, both for protecting the safety of patients and the community, and for therapeutic reasons (31, 32). Such measures are essential in preventing a person at risk from endangering themselves or causing harm to others. Although coercive measures have always been a psychiatric treatment tool, the ethical dilemma between patient dignity and the use of therapeutic coercive measures remains a contentious issue in mental health research and practice (33, 34).
The Ministry of Health and Social Welfare in Taiwan established legal guidelines to regulate the compulsory treatment of people with mental disorders (35). Compulsory treatment consists of a standard operating procedure for escorting psychiatric patients living in the community to medical treatment when it is needed. Through the trilogy of identify, coordinate, and escort to hospital, community members can assist people with suspected mental illness or psychiatric patients who have harmed themselves or others in seeking medical support. After obtaining supporting evidence from a public health nurse that the notified person is a mental patient, the next steps are to clarify the level of risk to the patient or community, identify how best to assist, and determine whether an emergency escort to a medical facility is required.
Case management
The literature shows that nurse-led case management of mental health promotion interventions are feasible, acceptable, and have sustained impact. Nurse-led care can effectively improve patient outcomes, reduce the use of expensive health care, and enhance clinical practice among home care providers (36). Case management originated in the United States in the 1950's and was first used with cases involving mental health problems. It was then mostly used to coordinate community services in caring for patients with high cost high-risk health problems (37). The case management model is an effective method in a primary care setting to improve medication adherence in patients with mental disorders (38, 39). It can reduce emergency room visits, readmissions, and the length of hospital stays (40, 41), and it improves clinical indicators and the satisfaction of the patients (42). Frontline medical staff such as public health nurses are often asked to manage cases. They can have a vital role in education, identification of health problems, and modification of health behavior through home visits.
In Taiwan's public health system, case management is one of the main tasks of the nursing staff. The purpose of case management is to improve the quality of care and clinical outcomes of the case, and to reduce inappropriate admissions, as well as the time spent in crisis and the length of the hospital stay. Good case management can also reduce resource utilization while ensuring the continuity of care and cost control. Thus, quality of care, length of hospital stay, resource utilization, the necessity of continuous care, and cost are all important indicators for the evaluation of case management (15, 43–45).
Little attention has been paid to whether home visits can predict the patient's need for an emergency medical escort (any visit to an emergency room accompanied by police or emergency medical technician). Several studies have identified specific risk factors for psychosis such as positive symptoms (46, 47). Rapid assessment of a person's mental state can be carried out in four dimensions: affect, behavior, cognition, and drive (48, 49). When public health nurses visit a patient in the community, they focus on risk assessment, not just symptom assessment. They are often exposed to complex and controversial emergency mental health issues. They must rely on their own competence to identify the early warning signs of mental illness in conjunction with current symptoms, and then they need to be able to take action to reduce a patient's likelihood of self-harm, or manage aggressive or violent behavior. In this way, public health nurses can reduce the need for an emergency medical escort and emergency room visits. In this study, we examine whether the change in a patient's illness severity as identified through home visits by public health nurses can predict the need for subsequent emergency medical escort services.
Method
In Taiwan, Community Care Services for Psychiatric Patients is a specific measure taken by the government to build a social safety net. The Ministry of Health and Welfare promulgated “Key Points of Community Home Visits for People with Mental Health Disorders,” which specifies that people with mental health illness must be enrolled in the Psychiatric Care Information Management System for care management. Public health nurses act as case managers and provide home visits combined with telephone interviews. Public health nurses can adjust visit frequency according to the grade of care from monthly to annually.
The Research Ethics Committee at the National Taiwan Normal University (202106HS013) and the Institutional Review Board of New Taipei City (1116360736) reviewed and approved the study protocol.
We used secondary data from the Psychiatric Care Information Management System to evaluate patient care by public health nurses. This study is not registered for clinical trials. Patients include those discharged from hospitals, released from prison, and those assigned by the health department supervisor. After visiting a patient who is newly assigned through the Psychiatric Care Information Management System, public health nurses key in nursing records including the patient's personal information, medical history, and health status. We used these records to composite our study sample.
Data refinement and analysis
We identified a total of 500 patients who received home visiting services by public health nurses due to a mental health illness in a district of the New Taipei City in Taiwan from 2018 to 2019 in the Psychiatric Care Information Management System. Each patient was retrospectively reviewed for medical records in 2 years. We excluded 33 patients from the study because they either moved out of the city or contracted another disease in 2018–2019. We excluded an additional 21 patients with incomplete records. A total of 425 patients were included in the study.
We focused on nine independent variables: gender, age, education, diagnosis, degree of disability, classification of major illness, the nurse's reported change in the intensity of care for the patient (visit frequency), and the nurse's reported change in the severity of illness of the patient. We defined the outcome variable, emergency escort, as any visit to an emergency room accompanied by police or emergency medical technician, including an observation stay that did not result in admission. We defined the severity of mental health illness according to Taiwan's Mental Health Act: patients who demonstrate strange thoughts and unusual behavior that are out of touch with reality so that they cannot handle their own affairs, and whose diagnosis is confirmed by a psychiatrist. which is categorized from. The grade is determined based on five dimensions: positive symptoms, life dysfunctions, psychological disturbance, patient care by primary caregivers, and medical adherence. Each dimension can be scored from 1 (none) to 4 (very serious). There are four home visit frequency based on the total score: 0 to 4 (grades 1), 5 to 8 (grade 2), 9 to 14 (grade 3), and 15 to 20 (grade 4). When scores assessed increase or decrease, the public health nurse change the home visit frequency to higher or lower grades, respectively.
We used SPSS 22.0 statistical software to manage the data and perform the statistical analyses. Missing data were all excluded from the analysis. We applied Chi-square tests to examine the bivariate associations related to the use of emergency medical escort services. F-test for logistic regression is significant which fits the assumption. Thus, we used multiple logistic regressions to predict the need for an emergency medical escort through social demographics and the records provided by the public health nurses.
Results
Sociodemographic characteristics
Of the 425 patients, 238 (56%) were female and 187 (44%) were male. Their ages ranged from 16 to 86 years, with a mean of 47.6 years old. 44% had only a junior school education or below. Schizophrenia was the most prevalent diagnosis (48%), followed by bipolar affective psychosis (33%). A total of 28, 32, and 7% were assessed as mild, moderate and severe functional impairment, respectively according to the International Classification of Functioning, Disability, and Health (ICF). The most severe cases were mainly diagnosed with schizophrenia.
Use of emergency medical escorts by demographics
The distribution of use of emergency medical escort services was as follows: a total of 57 emergency medical escorts for 33 (7.8%) persons, of which 19 (4.5%) were escorted to an emergency room once, eight (1.9%) went twice, four (0.9%) went thrice, one (0.2%) went four times, and one (0.2%) went six times. In terms of gender, 19 males (57.6%) and 14 females (42.4%) required emergency medical escorts. One person (3%) was under 19 years old, eight people (24.2%) were 20–34 years old, 18 (54.6%) people were 35–49 years old, and six (18.2%) were 50–64 years old. No one was over 65 years old. For education, 11 (30%) had a junior high school education, 15 (45.6%) had completed high school, and seven (21.2%) completed college. Thirteen persons (39.4%) were classified as disabled, and 18 (54.5%) were classified with major illness. Of the patients who required emergency medical escorts, 17 (51.5%) were diagnosed with schizophrenia with 26 visits to the emergency room, and 10 (30.3%) had bipolar disorder with 19 visits. Their diagnoses were as classified by The International Statistical Classification of Diseases and Related Health Problems 9th Revision (ICD-9). No significant difference in emergency escort use was found for gender, age, education, diagnosis, degree of disability, or classification of illness.
Prediction of the need for an emergency medical escort
We found significant differences between groups that differed in terms of the nurse's reported change in intensity of case management care (worsening assessment) (32.4%) (χ2 = 36.53, p < 0.05), and for the nurse's reported severity of illness (31.8%) (χ2 = 18.74, p < 0.05) (see Table 1).
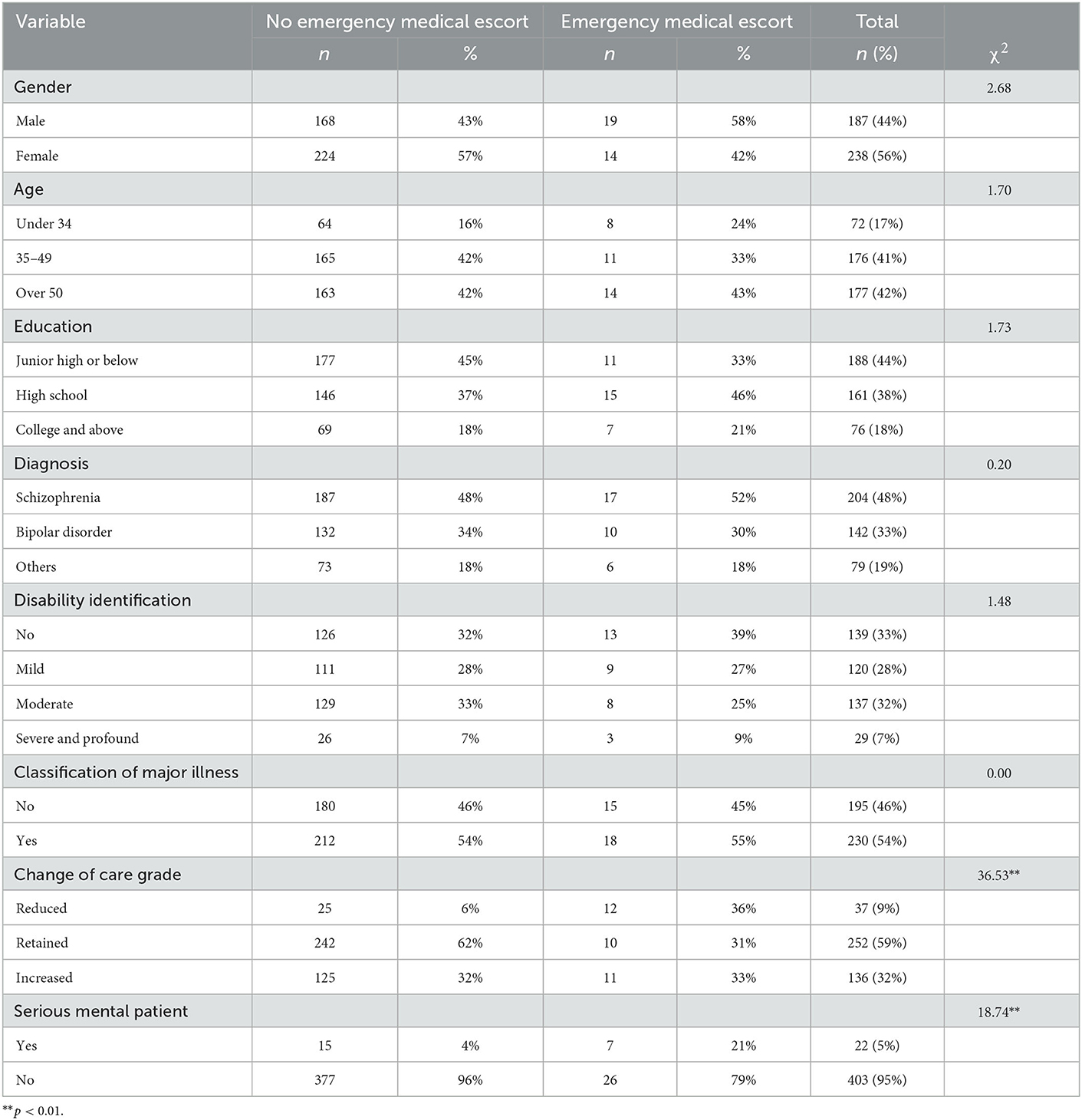
Table 1. The relationship between sociodemographic variables of people with mental illness in a district of a city and use emergency medical escort from 2018 to 2019.
Regardless of the type of visit by the public health nurse (home or telephone calls to patients or their family members), these groups did not have a statistically significant difference in the use of emergency medical escort services. According to the multiple logistic regression analysis, an increase in the intensity of case management care (OR = 6.99; 95% CI: 1.36–35.87) or in the reported severity of illness (OR = 12.91; 95% CI: 2.06–81.06) were significant predictors of the need for emergency escort services (see Table 2).
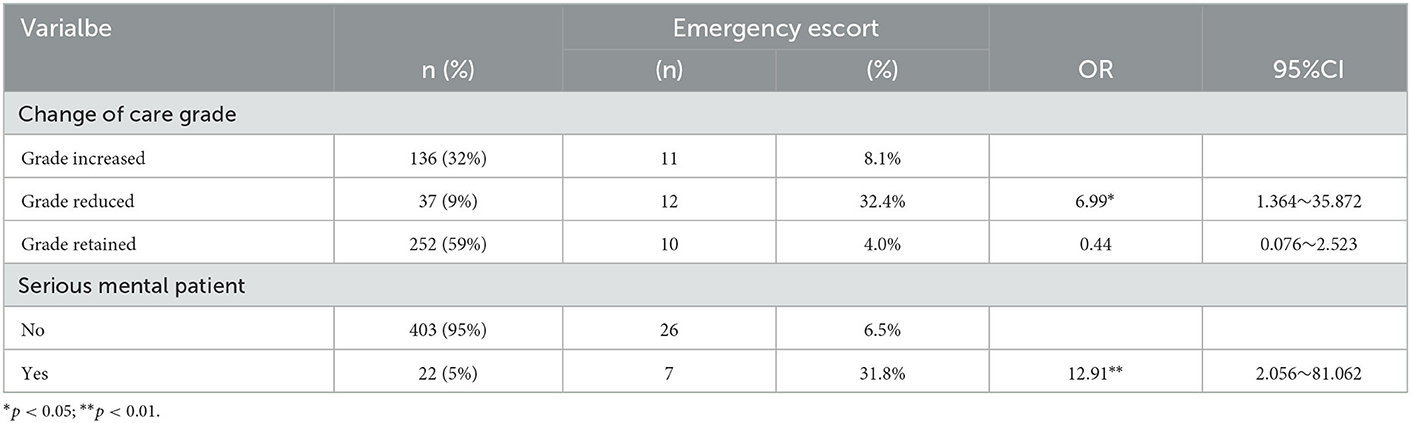
Table 2. Prediction of emergency medical escorts for people with mental illness in a district of a city located in North Taiwan from 2018 to 2019 using the logistic regression.
Discussion
This is one of the few studies to examine the relationship between emergency medical escort and home visiting services by public health nurses in patient with mental disorder. The finding is consistent with our hypothesis that patients who required to increase home visiting services were associated with an emergency medical escort. This result indicated that the public health nurses play an important role for the assessment patient conditions and provided crisis intervention for patients with mental disorder who live in community. This information may be of use in the development of a suitable strategy for managing these emergency services. This is consistent with a previous study showed that patients with psychosis attempts that increased risk for involuntary treatment in Taiwan (50). When patients who increased home visiting services indicated that the symptoms of psychosis conditions change for the worse. This suggests that public health nurse is a qualified evaluator in identifying the disease progress in early stages to prevent emergency escort to involuntary treatment or relapse of mental illness. A public health nurse with knowledge and skills and a professional manner can use telephone visits, home visits, or office visits to manage patients and to assess patient and family risk profiles. The benefit of being able to predict the need for medical escort services outweighs the cost of frequent home visits.
Community-based case management provided by nurses can improve patients' depression, anxiety, physical and social function, and improve their clinical indicators (29, 42). Mental health education in primary care settings, such as home visits and proactive strategies, can strengthen community and national mental care policies (51). Other researchers have pointed out that expanding home visits to high-risk groups improves medical comorbidities, and reduces readmissions within the year, alcohol use disorders, and bipolar disorder (52) and they can significantly lower medical expenditures and reduce the utilization rate of emergency departments and hospitalization (53). In Japan, the spread of home-visit care services for people with mental illness is now growing rapidly, and research shows that community psychiatric care can improve quality of life for patients and their families (54). High-intensity case management intervention requires a small caseload, regular follow-up, and multidisciplinary/interorganizational care planning. Community-based psychosocial interventions may have a favorable influence on clinical outcomes, including improved functioning; reduced hospital admissions, length of stay, emergency department visits, and health care costs; and increased patient motivation, self-management, care coordination, and efficacy of referral (55, 56). Public health nurses play a vital role in community mental health care. Patients with complex care needs can benefit the most (22, 57). When a public health nurse finds that the risk of a sudden onset of psychotic behavior is increasing, adjusting the visit frequency and early intervention are essential.
The finding indicated that to identify symptoms early and change the level of care can be integrated with different but complementary detection approaches across the community, primary, and secondary care (58). Coordinated care can improve patient outcomes during transitions, longitudinal high-risk care management, and unplanned acute episodic care (59). Health care administration and social welfare departments need to cooperate with family members to provide active public mental health care services, prevent mental illness, reduce the occurrence of community nuisance cases, reduce the burden on caregivers, and improve care satisfaction (60–62).
A study by Danish academics identified predictors of high psychiatric emergency room usage, which included mental illness, substance abuse, and shelter residence (63). However, the notification process of patients with severe mental illness is cumbersome. It is difficult to identify just who qualifies as a person with severe mental illness because psychiatrists may differ in opinion. Omissions or ignored reports by psychiatrists are possible, and more research is needed.
Contrary to previous research (64, 65), we found no association with gender or age and use of emergency escort services. However, male and younger patients had the highest proportion of emergency escorts, which is in line with studies conducted in Ethiopia and Australia (66, 67). Public health nurses need greater awareness and vigilance to identify and proactively discover high-risk groups to take precautions.
Limitations
There are a few limitations. This study adopts a retrospective medical record design and used the Psychiatric Care Information Management System database for analysis. Public health nurses manually entered the content of the database. There may be misplaced, inconsistent, or insufficient data entry and the authenticity of the data cannot be verified. Data used in this study were confined to a particular district in one city, which may limit its representativeness to the rest of the population and limit utility of inference based on the results.
Conclusions
For people with mental illness living in the community, changes in the intensity of care or in the severity of illness as reported by a public health nurse may have predictive power for the use of emergency medical escort services. This result supports the value of home visits and psychiatric care in the community. Public health nurses play an important role in community mental health care. When a public health nurse finds that the risk of the sudden onset of psychotic behavior is increased, it is necessary to take early intervention, such as assurance of medical adherence or schedule an inpatient visit as soon as possible.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Author contributions
M-CW and TS-HL designed the study and drafted the manuscript. M-CW collected and cleaned data. M-CW and C-CH performed the statistical computations and prepared the results. C-CH and TS-HL provided intellectual interpretation and conclusion. All authors drafted parts of the manuscript and approved the final manuscript.
Funding
This article was subsidized by the National Taiwan Normal University (NTNU), Taiwan, ROC. This work was financially supported by the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.
Acknowledgments
We are grateful to the patients.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rehm J. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatr Rep. (2019) 21:10. doi: 10.1007/s11920-019-0997-0
2. Department of Statistics of the Ministry of Health Welfare Taiwan. Naitonal Statistics for the International Day of Persons with Disabilities (2019). Available online at: https://dep.mohw.gov.tw/DOS/mp-113.html
3. Christensen MK, Lim CCW, Saha S, Plana-Ripoll O, Cannon D, Presley F, et al. The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci. (2020) 29:e161. doi: 10.1017/s204579602000075x
4. Doran CM, Kinchin I. A review of the economic impact of mental illness. Aust Health Rev. (2019) 43:43–8. doi: 10.1071/ah16115
5. Hazlett SB, McCarthy, ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to U.S. emergency departments. Acad Emerg Med. (2004) 11:193–5. doi: 10.1111/j.1553-2004,tb01434.x
6. Lang HC, Su TP. The cost of schizophrenia treatment in Taiwan. Psychiatr Serv. (2004) 55:928–30. doi: 10.1176/appi.ps.55.8.928
7. Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders: Do our societies react appropriately to the burden of mental disorders? EMBO Rep. (2016) 17:1245–9. doi: 10.15252/embr.201642951
8. Wang HH, Chang CM, Chang SS, Yang AC, Liu YH, Liao SC, et al. 10-year trends in depression care in Taiwan. J Formos Med Assoc. (2022) 011:2. doi: 10.1016/j.jfma.2022.02.011
9. Alissa NA. Social barriers as a challenge in seeking mental health among Saudi Arabians. J Educ Health Promot. (2021) 10:143–143. doi: 10.4103/jehp.jehp_819_20
10. Ridley, M, Rao G, Schilbach F, Patel V Poverty, depression, and anxiety: causal evidence and mechanisms. Science. (2020) 370:0214. doi: 10.1126./science.aay0214
11. McInerney SJ, Finnerty S, Walsh E, Spelman L, Edgar NE, Hallahan B, et al. Quality of life and social functioning of former long-stay psychiatric patients transferred into the community: a 10 year follow up study. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:795–801. doi: 10.1007/s00127-018-1520-3
12. Drake RE. The future of psychiatric rehabilitation. Epidemiol Psychiatr Sci. (2017) 26:209–10. doi: 10.1017/S2045796016000913
13. Freudenreich O. Psychiatric Rehabilitation and Recovery. In O. Freudenreich (Ed.), Psychotic Disorders: A Practical Guide. Springer International Publishing (2020) (pp. 323-334). doi: 10.1007./978-3-030-29450-2_24
14. Hsu W-T, Wu H-C, Chou F. A history of mental health laws in Taiwan. Taiwanese J Psychiatr. (2017) 31:195–203.
15. Liu F, Chen J, Du Y, Jiang W, Gong L, Mu J. Misidentification of acute psychiatric symptoms in the emergency room: Clinical experience in China. Front Psychiatry. (2021) 11:579484. doi: 10.3389/fpsyt.2020.579484
16. Mulligan O, Tan WT, Lowry G, Adamis D. Cognitive dysfunction in acute psychosis. Eur Psychiatry. (2017) 41:S745. doi: 10.1016/j.eurpsy011379
17. Taylor P, Hutton P, Wood L. Are people at risk of psychosis also at risk of suicide and self-harm? A systematic review and meta-analysis. Psychol Med. (2014) 1–16. doi: 10.1017./S0033291714002074
18. Thornicroft G, Becker T, Holloway F, Johnson S, Leese M, McCrone P, et al. Community mental health teams: evidence or belief? Br J Psychiatry J Mental Sci. (1999) 175:508–13. doi: 10.1192/bjp.175.6.508
19. Thornicroft G, Deb T, Henderson C. Community mental health care worldwide: current status and further developments. World Psychiatry. (2016) 15:276–86. doi: 10.1002/wps.20349
20. Huang XY, Ma WF, Shih HH, Li HF. Roles and functions of community mental health nurses caring for people with schizophrenia in Taiwan. J Clin Nurs. (2008) 17:3030–40. doi: 10.1111/j.1365-2008,02426.x
21. Kennedy CW, Polivka BJ, Chaudry R. Public health nurses' role in the care of adults with mental disabilities. Psychiatr Serv. (1997) 48:514–7. doi: 10.1176/ps.48.4.514
22. May SY, Clara N, Khin OK, Mar WW, Han AN, Maw SS, et al. Challenges faced by community health nurses to achieve universal health coverage in Myanmar: a mixed methods study. Int J Nurs Sci. (2021) 8:271–8. doi: 10.1016/j.ijnss.05003
23. Spohn E, Warinner A. The public health nurse in preventive and therapeutic psychiatry. Am J Orthopsych. (2010) 21:285–91. doi: 10.1111/j.1939-0025.1951.tb06102.x
24. Svensson B, Bjorkman T. The role of the nurse in community psychiatry. Med Arh. (1999) 53:153–7.
25. Blanka Kores, P. (2016). Relationship between a Doctor and a Patient with Mental Disorder. Medicine, Law andamp; Society, 9(1). doi: 10.18690/24637955.9.1.11-19(2016)
26. Bitter I, Fehér L, Tényi T, Czobor P. Treatment adherence and insight in schizophrenia. Psychiatr Hung. (2015) 30:18–26.
27. Lysaker PH, Pattison ML, Leonhardt BL, Phelps S, Vohs JL. Insight in schizophrenia spectrum disorders: relationship with behavior, mood and perceived quality of life, underlying causes and emerging treatments. World Psychiatry. (2018) 17:12–23. doi: 10.1002/wps.20508
28. Armijo J, Mendez E, Morales R, Schilling S, Castro A, Alvarado R, et al. Efficacy of community treatments for schizophrenia and other psychotic disorders: a literature review. Front Psychiatry. (2013) 4:116. doi: 10.3389/fpsyt.2013.00116
29. Halcomb EJ, McInnes S, Patterson C, Moxham L. Nurse-delivered interventions for mental health in primary care: a systematic review of randomized controlled trials. Fam Pract. (2019) 36:64–71. doi: 10.1093/fampra/cmy101
30. Barnett P, Matthews H, Lloyd-Evans B, Mackay E, Pilling S, Johnson S, et al. Compulsory community treatment to reduce readmission to hospital and increase engagement with community care in people with mental illness: a systematic review and meta-analysis. Lancet Psychiatry. (2018) 5:1013–22. doi: 10.1016/s2215-0366(18)30382-1
31. McLaughlin P, Giacco D, Priebe S. Use of coercive measures during involuntary psychiatric admission and treatment outcomes: data from a prospective study across 10 European countries. PLoS ONE. (2016) 11:e0168720. doi: 10.1371/journal.pone.0168720
32. Sashidharan SP, Mezzina R, Puras D. Reducing coercion in mental healthcare. Epidemiol Psychiatr Sci. (2019) 28:605–12. doi: 10.1017/S2045796019000350
33. Luciano M, Sampogna G, Del Vecchio V, Pingani L, Palumbo C, De Rosa C, et al. Use of coercive measures in mental health practice and its impact on outcome: a critical review. Expert Rev Neurotherap. (2014) 14:131–41. doi: 10.1586/14737175.2014.874286
34. Mitrossili M. Involuntary treatment of mental patients in the community: legal and ethical dilemmas. Psychiatriki. (2014) 25:285–92.
35. Shen GC, Eaton J, Snowden LR. Mainstreaming Mental Health Care In 42 Countries. Health Sys Reform. (2017) 3:313–24. doi: 10.1080/23288604.2017.1356424
36. Markle-Reid M, McAiney C, Forbes D, Thabane L, Gibson M, Browne G, et al. An interprofessional nurse-led mental health promotion intervention for older home care clients with depressive symptoms. BMC Geriatr. (2014) 14:62. doi: 10.1186/1471-2318-14-62
37. Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: a review of research on case management. Schizophr Bull. (1998) 24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314
38. Gensichen J, Beyer M, Muth C, Gerlach FM, Von Korff M, Ormel J. Case management to improve major depression in primary health care: a systematic review. Psychol Med. (2006) 36:7–14. doi: 10.1017/S0033291705005568
39. Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RCM, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. (2012) 157:785–95. doi: 10.7326/0003-4819-157-11-201212040-00538
40. Doménech-Briz V, Gómez Romero R, de Miguel-Montoya I, Juárez-Vela R, Martínez-Riera JR, Mármol-López MI, et al. Results of nurse case management in primary heath care: bibliographic review. Int J Environ Res Public Health. (2020) 17:9541. doi: 10.3390/ijerph17249541
41. Joo JY, Liu MF. Case management effectiveness in reducing hospital use: a systematic review. Int Nurs Rev. (2017) 64:296–308. doi: 10.1111/inr.12335
42. Joo JY, Huber DL. An integrative review of nurse-led community-based case management effectiveness. Int Nurs Rev. (2014) 61:14–24. doi: 10.1111/inr.12068
43. Dieterich M, Irving CB, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev. (2010) 10:Cd007906. doi: 10.1002/14651858.CD007906.pub2
44. Grover CA, Sughair J, Stoopes S, Guillen F, Tellez L, Wilson TM, et al. Case management reduces length of stay, charges, and testing in emergency department frequent users. West J Emerg Med. (2018) 19:238–44. doi: 10.5811/westjem.934710
45. Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. (2013) 44:717–29. doi: 10.1016/j.jemermed.08035
46. Joa I, Bjornestad J, Johannessen JO, Langeveld J, Stain HJ, Weibell M, et al. Early detection of ultra high risk for psychosis in a Norwegian catchment area: the two year follow-up of the prevention of psychosis study. Front Psychiatry. (2021) 12:193. doi: 10.3389/fpsyt.2021.573905
47. Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. (2010) 67:241–51. doi: 10.1001/archgenpsychiatry.2009.206
48. Shi J, Yao Y, Zhan C, Mao Z, Yin F, Zhao X, et al. The relationship between big five personality traits and psychotic experience in a large non-clinical youth sample: the mediating role of emotion regulation. Front Psychiatry. (2018) 648.
49. Wilt J, Revelle W. Affect, behaviour, cognition and desire in the Big Five: An analysis of item content and structure. Eur J Pers. (2015) 29:478–97. doi: 10.1002/per.2002
50. Schmitz-Buhl M, Gairing SK, Rietz C. A retrospective analysis of determinants of involuntary psychiatric in-patient treatment. BMC Psychiatry. (2019) 19:127. doi: 10.1186/s12888-019-2096-5
51. Nóbrega MPS, Venzel CMM, Sales ES, Próspero AC. Mental Health Nursing Education in Brazil: Perspectives for Primary Health Care. Texto & Contexto-Enfermagem (2020). p. 29. doi: 10.1590/1980-265X-TCE-2018-0441
52. Edgcomb JB, Sorter M, Lorberg B, Zima BT. Psychiatric readmission of children and adolescents: A systematic review and meta-analysis. Psychiatr Serv. (2020) 71:269–79. doi: 10.1176/appi.ps.201900234
53. Ruiz S, Snyder LP, Rotondo C, Cross-Barnet C, Colligan EM, Giuriceo K, et al. Innovative home visit models associated with reductions in costs, hospitalizations, and emergency department use. Health affairs (Project Hope). (2017) 36:425–32. doi: 10.1377/hlthaff.2016.1305
54. Kayama M, Setoya N, Doyle C. Expanding use of nurse home visiting for community psychiatric care in Japan. Psychiatric Quarterly. (2020) 91:571–6. doi: 10.1007/s11126-020-09721-w
55. Asher L, Patel V, Silva De MJ. Community-based psychosocial interventions for people with schizophrenia in low and middle-income countries: systematic review and meta-analysis. BMC Psychiatry. (2017) 17:355. doi: 10.1186/s12888-017-1516-7
56. Hudon C, Chouinard MC, Pluye P, El Sherif R, Bush PL, Rihoux B, et al. Characteristics of case management in primary care associated with positive outcomes for frequent users of health care: a systematic review. Annals Family Med. (2019) 17:448–58. doi: 10.1370/afm.2419
57. Morales D. R. Z., Moreno J. R. C. The mental health recovery model and its importance for Colombian nursing. Revista Colombiana de Psiquiatría. (2020) 49:305–10. doi: 10.1016/j.rcpeng.10007
58. Fusar-Poli P, Sullivan SA, Shah JL, Uhlhaas PJ. Improving the detection of individuals at clinical risk for psychosis in the community, primary and secondary care: an integrated evidence-based approach [Review]. Front Psychiatry. (2019) 10:774. doi: 10.3389./fpsyt.2019.00774
59. Clarke JL, Bourn S, Skoufalos A, Beck EH, Castillo DJ. An innovative approach to health care delivery for patients with chronic conditions. Popul Health Manag. (2017) 20:23–30. doi: 10.1089/pop.2016.0076
60. Cheng JF, Huang XY, Lin MJ, Wang YH, Yeh TP. The influence of a mental health home visit service partnership intervention on the caregivers' home visit service satisfaction and care burden. J Clin Nurs. (2018) 27:e668–77. doi: 10.1111/jocn.14123
61. Gabet M, Grenier G, Cao Z, Fleury MJ. Implementation of three innovative interventions in a psychiatric emergency department aimed at improving service use: a mixed-method study. BMC Health Serv Res. (2020) 20:854. doi: 10.1186/s12913-020-05708-2
62. Jackson-Triche ME, Unützer J, Wells KB. Achieving mental health equity: collaborative care [Review Article]. Psychiatric Clinics of North America. (2020) 43:501–10. doi: 10.1016/j.psc.05008
63. Aagaard J, Aagaard A, Buus N. Predictors of frequent visits to a psychiatric emergency room: a large-scale register study combined with a small-scale interview study. Int J Nurs Stud. (2014) 51:1003–13. doi: 10.1016/j.ijnurstu.11002
64. Saini P, McIntyre J, Corcoran R, Daras K, Giebel C, Fuller E, et al. Predictors of emergency department and GP use among patients with mental health conditions: a public health survey. Br J Gen Pract. (2020) 70:e1–8. doi: 10.3399/bjgp19X707093
65. Santo L, Peters ZJ, DeFrances CJ. Emergency department visits among adults with mental health disorders: United States, 2017–2019. NCHS Data Brief. (2021) 426:1–8.
66. Araya T, Ebnemelek E, Getachew R. Prevalence and associated factors of aggressive behavior among patients with schizophrenia at ayder comprehensive specialized hospital, Ethiopia. Biomed Res Int. (2020) 2020:7571939–7571939. doi: 10.1155/2020/7571939
Keywords: public health nurse, home visit, case management, mental disorder, emergency escort, community
Citation: Wu M-C, Hung C-C, Fang S-C and Lee TS-H (2023) Change of home visit frequency by public health nurses predicts emergency escorts for psychiatric patients living in the community: A retrospective medical record review. Front. Public Health 11:1066908. doi: 10.3389/fpubh.2023.1066908
Received: 11 October 2022; Accepted: 17 January 2023;
Published: 09 February 2023.
Edited by:
Julian Schwarz, Brandenburg Medical School Theodor Fontane, GermanyReviewed by:
María Isabel Mármol-López, Universitat de València, SpainLi-Chung Pien, Taipei Medical University, Taiwan
Copyright © 2023 Wu, Hung, Fang and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tony Szu-Hsien Lee,  dG9ueWxlZUBudG51LmVkdS50dw==
dG9ueWxlZUBudG51LmVkdS50dw==
†These authors have contributed equally to this work
 Meng-Chieh Wu1†
Meng-Chieh Wu1† Su-Chen Fang
Su-Chen Fang Tony Szu-Hsien Lee
Tony Szu-Hsien Lee